Tumor Budding Should Be in Oral Cavity Cancer Reporting: A Retrospective Cohort Study Based on Tumor Microenvironment
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
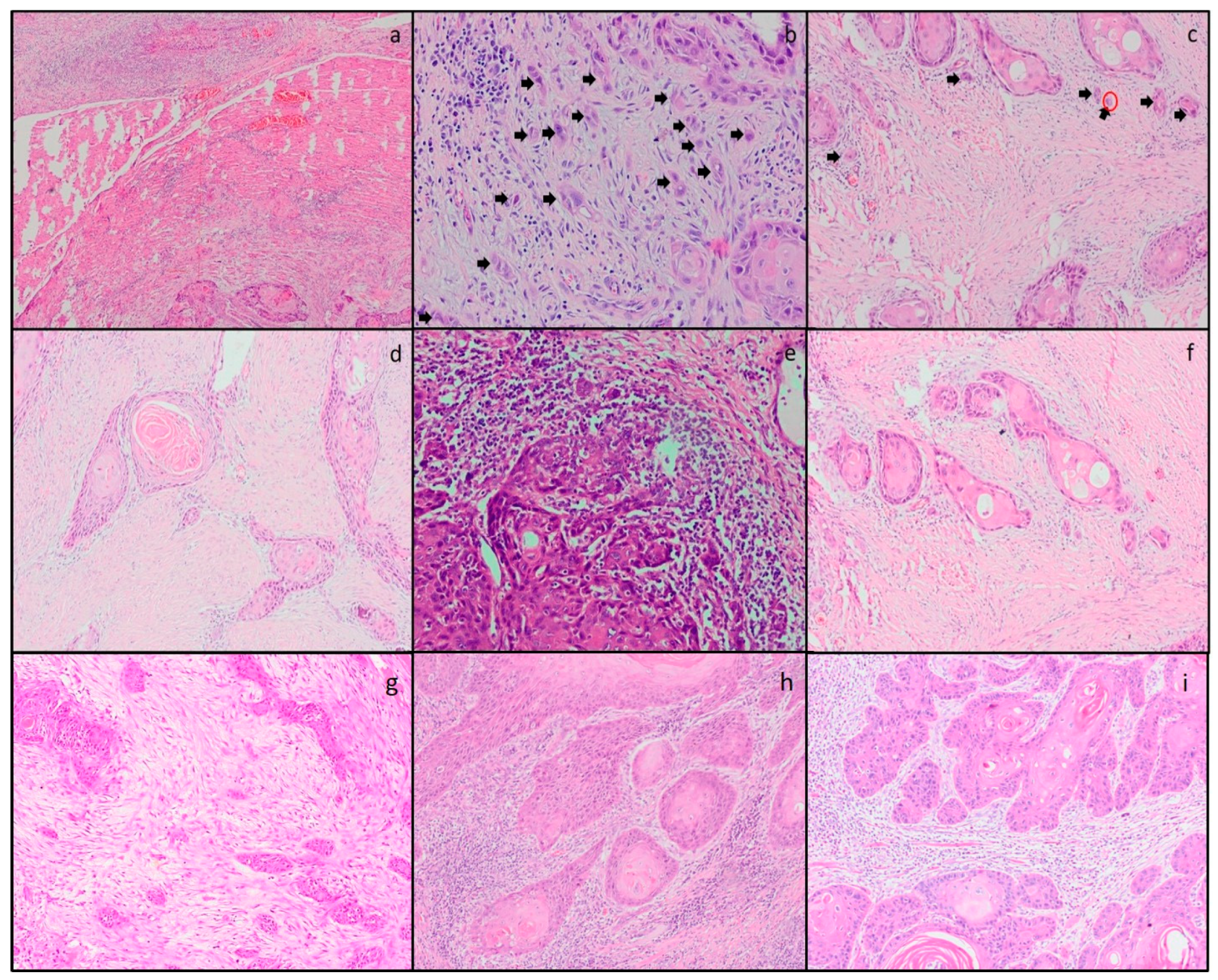
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Muller, S.; Tilakaratne, W.M. Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Tumours of the Oral Cavity and Mobile Tongue. Head Neck Pathol. 2022, 16, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009, 45, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, B.Y.; Chang, S.C.; Hashibe, M.; La Vecchia, C.; Zhang, Z.F. Alcohol consumption and cancers of the oral cavity and pharynx from 1988 to 2009: An update. Eur. J. Cancer Prev. 2010, 19, 431–465. [Google Scholar] [CrossRef]
- Gillison, M.L.; Chaturvedi, A.K.; Anderson, W.F.; Fakhry, C. Epidemiology of Human Papillomavirus-Positive Head and Neck Squamous Cell Carcinoma. J. Clin. Oncol. 2015, 33, 3235–3242. [Google Scholar] [CrossRef] [PubMed]
- Pilborough, A.E.; Lambert, D.W.; Khurram, S.A. Extranodal extension in oral cancer: A role for the nodal microenvironment? J. Oral Pathol. Med. 2019, 48, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Brandwein-Gensler, M.; Teixeira, M.S.; Lewis, C.M.; Lee, B.; Rolnitzky, L.; Hille, J.J.; Genden, E.; Urken, M.L.; Wang, B.Y. Oral squamous cell carcinoma: Histologic risk assessment, but not margin status, is strongly predictive of local disease-free and overall survival. Am. J. Surg. Pathol. 2005, 29, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Lugli, A.; Kirsch, R.; Ajioka, Y.; Bosman, F.; Cathomas, G.; Dawson, H.; El Zimaity, H.; Fléjou, J.F.; Hansen, T.P.; Hartmann, A.; et al. Recommendations for reporting tumor budding in colorectal cancer based on the International Tumor Budding Consensus Conference (ITBCC) 2016. Mod. Pathol. 2017, 30, 1299–1311. [Google Scholar] [CrossRef]
- Zare, S.Y.; Ciscato, A.; Fadare, O. Tumor budding activity is an independent prognostic factor in squamous cell carcinoma of the vulva. Hum. Pathol. 2022, 126, 77–86. [Google Scholar] [CrossRef]
- Wahab, A.; Onkamo, O.; Pirinen, M.; Almangush, A.; Salo, T. The budding and depth of invasion model in oral cancer: A systematic review and meta-analysis. Oral Dis. 2022, 28, 275–283. [Google Scholar] [CrossRef]
- Togni, L.; Caponio, V.C.A. The Emerging Impact of Tumor Budding in Oral Squamous Cell Carcinoma: Main Issues and Clinical Relevance of a New Prognostic Marker. Cancers 2022, 14, 3571. [Google Scholar] [CrossRef]
- Li, Z.W.; He, L.; Zheng, Z.; Zhang, Q.; Xu, Y.T.; Chen, J.Y.; Shi, J.; Huang, W.B.; Fan, X.S. Combined assessment of tumour cell nest size and desmoplastic reaction as an excellent prognostic predictor in oesophageal squamous cell carcinoma. Histopathology 2022, 80, 1112–1120. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, X.; Yang, J. A Novel Prognostic Stratified System Based on Tumor Budding and the Cell Nest Size in Ureter Urothelial Carcinoma. Appl. Bionics Biomech. 2022, 2022, 6988237. [Google Scholar] [CrossRef] [PubMed]
- Boxberg, M.; Kuhn, P.H.; Reiser, M.; Erb, A.; Steiger, K.; Pickhard, A.; Straßen, U.; Koob, I.; Kolk, A.; Warth, A.; et al. Tumor Budding and Cell Nest Size Are Highly Prognostic in Laryngeal and Hypopharyngeal Squamous Cell Carcinoma: Further Evidence for a Unified Histopathologic Grading System for Squamous Cell Carcinomas of the Upper Aerodigestive Tract. Am. J. Surg. Pathol. 2019, 43, 303–313. [Google Scholar] [CrossRef] [PubMed]
- Boxberg, M.; Jesinghaus, M.; Dorfner, C.; Mogler, C.; Drecoll, E.; Warth, A.; Steiger, K.; Bollwein, C.; Meyer, P.; Wolff, K.D.; et al. Tumour budding activity and cell nest size determine patient outcome in oral squamous cell carcinoma: Proposal for an adjusted grading system. Histopathology 2017, 70, 1125–1137. [Google Scholar] [CrossRef] [PubMed]
- Akimoto, N.; Väyrynen, J.P.; Zhao, M.; Ugai, T.; Fujiyoshi, K.; Borowsky, J.; Zhong, R.; Haruki, K.; Arima, K.; Lau, M.C.; et al. Desmoplastic Reaction, Immune Cell Response, and Prognosis in Colorectal Cancer. Front. Immunol. 2022, 13, 840198. [Google Scholar] [CrossRef]
- Almangush, A.; Bello, I.O.; Heikkinen, I.; Hagström, J.; Haglund, C.; Kowalski, L.P.; Nieminen, P.; Coletta, R.D.; Mäkitie, A.A.; Salo, T.; et al. Stromal categorization in early oral tongue cancer. Virchows Arch. 2021, 478, 925–932. [Google Scholar] [CrossRef]
- Almangush, A.; Alabi, R.O.; Troiano, G.; Coletta, R.D.; Salo, T.; Pirinen, M.; Mäkitie, A.A.; Leivo, I. Clinical significance of tumor-stroma ratio in head and neck cancer: A systematic review and meta-analysis. BMC Cancer 2021, 21, 480. [Google Scholar] [CrossRef]
- Mascitti, M.; Zhurakivska, K.; Togni, L.; Caponio, V.C.A.; Almangush, A. Addition of the tumour-stroma ratio to the 8th edition American Joint Committee on Cancer staging system improves survival prediction for patients with oral tongue squamous cell carcinoma. Histopathology 2020, 77, 810–822. [Google Scholar] [CrossRef]
- Heikkinen, I.; Bello, I.O.; Wahab, A.; Hagström, J.; Haglund, C.; Coletta, R.D.; Nieminen, P.; Mäkitie, A.A.; Salo, T.; Leivo, I.; et al. Assessment of Tumor-infiltrating Lymphocytes Predicts the Behavior of Early-stage Oral Tongue Cancer. Am. J. Surg. Pathol. 2019, 43, 1392–1396. [Google Scholar] [CrossRef]
- Bryne, M.; Koppang, H.S.; Lilleng, R.; Kjaerheim, A. Malignancy grading of the deep invasive margins of oral squamous cell carcinomas has high prognostic value. J. Pathol. 1992, 166, 375–381. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA A Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Almangush, A.; Heikkinen, I.; Bakhti, N.; Mäkinen, L.K.; Kauppila, J.H.; Pukkila, M.; Hagström, J.; Laranne, J.; Soini, Y.; Kowalski, L.P.; et al. Prognostic impact of tumour-stroma ratio in early-stage oral tongue cancers. Histopathology 2018, 72, 1128–1135. [Google Scholar] [CrossRef] [PubMed]
- Hendry, S.; Salgado, R.; Gevaert, T.; Russell, P.A.; John, T.; Thapa, B.; Christie, M.; van de Vijver, K.; Estrada, M.V.; Gonzalez-Ericsson, P.I.; et al. Assessing Tumor-Infiltrating Lymphocytes in Solid Tumors: A Practical Review for Pathologists and Proposal for a Standardized Method from the International Immuno-Oncology Biomarkers Working Group: Part 2: TILs in Melanoma, Gastrointestinal Tract Carcinomas, Non-Small Cell Lung Carcinoma and Mesothelioma, Endometrial and Ovarian Carcinomas, Squamous Cell Carcinoma of the Head and Neck, Genitourinary Carcinomas, and Primary Brain Tumors. Adv. Anat. Pathol. 2017, 24, 311–335. [Google Scholar] [CrossRef]
- Quinton, B.A.; Cabrera, C.I.; Tamaki, A.; Li, S.; Fowler, N.; Rezaee, R.; Lavertu, P.; Teknos, T.; Pan, Q.; Thuener, J. The impact of microscopic versus macroscopic extranodal extension in oral cavity squamous cell carcinoma: National cancer database analysis and review of the literature. Am. J. Otolaryngol. 2022, 43, 103511. [Google Scholar] [CrossRef]
- Carvalho, A.L.; Nishimoto, I.N.; Califano, J.A.; Kowalski, L.P. Trends in incidence and prognosis for head and neck cancer in the United States: A site-specific analysis of the SEER database. Int. J. Cancer 2005, 114, 806–816. [Google Scholar] [CrossRef] [PubMed]
- Pulte, D.; Brenner, H. Changes in survival in head and neck cancers in the late 20th and early 21st century: A period analysis. Oncologist 2010, 15, 994–1001. [Google Scholar] [CrossRef]
- Almangush, A.; Heikkinen, I.; Mäkitie, A.A.; Coletta, R.D.; Läärä, E.; Leivo, I.; Salo, T. Prognostic biomarkers for oral tongue squamous cell carcinoma: A systematic review and meta-analysis. Br. J. Cancer 2017, 117, 856–866. [Google Scholar] [CrossRef]
- Rodrigues, R.M.; Bernardo, V.G. How pathological criteria can impact prognosis of tongue and floor of the mouth squamous cell carcinoma. JAOS 2020, 28, e20190198. [Google Scholar] [CrossRef]
- Xu, B.; Salama, A.M.; Valero, C.; Yuan, A.; Khimraj, A.; Saliba, M.; Zanoni, D.K.; Ganly, I.; Patel, S.G.; Katabi, N.; et al. The prognostic role of histologic grade, worst pattern of invasion, and tumor budding in early oral tongue squamous cell carcinoma: A comparative study. Virchows Arch. 2021, 479, 597–606. [Google Scholar] [CrossRef]
- Almangush, A.; Bello, I.O.; Coletta, R.D.; Mäkitie, A.A.; Mäkinen, L.K.; Kauppila, J.H.; Pukkila, M.; Hagström, J.; Laranne, J.; Soini, Y.; et al. For early-stage oral tongue cancer, depth of invasion and worst pattern of invasion are the strongest pathological predictors for locoregional recurrence and mortality. Virchows Arch. 2015, 467, 39–46. [Google Scholar] [CrossRef]
- Silva, L.; Lopes, M.; Sá, M.C.; de Almeida Freitas, R.; Coletta, R.D.; da Silveira, E.J.D.; da Costa Miguel, M.C. Histopathologic grading and its relationship with outcome in oral tongue squamous cell carcinoma. J. Oral Pathol. Med. 2021, 50, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Wagner, V.P.; Webber, L.P.; Curra, M.; Klein, I.P.; Meurer, L.; Carrad, V.C.; Martins, M.D. Bryne’s grading system predicts poor disease-specific survival of oral squamous cell carcinoma: A comparative study among different histologic grading systems. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 123, 688–696. [Google Scholar] [CrossRef] [PubMed]
- Arora, A.; Husain, N.; Bansal, A.; Neyaz, A.; Jaiswal, R.; Jain, K.; Chaturvedi, A.; Anand, N.; Malhotra, K.; Shukla, S. Development of a New Outcome Prediction Model in Early-stage Squamous Cell Carcinoma of the Oral Cavity Based on Histopathologic Parameters with Multivariate Analysis: The Aditi-Nuzhat Lymph-node Prediction Score (ANLPS) System. Am. J. Surg. Pathol. 2017, 41, 950–960. [Google Scholar] [CrossRef]
- Muller, S.; Boy, S.C.; Day, T.A.; Magliocca, K.R.; Richardson, M.S.; Sloan, P.; Tilakaratne, W.M.; Zain, R.B.; Thompson, L.D.R. Data Set for the Reporting of Oral Cavity Carcinomas: Explanations and Recommendations of the Guidelines from the International Collaboration of Cancer Reporting. Arch. Pathol. Lab. Med. 2019, 143, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, D.; Bansal, V.; Malik, V.; Bhagat, R.; Punia, R.S.; Handa, U.; Gupta, A.; Dass, A. Tumor Budding and Worse Pattern of Invasion Can Predict Nodal Metastasis in Oral Cancers and Associated with Poor Survival in Early-Stage Tumors. Ear Nose Throat J. 2019, 98, E112–E119. [Google Scholar] [CrossRef] [PubMed]
- Hori, Y.; Kubota, A.; Yokose, T.; Furukawa, M.; Matsushita, T.; Oridate, N. Association between pathological invasion patterns and late lymph node metastases in patients with surgically treated clinical No early oral tongue carcinoma. Head Neck 2020, 42, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Kadota, K.; Nitadori, J.; Woo, K.M.; Sima, C.S.; Finley, D.J.; Rusch, V.W.; Adusumilli, P.S.; Travis, W.D. Comprehensive pathological analyses in lung squamous cell carcinoma: Single cell invasion, nuclear diameter, and tumor budding are independent prognostic factors for worse outcomes. J. Thorac. Oncol. 2014, 9, 1126–1139. [Google Scholar] [CrossRef]
- Regmi, P.; Paudyal, A.; Paudyal, P.; Hu, H.J.; Liu, F.; Ma, W.J.; Jin, Y.W.; Li, F.Y. Prognostic significance of tumor budding in biliary tract cancer. Eur. J. Surg. Oncol. 2022, 48, 160–168. [Google Scholar] [CrossRef]
- Jesinghaus, M.; Herz, A.L.; Kohlruss, M.; Silva, M.; Grass, A.; Lange, S.; Novotny, A.; Ott, K.; Schmidt, T.; Gaida, M.; et al. Post-neoadjuvant assessment of tumour budding according to ITBCC subgroups delivers stage- and regression-grade independent prognostic information in intestinal-type gastric adenocarcinoma. J. Pathol. Clin. Res. 2022, 8, 448–457. [Google Scholar] [CrossRef]
- Alessandrini, L.; Zanoletti, E.; Cazzador, D.; Sbaraglia, M.; Franz, L.; Tealdo, G.; Frigo, A.C.; Blandamura, S.; Nicolai, P.; Mazzoni, A.; et al. Tumor budding to investigate local invasion, metastasis and prognosis in temporal bone squamous cell carcinoma. Pathol. Res. Pract. 2022, 229, 153719. [Google Scholar] [CrossRef]
- Zhu, Y.; Liu, H.; Xie, N.; Liu, X.; Huang, H.; Wang, C.; Hou, J. Impact of tumor budding in head and neck squamous cell carcinoma: A meta-analysis. Head Neck 2019, 41, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Almangush, A.; Pirinen, M.; Heikkinen, I.; Mäkitie, A.A.; Salo, T.; Leivo, I. Tumour budding in oral squamous cell carcinoma: A meta-analysis. Br. J. Cancer 2018, 118, 577–586. [Google Scholar] [CrossRef]
- Dolens, E.D.S.; Dourado, M.R.; Almangush, A.; Salo, T.A.; Gurgel Rocha, C.A.; da Silva, S.D.; Brennan, P.A.; Coletta, R.D. The Impact of Histopathological Features on the Prognosis of Oral Squamous Cell Carcinoma: A Comprehensive Review and Meta-Analysis. Front. Oncol. 2021, 11, 784924. [Google Scholar] [CrossRef] [PubMed]
- Karjol, U.; Jonnada, P.; Annavarjula, V.; Cherukuru, S.; Chandranath, A.; Anwar, A. Prognostic Role of Tumor Budding in Carcinoma Tongue: A Systemic Review and Meta-Analysis. Cureus 2020, 12, e9316. [Google Scholar] [CrossRef]
- Bjerkli, I.H.; Laurvik, H.; Nginamau, E.S.; Søland, T.M.; Costea, D.; Hov, H.; Uhlin-Hansen, L.; Hadler-Olsen, E.; Steigen, S.E. Tumor budding score predicts lymph node status in oral tongue squamous cell carcinoma and should be included in the pathology report. PLoS ONE 2020, 15, e0239783. [Google Scholar] [CrossRef]
- Weichert, W.; Kossakowski, C.; Harms, A.; Schirmacher, P.; Muley, T.; Dienemann, H.; Warth, A. Proposal of a prognostically relevant grading scheme for pulmonary squamous cell carcinoma. Eur. Respir. J. 2016, 47, 938–946. [Google Scholar] [CrossRef] [PubMed]
- Hynes, S.O.; Coleman, H.G.; Kelly, P.J.; Irwin, S.; O’Neill, R.F.; Gray, R.T.; McGready, C.; Dunne, P.D.; McQuaid, S.; James, J.A.; et al. Back to the future: Routine morphological assessment of the tumour microenvironment is prognostic in stage II/III colon cancer in a large population-based study. Histopathology 2017, 71, 12–26. [Google Scholar] [CrossRef]
- Wang, K.; Ma, W.; Wang, J.; Yu, L.; Zhang, X.; Wang, Z.; Tan, B.; Wang, N.; Bai, B.; Yang, S.; et al. Tumor-stroma ratio is an independent predictor for survival in esophageal squamous cell carcinoma. J. Thorac. Oncol. 2012, 7, 1457–1461. [Google Scholar] [CrossRef]
- Zhang, X.L.; Jiang, C.; Zhang, Z.X.; Liu, F.; Zhang, F.; Cheng, Y.F. The tumor-stroma ratio is an independent predictor for survival in nasopharyngeal cancer. Oncol. Res. Treat. 2014, 37, 480–484. [Google Scholar] [CrossRef]
- van Pelt, G.W.; Sandberg, T.P.; Morreau, H.; Gelderblom, H.; van Krieken, J.; Tollenaar, R.; Mesker, W.E. The tumour-stroma ratio in colon cancer: The biological role and its prognostic impact. Histopathology 2018, 73, 197–206. [Google Scholar] [CrossRef]
- Dourado, M.R.; Miwa, K.Y.M.; Hamada, G.B.; Paranaíba, L.M.R.; Sawazaki-Calone, Í.; Domingueti, C.B.; Ervolino de Oliveira, C.; Furlan, E.C.B.; Longo, B.C.; Almangush, A. Prognostication for oral squamous cell carcinoma patients based on the tumour-stroma ratio and tumour budding. Histopathology 2020, 76, 906–918. [Google Scholar] [CrossRef] [PubMed]
- Pandya, P.H.; Murray, M.E.; Pollok, K.E.; Renbarger, J.L. The Immune System in Cancer Pathogenesis: Potential Therapeutic Approaches. J. Immunol. Res. 2016, 2016, 4273943. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Shao, X.; Zhang, Y.; Zhu, M.; Wang, F.X.C.; Mu, J.; Li, J.; Yao, H.; Chen, K. Role of tumor microenvironment in cancer progression and therapeutic strategy. Cancer Med. 2023, 12, 11149–11165. [Google Scholar] [CrossRef]
- Luo, W. Nasopharyngeal carcinoma ecology theory: Cancer as multidimensional spatiotemporal "unity of ecology and evolution" pathological ecosystem. Theranostics 2023, 13, 1607–1631. [Google Scholar] [CrossRef] [PubMed]
| Variable | Number of Patients (%) | |
|---|---|---|
| Age | <65 | 35 (47.9%) |
| ≥65 | 38 (52.1%) | |
| Gender | Female | 36 (49.3%) |
| Male | 37 (50.7%) | |
| Tumor localization | Tongue | 42 (57.5%) |
| Buccal mucosa | 26 (35.6%) | |
| Floor of mouth | 4 (5.5%) | |
| Palate | 1 (1.4%) | |
| Tumor size | 0–2 cm | 38 (52.1%) |
| >2 cm | 35 (47.9%) | |
| Histological grade | Well-differentiated | 11 (15.1%) |
| Moderately differentiated | 55 (75.3%) | |
| Poorly differentiated | 7 (9.6%) | |
| Depth of invasion | 0–5 mm | 32 (43.8%) |
| >5 mm | 41 (56.2%)a | |
| Surgical margin | Negative | 41 (56.2%) |
| Positive | 32 (43.8%) | |
| Perineural invasion | Absent | 55 (75.3%) |
| Present | 18 (24.7%) | |
| Lymphovascular invasion | Absent | 71 (97.3%) |
| Present | 2 (2.7%) | |
| Lymph node dissection | Absent | 18 (24.7%) |
| Present | 55 (75.3%) | |
| Lymph node metastasis | Absent | 27 (49.1%) |
| Present | 28 (50.9%) | |
| Extranodal extension | Absent | 15 (53.6%) |
| Present | 13 (46.4%) | |
| Size of extranodal extension | 0–2 mm | 8 (61.5%) |
| >2 mm | 5 (38.5%) | |
| pT | T1 | 22 (30.1%) |
| T2 | 34 (46.6%) | |
| T3 | 11 (15.1%) | |
| T4 | 6 (8.2%) | |
| pN | N0 | 45 (61.6%) |
| N1 | 5 (6.8%) | |
| N2 | 21 (28.8%) | |
| N3 | 2 (2.7%) | |
| AJCC stage | Stage I | 18 (24.7%) |
| Stage II | 24 (32.9%) | |
| Stage III | 6 (8.2%) | |
| Stage IV | 25 (34.2%) | |
| Locoregional recurrence | Absent | 54 (74%) |
| Present | 19 (26%) | |
| Distant metastasis | Absent | 67 (91.8%) |
| Present | 6 (8.2%) | |
| Variable | Number of Patients (%) | |
|---|---|---|
| Worst pattern of invasion (WPOI) | WPOI 2 | 1 (1.4%) |
| WPOI 3 | 9 (12.3%) | |
| WPOI 4 | 50 (68.5%) | |
| WPOI 5 | 13 (17.8%) | |
| Tumor budding | Absent | 20 (27.4%) |
| 1–4 buds | 26 (35.6%) | |
| 5–9 buds | 12 (16.4%) | |
| ≥10 buds | 15 (20.5%) | |
| Tumor cell nest size | >15 cells | 10 (13.7%) |
| 5–15 cells | 10 (13.7%) | |
| 2–4 cells | 20 (27.4%) | |
| Single-cell | 33 (45.2%) | |
| Tumor-stroma ratio | Stroma-poor | 26 (35.6%) |
| Stroma-rich | 47 (64.4%) | |
| Stromal lymphocyte infiltration | Low (0–30%) | 24 (32.9%) |
| Intermediate (31–60%) | 30 (41.1%) | |
| High (61–100%) | 19 (26%) | |
| Stroma type | Mature | 55 (75.3%) |
| Immature | 18 (24.7%) | |
| Variable | Worst Pattern of İnvasion | Tumor Budding | Tumor Cell Nest Size | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 4 | 5 | p | 0–4 Buds | ≥5 Buds | p | >1 Cell | Single Cell | p | |
| Age | |||||||||
| <65 | 24 (48%) | 8 (61.5%) | 0.53 | 20 (43.5%) | 15 (55.6%) | 0.34 | 18 (45%) | 17 (51.5%) | 0.64 |
| ≥65 | 26 (52%) | 5 (38.5%) | 26 (56.5%) | 12 (44.4%) | 22 (55%) | 16 (48.5%) | |||
| Gender | |||||||||
| Female | 23 (46%) | 8 (61.5%) | 0.36 | 20 (43.5%) | 16 (59.3%) | 0.23 | 18 (45%) | 18 (54.5%) | 0.48 |
| Male | 27 (54%) | 5 (38.5%) | 26 (56.5%) | 11 (40.7%) | 22 (55%) | 15 (45.5%) | |||
| Tumor size | |||||||||
| 0–2 cm | 26 (52%) | 7 (53.8%) | 1 | 25 (54.3%) | 13 (48.1%) | 0.63 | 21 (52.5%) | 17 (51.5%) | 1 |
| >2 cm | 24 (48%) | 6 (46.2%) | 21 (45.7%) | 14 (51.9%) | 19 (47.5%) | 16 (48.5%) | |||
| Depth of invasion | |||||||||
| 0–5 mm | 20 (40%) | 3 (23.1%) | 0.34 | 23 (50%) | 9 (33.3%) | 22 (55%) | 10 (30.3%) | 0.06 | |
| >5 mm | 30 (60%) | 10 (76.9%) | 23 (50%) | 18 (66.7%) | 18 (45%) | 23 (69.7%) | |||
| Histological grade | |||||||||
| Well | 6 (12%) | 0 | 0.35 | 8 (17.4%) | 3 (11.1%) | 0.12 | 8 (20%) | 3 (9.1%) | 0.18 |
| Moderately | 38 (76%) | 12 (92.3%) | 36 (78.3%) | 19 (70.4%) | 30 (75%) | 25 (75.8%) | |||
| Poorly | 6 (12%) | 1 (7.7%) | 2 (4.3%) | 5 (18.5%) | 2 (5%) | 5 (15.2%) | |||
| Surgical margin | |||||||||
| Negative | 30 (60%) | 5 (38.5%) | 0.21 | 27 (58.7%) | 14 (51.9%) | 0.63 | 24 (60%) | 17 (51.5%) | 0.48 |
| Positive | 20 (40%) | 8 (61.5%) | 19 (41.3%) | 13 (48.1%) | 16 (40%) | 16 (48.5%) | |||
| Perineural invasion | |||||||||
| Absent | 38 (76%) | 7 (53.8%) | 0.16 | 42 (91.3%) | 13 (48.1%) | <0.001 | 37 (92.5%) | 18 (54.5%) | <0.001 |
| Present | 12 (24%) | 6 (46.2%) | 4 (8.7%) | 14 (51.9%) | 3 (7.5%) | 15 (45.5%) | |||
| Lymphovascular invasion | |||||||||
| Absent | 49 (98%) | 12 (92.3%) | 0.37 | 45 (97.8%) | 26 (96.3%) | 1 | 39 (97.5%) | 32 (97%) | 1 |
| Present | 1 (2%) | 1 (7.7%) | 1 (2.2%) | 1 (3.7%) | 1 (2.5%) | 1 (3%) | |||
| Lymph node metastasis | |||||||||
| Absent | 22 (53.7%) | 1 (10%) | 0.01 | 16 (53.3%) | 11 (44%) | 0.59 | 15 (57.7%) | 12 (41.4%) | 0.28 |
| Present | 19 (46.3%) | 9 (90%) | 14 (46.7%) | 14 (56%) | 11 (42.3%) | 17 (58.6%) | |||
| Extranodal extension | |||||||||
| Absent | 10 (52.6%) | 5 (55.6%) | 1 | 11 (78.6%) | 4 (28.6%) | 0.02 | 8 (72.7%) | 7 (41.2%) | 0.21 |
| Present | 9 (47.4%) | 4 (44.4%) | 3 (21.4%) | 10 (71.4%) | 3 (27.3%) | 10 (58.8%) | |||
| Size of extranodal extension | |||||||||
| 0–2 mm | 4 (44.4%) | 1 (25%) | 1 | 2 (66.7%) | 3 (30%) | 0.51 | 2 (66.7%) | 3 (30%) | 0.51 |
| >2 mm | 5 (55.6%) | 3 (75%) | 1 (33.3%) | 7 (70%) | 1 (33.3%) | 7 (70%) | |||
| pT | |||||||||
| T1 | 14 (28%) | 3 (23.1%) | 0.21 | 16 (34.8%) | 6 (22.2%) | 0.01 | 14 (35%) | 8 (24.2%) | 0.02 |
| T2 | 25 (50%) | 4 (30.7%) | 23 (50%) | 11 (40.7%) | 21 (52.5%) | 13 (39.4%) | |||
| T3 | 8 (16%) | 3 (23.1%) | 7 (15.2%) | 4 (14.8%) | 5 (12.5%) | 6 (18.2%) | |||
| T4 | 3 (6%) | 3 (23.1%) | 0 | 6 (22.2%) | 0 | 6 (18.2%) | |||
| pN | |||||||||
| N0 | 31 (62%) | 4 (30.8%) | 0.12 | 32 (69.6%) | 13 (48.1%) | 0.02 | 29 (72.5%) | 16 (48.5%) | 0.08 |
| N1 | 4 (8%) | 1 (7.7%) | 3 (6.5%) | 2 (7.4%) | 3 (7.5%) | 2 (6.1%) | |||
| N2 | 14 (28%) | 7 (53.8%) | 11 (23.9%) | 10 (37%) | 8 (20%) | 13 (39.4%) | |||
| N3 | 1 (2%) | 1 (7.7%) | 0 | 2 (7.4%) | 0 | 2 (6.1%) | |||
| AJCC stage | |||||||||
| Stage I | 10 (20%) | 3 (23.1%) | 0.15 | 13 (28.3%) | 5 (18.5%) | 0.12 | 12 (30%) | 6 (18.2%) | 0.03 |
| Stage II | 18 (36%) | 1 (7.7%) | 17 (37%) | 7 (25.9%) | 15 (37.5%) | 9 (27.3%) | |||
| Stage III | 5 (10%) | 1 (7.7%) | 5 (10.9%) | 1 (3.7%) | 5 (12.5%) | 1 (3%) | |||
| Stage IV | 17 (34%) | 8 (61.5%) | 11 (23.9%) | 14 (51.9%) | 8 (20%) | 17 (51.5%) | |||
| AJCC stage | |||||||||
| Stage I–II | 28 (56%) | 4 (30.8%) | 0.12 | 30 (65.2%) | 12 (44.4%) | 0.09 | 27 (67.5%) | 15 (45.5%) | 0.09 |
| Stage III–IV | 22 (44%) | 9 (69.2%) | 16 (34.8%) | 15 (55.6%) | 13 (32.5%) | 18 (54.5%) | |||
| Locoregional recurrence | |||||||||
| Absent | 37 (74%) | 10 (76.9%) | 1 | 33 (71.7%) | 21 (77.78%) | 0.78 | 29 (72.5%) | 25 (75.8%) | 0.79 |
| Present | 13 (26%) | 3 (23.1%) | 13 (28.3%) | 6 (22.2%) | 11 (27.5%) | 8 (24.2%) | |||
| Distant metastasis | |||||||||
| Absent | 46 (92%) | 11 (84.6%) | 0.59 | 44 (95.7%) | 23 (85.2%) | 0.18 | 38 (95%) | 29 (87.9%) | 0.4 |
| Present | 4 (8%) | 2 (15.4%) | 2 (4.3%) | 4 (14.8%) | 2 (5%) | 4 (12.1%) | |||
| Variable | Tumor-Stroma Ratio | Stromal Lymphocyte İnfiltration | Stroma Type | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Stroma-Poor | Stroma-Rich | p | 0–30% | 31–100% | p | Mature | Immature | p | |
| Age | |||||||||
| <65 | 10 (38.5%) | 25 (53.2%) | 0.32 | 15 (62.5%) | 20 (40.8%) | 0.13 | 23 (41.8%) | 12 (66.7%) | 0.1 |
| ≥65 | 16 (61.5%) | 22 (46.8%) | 9 (37.5%) | 29 (59.2%) | 32 (58.2%) | 6 (33.3%) | |||
| Gender | |||||||||
| Female | 13 (50%) | 23 (48.9%) | 1 | 13 (54.2%) | 23 (46.9%) | 0.62 | 29 (52.7%) | 7 (38.9%) | 0.41 |
| Male | 13 (50%) | 24 (51.1%) | 11 (45.8%) | 26 (53.1%) | 26 (47.3%) | 11 (61.1%) | |||
| Tumor size | |||||||||
| 0–2 cm | 14 (53.8%) | 24 (51.1%) | 1 | 10 (41.7%) | 28 (57.1%) | 0.31 | 33 (60%) | 5 (27.8%) | 0.02 |
| >2 cm | 12 (46.2%) | 23 (48.9%) | 14 (58.3%) | 21 (42.9%) | 22 (40%) | 13 (72.2%) | |||
| Depth of invasion | |||||||||
| 0–5 mm | 16 (61.5%) | 16 (34%) | 0.02 | 7 (29.2%) | 25 (51%) | 0.08 | 27 (49.1%) | 5 (27.8%) | 0.19 |
| >5 mm | 10 (38.5%) | 31 (66%) | 17 (70.8%) | 24 (49%) | 28 (50.9%) | 13 (72.2%) | |||
| Histological grade | |||||||||
| Well | 7 (26.9%) | 4 (8.5%) | 0.09 | 3 (12.5%) | 8 (16.3%) | 0.09 | 10 (18.2%) | 1 (5.6%) | 0.01 |
| Moderately | 16 (61.5%) | 39 (83%) | 16 (66.7%) | 39 (79.6%) | 43 (78.2%) | 12 (66.7%) | |||
| Poorly | 3 (11.5%) | 4 (8.5%) | 5 (20.8%) | 2 (4.1%) | 2 (3.6%) | 5 (27.8%) | |||
| Surgical margin | |||||||||
| Negative | 14 (53.8%) | 27 (57.4%) | 0.8 | 10 (41.7%) | 31 (63.3%) | 0.08 | 30 (54.5%) | 11 (61.1%) | 0.78 |
| Positive | 12 (46.2%) | 20 (42.6%) | 14 (58.3%) | 18 (36.7%) | 25 (45.5%) | 7 (38.9%) | |||
| Perineural invasion | |||||||||
| Absent | 22 (84.6%) | 33 (70.2%) | 0.27 | 14 (58.3%) | 41 (83.7%) | 0.03 | 44 (80%) | 11 (61.1%) | 0.12 |
| Present | 4 (15.4%) | 14 (29.8%) | 10 (41.7%) | 8 (16.3%) | 11 (20%) | 7 (38.9%) | |||
| Lymphovascular invasion | |||||||||
| Absent | 26 (100%) | 45 (95.7%) | 0.53 | 22 (91.7%) | 49 (100%) | 0.1 | 54 (98.2%) | 17 (94.4%) | 0.43 |
| Present | 0 | 2 (4.3%) | 2 (8.3%) | 0 | 1 (1.8%) | 1 (5.6%) | |||
| Lymph node metastasis | |||||||||
| Absent | 9 (52.9%) | 18 (47.4%) | 0.77 | 10 (50%) | 17 (48.6%) | 1 | 21 (53.8%) | 6 (37.5%) | 0.37 |
| Present | 8 (47.1%) | 20 (52.6%) | 10 (50%) | 18 (51.4%) | 18 (46.2%) | 10 (62.5%) | |||
| Extranodal extension | |||||||||
| Absent | 4 (50%) | 11 (55%) | 1 | 3 (52.6%) | 12 (55.6%) | 0.11 | 13 (72.2%) | 2 (20%) | 0.01 |
| Present | 4 (50%) | 9 (45%) | 7 (47.4%) | 6 (44.4%) | 5 (27.8%) | 8 (80%) | |||
| Size of extranodal extension | |||||||||
| 0–2 mm | 2 (50%) | 3 (33.3%) | 0.56 | 3 (42.9%) | 2 (33.3%) | 0.72 | 2 (40%) | 3 (37.5%) | 0.51 |
| >2 mm | 2 (50%) | 6 (66.7%) | 4 (57.1%) | 4 (66.7%) | 3 (60%) | 5 (62.5%) | |||
| pT | |||||||||
| T1 | 9 (34.6%) | 13 (27.7%) | 0.62 | 5 (20.8%) | 17 (34.7%) | 0.05 | 19 (34.5%) | 3 (16.7%) | 0.07 |
| T2 | 13 (38.2%) | 21 (44.7%) | 11 (45.8%) | 23 (46.9%) | 26 (47.3%) | 8 (44.4%) | |||
| T3 | 2 (7.7%) | 9 (19.1%) | 3 (12.5%) | 8 (16.3%) | 8 (14.5%) | 3 (16.7%) | |||
| T4 | 2 (7.7%) | 4 (8.5%) | 5 (20.8%) | 1 (2%) | 2 (3.6%) | 4 (22.2%) | |||
| pN | |||||||||
| N0 | 18 (69.2%) | 27 (57.4%) | 0.7 | 14 (58.3%) | 31 (63.3%) | 0.25 | 37 (67.3%) | 8 (44.4%) | 0.05 |
| N1 | 1 (3.8%) | 4 (8.5%) | 1 (4.2%) | 4 (8.2%) | 4 (7.3%) | 1 (5.6%) | |||
| N2 | 7 (26.9%) | 14 (29.8%) | 7 (29.2%) | 14 (28.6%) | 14 (25.5%) | 7 (38.9%) | |||
| N3 | 0 | 2 (4.3%) | 2 (8.3%) | 0 | 0 | 2 (11.1%) | |||
| AJCC stage | |||||||||
| Stage I | 7 (26.9%) | 11 (23.4%) | 0.69 | 5 (20.8%) | 13 (26.5%) | 0.21 | 16 (29.1%) | 2 (11.1%) | 0.16 |
| Stage II | 10 (38.5%) | 14 (29.8%) | 8 (33.3%) | 16 (32.7%) | 19 (34.5%) | 5 (27.8%) | |||
| Stage III | 1 (3.8%) | 5 (10.6%) | 0 | 6 (12.2%) | 5 (9.1%) | 1 (5.6%) | |||
| Stage IV | 8 (30.8%) | 17 (36.2%) | 11(45.8%) | 14 (28.69%) | 15 (27.3%) | 10 (55.6%) | |||
| AJCC stage | |||||||||
| Stage I–II | 17 (65.4%) | 25 (53.2%) | 0.44 | 13 (54.2%) | 29 (59.2%) | 0.87 | 35 (63.6%) | 7 (38.9%) | 0.11 |
| Stage III–IV | 9 (34.6%) | 22 (46.8%) | 11 (45.8%) | 20 (40.8%) | 20 (36.4%) | 11 (61.1%) | |||
| Locoregional recurrence | |||||||||
| Absent | 18 (69.2%) | 36 (76.6%) | 0.58 | 20 (83.3%) | 34 (69.4%) | 0.32 | 39 (70.9%) | 15 (83.3%) | 0.36 |
| Present | 8 (30.8%) | 11 (23.4%) | 4 (16.7%) | 15 (30.6%) | 16 (29.1%) | 3 (16.7%) | |||
| Distant metastasis | |||||||||
| Absent | 25 (96.2%) | 42 (89.4%) | 0.41 | 21 (87.5%) | 46 (93.9%) | 0.38 | 51 (92.7%) | 16 (88.9%) | 0.63 |
| Present | 1 (3.8%) | 5 (10.6%) | 3 (12.5%) | 3 (6.1%) | 4 (7.3%) | 2 (11.1%) | |||
| 2 Year OS | HR (95%CI) | p | ||
|---|---|---|---|---|
| Age | <65 | 77.50% | 1 | 0.09 |
| ≥65 | 58.60% | 1.890 (0.873–4.093) | ||
| Gender | Female | 76.70% | 1 | 0.32 |
| Male | 58.50% | 1.456 (0.686–3.091) | ||
| Tumor localization | Tongue | 68.90% | 1 | 0.99 |
| Other localization | 65.60% | 0.996 (0.47–2.109) | ||
| Tumor size | 0–2 cm | 80.50% | 1 | 0.11 |
| >2 cm | 55.10% | 1.823 (0.848–3.918) | ||
| Histological grade | Well-differentiated | 54.50% | 1 | 0.17 |
| Moderately differentiated | 74.30% | 0.752 (0.279–2.028) | ||
| Poorly differentiated | 42.90% | 1.865 (0.539–6.456) | ||
| Depth of invasion | 0–5 mm | 73.10% | 1 | 0.4 |
| >5 mm | 63.60% | 1.388 (0.639–3.013) | ||
| Surgical margin | Negative | 72.90% | 1 | 0.21 |
| Positive | 58.70% | 1.348 (0.769–2.361) | ||
| Perineural invasion | Absent | 75.60% | 1 | <0.001 |
| Present | 43% | 3.272 (1.517–7.056) | ||
| Lymphovascular invasion | Absent | 68.20% | 1 | 0.15 |
| Present | 50% | 2.697(0.635–11.452) | ||
| Lymph node metastasis | Absent | 73.70% | 1 | 0.03 |
| Present | 56.90% | 2.368 (1.029–5.448) | ||
| Extranodal extension | Absent | 60.20% | 1 | 0.94 |
| Present | 53.80% | 1.037(0.361–2.977) | ||
| Size of extranodal extension | 0–2 mm | 60% | 1 | 0.99 |
| >2 mm | 50% | 0.993(0.215–4.599) | ||
| pT | T1 | 75.70% | 1 | 0.01 |
| T2 | 75.5 | 1.272(0.483–3.349) | ||
| T3 | 45 | 1.920(0.573–6.429) | ||
| T4 | 33 | 6.044 (1.608–22.710) | ||
| pN | N0 | 74.7 | 1 | 0.04 |
| N1 | 60 | 1.238(0.275–5.579) | ||
| N2 | 57 | 2.900 (1.315–6.400) | ||
| N3 | 50 | 3.246 (0.410–25.709) | ||
| Stage | Stage I–II | 75.30% | 1 | 0.03 |
| Stage III–IV | 57.80% | 2.220 (1.046–4.710) | ||
| Locoregional recurrence | Absent | 72.70% | 1 | 0.04 |
| Present | 54.20% | 2.166 (0.999–4.699) | ||
| Distant metastasis | Absent | 71.40% | 1 | 0.01 |
| Present | 22.20% | 3.226 (1.197–8.691) | ||
| WPOI | WPOI 2–3 | 80% | 1 | 0.17 |
| WPOI 4 | 67.10% | 2.358 (0.548–10.144) | ||
| WPOI 5 | 58.20% | 4.106 (0.821–20.533) | ||
| WPOI | WPOI 4 | 67.10% | 1 | 0.26 |
| WPOI 5 | 58.20% | 1.682 (0.659–4.292) | ||
| Tumor budding | Absent | 82.60% | 1 | <0.001 |
| 1–4 buds | 78.20% | 1.534 (0.513–4.580) | ||
| 5–9 buds | 61.90% | 1.471 (0.394–5.499) | ||
| ≥10 buds | 35.90% | 4.786 (1.622–14.119) | ||
| Tumor budding | 0–4 buds | 79.90% | 1 | 0.02 |
| ≥5 buds | 47% | 2.252 (1.068–4.748) | ||
| Tumor cell nest size | >15 cells | 80% | 1 | 0.15 |
| 5–15 cells | 87.50% | 1.685 (0.280–10.153) | ||
| 2–4 cells | 84.40% | 1.904 (0.395–9.184) | ||
| Single-cell | 47.60% | 3.627 (0.829–15.870) | ||
| Tumor cell nest size | >1 cell | 83.30% | 1 | 0.02 |
| Single-cell | 47.60% | 2.252 (1.060–4.781) | ||
| Tumor-stroma ratio | Stroma-poor | 73.80% | 1 | 0.33 |
| Stroma-rich | 64.40% | 1.324 (0.561–3.124) | ||
| Stromal lymphocyte infiltration | 0–30% | 52.10% | 1 | 0.25 |
| 31–60% | 70.40% | 0.593 (0.255–1.378) | ||
| 61–100% | 82.60% | 0.482 (0.180–1.289) | ||
| Stromal lymphocyte infiltration | 0–30% | 52.10% | 1 | 0.1 |
| 31–100% | 75% | 0.546 (0.258–1.156) | ||
| Stroma type | Mature | 69.50% | 1 | 0.38 |
| Immature | 62.50% | 0.581 (0.252–1.336) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, A.; Taskin, T. Tumor Budding Should Be in Oral Cavity Cancer Reporting: A Retrospective Cohort Study Based on Tumor Microenvironment. Cancers 2023, 15, 3905. https://doi.org/10.3390/cancers15153905
Tan A, Taskin T. Tumor Budding Should Be in Oral Cavity Cancer Reporting: A Retrospective Cohort Study Based on Tumor Microenvironment. Cancers. 2023; 15(15):3905. https://doi.org/10.3390/cancers15153905
Chicago/Turabian StyleTan, Ayca, and Toros Taskin. 2023. "Tumor Budding Should Be in Oral Cavity Cancer Reporting: A Retrospective Cohort Study Based on Tumor Microenvironment" Cancers 15, no. 15: 3905. https://doi.org/10.3390/cancers15153905
APA StyleTan, A., & Taskin, T. (2023). Tumor Budding Should Be in Oral Cavity Cancer Reporting: A Retrospective Cohort Study Based on Tumor Microenvironment. Cancers, 15(15), 3905. https://doi.org/10.3390/cancers15153905









