pCR and 2-Year Disease-Free Survival: A Combination of the Two Endpoints as a New Classification for Locally Advanced Rectal Cancer Patients—An Updated Pooled Analysis of Eleven International Randomized Trials
Abstract
Simple Summary
Abstract
1. Introduction
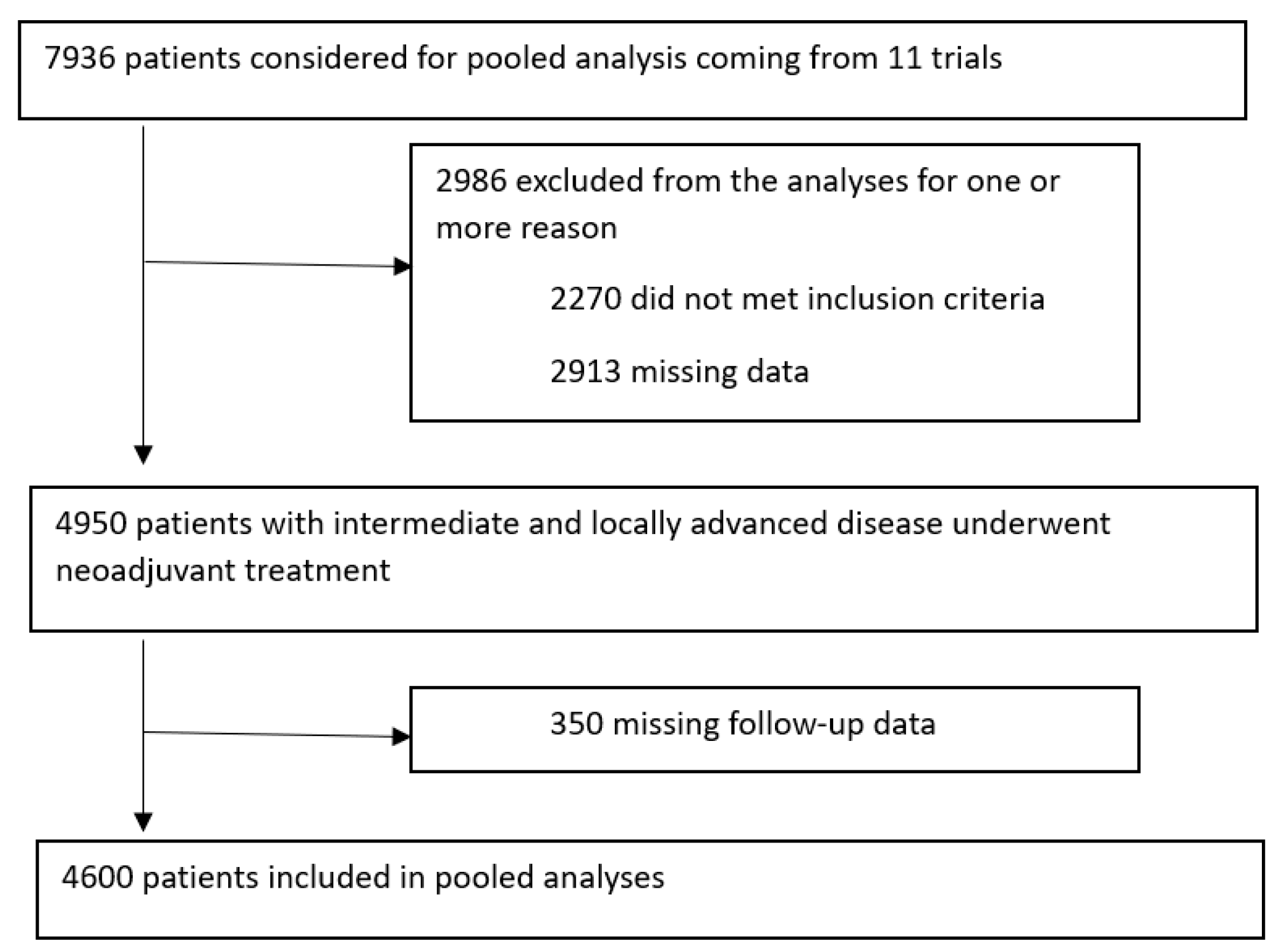
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Outcomes
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, N.; Brown, G. Preoperative staging of rectal cancer. Acta Oncol. 2008, 47, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, S.; Liu, Y.; Zhang, C.; Li, H.; Lai, B. Metastatic patterns and survival outcomes in patients with stage IV colon cancer: A population-based analysis. Cancer Med. 2020, 9, 361–373. [Google Scholar] [CrossRef] [PubMed]
- Gambacorta, M.A.; Masciocchi, C.; Chiloiro, G.; Meldolesi, E.; Macchia, G.; van Soest, J.; Peters, F.; Collette, L.; Gérard, J.P.; Ngan, S.; et al. Timing to achieve the highest rate of pCR after preoperative radiochemotherapy in rectal cancer: A pooled analysis of 3085 patients from 7 randomized trials. Radiother. Oncol. 2021, 154, 154–160. [Google Scholar] [CrossRef]
- Burbach, J.P.; den Harder, A.M.; Intven, M.; van Vulpen, M.; Verkooijen, H.M.; Reerink, O. Impact of radiotherapy boost on pathological complete response in patients with locally advanced rectal cancer: A systematic review and meta-analysis. Radiother. Oncol. 2014, 113, 1–9. [Google Scholar] [CrossRef]
- Sauer, R.; Liersch, T.; Merkel, S.; Fietkau, R.; Hohenberger, W.; Hess, C.; Becker, H.; Raab, H.R.; Villanueva, M.T.; Witzigmann, H.; et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: Results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J. Clin. Oncol. 2012, 30, 1926–1933. [Google Scholar] [CrossRef]
- Zhao, F.; Wang, J.; Yu, H.; Cheng, X.; Li, X.; Zhu, X.; Xu, X.; Lin, J.; Chen, X.; Yan, S. Neoadjuvant radiotherapy improves overall survival for T3/4N+M0 rectal cancer patients: A population-based study of 20300 patients. Radiat. Oncol. 2020, 15, 49. [Google Scholar] [CrossRef]
- Fiteni, F.; Westeel, V.; Pivot, X.; Borg, C.; Vernerey, D.; Bonnetain, F. Endpoints in cancer clinical trials. J. Visc. Surg. 2014, 151, 17–22. [Google Scholar] [CrossRef]
- Fokas, E.; Glynne-Jones, R.; Appelt, A.; Beets-Tan, R.; Beets, G.; Haustermans, K.; Marijnen, C.; Minsky, B.D.; Ludmir, E.; Quirke, P.; et al. Outcome measures in multimodal rectal cancer trials. Lancet Oncol. 2020, 21, e252–e264. [Google Scholar] [CrossRef]
- Maas, M.; Nelemans, P.J.; Valentini, V.; Das, P.; Rödel, C.; Kuo, L.J.; Calvo, F.A.; García-Aguilar, J.; Glynne-Jones, R.; Haustermans, K.; et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: A pooled analysis of individual patient data. Lancet Oncol. 2010, 11, 835–844. [Google Scholar] [CrossRef] [PubMed]
- Sargent, D.; Shi, Q.; Yothers, G.; Van Cutsem, E.; Cassidy, J.; Saltz, L.; Wolmark, N.; Bot, B.; Grothey, A.; Adjuvant Colon Cancer End-points (ACCENT) Group; et al. Two or three year disease-free survival (DFS) as a primary end-point in stage III adjuvant colon cancer trials with fluoropyrimidines with or without oxaliplatin or irinotecan: Data from 12,676 patients from MOSAIC, X-ACT, PETACC-3, C-06, C-07 and C89803. Eur. J. Cancer 2011, 47, 990–996. [Google Scholar] [CrossRef] [PubMed]
- Valentini, V.; van Stiphout, R.G.; Lammering, G.; Gambacorta, M.A.; Barba, M.C.; Bebenek, M.; Bonnetain, F.; Bosset, J.F.; Bujko, K.; Cionini, L.; et al. Selection of appropriate end-points (pCR vs 2yDFS) for tailoring treatments with prediction models in locally advanced rectal cancer. Radiother. Oncol. 2015, 114, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Sauer, R.; Becker, H.; Hohenberger, W.; Rödel, C.; Wittekind, C.; Fietkau, R.; Martus, P.; Tschmelitsch, J.; Hager, E.; German Rectal Cancer Study Group; et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N. Engl. J. Med. 2004, 351, 1731–1740. [Google Scholar] [CrossRef]
- Rödel, C.; Graeven, U.; Fietkau, R.; Hohenberger, W.; Hothorn, T.; Arnold, D.; Hofheinz, R.D.; Ghadimi, M.; Wolff, H.A.; German Rectal Cancer Study Group; et al. Oxaliplatin added to fluorouracil-based preoperative chemoradiotherapy and postoperative chemotherapy of locally advanced rectal cancer (the German CAO/ARO/AIO-04 study): Final results of the multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2015, 16, 979–989. [Google Scholar] [CrossRef]
- Bujko, K.; Nowacki, M.P.; Nasierowska-Guttmejer, A.; Michalski, W.; Bebenek, M.; Kryj, M. Long-term results of a randomized trial comparing preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal cancer. Br. J. Surg. 2006, 93, 1215–1223. [Google Scholar] [CrossRef]
- Bujko, K.; Wyrwicz, L.; Rutkowski, A.; Malinowska, M.; Pietrzak, L.; Kryński, J.; Michalski, W.; Olędzki, J.; Kuśnierz, J.; Zając, L.; et al. Long-course oxaliplatin-based preoperative chemoradiation versus 5 × 5 Gy and consolidation chemotherapy for cT4 or fixed cT3 rectal cancer: Results of a randomized phase III study. Ann. Oncol. 2016, 27, 834–842. [Google Scholar] [CrossRef] [PubMed]
- Bosset, J.F.; Collette, L.; Calais, G.; Mineur, L.; Maingon, P.; Radosevic-Jelic, L.; Daban, A.; Bardet, E.; Beny, A.; Ollier, J.C.; et al. Chemotherapy with preoperative radiotherapy in rectal cancer. N. Engl. J. Med. 2006, 355, 1114–1123, Erratum in N. Engl. J. Med. 2007, 357, 728. [Google Scholar] [CrossRef] [PubMed]
- Gérard, J.P.; Conroy, T.; Bonnetain, F.; Bouché, O.; Chapet, O.; Closon-Dejardin, M.T.; Untereiner, M.; Leduc, B.; Francois, E.; Maurel, J.; et al. Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3-4 rectal cancers: Results of FFCD 9203. J. Clin. Oncol. 2006, 24, 4620–4625. [Google Scholar] [CrossRef]
- Ngan, S.Y.; Burmeister, B.; Fisher, R.J.; Solomon, M.; Goldstein, D.; Joseph, D.; Ackland, S.P.; Schache, D.; McClure, B.; McLachlan, S.A.; et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J. Clin. Oncol. 2012, 30, 3827–3833, Erratum in J. Clin. Oncol. 2013, 31, 399. [Google Scholar] [CrossRef]
- Gérard, J.P.; Azria, D.; Gourgou-Bourgade, S.; Martel-Laffay, I.; Hennequin, C.; Etienne, P.L.; Vendrely, V.; François, E.; de La Roche, G.; Bouché, O.; et al. Comparison of two neoadjuvant chemoradiotherapy regimens for locally advanced rectal cancer: Results of the phase III trial ACCORD 12/0405-Prodige 2. J. Clin. Oncol. 2010, 28, 1638–1644. [Google Scholar] [CrossRef]
- Sainato, A.; Cernusco Luna Nunzia, V.; Valentini, V.; De Paoli, A.; Maurizi, E.R.; Lupattelli, M.; Aristei, C.; Vidali, C.; Conti, M.; Galardi, A.; et al. No benefit of adjuvant Fluorouracil Leucovorin chemotherapy after neoadjuvant chemoradiotherapy in locally advanced cancer of the rectum (LARC): Long term results of a randomized trial (I-CNR-RT). Radiother. Oncol. 2014, 113, 223–229. [Google Scholar] [CrossRef]
- Glynne-Jones, R.; Counsell, N.; Quirke, P.; Mortensen, N.; Maraveyas, A.; Meadows, H.M.; Ledermann, J.; Sebag-Montefiore, D. Chronicle: Results of a randomised phase III trial in locally advanced rectal cancer after neoadjuvant chemoradiation randomising postoperative adjuvant capecitabine plus oxaliplatin (XELOX) versus control. Ann. Oncol. 2014, 25, 1356–1362. [Google Scholar] [CrossRef]
- Valentini, V.; Gambacorta, M.A.; Cellini, F.; Aristei, C.; Coco, C.; Barbaro, B.; Alfieri, S.; D’Ugo, D.; Persiani, R.; Deodato, F.; et al. The INTERACT Trial: Long-term results of a randomised trial on preoperative capecitabine-based radiochemotherapy intensified by concomitant boost or oxaliplatin, for cT2 (distal)-cT3 rectal cancer. Radiother. Oncol. 2019, 134, 110–118. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 13 October 2022).
- Cotte, E.; Passot, G.; Decullier, E.; Maurice, C.; Glehen, O.; François, Y.; Lorchel, F.; Chapet, O.; Gerard, J.P. Pathologic Response, When Increased by Longer Interval, Is a Marker but Not the Cause of Good Prognosis in Rectal Cancer: 17-year Follow-up of the Lyon R90-01 Randomized Trial. Int. J. Radiat. Oncol. Biol. Phys. 2016, 94, 544–553. [Google Scholar] [CrossRef] [PubMed]
- Capirci, C.; Valentini, V.; Cionini, L.; De Paoli, A.; Rodel, C.; Glynne-Jones, R.; Coco, C.; Romano, M.; Mantello, G.; Palazzi, S.; et al. Prognostic value of pathologic complete response after neoadjuvant therapy in locally advanced rectal cancer: Long-term analysis of 566 ypCR patients. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Appelt, A.L.; Pløen, J.; Vogelius, I.R.; Bentzen, S.M.; Jakobsen, A. Radiation dose-response model for locally advanced rectal cancer after preoperative chemoradiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, 74–80. [Google Scholar] [CrossRef]
- Glynne-Jones, R.; Hughes, R. Critical appraisal of the ‘wait and see’ approach in rectal cancer for clinical complete responders after chemoradiation. Br. J. Surg. 2012, 99, 897–909. [Google Scholar] [CrossRef]
- Zhu, L.; Pan, Z.; Ma, Q.; Yang, W.; Shi, H.; Fu, C.; Yan, X.; Du, L.; Yan, F.; Zhang, H. Diffusion Kurtosis Imaging Study of Rectal Adenocarcinoma Associated with Histopathologic Prognostic Factors: Preliminary Findings. Radiology 2017, 284, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Dinapoli, N.; Barbaro, B.; Gatta, R.; Chiloiro, G.; Casà, C.; Masciocchi, C.; Damiani, A.; Boldrini, L.; Gambacorta, M.A.; Dezio, M.; et al. Magnetic Resonance, Vendor-independent, Intensity Histogram Analysis Predicting Pathologic Complete Response After Radiochemotherapy of Rectal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 765–774. [Google Scholar] [CrossRef]
- Jalil, O.; Afaq, A.; Ganeshan, B.; Patel, U.B.; Boone, D.; Endozo, R.; Groves, A.; Sizer, B.; Arulampalam, T. Magnetic resonance based texture parameters as potential imaging biomarkers for predicting long-term survival in locally advanced rectal cancer treated by chemoradiotherapy. Color. Dis. 2017, 19, 349–362. [Google Scholar] [CrossRef]
- Boldrini, L.; Cusumano, D.; Chiloiro, G.; Casà, C.; Masciocchi, C.; Lenkowicz, J.; Cellini, F.; Dinapoli, N.; Azario, L.; Teodoli, S.; et al. Delta radiomics for rectal cancer response prediction with hybrid 0.35 T magnetic resonance-guided radiotherapy (MRgRT): A hypothesis-generating study for an innovative personalized medicine approach. Radiol. Med. 2019, 124, 145–153. [Google Scholar] [CrossRef]
- Chiloiro, G.; Rodriguez-Carnero, P.; Lenkowicz, J.; Casà, C.; Masciocchi, C.; Boldrini, L.; Cusumano, D.; Dinapoli, N.; Meldolesi, E.; Carano, D.; et al. Delta Radiomics Can Predict Distant Metastasis in Locally Advanced Rectal Cancer: The Challenge to Personalize the Cure. Front. Oncol. 2020, 10, 595012. [Google Scholar] [CrossRef] [PubMed]

| Dataset | Pooled N | [%] | RT Only N | [%] | RT + Conc.CT N | [%] | RT + Adj.CT N | [%] | RT + Both CT N | [%] | p-Value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients | 4600 | [100] | 252 | [100] | 1295 | [100] | 608 | [100] | 2445 | [100] | |
| Sex | |||||||||||
| Male | 3164 | [68.8] | 180 | [71.4] | 878 | [67.8] | 405 | [66.6] | 1701 | [69.6] | 0.374 * |
| Female | 1428 | [31] | 72 | [28.6] | 410 | [31.7] | 203 | [33.4] | 743 | [30.4] | |
| No data | 8 | [0.2] | - | - | 7 | [0.5] | - | - | 1 | [0] | |
| Age (years) | |||||||||||
| Median | 62 | 63 | 62 | 60 | 62 | <0.001 # | |||||
| Range | 22–82 | 23–79 | 26–82 | 30–77 | 22–82 | ||||||
| cT stage | |||||||||||
| 1 + 2 | 294 | 6.47] | 0 | - | 156 | [12] | 12 | [2] | 126 | [5.1] | <0.001 * |
| 3 | 3618 | [78.6] | 214 | [84.9] | 910 | [70.3] | 487 | [80] | 2007 | [82.1] | |
| 4 | 305 | [6.6] | 27 | [10.7] | 82 | [6.3] | 41 | [6.7] | 155 | [6.1] | |
| No data | 383 | [8.3] | 11 | [4.4] | 147 | [11.3] | 68 | [11.2] | 157 | [6.3] | |
| cN stage | |||||||||||
| 0 | 1246 | [27.1] | 16 | [6.3] | 361 | [27.9] | 188 | [30.9] | 681 | [27.8] | <0.001 * |
| + | 1818 | [39.5] | 17 | [6.7] | 428 | [33] | 118 | [19.4] | 1255 | [51.3] | |
| No data | 1536 | [33.4] | 219 | [87] | 506 | [39] | 302 | [49.7] | 509 | [20.8] | |
| RT dose (Gy) | |||||||||||
| Median | 48.5 | 45 | 45 | 45 | 50.4 | <0.001 # | |||||
| Range | 26.4–61.2 | 41.4–50.4 | 28.8–61.2 | 39.6–55.8 | 26.4–58 | ||||||
| Conc.CT | |||||||||||
| 5FU/Cape | 2680 | [58.3] | - | - | 949 | [73.3] | - | - | 1731 | [70.8] | <0.001 * |
| Oxa-based | 1059 | [23] | - | - | 345 | [26.6] | - | - | 714 | [29.2] | |
| No CT/NA | 861 | [18.7] | 252 | [100] | 1 | [0] | 608 | [100] | - | - | |
| ypT stage | |||||||||||
| 0 | 640 | [13.9] | 19 | [7.5] | 269 | [20.8] | 13 | [2.1] | 339 | [13.9] | <0.001 * |
| 1 | 303 | [6.6] | 21 | [8.3] | 104 | [8] | 33 | [5.4] | 145 | [5.9] | |
| 2 | 1331 | [28.9] | 73 | [29] | 428 | [33] | 128 | [21] | 702 | [28.7] | |
| 3 | 2174 | [47.3] | 131 | [52] | 447 | [34.5] | 413 | [67.9] | 1183 | [48.4] | |
| 4 | 140 | [3] | 6 | [2.4] | 40 | [3.1] | 18 | [3] | 76 | [3.1] | |
| No data | 12 | [0.3] | 2 | [0.8] | 7 | [0.5] | 3 | [0.5] | - | - | |
| ypN stage | |||||||||||
| 0 | 3153 | [69] | 161 | [64] | 1042 | [80.5] | 328 | [54] | 1622 | [66.3] | <0.001 * |
| + | 1421 | [31] | 86 | [34] | 245 | [18.9] | 275 | [45.2] | 815 | [33.3] | |
| No data | 26 | [0.6] | 5 | [2] | 8 | [0.6] | 5 | [0.8] | 8 | [0.3] | |
| Adj.CT | |||||||||||
| 5FU/Cape | 2377 | [51.7] | - | - | - | - | 608 | [100] | 1769 | [72.3] | <0.001 * |
| Oxa-based | 671 | [14.6] | - | - | - | - | - | - | 671 | [27.4] | |
| No CT/NA | 1552 | [33.7] | 252 | [100] | 1295 | [100] | - | - | 5 | [0.2] | |
| Surgery | |||||||||||
| LAR | 3137 | [68] | 139 | [55.2] | 874 | [67.5] | 390 | [64.1] | 1734 | [70.9] | <0.001 * |
| APR | 1463 | [32] | 113 | [44.8] | 421 | [32.5] | 218 | [35.9] | 711 | [29.1] |
| Dataset | Pooled N 4600 | [100%] | nRT N 252 | [%] | nCRT N 1295 | [%] | nRT + Adj.CT N 608 | [%] | nCRT + Adj.CT N 2445 | [%] | p-Value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| pCR | |||||||||||
| Yes | 589 | [12.8] | 14 | [5.5] | 260 | [20] | 11 | [1.8] | 304 | [12.4] | <0.001 # |
| No | 4011 | [87.2] | 238 | [94.5] | 1035 | [80] | 597 | [98.2] | 2141 | [87.6] | |
| 2yDFS | |||||||||||
| Yes | 3652 | [79.4] | 161 | [64] | 1083 | [83.6] | 466 | [76.6] | 1942 | [79.4] | <0.001 # |
| No | 948 | [20.6] | 91 | [36] | 212 | [16.4] | 142 | [23.4] | 503 | [20.6] | |
| 5yOS | |||||||||||
| Yes | 1917 | [42] | 134 | [53.2] | 456 | [35.2] | 410 | [67.4] | 917 | [37.5] | <0.001 # |
| No | 850 | [18] | 77 | [30.5] | 256 | [19.8] | 102 | [16.8] | 415 | [17] | |
| NA | 1833 | [40] | 41 | [16.3] | 583 | [45] | 96 | [15.8] | 1113 | [45.5] |
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| p Value | Odds Ratio | 95% CI | p Value | Odds Ratio | 95% CI | |
| pCR | <0.001 | 0.386 | [0.276–0.530] | - | ||
| RT dose | <0.001 | 0.943 | [0.917–0.969] | <0.001 | 0.923 | [0.883–0.963] |
| Conc.CT | <0.001 | 1.485 | [1.227–1.803] | - | ||
| Conc.CT Oxa based | <0.001 | 1.406 | [1.111–1.777] | - | ||
| Adj.CT | <0.001 | 0.690 | [0.583–0.817] | <0.001 | 0.650 | [0.503–0.839] |
| Adj.CT Oxa based | <0.001 | 1.595 | [1.340–1.899] | - | ||
| LAR surgery | <0.001 | 0.525 | [0.444–0.620] | <0.001 | 0.562 | [0.440–0.717] |
| 2yDFS | <0.001 | 0.035 | [0.0279–0.044] | <0.001 | 0.036 | [0.027–0.048] |
| Age | <0.001 | 1.013 | [1.004–1.022] | <0.001 | 1.025 | [1.013–1.038] |
| Male sex | 0.026 | 1.223 | [1.024–1.465] | - | ||
| cT | 0.591 | 0.957 | [0.818–1.123] | - | ||
| ypT | <0.001 | 1.545 | [1.413–1.693] | <0.001 | 1.30 | [1.154–1.477] |
| ypN | <0.001 | 2.746 | [2.317–3.256] | - | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gambacorta, M.A.; Chiloiro, G.; Masciocchi, C.; Mariani, S.; Romano, A.; Gonnelli, A.; Gerard, J.-P.; Ngan, S.; Rödel, C.; Bujko, K.; et al. pCR and 2-Year Disease-Free Survival: A Combination of the Two Endpoints as a New Classification for Locally Advanced Rectal Cancer Patients—An Updated Pooled Analysis of Eleven International Randomized Trials. Cancers 2023, 15, 3209. https://doi.org/10.3390/cancers15123209
Gambacorta MA, Chiloiro G, Masciocchi C, Mariani S, Romano A, Gonnelli A, Gerard J-P, Ngan S, Rödel C, Bujko K, et al. pCR and 2-Year Disease-Free Survival: A Combination of the Two Endpoints as a New Classification for Locally Advanced Rectal Cancer Patients—An Updated Pooled Analysis of Eleven International Randomized Trials. Cancers. 2023; 15(12):3209. https://doi.org/10.3390/cancers15123209
Chicago/Turabian StyleGambacorta, Maria Antonietta, Giuditta Chiloiro, Carlotta Masciocchi, Silvia Mariani, Angela Romano, Alessandra Gonnelli, Jean-Pierre Gerard, Samuel Ngan, Claus Rödel, Krzysztof Bujko, and et al. 2023. "pCR and 2-Year Disease-Free Survival: A Combination of the Two Endpoints as a New Classification for Locally Advanced Rectal Cancer Patients—An Updated Pooled Analysis of Eleven International Randomized Trials" Cancers 15, no. 12: 3209. https://doi.org/10.3390/cancers15123209
APA StyleGambacorta, M. A., Chiloiro, G., Masciocchi, C., Mariani, S., Romano, A., Gonnelli, A., Gerard, J.-P., Ngan, S., Rödel, C., Bujko, K., Glynne-Jones, R., van Soest, J., Dekker, A., Damiani, A., & Valentini, V. (2023). pCR and 2-Year Disease-Free Survival: A Combination of the Two Endpoints as a New Classification for Locally Advanced Rectal Cancer Patients—An Updated Pooled Analysis of Eleven International Randomized Trials. Cancers, 15(12), 3209. https://doi.org/10.3390/cancers15123209






