Modern Management and Diagnostics in HER2+ Breast Cancer with CNS Metastasis
Abstract
Simple Summary
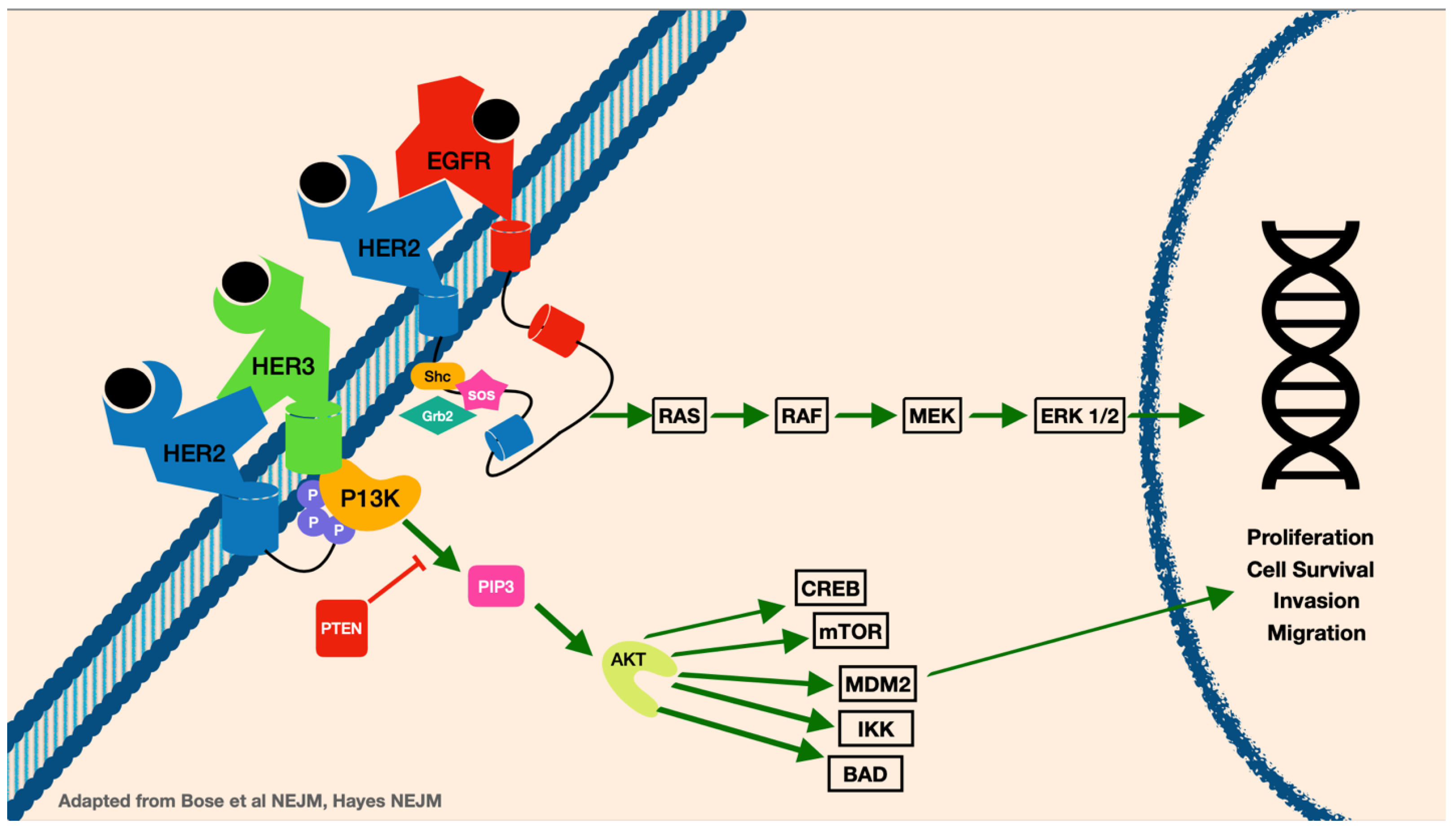
Abstract
1. Epidemiology of Breast Cancer and CNS Metastasis
2. Clinical Presentation of CNS Metastasis and Diagnostics
3. Treatment of HER2+ Breast Cancer with CNS Metastasis
3.1. Local Therapy
3.2. Systemic Therapy
3.3. Intrathecal Therapy
4. Prognosis of Patients with HER2+ Breast Cancer with Metastases to the Brain
5. Ongoing Studies/Future Directions
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lin, N.U.; Bellon, J.R.; Winer, E.P. CNS Metastases in Breast Cancer. J. Clin. Oncol. 2004, 22, 3608–3617. [Google Scholar] [CrossRef] [PubMed]
- Barnholtz-Sloan, J.S.; Sloan, A.E.; Davis, F.G.; Vigneau, F.D.; Lai, P.; Sawaya, R.E. Incidence Proportions of Brain Metastases in Patients Diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J. Clin. Oncol. 2004, 22, 2865–2872. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, A.S.; Van Swearingen, A.E.D.; Anders, C.K. HER2-positive breast cancer brain metastasis: A new and exciting landscape. Cancer Rep. 2022, 5, e1274. [Google Scholar] [CrossRef] [PubMed]
- Sperduto, P.W.; Mesko, S.; Li, J.; Cagney, D.; Aizer, A.; Lin, N.U.; Nesbit, E.; Kruser, T.J.; Chan, J.; Braunstein, S.; et al. Beyond an Updated Graded Prognostic Assessment (Breast GPA): A Prognostic Index and Trends in Treatment and Survival in Breast Cancer Brain Metastases from 1985 to Today. Int. J. Radiat. Oncol. Biol. Phys. 2020, 107, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Arvold, N.D.; Oh, K.S.; Niemierko, A.; Taghian, A.G.; Lin, N.U.; Abi-Raad, R.F.; Sreedhara, M.; Harris, J.R.; Alexander, B.M. Brain metastases after breast-conserving therapy and systemic therapy: Incidence and characteristics by biologic subtype. Breast Cancer Res. Treat. 2012, 136, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Slamon, D.J.; Clark, G.M.; Wong, S.G.; Levin, W.J.; Ullrich, A.; McGuire, W.L. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987, 235, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Kirsch, D.G.; Hochberg, F.H. Targeting HER2 in brain metastases from breast cancer. Clin. Cancer Res. 2003, 9, 5435–5436. [Google Scholar]
- Olson, E.M.; Najita, J.S.; Sohl, J.; Arnaout, A.; Burstein, H.J.; Winer, E.P.; Lin, N.U. Clinical outcomes and treatment practice patterns of patients with HER2-positive metastatic breast cancer in the post-trastuzumab era. Breast 2013, 22, 525–531. [Google Scholar] [CrossRef]
- Bendell, J.C.; Domchek, S.M.; Burstein, H.J.; Harris, L.; Younger, J.; Kuter, I.; Bunnell, C.; Rue, M.; Gelman, R.; Winer, E. Central nervous system metastases in women who receive trastuzumab-based therapy for metastatic breast carcinoma. Cancer 2003, 97, 2972–2977. [Google Scholar] [CrossRef]
- Valiente, M.; Ahluwalia, M.S.; Boire, A.; Brastianos, P.K.; Goldberg, S.B.; Lee, E.Q.; Le Rhun, E.; Preusser, M.; Winkler, F.; Soffietti, R. The Evolving Landscape of Brain Metastasis. Trends Cancer 2018, 4, 176–196. [Google Scholar] [CrossRef]
- Sevenich, L.; Bowman, R.L.; Mason, S.D.; Quail, D.F.; Rapaport, F.; Elie, B.T.; Brogi, E.; Brastianos, P.K.; Hahn, W.C.; Holsinger, L.J.; et al. Analysis of tumour- and stroma-supplied proteolytic networks reveals a brain-metastasis-promoting role for cathepsin S. Nat. Cell Biol. 2014, 16, 876–888. [Google Scholar] [CrossRef] [PubMed]
- Bailleux, C.; Eberst, L.; Bachelot, T. Treatment strategies for breast cancer brain metastases. Br. J. Cancer 2021, 124, 142–155. [Google Scholar] [CrossRef] [PubMed]
- Neman, J.; Termini, J.; Wilczynski, S.; Vaidehi, N.; Choy, C.; Kowolik, C.M.; Li, H.; Hambrecht, A.C.; Roberts, E.; Jandial, R. Human breast cancer metastases to the brain display GABAergic properties in the neural niche. Proc. Natl. Acad. Sci. USA 2014, 111, 984–989. [Google Scholar] [CrossRef]
- Weil, R.J.; Palmieri, D.C.; Bronder, J.L.; Stark, A.M.; Steeg, P.S. Breast cancer metastasis to the central nervous system. Am. J. Pathol. 2005, 167, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Andersen, C.; Astrup, J.; Gyldensted, C. Quantitation of peritumoural oedema and the effect of steroids using NMR-relaxation time imaging and blood-brain barrier analysis. Acta Neurochir Suppl. 1994, 60, 413–415. [Google Scholar] [CrossRef] [PubMed]
- Ryken, T.C.; McDermott, M.; Robinson, P.D.; Ammirati, M.; Andrews, D.W.; Asher, A.L.; Burri, S.H.; Cobbs, C.S.; Gaspar, L.E.; Kondziolka, D.; et al. The role of steroids in the management of brain metastases: A systematic review and evidence-based clinical practice guideline. J. Neurooncol. 2010, 96, 103–114. [Google Scholar] [CrossRef]
- Chang, S.M.; Messersmith, H.; Ahluwalia, M.; Andrews, D.; Brastianos, P.K.; Gaspar, L.E.; Gatson, N.T.N.; Jordan, J.T.; Khasraw, M.; Lassman, A.B.; et al. Anticonvulsant Prophylaxis and Steroid Use in Adults with Metastatic Brain Tumors: ASCO and SNO Endorsement of the Congress of Neurological Surgeons Guidelines. J. Clin. Oncol. 2019, 37, 1130–1135. [Google Scholar] [CrossRef]
- Soffietti, R.; Cornu, P.; Delattre, J.Y.; Grant, R.; Graus, F.; Grisold, W.; Heimans, J.; Hildebrand, J.; Hoskin, P.; Kalljo, M.; et al. EFNS Guidelines on diagnosis and treatment of brain metastases: Report of an EFNS Task Force. Eur. J. Neurol. 2006, 13, 674–681. [Google Scholar] [CrossRef]
- Dixit, K.S.; Kumthekar, P.U. Optimal Management of Corticosteroids in Patients with Intracranial Malignancies. Curr. Treat Options Oncol. 2020, 21, 77. [Google Scholar] [CrossRef]
- Chen, C.C.; Rennert, R.C.; Olson, J.J. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines on the Role of Prophylactic Anticonvulsants in the Treatment of Adults with Metastatic Brain Tumors. Neurosurgery 2019, 84, E195–E197. [Google Scholar] [CrossRef]
- Forsyth, P.A.; Weaver, S.; Fulton, D.; Brasher, P.M.; Sutherland, G.; Stewart, D.; Hagen, N.A.; Barnes, P.; Cairncross, J.G.; DeAngelis, L.M. Prophylactic anticonvulsants in patients with brain tumour. Can. J. Neurol. Sci. 2003, 30, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.S.; Trinh, V.T.; Suki, D.; Graham, S.; Forman, A.; Weinberg, J.S.; McCutcheon, I.E.; Prabhu, S.S.; Heimberger, A.B.; Sawaya, R.; et al. A prospective randomized trial of perioperative seizure prophylaxis in patients with intraparenchymal brain tumors. J. Neurosurg. 2013, 118, 873–883. [Google Scholar] [CrossRef] [PubMed]
- Patchell, R.A.; Tibbs, P.A.; Walsh, J.W.; Dempsey, R.J.; Maruyama, Y.; Kryscio, R.J.; Markesbery, W.R.; Macdonald, J.S.; Young, B. A randomized trial of surgery in the treatment of single metastases to the brain. N. Engl. J. Med. 1990, 322, 494–500. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Serizawa, T.; Higuchi, Y.; Sato, Y.; Kawagishi, J.; Yamanaka, K.; Shuto, T.; Akabane, A.; Jokura, H.; Yomo, S.; et al. A Multi-institutional Prospective Observational Study of Stereotactic Radiosurgery for Patients with Multiple Brain Metastases (JLGK0901 Study Update): Irradiation-related Complications and Long-term Maintenance of Mini-Mental State Examination Scores. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 31–40. [Google Scholar] [CrossRef]
- Ippolito, E.; Silipigni, S.; Matteucci, P.; Greco, C.; Carrafiello, S.; Palumbo, V.; Tacconi, C.; Talocco, C.; Fiore, M.; D’Angelillo, R.M.; et al. Radiotherapy for HER 2 Positive Brain Metastases: Urgent Need for a Paradigm Shift. Cancers 2022, 14, 1514. [Google Scholar] [CrossRef]
- Greene-Schloesser, D.; Moore, E.; Robbins, M.E. Molecular pathways: Radiation-induced cognitive impairment. Clin. Cancer Res. 2013, 19, 2294–2300. [Google Scholar] [CrossRef]
- Sun, B.; Huang, Z.; Wu, S.; Shen, G.; Cha, L.; Meng, X.; Ding, L.; Wang, J.; Song, S. Incidence and relapse risk of intracranial metastases within the perihippocampal region in 314 patients with breast cancer. Radiother. Oncol. 2016, 118, 181–186. [Google Scholar] [CrossRef]
- Brown, P.D.; Gondi, V.; Pugh, S.; Tome, W.A.; Wefel, J.S.; Armstrong, T.S.; Bovi, J.A.; Robinson, C.; Konski, A.; Khuntia, D.; et al. Hippocampal Avoidance during Whole-Brain Radiotherapy Plus Memantine for Patients with Brain Metastases: Phase III Trial NRG Oncology CC001. J. Clin. Oncol. 2020, 38, 1019–1029. [Google Scholar] [CrossRef]
- Costa, R.; Gill, N.; Rademaker, A.W.; Carneiro, B.A.; Chae, Y.K.; Kumthekar, P.; Gradishar, W.J.; Kurzrock, R.; Giles, F.J. Systematic analysis of early phase clinical studies for patients with breast cancer: Inclusion of patients with brain metastasis. Cancer Treat Rev. 2017, 55, 10–15. [Google Scholar] [CrossRef]
- Stemmler, H.J.; Schmitt, M.; Willems, A.; Bernhard, H.; Harbeck, N.; Heinemann, V. Ratio of trastuzumab levels in serum and cerebrospinal fluid is altered in HER2-positive breast cancer patients with brain metastases and impairment of blood-brain barrier. Anticancer. Drugs 2007, 18, 23–28. [Google Scholar] [CrossRef]
- Murthy, R.K.; Loi, S.; Okines, A.; Paplomata, E.; Hamilton, E.; Hurvitz, S.A.; Lin, N.U.; Borges, V.; Abramson, V.; Anders, C.; et al. Tucatinib, Trastuzumab, and Capecitabine for HER2-Positive Metastatic Breast Cancer. N. Engl. J. Med. 2020, 382, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Modi, S.; Saura, C.; Yamashita, T.; Park, Y.H.; Kim, S.B.; Tamura, K.; Andre, F.; Iwata, H.; Ito, Y.; Tsurutani, J.; et al. Trastuzumab Deruxtecan in Previously Treated HER2-Positive Breast Cancer. N. Engl. J. Med. 2020, 382, 610–621. [Google Scholar] [CrossRef] [PubMed]
- Pérez-García, J.M.; Vaz Batista, M.; Cortez, P.; Ruiz-Borrego, M.; Cejalvo, J.M.; de la Haba-Rodriguez, J.; Garrigós, L.; Racca, F.; Servitja, S.; Blanch, S.; et al. Trastuzumab deruxtecan in patients with central nervous system involvement from HER2-positive breast cancer: The DEBBRAH trial. Neuro. Oncol. 2023, 25, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Diéras, V.; Miles, D.; Verma, S.; Pegram, M.; Welslau, M.; Baselga, J.; Krop, I.E.; Blackwell, K.; Hoersch, S.; Xu, J.; et al. Trastuzumab emtansine versus capecitabine plus lapatinib in patients with previously treated HER2-positive advanced breast cancer (EMILIA): A descriptive analysis of final overall survival results from a randomised, open-label, phase 3 trial. Lancet Oncol. 2017, 18, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, F.; Delaloge, S.; Barrios, C.H.; Wuerstlein, R.; Anton, A.; Brain, E.; Hatschek, T.; Kelly, C.M.; Peña-Murillo, C.; Yilmaz, M.; et al. Trastuzumab emtansine (T-DM1) in patients with HER2-positive metastatic breast cancer and brain metastases: Exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trial(☆). Ann. Oncol. 2020, 31, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- Saura, C.; Oliveira, M.; Feng, Y.H.; Dai, M.S.; Chen, S.W.; Hurvitz, S.A.; Kim, S.B.; Moy, B.; Delaloge, S.; Gradishar, W.; et al. Neratinib Plus Capecitabine versus Lapatinib Plus Capecitabine in HER2-Positive Metastatic Breast Cancer Previously Treated with ≥2 HER2-Directed Regimens: Phase III NALA Trial. J. Clin. Oncol. 2020, 38, 3138–3149. [Google Scholar] [CrossRef]
- Lien, E.A.; Wester, K.; Lønning, P.E.; Solheim, E.; Ueland, P.M. Distribution of tamoxifen and metabolites into brain tissue and brain metastases in breast cancer patients. Br. J. Cancer 1991, 63, 641–645. [Google Scholar] [CrossRef]
- Hoefnagel, L.D.; van de Vijver, M.J.; van Slooten, H.J.; Wesseling, P.; Wesseling, J.; Westenend, P.J.; Bart, J.; Seldenrijk, C.A.; Nagtegaal, I.D.; Oudejans, J.; et al. Receptor conversion in distant breast cancer metastases. Breast Cancer Res. 2010, 12, R75. [Google Scholar] [CrossRef]
- Tolaney, S.M.; Sahebjam, S.; Le Rhun, E.; Bachelot, T.; Kabos, P.; Awada, A.; Yardley, D.; Chan, A.; Conte, P.; Diéras, V.; et al. A Phase II Study of Abemaciclib in Patients with Brain Metastases Secondary to Hormone Receptor-Positive Breast Cancer. Clin. Cancer Res. 2020, 26, 5310–5319. [Google Scholar] [CrossRef]
- Jaeckle, K.A.; Batchelor, T.; O’Day, S.J.; Phuphanich, S.; New, P.; Lesser, G.; Cohn, A.; Gilbert, M.; Aiken, R.; Heros, D.; et al. An Open Label Trial of Sustained-release Cytarabine (DepoCyt™) for the Intrathecal Treatment of Solid Tumor Neoplastic Meningitis. J. Neuro. Oncol. 2002, 57, 231–239. [Google Scholar] [CrossRef]
- Bazan, F.; Dobi, E.; Royer, B.; Curtit, E.; Mansi, L.; Menneveau, N.; Paillard, M.J.; Meynard, G.; Villanueva, C.; Pivot, X.; et al. Systemic high-dose intravenous methotrexate in patients with central nervous system metastatic breast cancer. BMC Cancer 2019, 19, 1029. [Google Scholar] [CrossRef] [PubMed]
- Jaeckle, K.A.; Dixon, J.G.; Anderson, S.K.; Moreno-Aspitia, A.; Colon-Otero, G.; Hebenstreit, K.; Patel, T.A.; Reddy, S.L.; Perez, E.A. Intra-CSF topotecan in treatment of breast cancer patients with leptomeningeal metastases. Cancer Med. 2020, 9, 7935–7942. [Google Scholar] [CrossRef] [PubMed]
- Groves, M.D.; Glantz, M.J.; Chamberlain, M.C.; Baumgartner, K.E.; Conrad, C.A.; Hsu, S.; Wefel, J.S.; Gilbert, M.R.; Ictech, S.; Hunter, K.U.; et al. A multicenter phase II trial of intrathecal topotecan in patients with meningeal malignancies. Neuro. Oncol. 2008, 10, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Comte, A.; Jdid, W.; Guilhaume, M.N.; Kriegel, I.; Piperno-Neumann, S.; Dieras, V.; Dorval, T.; Pierga, J.Y.; Cottu, P.H.; Mignot, L.; et al. Survival of breast cancer patients with meningeal carcinomatosis treated by intrathecal thiotepa. J. Neurooncol. 2013, 115, 445–452. [Google Scholar] [CrossRef]
- Kumthekar, P.U.; Avram, M.J.; Lassman, A.B.; Lin, N.U.; Lee, E.; Grimm, S.A.; Schwartz, M.; Bell Burdett, K.L.; Lukas, R.V.; Dixit, K.; et al. A phase I/II study of intrathecal trastuzumab in human epidermal growth factor receptor 2-positive (HER2-positive) cancer with leptomeningeal metastases: Safety, efficacy, and cerebrospinal fluid pharmacokinetics. Neuro Oncol. 2023, 25, 557–565. [Google Scholar] [CrossRef]
- Oberkampf, F.; Gutierrez, M.; Trabelsi Grati, O.; Rhun, É.L.; Trédan, O.; Turbiez, I.; Kadi, A.; Dubot, C.; Taillibert, S.; Vacher, S.; et al. Phase II study of intrathecal administration of trastuzumab in patients with HER2-positive breast cancer with leptomeningeal metastasis. Neuro Oncol. 2023, 25, 365–374. [Google Scholar] [CrossRef]
- Ellegård, S.; Engvall, K.; Asowed, M.; Hallbeck, A.L.; Elander, N.; Stål, O. Long-term follow-up of early stage HER2-positive breast cancer patients treated with trastuzumab: A population-based real world multicenter cohort study. Front. Oncol. 2022, 12, 861324. [Google Scholar] [CrossRef]
- Sperduto, P.W.; Mesko, S.; Li, J.; Cagney, D.; Aizer, A.; Lin, N.U.; Nesbit, E.; Kruser, T.J.; Chan, J.; Braunstein, S.; et al. Survival in Patients with Brain Metastases: Summary Report on the Updated Diagnosis-Specific Graded Prognostic Assessment and Definition of the Eligibility Quotient. J. Clin. Oncol. 2020, 38, 3773–3784. [Google Scholar] [CrossRef]
- Lara-Medina, F.; Crismatt, A.; Villarreal-Garza, C.; Alvarado-Miranda, A.; Flores-Hernández, L.; González-Pinedo, M.; Gamboa-Vignolle, C.; Ruiz-González, J.D.; Arrieta, O. Clinical features and prognostic factors in patients with carcinomatous meningitis secondary to breast cancer. Breast J. 2012, 18, 233–241. [Google Scholar] [CrossRef]
- Shen, Q.; Sahin, A.A.; Hess, K.R.; Suki, D.; Aldape, K.D.; Sawaya, R.; Ibrahim, N.K. Breast cancer with brain metastases: Clinicopathologic features, survival, and paired biomarker analysis. Oncologist 2015, 20, 466–473. [Google Scholar] [CrossRef]
- Subbiah, I.M.; Lei, X.; Weinberg, J.S.; Sulman, E.P.; Chavez-MacGregor, M.; Tripathy, D.; Gupta, R.; Varma, A.; Chouhan, J.; Guevarra, R.P.; et al. Validation and Development of a Modified Breast Graded Prognostic Assessment as a Tool for Survival in Patients with Breast Cancer and Brain Metastases. J. Clin. Oncol. 2015, 33, 2239–2245. [Google Scholar] [CrossRef] [PubMed]
- Dawood, S.; Broglio, K.; Esteva, F.J.; Ibrahim, N.K.; Kau, S.W.; Islam, R.; Aldape, K.D.; Yu, T.K.; Hortobagyi, G.N.; Gonzalez-Angulo, A.M. Defining prognosis for women with breast cancer and CNS metastases by HER2 status. Ann. Oncol. 2008, 19, 1242–1248. [Google Scholar] [CrossRef] [PubMed]
- Bergen, E.S.; Binter, A.; Starzer, A.M.; Heller, G.; Kiesel, B.; Tendl-Schulz, K.; Bago-Horvath, Z.; Furtner, J.; Leitner, J.; Exner, R.; et al. Favourable outcome of patients with breast cancer brain metastases treated with dual HER2 blockade of trastuzumab and pertuzumab. Ther. Adv. Med. Oncol. 2021, 13, 17588359211009002. [Google Scholar] [CrossRef] [PubMed]
- Darlix, A.; Louvel, G.; Fraisse, J.; Jacot, W.; Brain, E.; Debled, M.; Mouret-Reynier, M.A.; Goncalves, A.; Dalenc, F.; Delaloge, S.; et al. Impact of breast cancer molecular subtypes on the incidence, kinetics and prognosis of central nervous system metastases in a large multicentre real-life cohort. Br. J. Cancer 2019, 121, 991–1000. [Google Scholar] [CrossRef]
| Targeted Therapy for HER2-Positive Breast Cancer | ||||
|---|---|---|---|---|
| Regimen | Mechanism | Indications | Adverse Effects | Trials Included |
| Trastuzumab, pertuzumab, and taxane | Combination of MOAbs with two separate extracellular domains of HER2, taxane | First-line therapy | Diarrhea, neutropenia, rash, mucositis, alopecia, neuropathy, LV dysfunction * | APHINITY, CLEOPATRA, PERUSE |
| Ado-trastuzumab emtansine (T-DM1) | Antibody–drug conjugate with thioether linker and microtubule inhibitor | Second-line therapy in advanced/metastatic disease, adjuvant therapy | Thrombocytopenia, LFT abnormalities, increased bleeding risk independent of PLT count, LV dysfunction * | MARIANNE, TH3RESA, EMILIA, Destiny-Breast03 |
| Trastuzumab deruxtecan (T-DXd) | Antibody–drug conjugate with tetrapeptide-based linker and topoisomerase I inhibitor | Second- or third-line therapy for unresectable/metastatic disease that progressed on prior regimens | Interstitial lung disease; must be discontinued after Grade II pneumonitis | Destiny-Breast03 |
| Tucatinib, Trastuzumab, and Capecitabine | Combination of selective oral TKI, HER2 Moab, and oral Fluorouracil prodrug | Second- or third-line therapy for unresectable/metastatic disease, especially in brain metastases | Palmar–plantar erythrodysesthesia, diarrhea, LFT abnormalities | HER2CLIMB |
| Margetuximab | Fc-engineered HER2 MOAb | Third-line therapy | Fatigue, GI upset, cough, dyspnea, infusion reaction, palmar–plantar erythrodysesthesia, LV dysfunction | SOPHIA |
| Lapatinib, trastuzumab | Combination of Oral TKI (EGFR/HER2) and MOAb | Third-line therapy | Diarrhea, palmar–plantar erythrodysesthesia | EMILIA |
| Neratinib, Capecitabine | Combination of Oral TKI and oral Fluorouracil prodrug | Third-line therapy | Diarrhea, acute liver injury | NALA, ExteNET, SUMMIT |
| Agent | Description | Half-Life in the CSF | Recommended Schedules of Administration | Recommended Prophylaxis of Adverse Events |
|---|---|---|---|---|
| Cytarabine | Pyrimidine nucleoside analogue | <1 h | 10 mg twice weekly (total 4 weeks), then 10 mg once weekly (total 4 weeks), then 10 mg once monthly | None |
| Liposomal cytarabine * | Pyrimidine nucleoside analogue | 14–21 days | 50 mg every 2 weeks (total 8 weeks), then 50 mg once monthly | Oral steroids [40] |
| Methotrexate | Folate antimetabolite | 4.5–8 h | 10–15 mg twice weekly (total 4 weeks), then 10–15 mg once weekly (total 4 weeks), then 10–15 mg once monthly | Folinic acid rescue [41] |
| Topotecan | Topoisomerase 1 inhibitor | 1.3 h [42,43] | 0.4 mg twice weekly × 4–6 weeks, then weekly × 4, then every other weekly × 4 then monthly | |
| Thiotepa | Alkylating ethyleneimine compound | 3–4 h | 10 mg once every other week | Given with methylprednisone 40 mg [44] |
| Trastuzumab | Monoclonal antibody | 80 mg twice weekly or 150 mg weekly | None [45,46] |
| Clinical Trials for HER2-Positive Breast Cancer with Metastasis to the Brain | |||||||
|---|---|---|---|---|---|---|---|
| NCT Identifier | Title | Sponsor | Phase | N | Status | Trial Drug(s) | Results |
| NCT05800275 | Multicentric Single Arm Phase II Study Evaluating the Efficacy of Association of Tucatinib, Capecitabine and Intra-CSF Trastuzumab in HER2 Amplified Breast Cancer Patients With Leptomeningeal Metastases | UNICANCER | II | n/a | Not yet recruiting | Tucabinib, Capecitabine, Trastuzumab | n/a |
| NCT04158947 | A Randomized Study of HER2+ Breast Cancer Patients With Active Refractory Brain Metastases Treated With Afatinib in Combination With T-DM1 vs. T-DM1 Alone | Zhejiang University School of Medicine, Second Affiliated Hospital (Hangzhou, China) | I | n/a | Recruiting | Afatinib, T-DM1 | n/a |
| NCT03696030 | A Phase 1 Cellular Immunotherapy Study of Intraventricularly Administered Autologous HER2-Targeted Chimeric Antigen Receptor (HER2-CAR) T Cells in Patients With Brain and/or Leptomeningeal Metastases From HER2 Positive Cancers | City of Hope Medical Center | I | n/a | Recruiting | Autologous HER2-Targeted CAR T Cells | n/a |
| NCT04588545 | Phase I/II Study of Radiation Therapy Followed by Intrathecal Trastuzumab/Pertuzumab in the Management of HER2+ Breast Leptomeningeal Disease | H. Lee Moffitt Cancer Center and Research Institute | I/II | n/a | Recruiting | Radiation therapy, trastuzumab/pertuzumab | n/a |
| NCT05041842 | Treatment With Tucatinib in Addition to Pertuzumab and Trastuzumab in Patients With HER2-positive Metastatic Breast Cancer After Local Therapy of Isolated Brain Progression | UNICANCER | II | n/a | Recruiting | Tucatinib, pertuzumab and trastuzumab | n/a |
| NCT05018702 | A Prospective, Single-arm, Single-center Phase II Clinical Study of Recombinant Humanized Anti-HER2 Monoclonal Antibody-AS269 Conjugate (ARX788) in the Treatment of HER2-positive Breast Cancer Patients With Brain Metastases | Fudan University (Shanghai, China) | II | n/a | Recruiting | ARX788 (conjugate anti-HER2 MoAb) | n/a |
| NCT03765983 | Phase II Trial of GDC-0084 in Combination With Trastuzumab for Patients With HER2-Positive Breast Cancer Brain Metastases | Dana-Farber Cancer Institute | II | n/a | Recruiting | GDC-0084 (PI3K/mTOR inhibitor), Trastuzumab | n/a |
| NCT04158947 | A Randomized Study of HER2+ Breast Cancer Patients With Active Refractory Brain Metastases Treated With Afatinib in Combination With T-DM1 vs. T-DM1 Alone | Zhejiang University School of Medicine, Second Affiliated Hospital (Hangzhou, China) | II | n/a | Recruiting | Afatinib, T-DM1 | n/a |
| NCT03417544 | A Phase II Study of Atezolizumab in Combination With Pertuzumab Plus High-dose Trastuzumab for the Treatment of Central Nervous System Metastases in Patients With Her2-positive Breast Cancer | Dana-Farber Cancer Institute | II | n/a | Recruiting | Atezolizumab, Pertuzumab, Trastuzumab | n/a |
| NCT04622319 | A Phase 3, Multicenter, Randomized, Open-Label, Active-Controlled Study of Trastuzumab Deruxtecan (T-DXd) Versus Trastuzumab Emtansine (T-DM1) in Participants With High-Risk HER2-Positive Primary Breast Cancer Who Have Residual Invasive Disease in Breast or Axillary Lymph Nodes Following Neoadjuvant Therapy (DESTINY-Breast05) | Daiichi Sankyo, Inc. (Tokyo, Japan) | III | n/a | Recruiting | T-DXd, T-DM1 | n/a |
| NCT04739761 | An Open-Label, Multinational, Multicenter, Phase 3b/4 Study of Trastuzumab Deruxtecan in Patients With or Without Baseline Brain Metastasis With Previously Treated Advanced/Metastatic HER2-Positive Breast Cancer (DESTINY-Breast12) | AstraZeneca (Cambridge, UK) | III | n/a | Recruiting | Trastuzumab Deruxtecan (T-DXd) | n/a |
| NCT01921335 | Phase I Dose-escalation Trial of ARRY-380 in Combination With Trastuzumab in Participants With Brain Metastases From HER2+ Breast Cancer | Dana-Farber Cancer Institute (Boston, MA, USA) | I | 41 | Active | ARRY-380 (small molecule inhibitor of HER2), Trastuzumab | n/a |
| NCT04582968 | A Phase Ib/II Pilot Study of Pyrotinib Plus Capecitabine Combined With Brain Radiotherapy in HER2 Positive Breast Cancer Patients With Brain Metastases | Fudan University (Shanghai, China) | Ib/II | 39 | Active | Pyrotinib, Capecitabine | n/a |
| NCT03190967 | Phase I/II Study of T-DM1 Alone Versus T-DM1 and Metronomic Temozolomide in Secondary Prevention of HER2-Positive Breast Cancer Brain Metastases Following Stereotactic Radiosurgery | National Cancer Institute (NCI) (Bethesda, MD, USA) | I/II | 12 | Active | T-DM1, TMZ | n/a |
| NCT01494662 | A Phase II Trial of HKI-272 (Neratinib), Neratinib and Capecitabine, and Ado-Trastuzumab Emtansine for Patients with Human Epidermal Growth Factor Receptor 2 (HER2)-Positive Breast Cancer and Brain Metastases | Dana-Farber Cancer Institute | II | 140 | Active | Neratinib, Capecitabine, Ado-Trastuzumab Emtansine | n/a |
| NCT04752059 | Phase II Study of Trastuzumab-Deruxtecan (T-DX; DS-8201a) in HER2-positive Breast Cancer Patients With Newly Diagnosed or Progressing Brain Metastases | Medical University of Vienna | II | 15 | Active | Trastuzumab-Deruxtecan (T-DXd) | n/a |
| NCT03691051 | Pyrotinib Plus Capecitabine in Patients With Brain Metastases From HER2-positive Metastatic Breast Cancer: a Single-arm, Open-label, Ahead Study | Henan Cancer Hospital (Zhengzhou, China) | II | 78 | Active | Pyrotinib, Capecitabine | n/a |
| NCT00470847 | A Phase I Study of Lapatinib in Combination With Radiation Therapy in Patients With Brain Metastases From HER2-Positive Breast Cancer | Dana-Farber Cancer Institute | I | 35 | Completed | Lapatinib, WBRT, trastuzumab | Did not meet criteria for feasibility due to toxicity (7/27 with dose-limiting toxicity); CNS objective response rate was 79% by volumetric criteria, 46% progression-free at 6 mos. |
| NCT00614978 | Phase 1 Study of the Combination of Lapatinib and Temozolomide for the Treatment of Progressive Brain Disease in HER-2 Positive Breast Cancer (LAPTEM) | Jules Bordet Institute | I | 18 | Completed | Lapatinib, Temozolomide | Regimen well tolerated (MTD not reached); 10/15 patients assessed had SD but median PFS 2.6 months. |
| NCT01783756 | Phase 1b/2 Single-arm Trial Evaluating the Combination of Lapatinib, Everolimus and Capecitabine for the Treatment of Patients With HER2-positive Metastatic Breast Cancer With CNS Progression After Trastuzumab | Jonsson Comprehensive Cancer Center (UCLA) | I/II | 19 | Completed | Lapatinib ditosylate, everolimus, capecitabine | Regimen well tolerated (MTD reached), 3/11 (27%) with partial response, 7/11 with stable disease, best CNS objective response rate 28%, median PFS 6.2 mos, median OS 24.2 mos. However, 74% of participants pretrial had received lapatinib, capecitabine or both. |
| NCT01305941 | A Phase II Study Evaluating The Efficacy And Tolerability Of Everolimus (RAD001) In Combination With Trastuzumab And Vinorelbine In The Treatment Of Progressive HER2-Positive Breast Cancer Brain Metastases | UNC Lineberger Comprehensive Cancer Center | II | 32 | Completed | Everolimus, Trastuzumab, and Vinorelbine (vinca) | Intracranial response rate 4% (1 PR), clinical benefit rate 27% at 6 mos, median time to progression 3.9 mos, OS 12.2 mos. |
| NCT00967031 | A Multicenter Phase II Clinical Trial Assessing the Efficacy of the Combination of Lapatinib and Capecitabine in Patients With Non Pretreated Brain Metastasis From HER2 Positive Breast Cancer (LANDSCAPE) | UNICANCER | II | 45 | Completed | Lapatinib ditosylate, capecitabine | 66% (29/44) with PR, 49% (22/44) with grade 3 or 4 treatment-related adverse events (diarrhea, hand–foot), 4 patients had to discontinue due to toxicity, no toxic deaths |
| NCT01622868 | Phase II Randomized Study of Whole Brain Radiotherapy/Stereotactic Radiosurgery in Combination With Concurrent Lapatinib in Patients With Brain Metastasis From HER2-Positive Breast Cancer—A Collaborative Study of NRG Oncology and KROG | National Cancer Institute (NCI) (Bethesda, MD, USA) | II | 143 | Completed | Lapatinib | No significant difference in OS between arms of WBRT/SRS and WBRT/SRS with lapatinib; overall progression rate 70.4% in WBRT/SRS vs. 79.4% in WBRT/SRS with lapatinib |
| NCT04420598 | Multicenter, Open-Label, Single-Arm, Multicohort Phase II Clinical Trial of Trastuzumab Deruxtecan(DS-8201a) in Human Epidermal Growth Factor Receptor 2 HER2+ Advanced Breast Cancer With Brain Metastases and/or Leptomeningeal Carcinomatosis | MedSIR (Barcelona, Spain) | II | 41 | Completed | Trastuzumab deruxtecan | As of 10/2021: 16-week PFS 87.5%, overall intracranial ORR was 46.2%; all responders had partial responses, 2/21 (9.5%) suffered grade I pneumonitis/ILD |
| NCT01441596 | Lux-Breast 3; Randomised Phase II Study of Afatinib Alone or in Combination With Vinorelbine Versus Investigator’s Choice of Treatment in Patients with HER2 Positive Breast Cancer With Progressive Brain Metastases After Trastuzumab and/or Lapatinib Based Therapy | Boehringer Ingelheim (Ingelheim am Rhein, Germany) | II | 121 | Completed | Afatinib, Vinorelbine (vinca) | Patient benefit with afatinib-containing treatment arms (+/− vinorelbine) not different compared to investigator choice of treatment |
| NCT00263588 | A Phase II Study of Lapatinib for Brain Metastases in Subjects With ErbB2-Positive Breast Cancer Following Trastuzumab-based Systemic Therapy and Cranial Radiotherapy | Novartis Pharmaceuticals (Basel, Switzerland) | II | 242 | Completed | Lapatinib | 34 patients with CNS metastases included, ORR 21% with reported clinical improvement in neurologic symptoms; time to progression 22 weeks |
| NCT02260531 | A Phase II Study of Cabozantinib Alone or in Combination With Trastuzumab in Breast Cancer Patients With Brain Metastases | Dana-Farber Cancer Institute (Boston, MA, USA) | II | 36 | Completed | Cabozantinib (small molecule TKI) Trastuzumab | Insufficient activity among heavily pretreated BCBM patients (median 3 prior lines, craniotomy, WBRT/STS) |
| NCT02536339 | An Open-Label, Single-Arm, Phase II Study of Pertuzumab With High-Dose Trastuzumab for the Treatment of Central Nervous System Progression Post-Radiotherapy in Patients With HER2-Positive Metastatic Breast Cancer (PATRICIA) | Genentech, Inc. (South San Francisco, CA, USA) | II | 40 | Completed | Pertuzumab, High-Dose (6 mg/kg weekly) Trastuzumab | CNS ORR 11% with 4 PR, clinical benefit rate 68% at 4 months and 51% at 6 months |
| NCT00820222 | A Randomized, Multicentre, Open-Label, Phase III Study of Lapatinib Plus Capecitabine Versus Trastuzumab Plus Capecitabine in Patients With Anthracycline- or Taxane-Exposed ErbB2-Positive Metastatic (CEREBEL) | Novartis Pharmaceuticals (Basel, Switzerland) | III | 540 | Completed | Capecitabine, lapatinib, trastuzumab | Inconclusive for primary end point (incidence of CNS mets for patients without baseline CNS disease as first site of relapse), PFS longer with trastuzumab–capecitabine compared with lapatinib–capecitabine (HR 1.30, 95% CI 1.04 to 1.64) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Warrior, S.; Cohen-Nowak, A.; Kumthekar, P. Modern Management and Diagnostics in HER2+ Breast Cancer with CNS Metastasis. Cancers 2023, 15, 2908. https://doi.org/10.3390/cancers15112908
Warrior S, Cohen-Nowak A, Kumthekar P. Modern Management and Diagnostics in HER2+ Breast Cancer with CNS Metastasis. Cancers. 2023; 15(11):2908. https://doi.org/10.3390/cancers15112908
Chicago/Turabian StyleWarrior, Surbhi, Adam Cohen-Nowak, and Priya Kumthekar. 2023. "Modern Management and Diagnostics in HER2+ Breast Cancer with CNS Metastasis" Cancers 15, no. 11: 2908. https://doi.org/10.3390/cancers15112908
APA StyleWarrior, S., Cohen-Nowak, A., & Kumthekar, P. (2023). Modern Management and Diagnostics in HER2+ Breast Cancer with CNS Metastasis. Cancers, 15(11), 2908. https://doi.org/10.3390/cancers15112908






