Early Coronary Artery Calcification Progression over Two Years in Breast Cancer Patients Treated with Radiation Therapy: Association with Cardiac Exposure (BACCARAT Study)
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Radiotherapy
2.3. Radiation Doses
2.4. CAC CT Scans
2.5. Endpoint CAC Progression
2.6. Statistical Analyses
3. Results
3.1. Characteristics of The Study Population
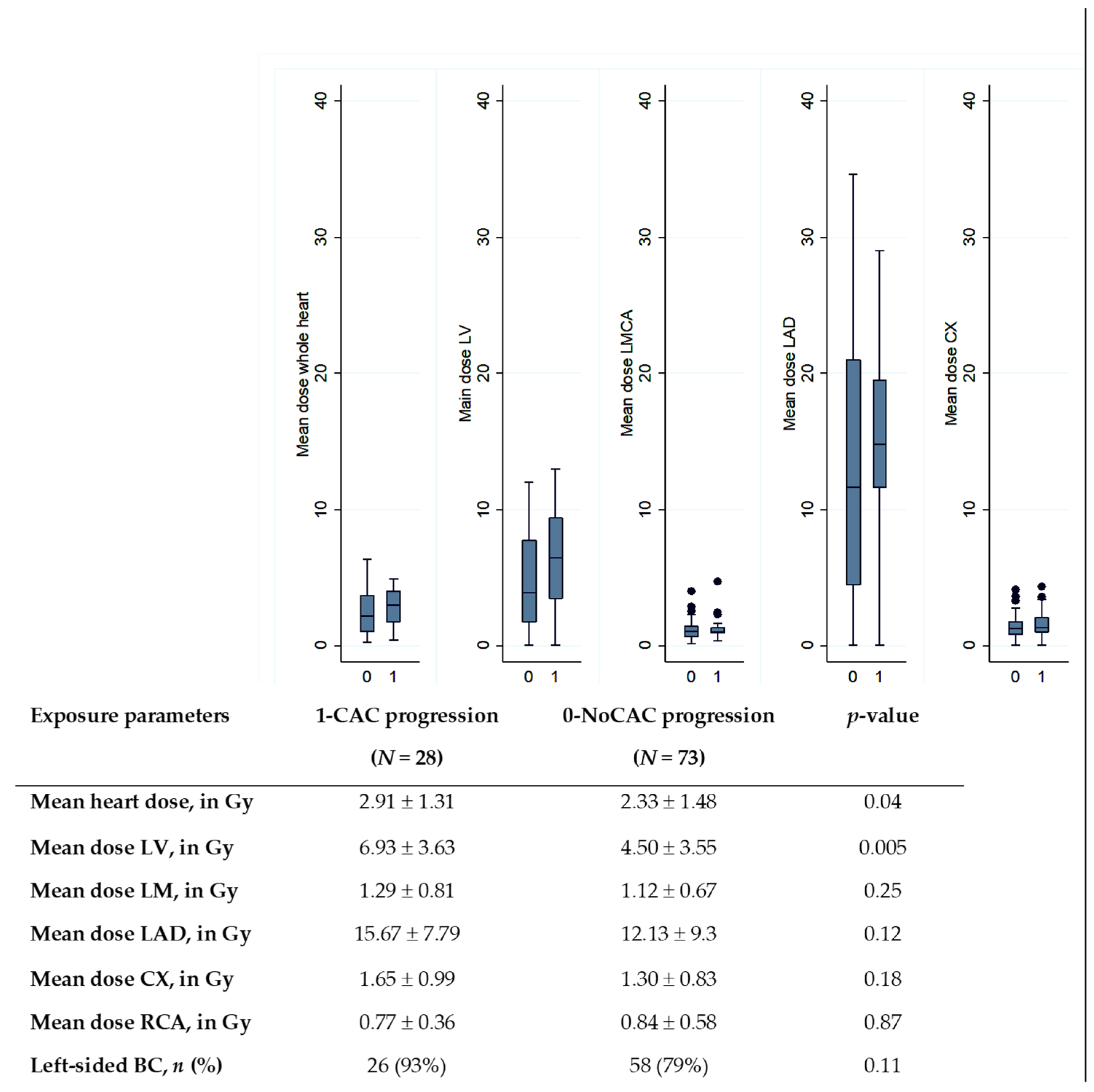
3.2. Cardiac Doses
3.3. CAC Progression
3.4. Association between CAC Progression and Non-radiation Cardiovascular Risk Factors
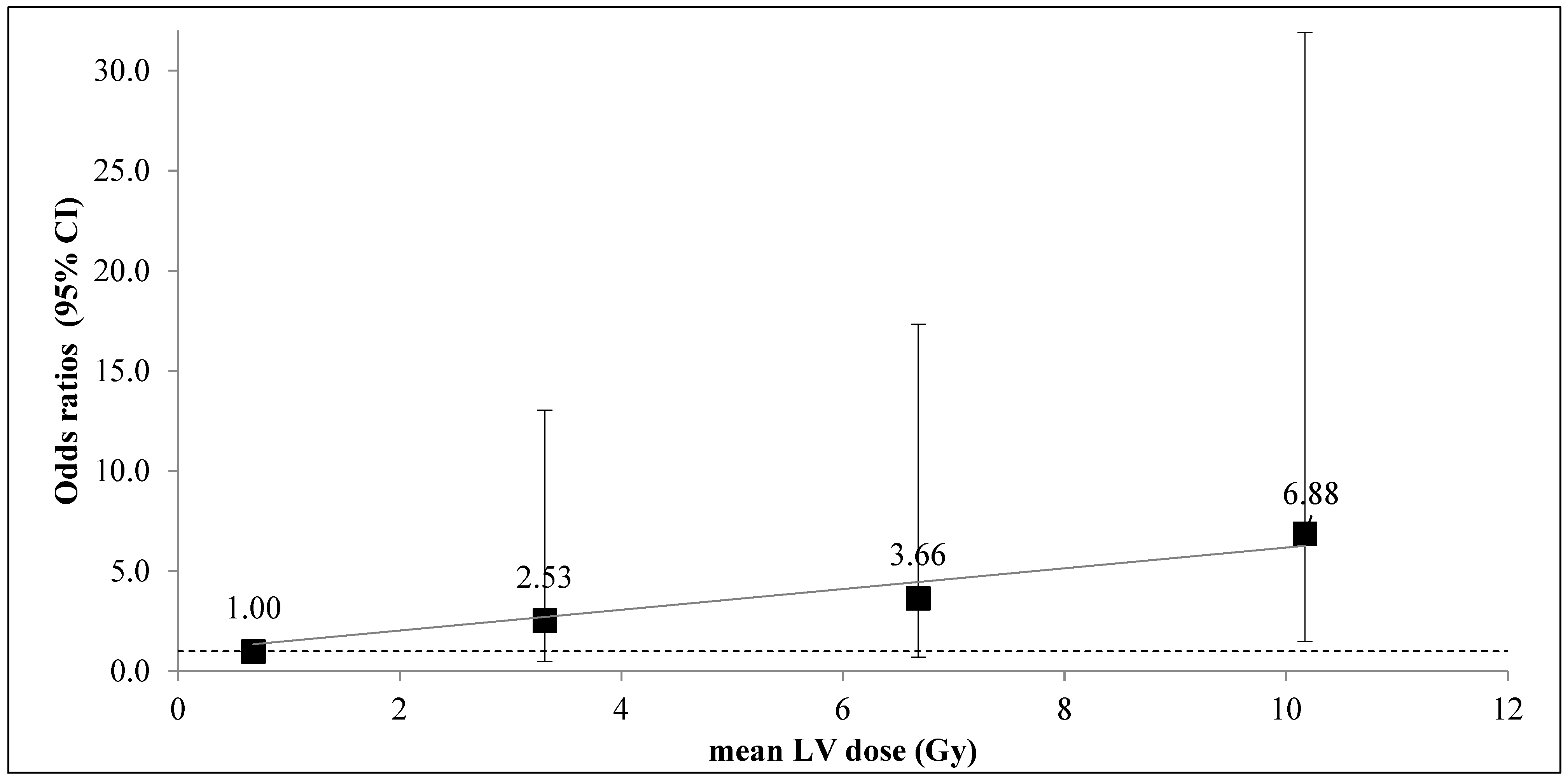
3.5. Association between CAC Progression and Cardiac Exposure
3.6. Association between CAC Increase in the LAD and Cardiac Exposure
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG); Darby, S.; McGale, P.; Correa, C.; Taylor, C.; Arriagada, R.; Clarke, M.; Cutter, D.; Davies, C.; Ewertz, M.; et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: Meta-analysis of individual patient data for 10 801 women in 17 randomised trials. Lancet 2011, 378, 1707–1716. [Google Scholar] [CrossRef] [PubMed]
- Bergom, C.; Bradley, J.A.; Ng, A.K.; Samson, P.; Robinson, C.; Lopez-Mattei, J.; Mitchell, J.D. Past, Present, and Future of Radiation-Induced Cardiotoxicity: Refinements in Targeting, Surveillance, and Risk Stratification. JACC CardioOncol. 2021, 3, 343–359. [Google Scholar] [CrossRef] [PubMed]
- Clarke, M.; Collins, R.; Darby, S.; Davies, C.; Elphinstone, P.; Evans, V.; Godwin, J.; Gray, R.; Hicks, C.; James, S.; et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: An overview of the randomised trials. Lancet 2005, 366, 2087–2106. [Google Scholar] [CrossRef]
- McGale, P.; Darby, S.C.; Hall, P.; Adolfsson, J.; Bengtsson, N.-O.; Bennet, A.M.; Fornander, T.; Gigante, B.; Jensen, M.-B.; Peto, R.; et al. Incidence of heart disease in 35,000 women treated with radiotherapy for breast cancer in Denmark and Sweden. Radiother. Oncol. 2011, 100, 167–175. [Google Scholar] [CrossRef]
- Darby, S.C.; Ewertz, M.; McGale, P.; Bennet, A.M.; Blom-Goldman, U.; Brønnum, D.; Correa, C.; Cutter, D.; Gagliardi, G.; Gigante, B.; et al. Risk of Ischemic Heart Disease in Women after Radiotherapy for Breast Cancer. N. Engl. J. Med. 2013, 368, 987–998. [Google Scholar] [CrossRef]
- van den Bogaard, V.A.; Ta, B.D.; Van Der Schaaf, A.; Bouma, A.B.; Middag, A.M.; Bantema-Joppe, E.J.; Van Dijk, L.V.; Van Dijk-Peters, F.B.; Marteijn, L.A.; De Bock, G.H.; et al. Validation and Modification of a Prediction Model for Acute Cardiac Events in Patients With Breast Cancer Treated With Radiotherapy Based on Three-Dimensional Dose Distributions to Cardiac Substructures. J. Clin. Oncol. 2017, 35, 1171–1178. [Google Scholar] [CrossRef]
- Greenland, P. Coronary Artery Calcium Score Combined With Framingham Score for Risk Prediction in Asymptomatic Individuals. JAMA 2004, 291, 210–215. [Google Scholar] [CrossRef]
- Gal, R.; van Velzen, S.G.M.; Hooning, M.J.; Emaus, M.J.; van der Leij, F.; Gregorowitsch, M.L.; Blezer, E.L.A.; Gernaat, S.A.M.; Lessmann, N.; Sattler, M.G.A.; et al. Identification of Risk of Cardiovascular Disease by Automatic Quantification of Coronary Artery Calcifications on Radiotherapy Planning CT Scans in Patients With Breast Cancer. JAMA Oncol. 2021, 7, 1024. [Google Scholar] [CrossRef]
- Kim, K.; Chung, S.Y.; Oh, C.; Cho, I.; Kim, K.H.; Byun, H.K.; Yoon, H.I.; Oh, J.; Chang, J.S. Automated coronary artery calcium scoring in patients with breast cancer to assess the risk of heart disease following adjuvant radiation therapy. Breast 2022, 65, 77–83. [Google Scholar] [CrossRef]
- Roos, C.T.; Bogaard, V.A.V.D.; Greuter, M.J.; Vliegenthart, R.; Schuit, E.; Langendijk, J.A.; van der Schaaf, A.; Crijns, A.P.; Maduro, J.H. Is the coronary artery calcium score associated with acute coronary events in breast cancer patients treated with radiotherapy? Radiother. Oncol. 2018, 126, 170–176. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, J.W.; Blaha, M.J.; DeFilippis, A.P.; Budoff, M.J.; Nasir, K.; Blumenthal, R.S.; Jones, S.R. Coronary Artery Calcium Progression: An Important Clinical Measurement?: A Review of Published Reports. J. Am. Coll. Cardiol. 2010, 56, 1613–1622. [Google Scholar] [CrossRef] [PubMed]
- Mast, M.E.; Heijenbrok, M.W.; Petoukhova, A.; Scholten, A.N.; Wolterbeek, R.; Schreur, J.H.M.; Struikmans, H.; Van Kempen-Harteveld, M.L. Less increase of CT-based calcium scores of the coronary arteries. Strahlenther. und Onkol. 2016, 192, 696–704. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.-H.; Chen, H.H.W.; Tsai, Y.-S. Accelerated coronary calcium burden in breast cancer patients after radiotherapy: A comparison with age and race matched healthy women. Radiat. Oncol. 2021, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Pathak, A.; Franck, D.; Latorzeff, I.; Jimenez, G.; Fondard, O.; Lapeyre, M.; Colombier, D.; Bruguiere, E.; Lairez, O.; et al. Early detection and prediction of cardiotoxicity after radiation therapy for breast cancer: The BACCARAT prospective cohort study. Radiat. Oncol. 2016, 11, 1–10. [Google Scholar] [CrossRef]
- Gagliardi, G.; Constine, L.S.; Moiseenko, V.; Correa, C.; Pierce, L.J.; Allen, A.M.; Marks, L.B. Radiation Dose–Volume Effects in the Heart. Int. J. Radiat. Oncol. 2010, 76, S77–S85. [Google Scholar] [CrossRef]
- Jacob, S.; Camilleri, J.; Derreumaux, S.; Walker, V.; Lairez, O.; Lapeyre, M.; Bruguière, E.; Pathak, A.; Bernier, M.-O.; Laurier, D.; et al. Is mean heart dose a relevant surrogate parameter of left ventricle and coronary arteries exposure during breast cancer radiotherapy: A dosimetric evaluation based on individually-determined radiation dose (BACCARAT study). Radiat. Oncol. 2019, 14, 1–10. [Google Scholar] [CrossRef]
- Agatston, A.S.; Janowitz, W.R.; Hildner, F.J.; Zusmer, N.R.; Viamonte, M., Jr.; Detrano, R. Quantification of coronary artery calcium using ultrafast computed tomography. J. Am. Coll. Cardiol. 1990, 15, 827–832. [Google Scholar] [CrossRef]
- Budoff, M.J.; Lane, K.L.; Bakhsheshi, H.; Mao, S.; Grassmann, B.O.; Friedman, B.C.; Brundage, B.H. Rates of progression of coronary calcium by electron beam tomography. Am. J. Cardiol. 2000, 86, 8–11. [Google Scholar] [CrossRef]
- Raggi, P.; Callister, T.Q.; Shaw, L.J. Progression of Coronary Artery Calcium and Risk of First Myocardial Infarction in Patients Receiving Cholesterol-Lowering Therapy. Arter. Thromb. Vasc. Biol. 2004, 24, 1272–1277. [Google Scholar] [CrossRef]
- Oei, H.-H.S.; Vliegenthart, R.; Hofman, A.; Oudkerk, M.; Witteman, J.C. Risk factors for coronary calcification in older subjects The Rotterdam Coronary Calcification Study. Eur. Hear. J. 2004, 25, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Maher, J.E.; Bielak, L.F.; Raz, J.A.; Sheedy, P.F.; Schwartz, R.S.; Peyser, P.A. Progression of Coronary Artery Calcification: A Pilot Study. Mayo Clin. Proc. 1999, 74, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Schmermund, A.; Baumgart, D.; Möhlenkamp, S.; Kriener, P.; Pump, H.; Grönemeyer, D.; Seibel, R.; Erbel, R. Natural History and Topographic Pattern of Progression of Coronary Calcification in Symptomatic Patients. Arter. Thromb. Vasc. Biol. 2001, 21, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Takx, R.A.P.; Vliegenthart, R.; Schoepf, U.J.; Pilz, L.R.; Schoenberg, S.O.; Morris, P.B.; Henzler, T.; Apfaltrer, P. Coronary artery calcium in breast cancer survivors after radiation therapy. Int. J. Cardiovasc. Imaging 2017, 353, 1425–1431. [Google Scholar] [CrossRef] [PubMed]
- Tjessem, K.H.; Bosse, G.; Fosså, K.; Reinertsen, K.V.; Fosså, S.D.; Johansen, S.; Fosså, A. Coronary calcium score in 12-year breast cancer survivors after adjuvant radiotherapy with low to moderate heart exposure – Relationship to cardiac radiation dose and cardiovascular risk factors. Radiother. Oncol. 2015, 114, 328–334. [Google Scholar] [CrossRef]
- Taylor, A.J.; Bindeman, J.; Feuerstein, I.; Cao, F.; Brazaitis, M.; O’Malley, P.G. Coronary Calcium Independently Predicts Incident Premature Coronary Heart Disease Over Measured Cardiovascular Risk Factors: Mean Three-Year Outcomes in the Prospective Army Coronary Calcium (PACC) Project. J. Am. Coll. Cardiol. 2005, 46, 807–814. [Google Scholar] [CrossRef]
- Gopal, A.; Nasir, K.; Liu, S.T.; Flores, F.R.; Chen, L.; Budoff, M.J. Coronary calcium progression rates with a zero initial score by electron beam tomography. Int. J. Cardiol. 2007, 117, 227–231. [Google Scholar] [CrossRef]
- Simonetto, C.; Kaiser, J.C.; Bogaard, V.A.V.D.; Langendijk, J.A.; Crijns, A.P. Breast cancer radiotherapy and the risk of acute coronary events–Insights from a process oriented model. Int. J. Radiat. Oncol. 2022, 114, 409–415. [Google Scholar] [CrossRef]
- Nilsson, G.; Holmberg, L.; Garmo, H.; Duvernoy, O.; Sjögren, I.; Lagerqvist, B.; Blomqvist, C. Distribution of Coronary Artery Stenosis After Radiation for Breast Cancer. J. Clin. Oncol. 2012, 30, 380–386. [Google Scholar] [CrossRef]
- Locquet, M.; Spoor, D.; Crijns, A.; van der Harst, P.; Eraso, A.; Guedea, F.; Fiuza, M.; Santos, S.C.R.; Combs, S.; Borm, K.; et al. Subclinical Left Ventricular Dysfunction Detected by Speckle-Tracking Echocardiography in Breast Cancer Patients Treated With Radiation Therapy: A Six-Month Follow-Up Analysis (MEDIRAD EARLY-HEART study). Front. Oncol. 2022, 12. [Google Scholar] [CrossRef]
- Walker, V.; Crijns, A.; Langendijk, J.; Spoor, D.; Vliegenthart, R.; Combs, S.E.; Mayinger, M.; Eraso, A.; Guedea, F.; Fiuza, M.; et al. Early Detection of Cardiovascular Changes After Radiotherapy for Breast Cancer: Protocol for a European Multicenter Prospective Cohort Study (MEDIRAD EARLY HEART Study). JMIR Res. Protoc. 2018, 7, e178. [Google Scholar] [CrossRef] [PubMed]
| Variables | Patients N = 101 |
|---|---|
| Age in years, mean ± SD | 58.4 ± 8.1 |
| Cancer treatment | |
| Laterality of BC, n (%) Left-sided BC Right-sided BC | 84 (83.2%) 17 (16.8%) |
| Histology, n (%) In situ Invasive | 19 (18.8%) 82 (81.2%) |
| Cancer grade, n (%) 1 2 3 | 39 (38.6 %) 50 (49.5%) 12 (11.9%) |
| Type of surgery, n (%) Conservative Mastectomy | 94 (93.1%) 7 (6.9%) |
| Protocol of radiotherapy, n (%) 50 Gy (25 x 2Gy) 47 Gy (20 x 2.35Gy) | 76 (75.2%) 25 (24.8%) |
| Regional lymph nodes irradiation, n (%) No Yes (Supraclavicular and/or Internal mammary Chain) | 73 (72.3%) 28 (27.7%) |
| Boost, n (%) No Yes | 9 (8.9%) 92 (91.1%) |
| Adjuvant endocrine therapy, n (%) No Yes Anti-aromatase * Tamoxifen * | 24 (23.8%) 77 (76.2%) 45 32 |
| Cardiovascular risk factors | |
| Body mass index in kg/m², mean ± SD | 24.4 ± 4.1 |
| Cardiovascular treatment, n (%) | 15 (14.8) |
| Diabetes mellitus, n (%) | 7 (6.9%) |
| Hypertension, n (%) | 15 (14.8%) |
| Smoking status, n (%) No Former Current | 55 (54.4%) 24 (23.7%) 22 (21.7%) |
| Dosimetric Variables | All Patients N = 101 | Right-Sided BC N = 17 | Left-Sided BC N = 84 | Comparison Right vs. Left |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | p-Value 1 | |
| Whole heart Mean dose (Gy) D2(Gy) V2(%) V5 (%) | 2.49 ± 1.45 22.67 ± 17.85 24.0 ± 14.9 7.6 ± 6.4 | 0.61 ± 0.46 2.47 ± 1.14 6.7 ± 13.0 0.3 ± 1.0 | 2.87 ± 1.28 26.76 ± 16.83 27.4 ± 12.7 9.1 ± 6.0 | <0.001 <0.001 <0.001 <0.001 |
| Left ventricle Mean dose (Gy) D2(Gy) V2(%) V5 (%) | 5.17 ± 3.72 28.62 ± 18.93 40.4 ±22.2 18.2 ± 12.5 | 0.17 ± 0.29 0.54 ± 0.60 1.0 ± 4.3 0 ± 0 | 6.18 ± 3.24 34.30 ± 15.40 48.4 ± 14.5 21.9 ± 10.3 | <0.001 <0.001 <0.001 - |
| LMCA Mean dose (Gy) D2(Gy) V2(%) V5 (%) | 1.17 ± 0.71 1.48 ± 0.91 8.9 ± 25.1 0 ± 0 | 0.63 ± 0.76 0.69 ± 0.80 8.3 ± 23.4 0 ± 0 | 1.27 ± 0.66 1.64 ± 0.84 11.7 ± 33.2 0 ± 0 | <0.001 <0.001 0.431 - |
| LAD Mean dose (Gy) D2(Gy) V2(%) V5 (%) | 13.11 ± 9.02 32.13 ± 19.25 71.9 ± 33.3 46.7 ± 28.1 | 0.28 ± 0.53 0.51 ± 0.74 6.6 ± 22.2 0 ± 0 | 15.71 ± 7.57 38.53 ± 14.14 85.1 ± 13.8 56.2 ± 20.3 | <0.001 <0.001 <0.001 - |
| CX Mean dose (Gy) D2(Gy) V2(%) V5 (%) | 1.40 ± 0.89 2.36 ± 4.79 18.3 ± 30.2 0.5 ± 4.6 | 0.28 ± 0.43 0.53 ± 0.72 2.9 ± 8.2 0 ± 0 | 1.63 ± 0.78 2.73 ± 5.16 21.4 ± 32.0 0.6 ± 5.1 | <0.001 <0.001 <0.001 - |
| RCA Mean dose (Gy) D2(Gy) V2(%) V5 (%) | 0.82 ± 0.53 1.42 ± 0.84 5.0 ± 15.1 0.14 ± 1.48 | 1.46 ± 0.78 2.10 ± 1.23 17.5 ± 27.0 0.87 ± 3.60 | 0.69 ± 0.34 1.28 ± 0.67 2.4 ± 9.8 0 ± 0 | <0.001 <0.001 <0.001 - |
| CAC Description | All Patients N = 101 | Right-Sided BC N = 17 | Left-Sided BC N = 84 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Before RT | RT+ Two Years | p-Value | Before RT | RT+ Two Years | p-Value | Before RT | RT+ Two Years | p-Value | |
| Overall CAC | |||||||||
| Non-zero CAC, N (%) | 25 (24.7%) | 30 (29.7%) | 0.062 | 3 (17.6%) | 3 (17.6%) | 1.000 1 | 22 (26.2%) | 27 (32.1%) | 0.062 1 |
| Median/Mean (± SD) | 0/35.8 (± 119.1) | 0/47.7 (± 140.0) | <0.001 | 0/3.2 (± 11.1) | 0/4.5 (± 14.9) | 0.158 2 | 0/42.4 (± 129.5) | 0/56.4 (± 151.9) | <0.001 2 |
| CAC progression, N (%) | 28 (27.7%) | 2 (11.7%) | 26 (30.1%) | ||||||
| Coronary artery-specific CAC | |||||||||
| LMCA CAC | |||||||||
| Non-zero CAC, N (%) | 2 (2.0%) | 2 (2.0%) | 1.000 | 0 | 0 | 1.000 1 | 2 (2.4%) | 2 (2.4%) | 1.000 1 |
| Median/Mean (± SD) | 0/0.3 (±2.8) | 0/ 0.5 (±4.9) | 0.157 | 0 | 0 | 1.000 2 | 0/ 0.4 (±3.1) | 0/ 0.6 (±5.4) | 0.157 2 |
| Increased CAC, N (%) | 2 (2.0%) | 0 | 2 (2.4%) | ||||||
| LAD CAC | |||||||||
| Non-zero CAC, N (%) | 20 (19.8%) | 26 (25.7%) | 0.031 | 1 (5.9%) | 2 (11.8%) | 1.000 1 | 19 (22.6%) | 24 (28.5%) | 0.062 1 |
| Median/Mean (± SD) | 0/20.6 (±58.9) | 0/ 27.6 (±74.3) | <0.001 | 0/ 0.3 (±1.5) | 0/ 1.0 (±3.4) | 0.158 2 | 0/ 24.7 (±63.9) | 0/ 33.1 (±80.5) | <0.001 2 |
| Increased CAC, N (%) | 26 (25.7%) | 2 (11.8%) | 24 (28.6%) | ||||||
| CX CAC | |||||||||
| Non-zero CAC, N (%) | 7 (6.9%) | 10 (9.9%) | 0.250 | 0 | 0 | 1.000 1 | 7 (8.3%) | 10 (11.9%) | 0.250 1 |
| Median/Mean (± SD) | 0/3.7 (±23.5) | 0/ 5.2 (±26.3) | 0.016 | 0 | 0 | 1.000 2 | 0/4.48±25.80 | 0/6.2 (±28.8) | 0.016 2 |
| Increased CAC, N (%) | 10 (9.9%) | 0 | 10 (11.9%) | ||||||
| RCA CAC | |||||||||
| Non-zero CAC, N (%) | 15 (14.8%) | 17 (16.8%) | 0.500 | 2 (11.7%) | 2 (11.7%) | 1.000 1 | 13 (15.4%) | 15 (17.8%) | 0.500 1 |
| Median/Mean ± SD | 0/11.2 (±55.2) | 0/16.3 (±68.9) | <0.001 | 0/2.8 (±11.1) | 0/3.7 (±14.7) | 0.158 2 | 0/12.8(±60.3) | 0/18.8 (±75.1) | <0.001 2 |
| Increased CAC, N (%) | 16 (16.7%) | 2 (11.7%) | 14 (16.7%) | ||||||
| Variables | OR (95% CI) | p-Value |
|---|---|---|
| Age, in years | 1.09 (1.03–1.16) | 0.005 |
| BMI, in kg/m² | 1.09 (0.98–1.21) | 0.107 |
| arterial hypertension | 3.71 (1.20–11.51) | 0.023 |
| Diabetes | 7.72 (1.40–42.50) | 0.019 |
| Smoking (former or current) | 2.15 (0.76–6.11) | 0.151 |
| Hypercholesterolemia | 1.86 (0.75–4.59) | 0.179 |
| Cardiovascular treatment | 5.29 (1.67–16.73) | 0.005 |
| Baseline CAC score > 0 | 163.3 (29.6–899.0) | <0.0001 |
| Endocrine therapy | 0.55 (0.21–1.45) | 0.224 |
| Exposure Variables | Univariate Model | Multivariable Model 1 | Multivariable Model 2 | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Left vs. Right-sided BC | 3.36 (0.72–15.78) | 0.12 | 3.22 (0.61–16.80) | 0.16 | 16.55 (0.091–302.26) | 0.08 |
| Heart | ||||||
| Mean dose, in Gy | 1.32 (0.97–1.80) | 0.07 | 1.29 (0.91–1.84) | 0.15 | 1.74 (0.94–3.21) | 0.08 |
| D2, in Gy | 1.03 (1.00–1.06) | 0.02 | 1.02 (0.99–1.05) | 0.13 | 1.03 (0.98–1.07) | 0.23 |
| V2, in % | 1.03 (0.99–1.05) | 0.10 | 1.01 (0.98–1.05) | 0.43 | 1.07 (1.01–1.12) | 0.01 |
| V5, in % | 1.04 (0.97–1.11) | 0.28 | 1.05 (0.97–1.14) | 0.25 | 1.11 (0.98–1.26) | 0.08 |
| Left Ventricle | ||||||
| Mean dose, in Gy | 1.20 (1.06–1.37) | 0.01 | 1.15 (1.00–1.32) | 0.04 | 1.29 (1.01–1.65) | 0.04 |
| D2, in Gy | 1.05 (1.02–1.08) | 0.01 | 1.04 (1.01–1.07) | 0.02 | 1.07 (1.01–1.14) | 0.03 |
| V2, in % | 1.03 (1.01–1.06) | 0.01 | 1.03 (0.99–1.06) | 0.05 | 1.07 (1.01–1.12) | 0.01 |
| V5, in % | 1.05 (1.01–1.09) | 0.02 | 1.04 (0.99–1.08) | 0.09 | 1.01 (1.01–1.19) | 0.02 |
| Exposure Variables | Univariate Model | Multivariable Model * | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Left vs. Right-sided BC | 3.00 (0.63–14.1) | 0.16 | 2.75 (0.54–14.11) | 0.22 |
| Heart | ||||
| Mean dose, in Gy | 1.24 (0.91–1.69) | 0.17 | 1.18 (0.82–1.70) | 0.36 |
| D2, in Gy | 1.03 (1.00–1.05) | 0.06 | 1.01 (0.99–1.04) | 0.34 |
| V2, in % | 1.02 (0.99–1.05) | 0.15 | 1.01 (0.98–1.05) | 0.54 |
| V5, in Gy | 1.03 (0.96–1.10) | 0.42 | 1.03 (0.95–1.12) | 0.43 |
| Left Ventricle | ||||
| Mean dose, in Gy | 1.20 (1.05–1.36) | 0.01 | 1.14 (0.99–1.31) | 0.06 |
| D2, in Gy | 1.04(1.01–1.07) | 0.01 | 1.03 (1.00–1.06) | 0.06 |
| V2, in % | 1.04 (1.01–1.06) | 0.01 | 1.03 (1.00–1.06) | 0.04 |
| V5, in Gy | 1.05 (1.01–1.09) | 0.02 | 1.04 (0.99–1.09) | 0.09 |
| LAD | ||||
| Mean dose, in Gy | 1.03 (0.98–1.09) | 0.20 | 1.04 (0.99–1.10) | 0.14 |
| D2, in Gy | 1.04 (1.01–1.07) | 0.02 | 1.03 (1.00–1.06) | 0.07 |
| V2, in % | 1.02 (1.00–1.03) | 0.08 | 1.02 (1.00–1.04) | 0.08 |
| V5, in Gy | 1.01 (0.99–1.03) | 0.31 | 1.01 (0.99–1.03) | 0.21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Honaryar, M.K.; Allodji, R.; Ferrières, J.; Panh, L.; Locquet, M.; Jimenez, G.; Lapeyre, M.; Camilleri, J.; Broggio, D.; de Vathaire, F.; et al. Early Coronary Artery Calcification Progression over Two Years in Breast Cancer Patients Treated with Radiation Therapy: Association with Cardiac Exposure (BACCARAT Study). Cancers 2022, 14, 5724. https://doi.org/10.3390/cancers14235724
Honaryar MK, Allodji R, Ferrières J, Panh L, Locquet M, Jimenez G, Lapeyre M, Camilleri J, Broggio D, de Vathaire F, et al. Early Coronary Artery Calcification Progression over Two Years in Breast Cancer Patients Treated with Radiation Therapy: Association with Cardiac Exposure (BACCARAT Study). Cancers. 2022; 14(23):5724. https://doi.org/10.3390/cancers14235724
Chicago/Turabian StyleHonaryar, Manoj Kumar, Rodrigue Allodji, Jean Ferrières, Loïc Panh, Médéa Locquet, Gaelle Jimenez, Matthieu Lapeyre, Jérémy Camilleri, David Broggio, Florent de Vathaire, and et al. 2022. "Early Coronary Artery Calcification Progression over Two Years in Breast Cancer Patients Treated with Radiation Therapy: Association with Cardiac Exposure (BACCARAT Study)" Cancers 14, no. 23: 5724. https://doi.org/10.3390/cancers14235724
APA StyleHonaryar, M. K., Allodji, R., Ferrières, J., Panh, L., Locquet, M., Jimenez, G., Lapeyre, M., Camilleri, J., Broggio, D., de Vathaire, F., & Jacob, S. (2022). Early Coronary Artery Calcification Progression over Two Years in Breast Cancer Patients Treated with Radiation Therapy: Association with Cardiac Exposure (BACCARAT Study). Cancers, 14(23), 5724. https://doi.org/10.3390/cancers14235724








