Lung Subregion Partitioning by Incremental Dose Intervals Improves Omics-Based Prediction for Acute Radiation Pneumonitis in Non-Small-Cell Lung Cancer Patients
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
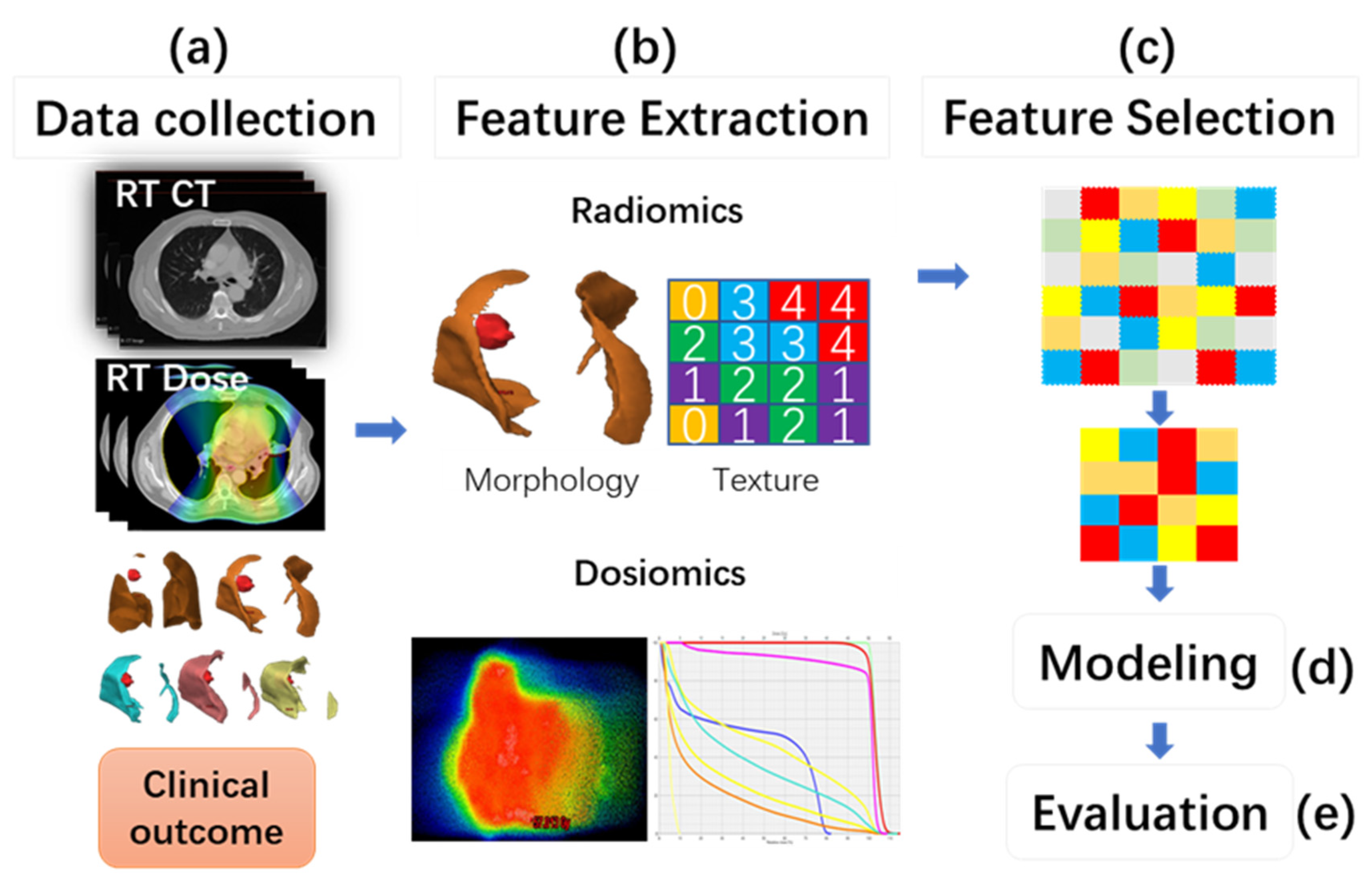
2.1. Study Workflow
2.2. Patient Data
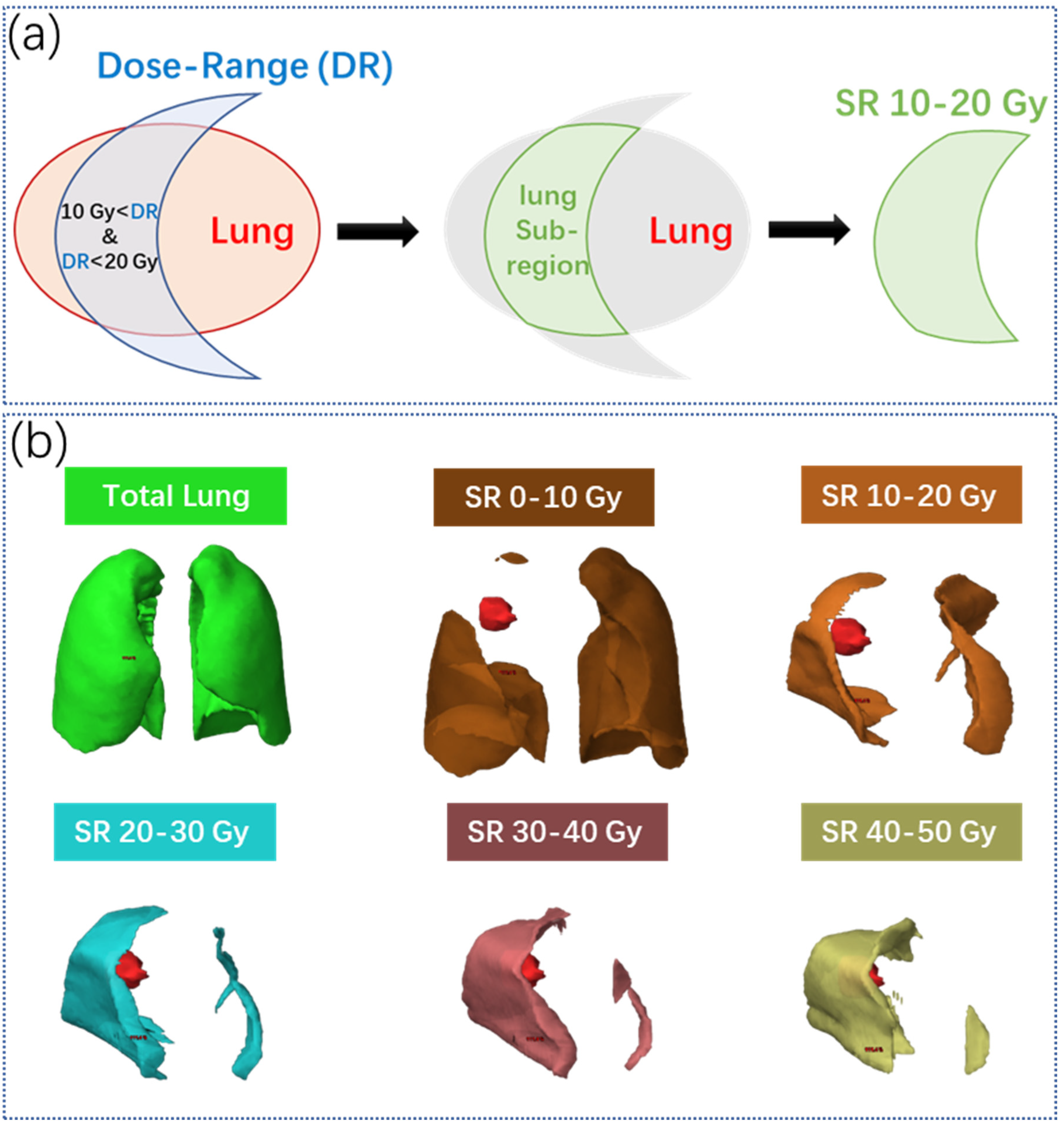
2.3. Lung Sub-Region Partitioning
2.4. Feature Extraction
- Scale-invariant 3D dose moments [19]: They describe the weighted dose center within the organ-at-risk (OAR) volume with varying orders along with anterior–posterior, medial–lateral, and craniocaudal directions [22]. In this study, the maximum order of 3 was chosen for each dimension, resulting in 64 possible combinations of orders. Scale invariance can be calculated by: , where , and are the orders in three directions, and is central moments which are defined in [19]. Since the order of , , results in a constant value of 1, a total of 63 dose moments were included in the dosiomics feature set.
- DVH parameters [20,21]: DVH summarizes the dose accumulation within a volume. It is defined as the isodose volume at varying levels of doses and is widely used in the clinic for convenient dose comparisons. DVH parameters, which are the dose values at specific volumes or volume values at specific doses, were commonly used as the evaluation metrics for plan quality assessment. In this study, we selected multiple DVH parameters of Vx and Dx from the DVH curve, where Vx was the volumes or relative volumes (of the whole organ) receiving more than x Gy, and Dx was the dose (Gy) to x% of the whole lung.
- Dosiomics [9]: A total of 91 first-order and higher-order radiomics features were extracted from the dose map to describe the dose histogram statistics and dose texture. Only the original dose map was employed without further preprocessing.
- In total, 213 dose features for each lung SR and the whole lung were extracted, resulting in 1278 dose features in total.
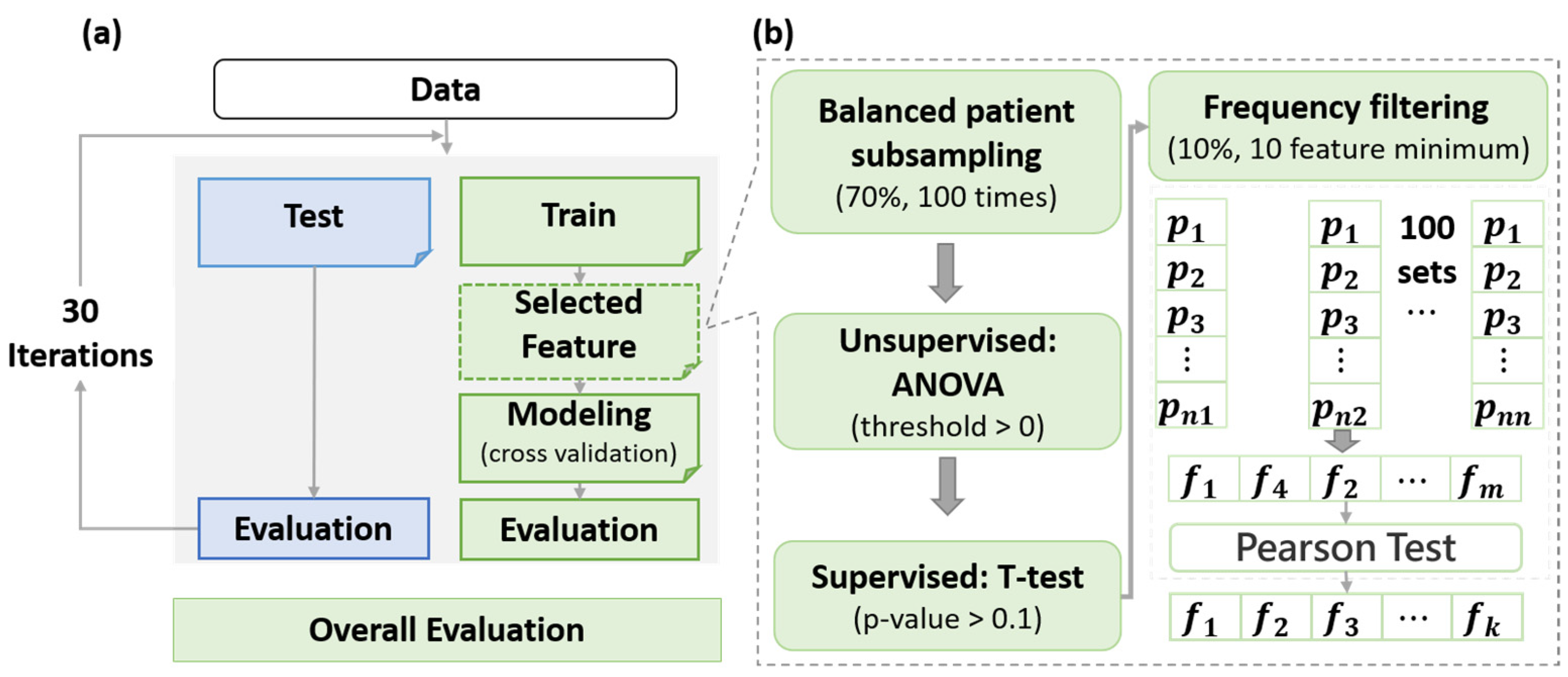
2.5. Feature Selection
2.6. Model Construction and Evaluation
3. Results
3.1. Patient Characteristics
3.2. Selected Features
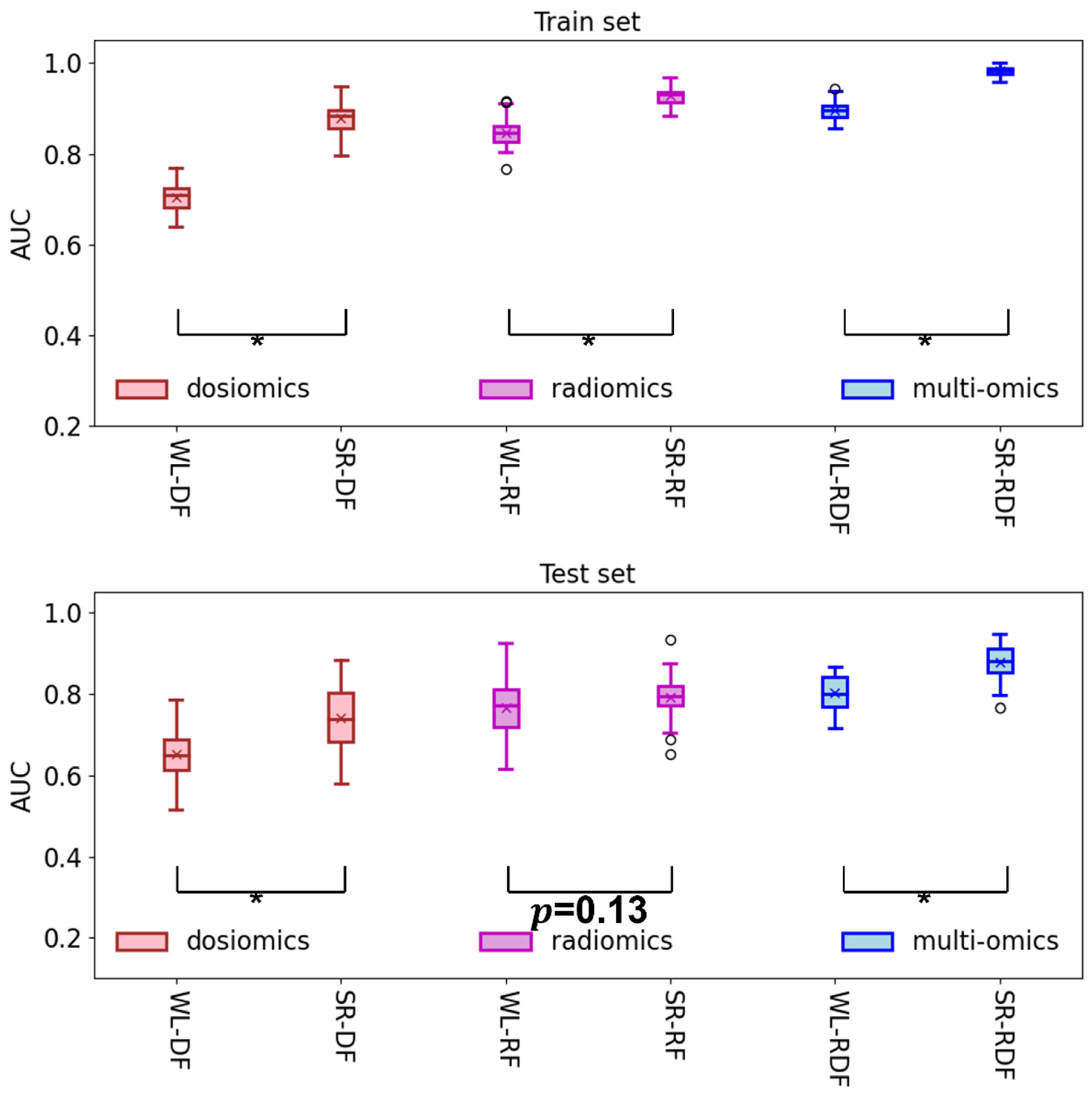
3.3. Model Evaluation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Cancer statistics for the year 2020: An overview. Int. J. Cancer 2021, 149, 778–789. [Google Scholar] [CrossRef] [PubMed]
- Schild, S.E. Optimizing the Radiotherapy of Lung Cancer. J. Thorac. Oncol. 2020, 15, 1559–1560. [Google Scholar] [CrossRef] [PubMed]
- Vinod, S.K.; Hau, E. Radiotherapy treatment for lung cancer: Current status and future directions. Respirology 2020, 25, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.-C.; Hsu, F.-M.; Yang, P.-C. Precision radiotherapy for non-small cell lung cancer. J. Biomed. Sci. 2020, 27, 82. [Google Scholar] [CrossRef] [PubMed]
- Baisden, J.M.; Romney, D.A.; Reish, A.G.; Cai, J.; Sheng, K.; Jones, D.R.; Benedict, S.H.; Read, P.W.; Larner, J.M. Dose as a function of lung volume and planned treatment volume in helical tomotherapy intensity-modulated radiation therapy-based stereotactic body radiation therapy for small lung tumors. Int. J. Radiat. Oncol. Biol. Phys. 2007, 68, 1229–1237. [Google Scholar] [CrossRef]
- Ge, H.; Cai, J.; Kelsey, C.R.; Yin, F.F. Quantification and minimization of uncertainties of internal target volume for stereotactic body radiation therapy of lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, 438–443. [Google Scholar] [CrossRef]
- Lafata, K.; Cai, J.; Wang, C.; Hong, J.; Kelsey, C.R.; Yin, F.F. Spatial-temporal variability of radiomic features and its effect on the classification of lung cancer histology. Phys. Med. Biol. 2018, 63, 225003. [Google Scholar] [CrossRef]
- Boonyawan, K.; Gomez, D.R.; Komaki, R.; Xu, Y.; Nantavithya, C.; Allen, P.K.; Mohan, R.; Liao, Z. Clinical and Dosimetric Factors Predicting Grade ≥2 Radiation Pneumonitis After Postoperative Radiotherapy for Patients With Non-Small Cell Lung Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2018, 101, 919–926. [Google Scholar] [CrossRef]
- Liang, B.; Yan, H.; Tian, Y.; Chen, X.; Yan, L.; Zhang, T.; Zhou, Z.; Wang, L.; Dai, J. Dosiomics: Extracting 3D Spatial Features From Dose Distribution to Predict Incidence of Radiation Pneumonitis. Front. Oncol. 2019, 9, 269. [Google Scholar] [CrossRef]
- Bourbonne, V.; Da-ano, R.; Jaouen, V.; Lucia, F.; Dissaux, G.; Bert, J.; Pradier, O.; Visvikis, D.; Hatt, M.; Schick, U. Radiomics analysis of 3D dose distributions to predict toxicity of radiotherapy for lung cancer. Radiother. Oncol. 2021, 155, 144–150. [Google Scholar] [CrossRef]
- Jiang, W.; Song, Y.; Sun, Z.; Qiu, J.; Shi, L. Dosimetric Factors and Radiomics Features Within Different Regions of Interest in Planning CT Images for Improving the Prediction of Radiation Pneumonitis. Int. J. Radiat. Oncol. Biol. Phys. 2021, 110, 1161–1170. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Malhotra, H.K.; Orton, C.G. A 3D-conformal technique is better than IMRT or VMAT for lung SBRT. Med. Phys. 2014, 41, 040601. [Google Scholar] [CrossRef] [PubMed]
- Seppenwoolde, Y.; De Jaeger, K.; Boersma, L.J.; Belderbos, J.S.A.; Lebesque, J.V. Regional differences in lung radiosensitivity after radiotherapy for non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2004, 60, 748–758. [Google Scholar] [CrossRef]
- Seppenwoolde, Y.; Muller, S.H.; Theuws, J.C.M.; Baas, P.; Belderbos, J.S.A.; Boersma, L.J.; Lebesque, J.V. Radiation dose-effect relations and local recovery in perfusion for patients with non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2000, 47, 681–690. [Google Scholar] [CrossRef]
- O’Reilly, S.; Jain, V.; Huang, Q.; Cheng, C.; Teo, B.K.K.; Yin, L.; Zhang, M.; Diffenderfer, E.; Li, T.; Levin, W.; et al. Dose to Highly Functional Ventilation Zones Improves Prediction of Radiation Pneumonitis for Proton and Photon Lung Cancer Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2020, 107, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Chopra, N.; Dou, T.; Sharp, G.; Sajo, E.; Mak, R.H. A Combined Radiomics-Dosiomics Machine Learning Approach Improves Prediction of Radiation Pneumonitis Compared to DVH Data in Lung Cancer Patients. Int. J. Radiat. Oncol. 2020, 108, e777. [Google Scholar] [CrossRef]
- Adachi, T.; Nakamura, M.; Shintani, T.; Mitsuyoshi, T.; Kakino, R.; Ogata, T.; Ono, T.; Tanabe, H.; Kokubo, M.; Sakamoto, T.; et al. Multi-institutional dose-segmented dosiomic analysis for predicting radiation pneumonitis after lung stereotactic body radiation therapy. Med. Phys. 2021, 48, 1781–1791. [Google Scholar] [CrossRef]
- Van Griethuysen, J.J.M.; Fedorov, A.; Parmar, C.; Hosny, A.; Aucoin, N.; Narayan, V.; Beets-Tan, R.G.H.; Fillion-Robin, J.C.; Pieper, S.; Aerts, H.J.W.L. Computational radiomics system to decode the radiographic phenotype. Cancer Res. 2017, 77, e104–e107. [Google Scholar] [CrossRef]
- Buettner, F.; Miah, A.B.; Gulliford, S.L.; Hall, E.; Harrington, K.J.; Webb, S.; Partridge, M.; Nutting, C.M. Novel approaches to improve the therapeutic index of head and neck radiotherapy: An analysis of data from the PARSPORT randomised phase III trial. Radiother. Oncol. 2012, 103, 82–87. [Google Scholar] [CrossRef]
- Faught, A.M.; Yamamoto, T.; Castillo, R.; Castillo, E.; Zhang, J.; Miften, M.; Vinogradskiy, Y. Evaluating which dose-function metrics are most critical for functional-guided radiotherapy with CT ventilation imaging. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 202–209. [Google Scholar] [CrossRef]
- Marks, L.B.; Bentzen, S.M.; Deasy, J.O.; Kong, F.M.; Bradley, J.D.; Vogelius, I.S.; El Naqa, I.; Hubbs, J.L.; Lebesque, J.V.; Timmerman, R.D.; et al. Radiation Dose-Volume Effects in the Lung. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Pham, M.T.; Woodford, O.J.; Perbet, F.; Maki, A.; Stenger, B.; Cipolla, R. A new distance for scale-invariant 3D shape recognition and registration. Proc. IEEE Int. Conf. Comput. Vis. 2011, 145–152. [Google Scholar] [CrossRef]
- Zheng, A.; Casari, A. Feature Engineering for Machine Learning: Principles and Techniques for Data Scientists; O’Reilly Media, Inc.: Sebastopol, CA, USA, 2016. [Google Scholar]
- Mukaka, M.M. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar] [PubMed]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G.M. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. Ann. Intern. Med. 2015, 162, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-learn: Machine Learning in Python Fabian. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar] [CrossRef]
- Borghetti, P.; Guerini, A.E.; Sangalli, C.; Piperno, G.; Franceschini, D.; La Mattina, S.; Arcangeli, S.; Filippi, A.R. Unmet needs in the management of unresectable stage III non-small cell lung cancer: A review after the ‘radio talk’ webinars. Expert Rev. Anticancer Ther. 2022, 22, 549–559. [Google Scholar] [CrossRef]
- Lee, E.; Zeng, J.; Miyaoka, R.S.; Saini, J.; Kinahan, P.E.; Sandison, G.A.; Wong, T.; Vesselle, H.J.; Rengan, R.; Bowen, S.R. Functional lung avoidance and response-adaptive escalation (FLARE) RT: Multimodality plan dosimetry of a precision radiation oncology strategy: Multimodality. Med. Phys. 2017, 44, 3418–3429. [Google Scholar] [CrossRef]
- Li, P.; Li, X.; Dai, L.; Zheng, X.; Wang, X.; Huang, Q.; Ma, X. A Unified Framework to Integrate SPECT Perfusion Imaging with Dose-volume Metrics for Estimation of Radiation Pneumonitis. 2020. Res. Square 2020. [Google Scholar] [CrossRef]
- Owen, D.R.; Sun, Y.; Boonstra, P.S.; McFarlane, M.; Viglianti, B.L.; Balter, J.M.; El Naqa, I.; Schipper, M.J.; Schonewolf, C.A.; Ten Haken, R.K.; et al. Investigating the SPECT Dose-Function Metrics Associated With Radiation-Induced Lung Toxicity Risk in Patients With Non-small Cell Lung Cancer Undergoing Radiation Therapy. Adv. Radiat. Oncol. 2021, 6, 100666. [Google Scholar] [CrossRef]
- Cai, J.; Read, P.W.; Larner, J.M.; Jones, D.R.; Benedict, S.H.; Sheng, K. Reproducibility of interfraction lung motion probability distribution function using dynamic MRI: Statistical analysis. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 1228–1235. [Google Scholar] [CrossRef]
- Joseph, D.; Denham, J.W.; Steigler, A.; Lamb, D.S.; Spry, N.A.; Stanley, J.; Shannon, T.; Duchesne, G.; Atkinson, C.; Matthews, J.H.L.; et al. Radiation Dose Escalation or Longer Androgen Suppression to Prevent Distant Progression in Men With Locally Advanced Prostate Cancer: 10-Year Data From the TROG 03.04 RADAR Trial. Int. J. Radiat. Oncol. Biol. Phys. 2020, 106, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Pan, W.Y.; Bian, C.; Zou, G.L.; Zhang, C.Y.; Hai, P.; Zhao, R.; Wang, Y.Y. Combing NLR, V20 and mean lung dose to predict radiation induced lung injury in patients with lung cancer treated with intensity modulated radiation therapy and chemotherapy. Oncotarget 2017, 8, 81387–81393. [Google Scholar] [CrossRef] [PubMed]
- Ryckman, J.M.; Baine, M.; Carmicheal, J.; Osayande, F.; Sleightholm, R.; Samson, K.; Zheng, D.; Zhen, W.; Lin, C.; Zhang, C. Correction to: Correlation of dosimetric factors with the development of symptomatic radiation pneumonitis in stereotactic body radiotherapy. Radiat. Oncol. 2021, 16, 67. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Nishimura, H.; Nakayama, M.; Mayahara, H.; Uezono, H.; Harada, A.; Hashimoto, N.; Ejima, Y.; Ishihara, T.; Sasaki, R. Dosimetric factors predicting radiation pneumonitis after CyberKnife stereotactic body radiotherapy for peripheral lung cancer. Br. J. Radiol. 2016, 89, 20160560. [Google Scholar] [CrossRef]
- Farr, K.P.; Kallehauge, J.F.; Møller, D.S.; Khalil, A.A.; Kramer, S.; Bluhme, H.; Morsing, A.; Grau, C. Inclusion of functional information from perfusion SPECT improves predictive value of dose-volume parameters in lung toxicity outcome after radiotherapy for non-small cell lung cancer: A prospective study. Radiother. Oncol. 2015, 117, 9–16. [Google Scholar] [CrossRef]
- Green, M.; Rosen, B.S.; Saripalli, A.; Bazzi, L.; Kong, F.M.; Matuszak, M.M.; Ten Haken, R.K.; Lawrence, T.S.; Jolly, S.; El Naqa, I. Radiomic Features Predict Esophagitis Risk in Non-Small Cell Lung Cancer Patients Treated with Radiation. Int. J. Radiat. Oncol. 2017, 99, S14. [Google Scholar] [CrossRef]
- Krafft, S.P.; Rao, A.; Stingo, F.; Briere, T.M.; Court, L.E.; Liao, Z.; Martel, M.K. The utility of quantitative CT radiomics features for improved prediction of radiation pneumonitis. Med. Phys. 2018, 45, 5317–5324. [Google Scholar] [CrossRef]
- Cui, S.; Luo, Y.; Tseng, H.-H.; Ten Haken, R.K.; Naqa, I. El Combining handcrafted features with latent variables in machine learning for prediction of radiation-induced lung damage. Med. Phys. 2019, 46, 2497–2511. [Google Scholar] [CrossRef]
- Luna, J.M.; Chao, H.H.; Diffenderfer, E.S.; Valdes, G.; Chinniah, C.; Ma, G.; Cengel, K.A.; Solberg, T.D.; Berman, A.T.; Simone, C.B. Predicting radiation pneumonitis in locally advanced stage II–III non-small cell lung cancer using machine learning. Radiother. Oncol. 2019, 133, 106–112. [Google Scholar] [CrossRef]
- Hirose, T.A.; Arimura, H.; Ninomiya, K.; Yoshitake, T.; Fukunaga, J.I.; Shioyama, Y. Radiomic prediction of radiation pneumonitis on pretreatment planning computed tomography images prior to lung cancer stereotactic body radiation therapy. Sci. Rep. 2020, 10, 20424. [Google Scholar] [CrossRef]
- Zwanenburg, A.; Leger, S.; Agolli, L.; Pilz, K.; Troost, E.G.C.; Richter, C.; Löck, S. Assessing robustness of radiomic features by image perturbation. Sci. Rep. 2019, 9, 614. [Google Scholar] [CrossRef] [PubMed]
- Salvestrini, V.; Greco, C.; Guerini, A.E.; Longo, S.; Nardone, V.; Boldrini, L.; Desideri, I.; De Felice, F. The role of feature-based radiomics for predicting response and radiation injury after stereotactic radiation therapy for brain metastases: A critical review by the Young Group of the Italian Association of Radiotherapy and Clinical Oncology (yAIRO). Transl. Oncol. 2022, 15, 101275. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Overall (126) |
|---|---|
| Gender | p = 0.04 |
| Male (N/%) | 109/86.5% |
| Female (N/%) | 17/13.5% |
| Age, median (range) | 61 (29–82) (p = 0.67) |
| Pathology | p = 0.46 |
| SCC (N/%) | 79/62.7% |
| ADC (N/%) | 42/33.3% |
| Others (N/%) | 5/4.0% |
| RT Dose, median (range) | 60 (50–70) Gy (p = 0.94) |
| Smoking | p = 0.23 |
| Activity or former (N/%) | 97/77.0% |
| Never (N/%) | 29/23.0% |
| Overall Stage | p = 0.30 |
| IIIA (N/%) | 80/63.5% |
| IIIB (N/%) | 46/36.5% |
| Treatment method | p = 0.97 |
| SCRT (N/%) | 83/65.9% |
| CCRT (N/%) | 42/33.3% |
| RT (N/%) | 1/0.8% |
| ARP (N/%) | 64/50.8% |
| Cohort | WL-DF | WL-RF | WL-RDF | SR-DF | SR-RF | SR-RDF | |
|---|---|---|---|---|---|---|---|
| AUC | Train | 0.70 | 0.85 | 0.90 | 0.88 | 0.93 | 0.98 |
| Test | 0.65 | 0.77 | 0.80 | 0.74 | 0.79 | 0.88 | |
| Acc | Train | 0.63 | 0.75 | 0.83 | 0.78 | 0.86 | 0.93 |
| Test | 0.59 | 0.70 | 0.74 | 0.71 | 0.74 | 0.83 | |
| Pre | Train | 0.41 | 0.56 | 0.67 | 0.59 | 0.71 | 0.82 |
| Test | 0.38 | 0.49 | 0.55 | 0.51 | 0.54 | 0.69 | |
| Re | Train | 0.68 | 0.75 | 0.81 | 0.81 | 0.86 | 0.96 |
| Test | 0.63 | 0.69 | 0.66 | 0.66 | 0.65 | 0.79 | |
| F1 | Train | 0.51 | 0.64 | 0.73 | 0.68 | 0.78 | 0.88 |
| Test | 0.47 | 0.56 | 0.59 | 0.57 | 0.59 | 0.73 |
| Reference | Features (n) | Classification | Methods | AUC | Patient Information |
|---|---|---|---|---|---|
| [37] | Radiomics (9) | 2 | Logistics regression | 0.75 | SBRT for 40 stages I NSCLC patients |
| [38] | Radiomics (8), DDF (5) | LASSO | 0.68 | IMRT/3DCRT for 192 NSCLC patients | |
| [39] | DDF (5), Clinical factors (13), Cytokines (30), miRNAs (62), SNPs (60) | 2 | RF, SVM, MLP | 0.831 | RT for 106 NSCLC patients |
| [40] | DDF (11), Clinical factors (21) | 2 | RF | 0.66 | RT for 203 stage II–III NSCLC patients |
| [11] | Radiomics (TL-GTV) Multi-ROIs radiomics | 2 | SVM | 0.71 0.94 | VMAT for 79 stages I-IV lung cancer patients |
| [16] | Radiomics, Dosiomics, Clinical factors | 2 | RF | 0.771 (V20) 0.763 (V5) | RT for 701 NSCLC patients |
| [41] | Radiomics (486) | 2 | Logistic regression | 0.871 (Training) 0.756 (Testing) | SBRT For 275 stage I NSCLC patients |
| [17] | Dosiomics | 2 | LightGBM | 0.846 | SBRT for 685 NSCLC patients |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, B.; Zheng, X.; Zhang, J.; Lam, S.; Guo, W.; Wang, Y.; Cui, S.; Teng, X.; Zhang, Y.; Ma, Z.; et al. Lung Subregion Partitioning by Incremental Dose Intervals Improves Omics-Based Prediction for Acute Radiation Pneumonitis in Non-Small-Cell Lung Cancer Patients. Cancers 2022, 14, 4889. https://doi.org/10.3390/cancers14194889
Li B, Zheng X, Zhang J, Lam S, Guo W, Wang Y, Cui S, Teng X, Zhang Y, Ma Z, et al. Lung Subregion Partitioning by Incremental Dose Intervals Improves Omics-Based Prediction for Acute Radiation Pneumonitis in Non-Small-Cell Lung Cancer Patients. Cancers. 2022; 14(19):4889. https://doi.org/10.3390/cancers14194889
Chicago/Turabian StyleLi, Bing, Xiaoli Zheng, Jiang Zhang, Saikit Lam, Wei Guo, Yunhan Wang, Sunan Cui, Xinzhi Teng, Yuanpeng Zhang, Zongrui Ma, and et al. 2022. "Lung Subregion Partitioning by Incremental Dose Intervals Improves Omics-Based Prediction for Acute Radiation Pneumonitis in Non-Small-Cell Lung Cancer Patients" Cancers 14, no. 19: 4889. https://doi.org/10.3390/cancers14194889
APA StyleLi, B., Zheng, X., Zhang, J., Lam, S., Guo, W., Wang, Y., Cui, S., Teng, X., Zhang, Y., Ma, Z., Zhou, T., Lou, Z., Meng, L., Ge, H., & Cai, J. (2022). Lung Subregion Partitioning by Incremental Dose Intervals Improves Omics-Based Prediction for Acute Radiation Pneumonitis in Non-Small-Cell Lung Cancer Patients. Cancers, 14(19), 4889. https://doi.org/10.3390/cancers14194889






