Low-Dose Acetylsalicylic Acid Treatment in Non-Skull-Base Meningiomas: Impact on Tumor Proliferation and Seizure Burden
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Data Recording and Radiological Features
2.3. Histopathology
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
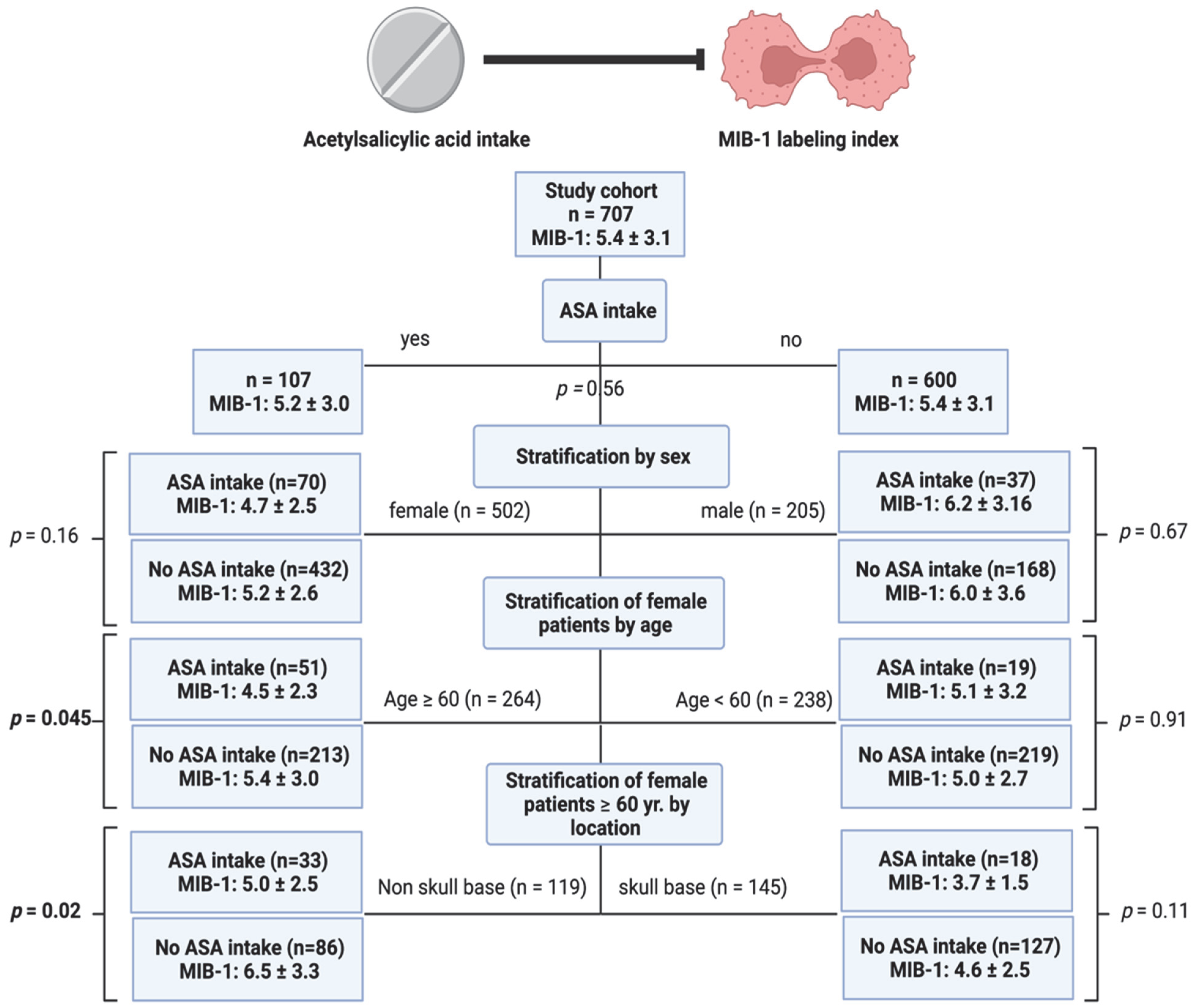
3.2. Identification of a Subgroup Benefiting from Low-Dose ASA Intake Regarding MIB-1 Labeling Index
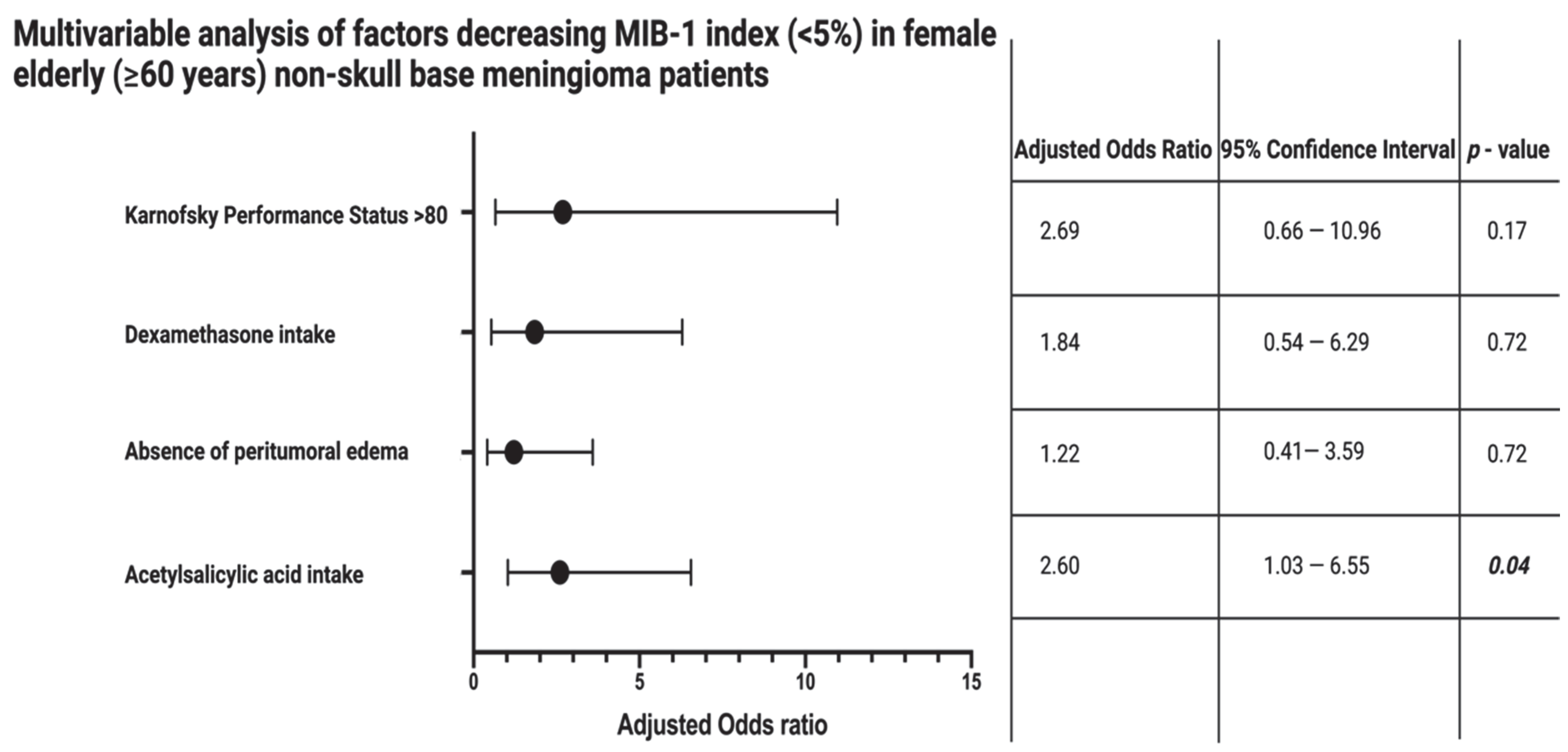
3.3. Impact of Low-Dose ASA Intake in Female Elderly Non-Skull-Base Meningioma Patients on MIB-1 Index
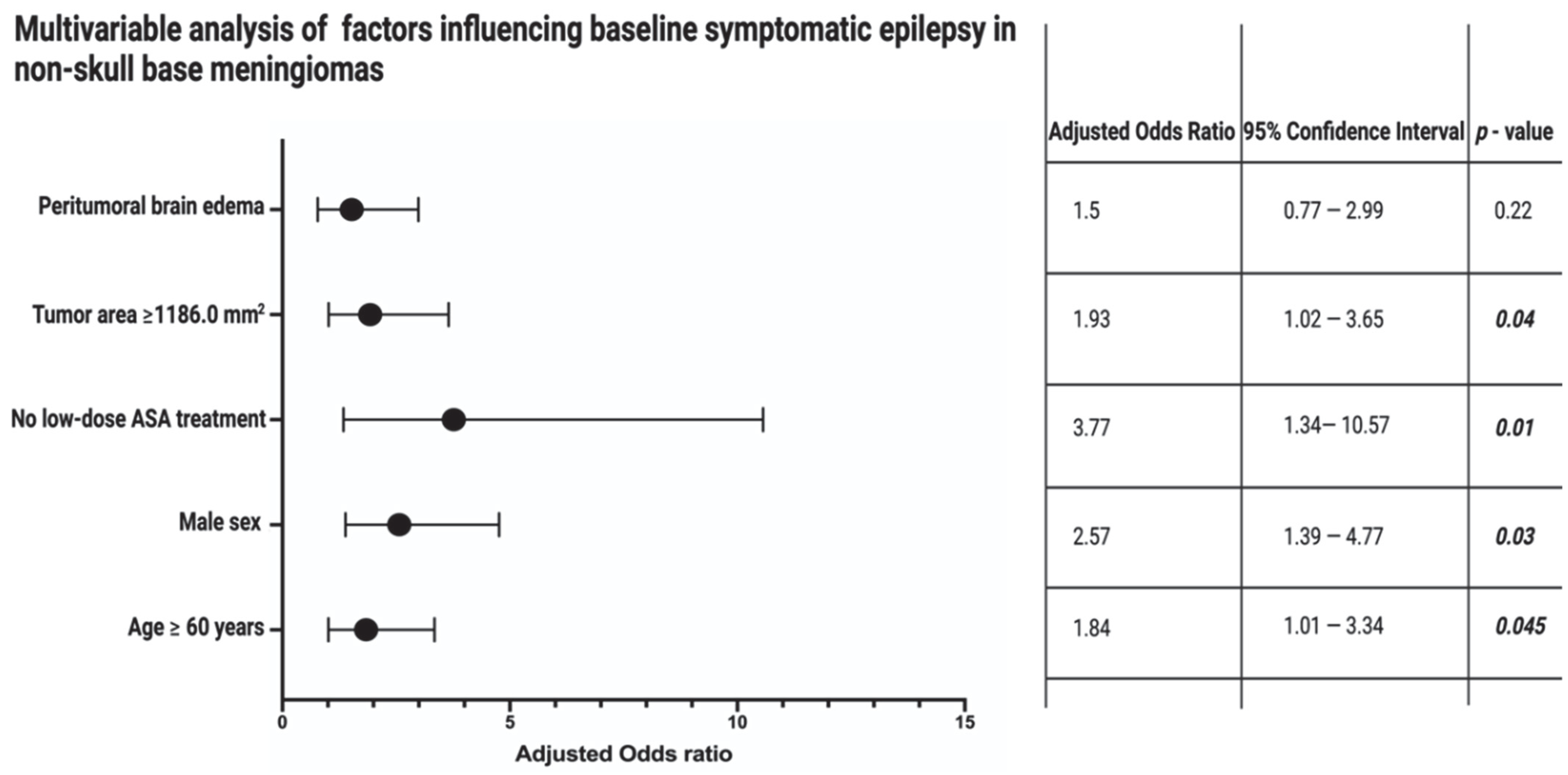
3.4. Impact of Low-Dose ASA Intake on Baseline Symptomatic Epilepsy in Non-Skull-Base Meningiomas
4. Discussion
4.1. COX-2 Inhibition by Low-Dose ASA Intake and MIB-1
4.2. Inflammation and Proliferation
4.3. Symptomatic Epilepsy in Meningiomas and Role of Inflammation
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ostrom, Q.T.; Gittleman, H.; Fulop, J.; Liu, M.; Blanda, R.; Kromer, C.; Wolinsky, Y.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2008–2012. Neuro Oncol. 2015, 17 (Suppl. 4), iv1–iv62. [Google Scholar] [CrossRef] [PubMed]
- Domingues, P.H.; Sousa, P.; Otero, Á.; Gonçalves, J.M.; Ruiz, L.; de Oliveira, C.; Lopes, M.C.; Orfao, A.; Tabernero, M.D. Proposal for a new risk stratification classification for meningioma based on patient age, WHO tumor grade, size, localization, and karyotype. Neuro Oncol. 2014, 16, 735–747. [Google Scholar] [CrossRef] [PubMed]
- Louis, D.N.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, W.K.; Ohgaki, H.; Wiestler, O.D.; Kleihues, P.; Ellison, D.W. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: A summary. Acta Neuropathol. 2016, 131, 803–820. [Google Scholar] [CrossRef] [PubMed]
- Alexiou, G.A.; Gogou, P.; Markoula, S.; Kyritsis, A.P. Management of meningiomas. Clin. Neurol. Neurosurg. 2010, 112, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Nigim, F.; Wakimoto, H.; Kasper, E.M.; Ackermans, L.; Temel, Y. Emerging Medical Treatments for Meningioma in the Molecular Era. Biomedicines 2018, 6, 86. [Google Scholar] [CrossRef]
- Van Diest, P.J.; Brugal, G.; Baak, J.P. Proliferation markers in tumours: Interpretation and clinical value. J. Clin. Pathol. 1998, 51, 716–724. [Google Scholar] [CrossRef]
- Wach, J.; Lampmann, T.; Güresir, Á.; Vatter, H.; Herrlinger, U.; Becker, A.; Toma, M.; Hölzel, M.; Güresir, E. Inflammatory Tumor Microenvironment in Cranial Meningiomas: Clinical Implications and Intraindividual Reproducbility. Diagnostics 2022, 12, 853. [Google Scholar] [CrossRef]
- Gerdes, J.; Schwab, U.; Lemke, H.; Stein, H. Production of a mouse monoclonal antibody reactive with a human nuclear antigen associated with cell proliferation. Int. J. Cancer. 1983, 31, 13–20. [Google Scholar] [CrossRef]
- Scholzen, T.; Gerdes, J. The Ki-67 protein: From the known and the unknown. J. Cell. Physiol. 2000, 182, 311–322. [Google Scholar] [CrossRef]
- Oya, S.; Kawai, K.; Nakatomi, H.; Saito, N. Significance of Simpson grading system in modern meningioma surgery: Integration of the grade with MIB-1 labeling index as a key to predict the recurrence of WHO Grade I meningiomas. J. Neurosurg. 2012, 117, 121–128. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.S.; Kim, K.H.; Lee, E.H.; Lee, Y.M.; Lee, S.H.; Kim, H.D.; Kim, Y.Z. Results of immunohistochemical staining for cell cycle regulators predict the recurrence of atypical meningiomas. J. Neurosurg. 2014, 121, 1189–1200. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; Song, S.Y.; Jiang, J.B.; Wang, T.J.; Yan, C.X. The prognostic role of Ki-67/MIB-1 in meningioma: A systematic review with meta-analysis. Medicine 2020, 99, e18644. [Google Scholar] [CrossRef] [PubMed]
- Wach, J.; Lampmann, T.; Güresir, Á.; Schuss, P.; Vatter, H.; Herrlinger, U.; Becker, A.; Hölzel, M.; Toma, M.; Güresir, E. FORGE: A Novel Scoring System to Predict the MIB-1 Labeling Index in Intracranial Meningiomas. Cancers 2021, 13, 3643. [Google Scholar] [CrossRef] [PubMed]
- Sobolewski, C.; Cerella, C.; Dicato, M.; Ghibelli, L.; Diederich, M. The role of cyclooxygenase-2 in cell proliferation and cell death in human malignancies. Int. J. Cell Biol. 2010, 2010, 215158. [Google Scholar] [CrossRef]
- Tsoi, K.K.F.; Ho, J.M.W.; Chan, F.C.H.; Sung, J.J.Y. Long-term use of low-dose aspirin for cancer prevention: A 10-year population cohort study in Hong Kong. Int. J. Cancer 2019, 145, 267–273. [Google Scholar] [CrossRef]
- Shebl, F.M.; Hsing, A.W.; Park, Y.; Hollenbeck, A.R.; Chu, L.W.; Meyer, T.E.; Koshiol, J. Non-steroidal anti-inflammatory drugs use is associated with reduced risk of inflammation-associated cancers: NIH-AARP study. PLoS ONE 2014, 9, e114633. [Google Scholar]
- Kato, Y.; Nishihara, H.; Mohri, H.; Kanno, H.; Kobayashi, H.; Kimura, T.; Tanino, M.; Terasaka, S.; Tanaka, S. Clinicopathological evaluation of cyclooxygenase-2 expression in meningioma: Immunohistochemical analysis of 76 cases of low and high-grade meningiomas. Brain Tumor Pathol. 2014, 31, 23–30. [Google Scholar] [CrossRef]
- Ragel, B.T.; Jensen, R.L.; Gillespie, D.L.; Prescott, S.M.; Couldwell, W.T. Ubiquitous expression of cyclooxygenase-2 in meningiomas and decrease in cell growth following in vitro treatment with the inhibitor celecoxib: Potential therapeutic application. J. Neurosurg. 2005, 103, 508–517. [Google Scholar] [CrossRef]
- Rawat, C.; Kukal, S.; Dahiya, U.R.; Kukreti, R. Cyclooxygenase-2 (COX-2) inhibitors: Future therapeutic strategies for epilepsy management. J. Neuroinflamm. 2019, 16, 197. [Google Scholar] [CrossRef]
- Skardelly, M.; Rother, C.; Noell, S.; Behling, F.; Wuttke, T.V.; Schittenhelm, J.; Bisdas, S.; Meisner, C.; Rona, S.; Tabatabai, G.; et al. Risk Factors of Preoperative and Early Postoperative Seizures in Patients with Meningioma: A Retrospective Single-Center Cohort Study. World Neurosurg. 2017, 97, 538–546. [Google Scholar] [CrossRef]
- Wach, J.; Lampmann, T.; Güresir, Á.; Vatter, H.; Herrlinger, U.; Becker, A.; Cases-Cunillera, S.; Hölzel, M.; Toma, M.; Güresir, E. Proliferative Potential, and Inflammatory Tumor Microenvironment in Meningioma Correlate with Neurological Function at Presentation and Anatomical Location—From Convexity to Skull Base and Spine. Cancers 2022, 14, 1033. [Google Scholar] [CrossRef]
- Faraji, A.H.; Tonetti, D.A.; Flickinger, J.C.; Engh, J.A. Alteration of the Ki-67 proliferative index following surgical resection with or without radiation therapy of intracranial meningiomas. Cureus 2017, 9, e1873. [Google Scholar] [CrossRef] [PubMed]
- Antinheimo, J.; Haapasalo, H.; Haltia, M.; Tatagiba, M.; Thomas, S.; Brandis, A.; Sainio, M.; Carpen, O.; Samii, M.; Jääskeläinen, J. Proliferation potential and histological features in neurofibromatosis 2-associated and sporadic meningiomas. J. Neurosurg. 1997, 87, 610–614. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.W.; Kim, M.S.; Kim, S.W.; Chang, C.H.; Kim, O.L. Peritumoral brain edema in meningiomas: Correlation of radiologic and pathologic features. J. Korean Neurosurg. Soc. 2011, 49, 26–30. [Google Scholar] [CrossRef]
- Wen, P.Y.; Chang, S.M.; Van den Bent, M.J.; Vogelbaum, M.A.; Macdonald, D.R.; Lee, E.Q. Response assessment in neuro-oncology clinical trials. J. Clin. Oncol. 2017, 35, 2439–2449. [Google Scholar] [CrossRef]
- Maiuri, F.; Mariniello, G.; Guadagno, E.; Barbato, M.; Corvino, S.; Del Basso De Caro, M. WHO grade proliferation index, and progesterone receptor expression are different according to the location of meningioma. Acta Neurochir. 2019, 161, 2553–2561. [Google Scholar] [CrossRef] [PubMed]
- Majores, M.; Schick, V.; Engels, G.; Fassunke, J.; Elger, C.E.; Schramm, J.; Blumcke, I.; Becker, A.J. Mutational and immunohistochemical analysis of ezrin-, radixin-, moesin (ERM) molecules in epilepsy-associated glioneuronal lesions. Acta Neuropathol. 2005, 110, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Majores, M.; von Lehe, M.; Fassunke, J.; Schramm, J.; Becker, A.J.; Simon, M. Tumor recurrence and malignant progression of gangliogliomas. Cancer 2008, 113, 3355–3363. [Google Scholar] [CrossRef]
- Schneider, M.; Borger, V.; Güresir, A.; Becker, A.; Vatter, H.; Schuss, P.; Güresir, E. High Mib-1-score correlates with new cranial nerve deficits after surgery for frontal skull base meningioma. Neurosurg. Rev. 2021, 44, 381–387. [Google Scholar] [CrossRef]
- Kasuya, H.; Kubo, O.; Tanaka, M.; Amano, K.; Kato, K.; Hori, T. Clinical and radiological features related to the growth potential of meninigioma. Neurosurg. Rev. 2006, 29, 293–296. [Google Scholar] [CrossRef]
- Matsuno, A.; Fujimaki, T.; Sasaki, T.; Nagashima, T.; Ide, T.; Asai, A.; Matsuura, R.; Utsunomiya, H.; Kirino, T. Clinical and histopathological analysis of proliferative potentials of recurrent and non-recurrent meningiomas. Acta Neuropathol. 1996, 91, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Haddad, A.F.; Young, J.S.; Kanungo, I.; Sudhir, S.; Chen, J.S.; Raleigh, D.R.; Magill, S.T.; McDermott, M.W.; Aghi, M.K. WHO grade I Meningioma Recurrence: Identifying High Risk Patients Using Histopathological Features and the MIB-1 Index. Front. Oncol. 2020, 10, 1522. [Google Scholar] [CrossRef] [PubMed]
- Ragel, B.T.; Jensen, R.L.; Gillespie, D.L.; Prescott, S.M.; Couldwell, W.T. Celecoxib inhibits meningioma tumor growth in a mouse xenograft model. Cancer 2007, 109, 588–597. [Google Scholar] [CrossRef]
- Sanz, J.; Ruiz, J.; Hernández, S.; Ferrer, M.; Zimman, H.; Sáez, C.; Hidalgo, P.; Martínez, A. Chromosome 1p36 loss and COX-2 overexpression predict recurrence-free survival in completely removed meningioma grade I and II. Rev. Española Patología 2013, 46, 14–25. [Google Scholar] [CrossRef]
- Lee, S.H.; Lee, Y.S.; Hong, Y.G.; Kang, C.S. Significance of COX-2 and VEGF expression in histopathologic grading and invasiveness of meningiomas. APMIS 2014, 122, 16–24. [Google Scholar] [CrossRef]
- Farkouh, A.; Baumgärtel, C.; Gottardi, R.; Hemetsberger, M.; Czejka, M.; Kautzky-Willer, A. Sex-Related Differences in Drugs with Anti-Inflammatory Properties. J. Clin. Med. 2021, 10, 1441. [Google Scholar] [CrossRef]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef]
- Al-Attar, A.; Presnell, S.R.; Peterson, C.A.; Thomas, D.; Lutz, C.T. The effect of sex on immune cells in healthy aging: Elderly women have more robust natural killer lymphocytes than do elderly men. Mech. Ageing Dev. 2016, 156, 25–33. [Google Scholar] [CrossRef]
- Domingues, P.H.; Teodosio, C.; Otero, A.; Sousa, P.; Ortiz, J.; Macias Mdel, C.; Goncalves, J.M.; Nieto, A.B.; Lopes, M.C.; de Oliveira, C.; et al. Association between inflammatory infiltrates and isolated monosomy 22/del(22q) in meningiomas. PLoS ONE 2013, 8, e74798. [Google Scholar] [CrossRef]
- Tabernero, M.D.; Espinosa, A.B.; Maillo, A.; Rebelo, O.; Vera, J.F.; Sayagues, J.M.; Merino, M.; Diaz, P.; Sousa, P.; Orfao, A. Patient gender is associated with distinct patterns of chromosomal abnormalities and sex chromosome linked gene-expression profiles in meningiomas. Oncologist 2007, 12, 1225–1235. [Google Scholar] [CrossRef]
- Ding, Y.; Qiu, L.; Xu, Q.; Song, L.; Yang, S.; Yang, T. Relationships between tumor microenvironment and clinicopathological parameters in meningioma. Int. J. Clin. Exp. Pathol. 2014, 7, 6973–6979. [Google Scholar] [PubMed]
- Kryczek, I.; Wei, S.; Zhu, G.; Myers, L.; Mottram, P.; Cheng, P.; Chen, L.; Coukos, G.; Zou, W. Relationship between B7-H4, regulatory T cells, and patient outcome in human ovarian carcinoma. Cancer Res. 2007, 67, 8900–8905. [Google Scholar] [CrossRef] [PubMed]
- Milne, K.; Köbel, M.; Kalloger, S.E.; Barnes, R.O.; Gao, D.; Gilks, C.B.; Watson, P.H.; Nelson, B.H. Systematic analysis of immune infiltrates in high-grade serous ovarian cancer reveals CD20, FoxP3 and TIA-1 as positive prognostic factors. PLoS ONE 2009, 4, e6412. [Google Scholar] [CrossRef]
- Erbe, R.; Wang, Z.; Wu, S.; Xiu, J.; Zaidi, N.; La, J.; Tuck, D.; Fillmore, N.; Giraldo, N.A.; Topper, M.; et al. Evaluating the impact of age on immune checkpoint therapy biomarkers. Cell Rep. 2021, 36, 109599. [Google Scholar] [CrossRef] [PubMed]
- Chiang, N.; Bermudez, E.A.; Ridker, P.M.; Hurwitz, S.; Serhan, C.N. Aspirin triggers anti-inflammatory 15-epi-lipoxin A4 and inhibits thromboxane in a randomized human trial. Proc. Natl. Acad. Sci. USA 2004, 101, 15178–15183. [Google Scholar] [CrossRef]
- Chiang, N.; Hurwitz, S.; Ridker, P.M.; Serhan, C.N. Aspirin has a gender-dependent impact on anti-inflammatory 15-epi-lipoxin A4 formation: A randomized human trial. Arter. Thromb. Vasc. Biol. 2006, 26, e14–e17. [Google Scholar] [CrossRef]
- Chiang, N.; Arita, M.; Serhan, C.N. Anti-inflammatory circuitry: Lipoxin, aspirin-triggered lipoxins and their receptor ALX. Prostaglandins Leukot. Essent. Fat. Acids 2005, 73, 163–177. [Google Scholar] [CrossRef]
- Schnittert, J.; Heinrich, M.A.; Kuninty, P.R.; Storm, G.; Prakash, J. Reprogramming tumor stroma using an endogenous lipid lipoxin A4 to treat pancreatic cancer. Cancer Lett. 2018, 420, 247–258. [Google Scholar] [CrossRef]
- Simões, R.L.; De-Brito, N.M.; Cunha-Costa, H.; Morandi, V.; Fierro, I.M.; Roitt, I.M.; Barja-Fidalgo, C. Lipoxin A4 selectively programs the profile of M2 tumor-associated macrophages which favour control of tumor progression. Int J. Cancer 2017, 140, 346–357. [Google Scholar] [CrossRef]
- Proctor, D.T.; Huang, J.; Lama, S.; Albakr, A.; Van Marle, G.; Sutherland, G.R. Tumor-associated macrophage infiltration in meningioma. Neuro-Oncol. Adv. 2019, 1, vdz018. [Google Scholar] [CrossRef]
- Zhang, T.; Yang, X.; Liu, P.; Zhou, J.; Luo, J.; Wang, H.; Li, A.; Zhou, Y. Association between nonsteroidal anti-inflammatory drugs use and risk of central nervous system tumors: A dose–response meta analysis. Oncotarget 2017, 8, 102486–102498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaist, D.; García-Rodríguez, L.A.; Sørensen, H.T.; Hallas, J.; Friis, S. Use of low-dose aspirin and non-aspirin nonsteroidal anti-inflammatory drugs and risk of glioma: A case–control study. Br. J. Cancer 2013, 108, 1189–1194. [Google Scholar] [CrossRef]
- Van Gompel, J.J.; Agazzi, S.; Carlson, M.L.; Adewumi, D.A.; Hadjipanayis, C.G.; Uhm, J.H.; Olson, J.J. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines on Emerging Therapies for the Treatment of Patients with Vestibular Schwannomas. Neurosurgery 2018, 82, E52–E54. [Google Scholar] [CrossRef] [PubMed]
- Hashemi Goradel, N.; Najafi, N.; Salehi, E.; Farhood, B.; Mortezaee, K. Cyclooxygenase-2 in cancer: A review. J. Cell. Physiol. 2019, 234, 5683–5699. [Google Scholar] [CrossRef] [PubMed]
- Klein, T.; Shephard, P.; Kleinert, H.; Komhoff, M. Regulation of cyclooxygenase-2 expression by cyclic AMP. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2007, 1773, 1605–1618. [Google Scholar] [CrossRef]
- Constantini, S.; Tamir, J.; Gomori, M.J.; Shohami, E. Tumor prostaglandin levels correlate with edema around supratentorial meningiomas. Neurosurgery 1993, 33, 204–210. [Google Scholar] [CrossRef]
- Rossi, M.L.; Cruz Sanchez, F.; Hughes, J.T.; Esiri, M.M.; Coakham, H.B. Immunocytochemical study of the cellular immune response in meningiomas. J. Clin. Pathol. 1988, 41, 314–319. [Google Scholar] [CrossRef]
- Grund, S.; Schittenhelm, J.; Roser, F.; Tatagiba, M.; Mawrin, C.; Kim, Y.J.; Bornemann, A. The microglial/macrophagic response at the tumour-brain border of invasive meningiomas. Neuropathol. Appl. Neurobiol. 2009, 35, 82–88. [Google Scholar] [CrossRef]
- Lisi, L.; Ciotti, G.M.; Braun, D.; Kalinin, S.; Curro, D.; Dello Russo, C.; Coli, A.; Mangiola, A.; Anile, C.; Feinstein, D.L.; et al. Expression of iNOS, CD163 and ARG-1 taken as M1 and M2 markers of microglial polarization in human glioblastoma and the surrounding normal parenchyma. Neurosci. Lett. 2017, 645, 106–112. [Google Scholar] [CrossRef]
- Ma, J.; Liu, L.; Che, G.; Yu, N.; Dai, F.; You, Z. The M1 form of tumor-associated macrophages in non-small cell lung cancer is positively associated with survival time. BMC Cancer 2010, 10, 112. [Google Scholar] [CrossRef]
- Biswas, S.K.; Mantovani, A. Macrophage plasticity and interaction with lymphocyte subsets: Cancer as a paradigm. Nat. Immunol. 2010, 11, 889–896. [Google Scholar] [CrossRef] [PubMed]
- Sica, A.; Larghi, P.; Mancino, A.; Rubino, L.; Porta, C.; Totaro, M.G.; Rimoldi, M.; Biswas, S.K.; Allavena, P.; Mantovani, A. Macrophage polarization in tumour progression. Semin Cancer Biol. 2008, 18, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.; Hagemann, T. Tumour-associated macrophages and cancer. Curr. Opin. Pharmacol. 2013, 13, 595–601. [Google Scholar] [CrossRef]
- Li, H.; Yang, B.; Huang, J.; Lin, Y.; Xiang, T.; Wan, J.; Li, H.; Chouaib, S.; Ren, G. Cyclooxygenase-2 in tumor-associated macrophages promotes breast cancer cell survival by triggering a positive-feedback loop between macrophages and cancer cells. Oncotarget 2015, 6, 29637–29650. [Google Scholar] [CrossRef] [PubMed]
- Waagemans, M.L.; van Nieuwenhuizen, D.; Dijkstra, M.; Wumkes, M.; Dirven, C.M.; Leenstra, S.; Reijneveld, J.C.; Klein, M.; Stalpers, L.J. Long-term impact of cognitive deficits and epilepsy on quality of life in patients with low-grade meningiomas. Neurosurgery 2011, 69, 72–78; discussion 78–79. [Google Scholar] [CrossRef]
- Gadot, R.; Khan, A.B.; Patel, R.; Goethe, E.; Shetty, A.; Hadley, C.C.; Bayley, J.C.; Harmanci, A.S.; Klisch, T.; Yoshor, D.; et al. Predictors of postoperative seizure outcome in supratentorial meningioma. J. Neurosurg. 2021, 137, 515–524. [Google Scholar] [CrossRef]
- Takemiya, T.; Suzuki, K.; Sugiura, H.; Yasuda, S.; Yamagata, K.; Kawakami, Y.; Maru, E. Inducible brain COX-2 facilitates the recurrence of hippocampal seizures in mouse rapid kindling. Prostaglandins Other Lipid Mediat. 2003, 71, 205–216. [Google Scholar] [CrossRef]
- Bauer, B.; Hartz, A.M.; Pekcec, A.; Toellner, K.; Miller, D.S.; Potschka, H. Seizure-induced up-regulation of P-glycoprotein at the blood–brain barrier through glutamate and cyclooxygenase-2 signaling. Mol. Pharmacol. 2008, 73, 1444–1453. [Google Scholar] [CrossRef]
- Lance, E.I.; Sreenivasan, A.K.; Zabel, T.A.; Kossoff, E.H.; Comi, A.M. Aspirin use in Sturge-Weber syndrome: Side effects and clinical outcomes. J. Child Neurol. 2013, 28, 213–218. [Google Scholar] [CrossRef]
- Godfred, R.M.; Parikh, M.S.; Haltiner, A.M.; Caylor, L.M.; Sepkuty, J.P.; Doherty, M.J. Does aspirin use make it harder to collect seizures during elective video-EEG telemetry. Epilepsy Behav. 2013, 27, 115–117. [Google Scholar] [CrossRef]
| Characteristics | N (%) |
|---|---|
| Sex | |
| Female | 502 (71.0%) |
| Male | 205 (29.0%) |
| Age, mean ± SD | 61.1 ± 13.7 |
| Body mass index, mean ± SD | 27.3 ± 5.9 |
| ASA intake | 107 (15.1%) |
| Preoperative KPS, mean ± SD | 88.7 ± 12.2 |
| Plasma fibrinogen, mean SD | 3.0 ± 0.9 |
| Serum c-reactive protein, mean SD | 3.7 ± 7.5 |
| Peritumoral brain edema | 303 (42.9%) |
| Location | |
| Non-skull-base meningioma | 327 (46.3%) |
| Skull-base meningioma | 380 (53.7%) |
| WHO grade | |
| 1 | 556 (78.6%) |
| 2 | 151 (21.4%) |
| MIB-1 labeling index, mean ± SD | 5.4 ± 3.1 |
| Mitotic figures, mean ± SD | 1.9 ± 2.6 |
| Characteristics | No ASA Intake% (86/119; 72.3%) | ASA Intake (33/119; 27.7%) | p-Value |
|---|---|---|---|
| Age (years), mean ± SD | 72.0 ± 77 | 71.2 ± 8.4 | 0.64 |
| Preoperative KPS, mean ± SD | 86.9 ± 13.9 | 84.1 ± 14.6 | 0.33 |
| Body mass index, mean ± SD | 26.7 ± 5.5 | 27.8 ± 5.4 | 0.35 |
| Preoperative KPS, mean ± SD | 86.2 ± 10.4 | 84.7 ± 9.6 | 0.70 |
| Plasma fibrinogen, mean ± SD | 3.0 ± 1.0 | 3.3 ± 1.0 | 0.19 |
| Rheumatoid arthritis with NSAID treatment | 2 (2.3%) | 1 (3.0%) | 0.99 |
| Regular cortisol intake | 14 (16.3%) | 7 (21.2%) | 0.59 |
| Serum c-reactive protein, mean ± SD | 4.9 ± 10.1 | 4.7 ± 6.8 | 0.90 |
| Tumor area, mean ± SD, mm2 | 1476.5 ± 988.9 | 1435.6 ± 974.8 | 0.85 |
| Peritumoral brain edema | 0.84 | ||
| Present | 44 (51.2%) | 16 (48.5%) | |
| Not present | 42 (48.8%) | 17 (51.5%) | |
| Preoperative dexamethasone intake | 0.81 | ||
| Present | 21 (24.4%) | 7 (21.2%) | |
| Absent | 65 (75.6%) | 26 (78.8%) | |
| Simpson grade | 0.99 | ||
| ≤III | 82 (95.3%) | 32 (97.0%) | |
| >III | 4 (4.7%) | 1 (3.0%) | |
| WHO grade | 0.07 | ||
| 1 | 58 (67.4%) | 28 (84.8%) | |
| 2 | 28 (32.6%) | 5 (15.2%) | |
| CD68+ macrophages (available in 91 patients) | 0.61 | ||
| Diffuse | 47 (73.4%) | 18 (66.7%) | |
| Focal | 17 (26.6%) | 9 (33.3%) |
| Characteristics | No Seizure (250/330; 75.8%) | Seizure (80/330; 24.2%) | p-Value |
|---|---|---|---|
| Age (years), mean ± SD | 57.6 ± 14.6 | 62.9 ± 13.9 | 0.004 |
| Sex | 0.01 | ||
| Female | 178/223 (79.8%) | 45/223 (20.2%) | |
| Male | 72/107 (67.3%) | 35/107 (32.7%) | |
| Preoperative KPS, mean ± SD | 89.4 ± 12.5 | 89.7 ± 11.7 | 0.82 |
| Body mass index, mean ± SD | 27.4 ± 5.5 | 28.0 ± 6.5 | 0.44 |
| ASA intake | 55 (22.0%) | 6 (7.5%) | 0.004 |
| Tumor area, mean ± SD, mm2 | 1379.9 ± 1034.8 | 1601.1 ± 1233.4 | 0.13 |
| Peritumoral brain edema | 0.0001 | ||
| Present | 99 (39.6%) | 55 (68.8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wach, J.; Güresir, Á.; Vatter, H.; Herrlinger, U.; Becker, A.; Toma, M.; Hölzel, M.; Güresir, E. Low-Dose Acetylsalicylic Acid Treatment in Non-Skull-Base Meningiomas: Impact on Tumor Proliferation and Seizure Burden. Cancers 2022, 14, 4285. https://doi.org/10.3390/cancers14174285
Wach J, Güresir Á, Vatter H, Herrlinger U, Becker A, Toma M, Hölzel M, Güresir E. Low-Dose Acetylsalicylic Acid Treatment in Non-Skull-Base Meningiomas: Impact on Tumor Proliferation and Seizure Burden. Cancers. 2022; 14(17):4285. https://doi.org/10.3390/cancers14174285
Chicago/Turabian StyleWach, Johannes, Ági Güresir, Hartmut Vatter, Ulrich Herrlinger, Albert Becker, Marieta Toma, Michael Hölzel, and Erdem Güresir. 2022. "Low-Dose Acetylsalicylic Acid Treatment in Non-Skull-Base Meningiomas: Impact on Tumor Proliferation and Seizure Burden" Cancers 14, no. 17: 4285. https://doi.org/10.3390/cancers14174285
APA StyleWach, J., Güresir, Á., Vatter, H., Herrlinger, U., Becker, A., Toma, M., Hölzel, M., & Güresir, E. (2022). Low-Dose Acetylsalicylic Acid Treatment in Non-Skull-Base Meningiomas: Impact on Tumor Proliferation and Seizure Burden. Cancers, 14(17), 4285. https://doi.org/10.3390/cancers14174285








