Simple Summary
The current paradigm concerning metastatic spread in uveal melanoma is that the critical point for dissemination occurs prior to presentation and that treatment of the primary tumor does not change outcome. However, we show that patients with small uveal melanomas with genetic characteristics typical for high risk for metastatic disease have a lower mortality rate from metastatic disease, if treated earlier. Our data demonstrate that such small melanomas are potentially lethal (like larger tumors), but that there is a window of opportunity to prevent life-threatening metastatic spread if actively treated, rather than being monitored, as is often done currently.
Abstract
Our aim was to determine whether size impacts on the difference in metastatic mortality of genetically high-risk (monosomy 3) uveal melanomas (UM). We undertook a retrospective analysis of data from a patient cohort with genetically characterized UM. All patients treated for UM in the Liverpool Ocular Oncology Centre between 2007 and 2014, who had a prognostic genetic tumor analysis. Patients were subdivided into those with small (≤2.5 mm thickness) and large (>2.5 mm thickness) tumors. Survival analyses were performed using Gray rank statistics to calculate absolute probabilities of dying as a result of metastatic UM. The 5-year absolute risk of metastatic mortality of those with small monosomy 3 UM was significantly lower (23%) compared to the larger tumor group (50%) (p = 0.003). Small disomy 3 UM also had a lower absolute risk of metastatic mortality (0.8%) than large disomy 3 UM (6.4%) (p = 0.007). Hazard rates showed similar differences even with lead time bias correction estimates. We therefore conclude that earlier treatment of all small UM, particularly monosomy 3 UM, reduces the risk of metastatic disease and death. Our results would support molecular studies of even small UM, rather than ‘watch-and-wait strategies’.
1. Introduction
The success of local control of primary uveal melanoma (UM) with radiotherapy or surgery is high (80–100%, depending on treatment modality) [1,2,3,4,5,6]. Recent advances in treatment regimens and the advent of intraocular laser therapies and drugs have increased the rates of eye- and vision retention [7,8,9,10,11]. Although certain treatments for metastatic UM, such as monoclonal antibody infusions or hepatic resections of isolated lesions, have shown some benefit [12,13,14,15,16,17,18,19,20,21], they are suitable for only select UM patients [22,23,24,25]. Clinical trials are underway for other treatments for patients with metastatic disease [26]; however, to date, the prognosis remains poor and the metastatic mortality rate associated with UM remains at 40–45% [27,28,29,30,31].
Prognostic parameters associated with an increased risk of developing metastatic UM are related to primary tumor characteristics, such as larger size, ciliary body involvement, extra-ocular extension and histologic features (e.g., epithelioid cell morphology, closed connective tissue loops, high mitotic count) [32,33,34]. In addition, chromosomal alterations, particularly loss of one copy of chromosome 3 (monosomy 3; M3) and gene mutations (e.g., in BAP1, SF3B1 and EIF1AX) play a major role in determining metastatic risk in UM [35,36,37,38,39,40,41] [33]. At the Liverpool Ocular Oncology Centre (LOOC), metastatic risk is determined using the Liverpool Uveal Melanoma Prognosticator Online (LUMPO) algorithm that incorporates clinical, histological and genetic parameters, to provide an individualized approach to patient management [33]. This prognostic algorithm has been validated externally in multiple centers worldwide [42,43,44].
Many UM patients present with advanced ocular disease, with approximately 23% reporting that their tumor was initially missed when they presented with symptoms [45,46]. Previously, it had been considered that systemic tumor cell dissemination occurs prior to presentation, and hence that ocular treatment does not reduce the risk of metastatic disease and mortality. However, there are indications that earlier detection and treatment of smaller UM are not only associated with better local outcomes but may also be associated with improved survival rates [47,48,49,50,51,52,53].
Herein, to address the question of whether earlier treatment of UM would result in a reduction in mortality from metastatic melanoma, we present an analysis of the outcomes of UM patients with high-risk monosomy 3 UM (M3-UM), comparing their absolute risks of mortality according to tumor size. Our hypothesis is that earlier detection and treatment of high-risk M3-UM may improve the patients’ chances of survival.
2. Results
During the 7-year study period, data were available for 940 patients whose UM underwent genetic testing. Of these, 403 (43%) were classified as M3; 432 (46%) as D3; and 105 (11%) were unclassifiable. The median age at diagnosis was 61 years (mean 60; range 24–94 years) with a male: female ratio of 525:415 (1.26:1). The median tumor diameter was 13.3mm (mean 14.3; range 1.8–26.0) and tumor thickness was 5.4mm (mean 6.5; range 0.7–18.3). Ciliary body involvement was present in 188 patients (Table 1).

Table 1.
Baseline patient and tumor characteristics (median and range) and primary treatment of small and large tumor categories.
Tumors were classified as ‘small’ (≤2.5 mm in thickness) (n = 196) and ‘large’ (>2.5 mm in thickness) (n = 744). This size cut-off is based on the clinical risk factors previously described for small melanocytic lesions [54] of 2 mm and the T1 staging of small melanomas of 3 mm [55].
As outlined in Table 1, primary treatment was enucleation in 407/940 (43%) patients; proton beam radiotherapy in 197 (21%), ruthenium-106 plaque brachytherapy in 222 (24%); photodynamic therapy in 2 (0.2%); trans-scleral local resection in 68 (7%); and transretinal endoresection in 42 (4%) patients. One case in each group had incomplete data on primary treatment. There were proportionally more cases treated with eye-conserving primary radiotherapy (either ruthenium-106 plaque brachytherapy or proton beam radiotherapy) in those with smaller tumors (72% vs. 37%, p < 0.00001), and higher rates of primary enucleation in the larger UM group (50% vs. 18%, p < 0.00001).
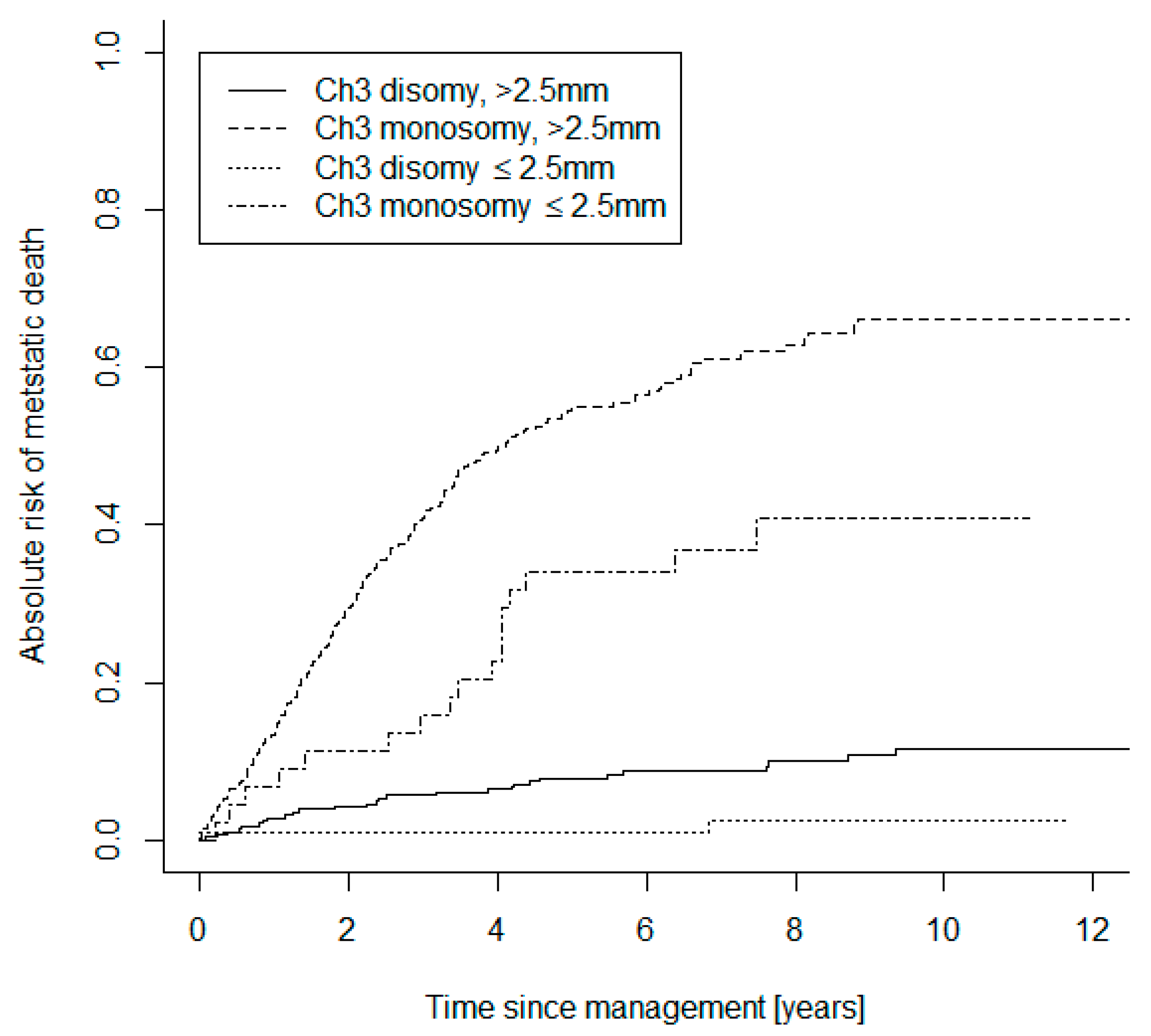
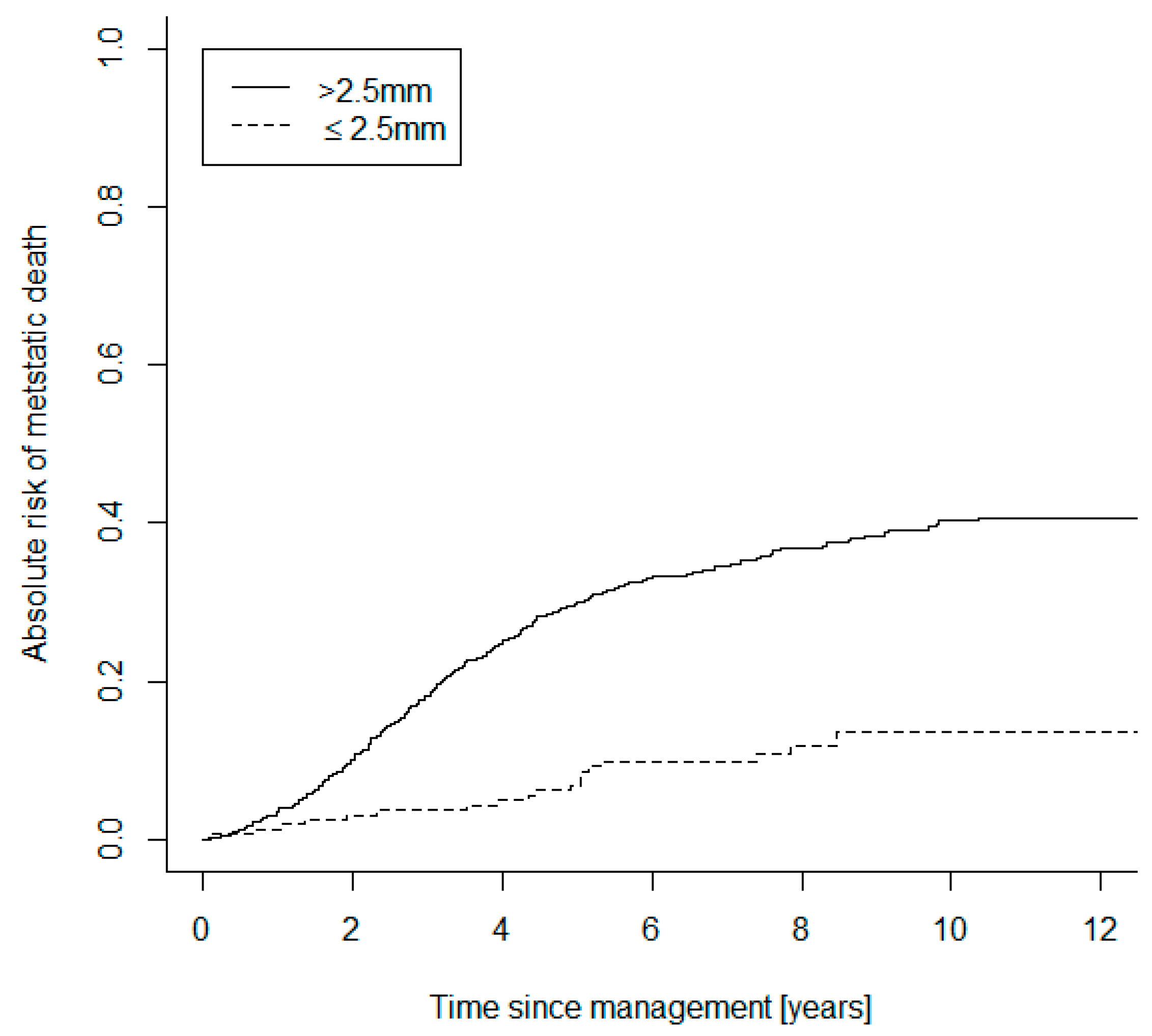
Of the small category tumors, 122 UM were D3 (62%), 44 were M3 (22%), and 30 (15%) were genetically unclassifiable. Of the large tumor group, 310 were D3-UM (42%), 359 were M3 (48%) and 75 (10%) were genetically unclassifiable. Both the small UM D3 and M3 subgroups were compared to the larger UM D3 and M3 cohorts, in terms of absolute risk of mortality due to metastasis (Figure 1). The Gray statistics showed significant evidence of an absolute risk difference between small and large M3-UM (p = 0.003) and between small and large D3-UM (p = 0.007). The small and large UM categories were also compared in terms of absolute risk of mortality (Figure 2). The Gray statistics (stratified by genetic class) also showed significant evidence of an absolute risk difference between small and large UM (p < 0.001).
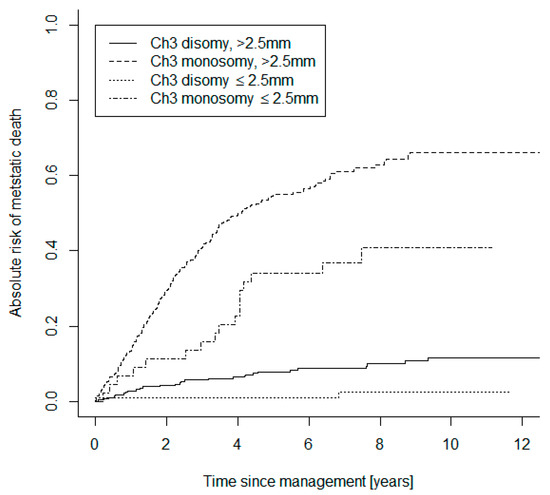
Figure 1.
Curves showing the comparative absolute risks of mortality due to metastatic UM in monosomy 3 and disomy 3 tumors subdivided into the defined ‘small’ and ‘large’ categories.
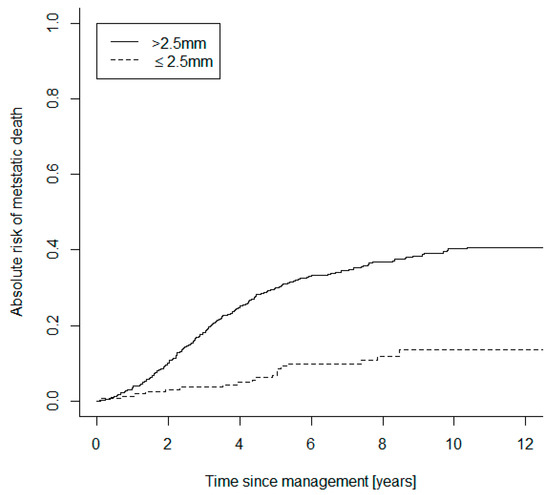
Figure 2.
Curves showing the comparative absolute risks of mortality due to metastatic UM subdivided into the defined ‘small’ and ‘large’ categories.
In particular, the 5-year absolute risk of mortality of small M3-UM was 23% versus larger M3-UM at 50% (small D3-UM 0.8%; large D3-UM 6.4%).
Log-rank analysis also demonstrated a significant difference in the hazard rates of small M3 versus large M3 UM (p = 0.003), between small D3 and large D3 UM (p = 0.007) and between each of the remaining subgroup comparisons (p < 0.001).
The relative risk (RR) of death over 5 years was 0.45 (95% CI 0.26–0.8) in the smaller M3 UM group compared to the larger M3 group, and the hazard ratio (HR) was 0.44 (95% CI 0.30–0.58). Assuming a ‘sojourn time’ of 1 year for detectability to symptomatology to correct for lead time bias as previously described [52], the modified RR of death was 0.69 (95% CI 0.45–1.05) and the modified HR was 0.67 (95% CI 0.53–0.81) (Table 2). The rates did not change significantly after 5-year correction for length time bias at a range of time courses (Appendix A).

Table 2.
Risk ratio and hazard rates of death for small M3 tumors in comparison to larger M3 UM. Lead time bias correction with an estimated sojourn time of 1 year still demonstrates a lower risk of death due to metastatic disease.
3. Discussion
Due to the peak of metastatic mortality occurring 2 years after enucleation for UM [56], early hypotheses (Zimmerman–McLean–Foster) suggested that enucleation itself may increase the risk of metastatic disease by systemic dissemination of tumor cells [57]. If this study had been performed in the 1970s, proponents of the Zimmerman–McLean–Foster hypothesis might have attributed the higher mortality in patients with larger tumors to the treatment of such tumors by enucleation. This theory has been largely refuted by the COMS study with similar mortality rates for those undergoing enucleation or plaque brachytherapy [58,59]. It has therefore been assumed that hematogeneous dissemination of UM cells occurs long before the primary tumor has been diagnosed [60]. Tumor doubling time calculations support this hypothesis by suggesting that the metastatic dissemination precedes the initial diagnosis and treatment [61,62]. Other studies suggest that most UM patients have circulating tumor cells (CTC), whereby the genotypic and phenotypic profiles of the CTCs match the primary tumor [62,63]. As such, there is a prevailing dogma that treatment of the primary UM is undertaken only to preserve vision (and, if possible, the eye) but will not prevent metastatic disease. Alternate opinions propose, however, that by “stemming the metastatic flow” of UM cells into the bloodstream, this could result in a reduction in the subsequent CTC load, and consequently reduce metastatic risk [50,51,64]. That is, there may indeed be a window of opportunity for metastatic disease prevention by treating UM earlier, and this would be particularly relevant in small lethal M3-UM [53].
It is well established in UM that various clinical risk factors, including tumor size, are related to the risk of metastatic disease and subsequent mortality, with small incremental increases in primary tumor size significantly affecting outcomes [47,65,66]. It has been assumed that larger UM are innately more aggressive, as they have either high-risk genetic factors from the outset or have accumulated these factors over time, termed ‘crescendo malignancy’ [67]. On this basis, it is conventional practice in many ocular oncology centers to monitor small, indeterminate uveal melanocytic tumors for months (or even years) until growth is documented [68,69,70,71,72]. Weis et al. demonstrated that most of these indeterminate lesions are low-risk D3-UM [73]. Our current study supports these findings, with 73% of the small melanocytic tumors being D3; however, importantly, we demonstrate that over one quarter (i.e., 27%) of these small lesions are M3-UM, and therefore have a high metastatic risk. Furthermore, whilst most of these small UM are D3 at this stage, it is unclear what proportion could subsequently transform into higher-risk M3-UM, if left untreated. Certainly, there are reports of genetic heterogeneity within larger UM [67,74,75,76,77], which suggests that there is an evolutionary process of uveal melanocytic lesions from low to high genetic risk. In addition, we have previously demonstrated that asymptomatic patients with UM identified via the annual UK national diabetic retinopathy screening program have lower mortality than those detected via alternative routes [52]. Taking all of these data into account, which suggest that early detection and treatment of UM may enable the prolongation of life in patients, there could be justification for the consideration of earlier treatment in small uveal melanocytic tumors. If these lesions are monitored, adequate patient counselling and informed consent are vital. Afshar et al. described a number of cases whereby patients were monitored for years by their optometrist or local ophthalmologist without being informed that there was a possibility that their ‘suspicious nevus’ was malignant; some of these patients were eventually found to have a lethal UM when biopsy was ultimately performed [78]. On the other hand, it is also important to emphasize here that we do not recommend treatment of all small, benign, melanocytic lesions; it can indeed be difficult to differentiate benign nevi from small melanomas. These are best assessed and treated by teams having the required expertise in ocular oncology so as to avoid unnecessary visual loss whilst not delaying treatment of life-threatening melanomas. For example, we were able to confirm malignancy in such small lesions by performing biopsy using skills and techniques that are now widely available.
At present, unfortunately, it is not possible using the available clinical imaging technologies to genetically subtype these small uveal melanocytic lesions. With the advent of artificial intelligence and its application in ophthalmology, however, this may change [79]. Consequently, at present, to determine the genetic status of the cells within an atypical uveal melanocytic lesion, intraocular biopsies must be performed. Our previous experience indicates that this procedure is safe in most patients and can be undertaken following radiotherapy [80,81].
In this analysis, we have attempted to control for lead time bias with previously published methods [82] requiring an estimate of sojourn time, which is the unobserved period of time during which the tumor is asymptomatic but detectable at screening, and thus it artificially increases the follow-up time. Sojourn time estimation is a difficult problem in general, particularly in UM, where often asymptomatic patients are detected at a routine screening visit [45]. Therefore, we have created a range of estimates, as suggested for other forms of cancer where sojourn time is undefined [82], in order to take this into account, as previously described [52]. Although these calculations come with their limitations, these corrected calculations have also supported a risk benefit of those small melanoma lesions treated at an earlier stage.
A weakness of our study is that only chromosome 3 aberrations were assessed. We have demonstrated chromosome 3 status to be of the greatest predictive value in stratifying metastatic risk [83]; as such, we have used this parameter in these small samples. Other genetic alterations are well-known to contribute to an increased metastatic risk (e.g., gains of chromosome 8q, class 2 gene expression profiles and BAP1 (BRCA associated protein 1) mutations) [84,85,86,87,88,89,90]. We and others have developed bespoke next-generation sequencing panels for UM requiring smaller DNA concentrations from small lesions, which can be applied to a range of processed and size-varying samples [91,92]. The application of this molecular panel in future UM cohorts may enable us to delve further into the genetic interactions and intricacies of each patient subgroup with different sized tumors.
4. Methods
4.1. Study Design
We performed a retrospective case–control study of data from a cohort of UM patients diagnosed at the LOOC over the period of 2007–2014, to enable a minimum of 5 years of follow-up. All patients who had consented to genetic testing of their tumor were included. The diagnosis of UM was established by the presence of clinical signs of malignancy (e.g., orange pigment, low ultrasound reflectivity, serous retinal detachment and/or documented growth) and followed by treatment with local radiotherapy (with trans-scleral or trans-retinal biopsy), tumor resection or enucleation. We analyzed data on all our cases with a M3 or disomy 3 (D3) genetic result (see below). Tumors were classified as ‘small’ (≤2.5 mm in thickness) and ‘large’ (>2.5 mm in thickness). This size cut-off is based on the clinical risk factors previously described for small melanocytic lesions [54] of 2 mm and the T1 staging of small melanomas of 3 mm [55].
4.2. Clinical Methods
Date and certified cause of death were automatically provided by the National Health Service (NHS) Cancer Registry, the patients having been flagged at the time of diagnosis. International patients and those from Ireland were excluded from this study as their outcomes were not recorded within this NHS database.
4.3. Tumor Sampling
Tumor sample collection included material obtained during enucleation, trans-scleral tumor resection and primary tumor endoresection. Those undergoing radiotherapy as primary treatment (either proton beam or ruthenium-106 plaque brachytherapy) were biopsied by either the trans-scleral or trans-retinal route. Trans-retinal samples were obtained with a 25-gauge vitreous cutter, as previously described [93,94]. Trans-scleral biopsies were initially obtained with 25 g fine-needle aspiration (FNAB), then with Essen forceps scleral flap technique.
4.4. Genetic Analysis
Tumor DNA extraction, DNA quality assessment and quantification were conducted, as previously described [95,96]. Chromosome 3 aberrations were assessed by either multiplex ligation-dependent probe amplification (MLPA) (MRC-Holland, Amsterdam, The Netherlands) or microsatellite analysis (MSA). MLPA and MSA methods have been previously described [95,96,97,98,99].
4.5. Statistical Analysis
Gray rank statistics [100] were utilized to assess the differences in absolute risks of dying due to metastatic UM amongst the groups, enabling the consideration of competing risks. Hazard rates were also compared with the standard log-rank test. Lead time and length time biases were estimated according to the method described by Duffy et al. [82].
5. Conclusions
Our study has shown that treatment of small M3-UM is potentially lifesaving in its early stages. It is, therefore, necessary to identify and treat malignancy in these small, potentially lethal lesions without delay, if necessary, after performing intraocular tumor biopsies. There appears to be a survival benefit in treating all small UM to reduce the flow of metastatic cells and, more controversially, perhaps also small D3 UM to prevent conversion from low- to high-risk tumor characteristics, such as in those cases of developing genetic heterogeneity. This challenges the prevailing paradigm that clinically significant micrometastases occur prior to diagnosis of the ocular tumor, and suggests that a window of opportunity exists to reduce the flow of UM micrometastases and subsequent incurable, lethal dissemination. This window may only be available in the early stages of tumor development. Consequently, these small, lethal M3-UM may represent the only melanocytic lesions for which ophthalmologists can indeed alter patient mortality outcome with early treatment.
Author Contributions
Conceptualization and methodology R.N.H., H.H.; Data curation R.N.H., C.G.; Validation H.K.; Data analysis R.N.H., A.F.G.T., A.E.; Original draft preparation R.N.H.; Review and editing H.H., S.E.C., B.E.D., H.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. IRB approval was not required due to the retrospective audit data involved. Patients were consented for their data to be utilized in this analysis.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request on a secured database within the Oncology Unit.
Acknowledgments
Gary Cheetham, Liverpool Ocular Oncology data manager for obtaining complete long-term data for patients.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Lead Time Bias Calculations with Range of Lead Time Estimates
| Relative Fatality Rate | Mixing Fraction | Large Tumours Metastases Detection Probability | Large Tumours Fatality Rate | True RR | Approximate HR | |
| 0.5 | 0.5 | 0.1333 | 0.6707 | 0.7761 | 0.6617 | |
| 0.6 | 0.5 | 0.1500 | 0.6363 | 0.7271 | 0.6141 | |
| 0.7 | 0.5 | 0.1647 | 0.6035 | 0.6981 | 0.5913 | |
| 0.4 | 0.5 | 0.1143 | 0.7061 | 0.8599 | 0.7631 | |
| 0.3 | 0.5 | 0.0923 | 0.7416 | 1.0138 | 1.0298 | |
| 0.5 | 0.6 | 0.1429 | 0.6294 | 0.7719 | 0.6701 | |
| 0.6 | 0.6 | 0.1579 | 0.6064 | 0.7249 | 0.6210 | |
| 0.7 | 0.6 | 0.1707 | 0.5831 | 0.6971 | 0.5962 | |
| 0.4 | 0.6 | 0.1250 | 0.6513 | 0.8524 | 0.7689 | |
| 0.3 | 0.6 | 0.1034 | 0.6708 | 1.0001 | 1.0001 | |
| 0.5 | 0.7 | 0.1538 | 0.5941 | 0.7593 | 0.6652 | |
| 0.6 | 0.7 | 0.1667 | 0.5798 | 0.7182 | 0.6211 | |
| 0.7 | 0.7 | 0.1772 | 0.5644 | 0.6938 | 0.5980 | |
| 0.4 | 0.7 | 0.1379 | 0.6064 | 0.8297 | 0.7502 | |
| 0.3 | 0.7 | 0.1176 | 0.6152 | 0.9589 | 0.9334 | |
| 0.5 | 0.4 | 0.1250 | 0.7193 | 0.7719 | 0.6377 | |
| 0.6 | 0.4 | 0.1429 | 0.6702 | 0.7249 | 0.5996 | |
| 0.7 | 0.4 | 0.1591 | 0.6258 | 0.6971 | 0.5830 | |
| 0.4 | 0.4 | 0.1053 | 0.7735 | 0.8524 | 0.7252 | |
| 0.3 | 0.4 | 0.0833 | 0.8328 | 1.0001 | 1.0002 | |
| 0.5 | 0.3 | 0.1176 | 0.7769 | 0.7593 | 0.5941 | |
| 0.6 | 0.3 | 0.1364 | 0.7087 | 0.7182 | 0.5767 | |
| 0.7 | 0.3 | 0.1538 | 0.6502 | 0.6938 | 0.5711 | |
| 0.4 | 0.3 | 0.0976 | 0.8573 | 0.8297 | 0.6382 | |
| 0.3 | 0.3 | 0.0759 | 0.9529 | 0.9589 | 0.8022 | |
| Parameter | Large | Small | RR | 95% CI or Range | HR | 95% CI or Range |
| No. of Cancers | 332 | 44 | ||||
| Number with fup > 5 years | 147 | 33 | ||||
| Number of deaths ≤ 5 years | 165 | 10 | ||||
| 5-year fatality rate | 0.52 | 0.23 | ||||
| 5-year survival | 0.48 | 0.77 | 0.45 | 0.26–0.8 | 0.44 | 0.3–0.58 |
| after Lead Time Bias correction | ||||||
| 5-year fatality rate | 0.52 | 0.35 | ||||
| 5-year survival | 0.48 | 0.65 | 0.69 | 0.45–1.05 | 0.67 | 0.53–0.81 |
| after Length Time Bias correction | ||||||
| 5-year fatality rate | 0.52 | 0.40 | ||||
| 5-year survival | 0.48 | 0.60 | 0.78 | 0.69–1.01 | 0.64 | 0.57–1.03 |
References
- De Potter, P.; Shields, C.L.; Shields, J.A.; Cater, J.R.; Tardio, D.J. Impact of enucleation versus plaque radiotherapy in the management of juxtapapillary choroidal melanoma on patient survival. Br. J. Ophthalmol. 1994, 78, 109–114. [Google Scholar] [CrossRef]
- Collaborative Ocular Melanoma Study Group. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma: V. Twelve-year mortality rates and prognostic factors: COMS report No. 28. Arch. Ophthalmol. 2006, 124, 1684–1693. [Google Scholar] [CrossRef] [PubMed]
- Finger, P.T. Radiation therapy for choroidal melanoma. Surv. Ophthalmol. 1997, 42, 215–232. [Google Scholar] [CrossRef]
- Chang, M.Y.; McCannel, T.A. Local treatment failure after globe-conserving therapy for choroidal melanoma. Br. J. Ophthalmol. 2013, 97, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Damato, B.; Kacperek, A.; Chopra, M.; Campbell, I.R.; Errington, R.D. Proton beam radiotherapy of choroidal melanoma: The Liverpool-Clatterbridge experience. Int. J. Radiat. Oncol. Biol. Phys. 2005, 62, 1405–1411. [Google Scholar] [CrossRef]
- Russo, A.; Laguardia, M.; Damato, B. Eccentric ruthenium plaque radiotherapy of posterior choroidal melanoma. Graefes Arch. Clin. Exp. Ophthalmol. 2012, 250, 1533–1540. [Google Scholar] [CrossRef] [PubMed]
- Jmor, F.; Hussain, R.N.; Damato, B.E.; Heimann, H. Photodynamic therapy as initial treatment for small choroidal melanomas. Photodiagn. Photodyn. 2017, 20, 175–181. [Google Scholar] [CrossRef]
- Journee-de Korver, J.G.; Oosterhuis, J.A.; de Wolff-Rouendaal, D.; Kemme, H. Histopathological findings in human choroidal melanomas after transpupillary thermotherapy. Br. J. Ophthalmol. 1997, 81, 234–239. [Google Scholar] [CrossRef]
- Mashayekhi, A.; Shields, C.L.; Rishi, P.; Atalay, H.T.; Pellegrini, M.; McLaughlin, J.P.; Patrick, K.A.; Morton, S.J.; Remmer, M.H.; Parendo, A.; et al. Primary transpupillary thermotherapy for choroidal melanoma in 391 cases: Importance of risk factors in tumor control. Ophthalmology 2015, 122, 600–609. [Google Scholar] [CrossRef]
- Oosterhuis, J.A.; Journée-de Korver, H.G.; Keunen, J.E. Transpupillary thermotherapy: Results in 50 patients with choroidal melanoma. Arch. Ophthalmol. 1998, 116, 157–162. [Google Scholar] [CrossRef]
- Horgan, N.; Shields, C.L.; Mashayekhi, A.; Shields, J.A. Classification and treatment of radiation maculopathy. Curr. Opin. Ophthalmol. 2010, 21, 233–238. [Google Scholar] [CrossRef]
- Damato, B.E.; Dukes, J.; Goodall, H.; Carvajal, R.D. Tebentafusp: T Cell Redirection for the Treatment of Metastatic Uveal Melanoma. Cancers 2019, 11, 971. [Google Scholar] [CrossRef] [PubMed]
- Homsi, J.; Bedikian, A.Y.; Papadopoulos, N.E.; Kim, K.B.; Hwu, W.J.; Mahoney, S.L.; Hwu, P. Phase 2 open-label study of weekly docosahexaenoic acid-paclitaxel in patients with metastatic uveal melanoma. Melanoma Res. 2010, 20, 507–510. [Google Scholar] [CrossRef] [PubMed]
- Schmittel, A.; Schmidt-Hieber, M.; Martus, P.; Bechrakis, N.E.; Schuster, R.; Siehl, J.M.; Foerster, M.H.; Thiel, E.; Keilholz, U. A randomized phase II trial of gemcitabine plus treosulfan versus treosulfan alone in patients with metastatic uveal melanoma. Ann. Oncol. 2006, 17, 1826–1829. [Google Scholar] [CrossRef] [PubMed]
- Spagnolo, F.; Grosso, M.; Picasso, V.; Tornari, E.; Pesce, M.; Queirolo, P. Treatment of metastatic uveal melanoma with intravenous fotemustine. Melanoma Res. 2013, 23, 196–198. [Google Scholar] [CrossRef]
- Spagnolo, F.; Caltabiano, G.; Queirolo, P. Uveal melanoma. Cancer Treat. Rev. 2012, 38, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Carvajal, R.D.; Sosman, J.A.; Quevedo, J.F.; Milhem, M.M.; Joshua, A.M.; Kudchadkar, R.R.; Linette, G.P.; Gajewski, T.F.; Lutzky, J.; Lawson, D.H.; et al. Effect of selumetinib vs chemotherapy on progression-free survival in uveal melanoma: A randomized clinical trial. JAMA 2014, 311, 2397–2405. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, S.; Moon, J.; Margolin, K.A.; Weber, J.S.; Lao, C.D.; Othus, M.; Aparicio, A.M.; Ribas, A.; Sondak, V.K. Phase II trial of sorafenib in combination with carboplatin and paclitaxel in patients with metastatic uveal melanoma: SWOG S0512. PLoS ONE 2012, 7, e48787. [Google Scholar] [CrossRef]
- Gomez, D.; Wetherill, C.; Cheong, J.; Jones, L.; Marshall, E.; Damato, B.; Coupland, S.E.; Ghaneh, P.; Poston, G.J.; Malik, H.Z.; et al. The Liverpool uveal melanoma liver metastases pathway: Outcome following liver resection. J. Surg. Oncol. 2014, 109, 542–547. [Google Scholar] [CrossRef]
- Marshall, E.; Romaniuk, C.; Ghaneh, P.; Wong, H.; McKay, M.; Chopra, M.; Coupland, S.E.; Damato, B.E. MRI in the detection of hepatic metastases from high-risk uveal melanoma: A prospective study in 188 patients. Br. J. Ophthalmol. 2013, 97, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Karydis, I.; Chan, P.Y.; Wheater, M.; Arriola, E.; Szlosarek, P.W.; Ottensmeier, C.H. Clinical activity and safety of Pembrolizumab in Ipilimumab pre-treated patients with uveal melanoma. Oncoimmunology 2016, 5, e1143997. [Google Scholar] [CrossRef]
- Maio, M.; Danielli, R.; Chiarion-Sileni, V.; Pigozzo, J.; Parmiani, G.; Ridolfi, R.; De Rosa, F.; Del Vecchio, M.; Di Guardo, L.; Queirolo, P.; et al. Efficacy and safety of ipilimumab in patients with pre-treated, uveal melanoma. Ann. Oncol. 2013, 24, 2911–2915. [Google Scholar] [CrossRef] [PubMed]
- Luke, J.J.; Callahan, M.K.; Postow, M.A.; Romano, E.; Ramaiya, N.; Bluth, M.; Giobbie-Hurder, A.; Lawrence, D.P.; Ibrahim, N.; Ott, P.A.; et al. Clinical activity of ipilimumab for metastatic uveal melanoma: A retrospective review of the Dana-Farber Cancer Institute, Massachusetts General Hospital, Memorial Sloan-Kettering Cancer Center, and University Hospital of Lausanne experience. Cancer 2013, 119, 3687–3695. [Google Scholar] [CrossRef] [PubMed]
- Khattak, M.A.; Fisher, R.; Hughes, P.; Gore, M.; Larkin, J. Ipilimumab activity in advanced uveal melanoma. Melanoma Res. 2013, 23, 79–81. [Google Scholar] [CrossRef]
- Kelderman, S.; van der Kooij, M.K.; van den Eertwegh, A.J.; Soetekouw, P.M.; Jansen, R.L.; van den Brom, R.R.; Hospers, G.A.; Haanen, J.B.; Kapiteijn, E.; Blank, C.U. Ipilimumab in pretreated metastastic uveal melanoma patients. Results of the Dutch Working group on Immunotherapy of Oncology (WIN-O). Acta Oncol. 2013, 52, 1786–1788. [Google Scholar] [CrossRef] [PubMed]
- Sacco, J.J.; Kalirai, H.; Kenyani, J.; Figueiredo, C.R.; Coulson, J.M.; Coupland, S.E. Recent breakthroughs in metastatic uveal melanoma: A cause for optimism? Future Oncol. 2018, 14, 1335–1338. [Google Scholar] [CrossRef]
- Diener-West, M.; Hawkins, B.S.; Markowitz, J.A.; Schachat, A.P. A review of mortality from choroidal melanoma. II. A meta-analysis of 5-year mortality rates following enucleation, 1966 through 1988. Arch. Ophthalmol. 1992, 110, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Kujala, E.; Makitie, T.; Kivela, T. Very long-term prognosis of patients with malignant uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2003, 44, 4651–4659. [Google Scholar] [CrossRef] [PubMed]
- Burr, J.M.; Mitry, E.; Rachet, B.; Coleman, M.P. Survival from uveal melanoma in England and Wales 1986 to 2001. Ophthalmic Epidemiol. 2007, 14, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Diener-West, M.; Reynolds, S.M.; Agugliaro, D.J.; Caldwell, R.; Cumming, K.; Earle, J.D.; Hawkins, B.S.; Hayman, J.A.; Jaiyesimi, I.; Jampol, L.M.; et al. Development of metastatic disease after enrollment in the COMS trials for treatment of choroidal melanoma: Collaborative Ocular Melanoma Study Group Report No. 26. Arch. Ophthalmol. 2005, 123, 1639–1643. [Google Scholar] [CrossRef]
- Rietschel, P.; Panageas, K.S.; Hanlon, C.; Patel, A.; Abramson, D.H.; Chapman, P.B. Variates of survival in metastatic uveal melanoma. J. Clin. Oncol. 2005, 23, 8076–8080. [Google Scholar] [CrossRef]
- Damato, B.; Duke, C.; Coupland, S.E.; Hiscott, P.; Smith, P.A.; Campbell, I.; Douglas, A.; Howard, P. Cytogenetics of uveal melanoma: A 7-year clinical experience. Ophthalmology 2007, 114, 1925–1931. [Google Scholar] [CrossRef]
- Eleuteri, A.; Taktak, A.F.G.; Coupland, S.E.; Heimann, H.; Kalirai, H.; Damato, B. Prognostication of metastatic death in uveal melanoma patients: A Markov multi-state model. Comput. Biol. Med. 2018, 102, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Kivela, T.; Kujala, E. Prognostication in eye cancer: The latest tumor, node, metastasis classification and beyond. Eye 2013, 27, 243–252. [Google Scholar] [CrossRef] [PubMed]
- Royer-Bertrand, B.; Torsello, M.; Rimoldi, D.; El Zaoui, I.; Cisarova, K.; Pescini-Gobert, R.; Raynaud, F.; Zografos, L.; Schalenbourg, A.; Speiser, D.; et al. Comprehensive Genetic Landscape of Uveal Melanoma by Whole-Genome Sequencing. Am. J. Hum. Genet. 2016, 99, 1190–1198. [Google Scholar] [CrossRef] [PubMed]
- Decatur, C.L.; Ong, E.; Garg, N.; Anbunathan, H.; Bowcock, A.M.; Field, M.G.; Harbour, J.W. Driver Mutations in Uveal Melanoma: Associations with Gene Expression Profile and Patient Outcomes. JAMA Ophthalmol. 2016, 134, 728–733. [Google Scholar] [CrossRef] [PubMed]
- Landreville, S.; Agapova, O.A.; Harbour, J.W. Emerging insights into the molecular pathogenesis of uveal melanoma. Future Oncol. 2008, 4, 629–636. [Google Scholar] [CrossRef] [PubMed]
- White, V.A.; Chambers, J.D.; Courtright, P.D.; Chang, W.Y.; Horsman, D.E. Correlation of cytogenetic abnormalities with the outcome of patients with uveal melanoma. Cancer 1998, 83, 354–359. [Google Scholar] [CrossRef]
- Scholes, A.G.; Damato, B.E.; Nunn, J.; Hiscott, P.; Grierson, I.; Field, J.K. Monosomy 3 in uveal melanoma: Correlation with clinical and histologic predictors of survival. Invest. Ophthalmol. Vis. Sci. 2003, 44, 1008–1011. [Google Scholar] [CrossRef]
- Damato, B.; Dopierala, J.; Klaasen, A.; van Dijk, M.; Sibbring, J.; Coupland, S.E. Multiplex ligation-dependent probe amplification of uveal melanoma: Correlation with metastatic death. Investig. Ophthalmol. Vis. Sci. 2009, 50, 3048–3055. [Google Scholar] [CrossRef]
- Shields, C.L.; Ganguly, A.; Bianciotto, C.G.; Turaka, K.; Tavallali, A.; Shields, J.A. Prognosis of uveal melanoma in 500 cases using genetic testing of fine-needle aspiration biopsy specimens. Ophthalmology 2011, 118, 396–401. [Google Scholar] [CrossRef]
- Rospond-Kubiak, I.; Wróblewska-Zierhoffer, M.; Twardosz-Pawlik, H.; Kociecki, J. The Liverpool Uveal Melanoma Prognosticator Online (LUMPO) for prognosing metastasis free survival in the absence of cytogenetic data after ruthenium brachytherapy for uveal melanoma. Acta Ophthalmol. 2015, 93. [Google Scholar] [CrossRef]
- DeParis, S.W.; Taktak, A.; Eleuteri, A.; Enanoria, W.; Heimann, H.; Coupland, S.E.; Damato, B. External Validation of the Liverpool Uveal Melanoma Prognosticator Online. Investig. Ophthalmol. Vis. Sci. 2016, 57, 6116–6122. [Google Scholar] [CrossRef] [PubMed]
- Rola, A.C.; Taktak, A.; Eleuteri, A.; Kalirai, H.; Heimann, H.; Hussain, R.; Bonnett, L.J.; Hill, C.J.; Traynor, M.; Jager, M.J.; et al. Multicenter External Validation of the Liverpool Uveal Melanoma Prognosticator Online: An OOG Collaborative Study. Cancers 2020, 12, 477. [Google Scholar] [CrossRef]
- Damato, E.M.; Damato, B.E. Detection and time to treatment of uveal melanoma in the United Kingdom: An evaluation of 2384 patients. Ophthalmology 2012, 119, 1582–1589. [Google Scholar] [CrossRef] [PubMed]
- Damato, B. Time to treatment of uveal melanoma in the United Kingdom. Eye 2001, 15, 155–158. [Google Scholar] [CrossRef]
- Shields, C.L.; Furuta, M.; Thangappan, A.; Nagori, S.; Mashayekhi, A.; Lally, D.R.; Kelly, C.C.; Rudich, D.S.; Nagori, A.V.; Wakade, O.A.; et al. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch. Ophthalmol. 2009, 127, 989–998. [Google Scholar] [CrossRef]
- Shields, C.L.; Sioufi, K.; Srinivasan, A.; Di Nicola, M.; Masoomian, B.; Barna, L.E.; Bekerman, V.P.; Say, E.A.T.; Mashayekhi, A.; Emrich, J.; et al. Visual Outcome and Millimeter Incremental Risk of Metastasis in 1780 Patients with Small Choroidal Melanoma Managed by Plaque Radiotherapy. JAMA Ophthalmol. 2018, 136, 1325–1333. [Google Scholar] [CrossRef] [PubMed]
- Straatsma, B.R.; Diener-West, M.; Caldwell, R.; Engstrom, R.E.; Collaborative Ocular Melanoma Study, G. Mortality after deferral of treatment or no treatment for choroidal melanoma. Am. J. Ophthalmol. 2003, 136, 47–54. [Google Scholar] [CrossRef]
- Damato, B. Ocular treatment of choroidal melanoma in relation to the prevention of metastatic death—A personal view. Prog. Retin. Eye Res. 2018, 66, 187–199. [Google Scholar] [CrossRef]
- Damato, B. Choroidal melanoma endoresection, dandelions and allegory-based medicine. Br. J. Ophthalmol. 2008, 92, 1013–1014. [Google Scholar] [CrossRef] [PubMed]
- Hussain, R.; Czanner, G.; Taktak, A.; Damato, B.; Praidou, A.; Heimann, H. Mortality of Patients with Uveal Melanoma Detected by Diabetic Retinopathy Screening. Retina 2020, 40, 2198–2206. [Google Scholar] [CrossRef] [PubMed]
- Damato, B.E.; Heimann, H.; Kalirai, H.; Coupland, S.E. Age, survival predictors, and metastatic death in patients with choroidal melanoma: Tentative evidence of a therapeutic effect on survival. JAMA Ophthalmol. 2014, 132, 605–613. [Google Scholar] [CrossRef]
- Shields, C.L.; Shields, J.A.; Kiratli, H.; De Potter, P.; Cater, J.R. Risk factors for growth and metastasis of small choroidal melanocytic lesions. Ophthalmology 1995, 102, 1351–1361. [Google Scholar] [CrossRef]
- Kujala, E.; Damato, B.; Coupland, S.E.; Desjardins, L.; Bechrakis, N.E.; Grange, J.D.; Kivela, T. Staging of ciliary body and choroidal melanomas based on anatomic extent. J. Clin. Oncol. 2013, 31, 2825–2831. [Google Scholar] [CrossRef] [PubMed]
- McLean, I.W.; Zimmerman, L.E.; Foster, W.D. Survival rates after enucleation of eyes with malignant melanoma. Am. J. Ophthalmol. 1979, 88, 794–797. [Google Scholar] [CrossRef]
- Zimmerman, L.E.; McLean, I.W.; Foster, W.D. Does enucleation of the eye containing a malignant melanoma prevent or accelerate the dissemination of tumour cells. Br. J. Ophthalmol. 1978, 62, 420–425. [Google Scholar] [CrossRef] [PubMed]
- COMS. The Collaborative Ocular Melanoma Study (COMS) randomized trial of pre-enucleation radiation of large choroidal melanoma III: Local complications and observations following enucleation COMS report no. 11. Am. J. Ophthalmol. 1998, 126, 362–372. [Google Scholar] [CrossRef]
- Diener-West, M.; Earle, J.D.; Fine, S.L.; Hawkins, B.S.; Moy, C.S.; Reynolds, S.M.; Schachat, A.P.; Straatsma, B.R.; Collaborative Ocular Melanoma Study Group. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma, II: Characteristics of patients enrolled and not enrolled. COMS Report No. 17. Arch. Ophthalmol. 2001, 119, 951–965. [Google Scholar] [CrossRef]
- Zimmerman, L.E.; McLean, I.W. Do growth and onset of symptoms of uveal melanomas indicate subclinical metastasis? Ophthalmology 1984, 91, 685–691. [Google Scholar] [CrossRef]
- Singh, A.D. Uveal melanoma: Implications of tumor doubling time. Ophthalmology 2001, 108, 829–831. [Google Scholar] [CrossRef]
- Eskelin, S.; Pyrhonen, S.; Summanen, P.; Hahka-Kemppinen, M.; Kivela, T. Tumor doubling times in metastatic malignant melanoma of the uvea: Tumor progression before and after treatment. Ophthalmology 2000, 107, 1443–1449. [Google Scholar] [CrossRef]
- Tura, A.; Merz, H.; Reinsberg, M.; Luke, M.; Jager, M.J.; Grisanti, S.; Luke, J. Analysis of monosomy-3 in immunomagnetically isolated circulating melanoma cells in uveal melanoma patients. Pigment. Cell Melanoma Res. 2016, 29, 583–589. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, J. Invited commentary. Uveal melanoma: Implications of tumor doubling time. Ophthalmology 2001, 108, 831–832. [Google Scholar] [CrossRef]
- Jouhi, S.; Jager, M.J.; de Geus, S.J.R.; Desjardins, L.; Eide, N.A.; Grange, J.D.; Kiilgaard, J.F.; Seregard, S.; Midena, E.; Parrozzani, R.; et al. The Small Fatal Choroidal Melanoma Study. A Survey by the European Ophthalmic Oncology Group. Am. J. Ophthalmol. 2019, 202, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Boldt, H.C.; Binkley, E. Treating Small Choroidal Melanoma: Smaller Is Better. JAMA Ophthalmol. 2018, 136, 1333–1334. [Google Scholar] [CrossRef] [PubMed]
- Dopierala, J.; Damato, B.E.; Lake, S.L.; Taktak, A.F.; Coupland, S.E. Genetic heterogeneity in uveal melanoma assessed by multiplex ligation-dependent probe amplification. Investig. Ophthalmol. Vis. Sci. 2010, 51, 4898–4905. [Google Scholar] [CrossRef] [PubMed]
- Murray, T.G.; Sobrin, L. The case for observational management of suspected small choroidal melanoma. Arch. Ophthalmol. 2006, 124, 1342–1344. [Google Scholar] [CrossRef]
- Curtin, V.T. Natural course of small malignant melanomas of choroid and ciliary body. Trans. Ophthalmol. Soc. NZ 1978, 30, 61. [Google Scholar]
- Char, D.H. The management of small choroidal melanomas. Surv. Ophthalmol. 1978, 22, 377–386. [Google Scholar] [CrossRef]
- Lane, A.M.; Egan, K.M.; Kim, I.K.; Gragoudas, E.S. Mortality after diagnosis of small melanocytic lesions of the choroid. Arch. Ophthalmol. 2010, 128, 996–1000. [Google Scholar] [CrossRef]
- Butler, P.; Char, D.H.; Zarbin, M.; Kroll, S. Natural history of indeterminate pigmented choroidal tumors. Ophthalmology 1994, 101, 710–716, discussion 717. [Google Scholar] [CrossRef]
- Weis, E.; Roelofs, K.; Larocque, M.; Murtha, A. Gene Expression Profiling as an Adjunctive Measure to Guide the Management of Indeterminate, High-Risk Choroidal Melanocytic Lesions: A Pilot Study. Ocul. Oncol. Pathol. 2019, 5, 102–109. [Google Scholar] [CrossRef]
- Miller, A.K.; Benage, M.J.; Wilson, D.J.; Skalet, A.H. Uveal Melanoma with Histopathologic Intratumoral Heterogeneity Associated with Gene Expression Profile Discordance. Ocul. Oncol. Pathol. 2017, 3, 156–160. [Google Scholar] [CrossRef]
- Callejo, S.A.; Dopierala, J.; Coupland, S.E.; Damato, B. Sudden growth of a choroidal melanoma and multiplex ligation-dependent probe amplification findings suggesting late transformation to monosomy 3 type. Arch. Ophthalmol. 2011, 129, 958–960. [Google Scholar] [CrossRef]
- Field, M.G.; Durante, M.A.; Anbunathan, H.; Cai, L.Z.; Decatur, C.L.; Bowcock, A.M.; Kurtenbach, S.; Harbour, J.W. Punctuated evolution of canonical genomic aberrations in uveal melanoma. Nat. Commun. 2018, 9, 116. [Google Scholar] [CrossRef]
- White, V.A.; McNeil, B.K.; Thiberville, L.; Horsman, D.E. Acquired homozygosity (isodisomy) of chromosome 3 during clonal evolution of a uveal melanoma: Association with morphologic heterogeneity. Genes Chromosomes Cancer 1996, 15, 138–143. [Google Scholar] [CrossRef]
- Afshar, A.R.; Deiner, M.; Allen, G.; Damato, B.E. The Patient’s Experience of Ocular Melanoma in the US: A Survey of the Ocular Melanoma Foundation. Ocul. Oncol. Pathol. 2018, 4, 280–290. [Google Scholar] [CrossRef]
- Hopkins, J.; Keane, P.A.; Balaskas, K. Delivering personalized medicine in retinal care: From artificial intelligence algorithms to clinical application. Curr. Opin. Ophthalmol. 2020, 31, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Hussain, R.N.; Kalirai, H.; Groenewald, C.; Kacperek, A.; Errington, R.D.; Coupland, S.E.; Heimann, H.; Damato, B. Prognostic Biopsy of Choroidal Melanoma after Proton Beam Radiation Therapy. Ophthalmology 2016, 123, 2264–2265. [Google Scholar] [CrossRef] [PubMed]
- Angi, M.; Kalirai, H.; Taktak, A.; Hussain, R.; Groenewald, C.; Damato, B.E.; Heimann, H.; Coupland, S.E. Prognostic biopsy of choroidal melanoma: An optimised surgical and laboratory approach. Br. J. Ophthalmol. 2017, 101, 1143–1146. [Google Scholar] [CrossRef]
- Duffy, S.W.; Nagtegaal, I.D.; Wallis, M.; Cafferty, F.H.; Houssami, N.; Warwick, J.; Allgood, P.C.; Kearins, O.; Tappenden, N.; O’Sullivan, E.; et al. Correcting for lead time and length bias in estimating the effect of screen detection on cancer survival. Am. J. Epidemiol. 2008, 168, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Damato, B.; Eleuteri, A.; Hussain, R.; Kalirai, H.; Thornton, S.; Taktak, A.; Heimann, H.; Coupland, S.E. Parsimonious Models for Predicting Mortality from Choroidal Melanoma. Investig. Ophthalmol. Vis. Sci. 2020, 61, 35. [Google Scholar] [CrossRef]
- Parrella, P.; Sidransky, D.; Merbs, S.L. Allelotype of posterior uveal melanoma: Implications for a bifurcated tumor progression pathway. Cancer Res. 1999, 59, 3032–3037. [Google Scholar]
- Field, M.G.; Harbour, J.W. Recent developments in prognostic and predictive testing in uveal melanoma. Curr. Opin. Ophthalmol. 2014, 25, 234–239. [Google Scholar] [CrossRef]
- Onken, M.D.; Worley, L.A.; Ehlers, J.P.; Harbour, J.W. Gene expression profiling in uveal melanoma reveals two molecular classes and predicts metastatic death. Cancer Res. 2004, 64, 7205–7209. [Google Scholar] [CrossRef] [PubMed]
- Onken, M.D.; Ehlers, J.P.; Worley, L.A.; Makita, J.; Yokota, Y.; Harbour, J.W. Functional gene expression analysis uncovers phenotypic switch in aggressive uveal melanomas. Cancer Res. 2006, 66, 4602–4609. [Google Scholar] [CrossRef] [PubMed]
- Harbour, J.W. The genetics of uveal melanoma: An emerging framework for targeted therapy. Pigment. Cell Melanoma Res. 2012, 25, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Harbour, J.W.; Onken, M.D.; Roberson, E.D.; Duan, S.; Cao, L.; Worley, L.A.; Council, M.L.; Matatall, K.A.; Helms, C.; Bowcock, A.M. Frequent mutation of BAP1 in metastasizing uveal melanomas. Science 2010, 330, 1410–1413. [Google Scholar] [CrossRef] [PubMed]
- Robertson, A.G.; Shih, J.; Yau, C.; Gibb, E.A.; Oba, J.; Mungall, K.L.; Hess, J.M.; Uzunangelov, V.; Walter, V.; Danilova, L.; et al. Integrative Analysis Identifies Four Molecular and Clinical Subsets in Uveal Melanoma. Cancer Cell 2017, 32, 204–220.e215. [Google Scholar] [CrossRef]
- Smit, K.N.; van Poppelen, N.M.; Vaarwater, J.; Verdijk, R.; van Marion, R.; Kalirai, H.; Coupland, S.E.; Thornton, S.; Farquhar, N.; Dubbink, H.J.; et al. Combined mutation and copy-number variation detection by targeted next-generation sequencing in uveal melanoma. Mod. Pathol. 2018, 31, 763–771. [Google Scholar] [CrossRef]
- Thornton, S.; Coupland, S.E.; Olohan, L.; Sibbring, J.S.; Kenny, J.G.; Hertz-Fowler, C.; Liu, X.; Haldenby, S.; Heimann, H.; Hussain, R.; et al. Targeted Next-Generation Sequencing of 117 Routine Clinical Samples Provides Further Insights into the Molecular Landscape of Uveal Melanoma. Cancers 2020, 12, 1039. [Google Scholar] [CrossRef] [PubMed]
- Grixti, A.; Angi, M.; Damato, B.E.; Jmor, F.; Konstantinidis, L.; Groenewald, C.; Heimann, H. Vitreoretinal surgery for complications of choroidal tumor biopsy. Ophthalmology 2014, 121, 2482–2488. [Google Scholar] [CrossRef] [PubMed]
- Sen, J.; Groenewald, C.; Hiscott, P.S.; Smith, P.A.; Damato, B.E. Transretinal choroidal tumor biopsy with a 25-gauge vitrector. Ophthalmology 2006, 113, 1028–1031. [Google Scholar] [CrossRef] [PubMed]
- Coupland, S.E.; Kalirai, H.; Ho, V.; Thornton, S.; Damato, B.E.; Heimann, H. Concordant chromosome 3 results in paired choroidal melanoma biopsies and subsequent tumour resection specimens. Br. J. Ophthalmol. 2015, 99, 1444–1450. [Google Scholar] [CrossRef] [PubMed]
- Thornton, S.; Coupland, S.E.; Heimann, H.; Hussain, R.; Groenewald, C.; Kacperek, A.; Damato, B.; Taktak, A.; Eleuteri, A.; Kalirai, H. Effects of plaque brachytherapy and proton beam radiotherapy on prognostic testing: A comparison of uveal melanoma genotyped by microsatellite analysis. Br. J. Ophthalmol. 2020, 104, 1462–1466. [Google Scholar] [CrossRef]
- Tschentscher, F.; Prescher, G.; Zeschnigk, M.; Horsthemke, B.; Lohmann, D.R. Identification of chromosomes 3, 6, and 8 aberrations in uveal melanoma by microsatellite analysis in comparison to comparative genomic hybridization. Cancer Genet. Cytogenet. 2000, 122, 13–17. [Google Scholar] [CrossRef]
- Thomas, S.; Pütter, C.; Weber, S.; Bornfeld, N.; Lohmann, D.R.; Zeschnigk, M. Prognostic significance of chromosome 3 alterations determined by microsatellite analysis in uveal melanoma: A long-term follow-up study. Br. J. Cancer 2012, 106, 1171–1176. [Google Scholar] [CrossRef] [PubMed]
- Lake, S.L.; Kalirai, H.; Dopierala, J.; Damato, B.E.; Coupland, S.E. Comparison of formalin-fixed and snap-frozen samples analyzed by multiplex ligation-dependent probe amplification for prognostic testing in uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2012, 53, 2647–2652. [Google Scholar] [CrossRef]
- Gray, R.J. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann. Stat. 1988, 16, 1141–1154. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).