Feasibility and Early Clinical Experience of Online Adaptive MR-Guided Radiotherapy of Liver Tumors
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
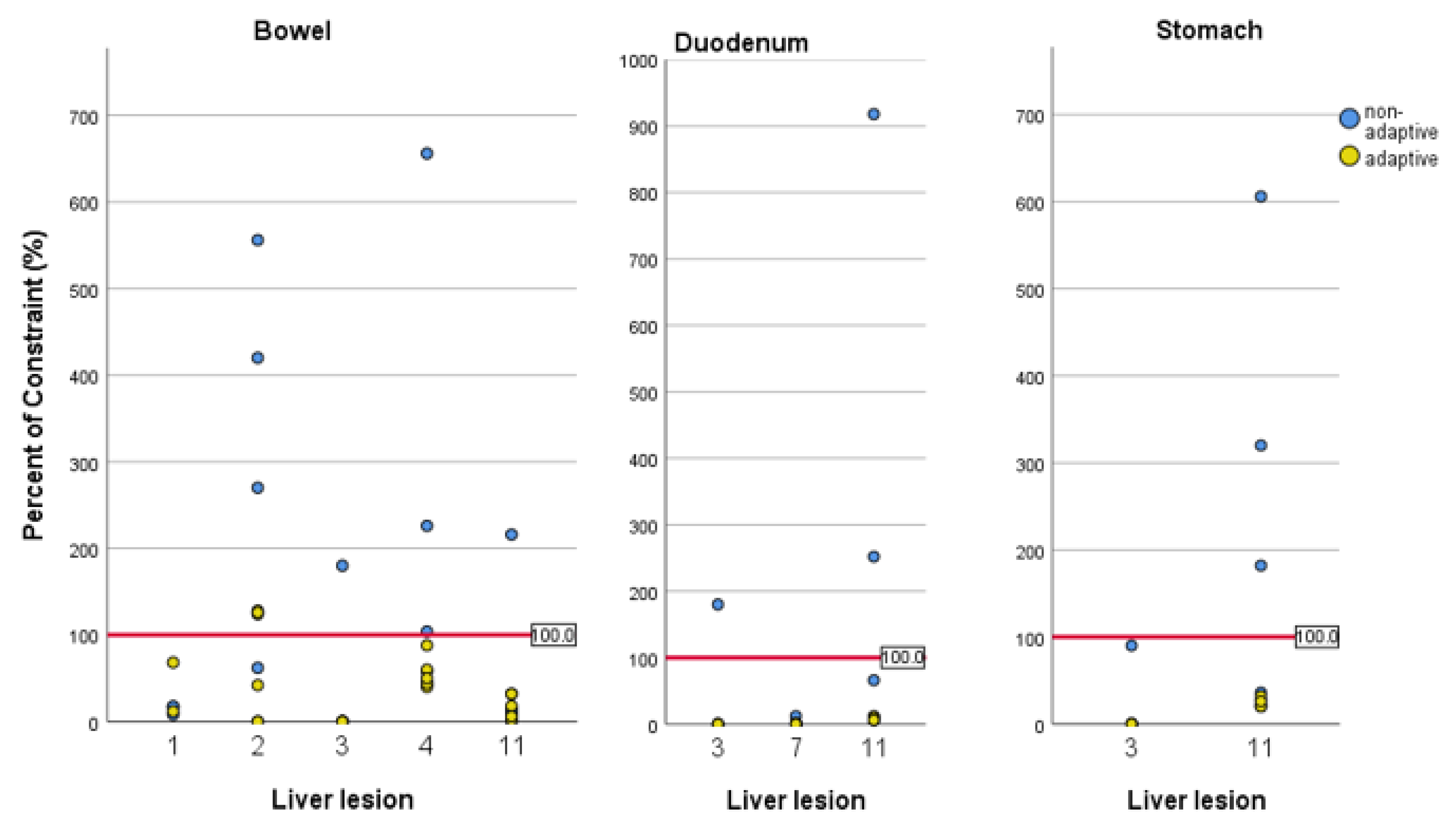
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosenberg, S.A.; Henke, L.E.; Shaverdian, N.; Mittauer, K.; Wojcieszynski, A.P.; Hullett, C.R.; Kamrava, M.; Lamb, J.; Cao, M.; Green, O.L.; et al. A Multi-Institutional Experience of MR-Guided Liver Stereotactic Body Radiation Therapy. Adv. Radiat. Oncol. 2019, 4, 142–149. [Google Scholar] [CrossRef]
- Ruers, T.; Van Coevorden, F.; Punt, C.J.A.; Pierie, J.P.E.N.; Borel-Rinkes, I.; Ledermann, J.A.; Poston, G.; Bechstein, W.; Lentz, M.A.; Mauer, M.; et al. Local Treatment of Unresectable Colorectal Liver Metastases: Results of a Randomized Phase II Trial. J. Natl. Cancer Inst. 2017, 109, djx015. [Google Scholar] [CrossRef]
- Ha, J.; Wong, R.J. Nonsurgical options for localized hepatocellular carcinoma. Clin. Liver Dis. 2017, 10, 103–106. [Google Scholar] [CrossRef]
- Hass, P.; Mohnike, K.; Kropf, S.; Brunner, T.B.; Walke, M.; Albers, D.; Petersen, C.; Damm, R.; Walter, F.; Ricke, J.; et al. Comparative analysis between interstitial brachytherapy and stereotactic body irradiation for local ablation in liver malignancies. Brachytherapy 2019, 18, 823–828. [Google Scholar] [CrossRef] [PubMed]
- Boldrini, L.; Romano, A.; Mariani, S.; Cusumano, D.; Catucci, F.; Placidi, L.; Mattiucci, G.C.; Chiloiro, G.; Cellini, F.; Gambacorta, M.A.; et al. MRI-guided stereotactic radiation therapy for hepatocellular carcinoma: A feasible and safe innovative treatment approach. J. Cancer Res. Clin. Oncol. 2021. [Google Scholar] [CrossRef]
- Gerum, S.; Heinz, C.; Belka, C.; Walter, F.; Paprottka, P.M.; De Toni, E.N.; Roeder, F. Stereotactic body radiotherapy in patients with hepatocellular carcinoma in a multimodal treatment setting. Strahlenther. Onkol. 2019. [Google Scholar] [CrossRef]
- Blechacz, B. Cholangiocarcinoma: Current knowledge and new developments. Gut Liver 2017, 11, 13–26. [Google Scholar] [CrossRef]
- Wahl, D.R.; Stenmark, M.H.; Tao, Y.; Pollom, E.L.; Caoili, E.M.; Lawrence, T.S.; Schipper, M.J.; Feng, M. Outcomes after stereotactic body radiotherapy or radiofrequency ablation for hepatocellular carcinoma. J. Clin. Oncol. 2016, 34, 452–459. [Google Scholar] [CrossRef]
- Sterzing, F.; Brunner, T.B.; Ernst, I.; Baus, W.W.; Greve, B.; Herfarth, K.; Guckenberger, M. Stereotaktische Strahlentherapie von Lebertumorenn: Grundlegende und praktische Leitlinien der DEGRO Arbeitsgruppe Stereotaxie. Strahlenther. Onkol. 2014, 190, 872–881. [Google Scholar] [CrossRef]
- Goodman, B.D.; Mannina, E.M.; Althouse, S.K.; Maluccio, M.A.; Cárdenes, H.R. Long-term safety and efficacy of stereotactic body radiation therapy for hepatic oligometastases. Pract. Radiat. Oncol. 2016, 6, 86–95. [Google Scholar] [CrossRef]
- Meyer, J.J.; Foster, R.D.; Lev-Cohain, N.; Yokoo, T.; Dong, Y.; Schwarz, R.E.; Rule, W.; Tian, J.; Xie, Y.; Hannan, R.; et al. A Phase I Dose-Escalation Trial of Single-Fraction Stereotactic Radiation Therapy for Liver Metastases. Ann. Surg. Oncol. 2016, 23, 218–224. [Google Scholar] [CrossRef]
- Rusthoven, K.E.; Kavanagh, B.D.; Cardenes, H.; Stieber, V.W.; Burri, S.H.; Feigenberg, S.J.; Chidel, M.A.; Pugh, T.J.; Franklin, W.; Kane, M.; et al. Multi-institutional phase I/II trial of stereotactic body radiation therapy for liver metastases. J. Clin. Oncol. 2009, 27, 1572–1578. [Google Scholar] [CrossRef]
- Clerici, E.; Comito, T.; Franzese, C.; Di Brina, L.; Tozzi, A.; Iftode, C.; Navarria, P.; Mancosu, P.; Reggiori, G.; Tomatis, S.; et al. Role of stereotactic body radiation therapy in the treatment of liver metastases: Clinical results and prognostic factors. Strahlenther. Onkol. 2020, 196, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Gkika, E.; Hallauer, L.; Kirste, S.; Adebahr, S.; Bartl, N.; Neeff, H.P.; Fritsch, R.; Brass, V.; Nestle, U.; Grosu, A.L.; et al. Stereotactic body radiotherapy (SBRT) for locally advanced intrahepatic and extrahepatic cholangiocarcinoma. BMC Cancer 2017, 17, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Brunner, T.B.; Blanck, O.; Lewitzki, V.; Abbasi-Senger, N.; Momm, F.; Riesterer, O.; Duma, M.N.; Wachter, S.; Baus, W.; Gerum, S.; et al. Stereotactic body radiotherapy dose and its impact on local control and overall survival of patients for locally advanced intrahepatic and extrahepatic cholangiocarcinoma. Radiother. Oncol. 2019, 132, 42–47. [Google Scholar] [CrossRef]
- Rule, W.; Timmerman, R.; Tong, L.; Abdulrahman, R.; Meyer, J.; Boike, T.; Schwarz, R.E.; Weatherall, P.; Cho, L.C. Phase i dose-escalation study of stereotactic body radiotherapy in patients with hepatic metastases. Ann. Surg. Oncol. 2011, 18, 1081–1087. [Google Scholar] [CrossRef]
- Tao, R.; Krishnan, S.; Bhosale, P.R.; Javle, M.M.; Aloia, T.A.; Shroff, R.T.; Kaseb, A.O.; Bishop, A.J.; Swanick, C.W.; Koay, E.J.; et al. Ablative radiotherapy doses lead to a substantial prolongation of survival in patients with inoperable intrahepatic cholangiocarcinoma: A retrospective dose response analysis. J. Clin. Oncol. 2016, 34, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Joo, J.H.; Park, J.H.; Kim, J.C.; Yu, C.S.; Lim, S.B.; Park, I.J.; Kim, T.W.; Hong, Y.S.; Kim, K.P.; Yoon, S.M.; et al. Local Control Outcomes Using Stereotactic Body Radiation Therapy for Liver Metastases From Colorectal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 876–883. [Google Scholar] [CrossRef]
- Abbas, H.; Chang, B.; Chen, Z. Motion management in gastrointestinal cancers. J. Gastrointest. Oncol. 2014, 5, 223–235. [Google Scholar] [CrossRef] [PubMed]
- Gargett, M.; Haddad, C.; Kneebone, A.; Booth, J.T.; Hardcastle, N. Clinical impact of removing respiratory motion during liver SABR. Radiat. Oncol. 2019, 14, 1–9. [Google Scholar] [CrossRef]
- Hong, T.S.; Wo, J.Y.; Yeap, B.Y.; Ben-Josef, E.; McDonnell, E.I.; Blaszkowsky, L.S.; Kwak, E.L.; Allen, J.N.; Clark, J.W.; Goyal, L.; et al. Multi-institutional phase II study of high-dose hypofractionated proton beam therapy in patients with localized, unresectable hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J. Clin. Oncol. 2016, 34, 460–468. [Google Scholar] [CrossRef]
- Gani, C.; Boeke, S.; McNair, H.; Ehlers, J.; Nachbar, M.; Mönnich, D.; Stolte, A.; Boldt, J.; Marks, C.; Winter, J.; et al. Marker-less online MR-guided stereotactic body radiotherapy of liver metastases at a 1.5 T MR-Linac—Feasibility, workflow data and patient acceptance. Clin. Transl. Radiat. Oncol. 2021, 26, 55–61. [Google Scholar] [CrossRef]
- Corradini, S.; Alongi, F.; Andratschke, N.; Belka, C.; Boldrini, L.; Cellini, F.; Debus, J.; Guckenberger, M.; Hörner-Rieber, J.; Lagerwaard, F.J.; et al. MR-guidance in clinical reality: Current treatment challenges and future perspectives. Radiat. Oncol. 2019, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Klüter, S.; Katayama, S.; Spindeldreier, C.K.; Koerber, S.A.; Major, G.; Alber, M.; Akbaba, S.; Debus, J.; Hörner-Rieber, J. First prospective clinical evaluation of feasibility and patient acceptance of magnetic resonance-guided radiotherapy in Germany. Strahlenther. Onkol. 2020, 196, 691–698. [Google Scholar] [CrossRef]
- Padgett, K.R.; Simpson, G.; Asher, D.; Portelance, L.; Bossart, E.; Dogan, N. Assessment of online adaptive MR-guided stereotactic body radiotherapy of liver cancers. Phys. Med. 2020, 77, 54–63. [Google Scholar] [CrossRef]
- Henke, L.; Kashani, R.; Robinson, C.; Curcuru, A.; DeWees, T.; Bradley, J.; Green, O.; Michalski, J.; Mutic, S.; Parikh, P.; et al. Phase I trial of stereotactic MR-guided online adaptive radiation therapy (SMART) for the treatment of oligometastatic or unresectable primary malignancies of the abdomen. Radiother. Oncol. 2018, 12, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Van Sörnsen de Koste, J.R.; Palacios, M.A.; Bruynzeel, A.M.E.; Slotman, B.J.; Senan, S.; Lagerwaard, F.J. MR-guided Gated Stereotactic Radiation Therapy Delivery for Lung, Adrenal, and Pancreatic Tumors: A Geometric Analysis. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 858–866. [Google Scholar] [CrossRef] [PubMed]
- Heinz, C.; Gerum, S.; Freislederer, P.; Ganswindt, U.; Roeder, F.; Corradini, S.; Belka, C.; Niyazi, M. Feasibility study on image guided patient positioning for stereotactic body radiation therapy of liver malignancies guided by liver motion. Radiat. Oncol. 2016, 11, 1–7. [Google Scholar] [CrossRef][Green Version]
- Feldman, A.M.; Modh, A.; Glide-Hurst, C.; Chetty, I.J.; Movsas, B. Real-time Magnetic Resonance-guided Liver Stereotactic Body Radiation Therapy: An Institutional Report Using a Magnetic Resonance-Linac System. Cureus 2019, 11. [Google Scholar] [CrossRef]
- Van Timmeren, J.E.; Chamberlain, M.; Krayenbuehl, J.; Wilke, L.; Ehrbar, S.; Bogowicz, M.; Hartley, C.; Zamburlini, M.; Andratschke, N.; Garcia Schüler, H.; et al. Treatment plan quality during online adaptive re-planning. Radiat. Oncol. 2020, 15, 1–11. [Google Scholar] [CrossRef]
- Stick, L.B.; Vogelius, I.R.; Risum, S.; Josipovic, M. Intrafractional fiducial marker position variations in stereotactic liver radiotherapy during voluntary deep inspiration breath-hold. Br. J. Radiol. 2020, 93, 20200859. [Google Scholar] [CrossRef]
- Son, S.H.; Choi, B.O.; Ryu, M.R.; Kang, Y.N.; Jang, J.S.; Bae, S.H.; Yoon, S.K.; Choi, I.B.; Kang, K.M.; Jang, H.S. Stereotactic body radiotherapy for patients with unresectable primary hepatocellular carcinoma: Dose-volumetric parameters predicting the hepatic complication. Int. J. Radiat. Oncol. Biol. Phys. 2010, 78, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Velec, M.; Haddad, C.R.; Craig, T.; Wang, L.; Lindsay, P.; Brierley, J.; Brade, A.; Ringash, J.; Wong, R.; Kim, J.; et al. Predictors of Liver Toxicity Following Stereotactic Body Radiation Therapy for Hepatocellular Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 939–946. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, K.A.; Caudell, J.J.; El-Haddad, G.; Berglund, A.E.; Welsh, E.A.; Yue, B.; Hoffe, S.E.; Naghavi, A.O.; Abuodeh, Y.A.; Frakes, J.M.; et al. Radiosensitivity Differences Between Liver Metastases Based on Primary Histology Suggest Implications for Clinical Outcomes After Stereotactic Body Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2016, 95, 1399–1404. [Google Scholar] [CrossRef] [PubMed]
- Mayo, S.C.; De Jong, M.C.; Pulitano, C.; Clary, B.M.; Reddy, S.K.; Gamblin, T.C.; Celinksi, S.A.; Kooby, D.A.; Staley, C.A.; Stokes, J.B.; et al. Surgical management of hepatic neuroendocrine tumor metastasis: Results from an international multi-institutional analysis. Ann. Surg. Oncol. 2010, 17, 3129–3136. [Google Scholar] [CrossRef]
- Gangi, A.; Howe, J.R. The Landmark Series: Neuroendocrine Tumor Liver Metastases. Ann. Surg. Oncol. 2020, 27, 3270–3280. [Google Scholar] [CrossRef]
- Pavel, M.; Baudin, E.; Couvelard, A.; Krenning, E.; Öberg, K.; Steinmüller, T.; Anlauf, M.; Wiedenmann, B.; Salazar, R. ENETS consensus guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 2012, 95, 157–176. [Google Scholar] [CrossRef]
- Howe, J.R.; Cardona, K.; Fraker, D.L.; Kebebew, E.; Untch, B.R.; Wang, Y.Z.; Law, C.H.; Liu, E.H.; Kim, M.K.; Menda, Y.; et al. The surgical management of small bowel neuroendocrine tumors. Pancreas 2017, 46, 715–731. [Google Scholar] [CrossRef]
- Moon, D.H.; Wang, A.Z.; Tepper, J.E. A prospective study of the safety and efficacy of liver stereotactic body radiotherapy in patients with and without prior liver-directed therapy. Radiother. Oncol. 2018, 126, 527–533. [Google Scholar] [CrossRef]


| Patients, n | 11 |
|---|---|
| Female, n (%) | 5 (45.5%) |
| Male, n (%) | 6 (54.5%) |
| Age (years), median (range) | 66 (47–86) |
| Karnofsky performance score, n (%) | |
| 100% | 1 (9.1%) |
| 90% | 6 (54.5%) |
| 80% | 3 (27.3%) |
| 60% | 1 (9.1%) |
| Histology of treated lesions, n (%) | |
| Cholangiocarcinoma | 2 (13.3%) |
| Metastasis neuroendocrine tumor | 6 (40.0%) |
| Metastasis colorectal adenocarcinoma | 4 (26.6%) |
| Metastasis sarcoma | 2 (13.3%) |
| Metastasis gastrointestinal stroma tumor | 1 (6.6%) |
| Pretreatments, n (%) | |
| Surgery | 4 (36.4%) |
| Brachytherapy | 3 (27.3%) |
| SIRT | 1 (9.1%) |
| No pretreatment | 4 (36.4%) |
| Dose Prescription | |
|---|---|
| 15 Gy × 3 (65% isodose, BED10: 112.5 Gy) | n = 2 (15.4%) |
| 12.5 Gy × 3 (65% isodose, BED10: 84.4 Gy) | n = 7 (53.8%) |
| 8 Gy × 5 (80% isodose, BED10: 72 Gy) | n = 2 (15.4%) |
| 7 Gy × 5 (80% isodose, BED10: 59.5) | n = 2 (15.4%) |
| PTV Prescription BED10 (Gy), median (range) | 84.4 (59.5–112.5) |
| PTV volume (cm3), median (range) | 39.1 (8.3–411.3) |
| GTV volume (cm3), median (range) | 16.5 (1.2–317.8) |
| GTV Mean BED10 (Gy), median (range) | 147.9 (71.7–200.5) |
| Liver volume (cm3), median (range) | 1242.5 (879.6–2625.3) |
| Liver Mean dose (Gy), median (range) | 5.6 (2.8–15.5) |
| Number of beams per fraction, median (range) | 11 (7–16) |
| Number of beam segments per fraction, median (range) | 33 (9–60) |
| Monitor units per fraction, median (range) | 3367 (1503–6776) |
| Calculated delivery time (min), median (range) | 13 (6–23) |
| Net beam-on time (min), median (range) | 10 (4–20) |
| Overall treatment duration (min), median (range) | 53 (46–78) |
| Online adaptive planning (number of fractions) | 46/47 fractions (97.8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogowski, P.; von Bestenbostel, R.; Walter, F.; Straub, K.; Nierer, L.; Kurz, C.; Landry, G.; Reiner, M.; Auernhammer, C.J.; Belka, C.; et al. Feasibility and Early Clinical Experience of Online Adaptive MR-Guided Radiotherapy of Liver Tumors. Cancers 2021, 13, 1523. https://doi.org/10.3390/cancers13071523
Rogowski P, von Bestenbostel R, Walter F, Straub K, Nierer L, Kurz C, Landry G, Reiner M, Auernhammer CJ, Belka C, et al. Feasibility and Early Clinical Experience of Online Adaptive MR-Guided Radiotherapy of Liver Tumors. Cancers. 2021; 13(7):1523. https://doi.org/10.3390/cancers13071523
Chicago/Turabian StyleRogowski, Paul, Rieke von Bestenbostel, Franziska Walter, Katrin Straub, Lukas Nierer, Christopher Kurz, Guillaume Landry, Michael Reiner, Christoph Josef Auernhammer, Claus Belka, and et al. 2021. "Feasibility and Early Clinical Experience of Online Adaptive MR-Guided Radiotherapy of Liver Tumors" Cancers 13, no. 7: 1523. https://doi.org/10.3390/cancers13071523
APA StyleRogowski, P., von Bestenbostel, R., Walter, F., Straub, K., Nierer, L., Kurz, C., Landry, G., Reiner, M., Auernhammer, C. J., Belka, C., Niyazi, M., & Corradini, S. (2021). Feasibility and Early Clinical Experience of Online Adaptive MR-Guided Radiotherapy of Liver Tumors. Cancers, 13(7), 1523. https://doi.org/10.3390/cancers13071523






