Bleeding by Bruton Tyrosine Kinase-Inhibitors: Dependency on Drug Type and Disease
Abstract
Simple Summary
Abstract
1. Introduction
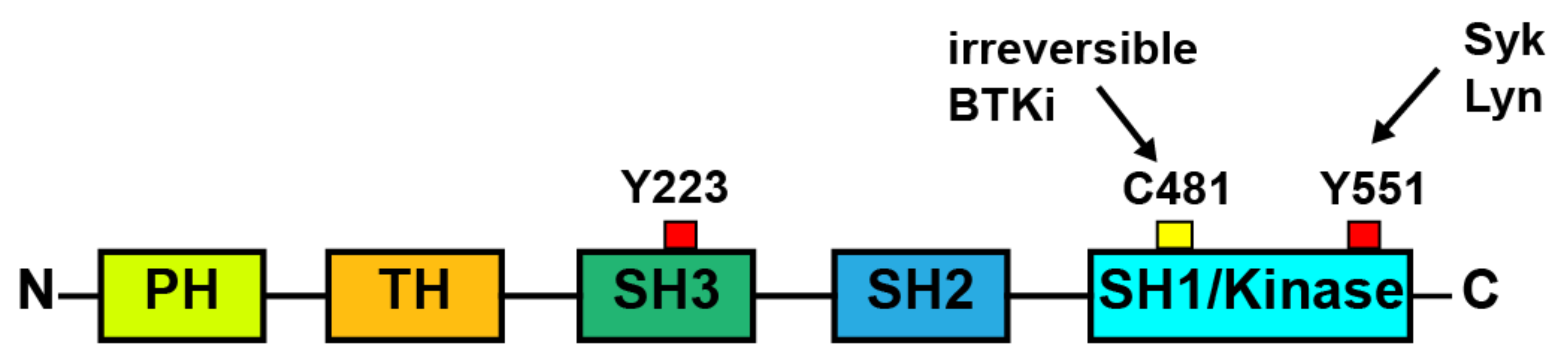
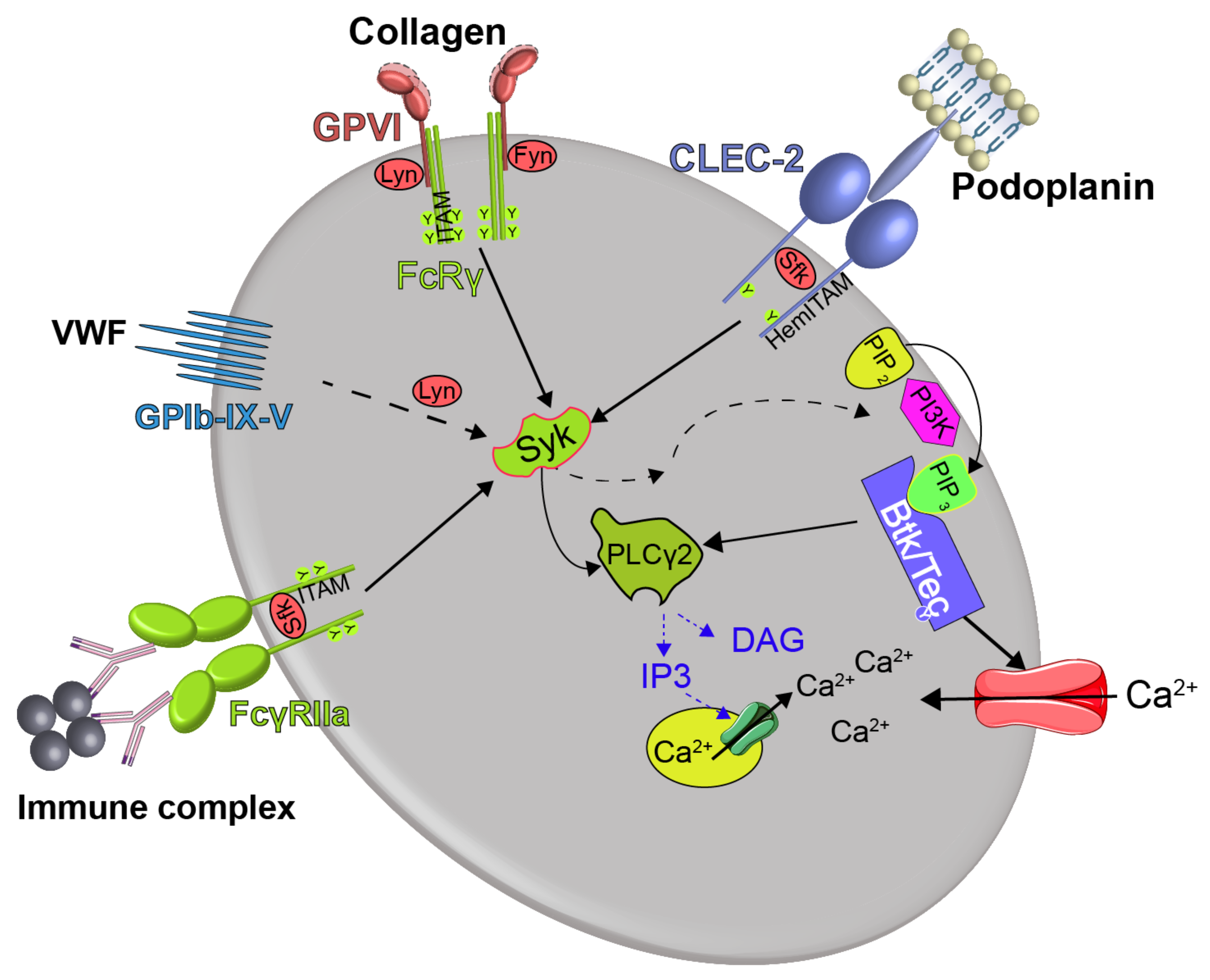
2. Role of Btk in Platelet Signaling and Platelet Effects of BTKi
2.1. Role of Btk in GPVI Signaling
2.2. Role of Btk in CLEC Signaling
2.3. Role of Btk in GPIb Signaling
2.4. Role of Btk in FcγRIIa Signaling
3. Btk Inhibitors (BTKi)
3.1. Irreversible Covalent BTKi
3.1.1. Ibrutinib
3.1.2. Acalabrutinib
3.1.3. Zanubrutinib
3.1.4. Tirabrutinib
3.1.5. Branebrutinib
3.1.6. BI 705564
3.2. Brain-Penetrant Irreversible Covalent BTKi
3.2.1. Evobrutinib
3.2.2. Tolebrutinib
3.3. Reversible BTKi
3.3.1. BMS-986142
3.3.2. Fenebrutinib
3.4. Rilzabrutinib, a Reversible Covalent BTKi
3.5. Novel Selective Covalent BTKi: Remibrutinib (LOU064), CHMFL-BTK-01
4. Bleeding After BTKi Treatment and Underlying Mechanisms
4.1. Bleeding Events in Patients with B-Cell Malignancies Treated with Irreversible BTKi
4.2. Disease-Related Mechanisms of Bleeding
4.3. Platelet-Dependent Mechanisms of Bleeding after Treatment of Patients with B-Cell Malignancies with Irreversible BTKi
4.4. No Bleeding in Clinical Trials with Reversible BTKi
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pal Singh, S.; Dammeijer, F.; Hendriks, R.W. Role of Bruton’s tyrosine kinase in B cells and malignancies. Mol. Cancer 2018, 17, 57. [Google Scholar] [CrossRef] [PubMed]
- Whang, J.A.; Chang, B.Y. Bruton’s tyrosine kinase inhibitors for the treatment of rheumatoid arthritis. Drug Discov. Today 2014, 19, 1200–1204. [Google Scholar] [CrossRef]
- Chang, B.Y.; Huang, M.M.; Francesco, M.; Chen, J.; Sokolove, J.; Magadala, P.; Robinson, W.H.; Buggy, J.J. The Bruton tyrosine kinase inhibitor PCI-32765 ameliorates autoimmune arthritis by inhibition of multiple effector cells. Arthritis Res. Ther. 2011, 13, R115. [Google Scholar] [CrossRef]
- Liang, C.; Tian, D.; Ren, X.; Ding, S.; Jia, M.; Xin, M.; Thareja, S. The development of Bruton’s tyrosine kinase (BTK) inhibitors from 2012 to 2017: A mini-review. Eur. J. Med. Chem. 2018, 151, 315–326. [Google Scholar] [CrossRef] [PubMed]
- Rigg, R.A.; Aslan, J.E.; Healy, L.D.; Wallisch, M.; Thierheimer, M.L.; Loren, C.P.; Pang, J.; Hinds, M.T.; Gruber, A.; McCarty, O.J. Oral administration of Bruton’s Tyrosine Kinase (Btk) inhibitors impairs GPVI-mediated platelet function. Am. J. Physiol. Cell Physiol. 2015, 310, C373–C380. [Google Scholar] [CrossRef]
- Futatani, T.; Watanabe, C.; Baba, Y.; Tsukada, S.; Ochs, H.D. Bruton’s tyrosine kinase is present in normal platelets and its absence identifies patients with X-linked agammaglobulinaemia and carrier females. Br. J. Haematol. 2001, 114, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Shillitoe, B.; Gennery, A. X-Linked Agammaglobulinaemia: Outcomes in the modern era. Clin. Immunol. 2017, 183, 54–62. [Google Scholar] [CrossRef]
- Busygina, K.; Jamasbi, J.; Seiler, T.; Deckmyn, H.; Weber, C.; Brandl, R.; Lorenz, R.; Siess, W. Oral Bruton tyrosine kinase inhibitors selectively block atherosclerotic plaque-triggered thrombus formation in humans. Blood 2018, 131, 2605–2616. [Google Scholar] [CrossRef]
- Busygina, K.; Denzinger, V.; Bernlochner, I.; Weber, C.; Lorenz, R.; Siess, W. Btk inhibitors as first oral atherothrombosis- selective antiplatelet drugs? Thromb. Haemost. 2019, 119, 1212–1221. [Google Scholar] [CrossRef]
- Nicolson, P.L.R.; Nock, S.H.; Hinds, J.; Garcia-Quintanilla, L.; Smith, C.W.; Campos, J.; Brill, A.; Pike, J.A.; Khan, A.O.; Poulter, N.S.; et al. Low dose Btk inhibitors selectively block platelet activation by CLEC-2. Haematologica 2020. [Google Scholar] [CrossRef]
- Payne, H.; Ponomaryov, T.; Watson, S.P.; Brill, A. Mice with a deficiency in CLEC-2 are protected against deep vein thrombosis. Blood 2017, 129, 2013–2020. [Google Scholar] [CrossRef]
- Nicolson, P.L.; Welsh, J.D.; Chauhan, A.; Thomas, M.R.; Kahn, M.L.; Watson, S.P. A rationale for blocking thromboinflammation in COVID-19 with Btk inhibitors. Platelets 2020, 31, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Goldmann, L.; Duan, R.; Kragh, T.; Wittmann, G.; Weber, C.; Lorenz, R.; von Hundelshausen, P.; Spannagl, M.; Siess, W. Oral Bruton tyrosine kinase inhibitors block activation of the platelet Fc receptor CD32a (FcγRIIA): A new option in HIT? Blood Adv. 2019, 3, 4021–4033. [Google Scholar] [CrossRef]
- Siess, W.; Hundelshausen, P.V.; Lorenz, R. Selective inhibition of thromboinflammation in COVID-19 by Btk inhibitors. Platelets 2020, 31, 989–992. [Google Scholar] [CrossRef]
- Treon, S.P.; Castillo, J.J.; Skarbnik, A.P.; Soumerai, J.D.; Ghobrial, I.M.; Guerrera, M.L.; Meid, K.; Yang, G. The BTK inhibitor ibrutinib may protect against pulmonary injury in COVID-19-infected patients. Blood 2020, 135, 1912–1915. [Google Scholar] [CrossRef]
- Roschewski, M.; Lionakis, M.S.; Sharman, J.P.; Roswarski, J.; Goy, A.; Monticelli, M.A.; Roshon, M.; Wrzesinski, S.H.; Desai, J.V.; Zarakas, M.A.; et al. Inhibition of Bruton tyrosine kinase in patients with severe COVID-19. Sci. Immunol. 2020, 5. [Google Scholar] [CrossRef]
- AstraZeneca. Update on CALAVI Phase II Trials for Calquence in Patients Hospitalised with Respiratory Symptoms of COVID-19. Available online: https://www.astrazeneca.com/media-centre/press-releases/2020/update-on-calavi-phase-ii-trials-for-calquence-in-patients-hospitalised-with-respiratory-symptoms-of-covid-19.html (accessed on 6 January 2021).
- Watson, S.P.; Herbert, J.M.; Pollitt, A.Y. GPVI and CLEC-2 in hemostasis and vascular integrity. J. Thromb. Haemost. 2010, 8, 1456–1467. [Google Scholar] [CrossRef] [PubMed]
- Moroi, A.J.; Watson, S.P. Impact of the PI3-kinase/Akt pathway on ITAM and hemITAM receptors: Haemostasis, platelet activation and antithrombotic therapy. Biochem. Pharm. 2015, 94, 186–194. [Google Scholar] [CrossRef]
- Arman, M.; Krauel, K. Human platelet IgG Fc receptor FcgammaRIIA in immunity and thrombosis. J. Thromb. Haemost. 2015, 13, 893–908. [Google Scholar] [CrossRef]
- Liu, J.; Fitzgerald, M.E.; Berndt, M.C.; Jackson, C.W.; Gartner, T.K. Bruton tyrosine kinase is essential for botrocetin/VWF-induced signaling and GPIb-dependent thrombus formation in vivo. Blood 2006, 108, 2596–2603. [Google Scholar] [CrossRef]
- Mohamed, A.J.; Yu, L.; Backesjo, C.M.; Vargas, L.; Faryal, R.; Aints, A.; Christensson, B.; Berglof, A.; Vihinen, M.; Nore, B.F.; et al. Bruton’s tyrosine kinase (Btk): Function, regulation, and transformation with special emphasis on the PH domain. Immunol. Rev. 2009, 228, 58–73. [Google Scholar] [CrossRef]
- Duarte, D.P.; Lamontanara, A.J.; La Sala, G.; Jeong, S.; Sohn, Y.K.; Panjkovich, A.; Georgeon, S.; Kükenshöner, T.; Marcaida, M.J.; Pojer, F.; et al. Btk SH2-kinase interface is critical for allosteric kinase activation and its targeting inhibits B-cell neoplasms. Nat. Commun. 2020, 11, 2319. [Google Scholar] [CrossRef]
- Watson, S.P.; Auger, J.M.; McCarty, O.J.; Pearce, A.C. GPVI and integrin alphaIIb beta3 signaling in platelets. J. Thromb. Haemost. 2005, 3, 1752–1762. [Google Scholar] [CrossRef]
- Baba, Y.; Hashimoto, S.; Matsushita, M.; Watanabe, D.; Kishimoto, T.; Kurosaki, T.; Tsukada, S. BLNK mediates Syk-dependent Btk activation. Proc. Natl. Acad. Sci. USA 2001, 98, 2582–2586. [Google Scholar] [CrossRef] [PubMed]
- Gibbins, J.M. Platelet adhesion signalling and the regulation of thrombus formation. J. Cell Sci. 2004, 117, 3415–3425. [Google Scholar] [CrossRef] [PubMed]
- Siess, W. Molecular mechanisms of platelet activation. Physiol. Rev. 1989, 69, 58–178. [Google Scholar] [CrossRef]
- Pasquet, J.M.; Quek, L.; Stevens, C.; Bobe, R.; Huber, M.; Duronio, V.; Krystal, G.; Watson, S.P. Phosphatidylinositol 3,4,5-trisphosphate regulates Ca(2+) entry via btk in platelets and megakaryocytes without increasing phospholipase C activity. Embo J. 2000, 19, 2793–2802. [Google Scholar] [CrossRef]
- Tomlinson, M.G.; Woods, D.B.; McMahon, M.; Wahl, M.I.; Witte, O.N.; Kurosaki, T.; Bolen, J.B.; Johnston, J.A. A conditional form of Bruton’s tyrosine kinase is sufficient to activate multiple downstream signaling pathways via PLC Gamma 2 in B cells. BMC Immunol. 2001, 2, 4. [Google Scholar] [CrossRef]
- Takata, M.; Kurosaki, T. A role for Bruton’s tyrosine kinase in B cell antigen receptor-mediated activation of phospholipase C-gamma 2. J. Exp. Med. 1996, 184, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Nicolson, P.L.R.; Hughes, C.E.; Watson, S.; Nock, S.H.; Hardy, A.T.; Watson, C.N.; Montague, S.J.; Malcor, J.D.; Thomas, M.R.; Pollitt, A.Y.; et al. Inhibition of Btk by Btk-specific concentrations of ibrutinib and acalabrutinib delays but does not block platelet aggregation to GPVI. Haematologica 2018, 103, 2097–2108. [Google Scholar] [CrossRef]
- Zeiler, M.; Moser, M.; Mann, M. Copy number analysis of the murine platelet proteome spanning the complete abundance range. Mol. Cell. Proteom. MCP 2014, 13, 3435–3445. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, J.M.; Vaudel, M.; Gambaryan, S.; Radau, S.; Walter, U.; Martens, L.; Geiger, J.; Sickmann, A.; Zahedi, R.P. The first comprehensive and quantitative analysis of human platelet protein composition allows the comparative analysis of structural and functional pathways. Blood 2012, 120, e73–e82. [Google Scholar] [CrossRef]
- Oda, A.; Ikeda, Y.; Ochs, H.D.; Druker, B.J.; Ozaki, K.; Handa, M.; Ariga, T.; Sakiyama, Y.; Witte, O.N.; Wahl, M.I. Rapid tyrosine phosphorylation and activation of Bruton’s tyrosine/Tec kinases in platelets induced by collagen binding or CD32 cross-linking. Blood 2000, 95, 1663–1670. [Google Scholar]
- Atkinson, B.T.; Ellmeier, W.; Watson, S.P. Tec regulates platelet activation by GPVI in the absence of Btk. Blood 2003, 102, 3592–3599. [Google Scholar] [CrossRef]
- Quek, L.S.; Bolen, J.; Watson, S.P. A role for Bruton’s tyrosine kinase (Btk) in platelet activation by collagen. Curr. Biol. CB 1998, 8, 1137–1140. [Google Scholar] [CrossRef]
- Kamel, S.; Horton, L.; Ysebaert, L.; Levade, M.; Burbury, K.; Tan, S.; Cole-Sinclair, M.; Reynolds, J.; Filshie, R.; Schischka, S.; et al. Ibrutinib inhibits collagen-mediated but not ADP-mediated platelet aggregation. Leukemia 2015, 29, 783–787. [Google Scholar] [CrossRef] [PubMed]
- Levade, M.; David, E.; Garcia, C.; Laurent, P.A.; Cadot, S.; Michallet, A.S.; Bordet, J.C.; Tam, C.; Sie, P.; Ysebaert, L.; et al. Ibrutinib treatment affects collagen and von Willebrand factor-dependent platelet functions. Blood 2014, 124, 3991–3995. [Google Scholar] [CrossRef]
- Bye, A.P.; Unsworth, A.J.; Desborough, M.J.; Hildyard, C.A.T.; Appleby, N.; Bruce, D.; Kriek, N.; Nock, S.H.; Sage, T.; Hughes, C.E.; et al. Severe platelet dysfunction in NHL patients receiving ibrutinib is absent in patients receiving acalabrutinib. Blood Adv. 2017, 1, 2610–2623. [Google Scholar] [CrossRef]
- Chen, J.; Kinoshita, T.; Gururaja, T.; Sukbuntherng, J.; James, D.; Lu, D.; Whang, J.; Versele, M.; Chang, B.Y. The effect of Bruton’s tyrosine kinase (BTK) inhibitors on collagen-induced platelet aggregation, BTK, and tyrosine kinase expressed in hepatocellular carcinoma (TEC). Eur. J. Haematol. 2018. [Google Scholar] [CrossRef]
- Denzinger, V.; Busygina, K.; Jamasbi, J.; Pekrul, I.; Spannagl, M.; Weber, C.; Lorenz, R.; Siess, W. Optimizing platelet GPVI inhibition versus hemostatic impairment by ibrutinib and the novel Btk-inhibitors acalabrutinib, ONO/GS-4059, BGB-3111 and evobrutinib. Thromb. Haemost. 2019, 119, 397–406. [Google Scholar] [PubMed]
- Toth, O.; Calatzis, A.; Penz, S.; Losonczy, H.; Siess, W. Multiple electrode aggregometry: A new device to measure platelet aggregation in whole blood. Thromb. Haemost. 2006, 96, 781–788. [Google Scholar] [PubMed]
- Bampalis, V.G.; Brantl, S.A.; Siess, W. Why and how to eliminate spontaneous platelet aggregation in blood measured by multiple electrode aggregometry. J. Thromb. Haemost. 2012, 10, 1710–1714. [Google Scholar] [CrossRef] [PubMed]
- Kodama, M.; Yamasaki, Y.; Sakamoto, K.; Yoshioka, R.; Matsuhisa, M.; Kajimoto, Y.; Kosugi, K.; Ueda, N.; Hori, M. Antiplatelet drugs attenuate progression of carotid intima-media thickness in subjects with type 2 diabetes. Thromb. Res. 2000, 97, 239–245. [Google Scholar] [CrossRef]
- Bye, A.P.; Gibbins, J.M. Move along, nothing to see here: Btk inhibitors stop platelets sticking to plaques. J. Thromb. Haemost. 2018. [Google Scholar] [CrossRef] [PubMed]
- Payrastre, B.; Ribes, A. Low-dose Btk inhibitors: An ‘aspirin’ of tomorrow? Haematologica 2021, 106, 2–4. [Google Scholar] [CrossRef]
- Kratzer, M.A.; Negrescu, E.V.; Hirai, A.; Yeo, Y.K.; Franke, P.; Siess, W. The Thrombostat system. A useful method to test antiplatelet drugs and diets. Semin. Thromb. Hemost. 1995, 21 (Suppl. S2), 25–31. [Google Scholar] [CrossRef]
- Kundu, S.K.; Heilmann, E.J.; Sio, R.; Garcia, C.; Davidson, R.M.; Ostgaard, R.A. Description of an in vitro platelet function analyzer--PFA-100. Semin. Thromb. Hemost. 1995, 21 (Suppl. S2), 106–112. [Google Scholar] [CrossRef]
- Cohen, S.; Tuckwell, K.; Katsumoto, T.R.; Zhao, R.; Galanter, J.; Lee, C.; Rae, J.; Toth, B.; Ramamoorthi, N.; Hackney, J.A.; et al. Fenebrutinib versus Placebo or Adalimumab in Rheumatoid Arthritis: A Randomized, Double-Blind, Phase II Trial (ANDES Study). Arthritis Rheumatol. 2020. [Google Scholar] [CrossRef]
- Jamasbi, J.; Ayabe, K.; Goto, S.; Nieswandt, B.; Peter, K.; Siess, W. Platelet receptors as therapeutic targets: Past, present and future. Thromb. Haemost. 2017, 117, 1249–1257. [Google Scholar] [CrossRef]
- Gruner, S.; Prostredna, M.; Aktas, B.; Moers, A.; Schulte, V.; Krieg, T.; Offermanns, S.; Eckes, B.; Nieswandt, B. Anti-glycoprotein VI treatment severely compromises hemostasis in mice with reduced alpha2beta1 levels or concomitant aspirin therapy. Circulation 2004, 110, 2946–2951. [Google Scholar] [CrossRef]
- Lee, R.H.; Piatt, R.; Conley, P.B.; Bergmeier, W. Effects of ibrutinib treatment on murine platelet function during inflammation and in primary hemostasis. Haematologica 2017, 102, e89–e92. [Google Scholar] [CrossRef] [PubMed]
- Ohlmann, P.; Hechler, B.; Ravanat, C.; Loyau, S.; Herrenschmidt, N.; Wanert, F.; Jandrot-Perrus, M.; Gachet, C. Ex vivo inhibition of thrombus formation by an anti-glycoprotein VI Fab fragment in non-human primates without modification of glycoprotein VI expression. J. Thromb. Haemost. 2008, 6, 1003–1011. [Google Scholar] [CrossRef] [PubMed]
- Reny, J.L.; De Moerloose, P.; Dauzat, M.; Fontana, P. Use of the PFA-100™ closure time to predict cardiovascular events in aspirin-treated cardiovascular patients: A systematic review and meta-analysis. J. Thromb. Haemost. 2008, 6, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Rayes, J.; Watson, S.P.; Nieswandt, B. Functional significance of the platelet immune receptors GPVI and CLEC-2. J. Clin. Investig. 2019, 129, 12–23. [Google Scholar] [CrossRef]
- Hitchcock, J.R.; Cook, C.N.; Bobat, S.; Ross, E.A.; Flores-Langarica, A.; Lowe, K.L.; Khan, M.; Dominguez-Medina, C.C.; Lax, S.; Carvalho-Gaspar, M.; et al. Inflammation drives thrombosis after Salmonella infection via CLEC-2 on platelets. J. Clin. Investig. 2015, 125, 4429–4446. [Google Scholar] [CrossRef]
- Kazianka, L.; Drucker, C.; Skrabs, C.; Thomas, W.; Melchardt, T.; Struve, S.; Bergmann, M.; Staber, P.B.; Porpaczy, E.; Einberger, C.; et al. Ristocetin-induced platelet aggregation for monitoring of bleeding tendency in CLL treated with ibrutinib. Leukemia 2017, 31, 1117–1122. [Google Scholar] [CrossRef] [PubMed]
- Alberelli, M.A.; Innocenti, I.; Autore, F.; Laurenti, L.; De Candia, E. Ibrutinib does not affect ristocetin-induced platelet aggregation evaluated by light transmission aggregometry in chronic lymphocytic leukemia patients. Haematologica 2018, 103, e119–e122. [Google Scholar] [CrossRef] [PubMed]
- Ninomoto, J.; Mokatrin, A.; Kinoshita, T.; Marimpietri, C.; Barrett, T.D.; Chang, B.Y.; Sukbuntherng, J.; James, D.F.; Crowther, M. Effects of ibrutinib on in vitro platelet aggregation in blood samples from healthy donors and donors with platelet dysfunction. Hematology 2020, 25, 112–117. [Google Scholar] [CrossRef]
- Hsu, J.; Gu, Y.; Tan, S.L.; Narula, S.; DeMartino, J.A.; Liao, C. Bruton’s Tyrosine Kinase mediates platelet receptor-induced generation of microparticles: A potential mechanism for amplification of inflammatory responses in rheumatoid arthritis synovial joints. Immunol. Lett. 2013, 150, 97–104. [Google Scholar] [CrossRef]
- Ankri, A.; Baranger, A.; Martin-Toutain, I.; Samson, Y.; Collet, J.P.; Montalescot, G.; Lejean, L. Impaired ristocetin–induced Platelet Aggregation in Whole Blood Assessed with a Multiplate© Analyser Suggests a New Mechanism of Antiplatelet Effect of Aspirin and Clopidogrel. Blood 2011, 118, 3362. [Google Scholar] [CrossRef]
- Kovacevic, K.D.; Greisenegger, S.; Langer, A.; Gelbenegger, G.; Buchtele, N.; Pabinger, I.; Petroczi, K.; Zhu, S.; Gilbert, J.C.; Jilma, B. The aptamer BT200 blocks von Willebrand factor and platelet function in blood of stroke patients. Sci. Rep. 2021, 11, 3092. [Google Scholar] [CrossRef]
- Veyradier, A. A new drug for an old concept: Aptamer to von Willebrand factor for prevention of arterial and microvascular thrombosis. Haematologica 2020, 105, 2512–2515. [Google Scholar] [CrossRef] [PubMed]
- Qiao, J.; Al-Tamimi, M.; Baker, R.I.; Andrews, R.K.; Gardiner, E.E. The platelet Fc receptor, FcgammaRIIa. Immunol. Rev. 2015, 268, 241–252. [Google Scholar] [CrossRef]
- Zufferey, A.; Kapur, R.; Semple, J.W. Pathogenesis and Therapeutic Mechanisms in Immune Thrombocytopenia (ITP). J. Clin. Med. 2017, 6. [Google Scholar] [CrossRef]
- Miltiadous, O.; Hou, M.; Bussel, J.B. Identifying and treating refractory ITP: Difficulty in diagnosis and role of combination treatment. Blood 2020, 135, 472–490. [Google Scholar] [CrossRef]
- Wei, G.; Luo, Q.; Wang, X.; Wu, X.; Xu, M.; Ding, N.; Zhao, Y.; Zhong, L.; Wang, J.; Wu, Y.; et al. Increased GPIbα shedding from platelets treated with immune thrombocytopenia plasma. Int. Immunopharmacol. 2019, 66, 91–98. [Google Scholar] [CrossRef]
- Reiff, S.D.; Muhowski, E.M.; Guinn, D.; Lehman, A.; Fabian, C.A.; Cheney, C.; Mantel, R.; Smith, L.; Johnson, A.J.; Young, W.B.; et al. Noncovalent inhibition of C481S Bruton tyrosine kinase by GDC-0853: A new treatment strategy for ibrutinib-resistant CLL. Blood 2018, 132, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Byrd, J.C.; Smith, S.; Wagner-Johnston, N.; Sharman, J.; Chen, A.I.; Advani, R.; Augustson, B.; Marlton, P.; Renee Commerford, S.; Okrah, K.; et al. First-in-human phase 1 study of the BTK inhibitor GDC-0853 in relapsed or refractory B-cell NHL and CLL. Oncotarget 2018, 9, 13023–13035. [Google Scholar] [CrossRef]
- Bond, D.A.; Woyach, J.A. Targeting BTK in CLL: Beyond Ibrutinib. Curr. Hematol. Malig. Rep. 2019, 14, 197–205. [Google Scholar] [CrossRef]
- Sunesis Pharmaceuticals. Sunesis Pharmaceuticals Announces Clinical Update on Vecabrutinib Program. Available online: https://www.globenewswire.com/news-release/2020/06/23/2051898/0/en/Sunesis-Pharmaceuticals-Announces-Clinical-Update-on-Vecabrutinib-Program.html (accessed on 15 December 2020).
- IMBRUVICA. Highlights of Prescribing Information. Available online: https://imbruvica.com/files/prescribing-information.pdf (accessed on 11 November 2020).
- Jaglowski, S.M.; Blazar, B.R. How ibrutinib, a B-cell malignancy drug, became an FDA-approved second-line therapy for steroid-resistant chronic GVHD. Blood Adv. 2018, 2, 2012–2019. [Google Scholar] [CrossRef]
- Pharmacyclics, Janssen Biotech. IMBRUVICA®—The Only Approved Oral, Once-Daily Treatment for Previously Treated Chronic Graft Versus Host Disease (cGVHD). Available online: https://imbruvicahcp.com/cgvhd (accessed on 10 December 2020).
- Advani, R.H.; Buggy, J.J.; Sharman, J.P.; Smith, S.M.; Boyd, T.E.; Grant, B.; Kolibaba, K.S.; Furman, R.R.; Rodriguez, S.; Chang, B.Y.; et al. Bruton tyrosine kinase inhibitor ibrutinib (PCI-32765) has significant activity in patients with relapsed/refractory B-cell malignancies. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 88–94. [Google Scholar] [CrossRef]
- De Vries, R.; Smit, J.W.; Hellemans, P.; Jiao, J.; Murphy, J.; Skee, D.; Snoeys, J.; Sukbuntherng, J.; Vliegen, M.; de Zwart, L.; et al. Stable isotope-labelled intravenous microdose for absolute bioavailability and effect of grapefruit juice on ibrutinib in healthy adults. Br. J. Clin. Pharmacol. 2016, 81, 235–245. [Google Scholar] [CrossRef] [PubMed]
- De Jong, J.; Skee, D.; Murphy, J.; Sukbuntherng, J.; Hellemans, P.; Smit, J.; de Vries, R.; Jiao, J.J.; Snoeys, J.; Mannaert, E. Effect of CYP3A perpetrators on ibrutinib exposure in healthy participants. Pharmacol. Res. Perspect. 2015, 3, e00156. [Google Scholar] [CrossRef]
- Byrd, J.C.; Harrington, B.; O’Brien, S.; Jones, J.A.; Schuh, A.; Devereux, S.; Chaves, J.; Wierda, W.G.; Awan, F.T.; Brown, J.R.; et al. Acalabrutinib (ACP-196) in Relapsed Chronic Lymphocytic Leukemia. N. Engl. J. Med. 2016, 374, 323–332. [Google Scholar] [CrossRef]
- Crawford, J.J.; Johnson, A.R.; Misner, D.L.; Belmont, L.D.; Castanedo, G.; Choy, R.; Coraggio, M.; Dong, L.; Eigenbrot, C.; Erickson, R.; et al. Discovery of GDC-0853: A Potent, Selective, and Noncovalent Bruton’s Tyrosine Kinase Inhibitor in Early Clinical Development. J. Med. Chem. 2018, 61, 2227–2245. [Google Scholar] [CrossRef] [PubMed]
- Senis, Y.A.; Mazharian, A.; Mori, J. Src family kinases: At the forefront of platelet activation. Blood 2014, 124, 2013–2024. [Google Scholar] [CrossRef]
- Bye, A.P.; Unsworth, A.J.; Vaiyapuri, S.; Stainer, A.R.; Fry, M.J.; Gibbins, J.M. Ibrutinib Inhibits Platelet Integrin alphaIIbbeta3 Outside-In Signaling and Thrombus Stability But Not Adhesion to Collagen. Arter. Thromb Vasc Biol 2015, 35, 2326–2335. [Google Scholar] [CrossRef] [PubMed]
- CALQUENCE. Highlights of Prescribing Information. 2020. Available online: https://www.azpicentral.com/calquence/calquence.pdf (accessed on 11 November 2020).
- Astrazeneca. Calquence Showed Long-Term Efficacy and Tolerability for Patients with Chronic Lymphocytic Leukaemia in Two Trials. Available online: https://www.astrazeneca.com/media-centre/press-releases/2020/calquence-showed-long-term-efficacy-and-tolerability-for-patients-with-chronic-lymphocytic-leukaemia-in-two-trials.html (accessed on 12 December 2020).
- BRUKINSA. Highlights of Prescribing Information. 2020. Available online: https://www.brukinsa.com/prescribing-information.pdf (accessed on 11 November 2020).
- Guo, Y.; Liu, Y.; Hu, N.; Yu, D.; Zhou, C.; Shi, G.; Zhang, B.; Wei, M.; Liu, J.; Luo, L.; et al. Discovery of Zanubrutinib (BGB-3111), a Novel, Potent, and Selective Covalent Inhibitor of Bruton’s Tyrosine Kinase. J. Med. Chem. 2019, 62, 7923–7940. [Google Scholar] [CrossRef]
- Tam, C.S.; Trotman, J.; Opat, S.; Burger, J.A.; Cull, G.; Gottlieb, D.; Harrup, R.; Johnston, P.B.; Marlton, P.; Munoz, J.; et al. Phase 1 study of the selective BTK inhibitor zanubrutinib in B-cell malignancies and safety and efficacy evaluation in CLL. Blood 2019, 134, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Dobie, G.; Kuriri, F.A.; Omar, M.M.A.; Alanazi, F.; Gazwani, A.M.; Tang, C.P.S.; Sze, D.M.; Handunnetti, S.M.; Tam, C.; Jackson, D.E. Ibrutinib, but not zanubrutinib, induces platelet receptor shedding of GPIb-IX-V complex and integrin αIIbβ3 in mice and humans. Blood Adv. 2019, 3, 4298–4311. [Google Scholar] [CrossRef] [PubMed]
- PMDA (Pharmaceuticals and Medical Devices Agency) Japan. VELEXBRU (Tirabrutinib). Japanese Prescribing Information. 2020. Available online: https://www.pmda.go.jp/files/000237315.pdf (accessed on 12 December 2020).
- Dhillon, S. Tirabrutinib: First Approval. Drugs 2020, 80, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Liclican, A.; Serafini, L.; Xing, W.; Czerwieniec, G.; Steiner, B.; Wang, T.; Brendza, K.M.; Lutz, J.D.; Keegan, K.S.; Ray, A.S.; et al. Biochemical characterization of tirabrutinib and other irreversible inhibitors of Bruton’s tyrosine kinase reveals differences in on—and off—target inhibition. Biochim. Et Biophys. Acta. Gen. Subj. 2020, 1864, 129531. [Google Scholar] [CrossRef] [PubMed]
- Walter, H.S.; Rule, S.A.; Dyer, M.J.; Karlin, L.; Jones, C.; Cazin, B.; Quittet, P.; Shah, N.; Hutchinson, C.V.; Honda, H.; et al. A phase 1 clinical trial of the selective BTK inhibitor ONO/GS-4059 in relapsed and refractory mature B-cell malignancies. Blood 2016, 127, 411–419. [Google Scholar] [CrossRef]
- Yu, H.; Truong, H.; Mitchell, S.A.; Liclican, A.; Gosink, J.J.; Li, W.; Lin, J.; Feng, J.Y.; Jürgensmeier, J.M.; Billin, A.; et al. Homogeneous BTK Occupancy Assay for Pharmacodynamic Assessment of Tirabrutinib (GS-4059/ONO-4059) Target Engagement. Slas Discov. 2018, 23, 919–929. [Google Scholar] [CrossRef]
- Series, J.; Ribes, A.; Garcia, C.; Souleyreau, P.; Bauters, A.; Morschhauser, F.; Jürgensmeier, J.M.; Sié, P.; Ysebaert, L.; Payrastre, B. Effects of novel Btk and Syk inhibitors on platelet functions alone and in combination in vitro and in vivo. J. Thromb. Haemost. 2020. [Google Scholar] [CrossRef]
- Watterson, S.H.; Liu, Q.; Beaudoin Bertrand, M.; Batt, D.G.; Li, L.; Pattoli, M.A.; Skala, S.; Cheng, L.; Obermeier, M.T.; Moore, R.; et al. Discovery of Branebrutinib (BMS-986195): A Strategy for Identifying a Highly Potent and Selective Covalent Inhibitor Providing Rapid in Vivo Inactivation of Bruton’s Tyrosine Kinase (BTK). J. Med. Chem. 2019, 62, 3228–3250. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Batt, D.G.; Chaudhry, C.; Lippy, J.S.; Pattoli, M.A.; Surti, N.; Xu, S.; Carter, P.H.; Burke, J.R.; Tino, J.A. Conversion of carbazole carboxamide based reversible inhibitors of Bruton’s tyrosine kinase (BTK) into potent, selective irreversible inhibitors in the carbazole, tetrahydrocarbazole, and a new 2,3-dimethylindole series. Bioorganic Med. Chem. Lett. 2018, 28, 3080–3084. [Google Scholar] [CrossRef] [PubMed]
- Catlett, I.M.; Nowak, M.; Kundu, S.; Zheng, N.; Liu, A.; He, B.; Girgis, I.G.; Grasela, D.M. Safety, pharmacokinetics and pharmacodynamics of branebrutinib (BMS-986195), a covalent, irreversible inhibitor of Bruton’s tyrosine kinase: Randomised phase I, placebo-controlled trial in healthy participants. Br. J. Clin. Pharmacol. 2020, 86, 1849–1859. [Google Scholar] [CrossRef]
- Litzenburger, T.; Steffgen, J.; Benediktus, E.; Müller, F.; Schultz, A.; Klein, E.; Ramanujam, M.; Harcken, C.; Gupta, A.; Wu, J.; et al. Safety, pharmacokinetics and pharmacodynamics of BI 705564, a highly selective, covalent inhibitor of Bruton’s tyrosine kinase, in Phase I clinical trials in healthy volunteers. Br. J. Clin. Pharmacol. 2020. [Google Scholar] [CrossRef]
- Caldwell, R.D.; Qiu, H.; Askew, B.C.; Bender, A.T.; Brugger, N.; Camps, M.; Dhanabal, M.; Dutt, V.; Eichhorn, T.; Gardberg, A.S.; et al. Discovery of Evobrutinib: An Oral, Potent, and Highly Selective, Covalent Bruton’s Tyrosine Kinase (BTK) Inhibitor for the Treatment of Immunological Diseases. J. Med. Chem. 2019, 62, 7643–7655. [Google Scholar] [CrossRef] [PubMed]
- Haselmayer, P.; Camps, M.; Liu-Bujalski, L.; Nguyen, N.; Morandi, F.; Head, J.; O’Mahony, A.; Zimmerli, S.C.; Bruns, L.; Bender, A.T.; et al. Efficacy and Pharmacodynamic Modeling of the BTK Inhibitor Evobrutinib in Autoimmune Disease Models. J. Immunol. 2019, 202, 2888–2906. [Google Scholar] [CrossRef] [PubMed]
- Piper, L. Evobrutinib fails to improve response rate in refractory RA patients. Med. Matters 2020. Available online: https://rheumatology.medicinematters.com/acr-2020/rheumatoid-arthritis-/evobrutinib-refractory-ra-patients/18571522 (accessed on 15 December 2020).
- Montalban, X.; Arnold, D.L.; Weber, M.S.; Staikov, I.; Piasecka-Stryczynska, K.; Willmer, J.; Martin, E.C.; Dangond, F.; Syed, S.; Wolinsky, J.S.; et al. Placebo-Controlled Trial of an Oral BTK Inhibitor in Multiple Sclerosis. N. Engl. J. Med. 2019, 380, 2406–2417. [Google Scholar] [CrossRef]
- Merck. Evobrutinib Relapsing Multiple Sclerosis (RMS) Update Call. Available online: https://www.merckgroup.com/investors/events-and-presentations/webcasts-and-presentations/2020/en/2020_Evobrutinib_Strategy_Update_EN.pdf (accessed on 17 December 2020).
- Carvalho, J. Tolebrutinib Prevents Myelin Loss of in Mouse Model of MS-Like Demyelination. Sclerosis News Today 2020. Available online: https://multiplesclerosisnewstoday.com/news-posts/2020/09/09/sanofi-genzyme-continues-research-to-improve-the-lives-of-patients-with-multiple-sclerosis-with-new-data-presented-at-msvirtual2020/ (accessed on 17 December 2020).
- Smith, P.F.; Owens, T.D.; Langrish, C.L.; Xing, Y.; Francesco, M.R.; Shu, J.; Hartmann, S.; Karr, D.; Burns, R.; Quesenberry, R.; et al. Phase 1 Clinical Trial of PRN2246 (SAR442168), a Covalent BTK Inhibitor Demonstrates Safety, CNSExposure and Therapeutic Levels of BTK Occupancy; Principia: London, UK, 2019; Poster; Available online: https://www.principiabio.com/wp-content/uploads/2019/12/2019.02-PRN2246-Smith-ACTRIMS.pdf (accessed on 15 December 2020).
- Watterson, S.H.; De Lucca, G.V.; Shi, Q.; Langevine, C.M.; Liu, Q.; Batt, D.G.; Beaudoin Bertrand, M.; Gong, H.; Dai, J.; Yip, S.; et al. Discovery of 6-Fluoro-5-(R)-(3-(S)-(8-fluoro-1-methyl-2,4-dioxo-1,2-dihydroquinazolin-3(4H)-yl)-2-methylphenyl)-2-(S)-(2-hydroxypropan-2-yl)-2,3,4,9-tetrahydro-1H-carbazole-8-carboxamide (BMS-986142): A Reversible Inhibitor of Bruton’s Tyrosine Kinase (BTK) Conformationally Constrained by Two Locked Atropisomers. J. Med. Chem. 2016, 59, 9173–9200. [Google Scholar] [CrossRef]
- Lee, S.K.; Xing, J.; Catlett, I.M.; Adamczyk, R.; Griffies, A.; Liu, A.; Murthy, B.; Nowak, M. Safety, pharmacokinetics, and pharmacodynamics of BMS-986142, a novel reversible BTK inhibitor, in healthy participants. Eur. J. Clin. Pharmacol. 2017, 73, 689–698. [Google Scholar] [CrossRef]
- Gillooly, K.M.; Pulicicchio, C.; Pattoli, M.A.; Cheng, L.; Skala, S.; Heimrich, E.M.; McIntyre, K.W.; Taylor, T.L.; Kukral, D.W.; Dudhgaonkar, S.; et al. Bruton’s tyrosine kinase inhibitor BMS-986142 in experimental models of rheumatoid arthritis enhances efficacy of agents representing clinical standard-of-care. PLoS ONE 2017, 12, e0181782. [Google Scholar] [CrossRef] [PubMed]
- Bristol-Myers Squibb. Efficacy and Safety Study of BMS-986142 in Patients with Moderate to Severe Rheumatoid Arthritis. In Clin. Trials Gov.; 2020. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02638948 (accessed on 16 December 2020).
- Di Paolo, J.A.; Huang, T.; Balazs, M.; Barbosa, J.; Barck, K.H.; Bravo, B.J.; Carano, R.A.; Darrow, J.; Davies, D.R.; DeForge, L.E.; et al. Specific Btk inhibition suppresses B cell- and myeloid cell-mediated arthritis. Nat. Chem. Biol. 2011, 7, 41–50. [Google Scholar] [CrossRef]
- Gabizon, R.; London, N. A Fast and Clean BTK Inhibitor. J. Med. Chem. 2020, 63, 5100–5101. [Google Scholar] [CrossRef] [PubMed]
- Herman, A.E.; Chinn, L.W.; Kotwal, S.G.; Murray, E.R.; Zhao, R.; Florero, M.; Lin, A.; Moein, A.; Wang, R.; Bremer, M.; et al. Safety, Pharmacokinetics, and Pharmacodynamics in Healthy Volunteers Treated With GDC-0853, a Selective Reversible Bruton’s Tyrosine Kinase Inhibitor. Clin. Pharmacol. Ther. 2018, 103, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- Isenberg, D.; Furie, R.; Jones, N.S.; Guibord, P.; Galanter, J.; Lee, C.; Mcgregor, A.; Toth, B.; Rae, J.; Hwang, O.; et al. Efficacy, safety, and pharmacodynamics effects of the Bruton’s tyrosine kinase inhibitor, fenebrutinib (GDC-0853), in moderate to severe systemic lupus erythematosus in a phase 2 controlled study. Ann. Rheum. Dis. 2020. Available online: https://ard.bmj.com/content/79/Suppl_1/148.1 (accessed on 16 December 2020).
- Bradshaw, J.M.; McFarland, J.M.; Paavilainen, V.O.; Bisconte, A.; Tam, D.; Phan, V.T.; Romanov, S.; Finkle, D.; Shu, J.; Patel, V.; et al. Prolonged and tunable residence time using reversible covalent kinase inhibitors. Nat. Chem. Biol. 2015, 11, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Murrell, D.F.; Gourlay, S.G.; Hill, R.J.; Bisconte, A.; Francesco, M.; Smith, P.; Karr, D.; Outerbridge, C.; Varjonen, K.; Goodale, E.C.; et al. Development of PRN1008, a novel, reversible covalent BTK inhibitor in clinical development for pemphigus. In Proceedings of the Medical Dermatology Society Annual Meeting, Washington, DC, USA, 3 March 2016; Available online: https://www.principiabio.com/wp-content/uploads/2016/03/2016_05_PRN473_PRN1008_Murrell_MDS.pdf (accessed on 17 December 2020).
- Smith, P.F.; Krishnarajah, J.; Nunn, P.A.; Hill, R.J.; Karr, D.; Tam, D.; Masjedizadeh, M.; Funk, J.O.; Gourlay, S.G. A phase I trial of PRN1008, a novel reversible covalent inhibitor of Bruton’s tyrosine kinase, in healthy volunteers. Br. J. Clin. Pharmacol. 2017, 83, 2367–2376. [Google Scholar] [CrossRef]
- Kuter, D.J.; Boccia, R.V.; Lee, E.-J.; Efraim, M.; Tzvetkov, N.; Mayer, J.; Trněný, M.; Kostal, M.; Hajek, R.; McDonald, V.; et al. Phase I/II, Open-Label, Adaptive Study of Oral Bruton Tyrosine Kinase Inhibitor PRN1008 in Patients with Relapsed/Refractory Primary or Secondary Immune Thrombocytopenia. Blood 2019, 134, 87. [Google Scholar] [CrossRef]
- Principia Biopharm. Principia Announces Positive Data from Its Phase 2 Part B Trial in Pemphigus. Available online: https://www.globenewswire.com/news-release/2020/06/12/2047632/0/en/Principia-Announces-Positive-Data-from-its-Phase-2-Part-B-Trial-in-Pemphigus.html (accessed on 29 November 2020).
- Langrish, C.L.; Bradshaw, J.M.; Owens, T.D.; Campbell, R.L.; Francesco, M.R.; Karr, D.E.; Murray, S.K.; Quesenberry, R.C.; Smith, P.F.; Taylor, M.D.; et al. PRN1008, a Reversible Covalent BTK Inhibitor in Clinical Development for Immune Thrombocytopenic Purpura. Blood 2017, 130, 1052. Available online: https://www.principiabio.com/wp-content/uploads/2019/12/2017.12-PRN1008-Langrish-ASH.pdf (accessed on 17 December 2020).
- Pulz, R.; Angst, D.; Dawson, J.; Gessier, F.; Gutmann, S.; Hersperger, R.; Hinniger, A.; Janser, P.; Koch, G.; Revesz, L.; et al. Design of Potent and Selective Covalent Inhibitors of Bruton’s Tyrosine Kinase Targeting an Inactive Conformation. ACS Med. Chem. Lett. 2019, 10, 1467–1472. [Google Scholar] [CrossRef] [PubMed]
- Angst, D.; Gessier, F.; Janser, P.; Vulpetti, A.; Wälchli, R.; Beerli, C.; Littlewood-Evans, A.; Dawson, J.; Nuesslein-Hildesheim, B.; Wieczorek, G.; et al. Discovery of LOU064 (Remibrutinib), a Potent and Highly Selective Covalent Inhibitor of Bruton’s Tyrosine Kinase. J. Med. Chem. 2020, 63, 5102–5118. [Google Scholar] [CrossRef] [PubMed]
- Liang, Q.; Chen, Y.; Yu, K.; Chen, C.; Zhang, S.; Wang, A.; Wang, W.; Wu, H.; Liu, X.; Wang, B.; et al. Discovery of N-(3-(5-((3-acrylamido-4-(morpholine-4-carbonyl)phenyl)amino)-1-methyl-6-oxo-1,6-dihydropyridin-3-yl)-2-methylphenyl)-4-(tert-butyl)benzamide (CHMFL-BTK-01) as a highly selective irreversible Bruton’s tyrosine kinase (BTK) inhibitor. Eur. J. Med. Chem. 2017, 131, 107–125. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Open-label, Multicenter, Extension Study to Evaluate Long-term Safety and Tolerability of LOU064 in Subjects With CSU. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04109313?term=LOU064&draw=2&rank=1 (accessed on 17 December 2020).
- Shatzel, J.J.; Olson, S.R.; Tao, D.L.; McCarty, O.J.T.; Danilov, A.V.; DeLoughery, T.G. Ibrutinib-associated bleeding: Pathogenesis, management and risk reduction strategies. J. Thromb. Haemost. 2017, 15, 835–847. [Google Scholar] [CrossRef] [PubMed]
- Sibaud, V.; Beylot-Barry, M.; Protin, C.; Vigarios, E.; Recher, C.; Ysebaert, L. Dermatological Toxicities of Bruton’s Tyrosine Kinase Inhibitors. Am. J. Clin. Dermatol. 2020, 21, 799–812. [Google Scholar] [CrossRef]
- Brown, J.R.; Moslehi, J.; Ewer, M.S.; O’Brien, S.M.; Ghia, P.; Cymbalista, F.; Shanafelt, T.D.; Fraser, G.; Rule, S.; Coutre, S.E.; et al. Incidence of and risk factors for major haemorrhage in patients treated with ibrutinib: An integrated analysis. Br. J. Haematol. 2019, 184, 558–569. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, A.H.; Farooqui, M.Z.; Tian, X.; Martyr, S.; Cullinane, A.M.; Nghiem, K.; Sun, C.; Valdez, J.; Niemann, C.U.; Herman, S.E.; et al. Incidence and risk factors of bleeding-related adverse events in patients with chronic lymphocytic leukemia treated with ibrutinib. Haematologica 2015, 100, 1571–1578. [Google Scholar] [CrossRef]
- Wang, M.; Rule, S.; Zinzani, P.L.; Goy, A.; Casasnovas, O.; Smith, S.D.; Damaj, G.; Doorduijn, J.; Lamy, T.; Morschhauser, F.; et al. Acalabrutinib in relapsed or refractory mantle cell lymphoma (ACE-LY-004): A single-arm, multicentre, phase 2 trial. Lancet 2018, 391, 659–667. [Google Scholar] [CrossRef]
- Rule, S.A.; Cartron, G.; Fegan, C.; Morschhauser, F.; Han, L.; Mitra, S.; Salles, G.; Dyer, M.J.S. Long-term follow-up of patients with mantle cell lymphoma (MCL) treated with the selective Bruton’s tyrosine kinase inhibitor tirabrutinib (GS/ONO-4059). Leukemia 2020, 34, 1458–1461. [Google Scholar] [CrossRef]
- Walter, H.S.; Jayne, S.; Rule, S.A.; Cartron, G.; Morschhauser, F.; Macip, S.; Karlin, L.; Jones, C.; Herbaux, C.; Quittet, P.; et al. Long-term follow-up of patients with CLL treated with the selective Bruton’s tyrosine kinase inhibitor ONO/GS-4059. Blood 2017, 129, 2808–2810. [Google Scholar] [CrossRef]
- Munakata, W.; Ando, K.; Hatake, K.; Fukuhara, N.; Kinoshita, T.; Fukuhara, S.; Shirasugi, Y.; Yokoyama, M.; Ichikawa, S.; Ohmachi, K.; et al. Phase I study of tirabrutinib (ONO-4059/GS-4059) in patients with relapsed or refractory B-cell malignancies in Japan. Cancer Sci. 2019, 110, 1686–1694. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.R.; Moslehi, J.; O’Brien, S.; Ghia, P.; Hillmen, P.; Cymbalista, F.; Shanafelt, T.D.; Fraser, G.; Rule, S.; Kipps, T.J.; et al. Characterization of atrial fibrillation adverse events reported in ibrutinib randomized controlled registration trials. Haematologica 2017, 102, 1796–1805. [Google Scholar] [CrossRef] [PubMed]
- Pulte, D.; Olson, K.E.; Broekman, M.J.; Islam, N.; Ballard, H.S.; Furman, R.R.; Olson, A.E.; Marcus, A.J. CD39 activity correlates with stage and inhibits platelet reactivity in chronic lymphocytic leukemia. J. Transl. Med. 2007, 5, 23. [Google Scholar] [CrossRef] [PubMed]
- Goerge, T.; Ho-Tin-Noe, B.; Carbo, C.; Benarafa, C.; Remold-O’Donnell, E.; Zhao, B.Q.; Cifuni, S.M.; Wagner, D.D. Inflammation induces hemorrhage in thrombocytopenia. Blood 2008, 111, 4958–4964. [Google Scholar] [CrossRef]
- Jamasbi, J.; Megens, R.T.; Bianchini, M.; Munch, G.; Ungerer, M.; Faussner, A.; Sherman, S.; Walker, A.; Goyal, P.; Jung, S.; et al. Differential Inhibition of Human Atherosclerotic Plaque-Induced Platelet Activation by Dimeric GPVI-Fc and Anti-GPVI Antibodies: Functional and Imaging Studies. J. Am. Coll. Cardiol. 2015, 65, 2404–2415. [Google Scholar] [CrossRef] [PubMed]
- Mato, A.R.; Timlin, C.; Ujjani, C.; Skarbnik, A.; Howlett, C.; Banerjee, R.; Nabhan, C.; Schuster, S.J. Comparable outcomes in chronic lymphocytic leukaemia (CLL) patients treated with reduced-dose ibrutinib: Results from a multi-centre study. Br. J. Haematol. 2018, 181, 259–261. [Google Scholar] [CrossRef]
- Chen, L.S.; Bose, P.; Cruz, N.D.; Jiang, Y.; Wu, Q.; Thompson, P.A.; Feng, S.; Kroll, M.H.; Qiao, W.; Huang, X.; et al. A pilot study of lower doses of ibrutinib in patients with chronic lymphocytic leukemia. Blood 2018, 132, 2249–2259. [Google Scholar] [CrossRef]
- Akhtar, O.S.; Attwood, K.; Lund, I.; Hare, R.; Hernandez-Ilizaliturri, F.J.; Torka, P. Dose reductions in ibrutinib therapy are not associated with inferior outcomes in patients with chronic lymphocytic leukemia (CLL). Leuk. Lymphoma 2019, 60, 1650–1655. [Google Scholar] [CrossRef]
- Parikh, S.A.; Achenbach, S.J.; Call, T.G.; Rabe, K.G.; Ding, W.; Leis, J.F.; Kenderian, S.S.; Chanan-Khan, A.A.; Koehler, A.B.; Schwager, S.M.; et al. The impact of dose modification and temporary interruption of ibrutinib on outcomes of chronic lymphocytic leukemia patients in routine clinical practice. Cancer Med. 2020, 9, 3390–3399. [Google Scholar] [CrossRef]
- Alexander, W.; Davis, S.; Ramakrishna, R.; Manoharan, A. Outcomes of Reduced Frequency Dosing of Ibrutinib in Chronic Lymphocytic Leukemia Patients Following Complete or Partial Remission: A Pilot Study. J. Hematol. 2020, 9, 55–61. [Google Scholar] [CrossRef]
- Florian, P.; Wonerow, P.; Harder, S.; Kuczka, K.; Dubar, M.; Graff, J. Anti-GPVI Fab SAR264565 effectively blocks GPVI function in ex vivo human platelets under arterial shear in a perfusion chamber. Eur. J. Clin. Pharmacol. 2017, 73, 949–956. [Google Scholar] [CrossRef] [PubMed]
- Joseph, R.E.; Amatya, N.; Fulton, D.B.; Engen, J.R.; Wales, T.E.; Andreotti, A. Differential impact of BTK active site inhibitors on the conformational state of full-length BTK. eLife 2020, 9, e60470. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.R.; Harb, W.A.; Hill, B.T.; Gabrilove, J.; Sharman, J.P.; Schreeder, M.T.; Barr, P.M.; Foran, J.M.; Miller, T.P.; Burger, J.A.; et al. Phase I study of single-agent CC-292, a highly selective Bruton’s tyrosine kinase inhibitor, in relapsed/refractory chronic lymphocytic leukemia. Haematologica 2016, 101, e295–e298. [Google Scholar] [CrossRef] [PubMed]

| Generic Name | Brand Name | First Designation | Mode of Inhibition | Disease | Development Stage | Bleeding | Off-Target |
|---|---|---|---|---|---|---|---|
| Irreversible BTKi | |||||||
| Ibrutinib | Imbruvica® | PCI-32765 | Covalent (Cys-481) | CCL MCL WM MZL GVHD | Approved (2013) Approved (2017) | 39% (any grade), 4% ≥ grade 3, 0.4% fatal Bleeding (>20%) | Tec, Src-kinases (Src, Lyn, Fyn, Yes) Itk |
| GVHD | Approved (2017) | Bleeding (>20%) | Itk | ||||
| Acalabrutinib | Calquence® | ACP-160 | Covalent (Cys-481) | MCL CCL | Approved (2017) FDA | 22% * (any grade), 3% ≥ grade 3, 0.1% fatal | Tec |
| Zanubrutinib | Brukinsa® | BGB-3111 | Covalent (Cys-481) | MCL | Approved (2019) FDA | 50% (any grade) 2% ≥ grade 3 | Tec |
| Tirabrutinib | Velexbru® | ONO/GS-4059 | Covalent (Cys-481) | PCNSL LPL WM | Approved (3/2020) Japan | Yes, see text | Tec |
| Branebrutinib | BMS-986195 | Covalent (Cys-481) | SLE, Sjögren syndrome | Phase 1 Phase 2 | No Unknown | Tec | |
| BI 705564 | Covalent (Cys-481) | SLE, RA | Phase 1 | 15% (grade 1,2) | Tec | ||
| Remibrutinib | LOU064 | Highly selective, Covalent (Cys-481) | CSU, Sjögren syndrome | Phase 2 | Not known | no | |
| Irreversible BTKi, brain-penetrant | |||||||
| Evobrutinib | M2951 | Covalent (Cys-481) | MS | Phase 1,2 Phase 3 ** | no | Tec | |
| Tolebrutinib | SAR- 442168, PRN2246 | Covalent (Cys-481) | MS | Preclinical, Phase 1 | no | Tec | |
| Reversible BTKi | |||||||
| BMS-986142 | reversible | RA | Phase 1,2 | no | Tec | ||
| Fenebrutinib | GDC-0853 | reversible | NHL,CLL RA SLE | Phase 1 Phase 2 Phase 2 | no no no | no | |
| Rilzabrutinib | PRN1008 | reversible, transient covalent (Cys-481) | ITP Pemphigus | Phase 2 Phase 2 | no no | Tec |
| BTKi | Dosage | GPVI—Mediated PA *, IC50, µM | FcγRIIa-Mediated PA ** IC50, µM | Plasma Concentration (Cmax) | Increased Bleeding Time In Vitro *** | Ref. | |
|---|---|---|---|---|---|---|---|
| µM | fold **** | ||||||
| Irreversible BTKi | |||||||
| Ibrutinib | 420 mg QD | 0.025 | 0.08 | 0.31 | 1 | 40 | 13, 41, 75 |
| Acalabrutinib | 100 mg BID | 0.372 | 0.38 | 1.78 | 5 | 13 | 13, 41, 78 |
| Zanubrutinib | 160 mg BID | 0.094 | 0.11 | 1.4 | nd | 13, 41, 86 | |
| Tirabrutinib | 480 mg QD | 0.268 | 0.42 | 2.36 | 5 | 18 | 13, 41, 91 |
| Evobrutinib | 75 mg QD 75 mg BID | 1.2 | 1.13 | not known | nd | 13, 41 | |
| Reversible BTKi | |||||||
| Fenebrutinib | 150 mg BID | 0.013 | 0.011 | 0.6 | no | 13, 111 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
von Hundelshausen, P.; Siess, W. Bleeding by Bruton Tyrosine Kinase-Inhibitors: Dependency on Drug Type and Disease. Cancers 2021, 13, 1103. https://doi.org/10.3390/cancers13051103
von Hundelshausen P, Siess W. Bleeding by Bruton Tyrosine Kinase-Inhibitors: Dependency on Drug Type and Disease. Cancers. 2021; 13(5):1103. https://doi.org/10.3390/cancers13051103
Chicago/Turabian Stylevon Hundelshausen, Philipp, and Wolfgang Siess. 2021. "Bleeding by Bruton Tyrosine Kinase-Inhibitors: Dependency on Drug Type and Disease" Cancers 13, no. 5: 1103. https://doi.org/10.3390/cancers13051103
APA Stylevon Hundelshausen, P., & Siess, W. (2021). Bleeding by Bruton Tyrosine Kinase-Inhibitors: Dependency on Drug Type and Disease. Cancers, 13(5), 1103. https://doi.org/10.3390/cancers13051103






