PPM1D Is a Therapeutic Target in Childhood Neural Tumors
Abstract
Simple Summary
Abstract
1. Introduction
2. Results
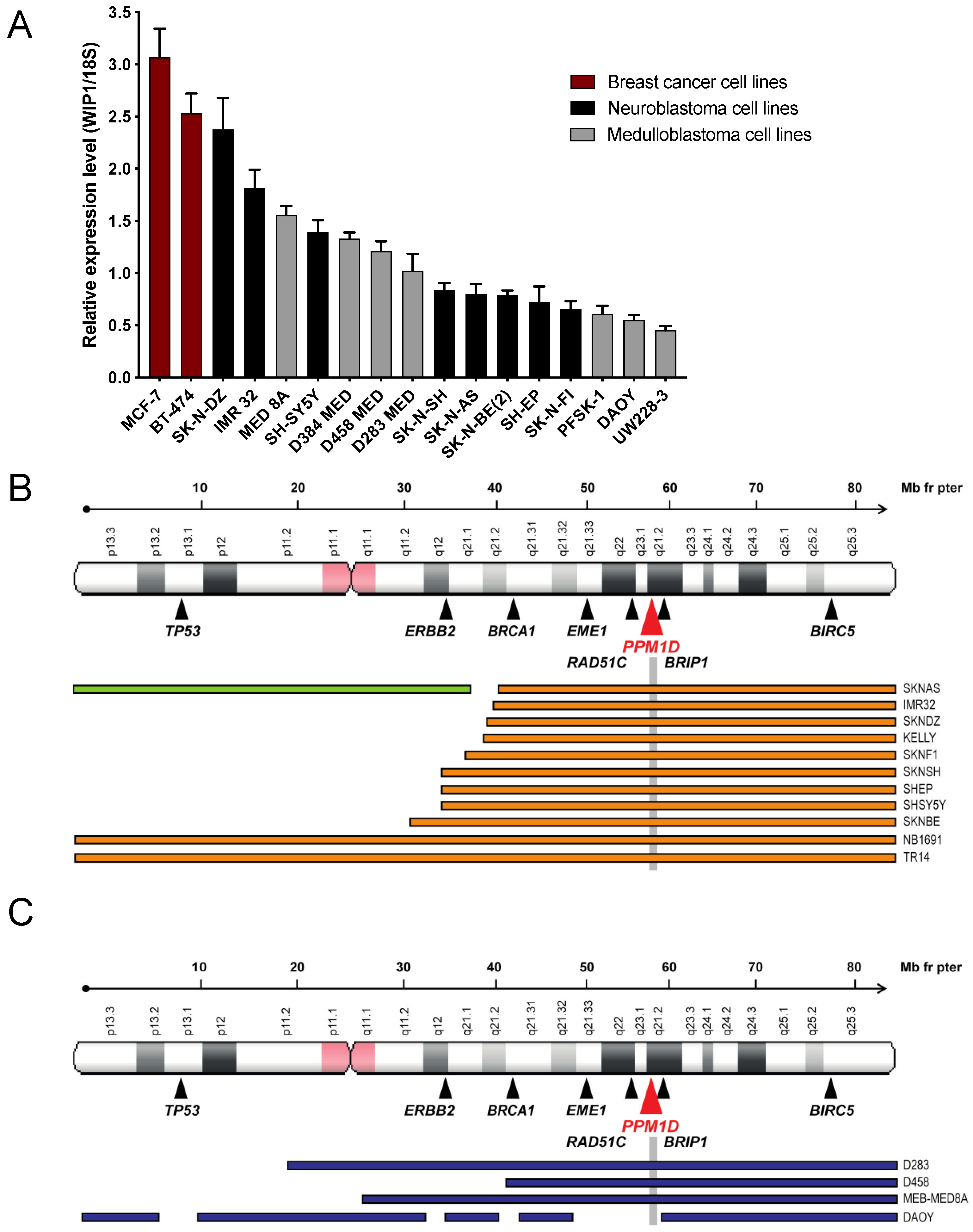
2.1. PPM1D Expression Correlates with Chromosome 17q Gains in Medulloblastoma and Neuroblastoma Cells
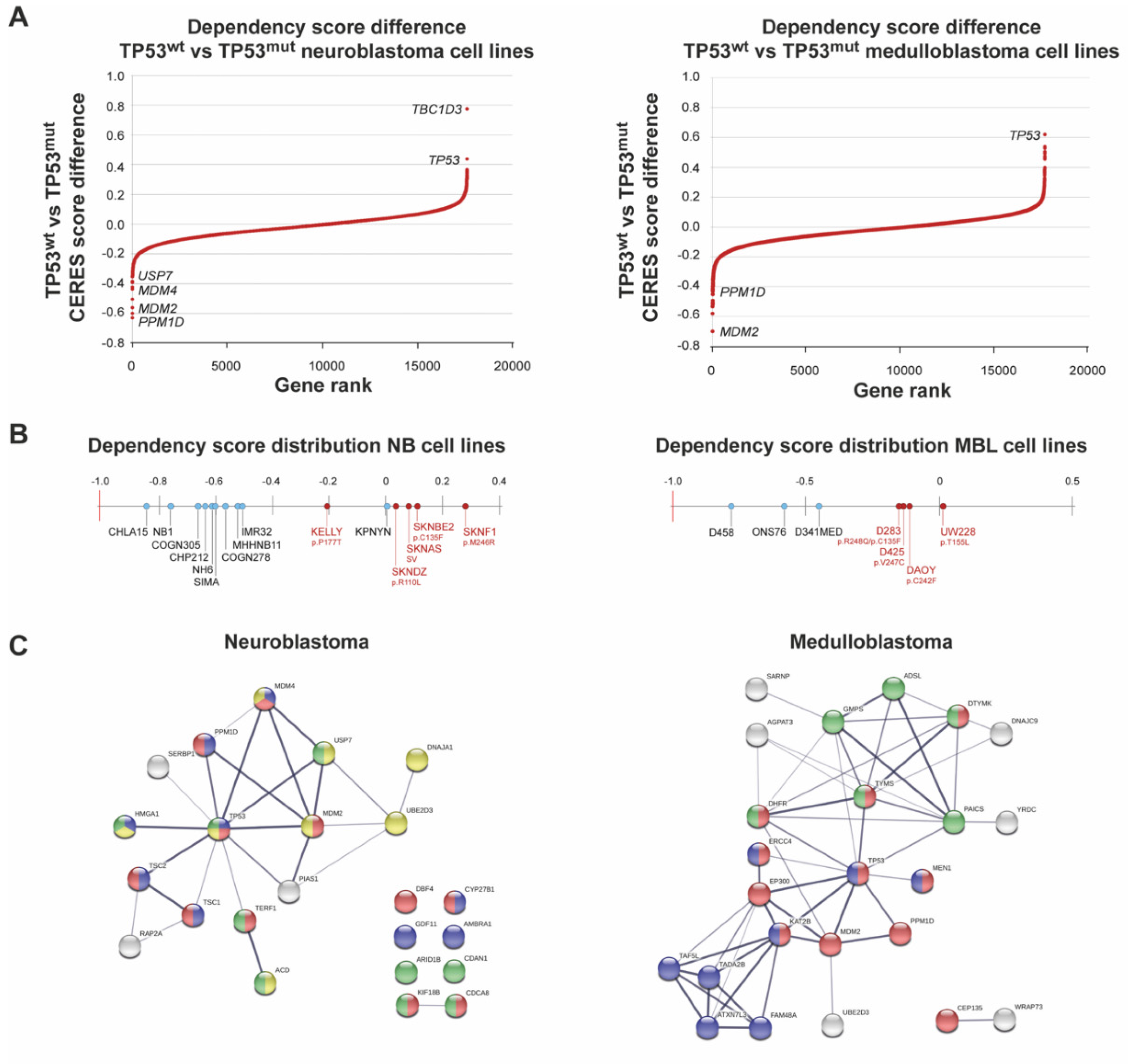
2.2. PPM1D Dependency in Medulloblastoma and Neuroblastoma
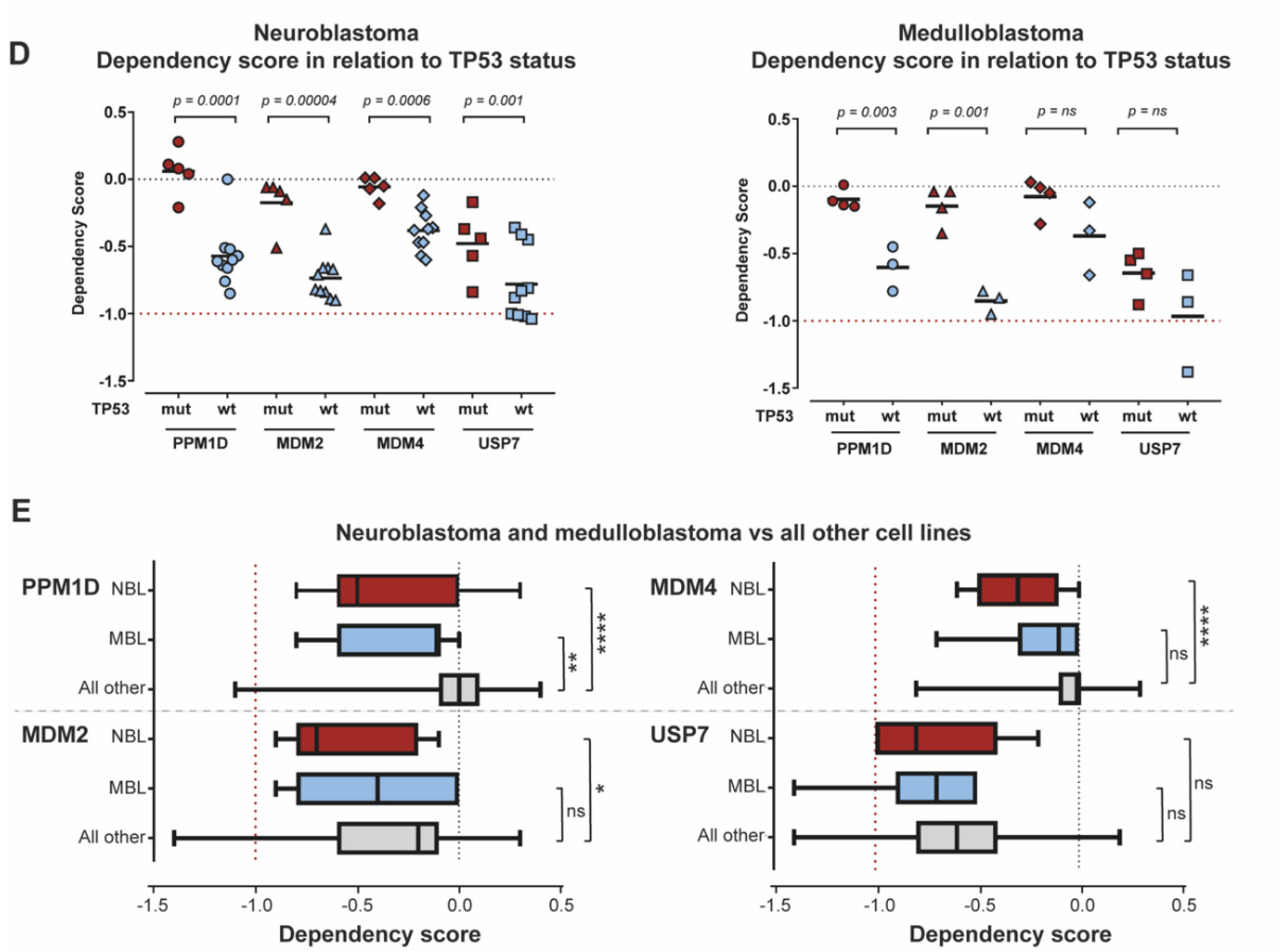
2.3. Downregulation of PPM1D Expression Impairs Growth and Sensitizes Medulloblastoma and Neuroblastoma Cells to Irradiation
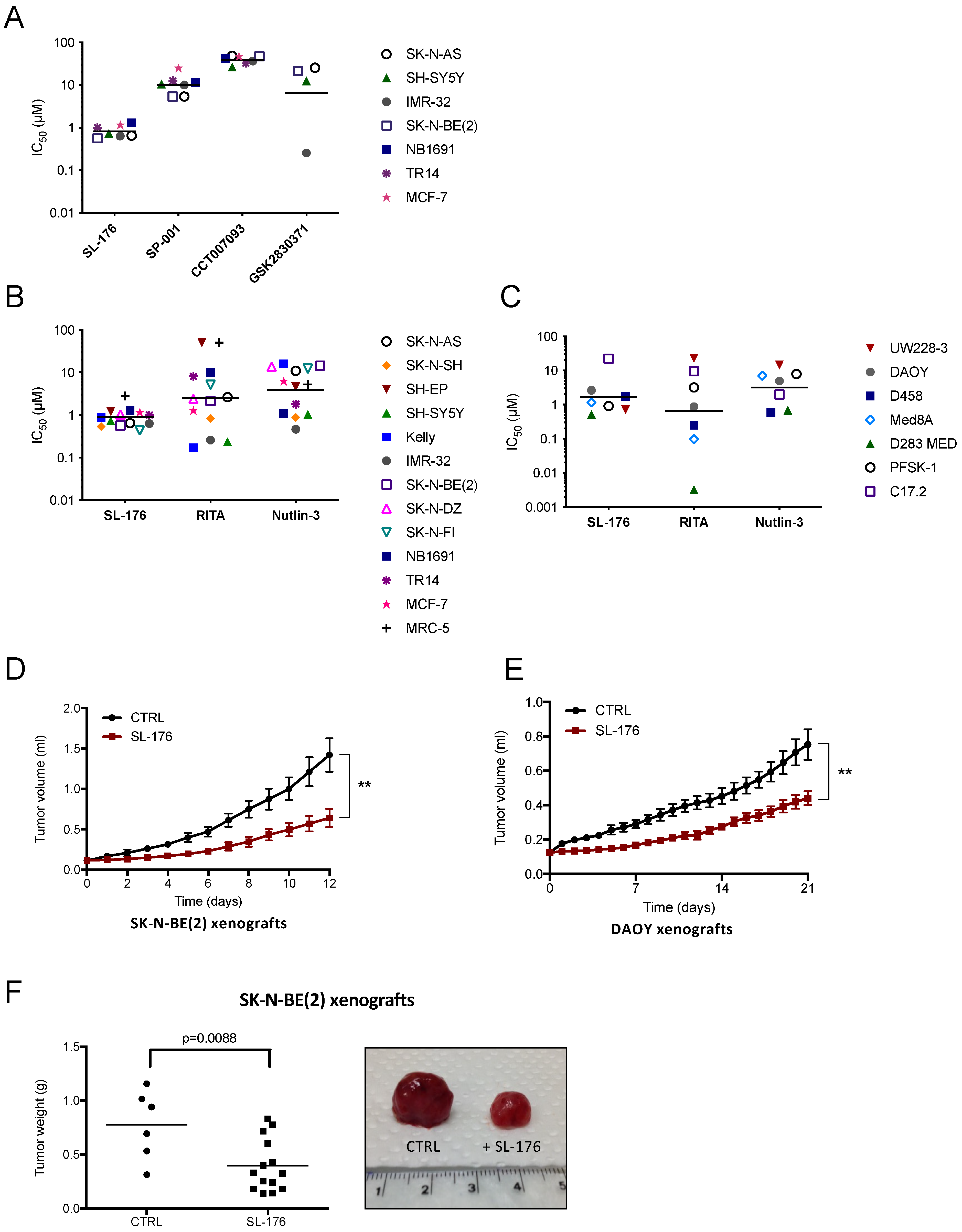
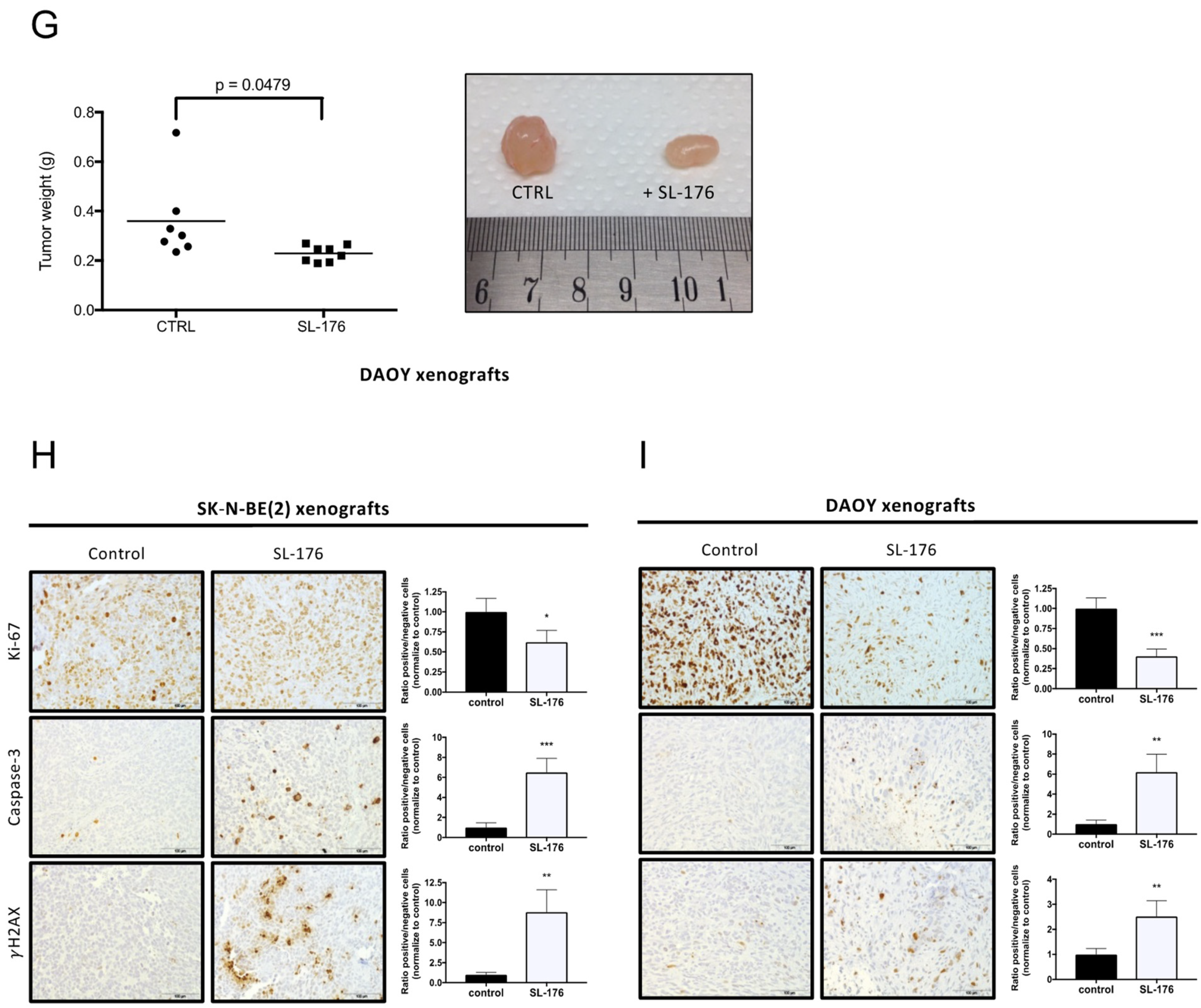
2.4. Pharmacological Targeting of WIP1 Impairs Medulloblastoma and Neuroblastoma Growth
3. Discussion
4. Materials and Methods
4.1. Cell Culture and Reagents
4.2. Short Hairpin RNA (shRNA)
4.3. Viability Assays
4.4. Irradiation of Human Cancer Cell Lines
4.5. Western Blot
4.6. Quantitative Real-Time RT-PCR Analyses
4.7. CRISPR-Cas9 Loss of Function Screening
4.8. Flow Cytometry
4.9. Ethical Permits
4.10. Xenograft Studies
4.11. Immunohistochemistry of Xenograft Tumors
4.12. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Hafner, A.; Bulyk, M.L.; Jambhekar, A.; Lahav, G. The Multiple Mechanisms That Regulate P53 Activity and Cell Fate. Nat. Rev. Mol. Cell Biol. 2019, 20, 199–210. [Google Scholar] [CrossRef]
- Bykov, V.J.N.; Eriksson, S.E.; Bianchi, J.; Wiman, K.G. Targeting Mutant P53 for Efficient Cancer Therapy. Nat. Rev. Cancer 2018, 18, 89–102. [Google Scholar] [CrossRef]
- Martin, B.; Verdebout, J.-M.; Mascaux, C.; Paesmans, M.; Rouas, G.; Verhest, A.; Ninane, V.; Sculier, J.-P. Expression of P53 in Preneoplastic and Early Neoplastic Bronchial Lesions. Oncol. Rep. 2002, 9, 223–229. [Google Scholar] [CrossRef][Green Version]
- Gröbner, S.N.; Worst, B.C.; Weischenfeldt, J.; Buchhalter, I.; Kleinheinz, K.; Rudneva, V.A.; Johann, P.D.; Balasubramanian, G.P.; Segura-Wang, M.; Brabetz, S.; et al. The Landscape of Genomic Alterations across Childhood Cancers. Nature 2018, 555, 321–327. [Google Scholar] [CrossRef]
- Carr-Wilkinson, J.; O’Toole, K.; Wood, K.M.; Challen, C.C.; Baker, A.G.; Board, J.R.; Evans, L.; Cole, M.; Cheung, N.-K.V.; Boos, J.; et al. High Frequency of P53/MDM2/P14ARF Pathway Abnormalities in Relapsed Neuroblastoma. Clin. Cancer Res. 2010, 16, 1108–1118. [Google Scholar] [CrossRef] [PubMed]
- Ramaswamy, V.; Remke, M.; Adamski, J.; Bartels, U.; Tabori, U.; Wang, X.; Huang, A.; Hawkins, C.; Mabbott, D.; Laperriere, N.; et al. Medulloblastoma Subgroup-Specific Outcomes in Irradiated Children: Who Are the True High-Risk Patients? Neuro Oncol. 2016, 18, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Bown, N.; Cotterill, S.; Lastowska, M.; O’Neill, S.; Pearson, A.D.; Plantaz, D.; Meddeb, M.; Danglot, G.; Brinkschmidt, C.; Christiansen, H.; et al. Gain of Chromosome Arm 17q and Adverse Outcome in Patients with Neuroblastoma. N. Engl. J. Med. 1999, 340, 1954–1961. [Google Scholar] [CrossRef] [PubMed]
- Abel, F.; Ejeskär, K.; Kogner, P.; Martinsson, T. Gain of Chromosome Arm 17q Is Associated with Unfavourable Prognosis in Neuroblastoma, but Does Not Involve Mutations in the Somatostatin Receptor 2 (SSTR2) Gene at 17q24. Br. J. Cancer 1999, 81, 1402–1409. [Google Scholar] [CrossRef][Green Version]
- Gilbert, F.; Feder, M.; Balaban, G.; Brangman, D.; Lurie, D.K.; Podolsky, R.; Rinaldt, V.; Vinikoor, N.; Weisband, J. Human Neuroblastomas and Abnormalities of Chromosomes 1 and 17. Cancer Res. 1984, 44, 5444–5449. [Google Scholar]
- Theissen, J.; Oberthuer, A.; Hombach, A.; Volland, R.; Hertwig, F.; Fischer, M.; Spitz, R.; Zapatka, M.; Brors, B.; Ortmann, M.; et al. Chromosome 17/17q Gain and Unaltered Profiles in High Resolution Array-CGH Are Prognostically Informative in Neuroblastoma. Genes Chromosomes Cancer 2014, 53, 639–649. [Google Scholar] [CrossRef]
- Łastowska, M.; Cotterill, S.; Pearson, A.D.J.; Roberts, P.; McGuckin, A.; Lewis, I.; Bown, N. Gain of Chromosome Arm 17q Predicts Unfavourable Outcome in Neuroblastoma Patients. Eur. J. Cancer 1997, 33, 1627–1633. [Google Scholar] [CrossRef]
- Meddeb, M.; Danglot, G.; Chudoba, I.; Vénuat, A.M.; Bénard, J.; Avet-Loiseau, H.; Vasseur, B.; Le Paslier, D.; Terrier-Lacombe, M.J.; Hartmann, O.; et al. Additional Copies of a 25 Mb Chromosomal Region Originating from 17q23.1-17qter Are Present in 90% of High-Grade Neuroblastomas. Genes Chromosomes Cancer 1996, 17, 156–165. [Google Scholar] [CrossRef]
- Plantaz, D.; Mohapatra, G.; Matthay, K.K.; Pellarin, M.; Seeger, R.C.; Feuerstein, B.G. Gain of Chromosome 17 Is the Most Frequent Abnormality Detected in Neuroblastoma by Comparative Genomic Hybridization. Am. J. Pathol 1997, 150, 81–89. [Google Scholar] [PubMed]
- Biegel, J.A.; Rorke, L.B.; Packer, R.J.; Sutton, L.N.; Schut, L.; Bonner, K.; Emanuel, B.S. Isochromosome 17q in Primitive Neuroectodermal Tumors of the Central Nervous System. Genes Chromosomes Cancer 1989, 1, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Bien-Willner, G.A.; Mitra, R.D. Mutation and Expression Analysis in Medulloblastoma Yields Prognostic Variants and a Putative Mechanism of Disease for I17q Tumors. Acta Neuropathol. Commun. 2014, 2, 74. [Google Scholar] [CrossRef] [PubMed]
- Bigner, S.H.; Mark, J.; Friedman, H.S.; Biegel, J.A.; Bigner, D.D. Structural Chromosomal Abnormalities in Human Medulloblastoma. Cancer Genet. Cytogenet. 1988, 30, 91–101. [Google Scholar] [CrossRef]
- Griffin, C.A.; Hawkins, A.L.; Packer, R.J.; Rorke, L.B.; Emanuel, B.S. Chromosome Abnormalities in Pediatric Brain Tumors. Cancer Res. 1988, 48, 175–180. [Google Scholar]
- Nahta, R.; Castellino, R.C. Phosphatase Magnesium-Dependent 1 δ (PPM1D), Serine/Threonine Protein Phosphatase and Novel Pharmacological Target in Cancer. Biochem. Pharmacol. 2021, 184, 114362. [Google Scholar] [CrossRef]
- Fiscella, M.; Zhang, H.; Fan, S.; Sakaguchi, K.; Shen, S.; Mercer, W.E.; Woude, G.F.V.; O’Connor, P.M.; Appella, E. Wip1, a Novel Human Protein Phosphatase That Is Induced in Response to Ionizing Radiation in a P53-Dependent Manner. Proc. Natl. Acad. Sci. USA 1997, 94, 6048–6053. [Google Scholar] [CrossRef] [PubMed]
- Kamada, R.; Kudoh, F.; Ito, S.; Tani, I.; Janairo, J.I.B.; Omichinski, J.G.; Sakaguchi, K. Metal-Dependent Ser/Thr Protein Phosphatase PPM Family: Evolution, Structures, Diseases and Inhibitors. Pharmacol. Ther. 2020, 215, 107622. [Google Scholar] [CrossRef]
- Fujimoto, H.; Onishi, N.; Kato, N.; Takekawa, M.; Xu, X.Z.; Kosugi, A.; Kondo, T.; Imamura, M.; Oishi, I.; Yoda, A.; et al. Regulation of the Antioncogenic Chk2 Kinase by the Oncogenic Wip1 Phosphatase. Cell Death Differ. 2006, 13, 1170–1180. [Google Scholar] [CrossRef]
- Lu, X.; Nannenga, B.; Donehower, L.A. PPM1D Dephosphorylates Chk1 and P53 and Abrogates Cell Cycle Checkpoints. Genes Dev. 2005, 19, 1162–1174. [Google Scholar] [CrossRef]
- Lu, X.; Nguyen, T.-A.; Donehower, L.A. Reversal of the ATM/ATR-Mediated DNA Damage Response by the Oncogenic Phosphatase PPM1D. Cell Cycle 2005, 4, 1060–1064. [Google Scholar] [CrossRef]
- Oliva-Trastoy, M.; Berthonaud, V.; Chevalier, A.; Ducrot, C.; Marsolier-Kergoat, M.-C.; Mann, C.; Leteurtre, F. The Wip1 Phosphatase (PPM1D) Antagonizes Activation of the Chk2 Tumour Suppressor Kinase. Oncogene 2007, 26, 1449–1458. [Google Scholar] [CrossRef]
- Shreeram, S.; Hee, W.K.; Demidov, O.N.; Kek, C.; Yamaguchi, H.; Fornace, A.J.; Anderson, C.W.; Appella, E.; Bulavin, D.V. Regulation of ATM/P53-Dependent Suppression of Myc-Induced Lymphomas by Wip1 Phosphatase. J. Exp. Med. 2006, 203, 2793–2799. [Google Scholar] [CrossRef] [PubMed]
- Yoda, H.; Inoue, T.; Shinozaki, Y.; Lin, J.; Watanabe, T.; Koshikawa, N.; Takatori, A.; Nagase, H. Direct Targeting of MYCN Gene Amplification by Site-Specific DNA Alkylation in Neuroblastoma. Cancer Res. 2019, 79, 830–840. [Google Scholar] [CrossRef] [PubMed]
- Castellino, R.C.; De Bortoli, M.; Lu, X.; Moon, S.-H.; Nguyen, T.-A.; Shepard, M.A.; Rao, P.H.; Donehower, L.A.; Kim, J.Y.H. Medulloblastomas Overexpress the P53-Inactivating Oncogene WIP1/PPM1D. J. Neurooncol. 2008, 86, 245–256. [Google Scholar] [CrossRef]
- Fuku, T.; Semba, S.; Yutori, H.; Yokozaki, H. Increased Wild-Type P53-Induced Phosphatase 1 (Wip1 or PPM1D) Expression Correlated with Downregulation of Checkpoint Kinase 2 in Human Gastric Carcinoma. Pathol. Int. 2007, 57, 566–571. [Google Scholar] [CrossRef]
- Hirasawa, A.; Saito-Ohara, F.; Inoue, J.; Aoki, D.; Susumu, N.; Yokoyama, T.; Nozawa, S.; Inazawa, J.; Imoto, I. Association of 17q21-Q24 Gain in Ovarian Clear Cell Adenocarcinomas with Poor Prognosis and Identification of PPM1D and APPBP2 as Likely Amplification Targets. Clin. Cancer Res. 2003, 9, 1995–2004. [Google Scholar] [PubMed]
- Lambros, M.B.; Natrajan, R.; Geyer, F.C.; Lopez-Garcia, M.A.; Dedes, K.J.; Savage, K.; Lacroix-Triki, M.; Jones, R.L.; Lord, C.J.; Linardopoulos, S.; et al. PPM1D Gene Amplification and Overexpression in Breast Cancer: A QRT-PCR and Chromogenic in Situ Hybridization Study. Mod. Pathol. 2010, 23, 1334–1345. [Google Scholar] [CrossRef]
- Nikbakht, H.; Panditharatna, E.; Mikael, L.G.; Li, R.; Gayden, T.; Osmond, M.; Ho, C.-Y.; Kambhampati, M.; Hwang, E.I.; Faury, D.; et al. Spatial and Temporal Homogeneity of Driver Mutations in Diffuse Intrinsic Pontine Glioma. Nat. Commun. 2016, 7, 11185. [Google Scholar] [CrossRef]
- Ruark, E.; Snape, K.; Humburg, P.; Loveday, C.; Bajrami, I.; Brough, R.; Rodrigues, D.N.; Renwick, A.; Seal, S.; Ramsay, E.; et al. Mosaic PPM1D Mutations Are Associated with Predisposition to Breast and Ovarian Cancer. Nature 2013, 493, 406–410. [Google Scholar] [CrossRef]
- Saito-Ohara, F.; Imoto, I.; Inoue, J.; Hosoi, H.; Nakagawara, A.; Sugimoto, T.; Inazawa, J. PPM1D Is a Potential Target for 17q Gain in Neuroblastoma. Cancer Res. 2003, 63, 1876–1883. [Google Scholar] [PubMed]
- Tan, D.S.P.; Lambros, M.B.K.; Rayter, S.; Natrajan, R.; Vatcheva, R.; Gao, Q.; Marchiò, C.; Geyer, F.C.; Savage, K.; Parry, S.; et al. PPM1D Is a Potential Therapeutic Target in Ovarian Clear Cell Carcinomas. Clin. Cancer Res. 2009, 15, 2269–2280. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Lu, C.; Wang, J.; McLellan, M.D.; Johnson, K.J.; Wendl, M.C.; McMichael, J.F.; Schmidt, H.K.; Yellapantula, V.; Miller, C.A.; et al. Age-Related Mutations Associated with Clonal Hematopoietic Expansion and Malignancies. Nat. Med. 2014, 20, 1472–1478. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Chen, L.H.; Wan, H.; Yang, R.; Wang, Z.; Feng, J.; Yang, S.; Jones, S.; Wang, S.; Zhou, W.; et al. Exome Sequencing Identifies Somatic Gain-of-Function PPM1D Mutations in Brainstem Gliomas. Nat. Genet. 2014, 46, 726–730. [Google Scholar] [CrossRef]
- Bulavin, D.V.; Phillips, C.; Nannenga, B.; Timofeev, O.; Donehower, L.A.; Anderson, C.W.; Appella, E.; Fornace, A.J. Inactivation of the Wip1 Phosphatase Inhibits Mammary Tumorigenesis through P38 MAPK–Mediated Activation of the P16Ink4a-P19Arf Pathway. Nat. Genet. 2004, 36, 343–350. [Google Scholar] [CrossRef]
- Doucette, T.A.; Yang, Y.; Pedone, C.; Kim, J.Y.H.; Dubuc, A.; Northcott, P.D.; Taylor, M.D.; Fults, D.W.; Rao, G. WIP1 Enhances Tumor Formation in a Sonic Hedgehog–Dependent Model of Medulloblastoma. Neurosurgery 2012, 70, 1003–1010. [Google Scholar] [CrossRef]
- Demidov, O.N.; Timofeev, O.; Lwin, H.N.Y.; Kek, C.; Appella, E.; Bulavin, D.V. Wip1 Phosphatase Regulates P53-Dependent Apoptosis of Stem Cells and Tumorigenesis in the Mouse Intestine. Cell Stem Cell 2007, 1, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wan, G.; Mlotshwa, S.; Vance, V.; Berger, F.G.; Chen, H.; Lu, X. Oncogenic Wip1 Phosphatase Is Inhibited by MiR-16 in the DNA Damage Signaling Pathway. Cancer Res. 2010, 70, 7176–7186. [Google Scholar] [CrossRef]
- Kryh, H.; Caren, H.; Erichsen, J.; Sjoberg, R.-M.; Abrahamsson, J.; Kogner, P.; Martinsson, T. Comprehensive SNP Array Study of Frequently Used Neuroblastoma Cell Lines; Copy Neutral Loss of Heterozygosity Is Common in the Cell Lines but Uncommon in Primary Tumors. BMC Genom. 2011, 12, 443. [Google Scholar] [CrossRef] [PubMed]
- Schleiermacher, G.; Raynal, V.; Janoueix-Lerosey, I.; Combaret, V.; Aurias, A.; Delattre, O. Variety and Complexity of Chromosome 17 Translocations in Neuroblastoma. Genes Chromosomes Cancer 2004, 39, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, A.J.; Meyers, R.M.; Weir, B.A.; Vazquez, F.; Zhang, C.-Z.; Ben-David, U.; Cook, A.; Ha, G.; Harrington, W.F.; Doshi, M.B.; et al. Genomic Copy Number Dictates a Gene-Independent Cell Response to CRISPR-Cas9 Targeting. Cancer Discov. 2016, 6, 914–929. [Google Scholar] [CrossRef]
- Carén, H.; Kryh, H.; Nethander, M.; Sjöberg, R.-M.; Träger, C.; Nilsson, S.; Abrahamsson, J.; Kogner, P.; Martinsson, T. High-Risk Neuroblastoma Tumors with 11q-Deletion Display a Poor Prognostic, Chromosome Instability Phenotype with Later Onset. Proc. Natl. Acad. Sci. USA 2010, 107, 4323–4328. [Google Scholar] [CrossRef]
- Northcott, P.A.; Robinson, G.W.; Kratz, C.P.; Mabbott, D.J.; Pomeroy, S.L.; Clifford, S.C.; Rutkowski, S.; Ellison, D.W.; Malkin, D.; Taylor, M.D.; et al. Medulloblastoma. Nat. Rev. Dis Primers 2019, 5, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Gilmartin, A.G.; Faitg, T.H.; Richter, M.; Groy, A.; Seefeld, M.A.; Darcy, M.G.; Peng, X.; Federowicz, K.; Yang, J.; Zhang, S.-Y.; et al. Allosteric Wip1 Phosphatase Inhibition through Flap-Subdomain Interaction. Nat. Chem. Biol. 2014, 10, 181–187. [Google Scholar] [CrossRef]
- Kozakai, Y.; Kamada, R.; Kiyota, Y.; Yoshimura, F.; Tanino, K.; Sakaguchi, K. Inhibition of C-Terminal Truncated PPM1D Enhances the Effect of Doxorubicin on Cell Viability in Human Colorectal Carcinoma Cell Line. Bioorg. Med. Chem. Lett. 2014, 24, 5593–5596. [Google Scholar] [CrossRef]
- Ogasawara, S.; Kiyota, Y.; Chuman, Y.; Kowata, A.; Yoshimura, F.; Tanino, K.; Kamada, R.; Sakaguchi, K. Novel Inhibitors Targeting PPM1D Phosphatase Potently Suppress Cancer Cell Proliferation. Bioorg. Med. Chem. 2015, 23, 6246–6249. [Google Scholar] [CrossRef]
- Rayter, S.; Elliott, R.; Travers, J.; Rowlands, M.G.; Richardson, T.B.; Boxall, K.; Jones, K.; Linardopoulos, S.; Workman, P.; Aherne, W.; et al. A Chemical Inhibitor of PPM1D That Selectively Kills Cells Overexpressing PPM1D. Oncogene 2008, 27, 1036–1044. [Google Scholar] [CrossRef]
- Yagi, H.; Chuman, Y.; Kozakai, Y.; Imagawa, T.; Takahashi, Y.; Yoshimura, F.; Tanino, K.; Sakaguchi, K. A Small Molecule Inhibitor of P53-Inducible Protein Phosphatase PPM1D. Bioorg. Med. Chem. Lett. 2012, 22, 729–732. [Google Scholar] [CrossRef] [PubMed]
- Northcott, P.A.; Lee, C.; Zichner, T.; Stütz, A.M.; Erkek, S.; Kawauchi, D.; Shih, D.J.; Hovestadt, V.; Zapatka, M.; Sturm, D.; et al. Enhancer Hijacking Activates GFI1 Family Oncogenes in Medulloblastoma. Nature 2014, 511, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Bouska, A.; McKeithan, T.W.; Deffenbacher, K.E.; Lachel, C.; Wright, G.W.; Iqbal, J.; Smith, L.M.; Zhang, W.; Kucuk, C.; Rinaldi, A.; et al. Genome-Wide Copy-Number Analyses Reveal Genomic Abnormalities Involved in Transformation of Follicular Lymphoma. Blood 2014, 123, 1681–1690. [Google Scholar] [CrossRef] [PubMed]
- Carless, M.A.; Griffiths, L.R. Cytogenetics of Melanoma and Nonmelanoma Skin Cancer. Adv. Exp. Med. Biol. 2014, 810, 160–181. [Google Scholar] [CrossRef]
- Herou, E.; Biloglav, A.; Johansson, B.; Paulsson, K. Partial 17q Gain Resulting from Isochromosomes, Unbalanced Translocations and Complex Rearrangements Is Associated with Gene Overexpression, Older Age and Shorter Overall Survival in High Hyperdiploid Childhood Acute Lymphoblastic Leukemia. Leukemia 2013, 27, 493–496. [Google Scholar] [CrossRef]
- Malouf, G.G.; Monzon, F.A.; Couturier, J.; Molinié, V.; Escudier, B.; Camparo, P.; Su, X.; Yao, H.; Tamboli, P.; Lopez-Terrada, D.; et al. Genomic Heterogeneity of Translocation Renal Cell Carcinoma. Clin. Cancer Res. 2013, 19, 4673–4684. [Google Scholar] [CrossRef]
- Sunpaweravong, P.; Thu, K.L.; Lam, W.L.; Mai, S. Assessment of the Clinical Relevance of 17q25.3 Copy Number and Three-Dimensional Telomere Organization in Non-Small Lung Cancer Patients. J. Cancer Res. Clin. Oncol. 2016, 142, 749–756. [Google Scholar] [CrossRef]
- Xiang, D.-B.; Wei, B.; Abraham, S.C.; Huo, L.; Albarracin, C.T.; Zhang, H.; Babiera, G.; Caudle, A.S.; Akay, C.L.; Rao, P.; et al. Molecular Cytogenetic Characterization of Mammary Neuroendocrine Carcinoma. Hum. Pathol. 2014, 45, 1951–1956. [Google Scholar] [CrossRef]
- Cardoso, M.; Paulo, P.; Maia, S.; Teixeira, M.R. Truncating and Missense PPM1D Mutations in Early-Onset and/or Familial/Hereditary Prostate Cancer Patients. Genes Chromosomes Cancer 2016, 55, 954–961. [Google Scholar] [CrossRef]
- Kahn, J.D.; Miller, P.G.; Silver, A.J.; Sellar, R.S.; Bhatt, S.; Gibson, C.; McConkey, M.; Adams, D.; Mar, B.; Mertins, P.; et al. PPM1D-Truncating Mutations Confer Resistance to Chemotherapy and Sensitivity to PPM1D Inhibition in Hematopoietic Cells. Blood 2018, 132, 1095–1105. [Google Scholar] [CrossRef]
- Richter, M.; Dayaram, T.; Gilmartin, A.G.; Ganji, G.; Pemmasani, S.K.; Van Der Key, H.; Shohet, J.M.; Donehower, L.A.; Kumar, R. WIP1 Phosphatase as a Potential Therapeutic Target in Neuroblastoma. PLoS ONE 2015, 10, e0115635. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Lee, J.; Malhotra, A.; Nahta, R.; Arnold, A.R.; Buss, M.C.; Brown, B.D.; Maier, C.; Kenney, A.M.; Remke, M.; et al. WIP1 Modulates Responsiveness to Sonic Hedgehog Signaling in Neuronal Precursor Cells and Medulloblastoma. Oncogene 2016, 35, 5552–5564. [Google Scholar] [CrossRef] [PubMed]
- Shiloh, Y. ATM and Related Protein Kinases: Safeguarding Genome Integrity. Nat. Rev. Cancer 2003, 3, 155–168. [Google Scholar] [CrossRef]
- Uyanik, B.; Grigorash, B.B.; Goloudina, A.R.; Demidov, O.N. DNA Damage-Induced Phosphatase Wip1 in Regulation of Hematopoiesis, Immune System and Inflammation. Cell Death Discov. 2017, 3, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Yoda, A.; Xu, X.Z.; Onishi, N.; Toyoshima, K.; Fujimoto, H.; Kato, N.; Oishi, I.; Kondo, T.; Minami, Y. Intrinsic Kinase Activity and SQ/TQ Domain of Chk2 Kinase as Well as N-Terminal Domain of Wip1 Phosphatase Are Required for Regulation of Chk2 by Wip1. J. Biol. Chem. 2006, 281, 24847–24862. [Google Scholar] [CrossRef] [PubMed]
- Adesina, A.M.; Nalbantoglu, J.; Cavenee, W.K. P53 Gene Mutation and Mdm2 Gene Amplification Are Uncommon in Medulloblastoma. Cancer Res. 1994, 54, 5649–5651. [Google Scholar]
- Brodeur, G.M. Neuroblastoma: Biological Insights into a Clinical Enigma. Nat. Rev. Cancer 2003, 3, 203–216. [Google Scholar] [CrossRef]
- Matthay, K.K.; Maris, J.M.; Schleiermacher, G.; Nakagawara, A.; Mackall, C.L.; Diller, L.; Weiss, W.A. Neuroblastoma. Nat. Rev. Dis. Primers 2016, 2, 16078. [Google Scholar] [CrossRef] [PubMed]
- Saylors, R.L.; Sidransky, D.; Friedman, H.S.; Bigner, S.H.; Bigner, D.D.; Vogelstein, B.; Brodeur, G.M. Infrequent P53 Gene Mutations in Medulloblastomas. Cancer Res. 1991, 51, 4721–4723. [Google Scholar]
- Chesler, L.; Goldenberg, D.D.; Collins, R.; Grimmer, M.; Kim, G.E.; Tihan, T.; Nguyen, K.; Yakovenko, S.; Matthay, K.K.; Weiss, W.A. Chemotherapy-Induced Apoptosis in a Transgenic Model of Neuroblastoma Proceeds Through P53 Induction. Neoplasia 2008, 10, 1268–1274. [Google Scholar] [CrossRef] [PubMed]
- Weiss, W.A.; Aldape, K.; Mohapatra, G.; Feuerstein, B.G.; Bishop, J.M. Targeted Expression of MYCN Causes Neuroblastoma in Transgenic Mice. EMBO J. 1997, 16, 2985–2995. [Google Scholar] [CrossRef] [PubMed]
- Wetmore, C.; Eberhart, D.E.; Curran, T. Loss of P53 but Not ARF Accelerates Medulloblastoma in Mice Heterozygous for Patched. Cancer Res. 2001, 61, 513–516. [Google Scholar]
- Issaeva, N.; Bozko, P.; Enge, M.; Protopopova, M.; Verhoef, L.G.G.C.; Masucci, M.; Pramanik, A.; Selivanova, G. Small Molecule RITA Binds to P53, Blocks P53–HDM-2 Interaction and Activates P53 Function in Tumors. Nat. Med. 2004, 10, 1321–1328. [Google Scholar] [CrossRef] [PubMed]
- Khoo, K.H.; Verma, C.S.; Lane, D.P. Drugging the P53 Pathway: Understanding the Route to Clinical Efficacy. Nat. Rev. Drug Discov. 2014, 13, 217–236. [Google Scholar] [CrossRef]
- Esfandiari, A.; Hawthorne, T.A.; Nakjang, S.; Lunec, J. Chemical Inhibition of Wild-Type P53-Induced Phosphatase 1 (WIP1/PPM1D) by GSK2830371 Potentiates the Sensitivity to MDM2 Inhibitors in a P53-Dependent Manner. Mol. Cancer 2016, 15, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Kamada, R.; Kimura, N.; Yoshimura, F.; Tanino, K.; Sakaguchi, K. Inhibition of Lipid Droplet Formation by Ser/Thr Protein Phosphatase PPM1D Inhibitor, SL-176. PLoS ONE 2019, 14, e0212682. [Google Scholar] [CrossRef]
- Burmakin, M.; Shi, Y.; Hedström, E.; Kogner, P.; Selivanova, G. Dual Targeting of Wild-Type and Mutant P53 by Small Molecule RITA Results in the Inhibition of N-Myc and Key Survival Oncogenes and Kills Neuroblastoma Cells In Vivo and In Vitro. Clin. Cancer Res. 2013, 19, 5092–5103. [Google Scholar] [CrossRef]
- Oghabi Bakhshaiesh, T.; Majidzadeh, A.K.; Esmaeili, R. Wip1: A Candidate Phosphatase for Cancer Diagnosis and Treatment. DNA Repair 2017, 54, 63–66. [Google Scholar] [CrossRef]
- Dudgeon, C.; Shreeram, S.; Tanoue, K.; Mazur, S.J.; Sayadi, A.; Robinson, R.C.; Appella, E.; Bulavin, D.V. Genetic Variants and Mutations of PPM1D Control the Response to DNA Damage. Cell Cycle 2013, 12, 2656–2664. [Google Scholar] [CrossRef] [PubMed]
- Kleiblova, P.; Shaltiel, I.A.; Benada, J.; Ševčík, J.; Pecháčková, S.; Pohlreich, P.; Voest, E.E.; Dundr, P.; Bartek, J.; Kleibl, Z.; et al. Gain-of-Function Mutations of PPM1D/Wip1 Impair the P53-Dependent G1 Checkpoint. J. Cell Biol. 2013, 201, 511–521. [Google Scholar] [CrossRef]
- Milosevic, J.; Fransson, S.; Gulyas, M.; Olsen, T.K.; Gallo-Oller, G.; Treis, D.; Elfman, L.H.M.; Wilhelm, M.; Martinsson, T.; Baryawno, N.; et al. High Expression of PPM1D Induces Tumors Phenotypically Similar to TP53 Loss-of-Function Mutations in Mice. Cancers 2021, 13, 5493. [Google Scholar] [CrossRef] [PubMed]
- Buss, M.C.; Remke, M.; Lee, J.; Gandhi, K.; Schniederjan, M.J.; Kool, M.; Northcott, P.A.; Pfister, S.M.; Taylor, M.D.; Castellino, R.C. The WIP1 Oncogene Promotes Progression and Invasion of Aggressive Medulloblastoma Variants. Oncogene 2015, 34, 1126–1140. [Google Scholar] [CrossRef] [PubMed]
- Meyers, R.M.; Bryan, J.G.; McFarland, J.M.; Weir, B.A.; Sizemore, A.E.; Xu, H.; Dharia, N.V.; Montgomery, P.G.; Cowley, G.S.; Pantel, S.; et al. Computational Correction of Copy Number Effect Improves Specificity of CRISPR–Cas9 Essentiality Screens in Cancer Cells. Nat. Genet. 2017, 49, 1779–1784. [Google Scholar] [CrossRef] [PubMed]
- Szklarczyk, D.; Morris, J.H.; Cook, H.; Kuhn, M.; Wyder, S.; Simonovic, M.; Santos, A.; Doncheva, N.T.; Roth, A.; Bork, P.; et al. The STRING Database in 2017: Quality-Controlled Protein–Protein Association Networks, Made Broadly Accessible. Nucleic Acids Res. 2017, 45, D362–D368. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Milosevic, J.; Treis, D.; Fransson, S.; Gallo-Oller, G.; Sveinbjörnsson, B.; Eissler, N.; Tanino, K.; Sakaguchi, K.; Martinsson, T.; Wickström, M.; et al. PPM1D Is a Therapeutic Target in Childhood Neural Tumors. Cancers 2021, 13, 6042. https://doi.org/10.3390/cancers13236042
Milosevic J, Treis D, Fransson S, Gallo-Oller G, Sveinbjörnsson B, Eissler N, Tanino K, Sakaguchi K, Martinsson T, Wickström M, et al. PPM1D Is a Therapeutic Target in Childhood Neural Tumors. Cancers. 2021; 13(23):6042. https://doi.org/10.3390/cancers13236042
Chicago/Turabian StyleMilosevic, Jelena, Diana Treis, Susanne Fransson, Gabriel Gallo-Oller, Baldur Sveinbjörnsson, Nina Eissler, Keiji Tanino, Kazuyasu Sakaguchi, Tommy Martinsson, Malin Wickström, and et al. 2021. "PPM1D Is a Therapeutic Target in Childhood Neural Tumors" Cancers 13, no. 23: 6042. https://doi.org/10.3390/cancers13236042
APA StyleMilosevic, J., Treis, D., Fransson, S., Gallo-Oller, G., Sveinbjörnsson, B., Eissler, N., Tanino, K., Sakaguchi, K., Martinsson, T., Wickström, M., Kogner, P., & Johnsen, J. I. (2021). PPM1D Is a Therapeutic Target in Childhood Neural Tumors. Cancers, 13(23), 6042. https://doi.org/10.3390/cancers13236042





