A Systematic Review of the Safety, Feasibility and Benefits of Exercise for Patients with Advanced Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
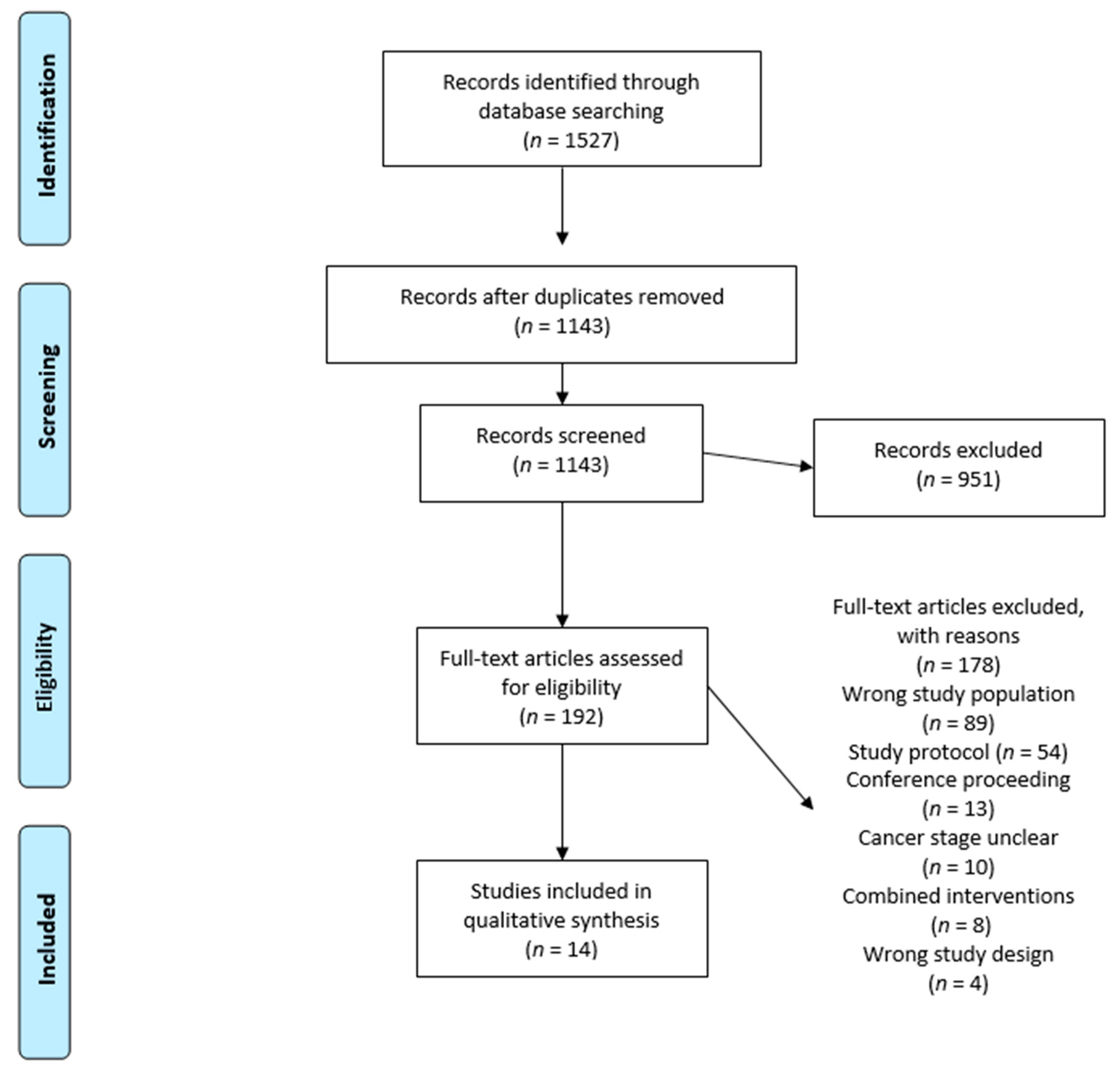
2. Materials and Methods
2.1. Information Sources and Searches
2.2. Study Selection
2.3. Outcome Assessment
2.4. Data Extraction and Quality Assessment
2.5. Data Syntheses and Statistical Analyses
3. Results
3.1. Characteristics of Included Trials and Participants
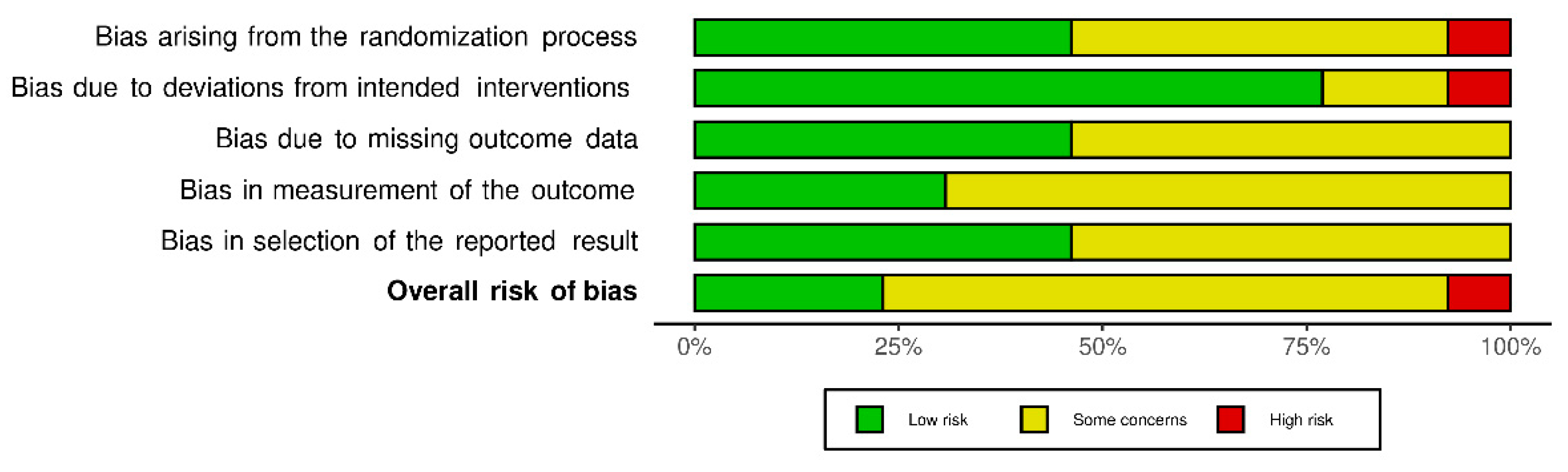
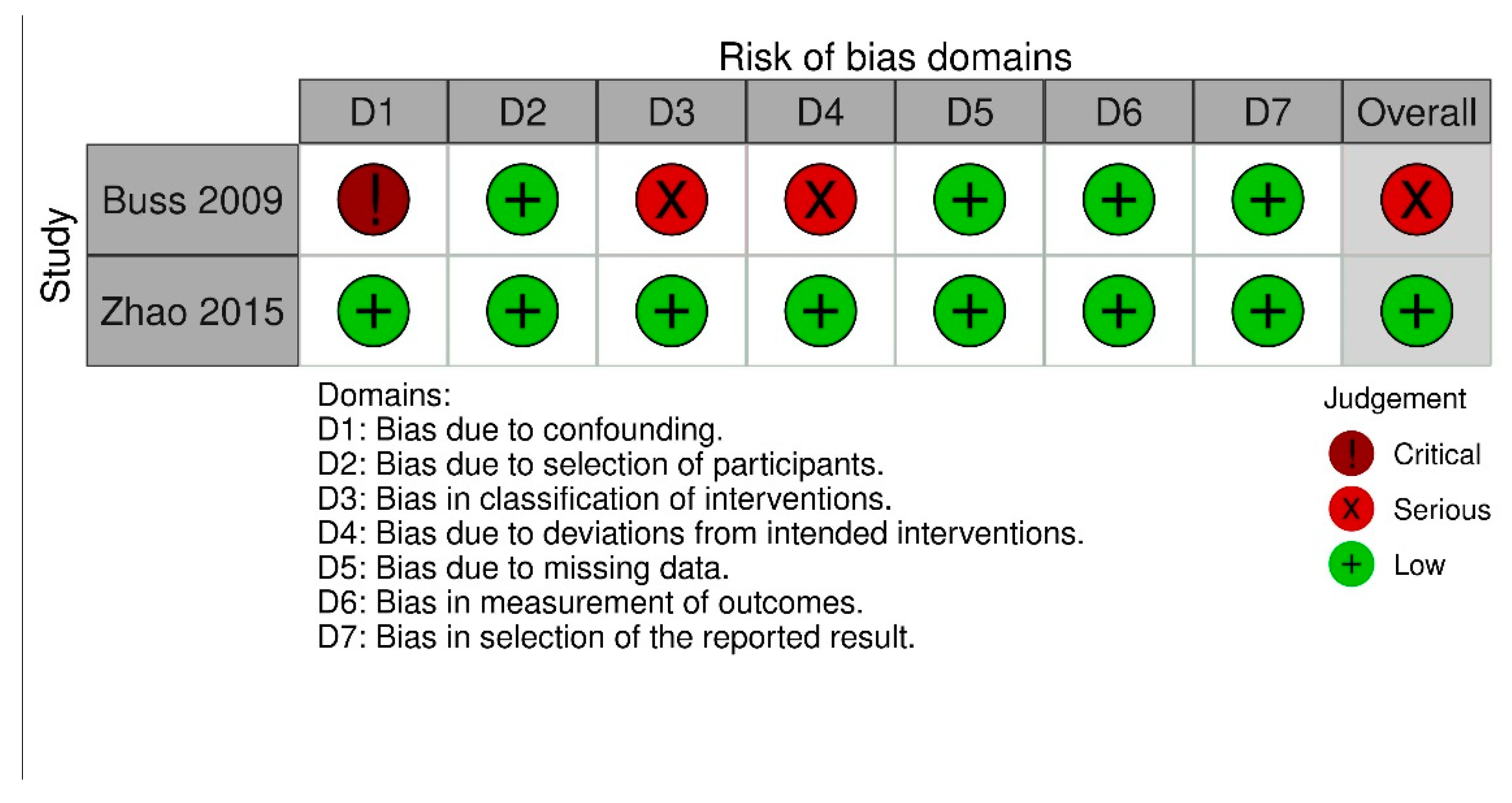
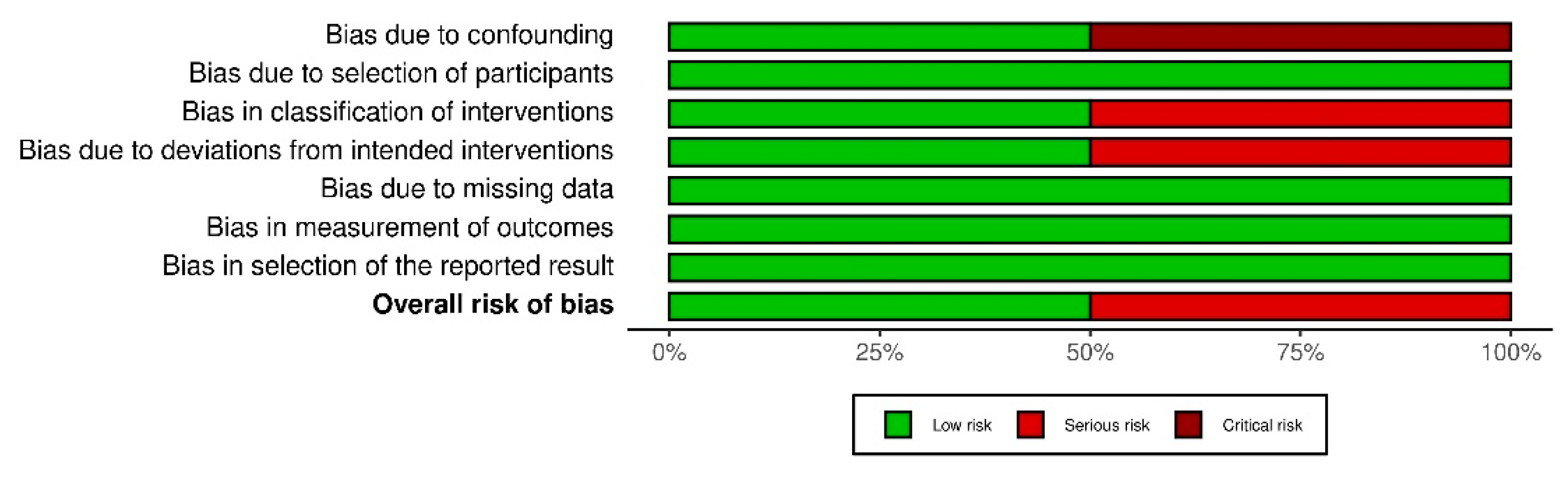
3.2. Quality Assessment
3.3. Intervention Description
3.4. Primary Outcome: Feasibility and Safety
3.5. Secondary Outcomes
3.5.1. Quality of Life
3.5.2. Fatigue
3.5.3. Physical Function
3.5.4. Regular Physical Activity Levels
3.5.5. Body Composition
3.5.6. Sleep
3.6. Effect According to Intervention
3.6.1. Combined Aerobic and Strength Exercise
3.6.2. Single Aerobic Exercise
3.6.3. Single Strength Exercise
3.6.4. Home-Based Exercise
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Data and Statistics on Cancer in Europe. Available online: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/cancer/data-and-statistics (accessed on 28 January 2021).
- Pinto, B.M.; Trunzo, J.J. Health behaviors during and after a cancer diagnosis. Cancer 2005, 104, 2614–2623. [Google Scholar] [CrossRef]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl, W.F. Early palliative care for patients with metastatic non–small-cell lung cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Basch, E.; Deal, A.M.; Dueck, A.C.; Scher, H.I.; Kris, M.G.; Hudis, C.; Schrag, D. Overall Survival Results of a Trial Assessing Patient-Reported Outcomes for Symptom Monitoring During Routine Cancer Treatment. JAMA 2017, 318, 197–198. [Google Scholar] [CrossRef] [Green Version]
- Potter, J.; Hami, F.; Bryan, T.; Quigley, C. Symptoms in 400 patients referred to palliative care services: Prevalence and patterns. Palliat. Med. 2003, 17, 310–314. [Google Scholar] [CrossRef]
- Tewes, M.; Baumann, F.; Teufel, M.; Ostgathe, C. Symptoms During Outpatient Cancer Treatment and Options for Their Management. Dtsch. Arztebl. Int. 2021, 118. [Google Scholar] [CrossRef]
- Al Maqbali, M.; Al Sinani, M.; Al Naamani, Z.; Al Badi, K. Prevalence of Fatigue in Patients with Cancer: A Systematic Review and Meta-Analysis. J. Pain Symptom Manag. 2020, 61, 167–189. [Google Scholar] [CrossRef] [PubMed]
- Van Lancker, A.; Velghe, A.; Van Hecke, A.; Verbrugghe, M.; Van Den Noortgate, N.; Grypdonck, M.; Verhaeghe, S.; Bekkering, G.; Beeckman, D. Prevalence of symptoms in older cancer patients receiving palliative care: A systematic review and meta-analysis. J. Pain Symptom Manag. 2014, 47, 90–104. [Google Scholar] [CrossRef]
- Rha, S.Y.; Lee, J. Symptom clusters during palliative chemotherapy and their influence on functioning and quality of life. Support. Care Cancer 2017, 25, 1519–1527. [Google Scholar] [CrossRef] [PubMed]
- Christensen, J.F.; Simonsen, C.; Hojman, P. Exercise training in cancer control and treatment. Compr. Physiol. 2011, 9, 165–205. [Google Scholar]
- Patel, A.V.; Friedenreich, C.M.; Moore, S.C.; Hayes, S.C.; Silver, J.K.; Campbell, K.L.; Winters-Stone, K.; Gerber, L.H.; George, S.M.; Fulton, J.E. American College of Sports Medicine roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med. Sci. Sports Exerc. 2019, 51, 2391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mustian, K.M.; Alfano, C.M.; Heckler, C.; Kleckner, A.S.; Kleckner, I.R.; Leach, C.R.; Mohr, D.; Palesh, O.G.; Peppone, L.J.; Piper, B.F. Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: A meta-analysis. JAMA Oncol. 2017, 3, 961–968. [Google Scholar] [CrossRef] [PubMed]
- Courneya, K.S.; McKenzie, D.C.; Mackey, J.R.; Gelmon, K.; Friedenreich, C.M.; Yasui, Y.; Reid, R.D.; Cook, D.; Jespersen, D.; Proulx, C. Effects of exercise dose and type during breast cancer chemotherapy: Multicenter randomized trial. J. Natl. Cancer Inst. 2013, 105, 1821–1832. [Google Scholar] [CrossRef] [Green Version]
- Brown, J.C.; Damjanov, N.; Courneya, K.S.; Troxel, A.B.; Zemel, B.S.; Rickels, M.R.; Ky, B.; Rhim, A.D.; Rustgi, A.K.; Schmitz, K.H. A randomized dose-response trial of aerobic exercise and health-related quality of life in colon cancer survivors. Psychooncology 2018, 27, 1221–1228. [Google Scholar] [CrossRef]
- Nakano, J.; Hashizume, K.; Fukushima, T.; Ueno, K.; Matsuura, E.; Ikio, Y.; Ishii, S.; Morishita, S.; Tanaka, K.; Kusuba, Y. Effects of Aerobic and Resistance Exercises on Physical Symptoms in Cancer Patients: A Meta-analysis. Integr. Cancer Ther. 2018, 17, 1048–1058. [Google Scholar] [CrossRef]
- van Waart, H.; Stuiver, M.M.; van Harten, W.H.; Geleijn, E.; Kieffer, J.M.; Buffart, L.M.; de Maaker-Berkhof, M.; Boven, E.; Schrama, J.; Geenen, M.M.; et al. Effect of Low-Intensity Physical Activity and Moderate- to High-Intensity Physical Exercise During Adjuvant Chemotherapy on Physical Fitness, Fatigue, and Chemotherapy Completion Rates: Results of the PACES Randomized Clinical Trial. J. Clin. Oncol. 2015, 33, 1918–1927. [Google Scholar] [CrossRef] [Green Version]
- Tian, L.; Lu, H.J.; Lin, L.; Hu, Y. Effects of aerobic exercise on cancer-related fatigue: A meta-analysis of randomized controlled trials. Support. Care Cancer 2016, 24, 969–983. [Google Scholar] [CrossRef]
- Scott, J.M.; Zabor, E.C.; Schwitzer, E.; Koelwyn, G.J.; Adams, S.C.; Nilsen, T.S.; Moskowitz, C.S.; Matsoukas, K.; Iyengar, N.M.; Dang, C.T.; et al. Efficacy of Exercise Therapy on Cardiorespiratory Fitness in Patients With Cancer: A Systematic Review and Meta-Analysis. J. Clin. Oncol. 2018, 36, 2297–2305. [Google Scholar] [CrossRef] [PubMed]
- Strasser, B.; Steindorf, K.; Wiskemann, J.; Ulrich, C.M. Impact of resistance training in cancer survivors: A meta-analysis. Med. Sci. Sports Exerc. 2013, 45, 2080–2090. [Google Scholar] [CrossRef]
- Winters-Stone, K.; Dobek, J.; Nail, L.; Bennett, J.; Leo, M.; Torgrimson-Ojerio, B.; Luoh, S.-W.; Schwartz, A. Impact+ resistance training improves bone health and body composition in prematurely menopausal breast cancer survivors: A randomized controlled trial. Osteoporos. Int. 2013, 24, 1637–1646. [Google Scholar] [CrossRef] [PubMed]
- Courneya, K.S.; Segal, R.J.; Mackey, J.R.; Gelmon, K.; Reid, R.D.; Friedenreich, C.M.; Ladha, A.B.; Proulx, C.; Vallance, J.K.; Lane, K.; et al. Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: A multicenter randomized controlled trial. J. Clin. Oncol. 2007, 25, 4396–4404. [Google Scholar] [CrossRef]
- Zhu, G.; Zhang, X.; Wang, Y.; Xiong, H.; Zhao, Y.; Sun, F. Effects of exercise intervention in breast cancer survivors: A meta-analysis of 33 randomized controlled trails. Onco Targets Ther. 2016, 9, 2153–2168. [Google Scholar] [CrossRef] [Green Version]
- Mustian, K.M.; Griggs, J.J.; Morrow, G.R.; McTiernan, A.; Roscoe, J.A.; Bole, C.W.; Atkins, J.N.; Issell, B.F. Exercise and side effects among 749 patients during and after treatment for cancer: A University of Rochester Cancer Center Community Clinical Oncology Program Study. Support. Care Cancer 2006, 14, 732–741. [Google Scholar] [CrossRef]
- Andersen, C.; Adamsen, L.; Moeller, T.; Midtgaard, J.; Quist, M.; Tveteraas, A.; Rorth, M. The effect of a multidimensional exercise programme on symptoms and side-effects in cancer patients undergoing chemotherapy—the use of semi-structured diaries. Eur. J. Oncol. Nurs. 2006, 10, 247–262. [Google Scholar] [CrossRef]
- Piraux, E.; Caty, G.; Aboubakar Nana, F.; Reychler, G. Effects of exercise therapy in cancer patients undergoing radiotherapy treatment: A narrative review. SAGE Open Med. 2020, 8, 2050312120922657. [Google Scholar] [CrossRef] [PubMed]
- Schumann, M.; Freitag, N.; Bloch, W. Advanced Exercise Prescription for Cancer Patients and its Application in Germany. J. Sci. Sport Exerc. 2020, 2, 201–214. [Google Scholar] [CrossRef]
- Heywood, R.; McCarthy, A.L.; Skinner, T.L. Efficacy of exercise interventions in patients with advanced cancer: A systematic review. Arch. Phys. Med. Rehabil. 2018, 99, 2595–2620. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- Cheville, A.L.; Kollasch, J.; Vandenberg, J.; Shen, T.; Grothey, A.; Gamble, G.; Basford, J.R. A home-based exercise program to improve function, fatigue, and sleep quality in patients with Stage IV lung and colorectal cancer: A randomized controlled trial. J. Pain Symptom Manag. 2013, 45, 811–821. [Google Scholar] [CrossRef] [PubMed]
- Oldervoll, L.M.; Loge, J.H.; Lydersen, S.; Paltiel, H.; Asp, M.B.; Nygaard, U.V.; Oredalen, E.; Frantzen, T.L.; Lesteberg, I.; Amundsen, L.; et al. Physical exercise for cancer patients with advanced disease: A randomized controlled trial. Oncologist 2011, 16, 1649–1657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rief, H.; Omlor, G.; Akbar, M.; Welzel, T.; Bruckner, T.; Rieken, S.; Haefner, M.F.; Schlampp, I.; Gioules, A.; Habermehl, D. Feasibility of isometric spinal muscle training in patients with bone metastases under radiation therapy-first results of a randomized pilot trial. BMC Cancer 2014, 14, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Henke, C.C.; Cabri, J.; Fricke, L.; Pankow, W.; Kandilakis, G.; Feyer, P.C.; de Wit, M. Strength and endurance training in the treatment of lung cancer patients in stages IIIA/IIIB/IV. Support. Care Cancer 2014, 22, 95–101. [Google Scholar] [CrossRef]
- Cormie, P.; Newton, R.U.; Spry, N.; Joseph, D.; Taaffe, D.R.; Galvao, D.A. Safety and efficacy of resistance exercise in prostate cancer patients with bone metastases. Prostate Cancer Prostatic Dis. 2013, 16, 328–335. [Google Scholar] [CrossRef] [Green Version]
- Poort, H.; Peters, M.; van der Graaf, W.T.A.; Nieuwkerk, P.T.; van de Wouw, A.J.; Nijhuis-van der Sanden, M.W.G.; Bleijenberg, G.; Verhagen, C.; Knoop, H. Cognitive behavioral therapy or graded exercise therapy compared with usual care for severe fatigue in patients with advanced cancer during treatment: A randomized controlled trial. Ann. Oncol. 2020, 31, 115–122. [Google Scholar] [CrossRef]
- Zhou, W.; Wan, Y.H.; Chen, Q.; Qiu, Y.R.; Luo, X.M. Effects of Tai Chi Exercise on Cancer-Related Fatigue in Patients with Nasopharyngeal Carcinoma Undergoing Chemoradiotherapy: A Randomized Controlled Trial. J. Pain Symptom Manag. 2018, 55, 737–744. [Google Scholar] [CrossRef] [Green Version]
- Galvao, D.A.; Taaffe, D.R.; Spry, N.; Cormie, P.; Joseph, D.; Chambers, S.K.; Chee, R.; Peddle-McIntyre, C.J.; Hart, N.H.; Baumann, F.T.; et al. Exercise Preserves Physical Function in Prostate Cancer Patients with Bone Metastases. Med. Sci. Sports Exerc. 2018, 50, 393–399. [Google Scholar] [CrossRef] [Green Version]
- Zimmer, P.; Trebing, S.; Timmers-Trebing, U.; Schenk, A.; Paust, R.; Bloch, W.; Rudolph, R.; Streckmann, F.; Baumann, F.T. Eight-week, multimodal exercise counteracts a progress of chemotherapy-induced peripheral neuropathy and improves balance and strength in metastasized colorectal cancer patients: A randomized controlled trial. Support. Care Cancer 2018, 26, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Tsianakas, V.; Harris, J.; Ream, E.; Van Hemelrijck, M.; Purushotham, A.; Mucci, L.; Green, J.S.; Fewster, J.; Armes, J. CanWalk: A feasibility study with embedded randomised controlled trial pilot of a walking intervention for people with recurrent or metastatic cancer. BMJ Open 2017, 7, e013719. [Google Scholar] [CrossRef] [Green Version]
- Pyszora, A.; Budzynski, J.; Wojcik, A.; Prokop, A.; Krajnik, M. Physiotherapy programme reduces fatigue in patients with advanced cancer receiving palliative care: Randomized controlled trial. Support. Care Cancer 2017, 25, 2899–2908. [Google Scholar] [CrossRef] [PubMed]
- Maddocks, M.; Halliday, V.; Chauhan, A.; Taylor, V.; Nelson, A.; Sampson, C.; Byrne, A.; Griffiths, G.; Wilcock, A. Neuromuscular electrical stimulation of the quadriceps in patients with non-small cell lung cancer receiving palliative chemotherapy: A randomized phase II study. PLoS ONE 2013, 8, e86059. [Google Scholar] [CrossRef]
- Rief, H.; Akbar, M.; Keller, M.; Omlor, G.; Welzel, T.; Bruckner, T.; Rieken, S.; Häfner, M.F.; Schlampp, I.; Gioules, A. Quality of life and fatigue of patients with spinal bone metastases under combined treatment with resistance training and radiation therapy-a randomized pilot trial. Radiat. Oncol. 2014, 9, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Buss, T.; de Walden-Galuszko, K.; Modlinska, A.; Osowicka, M.; Lichodziejewska-Niemierko, M.; Janiszewska, J. Kinesitherapy alleviates fatigue in terminal hospice cancer patients-an experimental, controlled study. Support. Care Cancer 2010, 18, 743–749. [Google Scholar] [CrossRef]
- Zhao, S.G.; Alexander, N.B.; Djuric, Z.; Zhou, J.; Tao, Y.; Schipper, M.; Feng, F.Y.; Eisbruch, A.; Worden, F.P.; Strath, S.J.; et al. Maintaining physical activity during head and neck cancer treatment: Results of a pilot controlled trial. Head Neck 2016, 38 (Suppl. 1), E1086–E1096. [Google Scholar] [CrossRef] [Green Version]
- Gauß, F.G.; Beller, R.; Boos, J.; Däggelmann, J.; Stalf, H.; Wiskemann, J.; Götte, M. Adverse events during supervised exercise interventions in Pediatric Oncology-a nationwide survey. Front. Pediatrics 2021, 9, 568. [Google Scholar] [CrossRef]
- Clauss, D.; Quirmbach, F.; Wiskemann, J.; Rosenberger, F. Adverse Events beim Training mit onkologischen Patienten: Wie sicher ist das Training außerhalb klinischer Studien? B G Beweg. Gesundh. 2019, 35, 194–201. [Google Scholar] [CrossRef]
- National Cancer Institute, N.C. Common Terminology Criteria for Adverse Events (CTCAE). Available online: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_5x7.pdf (accessed on 10 June 2021).
- Steins Bisschop, C.N.; Courneya, K.S.; Velthuis, M.J.; Monninkhof, E.M.; Jones, L.W.; Friedenreich, C.; van der Wall, E.; Peeters, P.H.; May, A.M. Control group design, contamination and drop-out in exercise oncology trials: A systematic review. PLoS ONE 2015, 10, e0120996. [Google Scholar] [CrossRef] [Green Version]
- Bullard, T.; Ji, M.; An, R.; Trinh, L.; Mackenzie, M.; Mullen, S.P. A systematic review and meta-analysis of adherence to physical activity interventions among three chronic conditions: Cancer, cardiovascular disease, and diabetes. BMC Public Health 2019, 19, 636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hui, D.; Glitza, I.; Chisholm, G.; Yennu, S.; Bruera, E. Attrition rates, reasons, and predictive factors in supportive care and palliative oncology clinical trials. Cancer 2013, 119, 1098–1105. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Hayes, S.C.; Spence, R.R.; Steele, M.L.; Millet, G.Y.; Gergele, L. Exercise and colorectal cancer: A systematic review and meta-analysis of exercise safety, feasibility and effectiveness. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 122. [Google Scholar] [CrossRef]
- Singh, B.; Spence, R.; Steele, M.L.; Hayes, S.; Toohey, K. Exercise for Individuals with Lung Cancer: A Systematic Review and Meta-Analysis of Adverse Events, Feasibility, and Effectiveness. Semin. Oncol. Nurs. 2020, 36, 151076. [Google Scholar] [CrossRef] [PubMed]
- Fassier, P.; Zelek, L.; Partula, V.; Srour, B.; Bachmann, P.; Touillaud, M.; Druesne-Pecollo, N.; Galan, P.; Cohen, P.; Hoarau, H.; et al. Variations of physical activity and sedentary behavior between before and after cancer diagnosis: Results from the prospective population-based NutriNet-Sante cohort. Medicine 2016, 95, e4629. [Google Scholar] [CrossRef]
- Mikkelsen, M.K.; Nielsen, D.L.; Vinther, A.; Lund, C.M.; Jarden, M. Attitudes towards physical activity and exercise in older patients with advanced cancer during oncological treatment—A qualitative interview study. Eur. J. Oncol. Nurs. 2019, 41, 16–23. [Google Scholar] [CrossRef] [Green Version]
- Elshahat, S.; Treanor, C.; Donnelly, M. Factors influencing physical activity participation among people living with or beyond cancer: A systematic scoping review. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 50. [Google Scholar] [CrossRef]
- Frikkel, J.; Gotte, M.; Beckmann, M.; Kasper, S.; Hense, J.; Teufel, M.; Schuler, M.; Tewes, M. Fatigue, barriers to physical activity and predictors for motivation to exercise in advanced Cancer patients. BMC Palliat. Care 2020, 19, 43. [Google Scholar] [CrossRef] [PubMed]
- Kartolo, A.; Cheng, S.; Petrella, T. Motivation and preferences of exercise programmes in patients with inoperable metastatic lung cancer: A need assessment. Support. Care Cancer 2016, 24, 129–137. [Google Scholar] [CrossRef]
- Adamsen, L.; Stage, M.; Laursen, J.; Rorth, M.; Quist, M. Exercise and relaxation intervention for patients with advanced lung cancer: A qualitative feasibility study. Scand. J. Med. Sci. Sports 2012, 22, 804–815. [Google Scholar] [CrossRef] [PubMed]
- Charalambous, A.; Kouta, C. Cancer Related Fatigue and Quality of Life in Patients with Advanced Prostate Cancer Undergoing Chemotherapy. Biomed. Res. Int. 2016, 2016, 3989286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kummer, F.; Catuogno, S.; Perseus, J.M.; Bloch, W.; Baumann, F.T. Relationship between cancer-related fatigue and physical activity in inpatient cancer rehabilitation. Anticancer. Res. 2013, 33, 3415–3422. [Google Scholar]
- Bower, J.E. Cancer-related fatigue--mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 2014, 11, 597–609. [Google Scholar] [CrossRef]
- Barsevick, A.; Frost, M.; Zwinderman, A.; Hall, P.; Halyard, M.; Consortium, G. I’m so tired: Biological and genetic mechanisms of cancer-related fatigue. Qual. Life Res. 2010, 19, 1419–1427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hardee, J.P.; Counts, B.R.; Carson, J.A. Understanding the Role of Exercise in Cancer Cachexia Therapy. Am. J. Lifestyle Med. 2019, 13, 46–60. [Google Scholar] [CrossRef]
- Radbruch, L.; Strasser, F.; Elsner, F.; Gonçalves, J.F.; Løge, J.; Kaasa, S.; Nauck, F.; Stone, P.; the Research Steering Committee of the European Association for Palliative Care (EAPC). Fatigue in palliative care patients—An EAPC approach. Palliat. Med. 2008, 22, 13–32. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-A.; Chung, S.H.; Lee, Y. Factors influencing the quality of life of patients with advanced cancer. Appl. Nurs. Res. 2017, 33, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Shallwani, S.M.; Simmonds, M.J.; Kasymjanova, G.; Spahija, J. Quality of life, symptom status and physical performance in patients with advanced non-small cell lung cancer undergoing chemotherapy: An exploratory analysis of secondary data. Lung Cancer 2016, 99, 69–75. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, A.M.; Chafranskaia, A.; Lopez, C.J.; Maganti, M.; Bernstein, L.J.; Chang, E.; Langelier, D.M.; Obadia, M.; Edwards, B.; Oh, P.; et al. CaRE @ Home: Pilot Study of an Online Multidimensional Cancer Rehabilitation and Exercise Program for Cancer Survivors. J. Clin. Med. 2020, 9, 92. [Google Scholar] [CrossRef]
- Bland, K.A.; Bigaran, A.; Campbell, K.L.; Trevaskis, M.; Zopf, E.M. Exercising in isolation? The role of telehealth in exercise oncology during the COVID-19 pandemic and beyond. Phys. Ther. 2020, 100, 1713–1716. [Google Scholar] [CrossRef] [PubMed]
- Morrison, K.S.; Paterson, C.; Toohey, K. The feasibility of exercise interventions delivered via telehealth for people affected by cancer: A rapid review of the literature. Semin. Oncol. Nurs. 2020, 36, 151092. [Google Scholar] [CrossRef]

| Author | Cancer Entities | Age | Treat | n (EX/C) | Description of Intervention | Exercise Modalities | Control | Recruit-ment (Participants/Eligible) | Drop-Out Rate: | Adherence | AE | EX vs. UC ↑ = Improvement ↓ = Worsening | EX vs. UC (Non Sign.) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cheville et al., 2013 [31] | Lung and colorectal cancer; Stage IV (n = 32 colon cancer; n = 34 lung cancer) | Ex: 63.8 ± 12.5; C: 65.5 ± 8.9 | CTx RTx MAB | 66 (33/33) | 8-wk homebased REX and walking exercise | 4x/wk: incremental Walking: 20 min, briskly, ~3.5 mets, REX: upper/lower body split, 5 exercise; 10–15 reps | Usual care | 66/93: (70.9%) | EX: 7/33 (21%) C: 3/33 (9.9%), in total 10/66 (15.1%) | 20/26 (76.9%) pts reached requirement for participation | 0 | ↑ AM-PAC mobility (p = 0.02) ↑Fatigue (FACT-F) (p = 0.03) ↑ Sleep (NRS) (p = 0.05) |  Ambulatory Post Acute Ambulatory Post AcuteCare Daily Activities Short Form (AM-PAC CAT)  QoL (FACT-G) QoL (FACT-G) |
| Cormie et al., 2013 ∞ [35] | Prostate cancer; secondary bone metastases (n = 20) | Ex: 73.1 ± 7.5; C: 71.2 ± 6.9 | Prev. AST RTx SX | 20 (10/10) | 12-wk suplow-level AEX and REX targeting major muscle groups | 2x/wk; REX on machines; 8–12 reps, 2–4 sets, ~60 min, Low-level aerobix exercise and stretching | Usual care | 20/27: (74%) | EX: 2/10 (20%) C: 3/10 (30%) in total 5/20 (25%) | 83% attendance (mean: 20.2 ± 7.6 out of 24 sessions); 70% pts completing 24/24 sessions | 0 | ↑ Physical function (p = 0.016) ↑ 400-m Walk (p = 0.010) ↑ 6 MWT; usual pace (p = 0.001) ↑ Body lean mass (p = 0.026) ↑ Lean mass (p = 0.003) |  Fatigue Fatigue QoL QoL |
| Galvao et al., 2018 [38] | Prostate cancer; bone metastases (n = 57) | Ex: 69.7 ± 7.6; C: 70.4 ± 9.3 | AST CTx | 57 (28/29) | 12-wk sup, combined AEX, REX, and flexibility exercise | 3x/wk: REX: progressively; 10–12 reps; 3 sets AEX: 20–30 min; Cycling/treadmill; 60–85% of max. HR, Flexibility EX: static stretching; 2–4 reps, each muscle group 30–60 s | Usual care | 57/103: (55.3%) | EX: 5/28 (17.8) C: 3/29 (10.3%) in total 8/57 (14%) | Session: 32 ± 10/36; 89% attendance | 0 | ↑ physical function (NBS) (p = 0.028) ↑ leg extension (p = 0.033) |  6 MWT 6 MWT 400 m walk test 400 m walk test  Up and Go Test Up and Go Test  SOT SOT  Lean mass Lean mass  Body fat mass. Body fat mass.  Fatigue (FACT-F) Fatigue (FACT-F) |
| Henke et al., 2013 [34] | Lung cancer Stage IIIA/IIIB/IV (n = 46) | n.a. * | CTx | 46 (25/21) | 3 chemotherapy cycles long: Sup Combined REX and AEX | 7x/wk REX: resistance bands; 50% of max. capacity. 10 reps, 3 sets 5x/wk: AEX: 6 min walking moderate intensity (55–70% of HRmax) | Conventional physiotherapy | 46/70: (65.7%) | EX: 6/24 (25%) C: 9/20 (45%) in total 15/44 (34%), n = 2 dropouts before randomization | n.a. * | n.a. * | ↑ 6 MWT (p < 0.05) ↑ Staircase walking (p = 0.05) ↑ Physical functioning (C-30/LC-13, p = 0.025) ↑ Cognitive functioning (C-30/LC-13, p = 0.050 |  Global health status/QoL Global health status/QoL Role functioning (C-30) Role functioning (C-30)  Emotional functioning (C-30) Emotional functioning (C-30)  Symptom Scales (C-30/L-13) Symptom Scales (C-30/L-13) |
| Maddocks et al., 2013 [42] | NSCLC cancer; Stage IV (n = 49) | Ex: 70; C: 68, n.a. * STD | CTx | 49 (30/19) | 3–4 chemotherapy cycles long (8–11 wk) self-administered neuromuscular electrical stimulation (NMES) of the quadriceps Muscle | 3–7x/wk; 30 min/session each leg; intensity: 50 Hz; frequency: 350 microseconds pulse width; duty cycle: 11–25%; 0–120 m) | n.a. * | 49/190: (25%) | EX: 15/30 (50%) C: 6/19 (31.5%) in total 21/49 (42.8%) | 9/15 completing at least 3x/wk | n = 3 NMES-related muscle discomfort resulting in dropout (CTC grade I) | ↑ Mental Fatigue (p = 0.03) |  Quadriceps muscle strength Quadriceps muscle strength  Thigh lean mass Thigh lean mass  Whole Body lean mass Whole Body lean mass  Step count Step count  Fatigue Fatigue QoL QoL |
| Oldervoll et al., 2011 [32] | Incurable, metastatic cancer, and life expectancy of 3–24 months (n = 41 gastrointestinal, n = 23 breast, n = 21 lung, n = 16 urological, n = 8 gynaecological, n = 2 hematological, and n = 10 other cancer) | Ex: 62.6 ± 11.3; C: 62.2 ± 10.7 | CTx RTx HT TT | 231 (121/110) | 8-wk sup, combined exercise | 2x/wk; 50–60 min, AEX: Warmup 10–15 min + Circuit EX: 6-station circuit; 2 min on, 1min off, combining strength, aerobic, and coordination elements. | n.a.* | 231/400: (57.7%) | EX: 43/121 (35.5%) C: 25/110 (22.7%) in total 68/231 (29.4%) | 69% finished pre and post assessment sessions: 11/16 | 0 | ↑ Shuttle walk test (p = 0.008) ↑ Handgrip strength (p = 0.01) |  Total fatigue Total fatigue  Physical fatigue Physical fatigue  Mental fatigue Mental fatigue  Sit-to-stand Sit-to-stand |
| Poort et al., 2020 [36] | Cancer patients with palliative systemic treatment (n = 35 breast, n = 21 colorectal, n = 19 prostate, n = 4 renal cell, n = 4 ovarian, n = 4 melanoma, n = 1 bladder cancer) | Ex: 60,67 ± 10.7; C: 63.9 ± 8.9 | CTx HT TT CTx + TT HT + TT IT | 134 (42/46 (+ 46 in ARM3) | 12-wk supcombined REX and AEX | 2x/wk, 120 min/session, AEX: 35 min, Interval cycling: 4 min, 60–80% HRmax/3 min on 35% HRmax, REX (large muscle groups): 35 min, circuit exercise; 60–80% 1RM; 8–12 reps, 3 sets | Usual care | 134/232: (57.7%) | EX: 7/34 (20.6%) C: 3/46 (4.7%) in total 10/80 (12.5%) n = 8 did not receive EX | sessions average: 8 ± 3.5/24 Treatment integrity 86% | EX: muscle pain overuse (n = 4), cardiac complaints (n = 1), increased fatigue after training (n = 1) | none |  Fatigue (CIS and C30) Fatigue (CIS and C30) QoL (C30) QoL (C30) Physical function (C30) Physical function (C30) Emotional function (C30) Emotional function (C30) Functional impairments (C30) Functional impairments (C30) |
| Psyzora et al., 2017 [41] | Advanced cancer patients, admitted to palliative care (n = 15) Alimentary system, n = 13 urogential system, n = 8 mammary gland, n = 6 Hematologica, n = 6 indefinite origin, n = 5 lung, n = 5 central nervous system, n = 1 mouth, n = 1 skin) | Ex: 72.4 ± 9.5; C: 69.3 ± 13.7 | n.a. | 60 (30/30) | 2-wk physiotherapeutic exercise, MFR, and PNF | 3x/wk, 30 min, active exercise of upper and lower limbs, selected techniques of MFR and PNF | Usual care | n.a. * | EX: 1/30 (3.3%) C: 1/30 (3.3%) in total 2/60 (3.3%) | n.a. * | n.a. * | ↑ Fatigue Severity (BFI and ESAS) (p < 0.01) |  Depression (ESAS) Depression (ESAS)  Anxiety (ESAS) Anxiety (ESAS) |
| Rief et al., 2014 + [33,43] | Cancer patients with metastatic progress in thoracic/lumbar spine or in sacrum (n = 20 lung, n = 14 prostate, n = 11 breast, n = 3 renal, n = 2 melanoma, n = 10 other) | Ex: 61.3 ± 10.1; C: 64.1 ± 10.9 | RTx | 60 (30/30) | 2-wk sup isometric REX followed by 12-wk home-based training | 5x/wk, 30 min isometric spinal training of the autochthonous muscles + unsupervised 3x weekly home training | Usual care, aspiration exercise, hot roll treatments | 60/80: (75%) | EX: 5/30 (16.6%) C: 7/30 (23.3%) in total 12/60 (20%) | patients completed the exercise protocol: 25/30 (83.3%) | n.a. * | ↑ 30 s sit-to-stand (p < 0.001), ↑ QoL (BM22) (p = 0.01) ↑ Fatigue (BM22) (p = 0.01) ↑ Pain (VAS) (p = 0.003) |  Functional interference (BM22) Functional interference (BM22)  Emotional interference (BM22) Emotional interference (BM22)  Cognitive interference (BM22) Cognitive interference (BM22) Overall survival Overall survival Progression-free survival Progression-free survival |
| Tsianakas et al., 2017 [40] | Recurrent advancing or metastatic cancer: n = 15 prostate, n = 9 gynecological, n = 9 hematological, n = 7 breast, n = 5 colorectal, n = 1 upper gastrointestinal | Ex: 65 ± 11.7 C: 66.2 ± 10.2 | n.a. | 42 (21/21) | 12-wk walking intervention | 30 min walking on alternate days | n.a. * | 42/110: (38.1%) | EX: 8/21 (38.1%) C: 7/21 (33.3%) in total 15/42 (35.7%) | n.a. * | 0 | none |  QoL (FACT-G) QoL (FACT-G) Global fatigue score Global fatigue score(BFI) |
| Zhou et al., 2017 [37] | Advanced nasopharyngeal cancer stage III/IV | n.a. * | CTx RTx | 114 (57/57) | Tai Chi exercise (24-form Yang style) n.a. duration | 5x/wk 60 min (10 min. warm up, 30 min Tai Chi exercise, 10 min breath and mediation; 10 min relaxation) | Usual care | 114/130: (87.6%) | EX: 15/57 (26.3%) C: 16/57 (28%) in total 31/114 (27.1%) | n.a. * | 0 | ↑ Fatigue (MFSI-SF) (p < 0.05) ↑ General fatigue (MFSI-SF) (p < 0.05) ↑ Physical fatigue (MFSI-SF) (p < 0.05) ↑ Emotional fatigue [MFSI-SF] (p < 0.05) |  Mental fatigue (MFSI-SF) Mental fatigue (MFSI-SF) |
| Zimmer et al., 2017 [39] | Metastasized colorectal cancer | Ex: 68.5 C: 70 | CTx + TT no treat TT | 30 (17/13) | 8-wk sup exercise, combining endurance, REX, and balance exercise | 2x/wk, 60 min (Warmup 10 min. balance training, AEX 60–70% of HRmax, 20 min, REX 5 stations circuit 60–80% of h1RM, 8–12 reps, 2 sets 60–80%; (cool down) | Usual care | n.a. * | EX: 2/17 (11.7%) C: 4/13 (30.7%) in total 6/30 (20%) | Mean training frequency: 88.3% | 0 | 8 wk: ↑ Trial Outcome Index (p = 0.028) ↑ Muscle strength (bench and leg press, lat pulldown) (p = 0.002) ↑ GGT_Reha static 2 (p < 0.025) 14 wk Follow-Up: ↑ Trial Outcome Index (p = 0.031) ↑ Muscle strength (bench and leg press, lat pulldown) (p < 0.05) | 8 wk/14 wk:  Physical Well-being (FACT/GOG-NTX) Physical Well-being (FACT/GOG-NTX)  Functional Well-being (FACT/GOG-NTX) Functional Well-being (FACT/GOG-NTX)  Social Well-being (FACT/GOG-NTX) Social Well-being (FACT/GOG-NTX)  Emotional Well-being (FACT/GOG-NTX) Emotional Well-being (FACT/GOG-NTX)  QoL (FACT-G) QoL (FACT-G) |
 ), resistance exercise (REX), sensory organization test (SOT), supervised (sup), The Edmonton Symptom Assessment System (ESAS), Trial Outcome Index (TOI—Sum of physical well-being and functional well-being intended as summary index of functional status), surgery (SX), quality of life (QoL), weeks (wk), participants (pts), target therapy (TT), 36-Item Short Form Survey (SF-36). * n.a. = data not available in publication/data not shown, ∞ Erratum from 2015 correction to: Prostate Cancer and Prostatic Diseases (2013) 16, 328–335; doi:10.1038/pcan.2013.22. + Studies by Rief et al. from 2014 (a) and (b) are summarized.
), resistance exercise (REX), sensory organization test (SOT), supervised (sup), The Edmonton Symptom Assessment System (ESAS), Trial Outcome Index (TOI—Sum of physical well-being and functional well-being intended as summary index of functional status), surgery (SX), quality of life (QoL), weeks (wk), participants (pts), target therapy (TT), 36-Item Short Form Survey (SF-36). * n.a. = data not available in publication/data not shown, ∞ Erratum from 2015 correction to: Prostate Cancer and Prostatic Diseases (2013) 16, 328–335; doi:10.1038/pcan.2013.22. + Studies by Rief et al. from 2014 (a) and (b) are summarized.| Author | Cancer Entities | Age | Treat | n (EX/C) | Description of Intervention | Exercise Modalities | Control | Recruitment | Drop-Out Rate: | Adherence | AE | EX vs. UC ↑ = Improvement; ↓ = Worsening; | EX vs. UC (Non Sign.) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Buss et al., 2009 [44] | Advanced cancer patients; short lifetime expectancy (approximately 1–2 months) | n.a. * | none | 57 (38/19) | 4-wk sup, individualized kinesiotherapy | 3x/wk, 20–30 min | n.a.* | 57/80 (71.2%) | EX: 12/38 (31.6%) C: 2/19 (10.5%) in total 14/57 (24.5%) | n.a. * | n.a. * | ↑ Fatigue (BFI) wk 3 and wk 4 (p < 0.001) ↓ Intensification physical symptoms (RSCL) (p < 0.05) |  QoL QoL Mental symptoms Mental symptoms |
| Zhao et al., 2015 [45] | Head and Neck squamous cell cancer, Stage III and IV (n = 14 oropharynx, n = 1 larynx, n = 1 nasopharynx, n = 2 unknown) | Ex: 57 ± 7 C: 57 ± 7 | CTx | 20 (11/9) | 14-wk REX and walking exercise (1st 7 wk sup, 2nd 7 wk home-based) | 3x/wk, 60 min, moderate intensity, REX: 8–12 reps, 3 sets lking EX: 30 min per wk, Home-based exercise individualized but also combined REX and walking exercise | Usual care | 20/27: (74.1%) | EX: 1/11 (9.0%) C:2/9 (22.2%) in total 3/20 (15%) | mean session: 15.2/21; attendance rate: 72% home- based training adherence n.a. | 0 | 7 wk: ↑Vitality/Fatigue (SF36) (p < 0.05) ↑Mental Well-being (SF36) (p < 0.05) 14 wk: ↑ strength knee extension (p < 0.05) ↑ Mental Well-being (SF36) (p < 0.05) | 7 wk:  6 MWT 6 MWT  BMI BMI  QoL [SF36] QoL [SF36]  Physical activity Physical activity Lean body mass Lean body mass14 wk:  6 MWT 6 MWT  BMI BMI  QoL [SF36] QoL [SF36]  Physical activity Physical activity Vitality/Fatigue [SF36) Vitality/Fatigue [SF36) Lean body mass Lean body mass |
 ), resistance exercise (REX), Six Minute Walk Test (6 MWT), supervised (sup), The Rotterdam Symptom Checklist (RSCL); week (wk). * n.a. = data not available in publication/ data not shown.
), resistance exercise (REX), Six Minute Walk Test (6 MWT), supervised (sup), The Rotterdam Symptom Checklist (RSCL); week (wk). * n.a. = data not available in publication/ data not shown.| Drop-Out | In Total n | Exercise n | Control n |
|---|---|---|---|
| Participants | 220 (100%) | 128 (58.7%) | 92 (41.8%) |
| Died due to cancer | 61 (27.7%) | 39 (30.5%) | 24 (26.0%) |
| Disease progression/health deterioration | 113 | 68 | 45 |
| (51.3%) | (53.1%) | (48.9%) | |
| Lost to follow-up/ non-compliant | 35 (15.9%) | 17 (13.3%) | 19.5 (20%) |
| Various reasons * | 6 (2.7%) | 1 (0.8%) | 5 (5.4%) |
| Adverse Events *1 | 3 (1.3%) | 3 (2.3%) | 0 (0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Lazzari, N.; Niels, T.; Tewes, M.; Götte, M. A Systematic Review of the Safety, Feasibility and Benefits of Exercise for Patients with Advanced Cancer. Cancers 2021, 13, 4478. https://doi.org/10.3390/cancers13174478
De Lazzari N, Niels T, Tewes M, Götte M. A Systematic Review of the Safety, Feasibility and Benefits of Exercise for Patients with Advanced Cancer. Cancers. 2021; 13(17):4478. https://doi.org/10.3390/cancers13174478
Chicago/Turabian StyleDe Lazzari, Nico, Timo Niels, Mitra Tewes, and Miriam Götte. 2021. "A Systematic Review of the Safety, Feasibility and Benefits of Exercise for Patients with Advanced Cancer" Cancers 13, no. 17: 4478. https://doi.org/10.3390/cancers13174478
APA StyleDe Lazzari, N., Niels, T., Tewes, M., & Götte, M. (2021). A Systematic Review of the Safety, Feasibility and Benefits of Exercise for Patients with Advanced Cancer. Cancers, 13(17), 4478. https://doi.org/10.3390/cancers13174478






