Motor Evoked Potential Warning Criteria in Supratentorial Surgery: A Scoping Review
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Study Selection
2.4. Data Extraction
2.5. Data Analysis and Synthesis of Results
3. Results
- -
- Reversible MEP changes did not result in a postoperative motor deficit in most cases. If a motor deficit occurred, it was more frequently transient than permanent. Irreversible MEP changes were associated with a higher number of permanent than transient motor deficits;
- -
- In almost all studies of the scoping review, specificity and NPV were high regardless of the timing of postoperative assessment. MEPs can reliably identify the true negative cases, and if no irreversible MEP alterations are observed, then it is not probable that the patient suffers a motor deficit immediately after surgery, in the short-term follow-up or in the long-term follow-up;
- -
- Sensitivity and PPV varied across the studies and were rather low or modest in most of them, whereas some individual studies reported a 100% sensitivity and others a 100% PPV. The sensitivity estimates appeared to be higher for permanent motor deficits compared with the early-transient and transient deficits and for the threshold criterion compared with the amplitude criterion. PPV seemed to be higher for the prediction of any motor deficit regardless of the postoperative duration of the deficit. The low and modest values are impacted by the low prevalence of motor deficits;
- -
- There was no remarkable difference in the diagnostic accuracy measures between TES and DCS in the included studies;
- -
- In most cases, the combination of mapping and monitoring yielded higher PPV for all type of deficits compared with monitoring criteria alone;
- -
- The CIs were narrow and indicated high precision of the specificity estimates, but the CIs of the sensitivity estimates were wide, implying greater uncertainty. The wider CIs for sensitivity are also attributed to the low incidence of postoperative deficits;
- -
- The summary of events for each study demonstrated that the rate of postoperative motor deficits and intraoperative MEP changes is low. Regarding MEP changes, reversible alterations appeared to be more frequent than irreversible;
- -
- The correlation analysis revealed a negative correlation between the proportion of reversible MEP changes and the proportion of new postoperative motor deficits associated with MEP changes (rspearman = −0.498, p < 0.001).
4. Discussion
4.1. Type and Range of Available Evidence
4.2. Study Population and Type of Lesions
4.3. Stimulation Techniques and Parameters
4.4. The Spectrum of MEP Warning Criteria
4.5. The Mapping-Monitoring “Crosstalk” and the Warning Sign Hierarchy
4.6. Different Patterns of Injury-Neurophysiological and Neurosurgical Considerations
4.7. MEP Warning Criteria and Postoperative Motor Deficit
4.8. MEPs as Surrogate Markers
4.9. Implications for Research
4.10. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Database and Search Strategy |
| PubMed Key concepts Concept 1: Motor evoked potentials Keywords: “motor evoked potential*”[tw], MEP[tw] MeSH terms: “Evoked Potentials, Motor”[Mesh] Query 1: ((“motor evoked potential*”[tw]) OR (MEP[tw])) OR (“Evoked Potentials, Motor”[Mesh]) Concept 2: warning criteria Keywords: “warning criteri*”[tw], warning [tw], alarm [tw], alert [tw], “alarm criteri*”[tw], mapping[tw], monitoring[tw] MeSH terms: “Intraoperative Neurophysiological Monitoring”[Mesh], “Brain Mapping”[Mesh] Query 2: ((((((((“warning criteri*”[tw]) OR (warning [tw])) OR (alarm [tw])) OR (alert [tw])) OR (“alarm criteri*”[tw])) OR (mapping[tw])) OR (monitoring[tw])) OR (“Intraoperative Neurophysiological Monitoring”[Mesh])) OR (“Brain Mapping”[Mesh]) Concept 3: motor deficit Keywords: “motor deficit”[tw], paresis[tw], hemiparesis[tw], paralysis[tw] MeSH terms: “Predictive Value of Tests”[MeSH], “Paresis/prevention and control”[Mesh], “Paralysis/prevention and control”[Mesh], “Neurologic Manifestations/injuries”[Mesh], “Neurologic Manifestations/prevention and control”[Mesh], “Neurologic Manifestations/surgery”[Mesh] Query 3: ((((“Predictive Value of Tests”[Mesh]) AND “Paresis/prevention and control”[Mesh]) AND “Paralysis/prevention and control”[Mesh]) AND (“Neurologic Manifestations/injuries”[Mesh] OR “Neurologic Manifestations/prevention and control”[Mesh] OR “Neurologic Manifestations/surgery”[Mesh])) OR (“motor deficit”[tw])) OR (paresis[tw])) OR (hemiparesis[tw])) OR (paralysis[tw]) Concept 4: supratentorial brain surgery Keywords: supratentorial [tw], brain surgery[tw], “supratentorial surgery”[tw], tumor*[tw], aneurysm*[tw], epilepsy[tw] MeSH terms: “Neurosurgical Procedures”[Mesh], “Brain Injuries/diagnosis”[Mesh], “Intracranial Aneurysm/surgery”[Mesh], “Brain Neoplasms/surgery”[Mesh], “Epilepsy/surgery”[Mesh], “Central Nervous System Vascular Malformations/surgery”[Mesh] Query 3: ((((((((((((supratentorial[tw]) OR (brain surgery[tw])) OR (“supratentorial surgery”[tw])) OR (tumor*[tw])) OR (aneurysm*[tw])) OR (epilepsy[tw])) OR (“Neurosurgical Procedures”[Mesh])) OR (“Brain Injuries/diagnosis”[Mesh])) OR (“Intracranial Aneurysm/surgery”[Mesh])) OR (“Brain Neoplasms/surgery”[Mesh]))) OR (“Epilepsy/surgery”[Mesh])) OR (“Central Nervous System Vascular Malformations/surgery”[Mesh]) Combined query (((((((((((“warning criteri*”[tw]) OR (warning [tw])) OR (alarm [tw])) OR (alert [tw])) OR (“alarm criteri*”[tw])) OR (mapping[tw])) OR (monitoring[tw])) OR (“Intraoperative Neurophysiological Monitoring”[Mesh])) OR (“Brain Mapping”[Mesh])) AND (((((“Predictive Value of Tests”[Mesh]) AND “Paresis/prevention and control”[Mesh]) AND “Paralysis/prevention and control”[Mesh]) AND (“Neurologic Manifestations/injuries”[Mesh] OR “Neurologic Manifestations/prevention and control”[Mesh] OR “Neurologic Manifestations/surgery”[Mesh])) OR (“motor deficit”[tw])) OR (paresis[tw])) OR (hemiparesis[tw])) OR (paralysis[tw])) AND (((((((((((((supratentorial[tw]) OR (brain surgery[tw])) OR (“supratentorial surgery”[tw])) OR (tumor*[tw])) OR (aneurysm*[tw])) OR (epilepsy[tw])) OR (“Neurosurgical Procedures”[Mesh])) OR (“Brain Injuries/diagnosis”[Mesh])) OR (“Intracranial Aneurysm/surgery”[Mesh])) OR (“Brain Neoplasms/surgery”[Mesh]))) OR (“Epilepsy/surgery”[Mesh])) OR (“Central Nervous System Vascular Malformations/surgery”[Mesh]))) AND (((“motor evoked potential*”[tw]) OR (MEP[tw])) OR (“Evoked Potentials, Motor”[Mesh])) |
| Embase, Scopus, CINAHL, Cochrane Library (“warning criteri*” OR warning OR alarm OR alert OR “alarm criteri*” OR mapping OR monitoring OR “Intraoperative Neurophysiological Monitoring” OR “Brain Mapping”) AND (“motor deficit” OR paresis OR hemiparesis OR paralysis) AND (supratentorial OR brain surgery OR “supratentorial surgery” OR tumor* OR aneurysm* OR epilepsy OR arteriovenous malformation) AND (“motor evoked potential*” OR MEP) |
| Grey literature databases (OpenGrey, NTIS, British Library Direct Plus, York’s CRD, Mednar) (“warning criteri*” OR warning OR alarm OR alert OR “alarm criteri*” OR mapping OR monitoring OR “Intraoperative Neurophysiological Monitoring” OR “Brain Mapping”) AND (“motor deficit” OR paresis OR hemiparesis OR paralysis) AND (supratentorial OR brain surgery OR “supratentorial surgery” OR tumor* OR aneurysm* OR epilepsy OR arteriovenous malformation) AND (“motor evoked potential*” OR MEP) |
Appendix B
| Authors | Reason for Exclusion |
| After full-text review (n = 140) | |
| Bidkar et al. (2021) [119] | Not a primary study |
| Keeble et al. (2021) [120] | No preoperatively defined MEP warning criteria |
| Lee et al. (2021) [121] | No MEP warning criteria |
| Simon et al. (2021) [122] | No MEP warning criteria |
| Wang et al. (2021) [123] | No motor outcome analysis |
| Bander et al. (2020) [124] | No MEP warning criteria |
| Brage et al. (2020) [125] | No sufficient motor outcome data in conjunction with MEP warning criteria |
| Fekete et al. (2020) [126] | Only spinal and brainstem lesions |
| Hayashi et al. (2020) [127] | No MEP warning criteria |
| Jahodová et al. (2020) [128] | No preoperatively defined cutoff value for MEP warning criteria |
| Kim et al. (2020) [129] | No MEP warning criteria |
| Lee et al. (2020) [130] | No MEP warning criteria |
| Porčnik et al. (2020) [131] | Motor outcome data of asleep patients cannot be distinguished from those of awake patients |
| Roth et al. (2020) [132] | No cutoff values for MEP warning criteria |
| Balaji et al. (2019) [133] | No MEP warning criteria |
| Chung et al. (2019) [134] | Only analysis of false-positive and false-negative cases |
| Hu et al. (2019) [135] | No MEP warning criteria |
| Kanaya et al. (2019) [136] | No MEP warning criteria |
| Rossi et al. (2019) [137] | No sufficient motor outcome data in conjunction with MEP warning criteria |
| Wang et al. (2019) [138] | No MEP warning criteria |
| Della Puppa et al. (2018) [139] | No MEP warning criteria |
| Han et al. (2018) [140] | No MEP warning criteria |
| Silverstein et al. (2018) [141] | No MEP warning criteria |
| Skrap et al. (2018) [142] | No clear MEP monitoring warning criteria and no sufficient motor outcome data in conjunction with MEPs-mixture with SSEP |
| Umemura et al. (2018) [143] | Motor outcome data of patients with supratentorial lesions were not clearly reported and could not be extracted |
| Wakui et al. (2018) [144] | No MEP warning criteria |
| Abboud et al. (2017) [100] | Predefined analysis of patients without a postoperative deficit and without MEP warning criteria to investigate pneumocephalus with MRI |
| Akiyama et al. (2017) [145] | No preoperatively defined MEP warning criteria |
| Lv X et al. (2017) [146] | No MEP monitoring |
| Pintea et al. (2017) [147] | No MEP warning criteria |
| Takagaki et al. (2017) [148] | No MEP monitoring |
| Carrabba et al. (2016) [149] | No MEP warning criteria |
| Gripp et al. (2016) [150] | No MEP warning criteria |
| Grossauer et al. (2016) [151] | No preoperatively defined MEP warning criteria |
| Ikedo et al. (2016) [152] | Evacuation of hematoma and control of the presence of MEPs after evacuation -not tumor, vascular or epileptogenic lesion |
| Imai et al. (2016) [153] | No motor outcome analysis |
| Isozaki et al. (2016) [154] | No MEP warning criteria |
| Koenig et al. (2016) [155] | No preoperatively defined MEP warning criteria |
| Nakagomi et al. (2016) [156] | No MEP warning criteria |
| Rossetto et al. (2016) [157] | No MEP warning criteria |
| Zhuang et al. (2016) [158] | Data for patients with supratentorial lesions cannot be extracted with certainty |
| Zhukov et al. (2016) [159] | No preoperatively defined MEP warning criteria |
| Wang et al. (2016) [160] | No MEP warning criteria |
| Eldin et al. (2015) [161] | No MEP warning criteria |
| Erdoğan et al. (2015) [162] | “Presence or absence” warning criterion but only the spinal and brainstem cases are adequately related to postoperative motor outcome |
| Jo et al. (2015) [163] | No MEP warning criteria |
| Joksimovic et al. (2015) [164] | No MEP warning criteria |
| Okamoto et al. (2015) [165] | No MEP warning criteria |
| Quan et al. (2015) [166] | No MEP warning criteria |
| Rashad et al. (2015) [167] | No MEP warning criteria |
| Shiban et al. (2015) [102] | No clear MEP warning criteria |
| Udaka et al. (2015) [168] | No MEP warning criteria |
| Raabe et al. (2014) [105] | Overlapping series from the same institution |
| Sahaya et al. (2014) [169] | Only 3 cases with MEP monitoring and no reporting of motor outcome for them |
| Schucht et al. (2014) [170] | No sufficient motor outcome data in conjunction with MEP warning criteria and mapping thresholds |
| Bulusu et al. (2013) [171] | No MEP warning criteria |
| Krieg et al. (2013) [172] | Overlapping series from the same institution |
| Krieg et al. (2013) [173] | No sufficient motor outcome data in conjunction with MEP warning criteria, data for asleep patients, and postoperative motor deficit cannot be extracted with certainty |
| Shah P.A. (2013) [174] | No clear MEP warning criteria |
| Vassal et al. (2013) [175] | No MEP warning criteria |
| Chen et al. (2012) [176] | No clear MEP warning criteria |
| Horton et al. (2012) [177] | No cutoff values for MEP warning criteria |
| Krieg et al. (2012) [96] | Overlapping series from the same institution |
| Ohue et al. (2012) [107] | No preoperatively defined MEP warning criteria |
| Ritzl EK. (2012) [178] | Not a primary study |
| Schucht et al. (2012) [179] | No sufficient motor outcome data in conjunction with MEP warning criteria |
| Seidel et al. (2012) [97] | No MEP monitoring warning criteria, only mapping warning criteria |
| Uchino et al. (2012) [180] | No sufficient motor outcome data in conjunction with MEP warning criteria |
| Zhu et al. (2012) [181] | No clear MEP warning criteria |
| Chang et al. (2011) [182] | No MEP warning criteria |
| Chen et al. (2011) [183] | No MEP monitoring |
| Fukaya et al. (2011) [184] | No MEP warning criteria |
| González-Darder(2011) [185] | No MEP warning criteria |
| Li et al. (2011) [186] | No sufficient motor outcome data in conjunction with MEP warning criteria |
| Lin et al. (2011) [187] | No cutoff values for MEP warning criteria |
| Nossek et al. (2011) [108] | No clear MEP monitoring warning criteria. No sufficient motor outcome data in conjunction with mapping warning criteria for the asleep patients. |
| Prabhu et al. (2011) [106] | No preoperatively defined MEP warning criteria |
| Szelényi et al. (2011) [103] | No MEP warning criteria |
| Tanaka et al. (2011) [188] | Numbers of MEP changes reported in percentages. Only motor palsy <2/5 MMRC and not postoperative motor deterioration is reported. |
| von Der Brelie et al. (2011) [189] | No MEP monitoring |
| Walter et al. (2011) [190] | No MEP warning criteria |
| Bello et al. (2010) [191] | No preoperatively defined MEP warning criteria |
| Bozzao et al. (2010) [192] | No MEP warning criteria |
| Feigl et al. (2010) [193] | No sufficient motor outcome data in conjunction with MEP warning criteria |
| Juretschke et al. (2010) [194] | No MEP warning criteria |
| Maesawa et al. (2010) [195] | No preoperatively defined MEP warning criteria |
| Sala et al. (2010) [196] | Not a primary study |
| Sanai et al. (2010) [197] | Not a primary study |
| Talacchi et al. (2010) [1] | No MEP monitoring warning criteria |
| Tanaka et al. (2010) [198] | Earlier series from the same institution |
| Yang et al. (2010) [199] | No MEP warning criteria |
| Gorji et al. (2009) [200] | No clear MEP warning criteria |
| Hattingen et al. (2009) [201] | Data for patients with supratentorial lesions cannot be extracted with certainty |
| Kamada et al. (2009) [109] | No preoperatively defined MEP warning criteria |
| Kombos et al. (2009) [202] | No sufficient motor outcome data in conjunction with MEP warning criteria |
| Krammer et al. (2009) [203] | Motor outcome data of patients with supratentorial lesions were not clearly reported and could not be extracted |
| Ozawa et al. (2009) [204] | No MEP warning criteria |
| Simon et al. (2009) [205] | No MEP warning criteria |
| Sugita et al. (2009) [206] | No MEP warning criteria |
| Von Lehe et al. (2009) [207] | No MEP warning criteria |
| Yamaguchi et al. (2009) [208] | No motor outcome analysis |
| Calancie et al. (2008) [209] | Only spinal cases |
| Berman et al. (2007) [210] | No MEP warning criteria |
| Mikuni et al. (2007) [211] | No MEP warning criteria |
| Neuloh et al. (2007) [212] | Overlapping series from the same institution |
| Szelényi et al. (2007) [6] | No MEP warning criteria |
| Yamaguchi et al. (2007) [213] | No motor outcome analysis |
| Fujiki et al. (2006) [214] | No clear preoperatively defined MEP warning criteria |
| Okada et al. (2006) [215] | No MEP warning criteria |
| Kamada et al. (2005) [216] | No MEP warning criteria |
| Szelényi et al. (2005) [101] | No motor outcome data in conjunction with MEP warning criteria |
| Keles et al. (2004) [217] | No MEP warning criteria |
| Kombos et al. (2004) [218] | No MEP warning criteria |
| Neuloh et al. (2004) [219] | No clear and preoperatively defined MEP warning criteria |
| Quiñones-Hinojosa et al. (2004) [220] | No sufficient motor outcome data in conjunction with MEP warning criteria |
| Sakuma et al. (2004) [221] | No MEP warning criteria |
| Signorelli et al. (2004) [222] | No MEP warning criteria |
| Yamamoto et al. (2004) [223] | Only D-wave recording |
| Duffau et al. (2003) [224] | No MEP monitoring warning criteria |
| Fukaya et al. (2003) [225] | Inclusion criterion in the study that the patient did not exhibit MEP amplitude decrease of >50% (warning criteria) intraoperatively |
| Sala et al. (2003) [111] | No sufficient motor outcome data in conjunction with MEP warning criteria |
| Suess et al. (2002) [226] | No MEP warning criteria |
| Kombos et al. (2000) [227] | No MEP warning criteria |
| Kofler et al. (1999) [228] | No MEP warning criteria |
| Kombos et al. (1999) [229] | No MEP warning criteria |
| Rohde et al. (1999) [230] | MEPs elicited through Transcranial Magnetic Stimulation(TMS) |
| Yingling et al. (1999) [231] | No MEP warning criteria |
| Krombach et al. (1998) [232] | No MEP warning criteria |
| Zentner et al. (1998) [233] | No correlation of MEPs with postoperative but with preoperative motor deficit |
| Zentner et al. (1996) [117] | No MEP warning criteria |
| Kawaguchi et al. (1996) [234] | No clear MEP warning criteria |
| Maertens et al. (1996) [235] | No clear MEP warning criteria |
| Pechstein et al. (1996) [236] | No MEP warning criteria |
| Rodi et al. (1996) [237] | No MEP warning criteria |
| Skirboll et al. (1996) [238] | No MEP warning criteria |
| Taniguchi et al. (1993) [5] | No MEP warning criteria |
| Ebeling et al. (1992) [239] | No MEP warning criteria |
| Schramm et al. (1990) [240] | Only SSEP monitoring |
| Zentner et al. (1988) [241] | No clear MEP warning criteria |
| After abstract screening (n = 73) | |
| Chen et al. (2021) [242] | Τechnical report, presentation of a new technique |
| Machetanz et al. (2021) [243] | MEPs elicited through Transcranial Magnetic Stimulation(TMS) |
| Cattaneo et al. (2020) [244] | Use of MEPs to investigate brain connectivity |
| Kang et al. (2020) [245] | Not a primary study |
| Policicchio et al. (2020) [246] | Not a primary study |
| Shibata et al. (2020) [247] | Awake craniotomy |
| Wang et al. (2020) [248] | Only SSEP analysis |
| Zuo et al. (2020) [249] | Not a primary study |
| NCT04178395(2019) [250] | Protocol for clinical trial |
| Hiruta et al. (2019) [251] | Τechnical report (cortical and subcortical stimulation ratio), no motor outcome data |
| Zhu et al. (2019) [91] | Not a primary study |
| Rajan et al. (2018) [252] | Not a primary study |
| Valci et al. (2018) [253] | No MEP monitoring to avoid a postoperative deficit, no MEP warning criteria |
| Abdulrauf et al. (2017) [254] | Awake surgery |
| Benavides et al. (2017) [255] | Not a clinical study; study in pigs |
| Bharadwaj et al. (2017) [256] | Τechnical report, application, and feasibility of a new monitoring system |
| Calancie B. (2017) [257] | Not a primary study |
| Grasso et al. (2017) [258] | Not a primary study |
| Hemmer et al. (2017) [259] | Not a primary study |
| Journée et al. (2017) [20] | Not a primary study |
| Ku et al. (2017) [260] | Case report of a patient with vestibular schwannoma |
| Liu et al. (2017) [21] | Spinal surgery |
| MacDonald DB. (2017) [9] | Not a primary study |
| Moser et al. (2017) [261] | MEPs elicited through Transcranial Magnetic Stimulation (TMS) |
| Sanmillan et al. (2017) [98] | Not a primary study |
| Schucht et al. (2017) [104] | Not a primary study |
| Thomas et al. (2017) [89] | Not a primary study |
| Alimohamadi et al. (2016) [262] | Awake craniotomy |
| Coppola et al. (2016) [263] | Not a primary study |
| Holdefer et al. (2016) [28] | Not a primary study |
| König, R. (2016) [264] | Not a primary study |
| Raabe et al. (2016) [265] | Not a primary study |
| Yao et al. (2016) [266] | The term MEP referred to Meningiomas-en-plaque, no MEP monitoring |
| Holdefer et al. (2015) [92] | Not a primary study |
| Ottenhausen et al. (2015) [267] | Not a primary study |
| Sala et al. (2015) [87] | Not a primary study |
| Nakamura et al. (2014) [268] | Only abstract available |
| Suzuki et al. (2014) [269] | Awake aneurysm clipping |
| Yang et al. (2014) [270] | Intraoperative neuromonitoring used as a mapping technique to find the corticospinal projections |
| Landazuri et al. (2013) [271] | Not a primary study |
| MacDonald et al. (2013) [7] | Not a primary study |
| Rajapakse et al. (2013) [272] | Not a primary study |
| Yamashita et al. (2013) [273] | Only abstract available |
| Bacigaluppi et al. (2012) [274] | Not a primary study |
| De Witt Hamer et al. (2012) [275] | Not a primary study |
| Emerson et al. (2012) [276] | Not a primary study |
| Hotson et al. (2012) [277] | Electrocorticography analysis |
| Ito et al. (2012) [278] | Spinal surgery |
| Guo et al. (2011) [90] | Review/Not a primary study |
| Guo et al. (2011) [279] | Letter to the Editor/not a primary study |
| Li et al. (2011) [280] | Case report of a patient with high-grade brainstem glioma |
| Deiner S. (2010) [281] | Spinal surgery |
| Pabon et al. (2010) [282] | Only abstract available |
| Lefaucheur et al. (2009) [283] | Electrode placement for neuropathic pain treatment |
| Sun et al. (2009) [284] | MEPs elicited through Transcranial Magnetic Stimulation (TMS) |
| Duffau, H. (2008)-1 [285] | Not a primary study |
| Duffau, H. (2008)-2 [286] | Not a primary study |
| Takashima et al. (2008) [287] | Not a primary study |
| Duffau H. (2007) [288] | Not a primary study |
| Tharin et al. (2007) [289] | Not a primary study |
| Duffau, H. (2006) [290] | Not a primary study |
| Schramm et al. (2006) [291] | Only abstract available |
| Shinoura et al. (2006) [292] | Awake surgery |
| Kuzniecky et al. (2005) [293] | Not a primary study |
| Binder et al. (2004) [294] | Correlation of intraoperative neuromonitoring and imaging with Kernohan’s notch syndrome |
| Hashiguchi et al. (2004) [295] | Only abstract available |
| Kondo et al. (2004) [296] | Only abstract available |
| Neuloh et al. (2004) [297] | Not a primary study |
| Sala et al. (2002) [93] | Not a primary study |
| Di Lazzaro et al. (1999) [298] | Neurological and not neurosurgical patients |
| Calancie et al. (1998) [299] | Spinal lesions |
| Reinhardt et al. (1996) [300] | Τechnical report, presentation of an optical navigation system |
| Newlon et al. (1984) [301] | MEPs in diagnosis/prognosis/follow-up. Not intraoperatively. |
| After title screening: Duplicate or irrelevant records (n = 381) | |
** Additional clarifications
| |
References
- Talacchi, A.; Turazzi, S.; Locatelli, F.; Sala, F.; Beltramello, A.; Alessandrini, F.; Manganotti, P.; Lanteri, P.; Gambin, R.; Ganau, M.; et al. Surgical treatment of high-grade gliomas in motor areas. The impact of different supportive technologies: A 171-patient series. J. Neuro Oncol. 2010, 100, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Deletis, V. What does intraoperative monitoring of motor evoked potentials bring to the neurosurgeon? Acta Neurochir. 2005, 147, 1015–1017. [Google Scholar] [CrossRef] [PubMed]
- Deletis, V.; Isgum, V.; Amassian, V.E. Neurophysiological mechanisms underlying motor evoked potentials in anesthetized humans.: Part 1. Recovery time of corticospinal tract direct waves elicited by pairs of transcranial electrical stimuli. Clin. Neurophysiol. 2001, 112, 438–444. [Google Scholar] [CrossRef]
- Deletis, V.; Rodi, Z.; Amassian, V.E. Neurophysiological mechanisms underlying motor evoked potentials in anesthetized humans.: Part 2. Relationship between epidurally and muscle recorded MEPs in man. Clin. Neurophysiol. 2001, 112, 445–452. [Google Scholar] [CrossRef]
- Taniguchi, M.; Cedzich, C.; Schramm, J. Modification of Cortical Stimulation for Motor Evoked Potentials under General Anesthesia. Neurosurgery 1993, 32, 219–226. [Google Scholar] [CrossRef]
- Szelényi, A.; Kothbauer, K.F.; Deletis, V. Transcranial electric stimulation for intraoperative motor evoked potential monitoring: Stimulation parameters and electrode montages. Clin. Neurophysiol. 2007, 118, 1586–1595. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, D.; Skinner, S.; Shils, J.; Yingling, C. Intraoperative motor evoked potential monitoring—A position statement by the American Society of Neurophysiological Monitoring. Clin. Neurophysiol. 2013, 124, 2291–2316. [Google Scholar] [CrossRef] [PubMed]
- Seidel, K.; Beck, J.; Stieglitz, L.; Schucht, P.; Raabe, A. The warning-sign hierarchy between quantitative subcortical motor mapping and continuous motor evoked potential monitoring during resection of supratentorial brain tumors. J. Neurosurg. 2013, 118, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, D.B. Overview on Criteria for MEP Monitoring. J. Clin. Neurophysiol. 2017, 34, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Kombos, T.; Suess, O.; Ciklatekerlio, Ö.; Brock, M. Monitoring of intraoperative motor evoked potentials to increase the safety of surgery in and around the motor cortex. J. Neurosurg. 2001, 95, 608–614. [Google Scholar] [CrossRef]
- Neuloh, G.; Pechstein, U.; Cedzich, C.; Schramm, J. Motor Evoked Potential Monitoring with Supratentorial Surgery. Neurosurgery 2004, 54, 1061–1072. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.H.; Ha, E.J.; Cho, W.-S.; Kang, H.-S.; Kim, J.E. Effectiveness and Limitations of Intraoperative Monitoring with Combined Motor and Somatosensory Evoked Potentials During Surgical Clipping of Unruptured Intracranial Aneurysms. World Neurosurg. 2017, 108, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Gorji, R.; Allott, G.; Modes, K.; Lunn, R.; Yang, Z.-J. The Usefulness of Intraoperative Neurophysiological Monitoring in Cervical Spine Surgery. J. Neurosurg. Anesthesiol. 2012, 24, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Malcharek, M.J.; Hesse, J.; Hesselbarth, K.; Thoma, K.; Wegner, C.; Sablotzki, A.; Hennig, G.; Gille, J. Warning criteria for MEP monitoring during carotid endarterectomy: A retrospective study of 571 patients. J. Clin. Monit. 2019, 34, 589–595. [Google Scholar] [CrossRef]
- Suess, O.; Suess, S.; Brock, M.; Kombos, T. Intraoperative electrocortical stimulation of Brodman area 4: A 10-year analysis of 255 cases. Head Face Med. 2006, 2, 20. [Google Scholar] [CrossRef] [PubMed]
- Szelényi, A.; Langer, D.; Kothbauer, K.; De Camargo, A.B.; Flamm, E.S.; Deletis, V. Monitoring of muscle motor evoked potentials during cerebral aneurysm surgery: Intraoperative changes and postoperative outcome. J. Neurosurg. 2006, 105, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Abboud, T.; Schaper, M.; Dührsen, L.; Schwarz, C.; Schmidt, N.O.; Westphal, M.; Martens, T. A novel threshold criterion in transcranial motor evoked potentials during surgery for gliomas close to the motor pathway. J. Neurosurg. 2016, 125, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Malcharek, M.; Ulkatan, S.; Marinò, V.; Geyer, M.; Lladó-Carbó, E.; Perez-Fajardo, G.; Arranz-Arranz, B.; Climent, J.; Aloj, F.; Franco, E.; et al. Intraoperative monitoring of carotid endarterectomy by transcranial motor evoked potential: A multicenter study of 600 patients. Clin. Neurophysiol. 2013, 124, 1025–1030. [Google Scholar] [CrossRef]
- Suzuki, K.; Kodama, N.; Sasaki, T.; Matsumoto, M.; Konno, Y.; Sakuma, J.; Oinuma, M.; Murakawa, M. Intraoperative monitoring of blood flow insufficiency in the anterior choroidal artery during aneurysm surgery. J. Neurosurg. 2003, 98, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Journée, H.L.; Berends, H.; Kruyt, M.C. The Percentage of Amplitude Decrease Warning Criteria for Transcranial MEP Monitoring. J. Clin. Neurophysiol. 2017, 34, 22–31. [Google Scholar] [CrossRef]
- Liu, Q.; Wang, Q.; Liu, H.; Wu, W.K.; Chan, M.T. Warning criteria for intraoperative neurophysiologic monitoring. Curr. Opin. Anaesthesiol. 2017, 30, 557–562. [Google Scholar] [CrossRef]
- Byoun, H.S.; Oh, C.W.; Kwon, O.-K.; Lee, S.U.; Ban, S.P.; Kim, S.H.; Kim, T.; Bang, J.S.; Choi, J.; Park, K.S. Intraoperative neuromonitoring during microsurgical clipping for unruptured anterior choroidal artery aneurysm. Clin. Neurol. Neurosurg. 2019, 186, 105503. [Google Scholar] [CrossRef] [PubMed]
- Obermueller, T.; Schaeffner, M.; Shiban, E.; Droese, D.; Negwer, C.; Meyer, B.; Ringel, F.; Krieg, S.M. Intraoperative neuromonitoring for function-guided resection differs for supratentorial motor eloquent gliomas and metastases. BMC Neurol. 2015, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Review Manager (RevMan) [Computer Program]. Version 5.4. The Cochrane Collaboration. 2020. Available online: https://training.cochrane.org/system/files/uploads/protected_file/RevMan5.4_user_guide.pdf (accessed on 15 April 2021).
- Holdefer, R.N.; MacDonald, D.B.; Guo, L.; Skinner, S.A. An evaluation of motor evoked potential surrogate endpoints during intracranial vascular procedures. Clin. Neurophysiol. 2016, 127, 1717–1725. [Google Scholar] [CrossRef] [PubMed]
- Giampiccolo, D.; Parisi, C.; Meneghelli, P.; Tramontano, V.; Basaldella, F.; Pasetto, M.; Pinna, G.; Cattaneo, L.; Sala, F. Long-term motor deficit in brain tumour surgery with preserved intra-operative motor-evoked potentials. Brain Commun. 2021, 3, fcaa226. [Google Scholar] [CrossRef] [PubMed]
- Gogos, A.J.; Young, J.S.; Morshed, R.A.; Avalos, L.N.; Noss, R.S.; Villanueva-Meyer, J.E.; Hervey-Jumper, S.L.; Berger, M.S. Triple motor mapping: Transcranial, bipolar, and monopolar mapping for supratentorial glioma resection adjacent to motor pathways. J. Neurosurg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Mammadkhanli, O.; Bozkurt, M.; Caglar, Y.S. Assesment of functional results for lesions located in eloquent areas with intraoperative cortical-subcortical stimulation and cortical mapping. Turk. Neurosurg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Seidel, K.; Schucht, P.; Beck, J.; Raabe, A. Continuous Dynamic Mapping to Identify the Corticospinal Tract in Motor Eloquent Brain Tumors: An Update. J. Neurol. Surg. Part A Cent. Eur. Neurosurg. 2020, 81, 105–110. [Google Scholar] [CrossRef]
- Abboud, T.; Schwarz, C.; Westphal, M.; Martens, T. A comparison between threshold criterion and amplitude criterion in transcranial motor evoked potentials during surgery for supratentorial lesions. J. Neurosurg. 2019, 131, 740–749. [Google Scholar] [CrossRef]
- Majchrzak, K.; Bobek-Billewicz, B.; Hebda, A.; Adamczyk, P.; Majchrzak, H.; Ładziński, P. Surgical treatment of adult patients with thalamic tumors with the aid of tractography, fMRI, transcranial electrical stimulation and direct electrical stimulation of the subcortical white matter. Neurol. Neurochir. Pol. 2018, 52, 720–730. [Google Scholar] [CrossRef] [PubMed]
- Moiyadi, A.; Velayutham, P.; Shetty, P.; Seidel, K.; Janu, A.; Madhugiri, V.; Singh, V.K.; Patil, A.; John, R. Combined Motor Evoked Potential Monitoring and Subcortical Dynamic Mapping in Motor Eloquent Tumors Allows Safer and Extended Resections. World Neurosurg. 2018, 120, e259–e268. [Google Scholar] [CrossRef] [PubMed]
- Plans, G.; Fernández-Conejero, I.; Rifà-Ros, X.; Fernández-Coello, A.; Rosselló, A.; Gabarrós, A. Evaluation of the High-Frequency Monopolar Stimulation Technique for Mapping and Monitoring the Corticospinal Tract in Patients With Supratentorial Gliomas. A Proposal for Intraoperative Management Based on Neurophysiological Data Analysis in a Series of Ninety-Two Patients. Neurosurgery 2017, 81, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Li, M.; Yi, L.; He, B.; Li, X.; Jiang, Y. Intraoperative neuromonitoring during brain arteriovenous malformation microsurgeries and postoperative dysfunction. Medicine 2017, 96, e8054. [Google Scholar] [CrossRef] [PubMed]
- Boex, C.; Haemmerli, J.; Momjian, S.; Schaller, K. Prognostic Values of Motor Evoked Potentials in Insular, Precental, or Postcentral Resections. J. Clin. Neurophysiol. 2016, 33, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Shiban, E.; Krieg, S.M.; Obermueller, T.; Wostrack, M.; Meyer, B.; Ringel, F. Continuous subcortical motor evoked potential stimulation using the tip of an ultrasonic aspirator for the resection of motor eloquent lesions. J. Neurosurg. 2015, 123, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; Kim, Y.I.; Hong, J.T.; Sung, J.H.; Lee, S.W.; Yang, S.H. Intraoperative Monitoring of Motor-Evoked Potentials for Supratentorial Tumor Surgery. J. Korean Neurosurg. Soc. 2014, 56, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Gempt, J.; Krieg, S.M.; Hüttinger, S.; Buchmann, N.; Ryang, Y.-M.; Shiban, E.; Meyer, B.; Zimmer, C.; Förschler, A.; Ringel, F. Postoperative ischemic changes after glioma resection identified by diffusion-weighted magnetic resonance imaging and their association with intraoperative motor evoked potentials. J. Neurosurg. 2013, 119, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Ostrý, S.; Belsan, T.; Otáhal, J.; Beneš, V.; Netuka, D. Is Intraoperative Diffusion Tensor Imaging at 3.0T Comparable to Subcortical Corticospinal Tract Mapping? Neurosurgery 2013, 73, 797–807. [Google Scholar] [CrossRef] [PubMed]
- Pastor, J.; Vega-Zelaya, L.; Pulido, P.; Garnés-Camarena, O.; Abreu, A.; Sola, R.G. Role of intraoperative neurophysiological monitoring during fluorescence-guided resection surgery. Acta Neurochir. 2013, 155, 2201–2213. [Google Scholar] [CrossRef]
- Sakurada, K.; Matsuda, K.; Funiu, H.; Kuge, A.; Takemura, S.; Sato, S.; Kayama, T. Usefulness of Multimodal Examination and Intraoperative Magnetic Resonance Imaging System in Glioma Surgery. Neurol. Med. Chir. 2012, 52, 553–557. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Senft, C.; Forster, M.-T.; Bink, A.; Mittelbronn, M.; Franz, K.; Seifert, V.; Szelényi, A. Optimizing the extent of resection in eloquently located gliomas by combining intraoperative MRI guidance with intraoperative neurophysiological monitoring. J. Neuro Oncol. 2012, 109, 81–90. [Google Scholar] [CrossRef]
- Hatiboglu, M.A.; Weinberg, J.S.; Suki, D.; Tummala, S.; Rao, G.; Sawaya, R.; Prabhu, S.S. Utilization of Intraoperative Motor Mapping in Glioma Surgery with High-Field Intraoperative Magnetic Resonance Imaging. Ster. Funct. Neurosurg. 2010, 88, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Ichikawa, T.; Suzuki, K.; Sasaki, T.; Matsumoto, M.; Sakuma, J.; Oinuma, M.; Kasuya, H.; Kodama, N. Utility and the Limit of Motor Evoked Potential Monitoring for Preventing Complications in Surgery for Cerebral Arteriovenous Malformation. Oper. Neurosurg. 2010, 67, ons222–ons228. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Szelényi, A.; Hattingen, E.; Weidauer, S.; Seifert, V.; Ziemann, U. Intraoperative Motor Evoked Potential Alteration in Intracranial Tumor Surgery and Its Relation to Signal Alteration in Postoperative Magnetic Resonance Imaging. Neurosurgery 2010, 67, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Kombos, T.; Süss, O.; Vajkoczy, P. Subcortical mapping and monitoring during insular tumor surgery. Neurosurg. Focus 2009, 27, E5. [Google Scholar] [CrossRef] [PubMed]
- Neuloh, G.; Schramm, J. Are there False-negative Results of Motor Evoked Potential Monitoring in Brain Surgery? Central Eur. Neurosurg. 2009, 70, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Neuloh, G.; Pechstein, U.; Schramm, J. Motor tract monitoring during insular glioma surgery. J. Neurosurg. 2007, 106, 582–592. [Google Scholar] [CrossRef]
- Zhou, H.H.; Kelly, P.J. Transcranial Electrical Motor Evoked Potential Monitoring for Brain Tumor Resection. Neurosurgery 2001, 48, 1075–1081. [Google Scholar] [CrossRef]
- Cedzich, C.; Taniguchi, M.; Schäfer, S.; Schramm, J. Somatosensory Evoked Potential Phase Reversal and Direct Motor Cortex Stimulation during Surgery in and around the Central Region. Neurosurgery 1996, 38, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Koo, D.L.; Lee, W.G.; Hong, S.-C.; Seo, D.-W. Clinical Usefulness of Intraoperative Motor-Evoked Potential Monitoring during Temporal Lobe Epilepsy Surgery. J. Clin. Neurol. 2019, 15, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Neuloh, G.C.; Bien, C.G.; Clusmann, H.; Von Lehe, M.; Schramm, J. Continuous motor monitoring enhances functional preservation and seizure-free outcome in surgery for intractable focal epilepsy. Acta Neurochir. 2010, 152, 1307–1314. [Google Scholar] [CrossRef] [PubMed]
- Guo, D.; Fan, X.; You, H.; Tao, X.; Qi, L.; Ling, M.; Li, Z.; Liu, J.; Qiao, H. Prediction of postoperative motor deficits using intraoperative motor-evoked potentials in middle cerebral artery aneurysm. Neurosurg. Rev. 2021, 44, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Park, D.; Kim, B.H.; Lee, S.-E.; Jeong, E.; Cho, K.; Park, J.K.; Choi, Y.-J.; Jin, S.; Hong, D.; Kim, M.-C. Usefulness of Intraoperative Neurophysiological Monitoring During the Clipping of Unruptured Intracranial Aneurysm: Diagnostic Efficacy and Detailed Protocol. Front. Surg. 2021, 8, 17. [Google Scholar] [CrossRef] [PubMed]
- You, H.; Fan, X.; Guo, D.; Li, Z.; Tao, X.; Qi, L.; Ling, M.; Liu, J.; Qiao, H. Efficacy of evoked potential monitoring for predicting postoperative motor status in internal carotid artery aneurysm surgeries. J. Clin. Monit. 2021. [Google Scholar] [CrossRef]
- Kameda, M.; Hishikawa, T.; Hiramatsu, M.; Yasuhara, T.; Kurozumi, K.; Date, I. Precise MEP monitoring with a reduced interval is safe and useful for detecting permissive duration for temporary clipping. Sci. Rep. 2020, 10, 3507. [Google Scholar] [CrossRef] [PubMed]
- Greve, T.; Stoecklein, V.M.; Dorn, F.; Laskowski, S.; Thon, N.; Tonn, J.-C.; Schichor, C. Introduction of intraoperative neuromonitoring does not necessarily improve overall long-term outcome in elective aneurysm clipping. J. Neurosurg. 2020, 132, 1188–1196. [Google Scholar] [CrossRef]
- Li, Z.; Fan, X.; Wang, M.; Tao, X.; Qi, L.; Ling, M.; Guo, D.; Qiao, H. Prediction of postoperative motor deficits using motor evoked potential deterioration duration in intracranial aneurysm surgery. Clin. Neurophysiol. 2019, 130, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, K.; Mikami, T.; Yokoyama, R.; Suzuki, Y.; Komura, S.; Enatsu, R.; Noshiro, S.; Miyata, K.; Akiyama, Y.; Mikuni, N. Electrophysiological influence of temporal occlusion of the parent artery during aneurysm surgery. J. Clin. Neurosci. 2017, 45, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Staarmann, B.; O’Neal, K.; Magner, M.; Zuccarello, M. Sensitivity and Specificity of Intraoperative Neuromonitoring for Identifying Safety and Duration of Temporary Aneurysm Clipping Based on Vascular Territory, a Multimodal Strategy. World Neurosurg. 2017, 100, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Jin, S.-J.; Karm, M.-H.; Moon, Y.-J.; Jeong, H.-W.; Kim, J.-W.; Ha, S.-I.; Kim, J.-U. Comparison of false-negative/positive results of intraoperative evoked potential monitoring between no and partial neuromuscular blockade in patients receiving propofol/remifentanil-based anesthesia during cerebral aneurysm clipping surgery. Medicine 2016, 95, e4725. [Google Scholar] [CrossRef]
- Maruta, Y.; Fujii, M.; Imoto, H.; Nomura, S.; Tanaka, N.; Inamura, A.; Sadahiro, H.; Oka, F.; Goto, H.; Shirao, S.; et al. Strategies and Pitfalls of Motor-Evoked Potential Monitoring during Supratentorial Aneurysm Surgery. J. Stroke Cerebrovasc. Dis. 2016, 25, 484–495. [Google Scholar] [CrossRef]
- Song, J.; Lang, L.; Zhu, W.; Gu, Y.; Xu, B.; Cai, J.; Yue, Q.; Xu, G.; Chen, L.; Mao, Y. Application of intraoperative motor evoked potential monitoring during giant internal carotid artery aneurysm surgery using prolonged temporary occlusion. Acta Neurochir. 2015, 157, 1833–1840. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, T.; Kon, H.; Saito, A.; Nakamura, T.; Abe, M.; Nishijima, M. Intraoperative Supporting Tools in Aneurysm Surgery: Roles of Electrophysiological Monitoring. Jpn. J. Neurosurg. 2014, 23, 716–720. [Google Scholar] [CrossRef][Green Version]
- Takebayashi, S.; Kamiyama, H.; Takizawa, K.; Kobayashi, T.; Saitoh, N. The Significance of Intraoperative Monitoring of Muscle Motor Evoked Potentials during Unruptured Large and Giant Cerebral Aneurysm Surgery. Neurol. Med. Chir. 2014, 54, 180–188. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yue, Q.; Zhu, W.; Gu, Y.; Xu, B.; Lang, L.; Song, J.; Cai, J.; Xu, G.; Chen, L.; Mao, Y. Motor Evoked Potential Monitoring During Surgery of Middle Cerebral Artery Aneurysms: A Cohort Study. World Neurosurg. 2014, 82, 1091–1099. [Google Scholar] [CrossRef] [PubMed]
- Dengler, J.; Cabraja, M.; Faust, K.; Picht, T.; Kombos, T.; Vajkoczy, P. Intraoperative neurophysiological monitoring of extracranial-intracranial bypass procedures. J. Neurosurg. 2013, 119, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Yao, P.; Wu, Z.; Yu, L. Ischemia changes and tolerance ratio of evoked potential monitoring in intracranial aneurysm surgery. Clin. Neurol. Neurosurg. 2013, 115, 552–556. [Google Scholar] [CrossRef]
- Maruta, Y.; Fujii, M.; Imoto, H.; Nomura, S.; Oka, F.; Goto, H.; Shirao, S.; Yoshikawa, K.; Yoneda, H.; Ideguchi, M.; et al. Intra-operative monitoring of lower extremity motor-evoked potentials by direct cortical stimulation. Clin. Neurophysiol. 2012, 123, 1248–1254. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Zhou, Q.; Zhang, M.; Jiang, Y. Assessment of intraoperative motor-evoked potentials for predicting postoperative motor function during the surgical clipping of intracranial aneurysms. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2012, 37, 244–249. [Google Scholar] [PubMed]
- Motoyama, Y.; Kawaguchi, M.; Yamada, S.; Nakagawa, I.; Nishimura, F.; Hironaka, Y.; Park, Y.-S.; Hayashi, H.; Abe, R.; Nakase, H. Evaluation of Combined Use of Transcranial and Direct Cortical Motor Evoked Potential Monitoring During Unruptured Aneurysm Surgery. Neurol. Med. Chir. 2011, 51, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Irie, T.; Yoshitani, K.; Ohnishi, Y.; Shinzawa, M.; Miura, N.; Kusaka, Y.; Miyazaki, S.; Miyamoto, S. The Efficacy of Motor-evoked Potentials on Cerebral Aneurysm Surgery and New-onset Postoperative Motor Deficits. J. Neurosurg. Anesthesiol. 2010, 22, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Yeon, J.Y.; Seo, D.-W.; Hong, S.-C.; Kim, J.-S. Transcranial motor evoked potential monitoring during the surgical clipping of unruptured intracranial aneurysms. J. Neurol. Sci. 2010, 293, 29–34. [Google Scholar] [CrossRef]
- Szelenyi, A.; Langer, D.; Beck, J.; Raabe, A.; Flamm, E.; Seifert, V.; Deletis, V. Transcranial and direct cortical stimulation for motor evoked potential monitoring in intracerebral aneurysm surgery. Neurophysiol. Clin. Neurophysiol. 2007, 37, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Weinzierl, M.R.; Reinacher, P.; Gilsbach, J.M.; Rohde, V. Combined motor and somatosensory evoked potentials for intraoperative monitoring: Intra- and postoperative data in a series of 69 operations. Neurosurg. Rev. 2007, 30, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Horiuchi, K.; Suzuki, K.; Sasaki, T.; Matsumoto, M.; Sakuma, J.; Konno, Y.; Oinuma, M.; Itakura, T.; Kodama, N. Intraoperative monitoring of blood flow insufficiency during surgery of middle cerebral artery aneurysms. J. Neurosurg. 2005, 103, 275–283. [Google Scholar] [CrossRef]
- Nakagawa, I.; Park, H.; Kotsugi, M.; Motoyama, Y.; Myochin, K.; Takeshima, Y.; Matsuda, R.; Nishimura, F.; Yamada, S.; Takatani, T.; et al. Diagnostic impact of monitoring transcranial motor-evoked potentials to prevent ischemic complications during endovascular treatment for intracranial aneurysms. Neurosurg. Rev. 2021, 44, 1493–1501. [Google Scholar] [CrossRef] [PubMed]
- Wilent, W.B.; Belyakina, O.; Korsgaard, E.; Tjoumakaris, S.I.; Gooch, M.R.; Jabbour, P.; Rosenwasser, R.; English, J.D.; Kim, W.; Tesdahl, E.; et al. Intraoperative vascular complications during 2278 cerebral endovascular procedures with multimodality IONM: Relationship between signal change, complication, intervention and postoperative outcome. J. NeuroInterventional. Surg. 2021, 13, 378–383. [Google Scholar] [CrossRef]
- Lee, S.; Kim, D.Y.; Bin Kim, S.; Kim, W.; Kang, M.-R.; Kim, H.-J.; Lee, K.H.; Yoo, M.; Choi, B.-S.; Kim, J.S.; et al. Predictive value of neurophysiologic monitoring during neurovascular intervention for postoperative new neurologic deficits. Neuroradiology 2018, 61, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Cubells, C.; Garcia, P.; Coll-Canti, J. Implementation of Intraoperative Neurophysiological Monitoring during Endovascular Procedures in the Central Nervous System. Interv. Neurol. 2015, 3, 85–100. [Google Scholar] [CrossRef]
- Hiraishi, T.; Fukuda, M.; Oishi, M.; Nishino, K.; Shinbo, J.; Sorimachi, T.; Ito, Y.; Fujii, Y. Usefulness of motor-evoked potential monitoring during coil embolization of anterior choroidal artery aneurysms: Technical reports. Neurol. Res. 2011, 33, 360–362. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Kumabe, T.; Saito, R.; Kanamori, M.; Yamashita, Y.; Sonoda, Y.; Tominaga, T. Preservation of the Long Insular Artery to Prevent Postoperative Motor Deficits After Resection of Insulo-opercular Glioma: Technical Case Reports. Neurol. Med. Chir. 2014, 54, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Szelényi, A.; De Camargo, A.B.; Flamm, E.S.; Deletis, V. Neurophysiological criteria for intraoperative prediction of pure motor hemiplegia during aneurysm surgery. J. Neurosurg. 2003, 99, 575–578. [Google Scholar] [CrossRef] [PubMed]
- Sala, F.; Di Rocco, C. Intraoperative Neurophysiological Monitoring in Neurosurgery: Moving the Debate from Evidence and Cost-Effectiveness to Education and Training. World Neurosurg. 2015, 83, 32–34. [Google Scholar] [CrossRef] [PubMed]
- Howick, J.; Cohen, B.A.; McCulloch, P.; Thompson, M.; Skinner, S.A. Foundations for evidence-based intraoperative neurophysiological monitoring. Clin. Neurophysiol. 2016, 127, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Thomas, B.; Guo, D. The Diagnostic Accuracy of Evoked Potential Monitoring Techniques During Intracranial Aneurysm Surgery for Predicting Postoperative Ischemic Damage: A Systematic Review and Meta-Analysis. World Neurosurg. 2017, 103, 829–840.e3. [Google Scholar] [CrossRef]
- Guo, L.; Gelb, A.W. The use of motor evoked potential monitoring during cerebral aneurysm surgery to predict pure motor deficits due to subcortical ischemia. Clin. Neurophysiol. 2011, 122, 648–655. [Google Scholar] [CrossRef]
- Zhu, F.; Chui, J.; Herrick, I.; Martin, J. Intraoperative evoked potential monitoring for detecting cerebral injury during adult aneurysm clipping surgery: A systematic review and meta-analysis of diagnostic test accuracy. BMJ Open 2019, 9, e022810. [Google Scholar] [CrossRef] [PubMed]
- Holdefer, R.; Macdonald, D.; Skinner, S. Somatosensory and motor evoked potentials as biomarkers for post-operative neurological status. Clin. Neurophysiol. 2015, 126, 857–865. [Google Scholar] [CrossRef] [PubMed]
- Sala, F.; Kržan, M.J.; Deletis, V. Intraoperative neurophysiological monitoring in pediatric neurosurgery: Why, when, how? Child’s Nerv. Syst. 2002, 18, 264–287. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J.A.; Lyon, R.; Feiner, J.; Diab, M.; Gregory, G.A. The Effect of Age on Motor Evoked Potentials in Children Under Propofol/Isoflurane Anesthesia. Anesthesia Analg. 2006, 103, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Resnick, T.J.; Alvarez, L.A.; Duchowny, M. Cortical stimulation thresholds in children being evaluated for resective surgery. Epilepsia 1998, 29, 651–652. [Google Scholar]
- Krieg, S.M.; Shiban, E.; Droese, D.; Gempt, J.; Buchmann, N.; Pape, H.; Ryang, Y.M.; Meyer, B.; Ringel, F. Predictive Value and Safety of Intraoperative Neurophysiological Monitoring With Motor Evoked Potentials in Glioma Surgery. Neurosurgery 2011, 70, 1060–1071. [Google Scholar] [CrossRef] [PubMed]
- Seidel, K.; Beck, J.; Stieglitz, L.; Schucht, P.; Raabe, A. Low-Threshold Monopolar Motor Mapping for Resection of Primary Motor Cortex Tumors. Oper. Neurosurg. 2012, 71, ons104–ons115. [Google Scholar] [CrossRef] [PubMed]
- SanMillan, J.L.; Plans, G.; Gabarrós, A.; Fernández-Conejero, I. Letter to the Editor: Threshold criterion in transcranial motor evoked potentials. J. Neurosurg. 2017, 126, 1744–1746. [Google Scholar] [CrossRef]
- Rothwell, J.; Burke, D.; Hicks, R.; Stephen, J.; Woodforth, I.; Crawford, M. Transcranial electrical stimulation of the motor cortex in man: Further evidence for the site of activation. J. Physiol. 1994, 481, 243–250. [Google Scholar] [CrossRef]
- Abboud, T.; Huckhagel, T.; Stork, J.-H.; Hamel, W.; Schwarz, C.; Vettorazzi, E.; Westphal, M.; Martens, T. Why Does Threshold Level Change in Transcranial Motor-evoked Potentials During Surgery for Supratentorial Lesions? J. Neurosurg. Anesthesiol. 2017, 29, 393–399. [Google Scholar] [CrossRef]
- Szelényi, A.; Kothbauer, K.; De Camargo, A.B.; Langer, D.; Flamm, E.S.; Deletis, V. Motor Evoked Potential Monitoring during Cerebral Aneurysm Surgery: Technical Aspects and Comparison of Transcranial and Direct Cortical Stimulation. Oper. Neurosurg. 2005, 57, 331. [Google Scholar] [CrossRef] [PubMed]
- Shiban, E.; Krieg, S.M.; Haller, B.; Buchmann, N.; Obermueller, T.; Boeckh-Behrens, T.; Wostrack, M.; Meyer, B.; Ringel, F. Intraoperative subcortical motor evoked potential stimulation: How close is the corticospinal tract? J. Neurosurg. 2015, 123, 711–720. [Google Scholar] [CrossRef]
- Szelényi, A.; Senft, C.; Jardan, M.; Forster, M.; Franz, K.; Seifert, V.; Vatter, H. Intra-operative subcortical electrical stimulation: A comparison of two methods. Clin. Neurophysiol. 2011, 122, 1470–1475. [Google Scholar] [CrossRef]
- Schucht, P.; Seidel, K.; Jilch, A.; Beck, J.; Raabe, A. A review of monopolar motor mapping and a comprehensive guide to continuous dynamic motor mapping for resection of motor eloquent brain tumors. Neurochirurgie 2017, 63, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Raabe, A.; Beck, J.; Schucht, P.; Seidel, K. Continuous dynamic mapping of the corticospinal tract during surgery of motor eloquent brain tumors: Evaluation of a new method. J. Neurosurg. 2014, 120, 1015–1024. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, S.S.; Gasco, J.; Tummala, S.; Weinberg, J.S.; Rao, G. Intraoperative magnetic resonance imaging–guided tractography with integrated monopolar subcortical functional mapping for resection of brain tumors. J. Neurosurg. 2011, 114, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Ohue, S.; Kohno, S.; Inoue, A.; Yamashita, D.; Harada, H.; Kumon, Y.; Kikuchi, K.; Miki, H.; Ohnishi, T. Accuracy of Diffusion Tensor Magnetic Resonance Imaging-Based Tractography for Surgery of Gliomas Near the Pyramidal Tract. Neurosurgery 2011, 70, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Nossek, E.; Korn, A.; Shahar, T.; Kanner, A.A.; Yaffe, H.; Marcovici, D.; Ben-Harosh, C.; Ben Ami, H.; Weinstein, M.; Shapira-Lichter, I.; et al. Intraoperative mapping and monitoring of the corticospinal tracts with neurophysiological assessment and 3-dimensional ultrasonography-based navigation. J. Neurosurg. 2011, 114, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Kamada, K.; Todo, T.; Ota, T.; Ino, K.; Masutani, Y.; Aoki, S.; Takeuchi, F.; Kawai, K.; Saito, N. The motor-evoked potential threshold evaluated by tractography and electrical stimulation. J. Neurosurg. 2009, 111, 785–795. [Google Scholar] [CrossRef] [PubMed]
- Bello, L.; Riva, M.; Fava, E.; Ferpozzi, V.; Castellano, A.; Raneri, F.; Pessina, F.; Bizzi, A.; Falini, A.; Cerri, G. Tailoring neurophysiological strategies with clinical context enhances resection and safety and expands indications in gliomas involving motor pathways. Neuro Oncol. 2014, 16, 1110–1128. [Google Scholar] [CrossRef]
- Sala, F.; Lanteri, P. Brain surgery in motor areas: The invaluable assistance of intraoperative neurophysiological monitoring. J. Neurosurg. Sci. 2003, 47. [Google Scholar]
- Han, S.J.; Morshed, R.A.; Troncon, I.; Jordan, K.M.; Henry, R.G.; Hervey-Jumper, S.L.; Berger, M.S. Subcortical stimulation mapping of descending motor pathways for perirolandic gliomas: Assessment of morbidity and functional outcome in 702 cases. J. Neurosurg. 2019, 131, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Drummond, J.C. The Lower Limit of Autoregulation. Anesthesiology 1997, 86, 1431–1433. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Yamazaki, K.; Chiba, Y.; Isobe, M.; Isu, T.; Hokari, M. The Relationship between Carotid Stump Pressure and Changes in Motor-Evoked Potentials in Carotid Endarterectomy Patients. J. Neurol. Surg. Part A Cent. Eur. Neurosurg. 2016, 77, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Trevethan, R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front. Public Heal. 2017, 5, 307. [Google Scholar] [CrossRef] [PubMed]
- Sjöberg, R.L.; Stålnacke, M.; Andersson, M.; Eriksson, J. The supplementary motor area syndrome and cognitive control. Neuropsychologia 2019, 129, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Zentner, J.; Hufnagel, A.; Pechstein, U.; Wolf, H.K.; Schramm, J. Functional results after resective procedures involving the supplementary motor area. J. Neurosurg. 1996, 85, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Aronson, J.K. Biomarkers and surrogate endpoints. Br. J. Clin. Pharmacol. 2005, 59, 491–494. [Google Scholar] [CrossRef]
- Bidkar, P.U.; Thakkar, A.; Manohar, N.; Rao, K.S. Intraoperative neurophysiological monitoring in paediatric neurosurgery. Int. J. Clin. Pract. 2021, e14160. [Google Scholar] [CrossRef]
- Keeble, H.; Lavrador, J.P.; Pereira, N.; Lente, K.; Brogna, C.; Gullan, R.; Bhangoo, R.; Vergani, F.; Ashkan, K. Electromagnetic Navigation Systems and Intraoperative Neuromonitoring: Reliability and Feasibility Study. Oper. Neurosurg. 2021, 20, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Jeon, Y.T.; Oh, T.K.; Lee, J.; Choi, E.S. Predictive factors of unacceptable movement and motor-evoked potentials during intraoperative neurophysiological monitoring in adult patients undergoing brain surgery: A retrospective study. Medicine 2021, 100, e24148. [Google Scholar] [CrossRef]
- Simon, M.V.; Lee, D.K.; Choi, B.D.; Talati, P.A.; Yang, J.C.; Koch, M.J.; Jones, P.S.; Curry, W.T. Neurophysiologic Mapping of Thalamocortical Tract in Asleep Craniotomies: Promising Results From an Early Experience. Oper. Neurosurg. 2021, 20, 219–225. [Google Scholar] [CrossRef]
- Wang, G.; Zhang, X.; Gou, Y.; Wen, Y.; Zhang, G.; Li, M.; Zhang, S.; Yin, Y.; Chen, S.; Qi, S.; et al. A Hybrid Strategy for Patients With Complex Cerebral Aneurysm: STA-MCA Bypass in Combination With Endovascular Embolization. Front. Neurol. 2021, 11, 614601. [Google Scholar] [CrossRef] [PubMed]
- Bander, E.D.; Shelkov, E.; Modik, O.; Kandula, P.; Karceski, S.C.; Ramakrishna, R. Use of the train-of-five bipolar technique to provide reliable, spatially accurate motor cortex identification in asleep patients. Neurosurg. Focus 2020, 48, E4. [Google Scholar] [CrossRef] [PubMed]
- Brage, L.; Pérez-Lorensu, P.J.; Plata-Bello, J.; Saponaro-González, Á.; Pérez-Orribo, L.; García-Conde, M.; Febles-García, P.; Roldán-Delgado, H.; García-Marín, V. Direct cortical stimulation with cylindrical depth electrodes in the interhemispheric fissure for leg motor evoked potential monitoring. Clin. Neurophysiol. 2020, 131, 127–132. [Google Scholar] [CrossRef]
- Fekete, G.; Bognár, L.; Gutema, E.; Novák, L. Intraoperative electrophysiology in children—Single institute experience of 96 examinations. Neurol. India 2020, 68, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, H.; Bebawy, J.F.; Koht, A.; Hemmer, L.B. Cautionary findings for motor evoked potential monitoring in intracranial aneurysm surgery after a single administration of rocuronium to facilitate tracheal intubation. J. Clin. Monit. Comput. 2020. [Google Scholar] [CrossRef] [PubMed]
- Jahodová, A.; Beňová, B.; Kudr, M.; Ježdík, P.; Janča, R.; Bělohlávková, A.; Liby, P.; Leško, R.; Tichý, M.; Čelakovský, P.; et al. A novel effective paradigm of intraoperative electrical stimulation mapping in children. J. Neurosurg. Pediatrics 2020, 26, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Jeon, H.J.; Kim, S.; Chung, J.; Park, K.Y.; Huh, S.K.; Lee, J.W. Microsurgical clipping of ruptured anterior choroidal artery aneurysms: Incidence of and risk factors for ischemic complications. Clin. Neurol. Neurosurg. 2020, 195, 105884. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, H.; Choi, B.S.; Jin, S.C. Unexpected abnormal intraoperative neurophysiologic monitoring change by multiple spontaneous intracerebral haemorrhage during endovascular coiling. Br. J. Neurosurg. 2020, 34, 342–345. [Google Scholar] [CrossRef]
- Porčnik, A.; Pešak, J.; Žele, T.; Koritnik, B.; Rodi, Z.; Prestor, B. Continuous Dynamic Mapping of the Corticospinal Tract in Motor Eloquent Tumor Surgery: Our Experience and Evaluation of the Method. Acta. Med. Acad. 2020, 49, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Roth, J.; Korn, A.; Sala, F.; Benvenisti, H.; Jubran, M.; Bitan-Talmor, Y.; Ekstein, M.; Constantini, S. Intraoperative neurophysiology in pediatric supratentorial surgery: Experience with 57 cases. Childs. Nerv. Syst. 2020, 36, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Balaji, A.; Rajagopal, N.; Yamada, Y.; Teranishi, T.; Kawase, T.; Kato, Y. A Retrospective Study in Microsurgical Procedures of Large and Giant Intracranial Aneurysms: An Outcome Analysis. World Neurosurg. X 2019, 2, 100007. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.; Park, W.; Hong, S.H.; Park, J.C.; Ahn, J.S.; Kwun, B.D.; Lee, S.A.; Kim, S.H.; Jeon, J.Y. Intraoperative use of transcranial motor/sensory evoked potential monitoring in the clipping of intracranial aneurysms: Evaluation of false-positive and false-negative cases. J. Neurosurg. 2018, 130, 936–994. [Google Scholar] [CrossRef] [PubMed]
- Hu, P.; Zhang, H.Q.; Li, X.Y.; Tong, X.Z. Double-Barrel Superficial Temporal Artery to Proximal Middle Cerebral Artery Bypass to Treat Complex Intracranial Aneurysms: A Reliable High Blood Flow Bypass. World Neurosurg. 2019, 125, e884–e890. [Google Scholar] [CrossRef] [PubMed]
- Kanaya, K.; Goto, T.; Horiuchi, T.; Hongo, K. Threshold variation of transcranial motor evoked potential with threshold criterion in frontotemporal craniotomy. Clin. Neurophysiol. Pract. 2019, 4, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Rossi, M.; Conti Nibali, M.; Viganò, L.; Puglisi, G.; Howells, H.; Gay, L.; Sciortino, T.; Leonetti, A.; Riva, M.; Fornia, L.; et al. Resection of tumors within the primary motor cortex using high-frequency stimulation: Oncological and functional efficiency of this versatile approach based on clinical conditions. J. Neurosurg. 2019, 133, 642–654. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.S.; Yang, Y.; Velz, J.; Keller, E.; Luft, A.R.; Regli, L.; Neidert, M.C.; Bozinov, O. Management of brainstem haemorrhages. Swiss Med. Wkly. 2019, 149, w20062. [Google Scholar] [CrossRef] [PubMed]
- Della Puppa, A.; Rossetto, M.; Volpin, F.; Rustemi, O.; Grego, A.; Gerardi, A.; Ortolan, R.; Causin, F.; Munari, M.; Scienza, R. Microsurgical Clipping of Intracranial Aneurysms Assisted by Neurophysiological Monitoring, Microvascular Flow Probe, and ICG-VA: Outcomes and Intraoperative Data on a Multimodal Strategy. World Neurosurg. 2018, 113, e336–e344. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Kwon, Y.C.; Kim, S.M.; Hyun, S.J.; Jahng, T.A.; Kim, K.J.; Kim, H.J.; Choi, H.Y.; Park, Y.S.; Seok Park, K. Risk Factor Analysis of Change in Intraoperative Neurophysiologic Monitoring During Cervical Open Door Laminoplasty. World Neurosurg. 2018, 119, e235–e243. [Google Scholar] [CrossRef]
- Silverstein, J.W.; Rosenthal, A.; Ellis, J.A. Direct Cortical Motor Evoked Potentials Versus Transcranial Motor Evoked Potentials for the Detection of Cortical Ischemia During Supratentorial Craniotomy: Case Report. Cureus 2018, 10, e3771. [Google Scholar] [CrossRef] [PubMed]
- Skrap, M.; Vescovi, M.C.; Pauletto, G.; Maieron, M.; Tomasino, B.; Bagatto, D.; Tuniz, F. Supratentorial Cavernous Malformations Involving the Corticospinal Tract and Sensory Motor Cortex: Treatment Strategies, Surgical Considerations, and Outcomes. Oper. Neurosurg. 2018, 15, 483–497. [Google Scholar] [CrossRef] [PubMed]
- Umemura, T.; Nishizawa, S.; Nakano, Y.; Saito, T.; Kitagawa, T.; Miyaoka, R.; Suzuki, K.; Yamamoto, J. Intraoperative monitoring of motor-evoked potential for parenchymal brain tumor removal: An analysis of false-negative cases. J. Clin. Neurosci. 2018, 57, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Wakui, D.; Ito, H.; Takasuna, H.; Onodera, H.; Oshio, K.; Tanaka, Y. Surgical removal of an arteriovenous malformation in the anterior perforated substance in a pregnant woman. Surg. Neurol. Int. 2018, 9, 117. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, Y.; Ohtaki, S.; Komatsu, K.; Toyama, K.; Enatsu, R.; Mikami, T.; Wanibuchi, M.; Mikuni, N. Intraoperative Mapping and Monitoring of the Pyramidal Tract Using Endoscopic Depth Electrodes. World Neurosurg. 2017, 105, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Lv, X.; Hu, X.; Li, W.; He, H.; Jiang, C.; Li, Y. Curative and adjunctive AVM Onyx embolization of AVMs through the choroidal arteries. Interv. Neuroradiol. 2017, 23, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Pintea, B.; Baumert, B.; Kinfe, T.M.; Gousias, K.; Parpaley, Y.; Boström, J.P. Early motor function after local treatment of brain metastases in the motor cortex region with stereotactic radiotherapy/radiosurgery or microsurgical resection: A retrospective study of two consecutive cohorts. Radiat. Oncol. 2017, 12, 177. [Google Scholar] [CrossRef] [PubMed]
- Takagaki, M.; Togami, Y.; Murasawa, A.; Nakao, K. Multiple fusiform aneurysms of the distal middle cerebral artery showing different radiological courses: A case report. Interdiscip. Neurosurg. 2017, 10, 8–10. [Google Scholar] [CrossRef]
- Carrabba, G.; Bertani, G.; Cogiamanian, F.; Ardolino, G.; Zarino, B.; Di Cristofori, A.; Locatelli, M.; Caroli, M.; Rampini, P. Role of Intraoperative Neurophysiologic Monitoring in the Resection of Thalamic Astrocytomas. World Neurosurg. 2016, 94, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Gripp, D.A.; Nakasone, F.J.; Maldaun, M.V.; de Aguiar, P.H.; Mathias, L.R., Jr. Giant pseudoaneurysm originated from distal middle cerebral artery dissection treated by trapping under sensitive evoked potential and motor evoked potential monitoring: Case report and discussion. Surg. Neurol. Int. 2016, 7 (Suppl. 9), S214–S218. [Google Scholar] [CrossRef][Green Version]
- Grossauer, S.; Koeck, K.; Kraschl, J.; Olipitz, O.; Hausegger, K.A.; Vince, G.H. Detection of Cerebral Vasospasm Following Aneurysmal Subarachnoid Hemorrhage Using Motor Evoked Potentials. Neurosurgery 2016, 78, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Ikedo, T.; Nakamura, K.; Sano, N.; Nagata, M.; Okada, Y.; Terakawa, Y.; Murata, T. Intraoperative Transcranial Motor-Evoked Potentials Predict Motor Function Outcome in Intracerebral Hemorrhage Surgery. World Neurosurg. 2016, 90, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Imai, H.; Watanabe, K.; Miyagishima, T.; Yoshimoto, Y.; Kin, T.; Nakatomi, H.; Saito, N. The outcome of a surgical protocol based on ischemia overprotection in large and giant aneurysms of the anterior cerebral circulation. Neurosurg. Rev. 2016, 39, 505–517. [Google Scholar] [CrossRef] [PubMed]
- Isozaki, M.; Satow, T.; Matsushige, T.; Mori, H.; Iihara, K. Superselective Provocative Test with Propofol Using Motor-Evoked Potential Monitoring for Managing Cerebral Arteriovenous Malformations Fed by the Anterior Choroidal Artery. J.Stroke. Cerebrovasc. Dis. 2016, 25, e153–e157. [Google Scholar] [CrossRef] [PubMed]
- Koenig, R.W.; Kapapa, T.; Antoniadis, G.; Roehrer, S.; Hagel, V.; Wirtz, C.R.; Pedro, M.T.; Kretschmer, T.; Schmidt, T.; Coburger, J. Surgery for brain arteriovenous malformations (BAVMs): The role of intraoperative imaging and neuromonitoring. Neurol. Psychiatry Brain Res. 2016, 22, 110–118. [Google Scholar] [CrossRef]
- Nakagomi, T.; Furuya, K.; Tanaka, J.; Takanashi, S.; Watanabe, T.; Shinohara, T.; Ogawa, A.; Fujii, N. Clipping Surgery for Unruptured Middle Cerebral Artery Aneurysms. Acta. Neurochir. Suppl. 2016, 123, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Rossetto, M.; Ciccarino, P.; Lombardi, G.; Rolma, G.; Cecchin, D.; Della Puppa, A. Surgery on motor area metastasis. Neurosurg. Rev. 2016, 39, 71–77; discussion 77–78. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, D.X.; Wu, J.S.; Yao, C.J.; Qiu, T.M.; Lu, J.F.; Zhu, F.P.; Xu, G.; Zhu, W.; Zhou, L.F. Intraoperative Multi-Information-Guided Resection of Dominant-Sided Insular Gliomas in a 3-T Intraoperative Magnetic Resonance Imaging Integrated Neurosurgical Suite. World Neurosurg. 2016, 89, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Zhukov, V.Y.; Goryaynov, S.A.; Ogurtsova, A.A.; Ageev, I.S.; Protskiy, S.V.; Pronin, I.N.; Tonoyan, A.S.; Kobyakov, G.L.; Nenashev, E.A.; Smirnov, A.S.; et al. Diffusion tensor imaging tractography and intraoperative neurophysiological monitoring in surgery of intracranial tumors located near the pyramidal tract. Zhurnal Vopr. Neirokhirurgii Im. N. N. Burd. 2016, 80, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.J.; Lin, F.X.; Zhao, B.; Wu, J.; Cao, Y.; Wang, S. Testing the Reliability of BOLD-fMRI Motor Mapping in Patients with Cerebral Arteriovenous Malformations by Electric Cortical Stimulation and Surgery Outcomes. World Neurosurg. 2016, 92, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Eldin, S.S.; Iwasaki, M.; Nishio, Y.; Jin, K.; Nakasato, N.; Tominaga, T. Resection of focal cortical dysplasia located in the upper pre-central gyrus. Epileptic. Disord. 2015, 17, 479–484. [Google Scholar] [CrossRef][Green Version]
- Erdoğan, E.T.; Karamürsel, S.; Kiriş, T. Effective Use of Multimodal Intraoperative Neuromonitoring in Neurosurgery. Neurosurg. Q. 2015, 25, 452–457. [Google Scholar] [CrossRef]
- Jo, K.I.; Kim, H.R.; Yeon, J.Y.; Hong, S.C.; Kim, J.S. Treatment outcomes of surgical clipping for unruptured anterior circulation aneurysm-single institute experiences in the era of neurophysiologic monitoring and endovascular treatment. Neurosurg. Rev. 2015, 38, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Joksimovic, B.; Szelenyi, A.; Seifert, V.; Damjanovic, A.; Damjanovic, A.; Rasulic, L. Transcranial electric stimulation for intraoperative motor evoked potential monitoring: Dependence of required stimulation current on interstimulus interval value. J. Neurol. Surg. A. Cent. Eur. Neurosurg. 2015, 76, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, E.; Ishikawa, E.; Yamamoto, T.; Matsuda, M.; Nakai, K.; Matsushita, A.; Masuda, Y.; Akutsu, H.; Ayuzawa, S.; Sakamaki, F.; et al. Variability in amplitude and stimulation threshold values in motor evoked potential (MEP) monitoring during the resection of brain lesions. Clin. Neurophysiol. 2015, 126, 1271–1278. [Google Scholar] [CrossRef]
- Quan, K.; Xu, G.; Zhao, F.; Zhu, W. Tailored keyhole surgery for basal ganglia cavernous malformation with preoperative three-dimensional pyramidal tracts assessment and intraoperative electrophysiological monitoring. Chin. Neurosurg. J. 2015, 1, 15. [Google Scholar] [CrossRef][Green Version]
- Rashad, S.; Endo, H.; Sultan, A.E.; Shimizu, H.; Fujimura, M.; Sato, K.; Matsumoto, Y.; Tominaga, T. Therapeutic Clip Occlusion of the Anterior Choroidal Artery Involved with Partially Thrombosed Fusiform Aneurysm: A Case Report. J. Stroke. Cerebrovasc. Dis. 2015, 24, e227–e230. [Google Scholar] [CrossRef]
- Udaka, Y.T.; Yoon, J.M.; Malicki, D.M.; Khanna, P.C.; Levy, M.L.; Crawford, J.R. Atypical Teratoid Rhabdoid Tumor in a Teenager with Unusual Infiltration Into the Jugular Foramen. World Neurosurg. 2015, 84, 2075.e13–2075.e16. [Google Scholar] [CrossRef] [PubMed]
- Sahaya, K.; Pandey, A.S.; Thompson, B.G.; Bush, B.R.; Minecan, D.N. Intraoperative monitoring for intracranial aneurysms: The Michigan experience. J. Clin. Neurophysiol. 2014, 31, 563–567. [Google Scholar] [CrossRef] [PubMed]
- Schucht, P.; Seidel, K.; Beck, J.; Murek, M.; Jilch, A.; Wiest, R.; Fung, C.; Raabe, A. Intraoperative monopolar mapping during 5-ALA-guided resections of glioblastomas adjacent to motor eloquent areas: Evaluation of resection rates and neurological outcome. Neurosurg. Focus 2014, 37, E16. [Google Scholar] [CrossRef]
- Bulusu, S.; Kassam, A.B.; Houlden, D.A.; Alkherayf, F. Intraoperative neurophysiological monitoring during circulatory arrest using deep hypothermia: A case report during brain aneurysm clipping. Neurodiagn. J. 2013, 53, 121–141. [Google Scholar] [PubMed]
- Krieg, S.M.; Schäffner, M.; Shiban, E.; Droese, D.; Obermüller, T.; Gempt, J.; Meyer, B.; Ringel, F. Reliability of intraoperative neurophysiological monitoring using motor evoked potentials during resection of metastases in motor-eloquent brain regions: Clinical article. J. Neurosurg. 2013, 118, 1269–1278. [Google Scholar] [CrossRef] [PubMed]
- Krieg, S.M.; Schnurbus, L.; Shiban, E.; Droese, D.; Obermueller, T.; Buchmann, N.; Gempt, J.; Meyer, B.; Ringel, F. Surgery of highly eloquent gliomas primarily assessed as non-resectable: Risks and benefits in a cohort study. BMC Cancer 2013, 13, 51. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.A. Transcranial motor evoked potential monitoring outcome in the high-risk brain and spine surgeries: Correlation of clinical and neurophysiological data—An Indian perspective. Ann. Indian. Acad. Neurol. 2013, 16, 609–613. [Google Scholar] [CrossRef]
- Vassal, F.; Schneider, F.; Nuti, C. Intraoperative use of diffusion tensor imaging-based tractography for resection of gliomas located near the pyramidal tract: Comparison with subcortical stimulation mapping and contribution to surgical outcomes. Br. J. Neurosurg. 2013, 27, 668–675. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Lang, L.; Zhou, L.; Song, D.; Mao, Y. Bypass or not? Adjustment of surgical strategies according to motor evoked potential changes in large middle cerebral artery aneurysm surgery. World Neurosurg. 2012, 77, 398.e1–398.e6. [Google Scholar] [CrossRef]
- Horton, T.G.; Barnes, M.; Johnson, S.; Kalapos, P.C.; Link, A.; Cockroft, K.M. Feasibility and efficacy of transcranial motor-evoked potential monitoring in neuroendovascular surgery. AJNR. Am. J. Neuroradiol. 2012, 33, 1825–1831. [Google Scholar] [CrossRef] [PubMed]
- Ritzl, E.K. Intraoperative neuromonitoring during glioma surgery: Bring in the expert neurophysiologists! J. Clin. Neurophysiol. 2012, 29, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Schucht, P.; Beck, J.; Abu-Isa, J.; Andereggen, L.; Murek, M.; Seidel, K.; Stieglitz, L.; Raabe, A. Gross total resection rates in contemporary glioblastoma surgery: Results of an institutional protocol combining 5-aminolevulinic acid intraoperative fluorescence imaging and brain mapping. Neurosurgery 2012, 71, 927–935; discussion 935–936. [Google Scholar] [CrossRef] [PubMed]
- Uchino, H.; Nakamura, T.; Kuroda, S.; Houkin, K.; Murata, J.; Saito, H. Intraoperative dual monitoring during carotid endarterectomy using motor evoked potentials and near-infrared spectroscopy. World Neurosurg. 2012, 78, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.P.; Wu, J.S.; Song, Y.Y.; Yao, C.J.; Zhuang, D.X.; Xu, G.; Tang, W.J.; Qin, Z.Y.; Mao, Y.; Zhou, L.F. Clinical application of motor pathway mapping using diffusion tensor imaging tractography and intraoperative direct subcortical stimulation in cerebral glioma surgery: A prospective cohort study. Neurosurgery 2012, 71, 1170–1183; discussion 1183–1184. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.F.; Clark, A.; Smith, J.S.; Polley, M.Y.; Chang, S.M.; Barbaro, N.M.; Parsa, A.T.; McDermott, M.W.; Berger, M.S. Functional mapping-guided resection of low-grade gliomas in eloquent areas of the brain: Improvement of long-term survival. Clinical article. J. Neurosurg. 2011, 114, 566–573. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Spetzler, R.F.; McDougall, C.G.; Albuquerque, F.C.; Xu, B. Detection of ischemia in endovascular therapy of cerebral aneurysms: A perspective in the era of neurophysiological monitoring. Neurosurg. Rev. 2011, 34, 69–75. [Google Scholar] [CrossRef]
- Fukaya, C.; Sumi, K.; Otaka, T.; Shijo, K.; Nagaoaka, T.; Kobayashi, K.; Oshima, H.; Watanabe, T.; Yamamoto, T.; Katayama, Y. Corticospinal descending direct wave elicited by subcortical stimulation. J. Clin. Neurophysiol. 2011, 28, 297–301. [Google Scholar] [CrossRef] [PubMed]
- González-Darder, J.M.; González-López, P.; Talamantes, F.; Quilis, V.; Cortés, V.; García-March, G.; Roldán, P. Multimodal navigation in the functional microsurgical resection of intrinsic brain tumors located in eloquent motor areas: Role of tractography. Neurosurg. Focus. 2010, 28, E5. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Deshaies, E.; Allott, G.; Gorji, R. Transcranial motor evoked potential changes induced by provocative testing during embolization of cerebral arteriovenous malformations in patients under total intravenous anesthesia. Am. J. Electroneurodiagnostic. Technol. 2011, 51, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Zhao, J.; Zhao, Y.; Zhang, D.; Wang, R.; Qiao, H.; Wang, S. Multiple intraoperative monitoring-assisted microneurosurgical treatment for anterior circulation cerebral aneurysm. J. Int. Med. Res. 2011, 39, 891–903. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Tashiro, T.; Gomi, A.; Takanashi, J.; Ujiie, H. Sensitivity and specificity in transcranial motor-evoked potential monitoring during neurosurgical operations. Surg. Neurol. Int. 2011, 2, 111. [Google Scholar] [CrossRef] [PubMed]
- von der Brelie, C.; von Lehe, M. Long term outcome in cerebral cavernous malformation associated drug resistant epilepsy. Acta Neurochirurgica 2011, 153, 1892. [Google Scholar]
- Walter, J.; Kuhn, S.A.; Waschke, A.; Kalff, R.; Ewald, C. Operative treatment of subcortical metastatic tumours in the central region. J. Neurooncol. 2011, 103, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Bello, L.; Castellano, A.; Fava, E.; Casaceli, G.; Riva, M.; Scotti, G.; Gaini, S.M.; Falini, A. Intraoperative use of diffusion tensor imaging fiber tractography and subcortical mapping for resection of gliomas: Technical considerations. Neurosurg. Focus. 2010, 28, E6. [Google Scholar] [CrossRef]
- Bozzao, A.; Romano, A.; Angelini, A.; D’Andrea, G.; Calabria, L.F.; Coppola, V.; Mastronardi, L.; Fantozzi, L.M.; Ferrante, L. Identification of the pyramidal tract by neuronavigation based on intraoperative magnetic resonance tractography: Correlation with subcortical stimulation. Eur. Radiol. 2010, 20, 2475–2481. [Google Scholar] [CrossRef] [PubMed]
- Feigl, G.C.; Ritz, R.; Moraes, M.; Klein, J.; Ramina, K.; Gharabaghi, A.; Krischek, B.; Danz, S.; Bornemann, A.; Liebsch, M.; et al. Resection of malignant brain tumors in eloquent cortical areas: A new multimodal approach combining 5-aminolevulinic acid and intraoperative monitoring. J. Neurosurg. 2010, 113, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Juretschke, F.R.; Güresir, E.; Marquardt, G.; Berkefeld, J.; Rosahl, S.; Klisch, J.; Raabe, A.; Seifert, V.; Gerlach, R. Trigonal and peritrigonal lesions of the lateral ventricle-surgical considerations and outcome analysis of 20 patients. Neurosurg. Rev. 2010, 33, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Maesawa, S.; Fujii, M.; Nakahara, N.; Watanabe, T.; Wakabayashi, T.; Yoshida, J. Intraoperative tractography and motor evoked potential (MEP) monitoring in surgery for gliomas around the corticospinal tract. World Neurosurg. 2010, 74, 153–161. [Google Scholar] [CrossRef]
- Sala, F.; Manganotti, P.; Grossauer, S.; Tramontanto, V.; Mazza, C.; Gerosa, M. Intraoperative neurophysiology of the motor system in children: A tailored approach. Child’s Nerv. Syst. 2010, 26, 473–490. [Google Scholar] [CrossRef] [PubMed]
- Sanai, N.; Berger, M.S. Intraoperative stimulation techniques for functional pathway preservation and glioma resection. Neurosurg. Focus. 2010, 28, E1. [Google Scholar] [CrossRef]
- Tanaka, S.; Kawasaki, M.; Kimura, I.; Takanashi, J.; Ujiie, H. Alarm Points in Transcranial Motor-Evoked Potential Monitoring during Neurosurgical Operations. Jpn. J. Neurosurg. 2010, 19, 57–65. [Google Scholar] [CrossRef]
- Yang, W.D.; Chen, Z.J.; Yu, Q.; Wang, Z.G.; Hao, Z.D.; Li, H.; Zhang, C.Z. Applications of blood oxygenation level dependent-functional magnetic resonance imaging, diffusion tensor imaging and intraoperative neurophysiology monitoring in secondary epileptic surgery in M1 area. Zhonghua Yi Xue Za Zhi 2010, 90, 2755–2758. [Google Scholar] [CrossRef] [PubMed]
- Gorji, R.; Deshaies, E.; Allott, G.; Li, F. Transcranial motor evoked potentials reliably predict changes in cerebral blood flow during methohexital testing. J. Neurosurg. Anesthesiol. 2009, 21, 424–425. [Google Scholar]
- Hattingen, E.; Szelényi, A.; Rathert, J.; Blasel, S.; Zanella, F.; Weidauer, S. Perioperative Läsionen des Tractus corticospinalis. Atiologie, neuroradiologische Befunde und klinischer Verlauf [Perioperative lesions of the corticospinal tract. Etiology, neuroradiological features and clinical outcome]. Radiologe 2009, 49, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Kombos, T.; Picht, T.; Derdilopoulos, A.; Suess, O. Impact of intraoperative neurophysiological monitoring on surgery of high-grade gliomas. J. Clin. Neurophysiol. 2009, 26, 422–425. [Google Scholar] [CrossRef]
- Krammer, M.J.; Wolf, S.; Schul, D.B.; Gerstner, W.; Lumenta, C.B. Significance of intraoperative motor function monitoring using transcranial electrical motor evoked potentials (MEP) in patients with spinal and cranial lesions near the motor pathways. Br. J. Neurosurg. 2009, 23, 48–55. [Google Scholar] [CrossRef]
- Ozawa, N.; Muragaki, Y.; Nakamura, R.; Iseki, H. Identification of the pyramidal tract by neuronavigation based on intraoperative diffusion-weighted imaging combined with subcortical stimulation. Stereotact. Funct. Neurosurg. 2009, 87, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.; Neuloh, G.; von Lehe, M.; Meyer, B.; Schramm, J. Insular gliomas: The case for surgical management. J. Neurosurg. 2009, 110, 685–695. [Google Scholar] [CrossRef]
- Sugita, M.; Kinouchi, H.; Nishiyama, Y.; Kanemaru, K.; Yoshioka, H.; Horikoshi, T. Direct clipping of a thrombosed giant cerebral aneurysm after thrombectomy without bleeding to minimize the temporary occlusion time-technical case report. Neurol. Med. Chir. 2009, 49, 600–603. [Google Scholar] [CrossRef] [PubMed][Green Version]
- von Lehe, M.; Wellmer, J.; Urbach, H.; Schramm, J.; Elger, C.E.; Clusmann, H. Epilepsy surgery for insular lesions. Rev. Neurol. 2009, 165, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, F.; Takahashi, H.; Teramoto, A. Navigation-assisted subcortical mapping: Intraoperative motor tract detection by bipolar needle electrode in combination with neuronavigation system. J. Neurooncol. 2009, 93, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Calancie, B.; Molano, M.R. Alarm criteria for motor-evoked potentials: What’s wrong with the “presence-or-absence” approach? Spine 2008, 33, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Berman, J.I.; Berger, M.S.; Chung, S.W.; Nagarajan, S.S.; Henry, R.G. Accuracy of diffusion tensor magnetic resonance imaging tractography assessed using intraoperative subcortical stimulation mapping and magnetic source imaging. J. Neurosurg. 2007, 107, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Mikuni, N.; Okada, T.; Enatsu, R.; Miki, Y.; Hanakawa, T.; Urayama, S.; Kikuta, K.; Takahashi, J.A.; Nozaki, K.; Fukuyama, H.; et al. Clinical impact of integrated functional neuronavigation and subcortical electrical stimulation to preserve motor function during resection of brain tumors. J. Neurosurg. 2007, 106, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Neuloh, G.; Simon, M.; Schramm, J. Stroke prevention during surgery for deep-seated gliomas. Neurophysiol. Clin. 2007, 37, 383–389. [Google Scholar] [CrossRef]
- Yamaguchi, F.; Takahashi, H.; Teramoto, A. Intra-operative detection of motor pathways using a simple electrode provides safe brain tumor surgery. J. Clin. Neurosci. 2007, 14, 1106–1110. [Google Scholar] [CrossRef] [PubMed]
- Fujiki, M.; Furukawa, Y.; Kamida, T.; Anan, M.; Inoue, R.; Abe, T.; Kobayashi, H. Intraoperative corticomuscular motor evoked potentials for evaluation of motor function: A comparison with corticospinal D and I waves. J. Neurosurg. 2006, 104, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Okada, T.; Mikuni, N.; Miki, Y.; Kikuta, K.; Urayama, S.; Hanakawa, T.; Fushimi, Y.; Yamamoto, A.; Kanagaki, M.; Fukuyama, H.; et al. Corticospinal tract localization: Integration of diffusion-tensor tractography at 3-T MR imaging with intraoperative white matter stimulation mapping--preliminary results. Radiology 2006, 240, 849–857. [Google Scholar] [CrossRef] [PubMed]
- Kamada, K.; Todo, T.; Masutani, Y.; Aoki, S.; Ino, K.; Takano, T.; Kirino, T.; Kawahara, N.; Morita, A. Combined use of tractography-integrated functional neuronavigation and direct fiber stimulation. J. Neurosurg. 2005, 102, 664–672. [Google Scholar] [CrossRef]
- Keles, G.E.; Lundin, D.A.; Lamborn, K.R.; Chang, E.F.; Ojemann, G.; Berger, M.S. Intraoperative subcortical stimulation mapping for hemispherical perirolandic gliomas located within or adjacent to the descending motor pathways: Evaluation of morbidity and assessment of functional outcome in 294 patients. J. Neurosurg. 2004, 100, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Kombos, T.; Suess, O.; Brock, M. Prognostic value of improved intraoperative motor evoked potentials. A case report. Zentralbl. Neurochir. 2004, 65, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Neuloh, G.; Schramm, J. Monitoring of motor evoked potentials compared with somatosensory evoked potentials and microvascular Doppler ultrasonography in cerebral aneurysm surgery. J. Neurosurg. 2004, 100, 389–399. [Google Scholar] [CrossRef] [PubMed]
- Quiñones-Hinojosa, A.; Alam, M.; Lyon, R.; Yingling, C.D.; Lawton, M.T. Transcranial motor evoked potentials during basilar artery aneurysm surgery: Technique application for 30 consecutive patients. Neurosurgery 2004, 54, 916–924; discussion 924. [Google Scholar] [CrossRef] [PubMed]
- Sakuma, J.; Suzuki, K.; Sasaki, T.; Matsumoto, M.; Oinuma, M.; Kawakami, M.; Itakura, T.; Kodama, N. Monitoring and preventing blood flow insufficiency due to clip rotation after the treatment of internal carotid artery aneurysms. J. Neurosurg. 2004, 100, 960–962. [Google Scholar] [CrossRef]
- Signorelli, F.; Guyotat, J.; Mottolese, C.; Schneider, F.; D’Acunzi, G.; Isnard, J. Intraoperative electrical stimulation mapping as an aid for surgery of intracranial lesions involving motor areas in children. Childs. Nerv. Syst. 2004, 20, 420–426. [Google Scholar] [CrossRef]
- Yamamoto, T.; Katayama, Y.; Nagaoka, T.; Kobayashi, K.; Fukaya, C. Intraoperative monitoring of the corticospinal motor evoked potential (D-wave): Clinical index for postoperative motor function and functional recovery. Neurol. Med. Chir. 2004, 44, 170–180; discussion 181–182. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Duffau, H.; Capelle, L.; Denvil, D.; Sichez, N.; Gatignol, P.; Taillandier, L.; Lopes, M.; Mitchell, M.C.; Roche, S.; Muller, J.C.; et al. Usefulness of intraoperative electrical subcortical mapping during surgery for low-grade gliomas located within eloquent brain regions: Functional results in a consecutive series of 103 patients. J. Neurosurg. 2003, 98, 764–778. [Google Scholar] [CrossRef] [PubMed]
- Fukaya, C.; Katayama, Y.; Kobayashi, K.; Kasai, M.; Oshima, H.; Yamamoto, T. Impairment of motor function after frontal lobe resection with preservation of the primary motor cortex. Acta. Neurochir. Suppl. 2003, 87, 71–74. [Google Scholar] [CrossRef]
- Suess, O.; Kombos, T.; Ciklatekerlio, O.; Stendel, R.; Suess, S.; Brock, M. Impact of brain shift on intraoperative neurophysiological monitoring with cortical strip electrodes. Acta. Neurochir. 2002, 144, 1279–1289; discussion 1289. [Google Scholar] [CrossRef] [PubMed]
- Kombos, T.; Suess, O.; Pietilä, T.; Brock, M. Subdural air limits the elicitation of compound muscle action potentials by high-frequency transcranial electrical stimulation. Br. J. Neurosurg. 2000, 14, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Kofler, M.; Morota, N.; Deletis, V. Preserved motor evoked potentials fail to predict functional outcome in quadriplegia because of bilateral lesions of the supplementary motor areas: A brief report. Am. J. Phys. Med. Rehabil. 1999, 78, 66–71. [Google Scholar] [CrossRef]
- Kombos, T.; Suess, O.; Kern, B.C.; Funk, T.; Hoell, T.; Kopetsch, O.; Brock, M. Comparison between monopolar and bipolar electrical stimulation of the motor cortex. Acta. Neurochir. 1999, 141, 1295–1301. [Google Scholar] [CrossRef] [PubMed]
- Rohde, V.; Will, B.E.; Hahn, G.; Bien, S.; Zentner, J. Motorisch evozierte Potentiale während der Embolisation arteriovenöser Malformationen zur Erfassung ischämischer Komplikationen [Motor evoked potentials during embolization of arteriovenous malformations for the detection of ischemic complications]. Zentralbl. Neurochir. 1999, 60, 74–80. [Google Scholar] [PubMed]
- Yingling, C.D.; Ojemann, S.; Dodson, B.; Harrington, M.J.; Berger, M.S. Identification of motor pathways during tumor surgery facilitated by multichannel electromyographic recording. J. Neurosurg. 1999, 91, 922–927. [Google Scholar] [CrossRef]
- Krombach, G.A.; Spetzger, U.; Rohde, V.; Gilsbach, J.M. Intraoperative localization of functional regions in the sensorimotor cortex by neuronavigation and cortical mapping. Comput. Aided. Surg. 1998, 3, 64–73. [Google Scholar] [CrossRef]
- Zentner, J.; Meyer, B. Diagnostic significance of MEP elicited by electrical and magnetoelectric stimulation in acute/subacute supratentorial lesions. Electromyogr. Clin. Neurophysiol. 1998, 38, 33–40. [Google Scholar] [PubMed]
- Kawaguchi, M.; Sakamoto, T.; Ohnishi, H.; Shimizu, K.; Karasawa, J.; Furuya, H. Intraoperative myogenic motor evoked potentials induced by direct electrical stimulation of the exposed motor cortex under isoflurane and sevoflurane. Anesth. Analg. 1996, 82, 593–599. [Google Scholar] [CrossRef]
- Maertens de Noordhout, A.; Born, J.D.; Hans, P.; Remacle, J.M.; Delwaide, P.J. Intraoperative localisation of the primary motor cortex using single electrical stimuli. J. Neurol. Neurosurg. Psychiatry 1996, 60, 442–444. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pechstein, U.; Cedzich, C.; Nadstawek, J.; Schramm, J. Transcranial high-frequency repetitive electrical stimulation for recording myogenic motor evoked potentials with the patient under general anesthesia. Neurosurgery 1996, 39, 335–343; discussion 343–344. [Google Scholar] [CrossRef]
- Rodi, Z.; Deletis, V.; Morota, N.; Vodusek, D.B. Motor evoked potentials during brain surgery. Pflug. Arch. 1996, 431, R291–R292. [Google Scholar] [CrossRef] [PubMed]
- Skirboll, S.S.; Ojemann, G.A.; Berger, M.S.; Lettich, E.; Winn, H.R. Functional cortex and subcortical white matter located within gliomas. Neurosurgery 1996, 38, 678–684; discussion 684–685. [Google Scholar] [CrossRef] [PubMed]
- Ebeling, U.; Schmid, U.D.; Ying, H.; Reulen, H.J. Safe surgery of lesions near the motor cortex using intra-operative mapping techniques: A report on 50 patients. Acta. Neurochir. 1992, 119, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Schramm, J.; Koht, A.; Schmidt, G.; Pechstein, U.; Taniguchi, M.; Fahlbusch, R. Surgical and electrophysiological observations during clipping of 134 aneurysms with evoked potential monitoring. Neurosurgery 1990, 26, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Zentner, J.; Schumacher, M.; Bien, S. Motor evoked potentials during interventional neuroradiology. Neuroradiology 1988, 30, 252–255. [Google Scholar] [CrossRef]
- Chen, D.F.; Willie, J.T.; Cabrera, D.; Bullinger, K.L.; Karakis, I. Continuous Intraoperative Neurophysiological Monitoring of the Motor Pathways Using Depth Electrodes During Surgical Resection of an Epileptogenic Lesion: A Novel Technique. Oper. Neurosurg. 2021, 20, E379–E385. [Google Scholar] [CrossRef] [PubMed]
- Machetanz, K.; Gallotti, A.L.; Leao Tatagiba, M.T.; Liebsch, M.; Trakolis, L.; Wang, S.; Tatagiba, M.; Gharabaghi, A.; Naros, G. Time-Frequency Representation of Motor Evoked Potentials in Brain Tumor Patients. Front. Neurol. 2021, 11, 633224. [Google Scholar] [CrossRef]
- Cattaneo, L.; Giampiccolo, D.; Meneghelli, P.; Tramontano, V.; Sala, F. Cortico-cortical connectivity between the superior and inferior parietal lobules and the motor cortex assessed by intraoperative dual cortical stimulation. Brain. Stimul. 2020, 13, 819–831. [Google Scholar] [CrossRef] [PubMed]
- Kang, P.B.; McMillan, H.J.; Kuntz, N.L.; Lehky, T.J.; Alter, K.E.; Fitzpatrick, K.F.; El Kosseifi, C.; Quijano-Roy, S. Utility and practice of electrodiagnostic testing in the pediatric population: An AANEM consensus statement. Muscle Nerve 2020, 61, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Policicchio, D.; Ticca, S.; Dipellegrini, G.; Doda, A.; Muggianu, G.; Boccaletti, R. Multimodal Surgical Management of Cerebral Lesions in Motor-Eloquent Areas Combining Intraoperative 3D Ultrasound with Neurophysiological Mapping. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2020. [Google Scholar] [CrossRef]
- Shibata, S.; Yamao, Y.; Kunieda, T.; Inano, R.; Nakae, T.; Nishida, S.; Inada, T.; Takahashi, Y.; Kikuchi, T.; Arakawa, Y.; et al. Intraoperative Electrophysiologic Mapping of Medial Frontal Motor Areas and Functional Outcomes. World Neurosurg. 2020, 138, e389–e404. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Li, Z.; Fan, X.; Tao, X.; Qi, L.; Ling, M.; Guo, D.; Qiao, H. A prediction of postoperative neurological deficits following intracranial aneurysm surgery using somatosensory evoked potential deterioration duration. Neurosurg. Rev. 2020, 43, 293–299. [Google Scholar] [CrossRef]
- Zuo, F.; Hu, K.; Kong, J.; Zhang, Y.; Wan, J. Surgical Management of Brain Metastases in the Perirolandic Region. Front. Oncol. 2020, 10, 572644. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. National Library of Medicine (U.S.). (2011 Apr 8- 2013 Nov 9). Early Neurophysiological Interventions in Acute Cerebral Lesions. Identifier NCT04178395. Available online: https://clinicaltrials.gov/ct2/show/NCT04178395?cond=NCT04178395&draw=2&rank=1 (accessed on 22 April 2021).
- Hiruta, R.; Fujii, M.; Furukawa, Y.; Ichikawa, T.; Suzuki, K.; Watanabe, Y.; Nemoto, M.; Sato, T.; Sakuma, J.; Saito, K. Corticospinal Tract Mapping by Calculating the Ratio of Subcortical to Cortical Stimulation Intensity: A Technical Note. No Shinkei Geka. 2019, 47, 957–960. [Google Scholar] [CrossRef] [PubMed]
- Rajan, S.; Sharma, D. Neuroanesthesia and Monitoring for Cranial and Complex Spinal Surgery. In Principles of Neurological Surgery, 4th ed.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 87–102. ISBN 978-03-2343-140-8. [Google Scholar]
- Valci, L.; Dalolio, M.; Kuhlen, D.; Pravatà, E.; Gobbi, C.; Reinert, M. Intradiploic encephalocele of the primary motor cortex in an adult patient: Electrophysiological implications during surgery. J. Neurosurg. 2018, 128, 871–874. [Google Scholar] [CrossRef] [PubMed]
- Abdulrauf, S.I.; Vuong, P.; Patel, R.; Sampath, R.; Ashour, A.M.; Germany, L.M.; Lebovitz, J.; Brunson, C.; Nijjar, Y.; Dryden, J.K.; et al. “Awake” clipping of cerebral aneurysms: Report of initial series. J. Neurosurg. 2017, 127, 311–318. [Google Scholar] [CrossRef]
- Benavides, F.D.; Santamaria, A.J.; Bodoukhin, N.; Guada, L.G.; Solano, J.P.; Guest, J.D. Characterization of Motor and Somatosensory Evoked Potentials in the Yucatan Micropig Using Transcranial and Epidural Stimulation. J. Neurotrauma. 2017, 34, 2595–2608. [Google Scholar] [CrossRef] [PubMed]
- Bharadwaj, S.; Haji, F.; Hebb, M.; Chui, J. Direct motor evoked potentials and cortical mapping using the NIM® nerve monitoring system: A technical note. J. Clin. Neurosci. 2017, 38, 111–113. [Google Scholar] [CrossRef] [PubMed]
- Calancie, B. Intraoperative Neuromonitoring and Alarm Criteria for Judging MEP Responses to Transcranial Electric Stimulation: The Threshold-Level Method. J. Clin. Neurophysiol. 2017, 34, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Grasso, G.; Landi, A.; Alafaci, C. Multimodal Intraoperative Neuromonitoring in Aneurysm Surgery. World.Neurosurg. 2017, 101, 763–765. [Google Scholar] [CrossRef] [PubMed]
- Hemmer, L.B.; Zeeni, C. Intracranial Arteriovenous Malformation Surgery. In Monitoring the Nervous System for Anesthesiologists and Other Health Care Professionals; Springer International Publishing: New York, NY, USA, 2017; pp. 367–376. ISBN 978-33-1946-542-5. [Google Scholar]
- Ku, J.; Mendelsohn, D.; Chew, J.; Shewchuk, J.; Dong, C.; Akagami, R. Ipsilateral Motor Innervation Discovered Incidentally on Intraoperative Monitoring: A Case Report. Neurosurgery 2017, 80, E194–E200. [Google Scholar] [CrossRef]
- Moser, T.; Bulubas, L.; Sabih, J.; Conway, N.; Wildschutz, N.; Sollmann, N.; Meyer, B.; Ringel, F.; Krieg, S.M. Resection of Navigated Transcranial Magnetic Stimulation-Positive Prerolandic Motor Areas Causes Permanent Impairment of Motor Function. Neurosurgery 2017, 81, 99–110. [Google Scholar] [CrossRef]
- Alimohamadi, M.; Shirani, M.; Shariat Moharari, R.; Pour-Rashidi, A.; Ketabchi, M.; Khajavi, M.; Arami, M.; Amirjamshidi, A. Application of Awake Craniotomy and Intraoperative Brain Mapping for Surgical Resection of Insular Gliomas of the Dominant Hemisphere. World Neurosurg. 2016, 92, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Coppola, A.; Tramontano, V.; Basaldella, F.; Arcaro, C.; Squintani, G.; Sala, F. Intra-operative neurophysiological mapping and monitoring during brain tumour surgery in children: An update. Childs. Nerv. Syst. 2016, 32, 1849–1859. [Google Scholar] [CrossRef]
- König, R. Surgical therapy of aneurysms. In Spontaneous Subarachnoid Haemorrhage: Well-Known and New Approaches, 1st ed.; Nova Science Publishers Inc.: New York, NY, USA, 2016; pp. 81–89. ISBN 978-16-3485-270-8. [Google Scholar]
- Raabe, A.; Seidel, K. Prevention of ischemic complications during aneurysm surgery. J. Neurosurg. Sci. 2016, 60, 95–103. [Google Scholar] [PubMed]
- Yao, A.; Sarkiss, C.A.; Lee, J.; Zarzour, H.K.; Shrivastava, R.K. Surgical limitations in convexity meningiomas en-plaque: Is radical resection necessary? J. Clin. Neurosci. 2016, 27, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Ottenhausen, M.; Krieg, S.M.; Meyer, B.; Ringel, F. Functional preoperative and intraoperative mapping and monitoring: Increasing safety and efficacy in glioma surgery. Neurosurg. Focus 2015, 38, E3. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Ikedo, T.; Sano, N.; Okada, Y.; Murata, T. Aneurysm and Vascular Malformations Transcranial electric motor-evoked potentials monitoring for intracranial aneurysm surgery: WSC-1330. Int. J. Stroke 2014, 9, 123. [Google Scholar] [CrossRef]
- Suzuki, K.; Mikami, T.; Sugino, T.; Wanibuchi, M.; Miyamoto, S.; Hashimoto, N.; Mikuni, N. Discrepancy between voluntary movement and motor-evoked potentials in evaluation of motor function during clipping of anterior circulation aneurysms. World Neurosurg. 2014, 82, e739–e745. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.F.; Chen, H.H.; Liang, M.L.; Chen, C.; Chiu, J.W.; Wang, J.C.; Lai, C.J.; Liao, K.K.; Chan, R.C. Intraoperative brain mapping to identify corticospinal projections during resective epilepsy surgery in children with congenital hemiparesis. Child’s Nerv. Syst. 2014, 30, 1559–1564. [Google Scholar] [CrossRef] [PubMed]
- Landazuri, P.; Eccher, M. Simultaneous direct cortical motor evoked potential monitoring and subcortical mapping for motor pathway preservation during brain tumor surgery: Is it useful? J. Clin. Neurophysiol. 2013, 30, 623–625. [Google Scholar] [CrossRef] [PubMed]
- Rajapakse, T.; Kirton, A. Non-invasive brain stimulation in children: Applications and future directions. Transl. Neurosci. 2013, 4, 217–233. [Google Scholar] [CrossRef]
- Yamashita, S.; Sasaki, O.; Suzuki, K.; Takao, T.; Nakamura, K.; Koike, T. Transcranial motor evoked potentials monitoring for cerebral aneurysm surgery. No Shinkei Geka. Neurol. Surg. 2013, 41, 15–24. [Google Scholar]
- Bacigaluppi, S.; Fontanella, M.; Manninen, P.; Ducati, A.; Tredici, G.; Gentili, F. Monitoring techniques for prevention of procedure-related ischemic damage in aneurysm surgery. World Neurosurg. 2012, 78, 276–288. [Google Scholar] [CrossRef] [PubMed]
- De Witt Hamer, P.C.; Robles, S.G.; Zwinderman, A.H.; Duffau, H.; Berger, M.S. Impact of intraoperative stimulation brain mapping on glioma surgery outcome: A meta-analysis. J. Clin. Oncol. 2012, 30, 2559–2565. [Google Scholar] [CrossRef] [PubMed]
- Emerson, R.G.; Adams, D.C. Intraoperative Monitoring by Evoked Potential Techniques. In Aminoff’s Electrodiagnosis in Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2012; pp. 651–670. ISBN 978-14-5570-308-1. [Google Scholar]
- Hotson, G.; Fifer, M.S.; Acharya, S.; Anderson, W.S.; Thakor, N.V.; Crone, N.E. Electrocorticographic decoding of ipsilateral reach in the setting of contralateral arm weakness from a cortical lesion. Annu. Int. Conf. IEEE. Eng. Med. Biol. Soc. 2012, 2012, 4104–4107. [Google Scholar] [CrossRef] [PubMed]
- Ito, Z.; Imagama, S.; Sakai, Y.; Katayama, Y.; Wakao, N.; Ando, K.; Hirano, K.; Tauchi, R.; Muramoto, A.; El Zahlawy, H.; et al. A new criterion for the alarm point for compound muscle action potentials. J. Neurosurg. Spine. 2012, 17, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Gelb, A.W. False negatives, muscle relaxants, and motor-evoked potentials. J. Neurosurg. Anesthesiol. 2011, 23, 64. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Deshaies, E.M.; Allott, G.; Canute, G.; Gorji, R. Direct cortical stimulation but not transcranial electrical stimulation motor evoked potentials detect brain ischemia during brain tumor resection. Am. J. Electroneurodiagnostic. Technol. 2011, 51, 191–197. [Google Scholar] [CrossRef]
- Deiner, S. Highlights of anesthetic considerations for intraoperative neuromonitoring. Semin. Cardiothorac. Vasc. Anesth. 2010, 14, 51–53. [Google Scholar] [CrossRef]
- Pabon, B.; Vargas, S.; Franco, A.; Arias, J.F. Intraoperative neurophysiological monitoring and provocative test during endovascular treatment of avms. Neuroradiol. J. 2010, 23, 333. [Google Scholar]
- Lefaucheur, J.P.; de Andrade, D.C. Intraoperative neurophysiologic mapping of the central cortical region for epidural electrode placement in the treatment of neuropathic pain by motor cortex stimulation. Brain Stimul. 2009, 2, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Fu, W.; Wang, D.; Wang, Y. Ipsilateral responses of motor evoked potential correlated with the motor functional outcomes after cortical resection. Int. J. Psychophysiol. 2009, 73, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Duffau, H. Intraoperative neurophysiology during surgery for cerebral tumor. In Handbook of Clinical Neurophysiology; Elsevier: Amsterdam, The Netherlands, 2008; pp. 491–507. ISBN 978-04-4451-824-8. [Google Scholar]
- Duffau, H. New insights into functional mapping in cerebral tumor surgery. In New Insights into Functional Mapping in Cerebral Tumor Surgery, 1st ed.; Nova Science Publishers Inc.: New York, NY, USA, 2008; pp. 1–95. ISBN 978-16-0692-136-4. [Google Scholar]
- Takashima, K.; Takahashi, M.; Yubune, N.; Inaba, N.; Omoto, K.; Kawano, M.; Sakurabayashi, I.; Ishikawa, M.; Kusaka, G.; Shinoda, S. Evoked potential monitoring in an operation of neurosurgery. Rinsho Byori 2008, 56, 475–485. [Google Scholar] [PubMed]
- Duffau, H. Contribution of cortical and subcortical electrostimulation in brain glioma surgery: Methodological and functional considerations. Neurophysiol. Clin. 2007, 37, 373–382. [Google Scholar] [CrossRef]
- Tharin, S.; Golby, A. Functional brain mapping and its applications to neurosurgery. Neurosurgery 2007, 60, 185–201; discussion 201–202. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Duffau, H. New concepts in surgery of WHO grade II gliomas: Functional brain mapping, connectionism and plasticity—A review. J. Neurooncol. 2006, 79, 77–115. [Google Scholar] [CrossRef] [PubMed]
- Schramm, J.; Neuloh, G. Brain surgery and endangared motor function: What MEP monitoring adds to mapping techniques. Riv. Med. 2006, 12, 67. [Google Scholar]
- Shinoura, N.; Suzuki, Y.; Yamada, R.; Kodama, T.; Takahashi, M.; Yagi, K. Restored activation of primary motor area from motor reorganization and improved motor function after brain tumor resection. AJNR Am. J. Neuroradiol. 2006, 27, 1275–1282. [Google Scholar] [PubMed]
- Kuzniecky, R.I.; Jackson, G.D. Extra-temporal lobe epilepsy. In Magnetic Resonance in Epilepsy; Elsevier: Amsterdam, The Netherlands, 2005; pp. 177–196. ISBN 978-01-2431-152-7. [Google Scholar]
- Binder, D.K.; Lyon, R.; Manley, G.T. Transcranial motor evoked potential recording in a case of Kernohan’s notch syndrome: Case report. Neurosurgery 2004, 54, 999–1002; discussion 1002–1003. [Google Scholar] [CrossRef] [PubMed]
- Hashiguchi, K.; Morioka, T.; Fukui, K.; Kawamura, T.; Shono, T.; Sakaki, T. Postoperative transient hemiplegia after resection of the medial frontal tumor involving the supplementary motor area: Report of two cases. No Shinkei Geka. Neurol. Surg. 2004, 32, 947–953. [Google Scholar]
- Kondo, R.; Saito, S.; Kuroki, A.; Sato, S.; Katakura, K.; Kayama, T. Significance and usefulness of corticospinal motor evoked potential monitoring for lesions adjacent to primary motor cortex. No To Shinkei 2004, 56, 496–502. [Google Scholar] [PubMed]
- Neuloh, G.; Schramm, J. Motor evoked potential monitoring for the surgery of brain tumours and vascular malformations. Adv. Tech. Stand. Neurosurg. 2004, 29, 171–228. [Google Scholar] [CrossRef] [PubMed]
- Di Lazzaro, V.; Oliviero, A.; Profice, P.; Ferrara, L.; Saturno, E.; Pilato, F.; Tonali, P. The diagnostic value of motor evoked potentials. Clin. Neurophysiol. 1999, 110, 1297–1307. [Google Scholar] [CrossRef]
- Calancie, B.; Harris, W.; Broton, J.G.; Alexeeva, N.; Green, B.A. ”Threshold-level” multipulse transcranial electrical stimulation of motor cortex for intraoperative monitoring of spinal motor tracts: Description of method and comparison to somatosensory evoked potential monitoring. J. Neurosurg. 1998, 88, 457–470. [Google Scholar] [CrossRef]
- Reinhardt, H.F.; Trippel, M.; Westermann, B.; Horstmann, G.A.; Gratzl, O. Computer assisted brain surgery for small lesions in the central sensorimotor region. Acta. Neurochir. 1996, 138, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Newlon, P.G.; Greenberg, R.P. Evoked potentials in severe head injury. J. Trauma. 1984, 24, 61–66. [Google Scholar] [CrossRef] [PubMed]
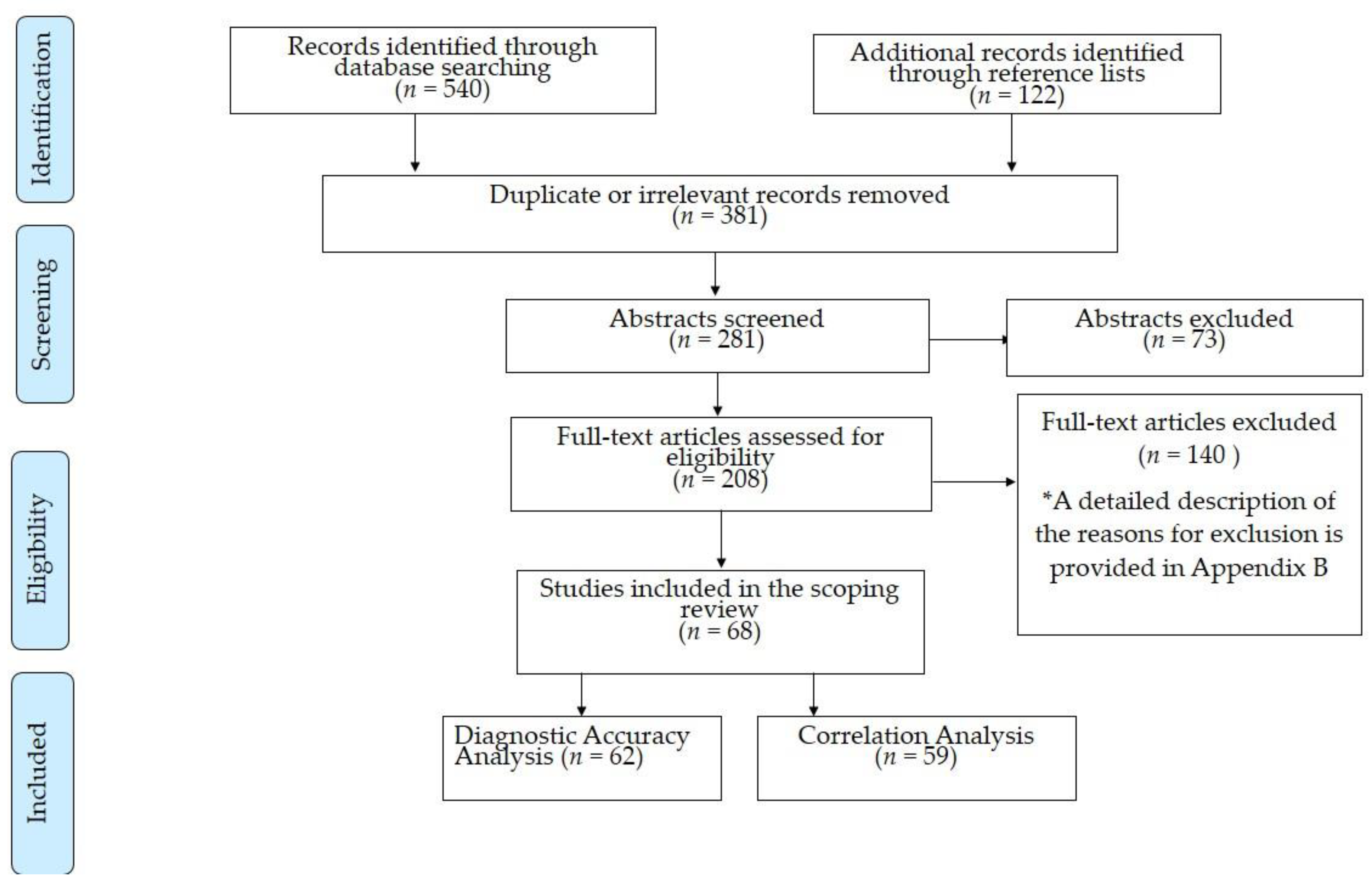

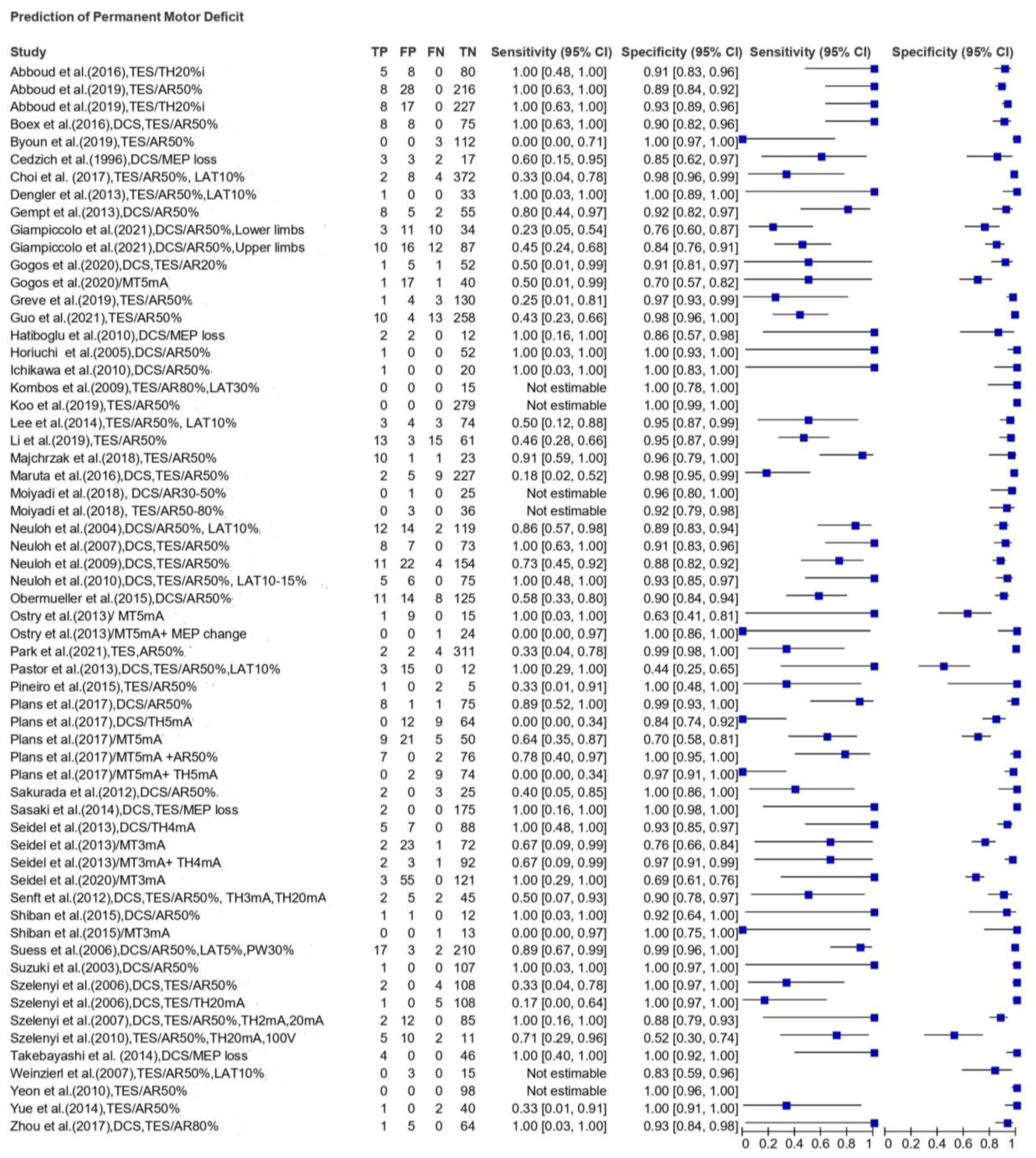
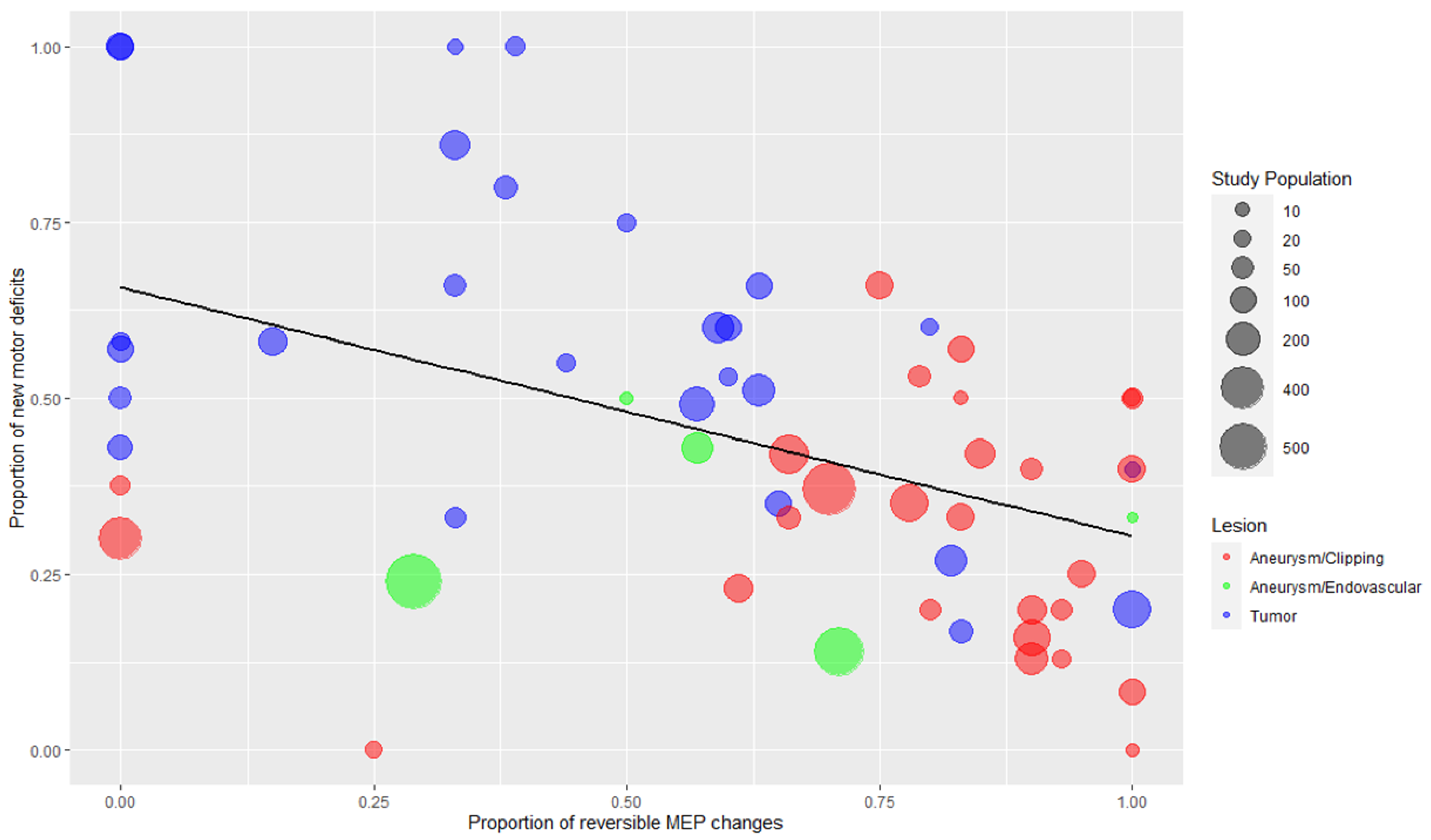
| Authors | No. of Patients | Study Design/ Country | STT | Warning Criterion | MEP Changes | Postoperative Motor Deficit in Relation to MEP Change | |
|---|---|---|---|---|---|---|---|
| Transient * | Permanent * | ||||||
| TUMORS AND OTHER BRAIN LESIONS | |||||||
| Giampiccolo et al. (2021) [29] | 125 | Retrospective Italy | DCS | AR > 50% | Upper Limbs AR/loss (n = 26) | 2d: 3/26 (11.5%) 5 d: 6/26 (23%) | 10/26 (38.5%) |
| Lower Limbs AR/loss (n = 14) | 2 d: 2/14 (14.3%) 5 d: 3/14 (21.4%) | 3/14 (21.4%) | |||||
| Gogos et al. (2020) [30] | 58 | Prospective USA | DCS TES ScS | AR > 20% MT ≤ 5 mA | IRR AR (n = 6) | 2/6 (33.3%) | 1/6 (16.6%) |
| MT ≤ 5 mA (n = 18) | 2/18 (11.1%) | 1/18 (5.5%) | |||||
| Mammadk-hanli et al. (2020) [31] | 145 | Retrospective Turkey | DCS | AR > 50% LTI > 10% | REV changes (n = 7) | 4/7 (57.1%), not specified if transient or permanent | |
| IRR changes (n = 14) | 14/14 (100%), not specified if transient or permanent | ||||||
| Seidel et al. (2020) [32] | 182 | Prospective Switzerland | DCS ScS | THI ≥ 4 mA MT ≤ 3 mA | MT ≤ 3 mA (n = 58) | 24 h: 13/58 (22.4%) discharge: 14/58 (24.1%) | 3/58 (5.1%) |
| MT ≤ 3 mA+ IRR THI/loss (n = 3) | - | 3/3 (100%) | |||||
| Abboud et al. (2019) [33] | 126 | Prospective Germany | TES | AR > 50% THI > 20%i | REV AR (n = 2) | - | - |
| IRR AR (n = 36) | 24 h: 6/36 (16.7%) discharge: 6/36 (16.7%) | 8/36 (22.2%) | |||||
| REV THI (n = 9) | - | - | |||||
| IRR THI (n = 25) | 24 h: 7/25 (28.0%) discharge: 7/25 (28.0%) | 8/25 (32.0%) | |||||
| Majchrzak et al. (2018) [34] | 35 | Prospective Poland | TES | AR > 50% | REV AR (n = 7) | 6/7 (85.7%) | 1/7 (14.3%) |
| IRR AR (n = 11) | 1/11 (9.1%) | 10/11 (90.9%) | |||||
| Moiyadi et al. (2018) [35] | 39 | Prospective India | DCS TES ScS | TES:AR > 50–80% DCS:AR > 30–50% MT ≤ 10 mA | TESIRR AR (n = 1) IRR loss (n = 2) | - ½ (50.0%) | - - |
| DCS REV AR (n = 1) REV loss (n = 1) IRR loss (n = 1) | - - 1/1 (100%) | - - - | |||||
| MT ≤ 10 mA (n = 13) | 4/13 (30.8%) | - | |||||
| MT ≤ 10 mA + AR/loss (n = 3) | 2/3 (66.6%) | - | |||||
| Plans et al. (2017) [36] | 92 | Retrospective Spain | DCS ScS | AR > 50% THI ≥ 5 mA MT ≤ 5 mA | IRR THI (n = 12) | 24 h: 4/12 (33.3%) | - |
| IRR AR (n = 2) | - | 2/2 (100%) | |||||
| IRR loss (n = 7) | - | 6/7 (85.7%) | |||||
| MT ≤ 5 mA (n = 30) | 24 h: 2/30 (6.7%) | 9/30 (30.0%) | |||||
| MT ≤ 5 mA + AR (n = 7) | - | 7/7 (100%) | |||||
| MT ≤ 5 mA + THI (n = 2) | 24 h: 2/2 (100%) | - | |||||
| MT ≤ 5 mA + THI/AR (n = 9) | 24 h: 2/9 (22.2%) | 7/9 (77.8%) | |||||
| Zhou et al. (2017) [37] | 70 | Retrospective China | DCS TES | AR > 80% | AR/loss (n = 6) | 5/6 (83.3%) | 1/6 (16.7%) |
| Abboud et al. (2016) [17] | 93 | Prospective Germany | TES | THI > 20%i | IRR THI (n = 13) | 8/13 (61.5%) | 5/13 (38.5%) |
| Boex et al. (2016) [38] | 104 | Retrospective Switzerland | DCS TES | AR > 50% | IRR AR/loss (n = 16) | 1 d: 5/16 (31.3%) discharge: 3/16 (18.8%) | 8/16 (50.0%) |
| Obermueller et al. (2015) [23] | 105 gliomas | Retrospective Germany | DCS | AR > 50% | REV AR (n = 85) | 14/85 (16.5%) | 5/85 (5.9%) |
| IRR AR (n = 11) | 2/11 (18.2%) | 8/11 (72.7%) | |||||
| 53 metastases | DCS | AR > 50% | REV AR (n = 32) | 5/32 (15.6%) | 2/32 (6.3%) | ||
| IRR AR/loss (n = 14) | - | 3/14 (21.4%) | |||||
| Shiban et al. (2015) [39] | 14 | Prospective Germany | DCS ScS | AR > 50% MT ≤ 3 mA | REV loss (n = 1) | 1/1 (100%) | - |
| IRR loss (n = 2) | 1/2 (50.0%) | 1/2 (50.0%) | |||||
| Lee et al. (2014) [40] | 84 | Retrospective Korea | TES | AR > 50% LTI > 10% | IRR AR (n = 7) | - | 3/7 (42.9%) |
| Gempt et al. (2013) [41] | 70 | Prospective Germany | DCS | AR > 50% | REV AR (n = 8) | 2/8 (25.0%) | 2/8 (25.0%) |
| IRR AR (n = 13) | 5/13 (38.5%) | 8/13 (61.5%) | |||||
| Ostrý et al. (2013) [42] | 25 | Prospective Czech Republic | DCS ScS | THI ≥ 2 mA MT ≤ 5 mA | THI (n = 6) | 4/6 (66.6%) | - |
| MT ≤ 5 mA (n = 10) | 3/10 (30.0%) | 1/10 (10%) | |||||
| MT ≤ 5 mA + MEP alteration (n = 2) | 2/2 (100%) | - | |||||
| Pastor et al. (2013) [43] | 30 | Prospective Spain | DCS TES | AR > 50% LTI > 10% | TES (n = 16) | 1 w: 4/16 (25.0%) | 3/16 (18.8%) |
| DCS (n = 2) | - | - | |||||
| Seidel et al. (2013) [8] | 100 | Prospective Switzerland | DCS ScS | THI ≥ 4 mA MT ≤ 3 mA | THI ≤ 15 min/unspecific changes (n = 18) | 24 h: 5/18 (27.8%) Discharge: 2/18 (11.1%) | - |
| THI ≥ 15 min (n = 8) | 24 h: 2/8 (25.0%) Discharge: 3/8 (37.5%) | 2/8 (25.0%) | |||||
| Loss ≥15 min (n = 4) | Discharge: 1/4 (25.0%) | 3/4 (75.0%) | |||||
| MT ≤ 3 mA (n = 25) | 24 h: 4/25 (16.0%) Discharge: 2/25 (8.0%) | 2/25 (8.0%) | |||||
| MT ≤ 3 mA+ THI ≥ 15 min/Loss ≥15 min (n = 5) | 24 h: 1/5 (20.0%) Discharge: 2/5 (40.0%) | 2/5 (40.0%) | |||||
| Sakurada et al. (2012) [44] | 30 | Retrospective Japan | DCS | AR > 50% | REV AR (n = 2) | 1/2 (50.0%) | - |
| IRR AR (n = 2) | - | 2/2 (100%) | |||||
| Senft et al. (2012) [45] | 54 | Retrospective Germany | TESDCS | AR > 50% THI ≥ 20 mA (TES) THI ≥ 3 mA (DCS) | MEP alterations (n = 7: 2 THI, 1 AR, 1 loss, 3 N/A) | 4/7 (57.1%) | 2/7 (28.6%) |
| Hatiboglu et al. (2010) [46] | 16 | Retrospective USA | DCS | MEP loss | Loss (n = 4) | 1/4 (25.0%) | 2/4 (50.0%) |
| Ichikawa et al. (2010) [47] | 21 | Retrospective Japan | DCS | AR > 50% | REV AR (n = 3) | 1/3 (33.3%) | - |
| REV loss (n = 1) | 1/1 (100%) | - | |||||
| IRR loss (n = 1) | - | 1/1 (100%) | |||||
| Szelényi et al. (2010) # [48] | 25 | Prospective Germany | TES | AR > 50% THI > 20 mA or >100 V | REV AR (n = 3) | - | - |
| IRR AR (n = 2) | 2/2 (100%) | - | |||||
| REV loss (n = 6) | 2/6 (33.3%) | 2/6 (33.3%) | |||||
| IRR loss (n = 5) | 2/5 (40.0%) | 2/5 (40.0%) | |||||
| REV THI (n = 3) | - | - | |||||
| IRR THI (n = 8) | 2/8 (25.0%) | 3/8 (37.5%) | |||||
| Kombos et al. (2009) [49] | 15 | Prospective Germany | TESScS | AR > 80% LTI > 30% MT ≤ 3 mA | REV AR + LTI (n = 5) | 2/5 (40.0%) | - |
| Neuloh et al. (2009) [50] | 191 | Prospective Germany | DCS TES | AR > 50% | REV AR (n = 50) | 19/50 (38.0%) | 1/50 (2.0%) |
| REV loss (n = 7) | 2/7 (28.6%) | 1/7 (14.3%) | |||||
| IRR AR (n = 26) | 11/26 (42.3%) | 5/26 (19.2%) | |||||
| IRR loss (n = 7) | 1/7 (14.3%) | 6/7 (85.7%) | |||||
| Neuloh et al. (2007) [51] | 88 | Prospective Germany | DCS TES | AR > 50% | REV AR/loss (n = 26) | 12/26 (46.2%) | - |
| IRR AR (n = 8) | 7/8 (87.5%) | 1/8 (12.5%) | |||||
| IRR loss (n = 7) | - | 7/7 (100%) | |||||
| Suess et al. (2006) [15] | 232 | Unclear Germany | DCS | AR > 50% LTI > 5% PWI > 30% | REV changes(n = 27) | 6/27 (22.2%) | - |
| IRR changes (n = 20) | - | 17/20 (85.0%) | |||||
| Neuloh et al. (2004) [11] | 159 | Prospective Germany | DCS | AR > 50% LTI > 10% | REV AR (n = 16) | 8/16 (50.0%) | 1/16 (6.3%) |
| IRR AR (n = 16) | 7/16 (43.8%) | 4/16 (25.0%) | |||||
| REV loss (n = 22) | 8/22 (36.4%) | 1/22 (4.5%) | |||||
| IRR loss (n = 10) | 2/10 (20.0%) | 8/10 (80.0%) | |||||
| Kombos et al. (2001) [10] | 70 | Prospective Germany | DCS | AR > 80% LTI > 15% | REV LTI (n = 3) | - | - |
| IRR LTI (n = 1) | 1/1 (100%), not specified if transient orpermanent | ||||||
| REV loss (n = 7) | - | - | |||||
| IRR loss (n = 1) | - | 1/1 (100%) | |||||
| Zhou et al. (2001) [52] | 50 | Prospective USA | TES | AR > 50% | REV AR (n = 4) | - | |
| IRR AR/loss (n = 8) | 8/8 (100%), not specified if transient orpermanent | ||||||
| Cedzich et al. (1996) [53] | 25 | Prospective Germany | DCS | MEP loss | REV loss (n = 9) | 4/9 (44.4%) | 1/9 (11.1%) |
| IRR loss (n = 6) | - | 3/6 (50.0%) | |||||
| EPILEPSY SURGERY | |||||||
| Koo et al. (2019) [54] | 279 | Prospective Korea | TES | AR > 50% | REV AR (n = 6) | 1/6 (16.7%) | - |
| REV loss (n = 4) | 1/4 (25.0%) | - | |||||
| Neuloh et al. (2010) [55] | 86 | Prospective Germany | DCSTES | AR > 50% LTI > 10–15% | REV changes (n = 20) | 4/20 (20.0%) | - |
| IRR changes (n = 11) | 2/11 (18.2%) | 5/11 (45.5%) | |||||
| Authors | No. of Patients | Study Design | STT | Warning Criterion | MEP Changes | Postoperative Motor Deficit in Relation to MEP Change | |
|---|---|---|---|---|---|---|---|
| Transient * | Permanent * | ||||||
| ANEURYSM CLIPPING | |||||||
| Guo et al. (2021) [56] | 285 | Retrospective China | TES | AR > 50% | REV AR/loss (n = 49) | 5/49 (10.2%) | 6/49 (12.2%) |
| IRR AR/loss (n = 14) | 1/14 (7.1%) | 10/14 (71.4%) | |||||
| Park et al. (2021) [57] | 319 | Retrospective Korea | TES | AR > 50% | REV AR (n = 1) | 1/1 (100%) | - |
| IRR AR (n = 3) | 2/3 (66.6%) | 1/3 (33.3%) | |||||
| IRR loss (n = 1) | - | 1/1 (100%) | |||||
| You et al. (2021) [58] | 138 | Retrospective China | TES | AR > 50% | REV AR (n = 28) | 11/28 (39.3%), not specified if transient or permanent | |
| IRR loss (n = 5) | 3/5 (60.0%), not specified if transient or permanent | ||||||
| Kameda et al. (2020) [59] | 42 | Retrospective Japan | DCS TES | AR > 50% | REV AR (n = 2) | 1/2 (50.0%) | - |
| Byoun et al. (2019) [22] | 115 | Retrospective Korea | TES | AR > 50% | REV AR (n = 5) | - | 2/5 (40.0%) |
| Greve et al. (2019) [60] | 133 | Retrospective Germany | TES | AR > 50% | REV AR (n = 8) | 1/8 (12.5%) | 1/8 (12.5%) |
| IRR AR (n = 4) | - | - | |||||
| IRR AR (n = 1) | - | 1/1 (100%) | |||||
| Li et al. (2019) [61] | 92 | Retrospective China | TES | AR > 50% | REV AR/loss (n = 76) | 24 h: 3/76 (3.9%) 1 w: 19/76 (25%) | 15/76 (19.7%) |
| IRR AR (n = 11) | 1 w: 1/11 (9.1%) | 9/11 (81.8%) | |||||
| IRR loss (n = 5) | 1 w: 1/5 (20.0%) | 4/5 (80.0%) | |||||
| Choi et al. (2017) [12] | 386 | Retrospective Korea | TES | AR > 50% LTI > 10% | REV AR (n = 4) | - | - |
| REV loss (n = 5) | 1/5 (20.0%) | 1/5 (20.0%) | |||||
| IRR loss (n = 1) | - | 1/1(100%) | |||||
| Komatsu et al. (2017) [62] | 9 | Retrospective Japan | DCS | AR > 50% | REV AR (n = 5) | - | - |
| Staarman et al. (2017) [63] | 123 | Retrospective USA | TES | AR > 50% | REV AR (n = 9 aneurysms) | 1/9 (11.1%) | N/A |
| IRR AR (n = 1 aneurysm) | 1/1 (100%) | N/A | |||||
| Kim et al. (2016) [64] | 685 | Retrospective Korea | TES | AR > 50% | REV AR (n = 30) | 10/30 (33.3%), not specified if transient or permanent | |
| IRR AR (n = 13) | 6/13 (46.2%), not specified if transient or permanent | ||||||
| Maruta et al. (2016) [65] | 243 | Retrospective Japan | DCS TES | AR > 50% (sMEP + mMEP) | REV AR (n = 47) | 2/47 (4.2%) | 1/47 (2.1%) |
| IRR AR (n = 5) | - | - | |||||
| REV loss (n = 19) | 3/19 (15.7%) | 4/19 (21.0%) | |||||
| IRR loss (n = 2) | - | 2/2 (100%) | |||||
| Song et al. (2015) [66] | 11 | Unclear China | TES | AR > 50% | REV AR (n = 5) | 2/5 (40.0%) | N/A |
| IRR AR (n = 1) | 1/1 (100%) | N/A | |||||
| Sasaki et al. (2014) [67] | 177 | Prospective Japan | DCS TES | MEP loss | REV loss (n = 20) | 1/20 (5.0%) | - |
| IRR loss (n = 2) | - | 2/2 (100%) | |||||
| Takebayashi et al. (2014) [68] | 50 | Unclear Japan | DCS | MEP loss | REV loss (n = 15) | 6/15 (40.0%) | - |
| IRR loss (n = 4) | - | 4/4 (100%) | |||||
| Yue et al. (2014) [69] | 43 | Prospective China | TES | AR > 50% | REV AR (n = 5) | Immediate: 1/5 (20.0%) | - |
| REV loss (n = 9) | - | 1/9 (11.1%) | |||||
| IRR loss (n = 1) | - | 1/1 (100%) | |||||
| Dengler et al. (2013) [70] | 30 | Prospective Germany | TES | AR > 50% LTI > 10% | REV changes (n = 14 cases) | 1/14 (7.1%) | - |
| IRR changes (n = 1 case) | - | 1/1 (100%) | |||||
| Kang et al. (2013) [71] | 37 | Unclear China | TES | AR > 50% | AR (n = 8) | 3/8 (37.5%) | N/A |
| Maruta et al. (2012) [72] | 22 | Prospective Japan | DCS TES | AR > 50% | REV AR (n = 1) | - | - |
| REV loss (n = 3) | 2/3 (66.6%) | - | |||||
| Shi et al. (2012) [73] | 68 | Unclear China | TES | AR > 50% | REV AR (n = 6) | - | - |
| IRR AR (n = 3) | - | 3/3 (100%) | |||||
| Motoyama et al. (2011) [74] | 48 | Retrospective Japan | DCSTES | AR > 50% | REV AR (n = 2) | - | N/A |
| REV loss (n = 2) | - | N/A | |||||
| IRR loss (n = 1) | 1/5 (20.0%), < 24 h | N/A | |||||
| Irie et al. (2010) [75] | 110 | Retrospective Japan | TES | AR > 50% THI > 20 mA | REV AR (n = 2) | - | - |
| REV +IRR loss (n = 4) | 2/4 (50.0%) | - | |||||
| Yeon et al. (2010) [76] | 98 | Prospective Japan | TES | AR > 50% | REV AR (n = 4) | - | - |
| REV loss (n = 8) | 1/8 (12.5%) | - | |||||
| Szelényi et al. (2007) [77] | 108 | Prospective and Retrospective Germany/USA | DCS TES | AR > 50% THI > 20 mA(TES) THI > 2 mA(DCS) | TES changes (n = 9: 1 IRR THI, 1 REV AR, 6 REV loss, 1 IRR loss) | 3/9 (33.3%) | - |
| DCS changes (n = 13: 1 REV THI, 3 IRR THI, 2 REV AR, 6 REV loss, 1 IRR loss) | - | 2/13 (15.4%) | |||||
| Weinzierl et al. (2007) [78] | 18 | Prospective Germany | TES | AR > 50% LTI > 10% | REV AR (n = 8) | - | - |
| IRR AR (n = 3) | - | - | |||||
| Szelényi et al. (2006) £ [16] | 116 | Prospective and Retrospective Germany | DCS TES | AR > 50% THI > 20 mA | REV loss (n = 8) | 1/8 (12.5%) | 3/8 (37.5%) |
| IRR loss (n = 2) | - | 2/2 (100%) | |||||
| REV THI (n = 1) | 1/1 (100%) | - | |||||
| IRR THI (n = 1) | - | 1/1 (100%) | |||||
| Horiuchi et al. (2005) [79] | 53 | Prospective Japan | DCS | AR > 50% | REV AR (n = 3) | - | - |
| REV loss (n = 6) | 3/6 (50.0%) | - | |||||
| IRR loss (n = 1) | - | 1/1 (100%) | |||||
| Suzuki et al. (2003) [19] | 108 | Prospective Japan | DCS | AR > 50% | REV changes (n = 19) | 4/19 (21.0%): * < 24 h, REV loss | - |
| IRR loss (n = 1) | - | 1/1 (100%) | |||||
| ENDOVASCULAR PROCEDURES FOR ANEURYSMS | |||||||
| Nakagawa et al. (2020) [80] | 164 | Retrospective Japan | TES | AR > 50% | REV AR (n = 3) | - | N/A |
| IRR AR (n = 2) | 2/2 (100%) | N/A | |||||
| REV loss (n = 1) | - | N/A | |||||
| IRR loss (n = 1) | 1/1 (100%) | N/A | |||||
| Wilent et al. (2020) [81] | 763 | Retrospective USA | TES | AR >40% | IRR AR (n = 36) | 12/36 (33.3%) | N/A |
| REV AR (n = 15) | - | N/A | |||||
| Lee et al. (2019) [82] | 561 | Retrospective Korea | TES | AR > 50% LTI > 10% | REV AR (n = 5) | - | N/A |
| IRR AR (n = 1) | - | N/A | |||||
| IRR loss (n = 1) | 1/1 (100%) | N/A | |||||
| Piñeiro et al. (2015) [83] | 8 | Prospective Spain | TES | AR > 50% | REV AR (n = 1) | - | - |
| IRR AR (n = 1) | - | 1/1 (100%) | |||||
| Hiraishi et al. (2011) [84] | 7 | Unclear Japan | TES | AR > 50% | REV AR (n = 3) | 1/3 (33.3%) | N/A |
| CASE REPORTS | |||||||
| Iwasaki et al. (2013) [85] | 2 (1 awake) | Case report Japan | TES | AR > 50% | Absence of MEP AR > 50% for >10 min after clipping as an indicator for the preservation of the long insular artery | ||
| Szelényi et al. (2003) [86] | 1 | Case report Germany | DCS TES | MEP loss | Arteriosclerotic aneurysm wall preventing the complete closure of the clip. REV loss and immediate postoperative hemiplegia still present at discharge (1 month). | ||
| Authors | Total No. of Patients (n) | No. of All MEP Changes (n) | No. of All New Motor Deficits (n) | No. of Permanent Motor Deficits (n) | No. of All MEP Changes/Total No of Patients (%) | No. of Reversible MEP Changes/No of All MEP Changes (%) | No. of Irreversible MEP Changes/No of All MEP Changes (%) | No. of Permanent Motor Deficits/Total No of Patients (%) | |
|---|---|---|---|---|---|---|---|---|---|
| TUMORS AND OTHER BRAIN LESIONS | |||||||||
| Giampiccolo et al. (2021) [29] | 125 | UL | 26 | 63 | 22 | 21% | N/A | N/A | 18% |
| 125 | LL | 14 | 21 | 13 | 11% | N/A | N/A | 10% | |
| Gogos et al. (2020) [30] | 58 | 6 | 6 | 2 | 10% | 0% | 100% | 3% | |
| Mammadk-hanli et al. (2020) [31] | 145 | 21 | N/A | N/A | 14% | 33% | 67% | N/A | |
| Seidel et al. (2020) [32] | 182 | N/A | 56 | 3 | N/A | N/A | N/A | 2% | |
| * Abboud et al. (2019) [33] | 126 | 72 | 44 | 18 | 14% | 15% | 85% | 4% | |
| Majchrzak et al. (2018) [34] | 35 | 18 | 18 | 11 | 51% | 39% | 61% | 31% | |
| Moiyadi et al. (2018) [35] | 39 | 6 | 7 | 0 | 15% | 33% | 67% | 0% | |
| ** Plans et al. (2017) [36] | 92 | 21 | 18 | 9 | 23% | 0% | 100% | 11% | |
| Zhou et al. (2017) [37] | 70 | 6 | 10 | 1 | 9% | N/A | N/A | 1% | |
| Abboud et al. (2016) [17] | 93 | 13 | 13 | 5 | 13% | 0% | 100% | 5% | |
| Boex et al. (2016) [38] | 104 | 16 | 19 | 8 | 18% | 0% | 100% | 8% | |
| Obermueller et al. (2015) [23] | 158 | 142 | 43 | 19 | 90% | 82% | 18% | 12% | |
| Shiban et al. (2015) [39] | 14 | 3 | 5 | 1 | 21% | 33% | 67% | 7% | |
| Lee et al. (2014) [40] | 84 | 7 | 14 | 6 | 8% | 0% | 100% | 7% | |
| Gempt et al. (2013) [41] | 70 | 21 | 23 | 10 | 30% | 38% | 62% | 14% | |
| Ostrý et al. (2013) [42] | 25 | 6 | 8 | 1 | 24% | N/A | N/A | 4% | |
| Pastor et al. (2013) [43] | 30 | 12 | 8 | 3 | 40% | 0% | 100% | 10% | |
| Seidel et al. (2013) [8] | 100 | 30 | 30 | 5 | 30% | 60% | 40% | 5% | |
| Sakurada et al. (2012) [44] | 30 | 4 | 7 | 5 | 13% | 50% | 50% | 17% | |
| Senft et al. (2012) [45] | 54 | 7 | 11 | 4 | 13% | N/A | N/A | 7% | |
| Hatiboglu et al. (2010) [46] | 16 | 4 | 8 | 2 | 25% | N/A | N/A | 13% | |
| Ichikawa et al. (2010) [47] | 21 | 5 | 3 | 1 | 24% | 80% | 20% | 5% | |
| * Szelényi et al. (2010) [48] | 25 | 27 | 15 | 7 | 96% | 44% | 56% | 25% | |
| Kombos et al. (2009) [49] | 15 | 5 | 2 | 0 | 33% | 100% | 0% | 0% | |
| Neuloh et al. (2009) [50] | 191 | 90 | 52 | 15 | 47% | 63% | 37% | 8% | |
| Neuloh et al. (2007) [51] | 88 | 41 | 27 | 8 | 47% | 63% | 37% | 9% | |
| Suess et al. (2006) [15] | 232 | 47 | 35 | 19 | 20% | 57% | 43% | 8% | |
| Neuloh et al. (2004) [11] | 159 | 64 | 61 | 14 | 40% | 59% | 41% | 9% | |
| Kombos et al. (2001) [10] | 70 | 12 | 8 | N/A | 17% | 83% | 17% | N/A | |
| Zhou et al. (2001) [52] | 50 | 12 | 8 | N/A | 24% | 33% | 67% | N/A | |
| Cedzich et al. (1996) [53] | 25 | 15 | 9 | 5 | 60% | 60% | 40% | 20% | |
| EPILEPSY SURGERY | |||||||||
| Koo et al. (2019) [54] | 279 | 10 | 2 | 0 | 4% | 100% | 0% | 0% | |
| Neuloh et al. (2010) [55] | 86 | 31 | 11 | 5 | 36% | 65% | 35% | 6% | |
| ANEURYSM CLIPPING | |||||||||
| Guo et al. (2021) [56] | 285 | 63 | 32 | 23 | 22% | 78% | 22% | 8% | |
| Park et al. (2021) [57] | 319 | 12 | 10 | 6 | 4% | 67% | 33% | 2% | |
| You et al. (2021) [58] | 138 | 33 | 17 | N/A | 24% | 85% | 15% | N/A | |
| Kameda et al. (2020) [59] | 42 | 2 | 2 | 0 | 5% | 100% | 0% | 0% | |
| Byoun et al. (2019) [22] | 115 | 5 | 3 | 3 | 4% | 100% | 0% | 3% | |
| Greve et al. (2019) [60] | 133 | 13 | 9 | 4 | 9% | 61% | 39% | 3% | |
| Li et al.(2019) [61] | 92 | 92 | 52 | 28 | 100% | 83% | 17% | 30% | |
| Choi et al. (2017) [12] | 386 | 10 | 8 | 6 | 3% | 0% | 100% | 2% | |
| Komatsu et al. (2017) [62] | 9 | 5 | 0 | 0 | 56% | 100% | 0% | 0% | |
| Staarman et al. (2017) [63] | 123 | 10 | 3 | N/A | 8% | 90% | 10% | N/A | |
| Kim et al. (2016) [64] | 685 | 43 | 36 | N/A | 6% | 70% | 30% | N/A | |
| Maruta et al. (2016) [65] | 243 | 73 | 18 | 11 | 30% | 90% | 10% | 5% | |
| Song et al. (2015) [66] | 11 | 6 | 3 | N/A | 55% | 83% | 17% | N/A | |
| Sasaki et al. (2014) [67] | 177 | 22 | 6 | 2 | 12% | 90% | 10% | 1% | |
| Takebayashi et al. (2014) [68] | 50 | 19 | 10 | 4 | 38% | 79% | 21% | 8% | |
| Yue et al. (2014) [69] | 43 | 15 | 4 | 3 | 35% | 93% | 7% | 7% | |
| * Dengler et al. (2013) [70] | 30 | 15 | 2 | 1 | 44% | 93% | 7% | 3% | |
| Kang et al. (2013) [71] | 37 | 8 | 3 | N/A | 22% | 0% | 100% | N/A | |
| Maruta et al. (2012) [72] | 22 | 4 | 3 | N/A | 18% | 100% | 0% | N/A | |
| Shi et al. (2012) [73] | 68 | 9 | N/A | N/A | 13% | 67% | 33% | N/A | |
| Motoyama et al. (2011) [74] | 48 | 5 | 1 | N/A | 11% | 80% | 20% | N/A | |
| Irie et al. (2010) [75] | 110 | 6 | 8 | N/A | 5% | 83% | 17% | N/A | |
| Yeon et al. (2010) [76] | 98 | 12 | 1 | 0 | 12% | 100% | 0% | 0% | |
| Szelényi et al. (2007) [77] | 108 | 22 | 5 | 2 | 13% | 73% | 27% | 2% | |
| Weinzierl et al. (2007) [78] | 18 | 4 | 0 | 0 | 22% | 25% | 75% | 0% | |
| Szelényi et al. (2006) [16] | 116 | 12 | 15 | 6 | 11% | 75% | 25% | 5% | |
| Horiuchi et al. (2005) [79] | 53 | 10 | 4 | 1 | 19% | 90% | 10% | 2% | |
| Suzuki et al. (2003) [19] | 108 | 20 | 5 | 1 | 19% | 95% | 5% | 1% | |
| ENDOVASCULAR PROCEDURES FOR ANEURYSMS | |||||||||
| Nakagawa et al. (2020) [80] | 164 | 7 | 10 | N/A | 4% | 57% | 43% | N/A | |
| Wilent et al. (2020) [81] | 763 | 51 | 13 | N/A | 7% | 29% | 71% | N/A | |
| Lee et al. (2019) [82] | 561 | 7 | 4 | N/A | 1% | 71% | 29% | N/A | |
| Piñeiro et al. (2015) [83] | 8 | 2 | 3 | 3 | 25% | 50% | 50% | 38% | |
| Hiraishi et al. (2011) [84] | 7 | 3 | 1 | N/A | 43% | 100% | 0% | N/A | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asimakidou, E.; Abut, P.A.; Raabe, A.; Seidel, K. Motor Evoked Potential Warning Criteria in Supratentorial Surgery: A Scoping Review. Cancers 2021, 13, 2803. https://doi.org/10.3390/cancers13112803
Asimakidou E, Abut PA, Raabe A, Seidel K. Motor Evoked Potential Warning Criteria in Supratentorial Surgery: A Scoping Review. Cancers. 2021; 13(11):2803. https://doi.org/10.3390/cancers13112803
Chicago/Turabian StyleAsimakidou, Evridiki, Pablo Alvarez Abut, Andreas Raabe, and Kathleen Seidel. 2021. "Motor Evoked Potential Warning Criteria in Supratentorial Surgery: A Scoping Review" Cancers 13, no. 11: 2803. https://doi.org/10.3390/cancers13112803
APA StyleAsimakidou, E., Abut, P. A., Raabe, A., & Seidel, K. (2021). Motor Evoked Potential Warning Criteria in Supratentorial Surgery: A Scoping Review. Cancers, 13(11), 2803. https://doi.org/10.3390/cancers13112803






