Interfractional Geometric Variations and Dosimetric Benefits of Stereotactic MRI Guided Online Adaptive Radiotherapy (SMART) of Prostate Bed after Radical Prostatectomy: Post-Hoc Analysis of a Phase II Trial
Abstract
Simple Summary
Abstract
1. Introduction
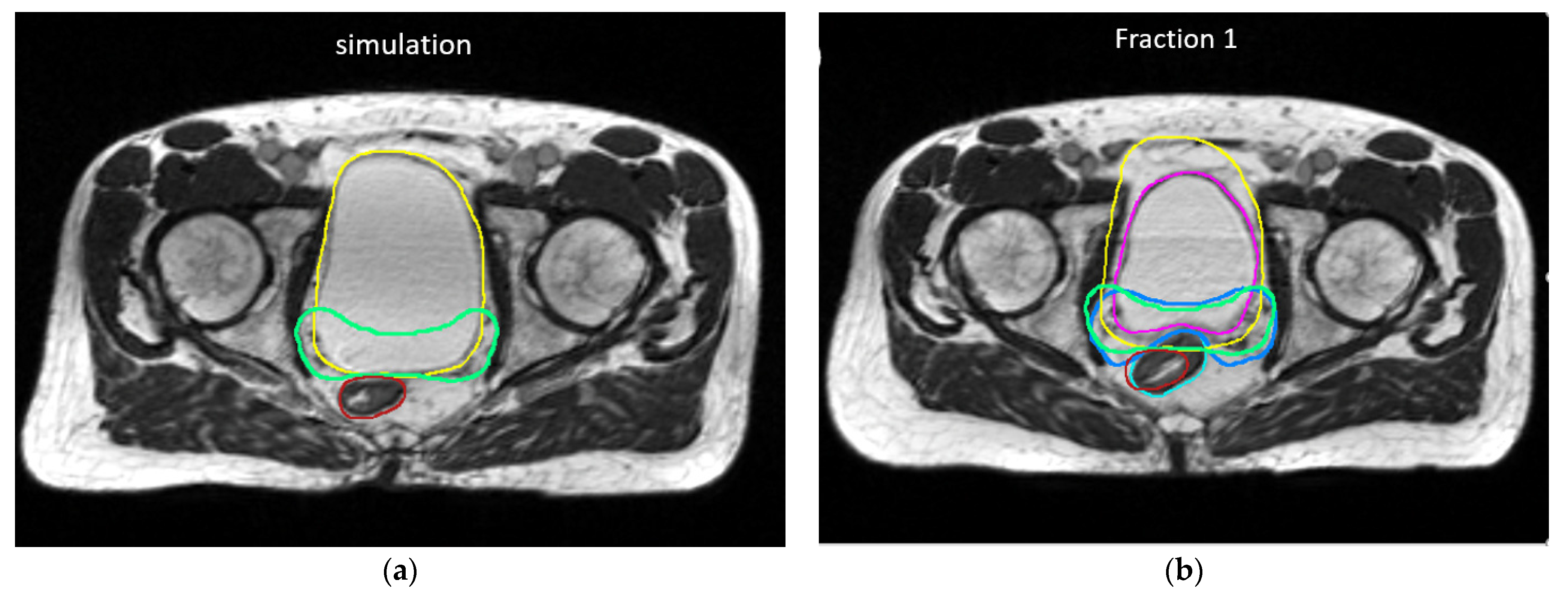
2. Materials and Methods
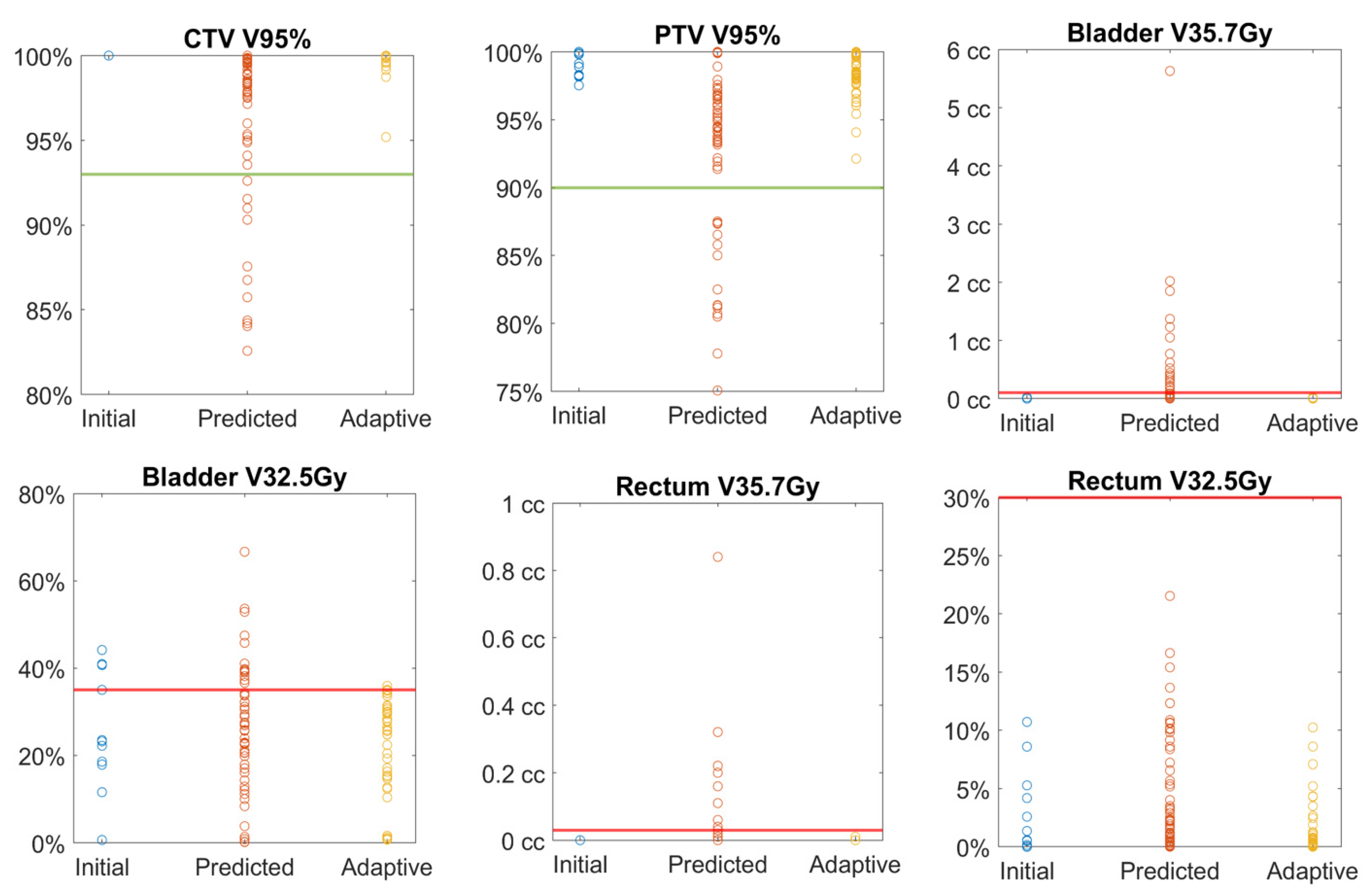
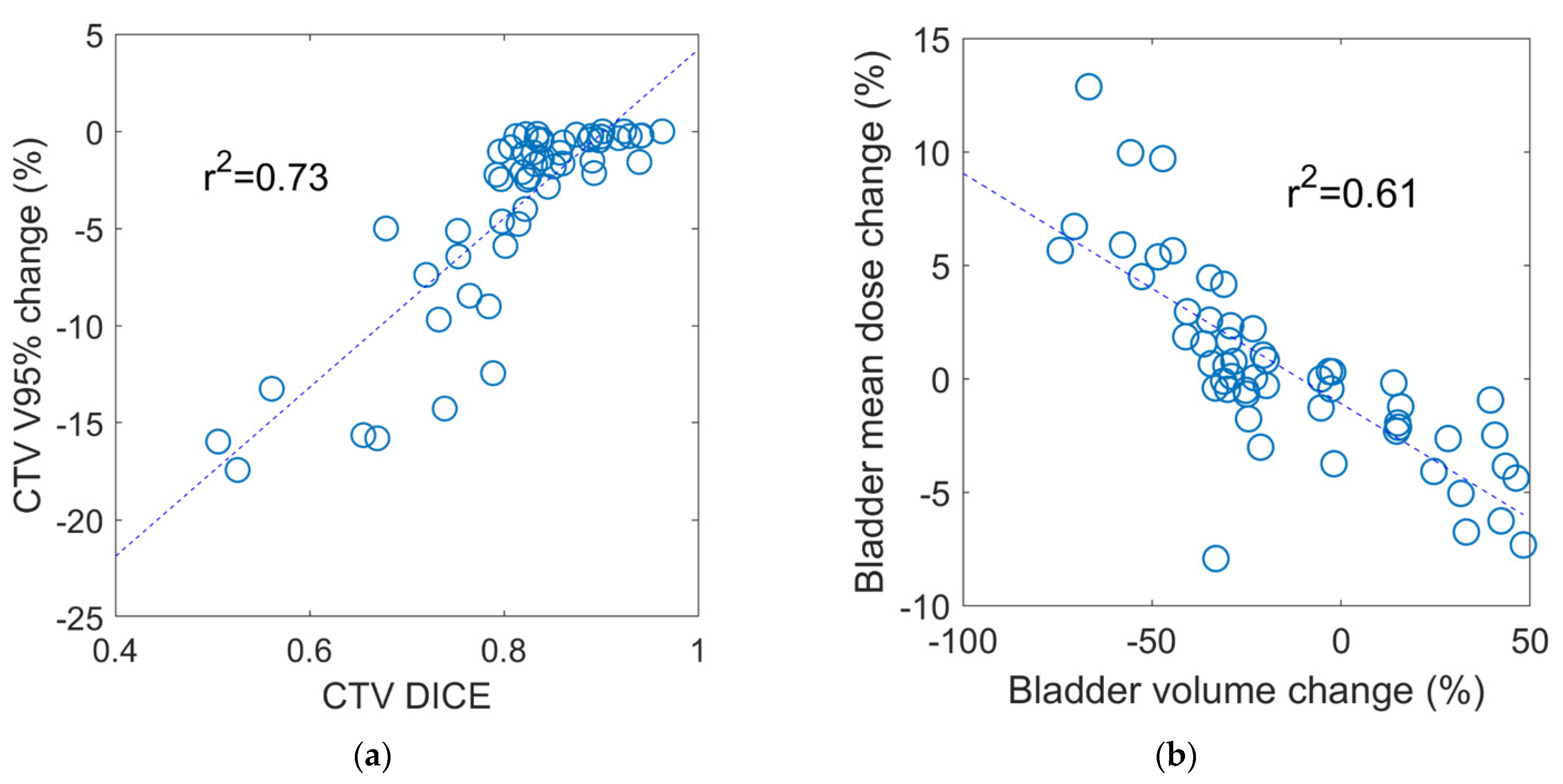
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sineshaw, H.M.; Gray, P.J.; Efstathiou, J.A.; Jemal, A. Declining Use of Radiotherapy for Adverse Features after Radical Prostatectomy: Results from the National Cancer Data Base. Eur. Urol. 2015, 68, 768–774. [Google Scholar] [CrossRef]
- Kishan, A.U.; Duchesne, G.; Wang, P.-C.; Rwigema, J.-C.M.; Kishan, A.U.; Saigal, C.; Rettig, M.; Steinberg, M.L.; King, C.R. Discord among Radiation Oncologists and Urologists in the Postoperative Management of High-Risk Prostate Cancer. Am. J. Clin. Oncol. 2018, 41, 739–746. [Google Scholar] [CrossRef]
- Brenner, D.J.; Hall, E.J. Fractionation and protraction for radiotherapy of prostate carcinoma. Int. J. Radiat. Oncol. 1999, 43, 1095–1101. [Google Scholar] [CrossRef]
- Kishan, A.U.; King, C.R. Stereotactic Body Radiotherapy for Low- and Intermediate-Risk Prostate Cancer. Semin. Radiat. Oncol. 2017, 27, 268–278. [Google Scholar] [CrossRef]
- Kishan, A.U.; Dang, A.; Katz, A.J.; Mantz, C.A.; Collins, S.P.; Aghdam, N.; Chu, F.I.; Kaplan, I.D.; Appelbaum, L.; Fuller, D.B.; et al. Long-term Outcomes of Stereotactic Body Radiotherapy for Low-Risk and Intermediate-Risk Prostate Cancer. JAMA Netw. Open 2019, 2, e188006. [Google Scholar] [CrossRef]
- Widmark, A.; Gunnlaugsson, A.; Beckman, L.; Thellenberg-Karlsson, C.; Hoyer, M.; Lagerlund, M.; Kindblom, J.; Ginman, C.; Johansson, B.; Björnlinger, K.; et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomised, non-inferiority, phase 3 trial. Lancet 2019, 394, 385–395. [Google Scholar] [CrossRef]
- Jackson, W.C.; Silva, J.; Hartman, H.E.; Dess, R.T.; Kishan, A.U.; Beeler, W.H.; Gharzai, L.A.; Jaworski, E.M.; Mehra, R.; Hearn, J.W.; et al. Stereotactic Body Radiation Therapy for Localized Prostate Cancer: A Systematic Review and Meta-Analysis of Over 6,000 Patients Treated on Prospective Studies. Int. J. Radiat. Oncol. 2019, 104, 778–789. [Google Scholar] [CrossRef] [PubMed]
- NCCN. Guidelines for Prostate Cancer. Available online: https://www.nccn.org/store/login/login.aspx?ReturnURL=https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf (accessed on 7 March 2021).
- Chin, S.; Fatimilehin, A.; Walshaw, R.; Argarwal, A.; Mistry, H.; Elliott, T.; Logue, J.; Wylie, J.; Choudhury, A. Ten-Year Outcomes of Moderately Hypofractionated Salvage Postprostatectomy Radiation Therapy and External Validation of a Contemporary Multivariable Nomogram for Biochemical Failure. Int. J. Radiat. Oncol. Biol. Phys. 2020, 107, 288–296. [Google Scholar] [CrossRef]
- Martell, K.; Cheung, P.; Morton, G.; Chung, H.; Deabreu, A.; Zhang, L.; Pang, G.; Alayed, Y.; Mamedov, A.; Gladwish, A.; et al. 5-Year Outcomes of a Prospective Phase 1/2 Study of Accelerated Hypofractionated Radiation Therapy to the Prostate Bed. Pract. Radiat. Oncol. 2019, 9, 354–361. [Google Scholar] [CrossRef]
- Picardi, C.; Perret, I.; Miralbell, R.; Zilli, T. Hypofractionated Radiotherapy for Prostate Cancer in the Postoperative Setting: What Is the Evidence so Far? Cancer Treat. Rev. 2018, 62, 91–96. [Google Scholar] [CrossRef]
- Vilotte, F.; Antoine, M.; Bobin, M.; Latorzeff, I.; Supiot, S.; Richaud, P.; Thomas, L.; LeDuc, N.; Guerif, S.; Iriondo-Alberdi, J.; et al. Post-Prostatectomy Image-Guided Radiotherapy: The Invisible Target Concept. Front. Oncol. 2017, 7, 34. [Google Scholar] [CrossRef][Green Version]
- Murray, J.R.; McNair, H.A.; Dearnaley, D.P. Rationale and development of image-guided intensity-modulated radiotherapy post-prostatectomy: The present standard of care? Cancer Manag. Res. 2015, 7, 331–344. [Google Scholar]
- Bell, L.J.; Cox, J.; Eade, T.; Rinks, M.; Kneebone, A. Prostate bed motion may cause geographic miss in post-prostatectomy image-guided intensity-modulated radiotherapy. J. Med. Imaging Radiat. Oncol. 2013, 57, 725–732. [Google Scholar] [CrossRef]
- Huang, K.; Palma, D.A.; Scott, D.; McGregor, D.; Gaede, S.; Yartsev, S.; Bauman, G.; Louie, A.V.; Rodrigues, G. Inter- and Intrafraction Uncertainty in Prostate Bed Image-Guided Radiotherapy. Int. J. Radiat. Oncol. 2012, 84, 402–407. [Google Scholar] [CrossRef]
- Yoon, S.; Cao, M.; Aghdam, N.; Shabsovich, D.; Kahlon, S.; Ballas, L.; Collins, S.; Steinberg, M.L.; Kishan, A.U. Prostate bed and organ-at-risk deformation: Prospective volumetric and dosimetric data from a phase II trial of stereotactic body radiotherapy after radical prostatectomy. Radiother Oncol. 2020, 148, 44–50. [Google Scholar] [CrossRef]
- Pathmanathan, A.U.; Van As, N.J.; Kerkmeijer, L.G.W.; Christodouleas, J.; Lawton, C.A.F.; Vesprini, D.; Van Der Heide, U.A.; Frank, S.J.; Nill, S.; Oelfke, U.; et al. Magnetic Resonance Imaging-Guided Adaptive Radiation Therapy: A “Game Changer” for Prostate Treatment? Int. J. Radiat. Oncol. Biol. Phys. 2018, 100, 361–373. [Google Scholar] [CrossRef]
- Rosenberg, S.A.; Henke, L.E.; Shaverdian, N.; Mittauer, K.; Wojcieszynski, A.P.; Hullett, C.R.; Kamrava, M.; Lamb, J.; Cao, M.; Green, O.L.; et al. A Multi-Institutional Experience of MR-Guided Liver Stereotactic Body Radiation Therapy. Adv. Radiat. Oncol. 2019, 4, 142–149. [Google Scholar] [CrossRef]
- Rudra, S.; Jiang, N.; Rosenberg, S.A.; Olsen, J.R.; Roach, M.C.; Wan, L.; Portelance, L.; Mellon, E.A.; Bruynzeel, A.; Lagerwaard, F.; et al. Using adaptive magnetic resonance image-guided radiation therapy for treatment of inoperable pancreatic cancer. Cancer Med. 2019, 8, 2123–2132. [Google Scholar] [CrossRef] [PubMed]
- Mazzola, R.; Figlia, V.; Rigo, M.; Cuccia, F.; Ricchetti, F.; Giaj-Levra, N.; Nicosia, L.; Vitale, C.; Sicignano, G.; De Simone, A.; et al. Feasibility and safety of 1.5 T MR-guided and daily adapted abdominal-pelvic SBRT for elderly cancer patients: Geriatric assessment tools and preliminary patient-reported outcomes. J. Cancer Res. Clin. Oncol. 2020, 146, 2379–2397. [Google Scholar] [CrossRef] [PubMed]
- Henke, L.; Kashani, R.; Robinson, C.; Curcuru, A.; DeWees, T.; Bradley, J.; Green, O.; Michalski, J.; Mutic, S.; Parikh, P.; et al. Phase I trial of stereotactic MR-guided online adaptive radiation therapy (SMART) for the treatment of oligometastatic or unresectable primary malignancies of the abdomen. Radiother Oncol. 2018, 126, 519–526. [Google Scholar] [CrossRef]
- Henke, L.; Contreras, J.; Green, O.; Cai, B.; Kim, H.; Roach, M.; Olsen, J.; Fischer-Valuck, B.; Mullen, D.; Kashani, R.; et al. Magnetic Resonance Image-Guided Radiotherapy (MRIgRT): A 4.5-Year Clinical Experience. Clin. Oncol. 2018, 30, 720–727. [Google Scholar] [CrossRef]
- Michalski, J.M.; Lawton, C.; El Naqa, I.; Ritter, M.; O’Meara, E.; Seider, M.J.; Lee, W.R.; Rosenthal, S.A.; Pisansky, T.; Catton, C.; et al. Development of RTOG Consensus Guidelines for the Definition of the Clinical Target Volume for Postoperative Conformal Radiation Therapy for Prostate Cancer. Int. J. Radiat. Oncol. 2010, 76, 361–368. [Google Scholar] [CrossRef]
- Allozi, R.; Li, X.A.; White, J.; Apte, A.; Tai, A.; Michalski, J.M.; Bosch, W.R.; El Naqa, I. Tools for Consensus Analysis of Experts’ Contours for Radiotherapy Structure Definitions. Radiol. Oncol. 2010, 97, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Lamb, J.; Cao, M.; Kishan, A.; Agazaryan, N.; Thomas, D.H.; Shaverdian, N.; Yang, Y.; Ray, S.A.; Low, D.; Raldow, A.; et al. Online Adaptive Radiation Therapy: Implementation of a New Process of Care. Cureus 2017, 9, e1618. [Google Scholar] [CrossRef]
- Bruynzeel, A.M.; Tetar, S.U.; Oei, S.S.; Senan, S.; Haasbeek, C.J.; Spoelstra, F.O.; Piet, A.H.; Meijnen, P.; van der Jagt, M.A.B.; Fraikin, T.; et al. A Prospective Single-Arm Phase 2 Study of Stereotactic Magnetic Resonance Guided Adaptive Radiation Therapy for Prostate Cancer: Early Toxicity Results. Int. J. Radiat. Oncol. 2019, 105, 1086–1094. [Google Scholar] [CrossRef] [PubMed]
- Alongi, F.; Rigo, M.; Figlia, V.; Cuccia, F.; Giaj-Levra, N.; Nicosia, L.; Ricchetti, F.; Sicignano, G.; De Simone, A.; Naccarato, S.; et al. 1.5 T MR-guided and daily adapted SBRT for prostate cancer: Feasibility, preliminary clinical tolerability, quality of life and patient-reported outcomes during treatment. Radiat. Oncol. 2020, 15, 69. [Google Scholar] [CrossRef] [PubMed]
- Ugurluer, G.; Atalar, B.; Zoto Mustafayev, T.; Gungor, G.; Aydin, G.; Sengoz, M.; Abacioglu, U.; Tuna, M.B.; Kural, A.R.; Ozyar, E. Magnetic resonance image-guided adaptive stereotactic body radiotherapy for prostate cancer: Preliminary results of outcome and toxicity. Br. J. Radiol. 2020, 94, 20200696. [Google Scholar] [CrossRef] [PubMed]
| Structure | Volume Change (%) | DSC | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | Median | Q1 | Q3 | Mean | Median | Q1 | Q3 | |
| CTV | 4.9 | 3.0 | −3.0 | 11.5 | 0.81 | 0.83 | 0.79 | 0.88 |
| Bladder | −14.8 | −24.5 | −34.6 | 14.5 | 0.76 | 0.79 | 0.74 | 0.82 |
| Rectum | 3.9 | 5.4 | −9.7 | 20.7 | 0.72 | 0.73 | 0.67 | 0.79 |
| Dosimetric Parameter | Adaptive Criterion | Initial Plan | Predicted Plan | Adaptive Plan | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | Q1 | Q3 | Mean | Median | Q1 | Q3 | Mean | Median | Q1 | Q3 | ||
| CTV mean dose (Gy) | 34.3 | 34.3 | 33.8 | 34.7 | 33.8 * | 33.8 | 33.3 | 34.6 | 34.2 | 34.2 | 33.5 | 34.9 | |
| CTV V95% | >93% | 100.0 | 100.0 | 100.0 | 100.0 | 96.2 * | 98.4 | 94.9 | 99.6 | 99.8 | 100.0 | 100.0 | 100.0 |
| PTV mean dose (Gy) | 34.0 | 34.0 | 33.4 | 34.6 | 33.5 * | 33.5 | 32.9 | 34.4 | 34.0 | 33.9 | 33.4 | 34.7 | |
| PTV V95% | >90% | 99.0 | 98.9 | 98.2 | 99.9 | 92.3 * | 94.4 | 88.5 | 96.5 | 98.2 + | 98.4 | 97.8 | 99.5 |
| Bladder mean dose (Gy) | 20.7 | 22.6 | 15.2 | 25.0 | 21.1 | 21.9 | 17.7 | 24.9 | 22.6 | 23.3 | 19.9 | 25.5 | |
| Bladder Dmax (Gy) | <36.7 Gy | 35.8 | 35.5 | 35.4 | 35.7 | 36.4 * | 36.0 | 35.6 | 37.0 | 35.6 + | 35.4 | 35.1 | 35.7 |
| Bladder V32.5Gy (%) | <35% | 25.3 | 23.2 | 17.9 | 40.7 | 25.7 | 25.7 | 17.3 | 34.2 | 24.2 | 27.7 | 16.5 | 33.6 |
| Rectum mean dose (Gy) | 15.4 | 15.5 | 12.7 | 18.6 | 15.4 | 14.7 | 12.9 | 18.4 | 15.6 | 15.6 | 13.6 | 18.3 | |
| Rectum Dmax (Gy) | <36.7 Gy | 34.5 | 35.0 | 33.4 | 35.2 | 35.5 * | 35.2 | 34.5 | 36.2 | 34.1 | 34.2 | 33.5 | 34.7 |
| Rectum V27.5Gy (%) | <45% | 10.2 | 8.1 | 5.2 | 14.1 | 11.4 | 9.1 | 6.4 | 15.6 | 8.5 + | 7.2 | 4.4 | 11.0 |
| Rectum V32.5Gy (%) | <30% | 3.1 | 1.4 | 0.2 | 5.3 | 4.9 * | 2.3 | 0.8 | 9.0 | 1.3 + | 0.4 | 0.1 | 1.1 |
| Rectal wall mean dose (Gy) | 15.6 | 15.3 | 12.7 | 18.7 | 15.3 | 14.6 | 12.7 | 18.3 | 15.7 | 15.8 | 13.5 | 18.2 | |
| Rectal wall V24Gy (%) | <50% | 19.9 | 20.7 | 13.8 | 24.1 | 19.4 | 18.2 | 15.2 | 24.5 | 19.5 | 19.0 | 13.4 | 23.9 |
| Dosimetric Parameter | Acceptable CTV95% | Unacceptable CTV95% | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Median | Q1 | Q3 | Mean | SD | Median | Q1 | Q3 | p-Value | |
| CTV V95% (%) | 98.36 | 1.75 | 98.91 | 97.71 | 99.75 | 87.33 | 3.51 | 86.75 | 84.24 | 90.82 | <0.001 |
| CTV Volume (cc) | 113.66 | 26.60 | 122.77 | 91.70 | 131.89 | 114.28 | 25.02 | 123.80 | 89.78 | 129.85 | 0.945 |
| Bladder volume (cc) | 232.31 | 127.85 | 206.66 | 134.36 | 308.92 | 191.05 | 119.56 | 121.57 | 90.49 | 313.92 | 0.337 |
| Rectum volume (cc) | 67.22 | 14.29 | 63.94 | 58.37 | 74.22 | 66.33 | 13.52 | 64.08 | 59.21 | 71.81 | 0.853 |
| CTV DSC | 0.85 | 0.06 | 0.84 | 0.82 | 0.89 | 0.68 | 0.10 | 0.72 | 0.58 | 0.76 | <0.001 |
| Bladder DSC | 0.77 | 0.11 | 0.79 | 0.75 | 0.82 | 0.74 | 0.07 | 0.76 | 0.70 | 0.79 | 0.490 |
| Rectum DSC | 0.73 | 0.08 | 0.74 | 0.69 | 0.80 | 0.68 | 0.08 | 0.68 | 0.62 | 0.73 | 0.042 |
| Bladder mean dose (Gy) | 21.50 | 5.22 | 22.60 | 17.94 | 25.33 | 19.70 | 4.65 | 20.38 | 16.20 | 22.68 | 0.300 |
| Bladder Dmax (Gy) | 36.25 | 0.94 | 36.02 | 35.65 | 36.59 | 37.24 | 2.82 | 37.41 | 34.53 | 39.76 | 0.052 |
| Bladder V32.5 (%) | 29.33 | 13.23 | 28.18 | 21.87 | 37.70 | 11.43 | 8.73 | 11.21 | 2.76 | 16.81 | 0.001 |
| Rectum mean dose (Gy) | 15.53 | 3.09 | 14.92 | 12.99 | 18.41 | 14.94 | 3.17 | 14.73 | 12.88 | 17.85 | 0.581 |
| Rectum Dmax (Gy) | 35.08 | 1.13 | 35.12 | 34.49 | 35.76 | 37.32 | 2.58 | 38.30 | 34.69 | 39.81 | <0.001 |
| Rectum V32.5 (%) | 4.60 | 5.21 | 2.28 | 0.79 | 8.47 | 5.90 | 5.08 | 5.18 | 1.06 | 10.47 | 0.461 |
| Rectm V27.5 (%) | 11.05 | 7.33 | 8.55 | 6.34 | 14.81 | 12.61 | 5.47 | 13.63 | 7.22 | 16.62 | 0.512 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, M.; Gao, Y.; Yoon, S.M.; Yang, Y.; Sheng, K.; Ballas, L.K.; Basehart, V.; Sachdeva, A.; Felix, C.; Low, D.A.; et al. Interfractional Geometric Variations and Dosimetric Benefits of Stereotactic MRI Guided Online Adaptive Radiotherapy (SMART) of Prostate Bed after Radical Prostatectomy: Post-Hoc Analysis of a Phase II Trial. Cancers 2021, 13, 2802. https://doi.org/10.3390/cancers13112802
Cao M, Gao Y, Yoon SM, Yang Y, Sheng K, Ballas LK, Basehart V, Sachdeva A, Felix C, Low DA, et al. Interfractional Geometric Variations and Dosimetric Benefits of Stereotactic MRI Guided Online Adaptive Radiotherapy (SMART) of Prostate Bed after Radical Prostatectomy: Post-Hoc Analysis of a Phase II Trial. Cancers. 2021; 13(11):2802. https://doi.org/10.3390/cancers13112802
Chicago/Turabian StyleCao, Minsong, Yu Gao, Stephanie M. Yoon, Yingli Yang, Ke Sheng, Leslie K. Ballas, Vincent Basehart, Ankush Sachdeva, Carol Felix, Daniel A. Low, and et al. 2021. "Interfractional Geometric Variations and Dosimetric Benefits of Stereotactic MRI Guided Online Adaptive Radiotherapy (SMART) of Prostate Bed after Radical Prostatectomy: Post-Hoc Analysis of a Phase II Trial" Cancers 13, no. 11: 2802. https://doi.org/10.3390/cancers13112802
APA StyleCao, M., Gao, Y., Yoon, S. M., Yang, Y., Sheng, K., Ballas, L. K., Basehart, V., Sachdeva, A., Felix, C., Low, D. A., Steinberg, M. L., & Kishan, A. U. (2021). Interfractional Geometric Variations and Dosimetric Benefits of Stereotactic MRI Guided Online Adaptive Radiotherapy (SMART) of Prostate Bed after Radical Prostatectomy: Post-Hoc Analysis of a Phase II Trial. Cancers, 13(11), 2802. https://doi.org/10.3390/cancers13112802







