Ablation in Pancreatic Cancer: Past, Present and Future
Abstract
:Simple Summary
Abstract
1. Introduction
2. Treatment Options for Locally Advanced Pancreatic Cancer
2.1. Surgery
2.2. Chemotherapy
2.3. Radiotherapy
2.4. Ablation
2.4.1. Radiofrequency Ablation
2.4.2. Microwave Ablation
2.4.3. Cryoablation
2.4.4. Photodynamic Therapy
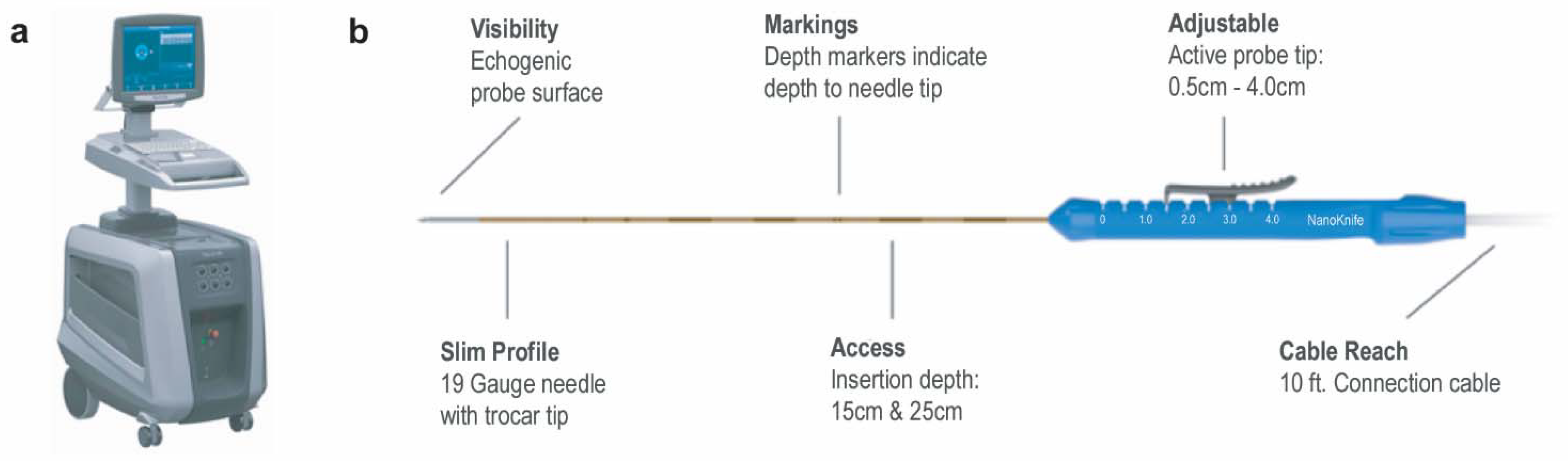
2.4.5. Irreversible Electroporation
2.4.6. Prospective IRE Trials
3. Post-Ablative Imaging in Pancreatic Cancer
4. The Future of IRE
4.1. Immunomodulatory Effects of IRE
4.2. High-Frequency IRE—An Emerging Technique
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef]
- Kamisawa, T.; Wood, L.D.; Itoi, T.; Takaori, K. Pancreatic cancer. Lancet 2016, 388, 73–85. [Google Scholar] [CrossRef]
- Suker, M.; Beumer, B.R.; Sadot, E.; Marthey, L.; Faris, J.E.; Mellon, E.A.; El-Rayes, B.F.; Wang-Gillam, A.; Lacy, J.; Hosein, P.J.; et al. FOLFIRINOX for locally advanced pancreatic cancer: A systematic review and patient-level meta-analysis. Lancet Oncol. 2016, 17, 801–810. [Google Scholar] [CrossRef] [Green Version]
- Gervais, D.A.; Fernandez-del Castillo, C.; O’Neill, M.J.; Hahn, P.F.; Mueller, P.R. Complications after Pancreatoduodenectomy: Imaging and Imaging-guided Interventional Procedures. Radiographics 2001, 21, 673–690. [Google Scholar] [CrossRef]
- Sohn, T.A.; Yeo, C.J.; Cameron, J.L.; Geschwind, J.F.; Mitchell, S.E.; Venbrux, A.C.; Lillemoe, K.D. Pancreaticoduodenectomy: Role of interventional radiologists in managing patients and complications. J. Gastrointest. Surg. 2003, 7, 209–219. [Google Scholar] [CrossRef]
- Malgras, B.; Duron, S.; Gaujoux, S.; Dokmak, S.; Aussilhou, B.; Rebours, V.; Palazzo, M.; Belghiti, J.; Sauvanet, A. Early biliary complications following pancreaticoduodenectomy: Prevalence and risk factors. HPB 2016, 18, 367–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bassi, D.C.; Butturini, G. Postoperative pancreatic fistula: An international study group (ISGPF) definition. Surgery 2005, 138, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Wente, M.N.; Veit, J.A.; Bassi, C.; Dervenis, C.; Fingerhut, A.; Gouma, D.J.; Izbicki, J.R.; Neoptolemos, J.P.; Padbury, R.T.; Sarr, M.G.; et al. Postpancreatectomy hemorrhage (PPH)–An International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 2007, 142, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, J.; Michalski, C.W.; Martignoni, M.E.; Büchler, M.W.; Friess, H. Pancreatic resection for pancreatic cancer. HPB 2006, 8, 346–351. [Google Scholar] [CrossRef] [Green Version]
- Conroy, T.; Hammel, P.; Hebbar, M.; Ben Abdelghani, M.; Wei, A.C.; Raoul, J.L.; Choné, L.; Francois, E.; Artru, P.; Biagi, J.J.; et al. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N. Engl. J. Med. 2018, 379, 2395–2406. [Google Scholar] [CrossRef]
- Petrelli, F.; Coinu, A.; Borgonovo, K.; Cabiddu, M.; Ghilardi, M.; Lonati, V.; Aitini, E.; Barni, S.; Gruppo Italiano per lo Studio dei Carcinomi dell’Apparato Digerente (GISCAD). FOLFIRINOX-based neoadjuvant therapy in borderline resectable or unresectable pancreatic cancer: A meta-analytical review of published studies. Pancreas 2015, 44, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Thibodeau, S.; Voutsadakis, I.A. FOLFIRINOX Chemotherapy in Metastatic Pancreatic Cancer: A Systematic Review and Meta-Analysis of Retrospective and Phase II Studies. J. Clin. Med. 2018, 7, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Hoff, D.D.; Ervin, T.; Arena, F.P.; Chiorean, E.G.; Infante, J.; Moore, M.; Seay, T.; Tjulandin, S.A.; Ma, W.W.; Saleh, M.N.; et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N. Engl. J. Med. 2013, 369, 1691–1703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chauffert, B.; Mornex, F.; Bonnetain, F.; Rougier, P.; Mariette, C.; Bouché, O.; Bosset, J.F.; Aparicio, T.; Mineur, L.; Azzedine, A.; et al. Phase III trial comparing intensive induction chemoradiotherapy (60 Gy, infusional 5-FU and intermittent cisplatin) followed by maintenance gemcitabine with gemcitabine alone for locally advanced unresectable pancreatic cancer. Definitive results of the 2000-01 FFCD/SFRO study. Ann. Oncol. 2008, 19, 1592–1599. [Google Scholar]
- Hammel, P.; Huguet, F.; van Laethem, J.L.; Goldstein, D.; Glimelius, B.; Artru, P.; Borbath, I.; Bouché, O.; Shannon, J.; André, T.; et al. Effect of Chemoradiotherapy vs Chemotherapy on Survival in Patients with Locally Advanced Pancreatic Cancer Controlled After 4 Months of Gemcitabine with or without Erlotinib: The LAP07 Randomized Clinical Trial. JAMA 2016, 315, 1844–1853. [Google Scholar] [CrossRef]
- Reyngold, M.; O’Reilly, E.M.; Varghese, A.M.; Fiasconaro, M.; Zinovoy, M.; Romesser, P.B.; Wu, A.; Hajj, C.; Cuaron, J.J.; Tuli, R.; et al. Association of Ablative Radiation Therapy with Survival Among Patients with Inoperable Pancreatic Cancer. JAMA Oncol. 2021, e210057. [Google Scholar]
- Rudra, S.; Jiang, N.; Rosenberg, S.A.; Olsen, J.R.; Roach, M.C.; Wan, L.; Portelance, L.; Mellon, E.A.; Bruynzeel, A.; Lagerwaard, F.; et al. Using adaptive magnetic resonance image-guided radiation therapy for treatment of inoperable pancreatic cancer. Cancer Med. 2019, 8, 2123–2132. [Google Scholar] [CrossRef]
- Haqq, J.; Howells, L.M.; Garcea, G.; Metcalfe, M.S.; Steward, W.P.; Dennison, A.R. Pancreatic stellate cells and pancreas cancer: Current perspectives and future strategies. Eur. J. Cancer 2014, 50, 2570–2582. [Google Scholar] [CrossRef]
- McMillin, D.W.; Negri, J.M.; Mitsiades, C.S. The role of tumour-stromal interactions in modifying drug response: Challenges and opportunities. Nat. Rev. Drug Discov. 2013, 12, 217–228. [Google Scholar] [CrossRef]
- Keane, M.G.; Bramis, K.; Pereira, S.P.; Fusai, G.K. Systematic review of novel ablative methods in locally advanced pancreatic cancer. World J. Gastroenterol. 2014, 20, 2267–2278. [Google Scholar] [CrossRef]
- Ruarus, A.; Vroomen, L.; Puijk, R.; Scheffer, H.; Meijerink, M. Locally Advanced Pancreatic Cancer: A Review of Local Ablative Therapies. Cancers 2018, 10, 16. [Google Scholar] [CrossRef] [Green Version]
- Lygidakis, N.J.; Sharma, S.K.; Papastratis, P.; Zivanovic, V.; Kefalourous, H.; Koshariya, M.; Lintzeris, I.; Porfiris, T.; Koutsiouroumba, D. Microwave ablation in locally advanced pancreatic carcinoma--A new look. Hepatogastroenterology 2007, 54, 1305–1310. [Google Scholar] [PubMed]
- Carrafiello, G.; Ierardi, A.M.; Fontana, F.; Petrillo, M.; Floridi, C.; Lucchina, N.; Cuffari, S.; Dionigi, G.; Rotondo, A.; Fugazzola, C. Microwave ablation of pancreatic head cancer: Safety and efficacy. J. Vasc. Interv. Radiol. 2013, 24, 1513–1520. [Google Scholar] [CrossRef] [PubMed]
- Vogl, T.J.; Panahi, B.; Albrecht, M.H.; Naguib, N.N.N.; Nour-Eldin, N.A.; Gruber-Rouh, T.; Thompson, Z.M.; Basten, L.M. Microwave ablation of pancreatic tumors. Minim. Invasive Ther. Allied Technol. 2018, 27, 33–40. [Google Scholar] [CrossRef]
- Li, J.; Chen, X.; Yang, H.; Wang, X.; Yuan, D.; Zeng, Y.; Wen, T.; Yan, L.; Li, B. Tumour cryoablation combined with palliative bypass surgery in the treatment of unresectable pancreatic cancer: A retrospective study of 142 patients. Postgrad. Med. J. 2011, 87, 89–95. [Google Scholar] [CrossRef]
- Song, Z.G.; Hao, J.H.; Gao, S.; Gao, C.T.; Tang, Y.; Liu, J.C. The outcome of cryoablation in treating advanced pancreatic cancer: A comparison with palliative bypass surgery alone. J. Dig. Dis. 2014, 15, 561–569. [Google Scholar] [CrossRef]
- Niu, L.; He, L.; Zhou, L.; Mu, F.; Wu, B.; Li, H.; Yang, Z.; Zuo, J.; Xu, K. Percutaneous ultrasonography and computed tomography guided pancreatic cryoablation: Feasibility and safety assessment. Cryobiology 2012, 65, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Henderson, B.W.; Dougherty, T.J. How does photodynamic therapy work? Photochem. Photobiol. 1992, 55, 145–157. [Google Scholar] [CrossRef]
- Agostinis, P.; Berg, K.; Cengel, K.A.; Foster, T.H.; Girotti, A.W.; Gollnick, S.O.; Hahn, S.M.; Hamblin, M.R.; Juzeniene, A.; Kessel, D.; et al. Photodynamic therapy of cancer: An update. CA Cancer J. Clin. 2011, 61, 250–281. [Google Scholar] [CrossRef]
- Bown, S.G.; Rogowska, A.Z.; Whitelaw, D.E.; Lees, W.R.; Lovat, L.B.; Ripley, P.; Jones, L.; Wyld, P.; Gillams, A.; Hatfield, A.W. Photodynamic therapy for cancer of the pancreas. Gut 2002, 50, 549–557. [Google Scholar] [CrossRef]
- Huggett, M.T.; Jermyn, M.; Gillams, A.; Illing, R.; Mosse, S.; Novelli, M.; Kent, E.; Bown, S.G.; Hasan, T.; Pogue, B.W.; et al. Phase I/II study of verteporfin photodynamic therapy in locally advanced pancreatic cancer. Br. J. Cancer. 2014, 110, 1698–1704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davalos, R.V.; Mir, I.L.; Rubinsky, B. Tissue ablation with irreversible electroporation. Ann. Biomed. Eng. 2005, 33, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Rubinsky, B.; Onik, G.; Mikus, P. Irreversible electroporation: A new ablation modality—Clinical implications. Technol. Cancer Res. Treat. 2007, 6, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, G.; Bhatia, S.; Echenique, A.; Suthar, R.; Barbery, K.; Yrizarry, J. Vessel patency post irreversible electroporation. Cardiovasc. Intervent. Radiol. 2014, 37, 1523–1529. [Google Scholar] [CrossRef]
- Charpentier, K.P.; Wolf, F.; Noble, L.; Winn, B.; Resnick, M.; Dupuy, D.E. Irreversible electroporation of the pancreas in swine: A pilot study. HPB 2010, 12, 348–351. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Li, W.; Procissi, D.; Tyler, P.; Omary, R.A.; Larson, A.C. Rapid dramatic alterations to the tumor microstructure in pancreatic cancer following irreversible electroporation ablation. Nanomedicine 2014, 9, 1181–1192. [Google Scholar] [CrossRef] [Green Version]
- Martin, R.C.G., 2nd. Irreversible electroporation of stage 3 locally advanced pancreatic cancer: Optimal technique and outcomes. J. Vis. Surg. 2015, 1, 4. [Google Scholar]
- Narayanan, G.; Hosein, P.J.; Arora, G.; Barbery, K.J.; Froud, T.; Livingstone, A.S.; Franceschi, D.; Rocha Lima, C.M.; Yrizarry, J. Percutaneous irreversible electroporation for downstaging and control of unresectable pancreatic adenocarcinoma. J. Vasc. Interv. Radiol. 2012, 23, 1613–1621. [Google Scholar] [CrossRef]
- Narayanan, G.; Hosein, P.J.; Beulaygue, I.C.; Froud, T.; Scheffer, H.J.; Venkat, S.R.; Echenique, A.M.; Hevert, E.C.; Livingstone, A.S.; Rocha-Lima, C.M.; et al. Percutaneous Image-Guided Irreversible Electroporation for the Treatment of Unresectable, Locally Advanced Pancreatic Adenocarcinoma. J. Vasc. Interv. Radiol. 2017, 28, 342–348. [Google Scholar] [CrossRef]
- Leen, E.; Picard, J.; Stebbing, J.; Abel, M.; Dhillon, T.; Wasan, H. Percutaneous irreversible electroporation with systemic treatment for locally advanced pancreatic adenocarcinoma. J. Gastrointest. Oncol. 2018, 9, 275–281. [Google Scholar] [CrossRef]
- Sugimoto, K.; Moriyasu, F.; Kobayashi, Y.; Saito, K.; Takeuchi, H.; Ogawa, S.; Ando, M.; Sano, T.; Mori, T.; Furuichi, Y.; et al. Irreversible electroporation for nonthermal tumor ablation in patients with hepatocellular carcinoma: Initial clinical experience in Japan. Jpn. J. Radiol. 2015, 33, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Scheffer, H.J.; Vroomen, L.G.; de Jong, M.C.; Melenhorst, M.C.; Zonderhuis, B.M.; Daams, F.; Vogel, J.A.; Besselink, M.G.; van Kuijk, C.; Witvliet, J.; et al. Ablation of Locally Advanced Pancreatic Cancer with Percutaneous Irreversible Electroporation: Results of the Phase I/II PANFIRE Study. Radiology 2017, 282, 585–597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruarus, A.H.; Vroomen, L.G.P.H.; Geboers, B.; van Veldhuisen, E.; Puijk, R.S.; Nieuwenhuizen, S.; Besselink, M.G.; Zonderhuis, B.M.; Kazemier, G.; de Gruijl, T.D.; et al. Percutaneous Irreversible Electroporation in Locally Advanced and Recurrent Pancreatic Cancer (PANFIRE-2): A Multicenter, Prospective, Single-Arm, Phase II Study. Radiology 2020, 294, 212–220. [Google Scholar] [CrossRef]
- He, C.; Wang, J.; Sun, S.; Zhang, Y.; Lin, X.; Lao, X.; Cui, B.; Li, S. Irreversible electroporation versus radiotherapy after induction chemotherapy on survival in patients with locally advanced pancreatic cancer: A propensity score analysis. BMC Cancer 2019, 19, 394. [Google Scholar]
- Liu, S.; Qin, Z.; Xu, J.; Zeng, J.; Chen, J.; Niu, L.; Liu, S.; Qin, Z.; Xu, J.; Zeng, J.; et al. Irreversible electroporation combined with chemotherapy for unresectable pancreatic carcinoma: A prospective cohort study. OncoTargets Ther. 2019, 12, 1341–1350. [Google Scholar] [CrossRef] [Green Version]
- Katz, M.H.; Fleming, J.B.; Bhosale, P.; Varadhachary, G.; Lee, J.E.; Wolff, R.; Wang, H.; Abbruzzese, J.; Pisters, P.W.; Vauthey, J.N.; et al. Response of borderline resectable pancreatic cancer to neoadjuvant therapy is not reflected by radiographic indicators. Cancer 2012, 118, 5749–5756. [Google Scholar] [CrossRef] [PubMed]
- Vroomen, L.G.P.H.; Scheffer, H.J.; Melenhorst, M.C.A.M.; de Jong, M.C.; van den Bergh, J.E.; van Kuijk, C.; van Delft, F.; Kazemier, G.; Meijerink, M.R. MR and CT imaging characteristics and ablation zone volumetry of locally advanced pancreatic cancer treated with irreversible electroporation. Eur. Radiol. 2017, 27, 2521–2531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, J.; Wen, X.; Tian, L.; Li, T.; Xu, C.; Wen, X.; Melancon, M.P.; Gupta, S.; Shen, B.; Peng, W.; et al. Irreversible electroporation reverses resistance to immune checkpoint blockade in pancreatic cancer. Nat. Commun. 2019, 10, 899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- White, S.B.; Zhang, Z.; Chen, J.; Gogineni, V.R.; Larson, A.C. Early Immunologic Response of Irreversible Electroporation versus Cryoablation in a Rodent Model of Pancreatic Cancer. J. Vasc. Interv. Radiol. 2018, 29, 1764–1769. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, T.J.; Passeri, M.; Lorenzo, M.F.; Sulzer, J.K.; Lyman, W.B.; Swet, J.H.; Vrochides, D.; Baker, E.H.; Iannitti, D.A.; Davalos, R.V.; et al. Experimental High-Frequency Irreversible Electroporation Using a Single-Needle Delivery Approach for Nonthermal Pancreatic Ablation In Vivo. J. Vasc. Interv. Radiol. 2019, 30, 854–862.e7. [Google Scholar] [CrossRef]
- Partridge, B.R.; O’Brien, T.J.; Lorenzo, M.F.; Coutermarsh-Ott, S.L.; Barry, S.L.; Stadler, K.; Muro, N.; Meyerhoeffer, M.; Allen, I.C.; Davalos, R.V.; et al. High-Frequency Irreversible Electroporation for Treatment of Primary Liver Cancer: A Proof-of-Principle Study in Canine Hepatocellular Carcinoma. J. Vasc. Interv. Radiol. 2020, 31, 482–491.e4. [Google Scholar] [CrossRef] [PubMed]

| Procedure | Mechanism of Action | Advantages | Limitations |
|---|---|---|---|
| Radiofrequency ablation (RFA) | Utilizes alternating electrical current to create a thermal ablation zone in the tissue. | Inexpensive compared to other ablation modalities. Widespread availability. | Serious adverse events include pancreatic fistula, acute pancreatitis, portal vein thrombosis, duodenal injury, biliary injury, gastric ulcer or fistula, hemoperitoneum, and liver failure. |
| Microwave ablation (MWA) | Creates a zone of ablation by generating frictional heat through agitation of water molecules. | Relatively larger ablation zones and faster ablation times compared to RFA. Does not require grounding pads. | Possible adverse events include mild pancreatitis, asymptomatic hyperamylasemia, pancreatic ascites, and minor bleeding. |
| Cryoablation | Utilizes changes in argon gas pressure to generate freeze–thaw cycles (i.e., the Joule–Thomson effect) in the tissue. The probe tip can reach temperatures as low as −185 °C, inducing cell death in the surrounding tissue. | Good visualization of ice ball, and less postoperative pain and damage to nearby critical structures when compared to RFA and MWA. | Possible postoperative complications include pancreatic or bile leak, gastrointestinal bleeding or obstruction, delayed gastric emptying, infection, or intra-abdominal bleeding. |
| Irreversible electroporation (IRE) | Nonthermal process uses DC surrent to create permanent pores in cell membrane, increasing the permeability and inducing cell death. | Nonthermal and is not limited by the heat-sink effect like the thermal ablation modalities. Preferred method when working near vascular and other critical structures. | Risk for generating cardiac arrhythmias. Need for general anesthesia with cardiac monitoring and muscle relaxation. Probe placement has to be parallel. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Narayanan, G.; Daye, D.; Wilson, N.M.; Noman, R.; Mahendra, A.M.; Doshi, M.H. Ablation in Pancreatic Cancer: Past, Present and Future. Cancers 2021, 13, 2511. https://doi.org/10.3390/cancers13112511
Narayanan G, Daye D, Wilson NM, Noman R, Mahendra AM, Doshi MH. Ablation in Pancreatic Cancer: Past, Present and Future. Cancers. 2021; 13(11):2511. https://doi.org/10.3390/cancers13112511
Chicago/Turabian StyleNarayanan, Govindarajan, Dania Daye, Nicole M. Wilson, Raihan Noman, Ashwin M. Mahendra, and Mehul H. Doshi. 2021. "Ablation in Pancreatic Cancer: Past, Present and Future" Cancers 13, no. 11: 2511. https://doi.org/10.3390/cancers13112511
APA StyleNarayanan, G., Daye, D., Wilson, N. M., Noman, R., Mahendra, A. M., & Doshi, M. H. (2021). Ablation in Pancreatic Cancer: Past, Present and Future. Cancers, 13(11), 2511. https://doi.org/10.3390/cancers13112511








