Angiogenesis-Related Functions of Wnt Signaling in Colorectal Carcinogenesis
Abstract
Simple Summary
Abstract
1. Introduction
2. Wnt/β-Catenin Signaling and Colorectal Cancer–General Comments
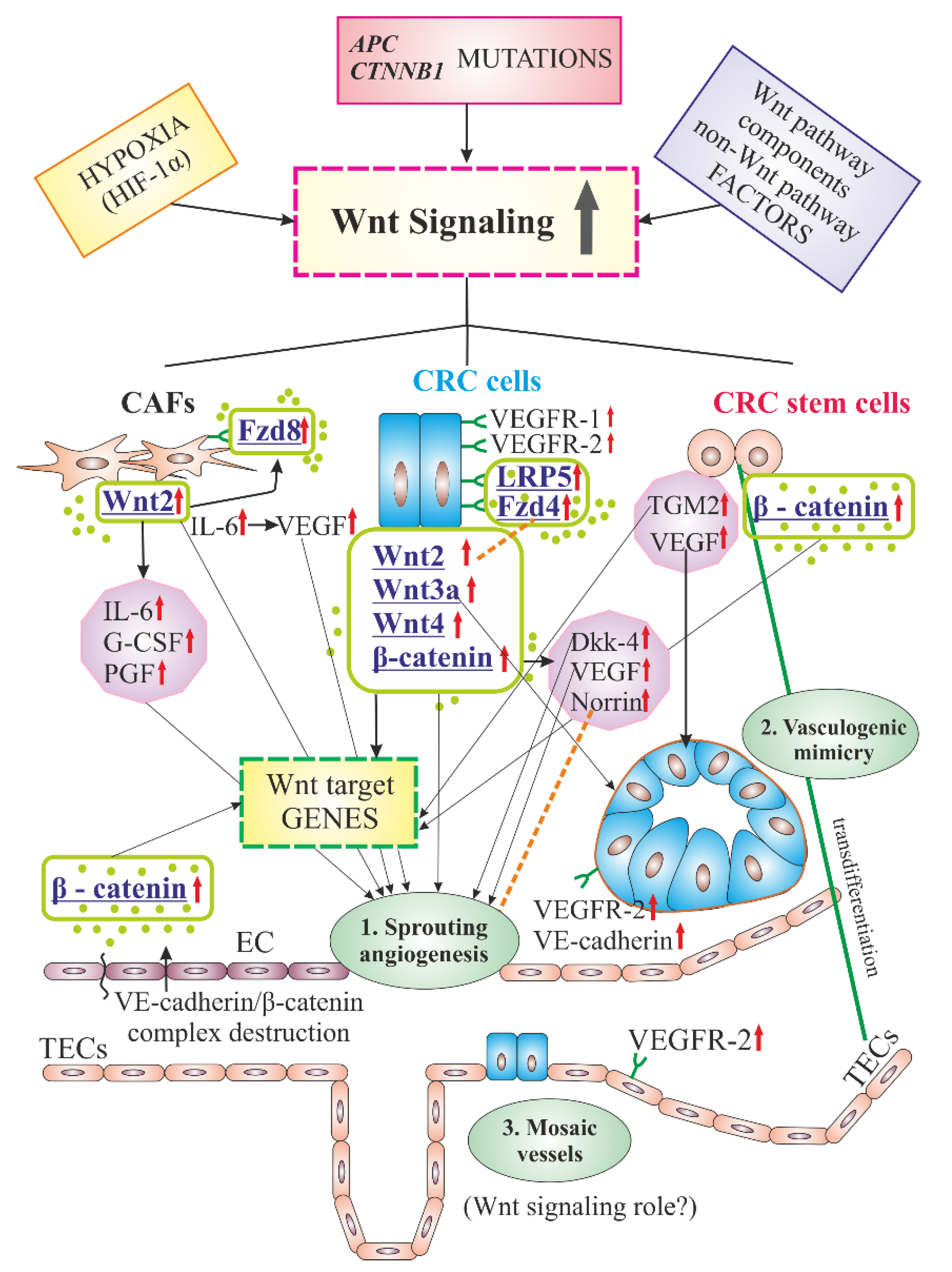
3. Typical Features of Angiogenesis in Solid Tumors (Including Colorectal Cancer (CRC))
4. Factors Promoting CRC Angiogenesis via Wnt/β-Catenin Signaling
5. Factors Inhibiting CRC Angiogenesis via Wnt/β-Catenin Signaling
6. Cellular Components of Tumors in Angiogenesis-Related Functions of Wnt/β-Catenin Signaling in CRC
6.1. Tumor Cells
6.2. Colorectal Cancer Stem(-Like) Cells (CRCSCs)
6.3. Cancer-Associated Fibroblasts (CAFs)
6.4. Tumor-Associated (Vascular) Endothelial Cells (TECs, TVECs)
7. Tissue Expression and Serum Levels of Wnt/β-Catenin Signaling Molecules–Diagnostic and Prognostic Role in CRC
8. Wnt/β-Catenin Signaling and Other Signalizing Partners in CRC Angiogenesis
9. The Role of Non-Coding RNAs in Angiogenesis via Wnt Signaling in CRC
9.1. MicroRNAs (miRNAs, miRs)
9.2. Long-Non Coding RNAs (lncRNAs)
9.3. Circular RNAs (circRNAs)
10. Anti-Angiogenic Therapy in CRC
Wnt/β-Catenin Signaling as a Potent Therapeutic Target in CRC-Associated Angiogenesis
11. Final Remarks and Future Perspectives
12. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| aa | Amino acids |
| Akt/AKT | Serine-threonine Protein Kinase (PKB, now called AKT1) |
| ANG-1, -2 | Angiopoietin-1, -2 |
| APC | Adenomatous Polyposis Coli |
| (b)FGF | (basic) Fibroblast Growth Factor |
| Bcl-2 | B-cell lymphoma protein |
| BCL9 | B cell CLL/lymphoma 9 protein |
| CDX | Caudal Type Homeobox-2 Protein |
| CD44, 184 | Cluster of Differentiation 44, 184 |
| COX-2 | Cyclooxygenase-2 |
| CRC | Colorectal Cancer |
| CXCL8 | C-X-C motif ligand 8 (chemokine) |
| CXCR4 | C-X-C chemokine receptor type 4 |
| DKK-1, -4 | Dickkopf-related protein 1;-4 |
| ECs | Endothelial Cells |
| ECM | Extracellular Matrix |
| EMT | Epithelial-Mesenchymal Transition |
| ERK1/2 | Extracellular Signal-regulated Kinase ½ |
| FAK | Focal Adhesion Kinase |
| FOXQ1 | Forkhead Box Q1 Protein |
| FRAT1 | Frequently Rearranged in Advanced T-cell Lymphoma 1 Protein |
| FRPs | Fzd-related Proteins |
| Fzd | Frizzleds proteins, a family of G protein-coupled receptor proteins |
| GDF-15 | Growth Differentiation Factor 15 |
| GSK3β | Glycogen Synthase Kinase 3 β |
| HIF-1α | Hypoxia-inducible Factor 1 α |
| HUVECs | Human Umbilical Vein ECs |
| IL | Interleukin |
| KRAS | Kirsten Rat Sarcoma Virus, proto-oncogene |
| LEF | Lymphoid Enhancer Factor |
| MAPK | A Mitogen-activated Protein Kinase |
| MMP-2, -9 | Matrix Metalloproteinase 2, 9 |
| MVD | Microvessel Density |
| PI3K | Phosphatidylinositol 3’ Kinase |
| PKA, B (AKT), C α | Protein Kinase A, B (AKT), C α |
| PKG | Type 1 cyclic Guanosine Monophosphate (cGMP)-dependent Protein Kinase |
| PLCγ1 | Phospholipase C γ1 |
| p-LPR6 | Phosphorylated Lipoprotein-related Protein 6 |
| ROS | Reactive Oxygen Species |
| RAR | Retinoic Acid Receptor |
| RORα | RAR-related Orphan Receptor α; |
| RYK | Related to Receptor Tyrosine Kinase protein |
| SALL4 | Zink Finger Transcription Factor Spalt (Sall)-like Protein 4 |
| SFRP2 | Secreted Frizzled-related Protein 2 |
| SMAD4 | SMAD family member 4, Mothers Against Decapentaplegic Homolog 4 |
| SMAR1 | Scaffold/Matrix Attachment Region Binding Protein 1 |
| STAT3 | Signal Transducer and Activator of Transcription Protein Activator of Transcription 3 |
| Tan IIA, TSA | Tanshinone IIA |
| TCF | T cell Factor, Transcription Factor |
| TCF7L2 | Transcription Factor 7-like 2 |
| TGF-β | Tumor Growth Factor beta |
| TGM2 | Tissue Transglutaminase 2 |
| TIPE2 (TNFAIP8L2) | TNFα-induced protein 8 like 2 |
| TNF-α | Tumor Necrosis Factor α |
| TNM | T—tumor; N—lymph nodes; M—metastasis |
| TOPFlash | TCF Reporter Plasmid |
| TP53 | Tumor Protein 53 |
| 3’UTR | 3’ Untranslated Region |
| VEGF | Vascular Endothelial Growth Factor |
| VEGF (R) | Vascular Endothelial Growth Factor (Receptor) |
References
- Gregorieff, A.; Clevers, H. Wnt signaling in the intestinal epithelium: From endoderm to cancer. Genes Dev. 2005, 19, 877–890. [Google Scholar] [CrossRef]
- Tenbaum, S.P.; Ordóñez-Morán, P.; Puig, I.; Chicote, I.; Arqués, O.; Landolfi, S.; Fernández, Y.; Herance, J.R.; Gispert, J.D.; Mendizabal, L.; et al. β-catenin confers resistance to PI3K and AKT inhibitors and subverts FOXO3a to promote metastasis in colon cancer. Nat. Med. 2012, 18, 892–901. [Google Scholar] [CrossRef]
- Zhan, T.; Rindtorff, N.; Boutros, M. Wnt signaling in cancer. Oncogene 2017, 36, 1461–1473. [Google Scholar] [CrossRef]
- Wiese, K.E.; Nusse, R.; van Amerongen, R. Wnt signalling: Conquering complexity. Development 2018, 145. [Google Scholar] [CrossRef]
- Nusse, R.; Varmus, H.E. Many tumors induced by the mouse mammary tumor virus contain a provirus integrated in the same region of the host genome. Cell 1982, 31, 99–109. [Google Scholar] [CrossRef]
- Chien, A.J.; Conrad, W.H.; Moon, R.T. A Wnt survival guide: From flies to human disease. J. Investig. Dermatol. 2009, 129, 1614–1627. [Google Scholar] [CrossRef]
- Nusse, R.; Varmus, H. Three decades of Wnts: A personal perspective on how a scientific field developed. EMBO J. 2012, 31, 2670–2684. [Google Scholar] [CrossRef]
- White, B.D.; Chien, A.J.; Dawson, D.W. Dysregulation of Wnt/β-catenin signaling in gastrointestinal cancers. Gastroenterology 2012, 142, 219–232. [Google Scholar] [CrossRef]
- Nusse, R.; Clevers, H. Wnt/β-Catenin Signaling, Disease, and Emerging Therapeutic Modalities. Cell 2017, 169, 985–999. [Google Scholar] [CrossRef]
- Zeitlin, B.D.; Ellis, L.M.; Nör, J.E. Inhibition of Vascular Endothelial Growth Factor Receptor-1/Wnt/{beta}-catenin Crosstalk Leads to Tumor Cell Death. Clin. Cancer Res. 2009, 15, 7453–7455. [Google Scholar] [CrossRef]
- Qi, L.; Song, W.; Liu, Z.; Zhao, X.; Cao, W.; Sun, B. Wnt3a Promotes the Vasculogenic Mimicry Formation of Colon Cancer via Wnt/β-Catenin Signaling. Int. J. Mol. Sci. 2015, 16, 18564–18579. [Google Scholar] [CrossRef]
- Olsen, J.J.; Pohl, S.Ö.; Deshmukh, A.; Visweswaran, M.; Ward, N.C.; Arfuso, F.; Agostino, M.; Dharmarajan, A. The Role of Wnt Signalling in Angiogenesis. Clin. Biochem. Rev. 2017, 38, 131–142. [Google Scholar] [PubMed]
- Goodwin, A.M.; D’Amore, P.A. Wnt signaling in the vasculature. Angiogenesis 2002, 5, 1–9. [Google Scholar] [CrossRef]
- Nie, X.; Liu, H.; Liu, L.; Wang, Y.D.; Chen, W.D. Emerging Roles of Wnt Ligands in Human Colorectal Cancer. Front. Oncol. 2020, 10. [Google Scholar] [CrossRef]
- Fodde, R.; Brabletz, T. Wnt/beta-catenin signaling in cancer stemness and malignant behavior. Curr. Opin. Cell Biol. 2007, 19, 150–158. [Google Scholar] [CrossRef]
- Vermeulen, L.; Felipe De Sousa, E.M.; Van Der Heijden, M.; Cameron, K.; De Jong, J.H.; Borovski, T.; Tuynman, J.B.; Todaro, M.; Merz, C.; Rodermond, H.; et al. Wnt activity defines colon cancer stem cells and is regulated by the microenvironment. Nat. Cell Biol. 2010, 12, 468–476. [Google Scholar] [CrossRef]
- Teeuwssen, M.; Fodde, R. Cell Heterogeneity and Phenotypic Plasticity in Metastasis Formation: The Case of Colon Cancer. Cancers 2019, 11, 1368, Correction in Cancers 2020, 12, 1392. [Google Scholar] [CrossRef]
- Keum, N.; Giovannucci, E. Global burden of colorectal cancer: Emerging trends, risk factors and prevention strategies. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 713–732. [Google Scholar] [CrossRef]
- He, F.; Chen, H.; Yang, P.; Yin, H.; Zhang, X.; He, T.; Song, S.; Sun, S.; Wang, B.; Li, Z.; et al. Gankyrin sustains PI3K/GSK-3β/β-catenin signal activation and promotes colorectal cancer aggressiveness and progression. Oncotarget 2016, 7, 81156–81171. [Google Scholar] [CrossRef]
- Lee, S.K.; Hwang, J.H.; Choi, K.Y. Interaction of the Wnt/β-catenin and RAS-ERK pathways involving co-stabilization of both β-catenin and RAS plays important roles in the colorectal tumorigenesis. Adv. Biol. Regul. 2018, 68, 46–54. [Google Scholar] [CrossRef]
- Fearon, E.R.; Vogelstein, B. A genetic model for colorectal tumorigenesis. Cell 1990, 61, 759–767. [Google Scholar] [CrossRef]
- Gerstung, M.; Jolly, C.; Leshchiner, I.; Dentro, S.C.; Gonzalez, S.; Rosebrock, D.; Mitchell, T.J.; Rubanova, Y.; Anur, P.; Yu, K.; et al. The evolutionary history of 2658 cancers. Nature 2020, 578, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Li, Y.; Semenov, M.; Han, C.; Baeg, G.H.; Tan, Y.; Zhang, Z.; Lin, X.; He, X. Control of beta-catenin phosphorylation/degradation by a dual-kinase mechanism. Cell 2002, 108, 837–847. [Google Scholar] [CrossRef]
- Mayer, C.D.; Giclais, S.M.; Alsehly, F.; Hoppler, S. Diverse LEF/TCF Expression in Human Colorectal Cancer Correlates with Altered Wnt-Regulated Transcriptome in a Meta-Analysis of Patient Biopsies. Genes 2020, 11, 538. [Google Scholar] [CrossRef]
- Doumpas, N.; Lampart, F.; Robinson, M.D.; Lentini, A.; Nestor, C.E.; Cantù, C.; Basler, K. TCF/LEF dependent and independent transcriptional regulation of Wnt/β-catenin target genes. EMBO J. 2019, 38. [Google Scholar] [CrossRef]
- Brabletz, T.; Jung, A.; Hermann, K.; Günther, K.; Hohenberger, W.; Kirchner, T. Nuclear overexpression of the oncoprotein beta-catenin in colorectal cancer is localized predominantly at the invasion front. Pathol. Res. Pract. 1998, 194, 701–704. [Google Scholar] [CrossRef]
- Yaeger, R.; Chatila, W.K.; Lipsyc, M.D.; Hechtman, J.F.; Cercek, A.; Sanchez-Vega, F.; Jayakumaran, G.; Middha, S.; Zehir, A.; Donoghue, M.T.A.; et al. Clinical Sequencing Defines the Genomic Landscape of Metastatic Colorectal Cancer. Cancer Cell 2018, 33, 125–136. [Google Scholar] [CrossRef]
- Albuquerque, C.; Baltazar, C.; Filipe, B.; Penha, F.; Pereira, T.; Smits, R.; Cravo, M.; Lage, P.; Fidalgo, P.; Claro, I.; et al. Colorectal cancers show distinct mutation spectra in members of the canonical WNT signaling pathway according to their anatomical location and type of genetic instability. Genes Chromosomes Cancer 2010, 49, 746–759. [Google Scholar] [CrossRef]
- Günther, K.; Brabletz, T.; Kraus, C.; Dworak, O.; Reymond, M.A.; Jung, A.; Hohenberger, W.; Kirchner, T.; Köckerling, F.; Ballhausen, W.G. Predictive value of nuclear betacatenin expression for the occurrence of distant metastases in rectal cancer. Dis. Colon Rectum 1998, 41, 1256–1261. [Google Scholar] [CrossRef]
- Zhao, H.; He, L.; Yin, D.; Song, B. Identification of β-catenin target genes in colorectal cancer by interrogating gene fitness screening data. Oncol. Lett. 2019, 18, 3769–3777. [Google Scholar] [CrossRef]
- Song, J.; Shu, H.; Zhang, L.; Xiong, J. Long noncoding RNA GAS5 inhibits angiogenesis and metastasis of colorectal cancer through the Wnt/β-catenin signaling pathway. J. Cell Biochem. 2019, 120, 6937–6951. [Google Scholar] [CrossRef] [PubMed]
- Sadanandam, A.; Lyssiotis, C.A.; Homicsko, K.; Collisson, E.A.; Gibb, W.J.; Wullschleger, S.; Ostos, L.C.; Lannon, W.A.; Grotzinger, C.; Del Rio, M.; et al. A colorectal cancer classification system that associates cellular phenotype and responses to therapy. Nat. Med. 2013, 19, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Guinney, J.; Dienstmann, R.; Wang, X.; de Reyniès, A.; Schlicker, A.; Soneson, C.; Marisa, L.; Roepman, P.; Nyamundanda, G.; Angelino, P.; et al. The consensus molecular subtypes of colorectal cancer. Nat. Med. 2015, 21, 1350–1356. [Google Scholar] [CrossRef]
- Isella, C.; Brundu, F.; Bellomo, S.E.; Galimi, F.; Zanella, E.; Porporato, R.; Petti, C.; Fiori, A.; Orzan, F.; Senetta, R.; et al. Selective analysis of cancer-cell intrinsic transcriptional traits defines novel clinically relevant subtypes of colorectal cancer. Nat. Commun. 2017, 8, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Mathonnet, M.; Perraud, A.; Christou, N.; Akil, H.; Melin, C.; Battu, S.; Jauberteau, M.O.; Denizot, Y. Hallmarks in colorectal cancer: Angiogenesis and cancer stem-like cells. World J. Gastroenterol. 2014, 20, 4189–4196. [Google Scholar] [CrossRef]
- Mody, K.; Baldeo, C.; Bekaii-Saab, T. Antiangiogenic Therapy in Colorectal Cancer. Cancer J. 2018, 24, 165–170. [Google Scholar] [CrossRef]
- Chen, W.Z.; Jiang, J.X.; Yu, X.Y.; Xia, W.J.; Yu, P.X.; Wang, K.; Zhao, Z.Y.; Chen, Z.G. Endothelial cells in colorectal cancer. World J. Gastrointest. Oncol. 2019, 11, 946–956. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. The hallmarks of cancer. Cell 2000, 100, 57–70. [Google Scholar] [CrossRef]
- Xing, Y.; Tu, J.; Zheng, L.; Guo, L.; Xi, T. Anti-angiogenic effect of tanshinone IIA involves inhibition of the VEGF/VEGFR2 pathway in vascular endothelial cells. Oncol. Rep. 2015, 33, 163–170. [Google Scholar] [CrossRef]
- Lizárraga-Verdugo, E.; Avendaño-Félix, M.; Bermúdez, M.; Ramos-Payán, R.; Pérez-Plasencia, C.; Aguilar-Medina, M. Cancer Stem Cells and Its Role in Angiogenesis and Vasculogenic Mimicry in Gastrointestinal Cancers. Front. Oncol. 2020, 10. [Google Scholar] [CrossRef]
- Hillen, F.; Griffioen, A.W. Tumour vascularization: Sprouting angiogenesis and beyond. Cancer Metastasis Rev. 2007, 26, 489–502. [Google Scholar] [CrossRef]
- Patan, S.; Munn, L.L.; Jain, R.K. Intussusceptive microvascular growth in a human colon adenocarcinoma xenograft: A novel mechanism of tumor angiogenesis. Microvasc. Res. 1996, 51, 260–272. [Google Scholar] [CrossRef] [PubMed]
- Maniotis, A.J.; Folberg, R.; Hess, A.; Seftor, E.A.; Gardner, L.M.; Pe’er, J.; Trent, J.M.; Meltzer, P.S.; Hendrix, M.J. Vascular channel formation by human melanoma cells in vivo and in vitro: Vasculogenic mimicry. Am. J. Pathol. 1999, 155, 739–752. [Google Scholar] [CrossRef]
- Folberg, R.; Hendrix, M.J.; Maniotis, A.J. Vasculogenic mimicry and tumor angiogenesis. Am. J. Pathol. 2000, 156, 361–381. [Google Scholar] [CrossRef]
- Chang, Y.S.; di Tomaso, E.; McDonald, D.M.; Jones, R.; Jain, R.K.; Munn, L.L. Mosaic blood vessels in tumors: Frequency of cancer cells in contact with flowing blood. Proc. Natl. Acad. Sci. USA 2000, 97, 14608–14613. [Google Scholar] [CrossRef]
- Folkman, J. Role of angiogenesis in tumor growth and metastasis. Semin. Oncol. 2002, 29 (Suppl. S16), 15–18. [Google Scholar] [CrossRef]
- Qian, C.N.; Tan, M.H.; Yang, J.P.; Cao, Y. Revisiting tumor angiogenesis: Vessel co-option, vessel remodeling, and cancer cell-derived vasculature formation. Chin. J. Cancer. 2016, 35, 10. [Google Scholar] [CrossRef]
- Liu, Z.; Sun, B.; Qi, L.; Li, H.; Gao, J.; Leng, X. Zinc finger E-box binding homeobox 1 promotes vasculogenic mimicry in colorectal cancer through induction of epithelial-to-mesenchymal transition. Cancer Sci. 2012, 103, 813–820. [Google Scholar] [CrossRef]
- Baeriswyl, V.; Christofori, G. The angiogenic switch in carcinogenesis. Semin. Cancer Biol. 2009, 19, 329–337. [Google Scholar] [CrossRef]
- Shahneh, F.Z.; Baradaran, B.; Zamani, F.; Aghebati-Maleki, L. Tumor angiogenesis and anti-angiogenic therapies. Hum. Antibodies 2013, 22, 15–19. [Google Scholar] [CrossRef]
- Soheilifar, M.; Grusch, M.; Neghab, H.K.; Amini, R.; Maadi, H.; Saidijam, M.; Wang, Z. Angioregulatory microRNAs in Colorectal Cancer. Cancers 2019, 12, 71. [Google Scholar] [CrossRef]
- Folkman, J.; D’Amore, P.A. Blood vessel formation: What is its molecular basis? Cell 1996, 87, 1153–1155. [Google Scholar] [CrossRef]
- Salinas-Vera, Y.M.; Marchat, L.A.; Gallardo-Rincón, D.; Ruiz-García, E.; Astudillo-De La Vega, H.; Echavarría-Zepeda, R.; López-Camarillo, C. AngiomiRs: MicroRNAs driving angiogenesis in cancer. Int. J. Mol. Med. 2019, 43, 657–670. [Google Scholar] [CrossRef]
- Bridges, E.M.; Harris, A.L. The angiogenic process as a therapeutic target in cancer. Biochem. Pharmacol. 2011, 81, 1183–1191. [Google Scholar] [CrossRef]
- Zhang, Z.; Neiva, K.G.; Lingen, M.W.; Ellis, L.M.; Nör, J.E. VEGF-dependent tumor angiogenesis requires inverse and reciprocal regulation of VEGFR1 and VEGFR2. Cell Death Differ. 2010, 17, 499–512. [Google Scholar] [CrossRef]
- Carmeliet, P.; Dor, Y.; Herbert, J.M.; Fukumura, D.; Brusselmans, K.; Dewerchin, M.; Neeman, M.; Bono, F.; Abramovitch, R.; Maxwell, P.; et al. Role of HIF-1α in hypoxia-mediated apoptosis, cell proliferation and tumour angiogenesis. Nature 1998, 394, 485–490. [Google Scholar] [CrossRef]
- Sun, X.; Hu, F.; Hou, Z.; Chen, Q.; Lan, J.; Luo, X.; Wang, G.; Hu, J.; Cao, Z. SIX4 activates Akt and promotes tumor angiogenesis. Exp. Cell Res. 2019, 383. [Google Scholar] [CrossRef]
- Krishnamachary, B.; Berg-Dixon, S.; Kelly, B.; Agani, F.; Feldser, D.; Ferreira, G.; Iyer, N.; LaRusch, J.; Pak, B.; Taghavi, P.; et al. Regulation of colon carcinoma cell invasion by hypoxia-inducible factor 1. Cancer Res. 2003, 63, 1138–1143. [Google Scholar]
- Zhang, X.; Gaspard, J.P.; Chung, D.C. Regulation of vascular endothelial growth factor by the Wnt and K-ras pathways in colonic neoplasia. Cancer Res. 2001, 61, 6050–6054. [Google Scholar]
- Easwaran, V.; Lee, S.H.; Inge, L.; Guo, L.; Goldbeck, C.; Garrett, E.; Wiesmann, M.; Garcia, P.D.; Fuller, J.H.; Chan, V.; et al. β-Catenin regulates vascular endothelial growth factor expression in colon cancer. Cancer Res. 2003, 63, 3145–3153. [Google Scholar]
- Dılek, F.H.; Topak, N.; Tokyol, Ç.; Akbulut, G.; Dılek, O.N. β-Catenin and its relation to VEGF and cyclin D1 expression in pT3 rectosigmoid cancers. Turk. J. Gastroenterol. 2010, 21, 365–371. [Google Scholar] [CrossRef]
- Fan, F.; Wey, J.S.; McCarty, M.F.; Belcheva, A.; Liu, W.; Bauer, T.W.; Somcio, R.J.; Wu, Y.; Hooper, A.; Hicklin, D.J.; et al. Expression and function of vascular endothelial growth factor receptor-1 on human colorectal cancer cells. Oncogene 2005, 24, 2647–2653. [Google Scholar] [CrossRef]
- Ahluwalia, A.; Jones, M.K.; Szabo, S.; Tarnawski, A.S. Aberrant, ectopic expression of VEGF and VEGF receptors 1 and 2 in malignant colonic epithelial cells. Implications for these cells growth via an autocrine mechanism. Biochem. Biophys. Res. Commun. 2013, 437, 515–520. [Google Scholar] [CrossRef]
- Catalano, V.; Turdo, A.; Di Franco, S.; Dieli, F.; Todaro, M.; Stassi, G. Tumor and its microenvironment: A synergistic interplay. Semin. Cancer Biol. 2013, 23, 522–532. [Google Scholar] [CrossRef]
- Naik, S.; Dothager, R.S.; Marasa, J.; Lewis, C.L.; Piwnica-Worms, D. Vascular Endothelial Growth Factor Receptor-1 Is Synthetic Lethal to Aberrant {beta}-Catenin Activation in Colon Cancer. Clin. Cancer Res. 2009, 15, 7529–7537. [Google Scholar] [CrossRef]
- Pate, K.T.; Stringari, C.; Sprowl-Tanio, S.; Wang, K.; TeSlaa, T.; Hoverter, N.P.; McQuade, M.M.; Garner, C.; Digman, M.A.; Teitell, M.A.; et al. Wnt signaling directs a metabolic program of glycolysis and angiogenesis in colon cancer. EMBO J. 2014, 33, 1454–1473. [Google Scholar] [CrossRef] [PubMed]
- Mani, M.; Carrasco, D.E.; Zhang, Y.; Takada, K.; Gatt, M.E.; Dutta-Simmons, J.; Ikeda, H.; Diaz-Griffero, F.; Pena-Cruz, V.; Bertagnolli, M.; et al. BCL9 promotes tumor progression by conferring enhanced proliferative, metastatic, and angiogenic properties to cancer cells. Cancer Res. 2009, 69, 7577–7586. [Google Scholar] [CrossRef]
- Vaish, V.; Sanyal, S.N. Role of Sulindac and Celecoxib in the regulation of angiogenesis during the early neoplasm of colon: Exploring PI3-K/PTEN/Akt pathway to the canonical Wnt/β-catenin signaling. Biomed. Pharmacother. 2012, 66, 354–367. [Google Scholar] [CrossRef]
- Santoyo-Ramos, P.; Likhatcheva, M.; García-Zepeda, E.A.; Castañeda-Patlán, M.C.; Robles-Flores, M. Hypoxia-inducible factors modulate the stemness and malignancy of colon cancer cells by playing opposite roles in canonical Wnt signaling. PLoS ONE 2014, 9. [Google Scholar] [CrossRef]
- Kumar, A.; Cherukumilli, M.; Mahmoudpour, S.H.; Brand, K.; Bandapalli, O.R. ShRNA-mediated knock-down of CXCL8 inhibits tumor growth in colorectal liver metastasis. Biochem. Biophys. Res. Commun. 2018, 500, 731–737. [Google Scholar] [CrossRef]
- Suman, S.; Kurisetty, V.; Das, T.P.; Vadodkar, A.; Ramos, G.; Lakshmanaswamy, R.; Damodaran, C. Activation of AKT signaling promotes epithelial-mesenchymal transition and tumor growth in colorectal cancer cells. Mol. Carcinog. 2014, 53 (Suppl. 1), E151–E160. [Google Scholar] [CrossRef]
- Lin, H.; Fang, Z.; Su, Y.; Li, P.; Wang, J.; Liao, H.; Hu, Q.; Ye, C.; Fang, Y.; Luo, Q.; et al. DHX32 Promotes Angiogenesis in Colorectal Cancer Through Augmenting β-catenin Signaling to Induce Expression of VEGFA. EBioMedicine 2017, 18, 62–72. [Google Scholar] [CrossRef]
- Kumaradevan, S.; Lee, S.Y.; Richards, S.; Agani, F.; Feldser, D.; Ferreira, G.; Iyer, N.; LaRusch, J.; Pak, B.; Taghavi, P.; et al. c-Cbl Expression Correlates with Human Colorectal Cancer Survival and Its Wnt/β-Catenin Suppressor Function Is Regulated by Tyr371 Phosphorylation. Am. J. Pathol. 2018, 188, 1921–1933. [Google Scholar] [CrossRef]
- Dupasquier, S.; Blache, P.; Picque Lasorsa, L.; Zhao, H.; Abraham, J.D.; Haigh, J.J.; Ychou, M.; Prévostel, C. Modulating PKCα Activity to Target Wnt/β-Catenin Signaling in Colon Cancer. Cancers 2019, 11, 693. [Google Scholar] [CrossRef]
- Yang, P.; Yu, D.; Zhou, J.; Zhuang, S.; Jiang, T. TGM2 interference regulates the angiogenesis and apoptosis of colorectal cancer via Wnt/β-catenin pathway. Cell Cycle 2019, 18, 1122–1134. [Google Scholar] [CrossRef]
- Böhm, J.; Sustmann, C.; Wilhelm, C.; Kohlhase, J. SALL4 is directly activated by TCF/LEF in the canonical Wnt signaling pathway. Biochem. Biophys. Res. Commun. 2006, 348, 898–907. [Google Scholar] [CrossRef]
- Peng, X.; Luo, Z.; Kang, Q.; Deng, D.; Wang, Q.; Peng, H.; Wang, S.; Wei, Z. FOXQ1 mediates the crosstalk between TGF-β and Wnt signaling pathways in the progression of colorectal cancer. Cancer Biol. Ther. 2015, 16, 1099–1109. [Google Scholar] [CrossRef]
- Hao, L.; Zhao, Y.; Wang, Z.; Yin, H.; Zhang, X.; He, T.; Song, S.; Sun, S.; Wang, B.; Li, Z.; et al. Expression and clinical significance of SALL4 and β-catenin in colorectal cancer. J. Mol. Histol. 2016, 47, 117–128. [Google Scholar] [CrossRef]
- Sampietro, J.; Dahlberg, C.L.; Cho, U.S.; Hinds, T.R.; Kimelman, D.; Xu, W. Crystal structure of a β-catenin/BCL9/Tcf4 complex. Mol. Cell. 2006, 24, 293–300. [Google Scholar] [CrossRef]
- Mosimann, C.; Hausmann, G.; Basler, K. β-catenin hits chromatin: Regulation of Wnt target gene activation. Nat. Rev. Mol. Cell Biol. 2009, 10, 276–286. [Google Scholar] [CrossRef]
- Pendás-Franco, N.; García, J.M.; Peña, C.; Valle, N.; Pálmer, H.G.; Heinäniemi, M.; Carlberg, C.; Jiménez, B.; Bonilla, F.; Muñoz, A.; et al. DICKKOPF-4 is induced by TCF/β-catenin and upregulated in human colon cancer, promotes tumour cell invasion and angiogenesis and is repressed by 1α,25-dihydroxyvitamin D3. Oncogene 2008, 27, 4467–4477. [Google Scholar] [CrossRef]
- Jiang, M.; Kang, Y.; Sewastianik, T.; Wang, J.; Tanton, H.; Alder, K.; Dennis, P.; Xin, Y.; Wang, Z.; Liu, R.; et al. BCL9 provides multi-cellular communication properties in colorectal cancer by interacting with paraspeckle proteins. Nat. Commun. 2020, 11. [Google Scholar] [CrossRef]
- Takada, K.; Zhu, D.; Bird, G.H.; Sukhdeo, K.; Zhao, J.J.; Mani, M.; Lemieux, M.; Carrasco, D.E.; Ryan, J.; Horst, D.; et al. Targeted disruption of the BCL9/β-catenin complex inhibits oncogenic Wnt signaling. Sci. Transl. Med. 2012, 4. [Google Scholar] [CrossRef]
- Hu, T.H.; Yao, Y.; Yu, S.; Han, L.L.; Wang, W.J.; Guo, H.; Tian, T.; Ruan, Z.P.; Kang, X.M.; Wang, J.; et al. SDF-1/CXCR4 promotes epithelial-mesenchymal transition and progression of colorectal cancer by activation of the Wnt/β-catenin signaling pathway. Cancer Lett. 2014, 354, 417–426. [Google Scholar] [CrossRef]
- Cheng, H.; Sun, X.; Li, J.; He, P.; Liu, W.; Meng, X. Knockdown of Uba2 inhibits colorectal cancer cell invasion and migration through downregulation of the Wnt/β-catenin signaling pathway. J. Cell Biochem. 2018, 119, 6914–6925. [Google Scholar] [CrossRef]
- Ayinde, O.; Wang, Z.; Pinton, G.; Moro, L.; Griffin, M. Transglutaminase 2 maintains a colorectal cancer stem phenotype by regulating epithelial-mesenchymal transition. Oncotarget 2019, 10, 4556–4569. [Google Scholar] [CrossRef]
- Sun, J.; Zhao, Z.; Zhang, W.; Tang, Q.; Yang, F.; Hu, X.; Liu, C.; Song, B.; Zhang, B.; Wang, H. Spalt-Like Protein 4 (SALL4) Promotes Angiogenesis by Activating Vascular Endothelial Growth Factor A (VEGFA) Signaling. Med. Sci. Monit. 2020, 26. [Google Scholar] [CrossRef]
- Pan, Q.; Pan, H.; Lou, H.; Xu, Y.; Tian, L. Inhibition of the angiogenesis and growth of Aloin in human colorectal cancer in vitro and in vivo. Cancer Cell Int. 2013, 13. [Google Scholar] [CrossRef]
- Peng, C.; Zhang, W.; Dai, C.; Li, W.; Shen, X.; Yuan, Y.; Yan, L.; Zhang, W.; Yao, M. Study of the aqueous extract of Aloe vera and its two active components on the Wnt/β-catenin and Notch signaling pathways in colorectal cancer cells. J. Ethnopharmacol. 2019, 243. [Google Scholar] [CrossRef]
- Liu, Z.; Sun, B.; Qi, L.; Li, Y.; Zhao, X.; Zhang, D.; Zhang, Y. Dickkopf-1 expression is down-regulated during the colorectal adenoma-carcinoma sequence and correlates with reduced microvessel density and VEGF expression. Histopathology 2015, 67, 158–166. [Google Scholar] [CrossRef]
- Wu, D.D.; Liu, S.Y.; Gao, Y.R.; Lu, D.; Hong, Y.; Chen, Y.G.; Dong, P.Z.; Wang, D.Y.; Li, T.; Li, H.M.; et al. Tumour necrosis factor-α-induced protein 8-like 2 is a novel regulator of proliferation, migration, and invasion in human rectal adenocarcinoma cells. J. Cell Mol. Med. 2019, 23, 1698–1713. [Google Scholar] [CrossRef]
- Lou, Y.; Liu, S. The TIPE (TNFAIP8) family in inflammation, immunity, and cancer. Mol. Immunol. 2011, 49, 4–7. [Google Scholar] [CrossRef]
- Kwon, I.K.; Schoenlein, P.V.; Delk, J.; Liu, K.; Thangaraju, M.; Dulin, N.O.; Ganapathy, V.; Berger, F.G.; Browning, D.D. Expression of cyclic guanosine monophosphate-dependent protein kinase in metastatic colon carcinoma cells blocks tumor angiogenesis. Cancer 2008, 112, 1462–1470. [Google Scholar] [CrossRef]
- Taye, N.; Alam, A.; Ghorai, S.; Chatterji, D.G.; Parulekar, A.; Mogare, D.; Singh, S.; Sengupta, P.; Chatterjee, S.; Bhat, M.K.; et al. SMAR1 inhibits Wnt/β-catenin signaling and prevents colorectal cancer progression. Oncotarget 2018, 9, 21322–21336. [Google Scholar] [CrossRef][Green Version]
- Lee, J.M.; Kim, I.S.; Kim, H.; Lee, J.S.; Kim, K.; Yim, H.Y.; Jeong, J.; Kim, J.H.; Kim, J.Y.; Lee, H.; et al. RORalpha attenuates Wnt/beta-catenin signaling by PKCalpha-dependent phosphorylation in colon cancer. Mol. Cell 2010, 37, 183–195. [Google Scholar] [CrossRef]
- Gwak, J.; Cho, M.; Gong, S.J.; Won, J.; Kim, D.E.; Kim, E.Y.; Lee, S.S.; Kim, M.; Kim, T.K.; Shin, J.G.; et al. Protein-kinase-C-mediated β-catenin phosphorylation negatively regulates the Wnt/ β-catenin pathway. J. Cell Sci. 2006, 119, 4702–4709. [Google Scholar] [CrossRef]
- Yang, C.; Zhang, J.J.; Zhang, X.P.; Xiao, R.; Li, P.G. Sporamin suppresses growth of xenografted colorectal carcinoma in athymic BALB/c mice by inhibiting liver β-catenin and vascular endothelial growth factor expression. World J. Gastroenterol. 2019, 25, 3196–3206. [Google Scholar] [CrossRef]
- Sui, H.; Zhao, J.; Zhou, L.; Wen, H.; Deng, W.; Li, C.; Ji, Q.; Liu, X.; Feng, Y.; Chai, N.; et al. Tanshinone IIA inhibits β-catenin/VEGF-mediated angiogenesis by targeting TGF-β1 in normoxic and HIF-1α in hypoxic microenvironments in human colorectal cancer. Cancer Lett. 2017, 403, 86–97. [Google Scholar] [CrossRef]
- Pooja, T.; Karunagaran, D. Emodin suppresses Wnt signaling in human colorectal cancer cells SW480 and SW620. Eur. J. Pharmacol. 2014, 742, 55–64. [Google Scholar] [CrossRef]
- Gu, J.; Cui, C.F.; Yang, L.; Wang, L.; Jiang, X.H. Emodin Inhibits Colon Cancer Cell Invasion and Migration by Suppressing Epithelial-Mesenchymal Transition via the Wnt/β-Catenin Pathway. Oncol. Res. 2019, 27, 193–202. [Google Scholar] [CrossRef]
- Farombi, E.O.; Ajayi, B.O.; Adedara, I.A. 6-Gingerol delays tumorigenesis in benzo [a] pyrene and dextran sulphate sodium-induced colorectal cancer in mice. Food Chem. Toxicol. 2020, 142. [Google Scholar] [CrossRef]
- de Lima, R.M.T.; Dos Reis, A.C.; de Menezes, A.P.M.; Santos, J.V.O.; Filho, J.W.G.O.; Ferreira, J.R.O.; de Alencar, M.V.O.B.; da Mata, A.M.O.F.; Khan, I.N.; Islam, A.; et al. Protective and therapeutic potential of ginger (Zingiber officinale) extract and [6]-gingerol in cancer: A comprehensive review. Phytother. Res. 2018, 32, 1885–1907. [Google Scholar] [CrossRef] [PubMed]
- Naz, I.; Ramchandani, S.; Khan, M.R.; Yang, M.H.; Ahn, K.S. Anticancer Potential of Raddeanin A, a Natural Triterpenoid Isolated from Anemone raddeana Regel. Molecules 2020, 25, 1035. [Google Scholar] [CrossRef]
- Wang, Y.; Bao, X.; Zhao, A.; Zhang, J.; Zhang, M.; Zhang, Q.; Ma, B. Raddeanin A inhibits growth and induces apoptosis in human colorectal cancer through downregulating the Wnt/β-catenin and NF-κB signaling pathway. Life Sci. 2018, 207, 532–549. [Google Scholar] [CrossRef]
- Guan, Y.Y.; Liu, H.J.; Luan, X.; Xu, J.R.; Lu, Q.; Liu, Y.R.; Gao, Y.G.; Zhao, M.; Chen, H.Z.; Fang, C. Raddeanin A, a triterpenoid saponin isolated from Anemone raddeana, suppresses the angiogenesis and growth of human colorectal tumor by inhibiting VEGFR2 signaling. Phytomedicine 2015, 22, 103–110. [Google Scholar] [CrossRef]
- Unterleuthner, D.; Neuhold, P.; Schwarz, K.; Janker, L.; Neuditschko, B.; Nivarthi, H.; Crncec, I.; Kramer, N.; Unger, C.; Hengstschläger, M.; et al. Cancer-associated fibroblast-derived WNT2 increases tumor angiogenesis in colon cancer. Angiogenesis 2020, 23, 159–177. [Google Scholar] [CrossRef]
- Kramer, N.; Schmöllerl, J.; Unger, C.; Nivarthi, H.; Rudisch, A.; Unterleuthner, D.; Scherzer, M.; Riedl, A.; Artaker, M.; Crncec, I.; et al. Autocrine WNT2 signaling in fibroblasts promotes colorectal cancer progression. Oncogene 2017, 36, 5460–5472. [Google Scholar] [CrossRef]
- Aizawa, T.; Karasawa, H.; Funayama, R.; Shirota, M.; Suzuki, T.; Maeda, S.; Suzuki, H.; Yamamura, A.; Naitoh, T.; Nakayama, K.; et al. Cancer-associated fibroblasts secrete Wnt2 to promote cancer progression in colorectal cancer. Cancer Med. 2019, 8, 6370–6382. [Google Scholar] [CrossRef]
- Huang, Z.; Feng, Y. Exosomes derived from hypoxic colorectal cancer cells promote angiogenesis through Wnt4-induced β-catenin signaling in endothelial cells. Oncol. Res. Featur. Preclin. Clin. Cancer Ther. 2017, 25, 651–661. [Google Scholar] [CrossRef]
- Shangguan, W.; Fan, C.; Chen, X.; Lu, R.; Liu, Y.; Li, Y.; Shang, Y.; Yin, D.; Zhang, S.; Huang, Q.; et al. Endothelium originated from colorectal cancer stem cells constitute cancer blood vessels. Cancer Sci. 2017, 108, 1357–1367. [Google Scholar] [CrossRef]
- Munro, M.J.; Wickremesekera, S.K.; Peng, L.; Tan, S.T.; Itinteang, T. Cancer stem cells in colorectal cancer: A review. J. Clin. Pathol. 2018, 71, 110–116. [Google Scholar] [CrossRef]
- Wei, B.; Han, X.Y.; Qi, C.L.; Zhang, S.; Zheng, Z.H.; Huang, Y.; Chen, T.F.; Wei, H.B. Coaction of spheroid-derived stem-like cells and endothelial progenitor cells promotes development of colon cancer. PLoS ONE 2012, 7. [Google Scholar] [CrossRef]
- Garza Treviño, E.N.; González, P.D.; Valencia Salgado, C.I.; Martinez Garza, A. Effects of pericytes and colon cancer stem cells in the tumor microenvironment. Cancer Cell. Int. 2019, 19, 173. [Google Scholar] [CrossRef]
- Planutis, K.; Planutiene, M.; Moyer, M.P.; Nguyen, A.V.; Pérez, C.A.; Holcombe, R.F. Regulation of norrin receptor frizzled-4 by Wnt2 in colon-derived cells. BMC Mol. Cell Biol. 2007, 8. [Google Scholar] [CrossRef]
- Planutis, K.; Planutiene, M.; Holcombe, R.F. A novel signaling pathway regulates colon cancer angiogenesis through Norrin. Sci. Rep. 2014, 4, 1–5. [Google Scholar] [CrossRef]
- Mitselou, A.; Galani, V.; Skoufi, U.; Arvanitis, D.L.; Lampri, E.; Ioachim, E. Syndecan-1, Epithelial-Mesenchymal Transition Markers (E-cadherin/β-catenin) and Neoangiogenesis-related Proteins (PCAM-1 and Endoglin) in Colorectal Cancer. Anticancer Res. 2016, 36, 2271–2280. [Google Scholar]
- Bhowmick, N.A.; Neilson, E.G.; Moses, H.L. Stromal fibroblasts in cancer initiation and progression. Nature 2004, 432, 332–337. [Google Scholar] [CrossRef]
- Wang, F.T.; Sun, W.; Zhang, J.T.; Fan, Y.Z. Cancer-associated fibroblast regulation of tumor neo-angiogenesis as a therapeutic target in cancer. Oncol. Lett. 2019, 17, 3055–3065. [Google Scholar] [CrossRef]
- Nagasaki, T.; Hara, M.; Nakanishi, H.; Takahashi, H.; Sato, M.; Takeyama, H. Interleukin-6 released by colon cancer-associated fibroblasts is critical for tumour angiogenesis: Anti-interleukin-6 receptor antibody suppressed angiogenesis and inhibited tumour-stroma interaction. Br. J. Cancer. 2014, 110, 469–478. [Google Scholar] [CrossRef]
- Zhang, L.; Jiang, X.; Li, Y.; Fan, Q.; Li, H.; Jin, L.; Li, L.; Jin, Y.; Zhang, T.; Mao, Y.; et al. Clinical correlation of Wnt2 and COL8A1 with colon adenocarcinoma prognosis. Front. Oncol. 2020, 10. [Google Scholar] [CrossRef]
- Jung, Y.S.; Jun, S.; Lee, S.H.; Sharma, A.; Park, J.I. Wnt2 complements Wnt/β-catenin signaling in colorectal cancer. Oncotarget 2015, 6, 37257–37268. [Google Scholar] [CrossRef]
- Guo, M.; Breslin, J.W.; Wu, M.H.; Gottardi, C.J.; Yuan, S.Y. VE-cadherin and beta-catenin binding dynamics during histamine-induced endothelial hyperpermeability. Am. J. Physiol. Cell Physiol. 2008, 294, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Gavard, J. Endothelial permeability and VE-cadherin: A wacky comradeship. Cell Adhes. Migr. 2013, 7, 455–461. [Google Scholar] [CrossRef]
- Ichikawa, Y.; Ishikawa, T.; Momiyama, N.; Kamiyama, M.; Sakurada, H.; Matsuyama, R.; Hasegawa, S.; Chishima, T.; Hamaguchi, Y.; Fujii, S.; et al. Matrilysin (MMP-7) degrades VE-cadherin and accelerates accumulation of beta-catenin in the nucleus of human umbilical vein endothelial cells. Oncol. Rep. 2006, 15, 311–315. [Google Scholar] [CrossRef]
- Zhao, Y.; Li, J.; Ting, K.K.; Chen, J.; Coleman, P.; Liu, K.; Wan, L.; Moller, T.; Vadas, M.A.; Gamble, J.R. The VE-Cadherin/β-catenin signalling axis regulates immune cell infiltration into tumours. Cancer Lett. 2020, 496, 1–15. [Google Scholar] [CrossRef]
- Reis, M.; Liebner, S. Wnt signaling in the vasculature. Exp. Cell Res. 2013, 319, 1317–1323. [Google Scholar] [CrossRef]
- Martowicz, A.; Trusohamn, M.; Jensen, N.; Wisniewska-Kruk, J.; Corada, M.; Ning, F.C.; Kele, J.; Dejana, E.; Nyqvist, D. Endothelial β-Catenin Signaling Supports Postnatal Brain and Retinal Angiogenesis by Promoting Sprouting, Tip Cell Formation, and VEGFR (Vascular Endothelial Growth Factor Receptor) 2 Expression. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 2273–2288. [Google Scholar] [CrossRef]
- Maishi, N.; Hida, K. Tumor endothelial cells accelerate tumor metastasis. Cancer Sci. 2017, 108, 1921–1926. [Google Scholar] [CrossRef]
- Fujiwara-Tani, R.; Sasaki, T.; Fujii, K.; Luo, Y.; Mori, T.; Kishi, S.; Mori, S.; Matsushima-Otsuka, S.; Nishiguchi, Y.; Goto, K.; et al. Diabetes mellitus is associated with liver metastasis of colorectal cancer through production of biglycan-rich cancer stroma. Oncotarget 2020, 11, 2982–2994. [Google Scholar] [CrossRef]
- Liu, Z.; Qi, L.; Li, Y.; Zhao, X.; Sun, B. VEGFR2 regulates endothelial differentiation of colon cancer cells. BMC Cancer 2017, 17, 593. [Google Scholar] [CrossRef]
- Wang, G.; Yang, Q.; Li, M.; Zhang, Y.; Cai, Y.; Liang, X.; Fu, Y.; Xiao, Z.; Zhou, M.; Xie, Z.; et al. Quantitative proteomic profiling of tumor-associated vascular endothelial cells in colorectal cancer. Biol. Open 2019, 8. [Google Scholar] [CrossRef]
- Suzuki, H.; Masuda, N.; Shimura, T.; Araki, K.; Kobayashi, T.; Tsutsumi, S.; Asao, T.; Kuwano, H. Nuclear β-catenin expression at the invasive front and in the vessels predicts liver metastasis in colorectal carcinoma. Anticancer Res. 2008, 28, 1821–1830. [Google Scholar]
- Wang, L.; Cheng, H.; Liu, Y.; Wang, L.; Yu, W.; Zhang, G.; Chen, B.; Yu, Z.; Hu, S. Prognostic value of nuclear β-catenin overexpression at invasive front in colorectal cancer for synchronous liver metastasis. Ann. Surg. Oncol. 2011, 18, 1553–1559. [Google Scholar] [CrossRef]
- Serafino, A.; Moroni, N.; Zonfrillo, M.; Andreola, F.; Mercuri, L.; Nicotera, G.; Nunziata, J.; Ricci, R.; Antinori, A.; Rasi, G.; et al. WNT-pathway components as predictive markers useful for diagnosis, prevention and therapy in inflammatory bowel disease and sporadic colorectal cancer. Oncotarget 2014, 5, 978–992. [Google Scholar] [CrossRef]
- Sulkowska, M.; Famulski, W.; Wincewicz, A.; Moniuszko, T.; Kedra, B.; Koda, M.; Zalewski, B.; Baltaziak, M.; Sulkowski, S. Levels of VE-cadherin increase independently of VEGF in preoperative sera of patients with colorectal cancer. Tumori J. 2006, 92, 67–71. [Google Scholar] [CrossRef]
- Agarwal, A.; Das, K.; Lerner, N.; Sathe, S.; Cicek, M.; Casey, G.; Sizemore, N. The AKT/I κB kinase pathway promotes angiogenic/metastatic gene expression in colorectal cancer by actiating nuclear factor-κB and β-catenin. Oncogene 2005, 24, 1021–1031. [Google Scholar] [CrossRef]
- Shao, J.; Jung, C.; Liu, C.; Sheng, H. Prostaglandin E2 Stimulates the β-catenin/T cell factor-dependent transcription in colon cancer. J. Biol. Chem. 2005, 280, 26565–26572. [Google Scholar] [CrossRef]
- Jeong, W.J.; Ro, E.J.; Choi, K.Y. Interaction between Wnt/β-catenin and RAS-ERK pathways and an anti-cancer strategy via degradations of β-catenin and RAS by targeting the Wnt/β-catenin pathway. NPJ Precis. Oncol. 2018, 2, 5. [Google Scholar] [CrossRef]
- Liang, J.; Tang, J.; Shi, H.; Li, H.; Zhen, T.; Duan, J.; Kang, L.; Zhang, F.; Dong, Y.; Han, A. miR-27a-3p targeting RXRα promotes colorectal cancer progression by activating Wnt/β-catenin pathway. Oncotarget 2017, 8, 82991–83008. [Google Scholar] [CrossRef]
- Cheng, X.; Xu, X.; Chen, D.; Zhao, F.; Wang, W. Therapeutic potential of targeting the Wnt/β-catenin signaling pathway in colorectal cancer. Biomed. Pharmacother. 2019, 110, 473–481. [Google Scholar] [CrossRef]
- Xue, M.; Zhuo, Y.; Shan, B. MicroRNAs, Long Noncoding RNAs, and Their Functions in Human Disease. Methods Mol. Biol. 2017, 1617, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Patop, I.L.; Kadener, S. circRNAs in Cancer. Curr. Opin. Genet. Dev. 2018, 48, 121–127. [Google Scholar] [CrossRef]
- Zhao, W.; Dong, M.; Pan, J.; Wang, Y.; Zhou, J.; Ma, J.; Liu, S. Circular RNAs: A novel target among non-coding RNAs with potential roles in malignant tumors. Mol. Med. Rep. 2019, 20, 3463–3474. [Google Scholar] [CrossRef]
- Lewis, B.P.; Burge, C.B.; Bartel, D.P. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell 2005, 120, 15–20. [Google Scholar] [CrossRef]
- Balacescu, O.; Sur, D.; Cainap, C.; Visan, S.; Cruceriu, D.; Manzat-Saplacan, R.; Muresan, M.S.; Balacescu, L.; Lisencu, C.; Irimie, A. The Impact of miRNA in Colorectal Cancer Progression and Its Liver Metastases. Int. J. Mol. Sci. 2018, 19, 3711. [Google Scholar] [CrossRef] [PubMed]
- Ji, S.; Ye, G.; Zhang, J.; Wang, L.; Wang, T.; Wang, Z.; Zhang, T.; Wang, G.; Guo, Z.; Luo, Y.; et al. miR-574-5p negatively regulates Qki6/7 to impact β-catenin/Wnt signalling and the development of colorectal cancer. Gut 2013, 62, 716–726. [Google Scholar] [CrossRef]
- Li, Y.; Lauriola, M.; Kim, D.; Francesconi, M.; D’Uva, G.; Shibata, D.; Malafa, M.P.; Yeatman, T.J.; Coppola, D.; Solmi, R.; et al. Adenomatous polyposis coli (APC) regulates miR17-92 cluster through β-catenin pathway in colorectal cancer. Oncogene 2016, 35, 4558–4568. [Google Scholar] [CrossRef]
- Zhang, G.J.; Li, L.F.; Yang, G.D.; Xia, S.S.; Wang, R.; Leng, Z.W.; Liu, Z.L.; Tian, H.P.; He, Y.; Meng, C.Y.; et al. MiR-92a promotes stem cell-like properties by activating Wnt/β-catenin signaling in colorectal cancer. Oncotarget 2017, 8, 101760–101770. [Google Scholar] [CrossRef]
- Li, T.; Jian, X.; He, H.; Lai, Q.; Li, X.; Deng, D.; Liu, T.; Zhu, J.; Jiao, H.; Ye, Y.; et al. MiR-452 promotes an aggressive colorectal cancer phenotype by regulating a Wnt/β-catenin positive feedback loop. J. Exp. Clin. Cancer Res. 2018, 37, 238. [Google Scholar] [CrossRef]
- Zhang, F.; Meng, F.; Li, H.; Dong, Y.; Yang, W.; Han, A. Suppression of retinoid X receptor alpha and aberrant β-catenin expression significantly associates with progression of colorectal carcinoma. Eur. J. Cancer 2011, 47, 2060–2067. [Google Scholar] [CrossRef]
- Han, A.; Tong, C.; Hu, D.; Bi, X.; Yang, W. A direct protein-protein interaction is involved in the suppression of beta-catenin transcription by retinoid X receptor alpha in colorectal cancer cells. Cancer Biol. Ther. 2008, 7, 454–459. [Google Scholar] [CrossRef]
- Li, T.; Lai, Q.; Wang, S.; Cai, J.; Xiao, Z.; Deng, D.; He, L.; Jiao, H.; Ye, Y.; Liang, L.; et al. MicroRNA-224 sustains Wnt/β-catenin signaling and promotes aggressive phenotype of colorectal cancer. J. Exp. Clin. Cancer Res. 2016, 35, 21. [Google Scholar] [CrossRef]
- Zheng, K.; Zhou, X.; Yu, J.; Li, Q.; Wang, H.; Li, M.; Shao, Z.; Zhang, F.; Luo, Y.; Shen, Z.; et al. Epigenetic silencing of miR-490-3p promotes development of an aggressive colorectal cancer phenotype through activation of the Wnt/β-catenin signaling pathway. Cancer Lett. 2016, 376, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, M.; Rao, S.R.; Thacker, P.; Chatterjee, S.; Karunagaran, D. MiR-29b downregulates canonical Wnt signaling by suppressing coactivators of β-catenin in human colorectal cancer cells. J. Cell Biochem. 2014, 115, 1974–1984. [Google Scholar] [CrossRef]
- Yuan, Z.; Yu, X.; Ni, B.; Chen, D.; Yang, Z.; Huang, J.; Wang, J.; Chen, D.; Wang, L. Overexpression of long non-coding RNA-CTD903 inhibits colorectal cancer invasion and migration by repressing Wnt/β-catenin signaling and predicts favorable prognosis. Int. J. Oncol. 2016, 48, 2675–2685. [Google Scholar] [CrossRef]
- Yu, J.; Han, Z.; Sun, Z.; Wang, Y.; Zheng, M.; Song, C. LncRNA SLCO4A1-AS1 facilitates growth and metastasis of colorectal cancer through β-catenin-dependent Wnt pathway. J. Exp. Clin. Cancer Res. 2018, 37, 222. [Google Scholar] [CrossRef]
- Javed, Z.; Khan, K.; Sadia, H.; Raza, S.; Salehi, B.; Sharifi-Rad, J.; Cho, W.C. LncRNA & Wnt signaling in colorectal cancer. Cancer Cell Int. 2020, 20, 326. [Google Scholar] [CrossRef]
- Wang, F.W.; Cao, C.H.; Han, K.; Zhao, Y.X.; Cai, M.Y.; Xiang, Z.C.; Zhang, J.X.; Chen, J.W.; Zhong, L.P.; Huang, Y.; et al. APC-activated long noncoding RNA inhibits colorectal carcinoma pathogenesis through reduction of exosome production. J. Clin. Investig. 2019, 129, 727–743. [Google Scholar] [CrossRef]
- Fang, Q.; Yang, A.; Dong, A.; Zhao, L. circPDSS1 Stimulates the Development of Colorectal Cancer via Activating the Wnt/β-Catenin Signaling. Onco Targets Ther. 2020, 13, 6329–6337. [Google Scholar] [CrossRef]
- Kircher, S.M.; Nimeiri, H.S.; Benson, A.B., III. Targeting Angiogenesis in Colorectal Cancer: Tyrosine Kinase Inhibitors. Cancer J. 2016, 22, 182–189. [Google Scholar] [CrossRef]
- Karasic, T.B.; Rosen, M.A.; O’Dwyer, P.J. Antiangiogenic tyrosine kinase inhibitors in colorectal cancer: Is there a path to making them more effective? Cancer Chemother. Pharmacol. 2017, 80, 661–671. [Google Scholar] [CrossRef]
- Riechelmann, R.P.; Leite, L.S.; Bariani, G.M.; Glasberg, J.; Rivelli, T.G.; da Fonseca, L.G.; Nebuloni, D.R.; Braghiroli, M.I.; Queiroz, M.A.; Isejima, A.M.; et al. Regorafenib in Patients with Antiangiogenic-Naïve and Chemotherapy-Refractory Advanced Colorectal Cancer: Results from a Phase IIb Trial. Oncologist 2019, 24, 1180–1187. [Google Scholar] [CrossRef]
- Iwasa, S.; Okita, N.; Kuchiba, A.; Ogawa, G.; Kawasaki, M.; Nakamura, K.; Shoji, H.; Honma, Y.; Takashima, A.; Kato, K.; et al. Phase II study of lenvatinib for metastatic colorectal cancer refractory to standard chemotherapy: The LEMON study (NCCH1503). ESMO Open 2020, 5. [Google Scholar] [CrossRef]
- Zhang, Y.; Zou, J.Y.; Wang, Z.; Wang, Y. Fruquintinib: A novel antivascular endothelial growth factor receptor tyrosine kinase inhibitor for the treatment of metastatic colorectal cancer. Cancer Manag. Res. 2019, 11, 7787–7803. [Google Scholar] [CrossRef]
- Xie, Y.H.; Chen, Y.X.; Fang, J.Y. Comprehensive review of targeted therapy for colorectal cancer. Signal. Transduct. Target. Ther. 2020, 5, 22. [Google Scholar] [CrossRef]
- De Mattia, E.; Bignucolo, A.; Toffoli, G.; Cecchin, E. Genetic Markers of the Host to Predict the Efficacy of Colorectal Cancer Targeted Therapy. Curr. Med. Chem. 2020, 27, 4249–4273. [Google Scholar] [CrossRef]
- Sebio, A.; Kahn, M.; Lenz, H.J. The potential of targeting Wnt/β-catenin in colon cancer. Expert Opin. Ther. Targets 2014, 18, 611–615. [Google Scholar] [CrossRef]
- Katoh, M.; Katoh, M. Molecular genetics and targeted therapy of WNT-related human diseases. Int. J. Mol. Med. 2017, 40, 587–606. [Google Scholar] [CrossRef]
- Lau, T.; Chan, E.; Callow, M.; Waaler, J.; Boggs, J.; Blake, R.A.; Magnuson, S.; Sambrone, A.; Schutten, M.; Firestein, R.; et al. A novel tankyrase small-molecule inhibitor suppresses APC mutation-driven colorectal tumor growth. Cancer Res. 2013, 73, 3132–3144. [Google Scholar] [CrossRef]
- Verma, S.; Das, P.; Kumar, V.L. Chemoprevention by artesunate in a preclinical model of colorectal cancer involves down regulation of β-catenin, suppression of angiogenesis, cellular proliferation and induction of apoptosis. Chem. Biol. Interact. 2017, 278, 84–91. [Google Scholar] [CrossRef]
- Wierzbicka, J.M.; Binek, A.; Ahrends, T.; Nowacka, J.D.; Szydłowska, A.; Turczyk, Ł.; Wąsiewicz, T.; Wierzbicki, P.M.; Sądej, R.; Tuckey, R.C.; et al. Differential antitumor effects of vitamin D analogues on colorectal carcinoma in culture. Int. J. Oncol. 2015, 47, 1084–1096. [Google Scholar] [CrossRef]
- Sun, H.; Jiang, C.; Cong, L.; Wu, N.; Wang, X.; Hao, M.; Liu, T.; Wang, L.; Liu, Y.; Cong, X. CYP24A1 Inhibition Facilitates the Antiproliferative Effect of 1,25(OH)2D3 Through Downregulation of the WNT/β-Catenin Pathway and Methylation-Mediated Regulation of CYP24A1 in Colorectal Cancer Cells. DNA Cell Biol. 2018, 37, 742–749. [Google Scholar] [CrossRef]
- Razak, S.; Afsar, T.; Almajwal, A.; Alam, I.; Jahan, S. Growth inhibition and apoptosis in colorectal cancer cells induced by Vitamin D-Nanoemulsion (NVD): Involvement of Wnt/β-catenin and other signal transduction pathways. Cell Biosci. 2019, 9, 15. [Google Scholar] [CrossRef]
- Ferrer-Mayorga, G.; Larriba, M.J.; Crespo, P.; Muñoz, A. Mechanisms of action of vitamin D in colon cancer. J. Steroid Biochem. Mol. Biol. 2019, 185, 1–6. [Google Scholar] [CrossRef]
- Leyssens, C.; Verlinden, L.; Verstuyf, A. Antineoplastic effects of 1,25(OH)2D3 and its analogs in breast, prostate and colorectal cancer. Endocr. Relat. Cancer 2013, 20, 31–47. [Google Scholar] [CrossRef]
- Aguilera, O.; Peña, C.; García, J.M.; Larriba, M.J.; Ordóñez-Morán, P.; Navarro, D.; Barbáchano, A.; López de Silanes, I.; Ballestar, E.; Fraga, M.F.; et al. The Wnt antagonist DICKKOPF-1 gene is induced by 1alpha,25-dihydroxyvitamin D3 associated to the differentiation of human colon cancer cells. Carcinogenesis 2007, 28, 1877–1884. [Google Scholar] [CrossRef]
- Ferrer-Mayorga, G.; Gómez-López, G.; Barbáchano, A.; Fernández-Barral, A.; Peña, C.; Pisano, D.G.; Cantero, R.; Rojo, F.; Muñoz, A.; Larriba, M.J. Vitamin D receptor expression and associated gene signature in tumour stromal fibroblasts predict clinical outcome in colorectal cancer. Gut 2017, 66, 1449–1462. [Google Scholar] [CrossRef]
- Xiao, J.H.; Ghosn, C.; Hinchman, C.; Forbes, C.; Wang, J.; Snider, N.; Cordrey, A.; Zhao, Y.; Chandraratna, R.A. Adenomatous polyposis coli (APC)-independent regulation of beta-catenin degradation via a retinoid X receptor-mediated pathway. J. Biol. Chem. 2003, 278, 29954–29962. [Google Scholar] [CrossRef]
- Dillard, A.C.; Lane, M.A. Retinol Increases beta-catenin-RXRα binding leading to the increased proteasomal degradation of β-catenin and RXRα. Nutr. Cancer 2008, 60, 97–108. [Google Scholar] [CrossRef]
- Dillard, A.C.; Lane, M.A. Retinol decreases β-catenin protein levels in retinoic acid-resistant colon cancer cell lines. Mol. Carcinog. 2007, 46, 315–329. [Google Scholar] [CrossRef]
- Ghosh, N.; Hossain, U.; Mandal, A.; Sil, P.C. The Wnt signaling pathway: A potential therapeutic target against cancer. Ann. N. Y. Acad. Sci. 2019, 1443, 54–74. [Google Scholar] [CrossRef]
- Emons, G.; Spitzner, M.; Reineke, S.; Möller, J.; Auslander, N.; Kramer, F.; Hu, Y.; Beissbarth, T.; Wolff, H.A.; Rave-Fränk, M.; et al. Chemoradiotherapy Resistance in Colorectal Cancer Cells is Mediated by Wnt/β-catenin Signaling. Mol. Cancer Res. 2017, 15, 1481–1490. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.H.; Hu, Q.; Sui, H.; Ci, S.J.; Wang, Y.; Liu, X.; Liu, N.N.; Yin, P.H.; Qin, J.M.; Li, Q. Tanshinone II--a inhibits angiogenesis through down regulation of COX-2 in human colorectal cancer. Asian Pac. J. Cancer Prev. 2012, 13, 4453–4458. [Google Scholar] [CrossRef]
- Nagoor Meeran, M.F.; Javed, H.; Al Taee, H.; Azimullah, S.; Ojha, S.K. Pharmacological Properties and Molecular Mechanisms of Thymol: Prospects for Its Therapeutic Potential and Pharmaceutical Development. Front. Pharmacol. 2017, 8. [Google Scholar] [CrossRef]
- Chauhan, A.K.; Bahuguna, A.; Paul, S.; Kang, S.C. Thymol Elicits HCT-116 Colorectal Carcinoma Cell Death Through Induction of Oxidative Stress. Anticancer Agents Med. Chem. 2018, 17, 1942–1950. [Google Scholar] [CrossRef]
- Zeng, Q.; Che, Y.; Zhang, Y.; Chen, M.; Guo, Q.; Zhang, W. Thymol Isolated from Thymus vulgaris L. Inhibits Colorectal Cancer Cell Growth and Metastasis by Suppressing the Wnt/β-Catenin Pathway. Drug Des. Dev. Ther. 2020, 14, 2535–2547. [Google Scholar] [CrossRef]
- Wu, X.; Yu, N.; Zhang, Y.; Ye, Y.; Sun, W.; Ye, L.; Wu, H.; Yang, Z.; Wu, L.; Wang, F. Radix Tetrastigma hemsleyani flavone exhibits antitumor activity in colorectal cancer via Wnt/β-catenin signaling pathway. Onco Targets Ther. 2018, 11, 6437–6446. [Google Scholar] [CrossRef]
- Deguchi, A. Curcumin targets in inflammation and cancer. Endocr. Metab. Immune Disord. Drug Targets 2015, 15, 88–96. [Google Scholar] [CrossRef]
- Dou, H.; Shen, R.; Tao, J.; Huang, L.; Shi, H.; Chen, H.; Wang, Y.; Wang, T. Curcumin Suppresses the Colon Cancer Proliferation by Inhibiting Wnt/β-Catenin Pathways via miR-130a. Front. Pharmacol. 2017, 8. [Google Scholar] [CrossRef]
- Jiang, X.; Li, S.; Qiu, X.; Cong, J.; Zhou, J.; Miu, W. Curcumin Inhibits Cell Viability and Increases Apoptosis of SW620 Human Colon Adenocarcinoma Cells via the Caudal Type Homeobox-2 (CDX2)/Wnt/β-Catenin Pathway. Med. Sci Monit. 2019, 25, 7451–7458. [Google Scholar] [CrossRef]
- Li, Y.; Qin, X.; Li, P.; Zhang, H.; Lin, T.; Miao, Z.; Ma, S. Isobavachalcone isolated from Psoralea corylifolia inhibits cell proliferation and induces apoptosis via inhibiting the AKT/GSK-3β/β-catenin pathway in colorectal cancer cells. Drug Des. Dev. Ther. 2019, 13, 1449–1460. [Google Scholar] [CrossRef]
- Albring, K.F.; Weidemüller, J.; Mittag, S.; Weiske, J.; Friedrich, K.; Geroni, M.C.; Lombardi, P.; Huber, O. Berberine acts as a natural inhibitor of Wnt/β-catenin signaling—Identification of more active 13-arylalkyl derivatives. Biofactors 2013, 39, 652–662. [Google Scholar] [CrossRef]
- Ruan, H.; Zhan, Y.Y.; Hou, J.; Xu, B.; Chen, B.; Tian, Y.; Wu, D.; Zhao, Y.; Zhang, Y.; Chen, X.; et al. Berberine binds RXRα to suppress β-catenin signaling in colon cancer cells. Oncogene 2017, 36, 6906–6918. [Google Scholar] [CrossRef]
- Ortiz, L.M.; Lombardi, P.; Tillhon, M.; Scovassi, A.I. Berberine, an epiphany against cancer. Molecules 2014, 19, 12349–12367. [Google Scholar] [CrossRef]
- Gungor, H.; Ilhan, N.; Eroksuz, H. The effectiveness of cyclooxygenase-2 inhibitors and evaluation of angiogenesis in the model of experimental colorectal cancer. Biomed. Pharmacother. 2018, 102, 221–229. [Google Scholar] [CrossRef]
- Madan, B.; Ke, Z.; Harmston, N.; Ho, S.Y.; Frois, A.O.; Alam, J.; Jeyaraj, D.A.; Pendharkar, V.; Ghosh, K.; Virshup, I.H.; et al. Wnt addiction of genetically defined cancers reversed by PORCN inhibition. Oncogene 2016, 35, 2197–2207. [Google Scholar] [CrossRef]
- Fang, L.; Zhu, Q.; Neuenschwander, M.; Specker, E.; Wulf-Goldenberg, A.; Weis, W.I.; von Kries, J.P.; Birchmeier, W. A Small-Molecule Antagonist of the β-Catenin/TCF4 Interaction Blocks the Self-Renewal of Cancer Stem Cells and Suppresses Tumorigenesis. Cancer Res. 2016, 76, 891–901. [Google Scholar] [CrossRef]
- Storm, E.E.; Durinck, S.; de Sousa e Melo, F.; Tremayne, J.; Kljavin, N.; Tan, C.; Ye, X.; Chiu, C.; Pham, T.; Hongo, J.A.; et al. Targeting PTPRK-RSPO3 colon tumours promotes differentiation and loss of stem-cell function. Nature 2016, 529, 97–100. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, H. Genistein attenuates WNT signaling by up-regulating sFRP2 in a human colon cancer cell line. Exp. Biol. Med. 2011, 236, 714–722. [Google Scholar] [CrossRef]
- Zhu, J.; Ren, J.; Tang, L. Genistein inhibits invasion and migration of colon cancer cells by recovering WIF1 expression. Mol. Med. Rep. 2018, 17, 7265–7273. [Google Scholar] [CrossRef]
- Jeong, J.B.; Lee, J.; Lee, S.H. TCF4 Is a Molecular Target of Resveratrol in the Prevention of Colorectal Cancer. Int. J. Mol. Sci. 2015, 16, 10411–10425. [Google Scholar] [CrossRef]
- Vacante, M.; Borzì, A.M.; Basile, F.; Biondi, A. Biomarkers in colorectal cancer: Current clinical utility and future perspectives. World J. Clin. Cases 2018, 6, 869–881. [Google Scholar] [CrossRef]
- Vacante, M.; Ciuni, R.; Basile, F.; Biondi, A. The Liquid Biopsy in the Management of Colorectal Cancer: An Overview. Biomedicines 2020, 8, 308. [Google Scholar] [CrossRef]
| Action | Family of Factors | Factor | Molecular Mechanisms/Effects on Angiogenesis | Ref. |
|---|---|---|---|---|
| Pro-angiogenic | Wnt pathway components | DKK-4 | (i) ↑expression in CRC cells; (ii) ↑migration and formation of capillary-like tubules of human primary microvascular ECs | [81] |
| BCL9 | (i) directly binds to β-catenin; (ii)BCL9 knockdown attenuated the expression of pro-angiogenic factors (e.g., CD44, and VEGF), which resulted in a reduction of tumor metastasis and angiogenesis | [67,79,80] | ||
| Wnt2 | (i) ↑expression in CAFs, which correlates with clinical data; (ii) induces CRC cells and EC migration and invasion; (iii) ↑vessels density and tumor volume; (iv) activates Wnt signaling in autocrine and paracrine manner | [106,107,108] | ||
| Non-Wnt pathway factors | DHX32 | (i) ↑VEGF-A and stabilization of β-catenin; (ii) ↑↑- is a poor prognostic factor | [72] | |
| gankyrin (PSMD10) | (i) coordinates cooperation between PI3K/Akt and canonical Wnt/β-catenin signaling pathways; (ii) overexpressing gankyrin promoted angiogenesis, chemoresistance and metastasis of CRC cells both in vitro and in vivo | [19] | ||
| Uba2 | Regulates Wnt signaling and enhances EMT | [85] | ||
| TGM2 | ↑expression of MMP-2, MMP-9, Wnt3a, β-catenin and cyclin D1 | [75,86] | ||
| c-Cbl gene | Mutant C-Cbl-Y371H shows ↑Wnt/β-catenin signaling, increased Wnt genes, angiogenesis, and CRC growth via phosphorylation of c-Cbl Tyr371 | [73] | ||
| AKT | ↑↑EMT-related transcription factors (including β-catenin) | [71] | ||
| CXCL8 | (i) ↑VEGF-A and Bcl2; (ii) ↑cell invasion via AKT/GSK3β/β-catenin/MMP7 pathway | [70] | ||
| CXCR4 | SDF-1 induces CXCR4-positive CRC cell invasion and EMT via activation of Wnt/β-catenin signaling | [84] | ||
| SALL4 | (i) directly binds to β-catenin; (ii) co-expression with β-catenin promoting lymph node metastasis and advanced stage; (iii) modulates VEGF-A expression in HUVECs | [76,78,87] | ||
| FOXQ1 | (i) ↑↑correlates with stage and lymph nodes metastasis; (ii) modulates cell invasion, EMT, and resistance to drug-induced apoptosis | [77] | ||
| Bioactive compound of plants | Aloin, aloesin | (i) aloin activates Wnt/β-catenin signaling in the presence of Wnt3a in CRC cells; (ii) aloesin directly activates Wnt signaling in Wnt3a independent manner | [89] | |
| Anti-angiogenic | Wnt pathway components | DKK-1 | (i) ↓MVD and VEGF expression vs. control; (ii) inhibits tube-like structure formation and ↓VEGF expression in HUVECs | [90] |
| Non-Wnt pathway factors | TIPE2 (TNFAIP8L2) | ↓expression of Wnt3a, phospho-β-catenin, and GSK-3β in rectal adenocarcinoma cells; (ii) cooperates with Wnt/β-catenin and TGF-β/Smad2/3 signaling pathways | [91] | |
| SMAR1 | Inhibits β-catenin mRNA production and promoter activity by recruiting Histone deacetylase-5 to β-catenin promoter | [94] | ||
| PKG | ↓VEGF and β-catenin expression in TCF-dependent transcription | [93] | ||
| PKCα | (i) inhibits β-catenin transcriptional activity via Wnt5a/PKCα-dependent phosphorylation on SER35 of ROR α; (ii) phosphorylates of β-catenin | [95,96] | ||
| Bioactive compound of plants | Aloin | (i) inhibits HUVECs proliferation, migration and tube formation in vitro; (ii) inhibits VEGFR-2 and STAT3 phosphorylation in ECs; (iii) ↓VEGF antiapoptotic, pro-proliferative factors (C-Myc) in CRC cells | [88] | |
| Sporamin | ↓β-catenin and VEGF production | [97] | ||
| Tan IIA (TSA) | (i) inhibits secretion of VEGF and bFGF; (ii) suppresses the proliferation, tube formation and metastasis of HUVECs; (iii) inhibits β-catenin/VEGF-mediated angiogenesis by decreasing TGF-β (via HIF-1α inhibition) | [98] | ||
| Emodin | (i) ↓TCF/LEF transcriptional activity; (ii) inhibits EMT proteins, β-catenin and TCF7L2, VEGF production; (iii)↑cadherin E mRNA expression | [99,100] | ||
| 6-Gingerol | (i) inhibits Wnt3a and β-catenin expression; (ii) ↓VEGF, ANG-1, FGF, GDF-15 levels | [101] | ||
| Raddeanin A | (i) modulates VEGF-mediated phosphorylation of VEGFR-2 and downstream kinases FAK, PLCγ1, Src, and Akt; (ii) inhibits p-LPR6, inactivates AKT, removes GSK-3β inhibition and attenuation of β-catenin; (iii) inhibits HUVECs proliferation, motility, migration, and tube formation | [104,105] |
| Type of Non-Coding RNAs | Interacting Molecules | Molecular Mechanism of Angiogenesis | Effect on Wnt Pathway | Ref. | |
|---|---|---|---|---|---|
| miRNAs | miR-574-5p | Qki | (i) ↑expression correlated with ↑expression of β-catenin and p27 (Kip1 protein), cell proliferation, invasion, and migration; (ii) ↑expression inversely correlated with Qkis isoforms | activates | [146] |
| miR-17-92 cluster (including miR-19a) | β-catenin | (i) β-catenin binds to and activates the miR-17-92 promoter; (ii) miR-19a correlates with β-catenin level and aggressive stage of CRC | activates | [147] | |
| miR-92a | Wnt/β-catenin | (i) ↑expression in CRC cells; (ii) enhances Wnt/β-catenin signaling through KLF4, GSK3β and DKK-3; (iii) increased miR-92a promotes of stem-like phenotypes of CRC cells | activates | [148] | |
| miR-452 | 3’-UTR of GSK3β; β-catenin | (i) ↑expression in ~70% CRC tissue and CRC cell lines; (ii) promotes nuclear relocalization of β-catenin and the expression of the target genes; (iii) direct regulation on the 3’-UTR of the GSK3 | activates | [149] | |
| miR-27a-3p | RXRα | (i) ↑expression in CRC tissue and positive correlation with clinical data; (ii) negative correlation with RXRα; (iii) downregulation of RXRα which prevents β-catenin degradation | activates | [139] | |
| miR-224 | 3’-UTR of GSK3β and SFRP2 genes | (i) leads to nuclear translocation of β-catenin; (ii) upregulated miR-224 inhibits the expression of GSK3β/SFRP2 and enhances CRC proliferation and invasion | activates | [152] | |
| miR-490-3p | FRAT1 | (i) ↓expression in CRC cells via hypermethylation of the miR-490-3p promoter; (ii) suppresses CRC cells proliferation, inhibits invasion (via repressing EMT); (iii) inhibits β-catenin expression in nuclear fractions of CRC cells | inhibits | [153] | |
| miR-29b | 3’UTR of BCL9L | (i) downregulates coactivators of β-catenin (TCF7L2, Snail, BCL9L); (ii) decreases nuclear translocation of β-catenin; (iii) ↓tube formation in ECs | inhibits | [154] | |
| lncRNAs | lncRNA SLCO4A1-AS1 | Wnt/β-catenin | (i) ↑expression in CRC tissues correlates with poor prognosis and metastasis; (ii) promotes cell proliferation, migration, and invasion (via EMT); (iii) enhances β-catenin stability | activates | [156] |
| lncRNA-CTD903 | Wnt/β-catenin | (i) ↑expression in CRC tissues vs. control; (ii) is independent factor of favorable prognosis; (iii) downregulated enhances Wnt/β-catenin activation and their downstream transcription factors | inhibits | [155] | |
| lncRNA GAS5 | Wnt/β-catenin | (i) weak expression in CRC tissues and cells; (ii) upregulated inhibits CRC cells invasion and migration in vitro; (iii) inhibits of tumor growth, angiogenesis, and liver metastasis in vivo | inhibits | [31] | |
| lncRNA-APC1 | APC | (i) ↑expression inhibits CRC cell growth, metastasis, and tumor angiogenesis by suppressing exosome production; (ii) inhibits MAPK pathway in ECs and suppress angiogenesis | inhibits | [158] | |
| circRNAs | circPDSS1 | Wnt/β-catenin | (i) ↑expression in CRC tissues vs. control; (ii) higher level predicts high rates of metastasis, and overall survival; (iii) knockdown of PDSS1 results in attenuation of migratory abilities and angiogenesis in CRC cells | activates | [159] |
| Class of Agents | Name of Targeted Agents | Target | Mechanism of Action and Effects in CRC Cells | Effect on Angiogenesis | Stage of Development | Ref. |
|---|---|---|---|---|---|---|
| NSAIDs | Sulindac (Clinoril) | β-catenin | (i) both drugs ↑ expression of PTEN and GSK3β, inhibit of Akt (and β-catenin), MMPs, and iNOS activation; (ii) inhibit proliferation, have pro-apoptotic effects; (iii) ↓CD133 expression, a marker of cancer stem cells; (iv) inhibit COX-2 and progression of tumor | inhibits | clinical | [68,140,167,195] |
| Celecoxib | TCF | inhibits | clinical | |||
| Other anti-inflammatory drugs | Artesunate | β-catenin | (i) both drugs down-regulate β-catenin signaling and ↓levels of VEGF, and MMP-9; (ii) inhibit proliferation, and have pro-apoptotic effects | inhibits | clinical | [170] |
| Aspirin | β-catenin | inhibits | clinical | |||
| Vitamins and their derivatives | Vitamin D3 metabolites (Cholecalciferol) | Wnt/β-catenin with upstream and downstream targets | (i) anti-proliferative effects in vitro and in vivo; (ii) ↑DKK-1 gene and ↓DKK-4 gene | inhibits | Phase 1–3 * | [81,140,171,172,173,174,175,176] |
| Vitamin A and its other forms (e.g., retinoic acid, retinol) | Wnt/β-catenin and downstream targets | (i) ↑β-catenin degradation in proteasomes via RXR-mediated pathway; (ii) ↓transcription of the TOPFlash reporter and mRNA levels of the cyclin D1 and C-Myc genes | nd | clinical | [178,180] | |
| Specific small molecules | ETC-159 | Wnt, PORCN | PORCN inhibitor; effective in treating RSPO-translocation bearing CRC patient-derived xenografts | nd | Phase 1 | [196] |
| Wnt-974 | Wnt, PORCN | Inhibitory effects in metastatic CRC | nd | Phase 1/2 | [165] | |
| LGK-974 | Wnt, PORCN | Inhibitory effects in multiple tumor including CRC | nd | Phase 1 | [140,165,167] | |
| Foxy-5 | Wnt5 mimicking | Inhibitory effects in multiple tumors including CRC | nd | Phase 1 | [165,167] | |
| G007-LK | Axin | Both are tankyrase inhibitors; both promote β-catenin destabilization; G007-LK inhibits tumor growth in vivo in a subset of APC-mutant CRC xenograft models | nd | preclinical | [169] | |
| G244-LM | ||||||
| LF3 (4-thioureido-benzenesulphonamide derivative) | β-catenin/TCF | (i) antagonises of β-catenin/TCF4 interactions; (ii) suppresses cell motility, cell-cycle progression; (iii) ↓tumor growth and induces differentiation in a mouse xenografts of CRC | nd | discovery | [197] | |
| SAH-BCL9 | Blockade of β-catenin protein-protein interactions | (i) dissociates native β-catenin/BCL9 complexes, selectively suppresses Wnt transcription, and exhibits antitumor effects; (ii) suppresses tumor growth and angiogenesis in mouse xenograft model of CRC | inhibits | preclinical | [83] | |
| XAV-939 | β-catenin, Axin | Inhibits β-catenin which resulted in sensitization of CRC cells to chemotherapy | nd | discovery | [182] | |
| Antibodies | Anti-RSPO3 mAb (Rosmantuzumab, OMP-131R10) | RSPO3 (Wnt agonist) | In PTPRK-RSPO3-fusion positive human colon tumors xenografts inhibits tumor growth and promotes differentiation | nd | Phase 1 | [198] |
| Plant-based agents | Berberine and synthetic 13-arylalkyl derivatives | β-catenin | (i) inhibits β-catenin transcriptional activity by binding to a unique RXRα region; (ii) weakening of anchorage-independent growth (↓E-cadherin expression) | nd | discovery | [192,193,194] |
| Bryostatin 1 | Wnt/β-catenin | (i) natural PKCα activator; (ii) PKCα triggers the death of CRC cells; (iii) PKCα activity is drug-inducible | nd | Phase 2 | [74] | |
| Curcumin (diferuloymethane) | Wnt/β-catenin and downstream proteins | anti-tumor activity via inhibition of cell proliferation, pro-apoptotic effects, decrease in CDX2 and expression of Wnt3a, c-Myc, survivin, and cyclin D1 | nd | Phase 1–3 * | [140,188,189,190] | |
| Genistein | Wnt/β-catenin and downstream proteins | (i) ↓nuclear β-catenin and increases phospho-β-catenin accumulation; (ii) inhibits cell viability, cell invasion, cell migration by recovering WIF1, ↑apoptosis; (iii) ↑sFRP2 gene expression by demethylating its silenced promoter; (iv) ↓MMP-2 and MMP-9, but ↑E-cadherin | nd | Phase 1–2 * | [199,200] | |
| Isobavachalcone | AKT/GSK3β/β-catenin pathway | inhibits growth and colony formation of tumor cells, as well as induces apoptosis | nd | discovery | [190] | |
| Resveratrol (SRT501, grapes) | TCF4 | (i) ↓cellular accumulation of endogenously-introduced TCF4 protein; (ii) represses the growth of CRC cells | nd | Phase 1 | [140,201] | |
| RTHF | Wnt/β-catenin | ↓β-catenin and downstream protein expression (Lgr5, c-Myc, and cyclin D1) | nd | discovery | [187] | |
| Thymol | Wnt/β-catenin | (i) prevents EMT, invasion, and CRC metastasis | nd | discovery | [186] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kasprzak, A. Angiogenesis-Related Functions of Wnt Signaling in Colorectal Carcinogenesis. Cancers 2020, 12, 3601. https://doi.org/10.3390/cancers12123601
Kasprzak A. Angiogenesis-Related Functions of Wnt Signaling in Colorectal Carcinogenesis. Cancers. 2020; 12(12):3601. https://doi.org/10.3390/cancers12123601
Chicago/Turabian StyleKasprzak, Aldona. 2020. "Angiogenesis-Related Functions of Wnt Signaling in Colorectal Carcinogenesis" Cancers 12, no. 12: 3601. https://doi.org/10.3390/cancers12123601
APA StyleKasprzak, A. (2020). Angiogenesis-Related Functions of Wnt Signaling in Colorectal Carcinogenesis. Cancers, 12(12), 3601. https://doi.org/10.3390/cancers12123601






