Comparison of Poly (ADP-ribose) Polymerase Inhibitors (PARPis) as Maintenance Therapy for Platinum-Sensitive Ovarian Cancer: Systematic Review and Network Meta-Analysis
Simple Summary
Abstract
1. Introduction
2. Results
2.1. Baseline Patient and Tumor Characteristics
2.2. Study Description
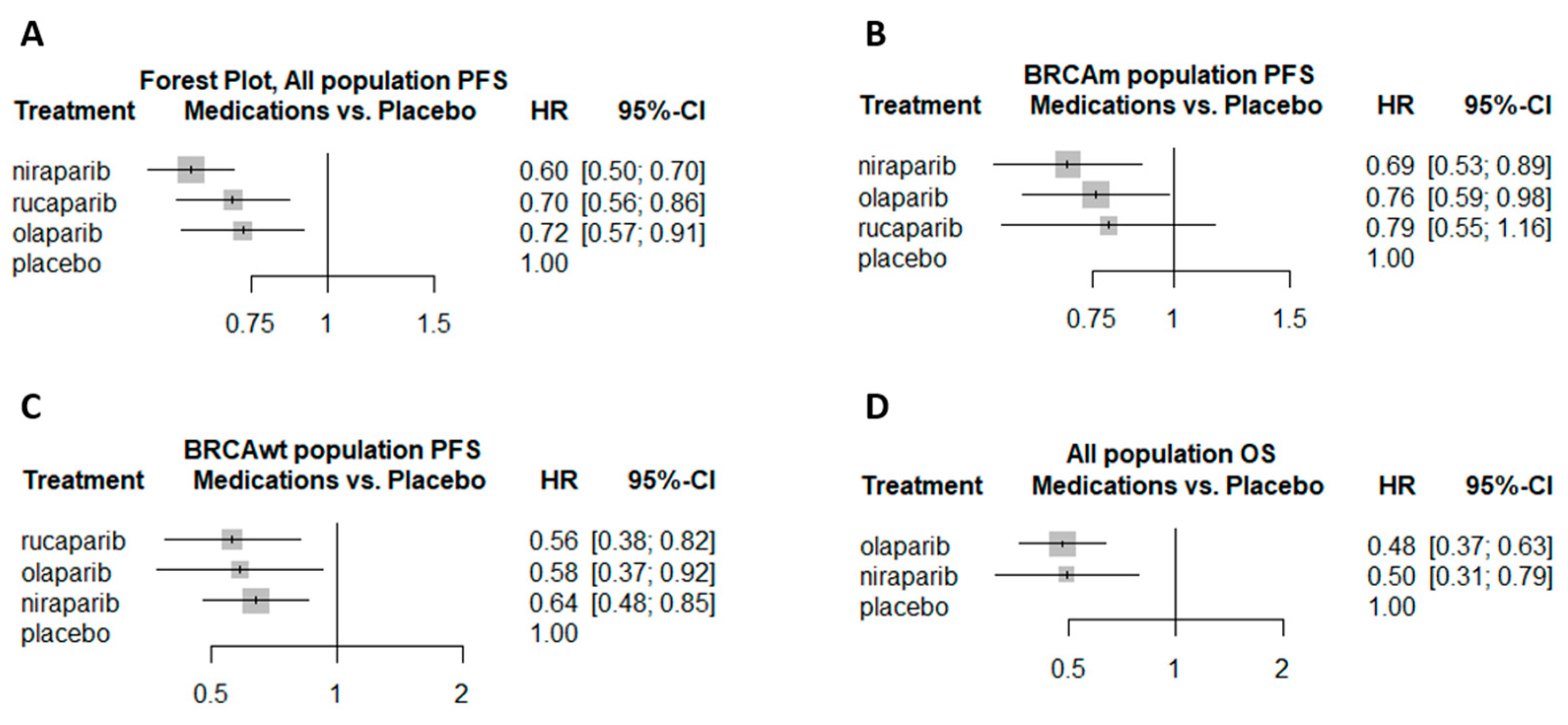
2.3. PFS and OS
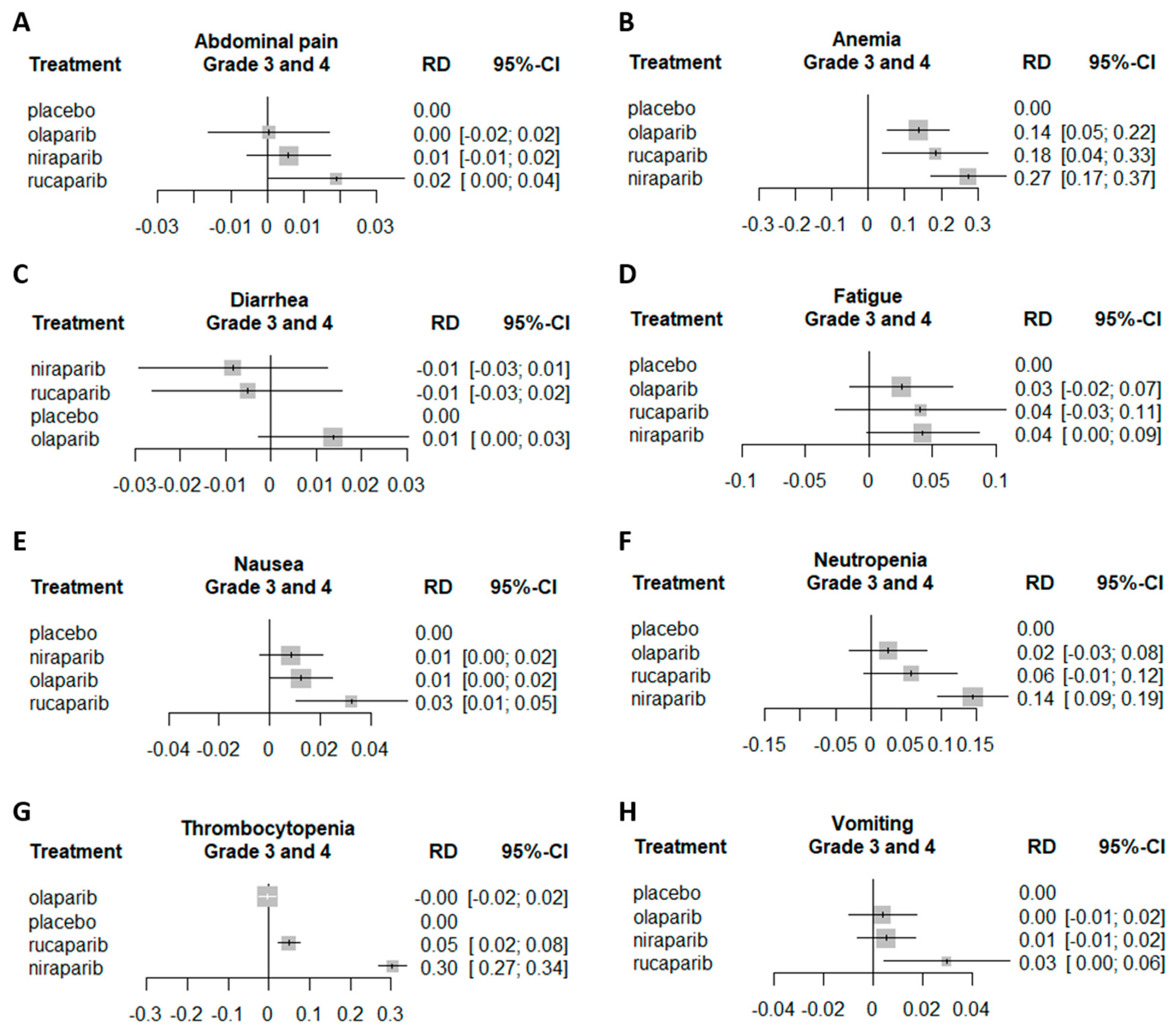
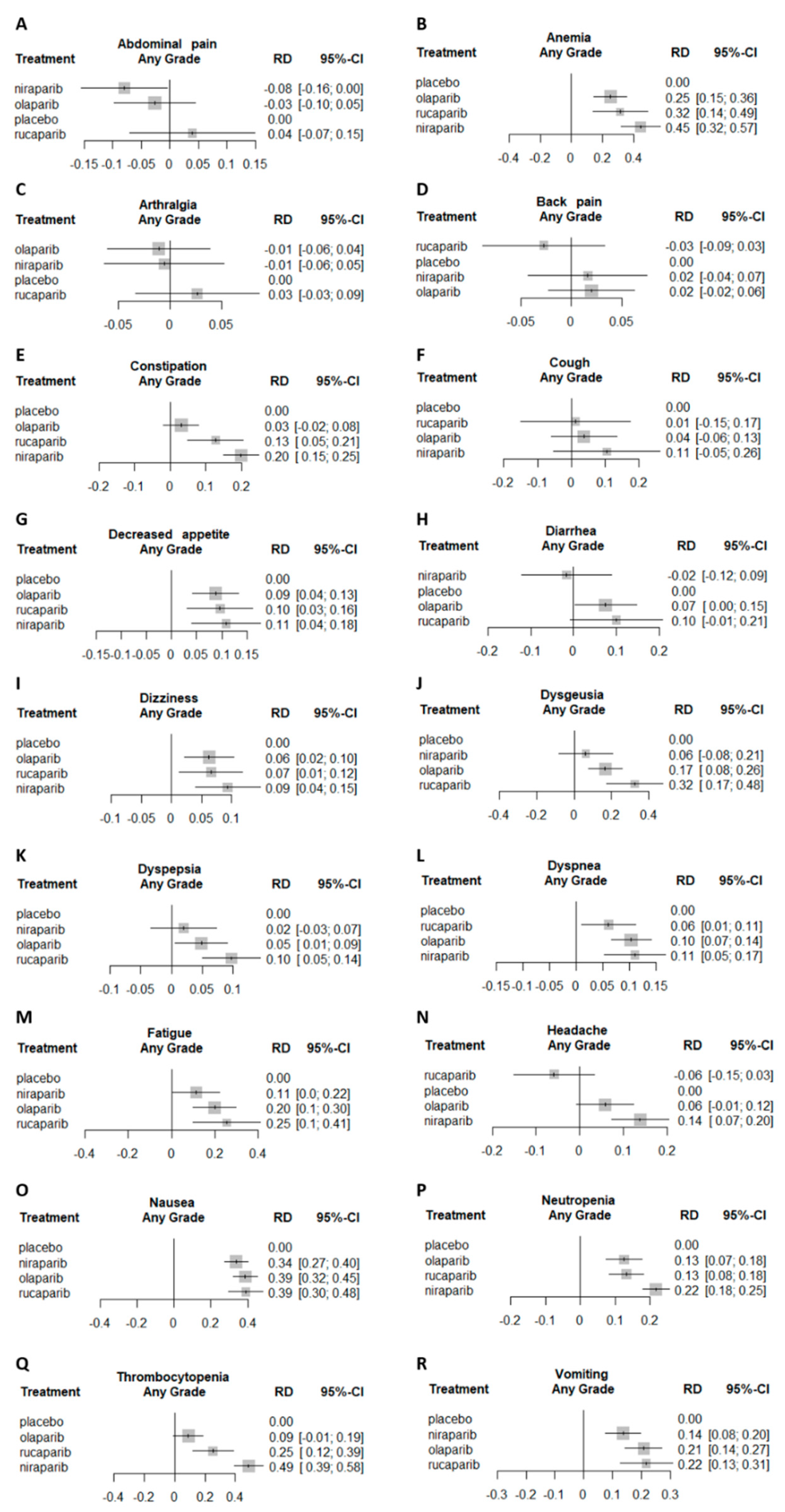
2.4. Adverse Events
2.5. Risk of Biased Assessment
3. Discussion
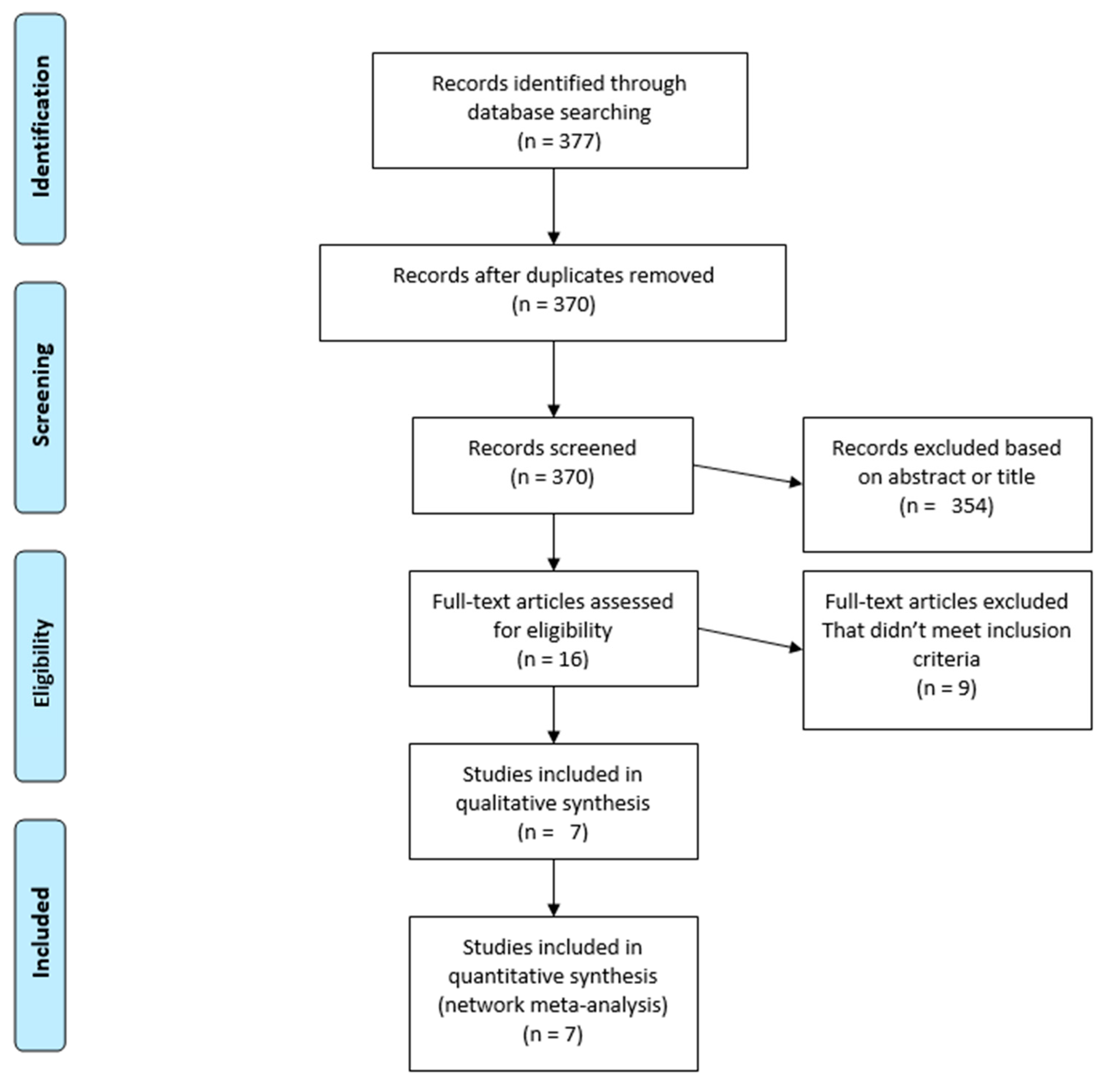
4. Methods
4.1. Systematic Review
4.2. Outcomes of Interest
4.3. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.B.F. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France, 2018; Available online: https://gco.iarc.fr/today (accessed on 25 February 2020).
- Leslie, R.; Boyd, M.F.M.M.M. Carboplatin/Paclitaxel Induction in Ovarian Cancer: The Finer Points. Oncology 2018, 32, 418–420. [Google Scholar]
- Jayson, G.C.; Kohn, E.C.; Kitchener, H.C.; Ledermann, J.A. Ovarian cancer. Lancet 2014, 384, 1376–1388. [Google Scholar] [CrossRef]
- Matulonis, U.A.; Sood, A.K.; Fallowfield, L.; Howitt, B.E.; Sehouli, J.; Karlan, B.Y. Ovarian cancer. Nat. Rev. Dis. Prim. 2016, 2, 1–22. [Google Scholar] [CrossRef]
- Jiang, X.; Li, W.; Li, X.; Bai, H.; Zhang, Z. Current status and future prospects of PARP inhibitor clinical trials in ovarian cancer. Cancer Manag. Res. 2019, 11, 4371–4390. [Google Scholar] [CrossRef]
- Stewart, C.; Ralyea, C.; Lockwood, S. Ovarian Cancer: An Integrated Review. Semin. Oncol. Nurs. 2019, 35, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Fong, P.C.; Boss, D.S.; Yap, T.A.; Tutt, A.; Wu, P.; Mergui-Roelvink, M.; Mortimer, P.; Swaisland, H.; Lau, A.; O’Connor, M.J.; et al. Inhibition of Poly(ADP-Ribose) Polymerase in Tumors from BRCA Mutation Carriers. N. Engl. J. Med. 2009, 361, 123–134. [Google Scholar] [CrossRef]
- Mukhopadhyay, A.; Plummer, E.R.; Elattar, A.; Soohoo, S.; Uzir, B.; Quinn, J.E.; McCluggage, W.G.; Maxwell, P.; Aneke, H.; Curtin, N.J.; et al. Clinicopathological features of homologous recombination-deficient epithelial ovarian cancers: Sensitivity to PARP inhibitors, platinum, and survival. Cancer Res. 2012, 72, 5675–5682. [Google Scholar] [CrossRef]
- Yap, T.A.; Plummer, R.; Azad, N.S.; Helleday, T. The DNA Damaging Revolution: PARP Inhibitors and Beyond. Am. Soc. Clin. Oncol. Educ. B 2019, 185–195. [Google Scholar] [CrossRef]
- FDA Approved Olaparib (LYNPARZA, AstraZeneca Pharmaceuticals LP) for the Maintenance Treatment of Adult Patients with Deleterious or Suspected Deleterious Germline or Somatic BRCA-Mutated (gBRCAm or sBRCAm) Advanced Epithelial Ovarian, Fallopian Tube or Primary Peritoneal Cancer Who Are in Complete or Partial Response to First-Line Platinum-Based. Available online: https://www.fda.gov/drugs/fda-approved-olaparib-lynparza-astrazeneca-pharmaceuticals-lp-maintenance-treatment-adult-patients (accessed on 27 February 2020).
- FDA Approves Rucaparib for Maintenance Treatment of Recurrent Ovarian, Fallopian Tube, or Primary Peritoneal Cancer. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-rucaparib-maintenance-treatment-recurrent-ovarian-fallopian-tube-or-primary-peritoneal (accessed on 27 February 2020).
- Niraparib (ZEJULA). Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/niraparib-zejula (accessed on 27 February 2020).
- FDA Approves Niraparib for First-Line Maintenance of Advanced Ovarian Cancer. Available online: https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-niraparib-first-line-maintenance-advanced-ovarian-cancer (accessed on 27 August 2020).
- Antolin, A.A.; Ameratunga, M.; Banerji, U.; Clarke, P.A.; Workman, P.; Al-Lazikani, B. The kinase polypharmacology landscape of clinical PARP inhibitors. Sci. Rep. 2020, 10, 1–14. [Google Scholar] [CrossRef]
- Tonin, F.S.; Rotta, I.; Mendes, A.M.; Pontarolo, R. Network meta-analysis: A technique to gather evidence from direct and indirect comparisons. Pharm. Pract. (Granada) 2017, 15, 4. [Google Scholar] [CrossRef]
- González-Martín, A.; Pothuri, B.; Vergote, I.; DePont Christensen, R.; Graybill, W.; Mirza, M.R.; McCormick, C.; Lorusso, D.; Hoskins, P.; Freyer, G.; et al. Niraparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2019, 381, 2391–2402. [Google Scholar] [CrossRef] [PubMed]
- Mirza, M.R.; Monk, B.J.; Herrstedt, J.; Oza, A.M.; Mahner, S.; Redondo, A.; Fabbro, M.; Ledermann, J.A.; Lorusso, D.; Vergote, I.; et al. Niraparib Maintenance Therapy in Platinum-Sensitive, Recurrent Ovarian Cancer. N. Engl. J. Med. 2016, 375, 2154–2164. [Google Scholar] [CrossRef] [PubMed]
- Coleman, R.L.; Oza, A.M.; Lorusso, D.; Aghajanian, C.; Oaknin, A.; Dean, A.; Colombo, N.; Weberpals, J.I.; Clamp, A.; Scambia, G.; et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 390, 1949–1961. [Google Scholar] [CrossRef]
- Moore, K.; Colombo, N.; Scambia, G.; Kim, B.-G.; Oaknin, A.; Friedlander, M.; Lisyanskaya, A.; Floquet, A.; Leary, A.; Sonke, G.S.; et al. Maintenance Olaparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2018, 379, 2495–2505. [Google Scholar] [CrossRef]
- Ledermann, J.; Harter, P.; Gourley, C.; Friedlander, M.; Vergote, I.; Rustin, G.; Scott, C.; Meier, W.; Shapira-Frommer, R.; Safra, T.; et al. Olaparib Maintenance Therapy in Platinum-Sensitive Relapsed Ovarian Cancer. N. Engl. J. Med. 2012, 366, 1382–1392. [Google Scholar] [CrossRef] [PubMed]
- Ledermann, J.; Harter, P.; Gourley, C.; Friedlander, M.; Vergote, I.; Rustin, G.; Scott, C.L.; Meier, W.; Shapira-Frommer, R.; Safra, T.; et al. Olaparib maintenance therapy in patients with platinum-sensitive relapsed serous ovarian cancer: A preplanned retrospective analysis of outcomes by BRCA status in a randomised phase 2 trial. Lancet Oncol. 2014, 15, 852–861. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, M.; Matulonis, U.; Gourley, C.; du Bois, A.; Vergote, I.; Rustin, G.; Scott, C.; Meier, W.; Shapira-Frommer, R.; Safra, T.; et al. Long-term efficacy, tolerability and overall survival in patients with platinum-sensitive, recurrent high-grade serous ovarian cancer treated with maintenance olaparib capsules following response to chemotherapy. Br. J. Cancer 2018, 119, 1075–1085. [Google Scholar] [CrossRef]
- Pujade-Lauraine, E.; Ledermann, J.A.; Selle, F.; Gebski, V.; Penson, R.T.; Oza, A.M.; Korach, J.; Huzarski, T.; Poveda, A.; Pignata, S.; et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): A double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017, 18, 1274–1284. [Google Scholar] [CrossRef]
- Ledermann, J.A.; Pujade-Lauraine, E. Olaparib as maintenance treatment for patients with platinum-sensitive relapsed ovarian cancer. Ther. Adv. Med. Oncol. 2019, 11, 1758835919849753. [Google Scholar] [CrossRef]
- Berek, J.S.; Matulonis, U.A.; Peen, U.; Ghatage, P.; Mahner, S.; Redondo, A.; Lesoin, A.; Colombo, N.; Vergote, I.; Rosengarten, O.; et al. Safety and dose modification for patients receiving niraparib. Ann. Oncol. 2018, 29, 1784–1792. [Google Scholar] [CrossRef]
- Thorsell, A.G.; Ekblad, T.; Karlberg, T.; Löw, M.; Pinto, A.F.; Trésaugues, L.; Moche, M.; Cohen, M.S.; Schüler, H. Structural Basis for Potency and Promiscuity in Poly(ADP-ribose) Polymerase (PARP) and Tankyrase Inhibitors. J. Med. Chem. 2017, 60, 1262–1271. [Google Scholar] [CrossRef] [PubMed]
- Antolín, A.A.; Mestres, J. Linking off-target kinase pharmacology to the differential cellular effects observed among PARP inhibitors. Oncotarget 2014, 5, 3023–3028. [Google Scholar] [CrossRef]
- LaFargue, C.J.; Dal Molin, G.Z.; Sood, A.K.; Coleman, R.L. Exploring and comparing adverse events between PARP inhibitors. Lancet Oncol. 2019, 20, e15–e28. [Google Scholar] [CrossRef]
- Friedlander, M.; Gebski, V.; Gibbs, E.; Davies, L.; Bloomfield, R.; Hilpert, F.; Wenzel, L.B.; Eek, D.; Rodrigues, M.; Clamp, A.; et al. Health-related quality of life and patient-centred outcomes with olaparib maintenance after chemotherapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT Ov-21): A placebo-controlled, phase 3 randomised trial. Lancet Oncol. 2018, 19, 1126–1134. [Google Scholar] [CrossRef]
- Ledermann, J.A.; Harter, P.; Gourley, C.; Friedlander, M.; Vergote, I.; Rustin, G.; Scott, C.; Meier, W.; Shapira-Frommer, R.; Safra, T.; et al. Quality of life during olaparib maintenance therapy in platinum-sensitive relapsed serous ovarian cancer. Br. J. Cancer 2016, 115, 1313–1320. [Google Scholar] [CrossRef]
- Matulonis, U.A.; Walder, L.; Nøttrup, T.J.; Bessette, P.; Mahner, S.; Gil-Martin, M.; Kalbacher, E.; Ledermann, J.A.; Wenham, R.M.; Woie, K.; et al. Niraparib maintenance treatment improves time without symptoms or toxicity (twist) versus routine surveillance in recurrent ovarian cancer: A twist analysis of the engot-ov16/ nova trial. J. Clin. Oncol. 2019, 37, 3183–3191. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Hong, H.; Carlin, B.P.; Shamliyan, T.A.; Wyman, J.F.; Ramakrishnan, R.; Sainfort, F.; Kane, R.L. Comparing Bayesian and frequentist approaches for multiple outcome mixed treatment comparisons. Med. Decis. Mak. 2013, 33, 702–714. [Google Scholar] [CrossRef] [PubMed]
- Comparing Bayesian and Frequentist Approaches for Network Meta-Analysis: An Empirical Study Colloquium Abstracts. Available online: https://abstracts.cochrane.org/2017-global-evidence-summit/comparing-bayesian-and-frequentist-approaches-network-meta-analysis (accessed on 28 February 2020).
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2015. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Study 19 Ledermann 2012+ Friedlander 2018 | Nova Mirza 2016 | Ariel 3 Coleman 2017 | Solo2 Pujade-lauraine 2017 | Prima Gonzalez-martin 2019 | Solo1 Moore 2018 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ola | Pla | Nir | Pla | Ruc | Pla | Ola | Pla | Nir | Pla | Ola | Pla | |||
| Median age (range) years | 58 (21–89) | 59 (33–84) | 57,63 (33–84) | 58, 61 (34–82) | 61 (53–67) | 62 (53–68) | 56 (51–63) | 56 (49–63) | 62 (32–85) | 62 (33–88) | 53 (29–82) | 53 (31–84) | ||
| Primary tumor location, n (%) | Ovary | 119 (87.5) | 109 (84.5) | 314 (84.4) | 149 (82.3) | 312 (83) | 149 (79) | 164 (84) | 86 (87) | 388 (79.7) | 201 (81.7) | 220 (85) | 113 (86) | |
| Fallopian | 3 (2.2) | 4 (3.1) | 27 (7.2) | 17 (9.4) | 32 (9) | 10 (5) | 31 (16) | 13 (13) | 65 (13.3) | 32 (13.0) | 22 (8) | 11 (8) | ||
| Peritoneum | 14 (10.3) | 16 (12.4) | 31 (8.3) | 14 (7.8) | 31 (8) | 19 (10) | NR | NR | 34 (7.0) | 13 (5.3) | 15 (6) | 7 (5) | ||
| Time to progression after completion of penultimate platinum-based regime, n (%) | 6 to 12 months | 53 (39.0) | 54 (41.9) | 144 (38.7) | 70 (38.7) | 151 (40) | 76 (40) | 79 (40) | 40 (40) | NR | NR | NR | NR | |
| above 12 months | 83 (61.0) | 75 (58.1) | 228 (61.3) | 111 (61.3) | 224 (60) | 113 (60) | 117 (60) | 59 (60) | NR | NR | NR | NR | ||
| Objective response to most recent platinum-based regimen, n (%) | Complete response | 57 (41.9) | 63 (48.8) | 188 (50.5) | 93 (51.4) | 126 (34) | 64 (34) | 91 (46) | 47 (47) | 337 (69.2) | 172 (70.0) | 213 (82) | 107 (82) | |
| Partial response | 79 (58.1) | 66 (51.2) | 184 (49.5) | 88 (48.6) | 249 (66) | 125 (66) | 105 (54) | 52 (53) | 150 (30.8) | 74 (30.0) | 47 (18) | 24 (18) | ||
| BRCA status, n (%) | BRCA1 or BRCA2 | 31 (22.8) | 28 (21.7) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | |
| BRCA1 | 25 (18.4) | 20 (15.5) | 85 (22.8) | 43 (23.8) | 80 (21) | 37 (20) | 132 (67) | 61 (62) | NR | NR | 191 (73) | 91 (69) | ||
| BRCA2 | 6 (4.4) | 7 (5.4) | 51 (13.7) | 18 (9.9) | 50 (13) | 29 (15) | 58 (30) | 35 (35) | NR | NR | 66 (25) | 40 (31) | ||
| Both | 0 | 1 (0.8) | 9 (2.4) | 4 (2.2) | NR | NR | 0 | 0 | NR | NR | 3 (1) | 0 | ||
| Wildtype | 98 (37) | NR | NR | 245 (65) | 123 (65) | NR | NR | NR | NR | NR | NR | |||
| Mutation | 111 (42) | NR | NR | 130 (35) | 66 (35) | NR | NR | NR | NR | NR | NR | |||
| Previous chemotherapy regimens, n (%) | 1,2 | 59 (43) | 63 (49) | 226 (60.8) | 107 (59.1) | 231 (62) | 124 (66) | 110 (56) * | 62 (63) * | NR | NR | NR | NR | |
| ≥3 | 77 (57) | 66 (51) | 146 (39.2) | 73 (40.3) | 144 (38) | 65 (34) | 85 (44) * | 37 (37) * | NR | NR | NR | NR | ||
| Stage, n (%) | 1,2 | NR | NR | 45 (12.1) | 15 (8.3) | NR | NR | NR | NR | 0 | 0 | 0 | 0 | |
| 3 | NR | NR | 268 (72.0) | 132 (72.9) | NR | NR | NR | NR | 318 (65.3) | 158 (64.2) | 220 (85) | 105 (80) | ||
| 4 | NR | NR | 58 (15.6) | 33 (18.2) | NR | NR | NR | NR | 169 (34.7) | 88 (35.8) | 40 (15) | 26 (20) | ||
| ECOG, n (%) | 0 1 2 Unknown | 110 (80.9) 23 (16.9) 1 (0.7) 2 (1.5) | 95 (73.6) 30(23.3) 2(1.6) 2(1.6) | 251(67.4) 121(33.6) -- -- | 126(69.6) 55(30.4) -- -- | 280(75) 95 (25) | 136 (72) 53 (28) | 162 (83) 32 (16) 2 (1) | 77 (78) 22 (22) 0 | 337 (69.2) 65 (26.3) | 174 (70.4) 72 (29.3) | 200 (76.9) 60 (23.1) 0 | 105 (80.2) 25 (19.1) 1 (0.8) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stemmer, A.; Shafran, I.; Stemmer, S.M.; Tsoref, D. Comparison of Poly (ADP-ribose) Polymerase Inhibitors (PARPis) as Maintenance Therapy for Platinum-Sensitive Ovarian Cancer: Systematic Review and Network Meta-Analysis. Cancers 2020, 12, 3026. https://doi.org/10.3390/cancers12103026
Stemmer A, Shafran I, Stemmer SM, Tsoref D. Comparison of Poly (ADP-ribose) Polymerase Inhibitors (PARPis) as Maintenance Therapy for Platinum-Sensitive Ovarian Cancer: Systematic Review and Network Meta-Analysis. Cancers. 2020; 12(10):3026. https://doi.org/10.3390/cancers12103026
Chicago/Turabian StyleStemmer, Amos, Inbal Shafran, Salomon M. Stemmer, and Daliah Tsoref. 2020. "Comparison of Poly (ADP-ribose) Polymerase Inhibitors (PARPis) as Maintenance Therapy for Platinum-Sensitive Ovarian Cancer: Systematic Review and Network Meta-Analysis" Cancers 12, no. 10: 3026. https://doi.org/10.3390/cancers12103026
APA StyleStemmer, A., Shafran, I., Stemmer, S. M., & Tsoref, D. (2020). Comparison of Poly (ADP-ribose) Polymerase Inhibitors (PARPis) as Maintenance Therapy for Platinum-Sensitive Ovarian Cancer: Systematic Review and Network Meta-Analysis. Cancers, 12(10), 3026. https://doi.org/10.3390/cancers12103026





