Arthralgia Induced by BRAF Inhibitor Therapy in Melanoma Patients
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Data Collection
2.3. Statistical Analysis
2.4. Ethical Approval
3. Results
3.1. Patient Characteristics
3.2. Arthralgia
3.3. Influencing Factors in the Development of Arthralgia
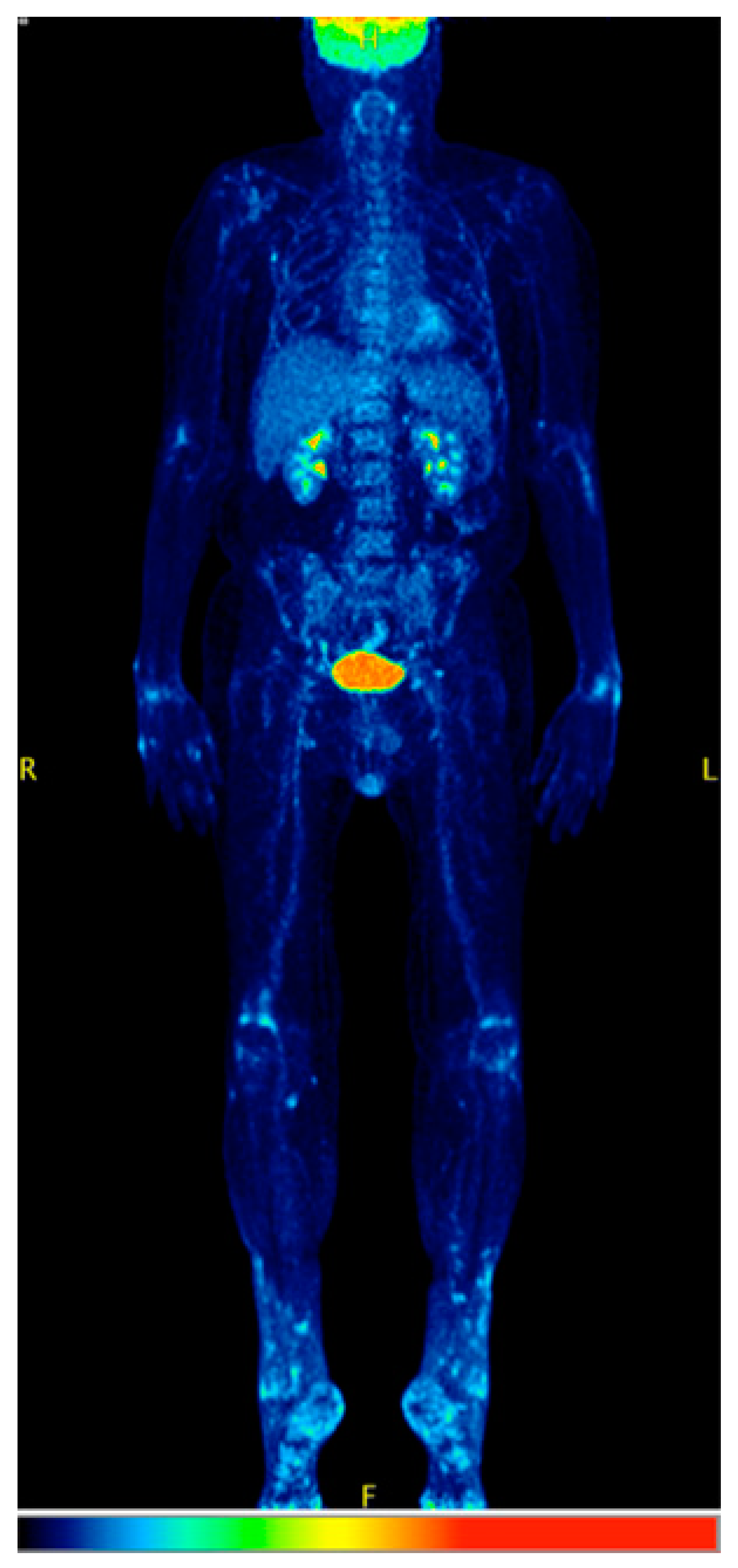
3.4. Imaging
3.5. Serology
3.6. Management of Arthralgia
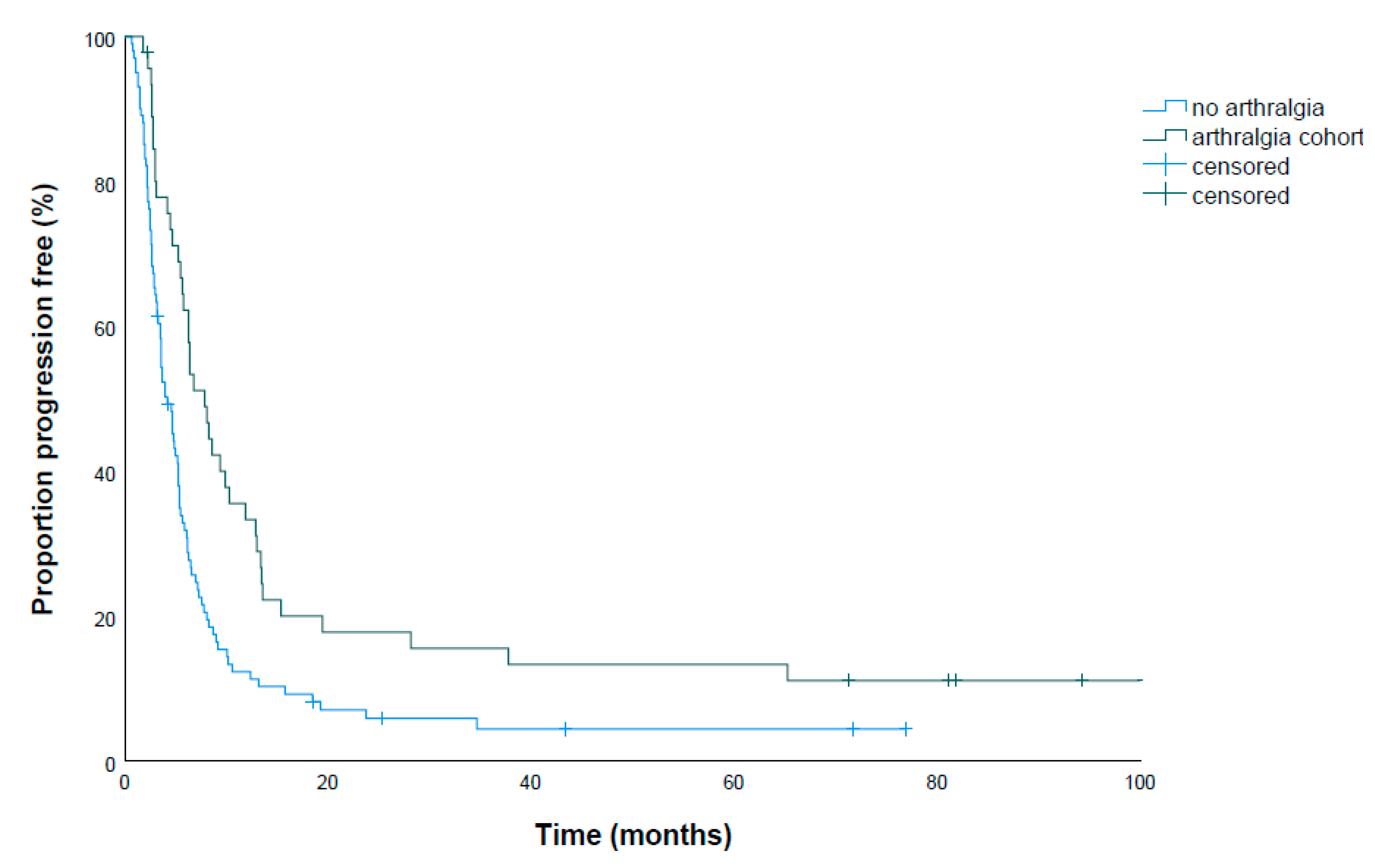
3.7. Treatment Efficacy
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ACPA | Anti-citrullinated protein antibodies |
| ANA | Antinuclear antibodies |
| BRAFi | BRAF inhibitor |
| CI | Confidence interval |
| CRP | C-reactive protein |
| CT | Computed tomography |
| DMARD | Disease-modifying antirheumatic drug |
| FDG-PET | Fludeoxyglucose positron emission tomography |
| ICI | Immune-checkpoint inhibitor |
| irAE | Immune-related adverse event |
| MEKi | MEK inhibitor |
| MM | Metastatic melanoma |
| MRI | Magnetic resonance imaging |
| NCT | National Center for Tumor Diseases, Heidelberg |
| NSAID | Non-steroidal antirheumatic drug |
| OS | Overall survival |
| PFS | Progression-free survival |
References
- US Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE), Version 4.03; US Department of Health and Human Services: Washington, DC, USA; Bethesda: Rockville, MD, USA, 2010.
- Chapman, P.B.; Hauschild, A.; Robert, C.; Haanen, J.B.; Ascierto, P.; Larkin, J.; Dummer, R.; Garbe, C.; Testori, A.; Maio, M.; et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 2011, 364, 2507–2516. [Google Scholar] [CrossRef] [PubMed]
- Sosman, J.A.; Kim, K.B.; Schuchter, L.; Gonzalez, R.; Pavlick, A.C.; Weber, J.S.; McArthur, G.A.; Hutson, T.E.; Moschos, S.J.; Flaherty, K.T.; et al. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N. Engl. J. Med. 2012, 366, 707–714. [Google Scholar] [CrossRef] [PubMed]
- Larkin, J.; Del Vecchio, M.; Ascierto, P.A.; Krajsova, I.; Schachter, J.; Neyns, B.; Espinosa, E.; Garbe, C.; Sileni, V.C.; Gogas, H.; et al. Vemurafenib in patients with BRAF(V600) mutated metastatic melanoma: An open-label, multicentre, safety study. Lancet Oncol. 2014, 15, 436–444. [Google Scholar] [CrossRef]
- Kim, G.; McKee, A.E.; Ning, Y.M.; Hazarika, M.; Theoret, M.; Johnson, J.R.; Xu, Q.C.; Tang, S.; Sridhara, R.; Jiang, X.; et al. FDA approval summary: Vemurafenib for treatment of unresectable or metastatic melanoma with the BRAFV600E mutation. Clin. Cancer Res. 2014, 20, 4994–5000. [Google Scholar] [CrossRef] [PubMed]
- Arance, A.M.; Berrocal, A.; Lopez-Martin, J.A.; de la Cruz-Merino, L.; Soriano, V.; Martin Algarra, S.; Alonso, L.; Cerezuela, P.; La Orden, B.; Espinosa, E. Safety of vemurafenib in patients with BRAF (V600) mutated metastatic melanoma: The Spanish experience. Clin. Transl. Oncol. 2016, 18, 1147–1157. [Google Scholar] [CrossRef]
- Blank, C.U.; Larkin, J.; Arance, A.M.; Hauschild, A.; Queirolo, P.; Del Vecchio, M.; Ascierto, P.A.; Krajsova, I.; Schachter, J.; Neyns, B.; et al. Open-label, multicentre safety study of vemurafenib in 3219 patients with BRAF(V600) mutation-positive metastatic melanoma: 2-year follow-up data and long-term responders’ analysis. Eur. J. Cancer 2017, 79, 176–184. [Google Scholar] [CrossRef]
- Maio, M.; Lewis, K.; Demidov, L.; Mandala, M.; Bondarenko, I.; Ascierto, P.A.; Herbert, C.; Mackiewicz, A.; Rutkowski, P.; Guminski, A.; et al. Adjuvant vemurafenib in resected, BRAF(V600) mutation-positive melanoma (BRIM8): A randomised, double-blind, placebo-controlled, multicentre, phase 3 trial. Lancet Oncol. 2018, 19, 510–520. [Google Scholar] [CrossRef]
- Dummer, R.; Ascierto, P.A.; Gogas, H.J.; Arance, A.; Mandala, M.; Liszkay, G.; Garbe, C.; Schadendorf, D.; Krajsova, I.; Gutzmer, R.; et al. Overall survival in patients with BRAF-mutant melanoma receiving encorafenib plus binimetinib versus vemurafenib or encorafenib (COLUMBUS): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2018, 19, 1315–1327. [Google Scholar] [CrossRef]
- Si, L.; Zhang, X.; Xu, Z.; Jiang, Q.; Bu, L.; Wang, X.; Mao, L.; Zhang, W.; Richie, N.; Guo, J. Vemurafenib in Chinese patients with BRAF(V600) mutation-positive unresectable or metastatic melanoma: An open-label, multicenter phase I study. BMC Cancer 2018, 18, 520. [Google Scholar] [CrossRef]
- Hauschild, A.; Grob, J.J.; Demidov, L.V.; Jouary, T.; Gutzmer, R.; Millward, M.; Rutkowski, P.; Blank, C.U.; Miller, W.H., Jr.; Kaempgen, E.; et al. Dabrafenib in BRAF-mutated metastatic melanoma: A multicentre, open-label, phase 3 randomised controlled trial. Lancet 2012, 380, 358–365. [Google Scholar] [CrossRef]
- Flaherty, K.T.; Infante, J.R.; Daud, A.; Gonzalez, R.; Kefford, R.F.; Sosman, J.; Hamid, O.; Schuchter, L.; Cebon, J.; Ibrahim, N.; et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. N. Engl. J. Med. 2012, 367, 1694–1703. [Google Scholar] [CrossRef] [PubMed]
- Ascierto, P.A.; Minor, D.; Ribas, A.; Lebbe, C.; O’Hagan, A.; Arya, N.; Guckert, M.; Schadendorf, D.; Kefford, R.F.; Grob, J.J.; et al. Phase II trial (BREAK-2) of the BRAF inhibitor dabrafenib (GSK2118436) in patients with metastatic melanoma. J. Clin. Oncol. 2013, 31, 3205–3211. [Google Scholar] [CrossRef] [PubMed]
- Long, G.V.; Stroyakovskiy, D.; Gogas, H.; Levchenko, E.; de Braud, F.; Larkin, J.; Garbe, C.; Jouary, T.; Hauschild, A.; Grob, J.J.; et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N. Engl. J. Med. 2014, 371, 1877–1888. [Google Scholar] [CrossRef] [PubMed]
- Ribas, A.; Gonzalez, R.; Pavlick, A.; Hamid, O.; Gajewski, T.F.; Daud, A.; Flaherty, L.; Logan, T.; Chmielowski, B.; Lewis, K.; et al. Combination of vemurafenib and cobimetinib in patients with advanced BRAF(V600)-mutated melanoma: A phase 1b study. Lancet Oncol. 2014, 15, 954–965. [Google Scholar] [CrossRef]
- Mackin, A.G.; Pecen, P.E.; Dinsmore, A.L.; Patnaik, J.L.; Gonzalez, R.; Robinson, W.A.; Palestine, A.G. Inflammatory side effects of BRAF and MEK inhibitors. Melanoma Res. 2019, 29, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Buder-Bakhaya, K.; Benesova, K.; Schulz, C.; Anwar, H.; Dimitrakopoulou-Strauss, A.; Weber, T.F.; Enk, A.; Lorenz, H.M.; Hassel, J.C. Characterization of arthralgia induced by PD-1 antibody treatment in patients with metastasized cutaneous malignancies. Cancer Immunol. Immunother. 2018, 67, 175–182. [Google Scholar] [CrossRef]
- Benesova, K.L.; Lorenz, H.-M.; Leipe, J.; Jordan, K. How I treat cancer: Treatment of rheumatological side effects of immunotherapy. ESMO Open 2019, 4, e000529. [Google Scholar] [CrossRef]
- Zimmer, L.; Livingstone, E.; Hillen, U.; Domkes, S.; Becker, A.; Schadendorf, D. Panniculitis with arthralgia in patients with melanoma treated with selective BRAF inhibitors and its management. Arch. Dermatol. 2012, 148, 357–361. [Google Scholar] [CrossRef]
- Mossner, R.; Zimmer, L.; Berking, C.; Hoeller, C.; Loquai, C.; Richtig, E.; Kahler, K.C.; Hassel, J.C.; Gutzmer, R.; Ugurel, S. Erythema nodosum-like lesions during BRAF inhibitor therapy: Report on 16 new cases and review of the literature. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 1797–1806. [Google Scholar] [CrossRef]
- Babacan, T.; Turkbeyler, I.H.; Balakan, O.; Pehlivan, Y.; Suner, A.; Kisacik, B. A case of vemurafenib-induced polyarhritis in a patient with melanoma: How to manage it? Int. J. Rheum. Dis. 2017, 20, 398–401. [Google Scholar] [CrossRef]
- Heinzerling, L.; Eigentler, T.K.; Fluck, M.; Hassel, J.C.; Heller-Schenck, D.; Leipe, J.; Pauschinger, M.; Vogel, A.; Zimmer, L.; Gutzmer, R. Tolerability of BRAF/MEK inhibitor combinations: Adverse event evaluation and management. ESMO Open 2019, 4, e000491. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Dimitrakopoulou-Strauss, A. Monitoring of patients with metastatic melanoma treated with immune checkpoint inhibitors using PET-CT. Cancer Immunol. Immunother. 2019, 68, 813–822. [Google Scholar] [CrossRef] [PubMed]
- Arnett, F.C.; Edworthy, S.M.; Bloch, D.A.; McShane, D.J.; Fries, J.F.; Cooper, N.S.; Healey, L.A.; Kaplan, S.R.; Liang, M.H.; Luthra, H.S.; et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O., 3rd; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef]
- Kostine, M.; Finckh, A.; Bingham, C.O., 3rd; Visser, K.; Leipe, J.; Schulze-Koops, H.; Choy, E.H.; Benesova, K.; Radstake, T.; Cope, A.P.; et al. EULAR points to consider for the diagnosis and management of rheumatic immune-related adverse events due to cancer immunotherapy with checkpoint inhibitors. Ann. Rheum. Dis. 2020. [Google Scholar] [CrossRef]
- Mouterde, G.; Rincheval, N.; Lukas, C.; Daien, C.; Saraux, A.; Dieudé, P.; Morel, J.; Combe, B. Outcome of patients with early arthritis without rheumatoid factor and ACPA and predictors of rheumatoid arthritis in the ESPOIR cohort. Arthritis Res. Ther. 2019, 21, 140. [Google Scholar] [CrossRef]
- Charpin, C.; Arnoux, F.; Martin, M.; Toussirot, E.; Lambert, N.; Balandraud, N.; Wendling, D.; Diot, E.; Roudier, J.; Auger, I. New autoantibodies in early rheumatoid arthritis. Arthritis Res. Ther. 2013, 15, R78. [Google Scholar] [CrossRef]
- Weisbart, R.H.; Chan, G.; Heinze, E.; Mory, R.; Nishimura, R.N.; Colburn, K. BRAF drives synovial fibroblast transformation in rheumatoid arthritis. J. Biol. Chem. 2010, 285, 34299–34303. [Google Scholar] [CrossRef]
- Weisbart, R.H.; Chan, G.; Li, E.; Farmani, N.; Heinze, E.; Rubell, A.; Nishimura, R.N.; Colburn, K. BRAF splice variants in rheumatoid arthritis synovial fibroblasts activate MAPK through CRAF. Mol. Immunol. 2013, 55, 247–252. [Google Scholar] [CrossRef]
- Arnoux, F.; Fina, F.; Lambert, N.; Balandraud, N.; Martin, M.; Ouafik, L.; Kanaan, S.B.; Roudier, J.; Auger, I. Newly Identified BRAF Mutation in Rheumatoid Arthritis. Arthritis Rheumatol. 2016, 68, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Auger, I.; Balandraud, N.; Rak, J.; Lambert, N.; Martin, M.; Roudier, J. New autoantigens in rheumatoid arthritis (RA): Screening 8268 protein arrays with sera from patients with RA. Ann. Rheum. Dis. 2009, 68, 591–594. [Google Scholar] [CrossRef] [PubMed]
- Charpin, C.; Martin, M.; Balandraud, N.; Roudier, J.; Auger, I. Autoantibodies to BRAF, a new family of autoantibodies associated with rheumatoid arthritis. Arthritis Res. Ther. 2010, 12, R194. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Wang, Y.; Hong, Y.; Ye, X.; Shi, P.; Zhang, J.; Zhao, Q. Incidence and relative risk of cutaneous squamous cell carcinoma with single-agent BRAF inhibitor and dual BRAF/MEK inhibitors in cancer patients: A meta-analysis. Oncotarget 2017, 8, 83280–83291. [Google Scholar] [CrossRef]
- Hassel, J.C.; Groesser, L.; Herschberger, E.; Weichert, W.; Hafner, C. RAS mutations in benign epithelial tumors associated with BRAF inhibitor treatment of melanoma. J. Investig. Dermatol. 2015, 135, 636–639. [Google Scholar] [CrossRef] [PubMed]
- Thiel, M.J.; Schaefer, C.J.; Lesch, M.E.; Mobley, J.L.; Dudley, D.T.; Tecle, H.; Barrett, S.D.; Schrier, D.J.; Flory, C.M. Central role of the MEK/ERK MAP kinase pathway in a mouse model of rheumatoid arthritis: Potential proinflammatory mechanisms. Arthritis Rheum. 2007, 56, 3347–3357. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Kakefuda, R.; Tanimoto, A.; Watanabe, Y.; Tajima, N. Suppressive effect of an orally active MEK1/2 inhibitor in two different animal models for rheumatoid arthritis: A comparison with leflunomide. Inflamm. Res. 2012, 61, 445–454. [Google Scholar] [CrossRef]
- Chan, K.K.; Bass, A.R. Checkpoint inhibitor-induced polymyalgia rheumatica controlled by cobimetinib, a MEK 1/2 inhibitor. Ann. Rheum. Dis. 2019, 78, e70. [Google Scholar] [CrossRef]
- Ben-Betzalel, G.; Baruch, E.N.; Boursi, B.; Steinberg-Silman, Y.; Asher, N.; Shapira-Frommer, R.; Schachter, J.; Markel, G. Possible immune adverse events as predictors of durable response to BRAF inhibitors in patients with BRAF V600-mutant metastatic melanoma. Eur. J. Cancer 2018, 101, 229–235. [Google Scholar] [CrossRef]
- Braaten, T.J.; Brahmer, J.R.; Forde, P.M.; Le, D.; Lipson, E.J.; Naidoo, J.; Schollenberger, M.; Zheng, L.; Bingham, C.O.; Shah, A.A.; et al. Immune checkpoint inhibitor-induced inflammatory arthritis persists after immunotherapy cessation. Ann. Rheum. Dis. 2020, 79, 332–338. [Google Scholar] [CrossRef]
- Sachpekidis, C.; Kopp-Schneider, A.; Hakim-Meibodi, L.; Dimitrakopoulou-Strauss, A.; Hassel, J.C. 18F-FDG PET/CT longitudinal studies in patients with advanced metastatic melanoma for response evaluation of combination treatment with vemurafenib and ipilimumab. Melanoma Res. 2019, 29, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Welsh, S.J.; Corrie, P.G. Management of BRAF and MEK inhibitor toxicities in patients with metastatic melanoma. Ther. Adv. Med. Oncol. 2015, 7, 122–136. [Google Scholar] [CrossRef] [PubMed]
- Benesova, K.; Diekmann, L.; Lorenz, H.M.; Jordan, K.; Leipe, J. OP0270 trheuma registry explores characteristics and suitable diagnostic and therapeutic management of rheumatic immune-related adverse events (IRAES). Ann. Rheum. Dis. 2020, 79, 168–169. [Google Scholar] [CrossRef]

| Drug | Study | n | Arthralgia Any Grade (%) | Arthralgia Grade 3/4 (%) | Comments |
|---|---|---|---|---|---|
| Vemurafenib | Chapman et al. 2011 [2] | 336 | n/a | 11 (3) | grade 1 not documented; 60 patients (18%) experienced grade 2 arthralgia |
| Sosman et al. 2012 [3] | 132 | 78 (59) | 8 (6) | ||
| Larkin et al. 2014 [4] | 3222 | 1259 (39) | 106 (3) | ||
| Kim et al. 2014 [5] | 336 | 180 (54) | 15 (5) | vs. dacarbacine (3% overall) | |
| Arance et al. 2016 [6] | 301 | 134 (44) | 16 (5) | ||
| Blank et al. 2017 [7] | 3219 | 1201 (37) | 102 (3) | ||
| Maio et al. 2018 [8] | 247 | 151 (61) | 17 (7) | adjuvant; vs. placebo (22% overall) | |
| Dummer et al. 2018 [9] | 186 | 85 (46) | 11 (6) | ||
| Si et al. 2018 [10] | 46 | 30 (65) | 0 (0) | ||
| Vemurafenib + Cobimetinib | Ribas et al. 2014 [15] | 63 | 30 (48) | 7 (11) | |
| (Ribas et al. 2014 [15]) | 66 | 8 (12) | 1 (2) | patients had progressed under previous vemurafenib therapy | |
| Dabrafenib | Hauschild et al. 2012 [11] | 100 | n/a | 1 (1) | Grade 1 not documented; 9 (5%) patients experienced grade 2 arthralgia |
| Flaherty et al. 2012 [12] | 53 | 18 (34) | 0 (0) | ||
| Ascierto et al. 2013 [13] | 92 | 30 (33) | 1 (1) | ||
| Long et al. 2014 [14] | 211 | 58 (27) | 0 (0) | ||
| Dabrafenib + Trametinib | Flaherty et al. 2012 [12] | 55 | 15 (27) | 0 (0) | 44% any grade in 1 mg trametinib group |
| Long et al. 2014 [14] | 209 | 52 (24) | 1 (0) | ||
| Encorafenib | Dummer et al. 2018 [9] | 192 | 85 (44) | 18 (9) | |
| Encorafenib + Binimetinib | Dummer et al. 2018 [9] | 192 | 54 (28) | 2 (1) |
| Parameter | Number of Patients in Total Cohort | Number of Patients in Arthralgia Cohort | ||
|---|---|---|---|---|
| (%) | (%) | |||
| Total number of patients | 154 | 100 | 48 | 31.2 |
| Age in years, median (range) | 56 (21–86) | 53 (28–79) | ||
| Gender | ||||
| Male | 97 | 63.0 | 28 | 58.3 |
| Female | 57 | 37.0 | 20 | 41.7 |
| BRAF mutation | ||||
| V600E | 128 | 83.1 | 42 | 89.4 |
| V600K | 15 | 9.7 | 4 | 8.5 |
| V600R | 2 | 1.3 | 0 | 0 |
| V600G | 1 | 0.6 | 0 | 0 |
| unknown | 8 | 5.2 | 2 | 4.2 |
| Type of BRAFi used | ||||
| Vemurafenib | 85 | 55.2 | 31 | 64.6 |
| Vemurafenib + Cobimetinib | 4 | 2.6 | 0 | 0 |
| Dabrafenib | 13 | 8.4 | 3 | 6.3 |
| Dabrafenib + Trametinib | 52 | 33.8 | 14 | 29.2 |
| BRAFi monotherapy | 98 | 63.6 | 34 | 70.8 |
| BRAFi + MEKi | 56 | 36.4 | 14 | 29.2 |
| Duration of BRAFi treatment, median in months, (range in months) | 4.2 | (0.5–93.5) | 7.5 | (1.4–93.5) |
| Number of prior treatments (range) | (0–4) | (0–4) | ||
| 0 | 88 | 57.1 | 32 | 66.7 |
| 1 | 44 | 28.6 | 9 | 18.8 |
| >1 | 22 | 14.3 | 7 | 14.6 |
| Previous checkpoint inhibitor therapy | 45 | 29.2 | 7 | 14.6 |
| Previous PD1-inhibitor | 22 | 14.2 | 3 | 6.3 |
| Previous ipilimumab | 38 | 24.7 | 5 | 10.4 |
| Previous ipilimumab + nivolumab | 10 | 6.5 | 1 | 2.1 |
| Discontinued due to progression | 36 (of 45) | 80.0 | 6 (of 7) | 85.7 |
| Discontinued due to toxicity | 9 (of 45) | 20.0 | 1 (of 7) | 14.3 |
| Previous adjuvant interferon | 44 | 28.6 | 13 | 27.1 |
| Response | 79 | 54.5 | 31 | 64.6 |
| Disease control | 109 | 75.2 | 41 | 85.4 |
| Progression-free survival (median in months) [95% CI] | 5.3 | [4.7–5.9] | 7.9 | [5.7–10.1] |
| Overall survival (median in months) [95% CI] | 10.1 | [8.8–11.4] | 14.9 | [12.4–17.4] |
| Any adverse event | 154 | 100 | 48 | 100 |
| Treatment discontinued | 146 | 94.8 | 45 | 93.8 |
| Parameter | Number of Patients | |
|---|---|---|
| (%) | ||
| Arthralgia with detailed information | 36 | 100 |
| Involvement of small joints | 27 | 75 |
| Finger joints | 19 | 52.8 |
| Wrists | 16 | 44.4 |
| Feet/toes | 6 | 16.7 |
| Involvement of large joints | 19 | 52.8 |
| Knees | 12 | 33.3 |
| Ankles | 10 | 27.8 |
| Shoulders | 8 | 25 |
| Hips | 1 | 2.8 |
| Back | 1 | 2.8 |
| Involvement of small joints only | 17 | 47.2 |
| Involvement of large joints only | 9 | 25.0 |
| Involvement of small and large joints | 10 | 27.8 |
| Symmetrical involvement | 32 (of 41 evaluable) | 78.0 |
| Symmetrical polyarthritis of primarily small joints | 24 | 66.7 |
| Parameter | Category | n | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|---|
| Median PFS (Months) | CI (95%) (Months) | p | Odds Ratio | CI (95%) | p | |||
| Age | <60 | 89 | 5.3 | 4.0–6.6 | 0.603 | 1.03 | 0.71–1.48 | 0.881 |
| >60 | 58 | 4.8 | 4.1–5.5 | |||||
| Sex | Male | 91 | 4.8 | 3.7–5.9 | 0.114 | 0.82 | 0.56–1.20 | 0.302 |
| Female | 56 | 6.2 | 4.9–7.5 | |||||
| Stage (brain metastases) | M0 *–M1c | 86 | 6.2 | 5.4–7.0 | 0.000 | 1.63 | 1.10–2.45 | 0.017 |
| M1d | 61 | 4.2 | 3.0–5.4 | |||||
| Previous ICI treatment | no | 104 | 5.3 | 4.0–6.6 | 0.948 | 0.74 | 0.49–1.13 | 0.487 |
| yes | 43 | 5.3 | 4.6–6.0 | |||||
| Glucocorticoid intake | no | 111 | 5.7 | 4.9–6.5 | 0.000 | 1.92 | 1.23–3.00 | 0.004 |
| yes (any dose) | 36 | 3.2 | 2.6–3.8 | |||||
| MEK inhibitor used | no | 93 | 4.8 | 3.2–6.4 | 0.367 | 0.76 | 0.52–1.12 | 0.165 |
| yes | 54 | 5.4 | 4.6–6.2 | |||||
| BRAF mutation | V600E | 122 | 5.4 | 4.6–6.2 | 0.002 | 1.93 | 1.20–3.11 | 0.007 |
| other | 25 | 3.1 | 2.5–3.7 | |||||
| Elevated LDH | no | 74 | 6.3 | 4.8–7.8 | 0.000 | 2.09 | 1.44–3.02 | 0.000 |
| yes | 69 | 3.6 | 2.8–4.4 | |||||
| Arthralgia | no | 101 | 4.2 | 3.3–5.1 | 0.001 | 0.52 | 0.34–0.78 | 0.002 |
| yes | 46 | 7.9 | 5.7–10.1 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salzmann, M.; Benesova, K.; Buder-Bakhaya, K.; Papamichail, D.; Dimitrakopoulou-Strauss, A.; Lorenz, H.-M.; Enk, A.H.; Hassel, J.C. Arthralgia Induced by BRAF Inhibitor Therapy in Melanoma Patients. Cancers 2020, 12, 3004. https://doi.org/10.3390/cancers12103004
Salzmann M, Benesova K, Buder-Bakhaya K, Papamichail D, Dimitrakopoulou-Strauss A, Lorenz H-M, Enk AH, Hassel JC. Arthralgia Induced by BRAF Inhibitor Therapy in Melanoma Patients. Cancers. 2020; 12(10):3004. https://doi.org/10.3390/cancers12103004
Chicago/Turabian StyleSalzmann, Martin, Karolina Benesova, Kristina Buder-Bakhaya, Dimitrios Papamichail, Antonia Dimitrakopoulou-Strauss, Hanns-Martin Lorenz, Alexander H. Enk, and Jessica C. Hassel. 2020. "Arthralgia Induced by BRAF Inhibitor Therapy in Melanoma Patients" Cancers 12, no. 10: 3004. https://doi.org/10.3390/cancers12103004
APA StyleSalzmann, M., Benesova, K., Buder-Bakhaya, K., Papamichail, D., Dimitrakopoulou-Strauss, A., Lorenz, H.-M., Enk, A. H., & Hassel, J. C. (2020). Arthralgia Induced by BRAF Inhibitor Therapy in Melanoma Patients. Cancers, 12(10), 3004. https://doi.org/10.3390/cancers12103004






