Malignant Rhabdoid Tumor, an Aggressive Tumor Often Misclassified as Small Cell Variant of Hepatoblastoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Samples
2.2. Immunohistochemistry
2.3. Molecular Analysis
2.3.1. Somatic Copy Number Variant Analysis (SCNA)
2.3.2. Cancer Whole Exome Sequencing and Transcriptome
3. Results
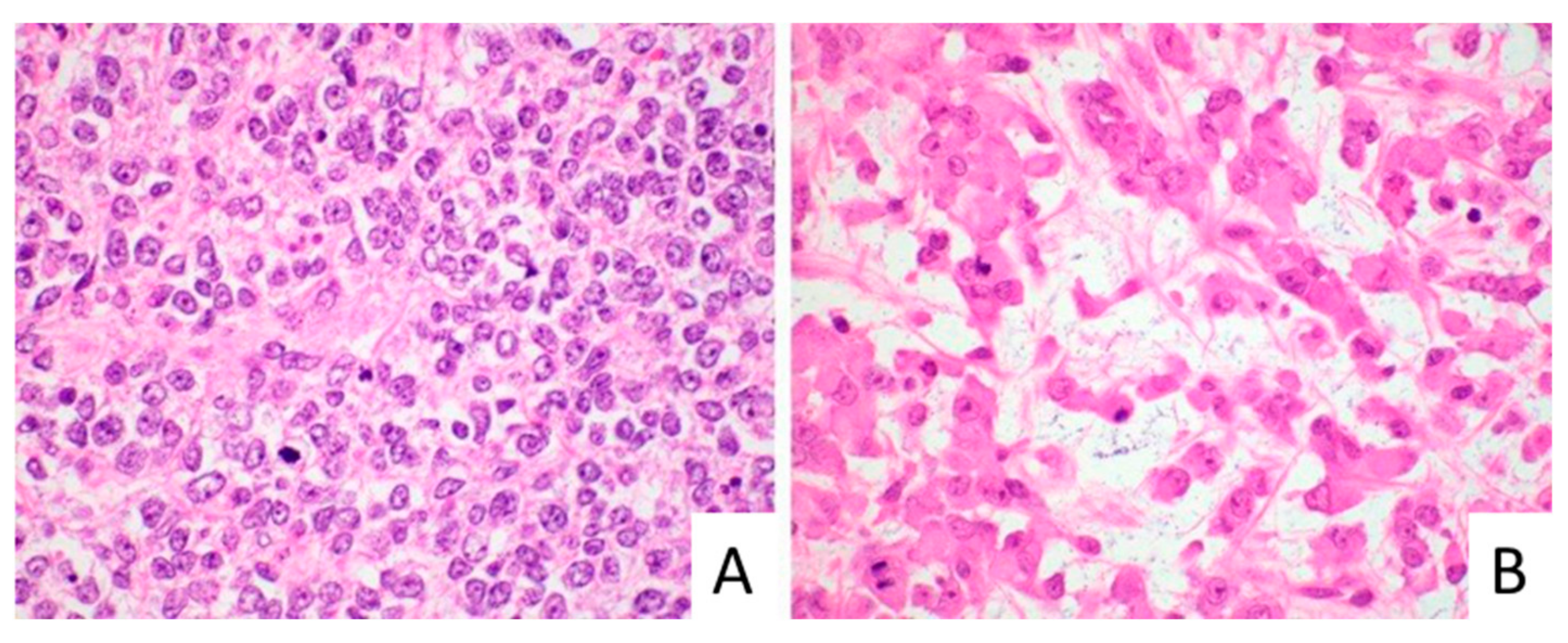
3.1. Clinical and Histopathologic Characterization of MRT
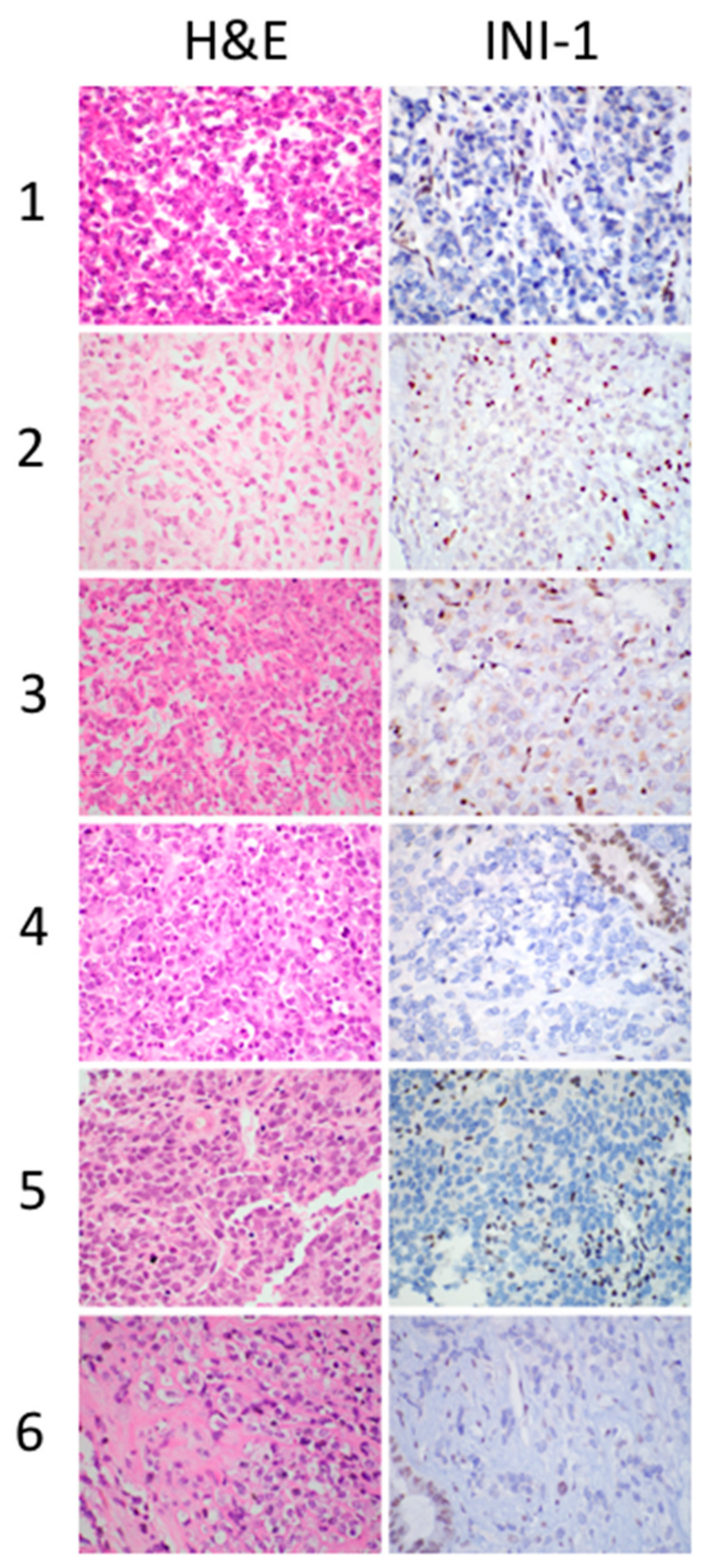
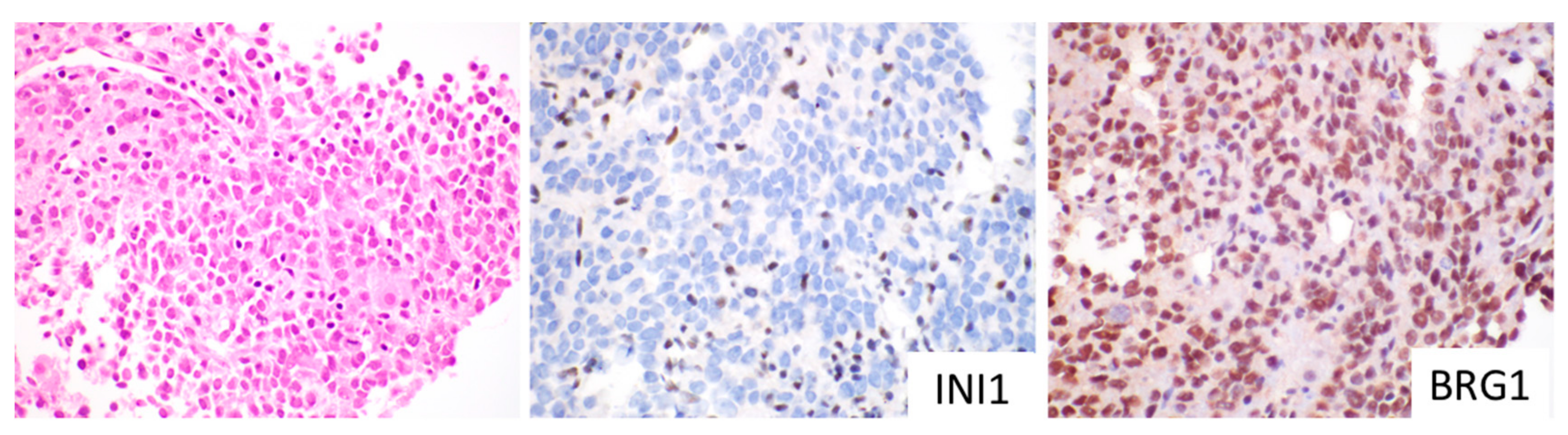
3.2. Immunohistochemical Profile of MRT
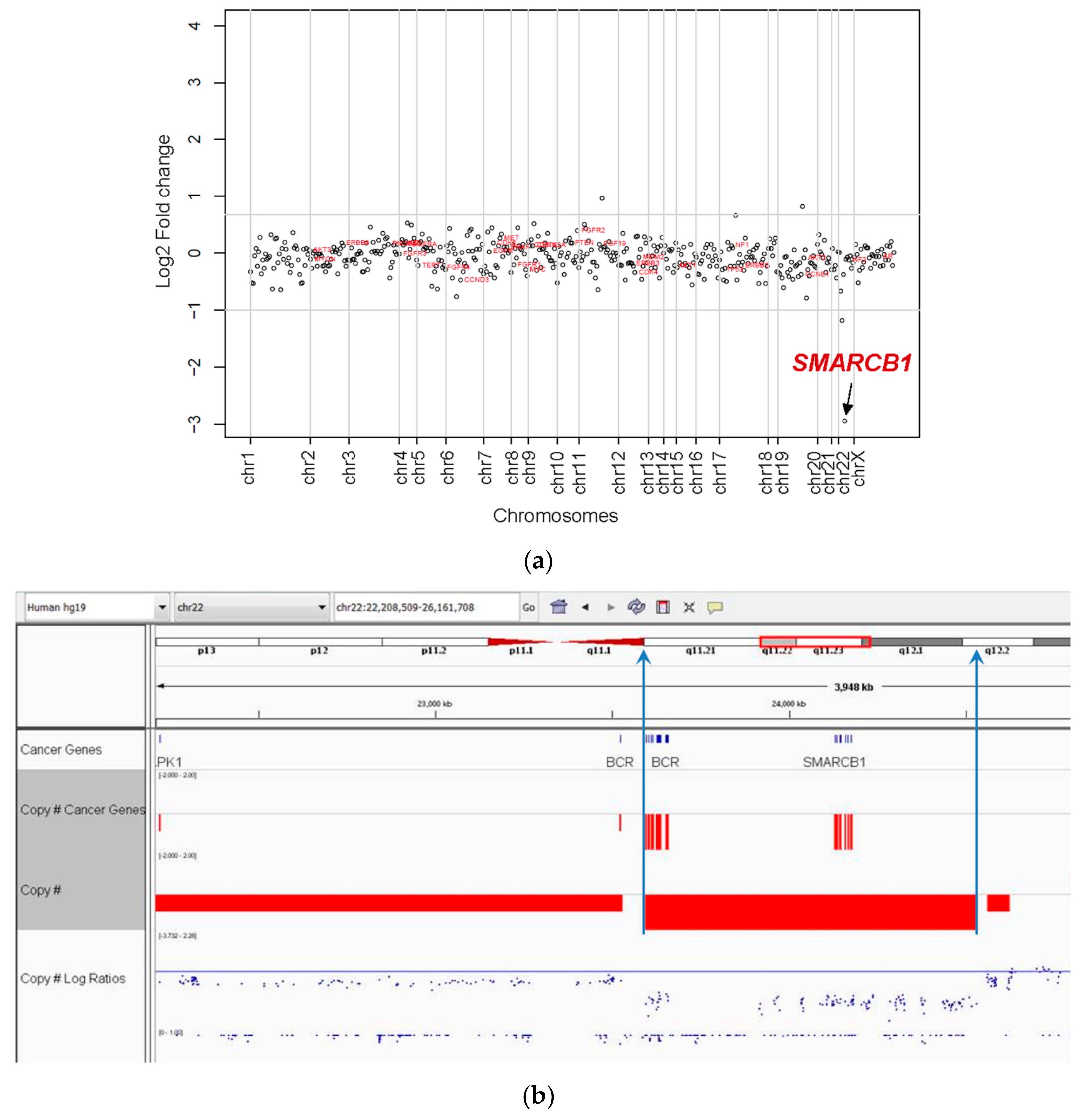
3.3. Molecular Characterization of MRT
3.4. Clinical Treatment and Outcome of MRT
4. Discussion
4.1. Establishing the Diagnosis of Hepatic MRT
4.1.1. MRT Are Tumors Typically Characterized by SMARCB1 Deletions with INI1 Loss
4.1.2. MRT and SCUD-HB Represent the Same Tumor
4.2. MRT of the Liver Most Commonly Have a Small Cell Morphology
4.3. INI1 Immunohistochemical Staining can Establish the Diagnosis of MRT in the Absence of Rhabdoid Morphology
4.4. Elimination of the Term INI Negative HB
4.5. Treatment of Liver MRT
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Biggs, P.J.; Garen, P.D.; Powers, J.M.; Garvin, A.J. Malignant rhabdoid tumor of the central nervous system. Hum. Pathol. 1987, 18, 332–337. [Google Scholar] [CrossRef]
- Rorke, L.B.; Packer, R.; Biegel, J. Central nervous system atypical teratoid/rhabdoid tumors of infancy and childhood. J. Neurooncol. 1995, 24, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Biernat, W. 2000 World Health Organization classification of tumors of the nervous system. Pol. J. Pathol. 2000, 51, 107–114. [Google Scholar] [PubMed]
- Beckwith, J.B.; Palmer, N.F. Histopathology and prognosis of Wilms tumors: Results from the First National Wilms’ Tumor Study. Cancer 1978, 41, 1937–1948. [Google Scholar] [CrossRef]
- Bonnin, J.M.; Rubinstein, L.J.; Palmer, N.F.; Beckwith, J.B. The association of embryonal tumors originating in the kidney and in the brain. A report of seven cases. Cancer 1984, 54, 2137–2146. [Google Scholar] [CrossRef]
- Gonzalez-Crussi, F.; Goldschmidt, R.A.; Hsueh, W.; Trujillo, Y.P. Infantile sarcoma with intracytoplasmic filamentous inclusions: Distinctive tumor of possible histiocytic origin. Cancer 1982, 49, 2365–2375. [Google Scholar] [CrossRef]
- Bourdeaut, F.; Freneaux, P.; Thuille, B.; Bergeron, C.; Laurence, V.; Brugieres, L.; Verite, C.; Michon, J.; Delattre, O.; Orbach, D. Extra-renal non-cerebral rhabdoid tumours. Pediatr. Blood Cancer 2008, 51, 363–368. [Google Scholar] [CrossRef]
- Gururangan, S.; Bowman, L.C.; Parham, D.M.; Wilimas, J.A.; Rao, B.; Pratt, C.B.; Douglass, E.C. Primary extracranial rhabdoid tumors. Clinicopathologic features and response to ifosfamide. Cancer 1993, 71, 2653–2659. [Google Scholar] [CrossRef]
- Trobaugh-Lotrario, A.D.; Finegold, M.J.; Feusner, J.H. Rhabdoid tumors of the liver: Rare, aggressive, and poorly responsive to standard cytotoxic chemotherapy. Pediatr. Blood Cancer 2011, 57, 423–428. [Google Scholar] [CrossRef]
- Al Nassan, A.; Sughayer, M.; Matalka, I.; Ghandour, K.; Masarweh, M.; Zimmermann, A.; Sultan, I. INI1 (BAF 47) immunohistochemistry is an essential diagnostic tool for children with hepatic tumors and low alpha fetoprotein. J. Pediatr. Hematol. Oncol. 2010, 32, e79–e81. [Google Scholar] [CrossRef]
- Geller, J.I.; Roth, J.J.; Biegel, J.A. Biology and Treatment of Rhabdoid Tumor. Crit. Rev. Oncog. 2015, 20, 199–216. [Google Scholar] [CrossRef]
- Biegel, J.A.; Zhou, J.Y.; Rorke, L.B.; Stenstrom, C.; Wainwright, L.M.; Fogelgren, B. Germ-line and acquired mutations of INI1 in atypical teratoid and rhabdoid tumors. Cancer Res. 1999, 59, 74–79. [Google Scholar] [PubMed]
- Versteege, I.; Sevenet, N.; Lange, J.; Rousseau-Merck, M.F.; Ambros, P.; Handgretinger, R.; Aurias, A.; Delattre, O. Truncating mutations of hSNF5/INI1 in aggressive paediatric cancer. Nature 1998, 394, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Biegel, J.A.; Allen, C.S.; Kawasaki, K.; Shimizu, N.; Budarf, M.L.; Bell, C.J. Narrowing the critical region for a rhabdoid tumor locus in 22q11. Genes Chromosom. Cancer 1996, 16, 94–105. [Google Scholar] [CrossRef]
- Biegel, J.A.; Burk, C.D.; Parmiter, A.H.; Emanuel, B.S. Molecular analysis of a partial deletion of 22q in a central nervous system rhabdoid tumor. Genes Chromosom. Cancer 1992, 5, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.W.; Biegel, J.A. The role of SMARCB1/INI1 in development of rhabdoid tumor. Cancer Biol. 2009, 8, 412–416. [Google Scholar] [CrossRef]
- Sredni, S.T.; Tomita, T. Rhabdoid tumor predisposition syndrome. Pediatr. Dev. Pathol. 2015, 18, 49–58. [Google Scholar] [CrossRef]
- Peterson, C.L.; Dingwall, A.; Scott, M.P. Five SWI/SNF gene products are components of a large multisubunit complex required for transcriptional enhancement. Proc. Natl. Acad. Sci. USA 1994, 91, 2905–2908. [Google Scholar] [CrossRef]
- Feinberg, A.P.; Koldobskiy, M.A.; Gondor, A. Epigenetic modulators, modifiers and mediators in cancer aetiology and progression. Nat. Rev. Genet. 2016, 17, 284–299. [Google Scholar] [CrossRef]
- Reisman, D.; Glaros, S.; Thompson, E.A. The SWI/SNF complex and cancer. Oncogene 2009, 28, 1653–1668. [Google Scholar] [CrossRef]
- Russo, P.; Biegel, J.A. SMARCB1/INI1 alterations and hepatoblastoma: Another extrarenal rhabdoid tumor revealed? Pediatr. Blood Cancer 2009, 52, 312–313. [Google Scholar] [CrossRef] [PubMed]
- Hoot, A.C.; Russo, P.; Judkins, A.R.; Perlman, E.J.; Biegel, J.A. Immunohistochemical analysis of hSNF5/INI1 distinguishes renal and extra-renal malignant rhabdoid tumors from other pediatric soft tissue tumors. Am. J. Surg. Pathol. 2004, 28, 1485–1491. [Google Scholar] [CrossRef] [PubMed]
- Wagner, L.M.; Garrett, J.K.; Ballard, E.T.; Hill, D.A.; Perry, A.; Biegel, J.A.; Collins, M.H. Malignant rhabdoid tumor mimicking hepatoblastoma: A case report and literature review. Pediatr. Dev. Pathol. 2007, 10, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Terrada, D.; Alaggio, R.; de Davila, M.T.; Czauderna, P.; Hiyama, E.; Katzenstein, H.; Leuschner, I.; Malogolowkin, M.; Meyers, R.; Ranganathan, S.; et al. Towards an international pediatric liver tumor consensus classification: Proceedings of the Los Angeles COG liver tumors symposium. Mod. Pathol. 2014, 27, 472–491. [Google Scholar] [CrossRef]
- Rudzinski, E.; Ranganathan, S.; Hicks, J.; Kim, G.; College of American Pathologists. Protocol for the Examination of Specimens from Pediatric Patients with Hepatoblastoma. Available online: http://www.cap.org/ShowProperty?nodePath=/UCMCon/Contribution%20Folders/WebContent/pdf/cp-hepatoblast-16protocol-3202.pdf (accessed on 26 August 2019).
- Trobaugh-Lotrario, A.D.; Tomlinson, G.E.; Finegold, M.J.; Gore, L.; Feusner, J.H. Small cell undifferentiated variant of hepatoblastoma: Adverse clinical and molecular features similar to rhabdoid tumors. Pediatr. Blood Cancer 2009, 52, 328–334. [Google Scholar] [CrossRef]
- Zhou, S.; Gomulia, E.; Mascarenhas, L.; Wang, L. Is INI1-retained small cell undifferentiated histology in hepatoblastoma unfavorable? Hum. Pathol. 2015, 46, 620–624. [Google Scholar] [CrossRef]
- Sireci, A.N.; Aggarwal, V.S.; Turk, A.T.; Gindin, T.; Mansukhani, M.M.; Hsiao, S.J. Clinical Genomic Profiling of a Diverse Array of Oncology Specimens at a Large Academic Cancer Center: Identification of Targetable Variants and Experience with Reimbursement. J. Mol. Diagn. 2017, 19, 277–287. [Google Scholar] [CrossRef]
- Oberg, J.A.; Glade Bender, J.L.; Sulis, M.L.; Pendrick, D.; Sireci, A.N.; Hsiao, S.J.; Turk, A.T.; Dela Cruz, F.S.; Hibshoosh, H.; Remotti, H.; et al. Implementation of next generation sequencing into pediatric hematology-oncology practice: Moving beyond actionable alterations. Genome Med. 2016, 8, 133. [Google Scholar] [CrossRef]
- Magi, A.; Tattini, L.; Cifola, I.; D’Aurizio, R.; Benelli, M.; Mangano, E.; Battaglia, C.; Bonora, E.; Kurg, A.; Seri, M.; et al. EXCAVATOR:detecting copy number variants from whole-exome sequencing data. Genome Biol. 2013, 14, 120. [Google Scholar] [CrossRef]
- Fazlollahi, L.; Hsiao, S.J.; Mansukhani, M.M.; Glade Bender, J.L.; Kung, A.L.; Yamashiro, D.J.; Remotti, H.E. INI1 negative hepatoblastoma, a vanishing entity representing malignant rhabdoid tumor. Hum. Pathol. Case Rep. 2018, 12, 42–47. [Google Scholar] [CrossRef]
- Biegel, J.A.; Kalpana, G.; Knudsen, E.S.; Packer, R.J.; Roberts, C.W.; Thiele, C.J.; Weissman, B.; Smith, M. The role of INI1 and the SWI/SNF complex in the development of rhabdoid tumors: Meeting summary from the workshop on childhood atypical teratoid/rhabdoid tumors. Cancer Res. 2002, 62, 323–328. [Google Scholar] [PubMed]
- Foulkes, W.D.; Clarke, B.A.; Hasselblatt, M.; Majewski, J.; Albrecht, S.; McCluggage, W.G. No small surprise—Small cell carcinoma of the ovary, hypercalcaemic type, is a malignant rhabdoid tumour. J. Pathol. 2014, 233, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Fruhwald, M.C.; Hasselblatt, M.; Wirth, S.; Kohler, G.; Schneppenheim, R.; Subero, J.I.; Siebert, R.; Kordes, U.; Jurgens, H.; Vormoor, J. Non-linkage of familial rhabdoid tumors to SMARCB1 implies a second locus for the rhabdoid tumor predisposition syndrome. Pediatr. Blood Cancer 2006, 47, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Schneppenheim, R.; Fruhwald, M.C.; Gesk, S.; Hasselblatt, M.; Jeibmann, A.; Kordes, U.; Kreuz, M.; Leuschner, I.; Martin Subero, J.I.; Obser, T.; et al. Germline nonsense mutation and somatic inactivation of SMARCA4/BRG1 in a family with rhabdoid tumor predisposition syndrome. Am. J. Hum. Genet. 2010, 86, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Witkowski, L.; Lalonde, E.; Zhang, J.; Albrecht, S.; Hamel, N.; Cavallone, L.; May, S.T.; Nicholson, J.C.; Coleman, N.; Murray, M.J.; et al. Familial rhabdoid tumour ‘avant la lettre’—From pathology review to exome sequencing and back again. J. Pathol. 2013, 231, 35–43. [Google Scholar] [CrossRef]
- Burger, P.C.; Yu, I.T.; Tihan, T.; Friedman, H.S.; Strother, D.R.; Kepner, J.L.; Duffner, P.K.; Kun, L.E.; Perlman, E.J. Atypical teratoid/rhabdoid tumor of the central nervous system: A highly malignant tumor of infancy and childhood frequently mistaken for medulloblastoma: A Pediatric Oncology Group study. Am. J. Surg. Pathol. 1998, 22, 1083–1092. [Google Scholar] [CrossRef]
- Vokuhl, C.; Oyen, F.; Haberle, B.; von Schweinitz, D.; Schneppenheim, R.; Leuschner, I. Small Cell Undifferentiated Hepatoblastomas (SCUD): All Malignant Rhabdoid Tumors? Genes Chromosom. Cancer 2016, 55, 925–931. [Google Scholar] [CrossRef]
- Dufour, C.; Beaugrand, A.; Le Deley, M.C.; Bourdeaut, F.; Andre, N.; Leblond, P.; Bertozzi, A.I.; Frappaz, D.; Rialland, X.; Fouyssac, F.; et al. Clinicopathologic prognostic factors in childhood atypical teratoid and rhabdoid tumor of the central nervous system: A multicenter study. Cancer 2012, 118, 3812–3821. [Google Scholar] [CrossRef]
- Saxena, R.; Quaglia, A. WHO Classification of Tumours Editorial Board. Hepatoblastoma. In Digestive System Tumours, 5th ed.; International Agency for Research on Cancer: Lyon, France, 2019; Volume 1. [Google Scholar]
- Cornet, M.; De Lambert, G.; Pariente, D.; Planchon, J.M.; Guettier, C.; Martelli, H.; Guerin, F.; Branchereau, S. Rhabdoid tumor of the liver: Report of 6 pediatric cases treated at a single institute. J. Pediatr. Surg. 2018, 53, 567–571. [Google Scholar] [CrossRef]
- Mosse, Y.P.; Fox, E.; Teachey, D.T.; Reid, J.M.; Sagfren, S.L.; Carol, H.; Lock, R.B.; Houghton, P.J.; Smith, M.A.; Hall, D.C.; et al. A Phase 2 Study of Alisertib in Children with Recurrent/Refractory Solid Tumors or Leukemia: Children’s Oncology Group Phase 1 and Pilot Consortium ADVL0921). Clin. Cancer Res. 2019, 25, 3229–3238. [Google Scholar] [CrossRef]
- Brennan, B.; De Salvo, G.L.; Orbach, D.; De Paoli, A.; Kelsey, A.; Mudry, P.; Francotte, N.; Van Noesel, M.; Bisogno, G.; Casanova, M.; et al. Outcome of extracranial malignant rhabdoid tumours in children registered in the European Paediatric Soft Tissue Sarcoma Study Group Non-Rhabdomyosarcoma Soft Tissue Sarcoma 2005 Study-EpSSG NRSTS 2005. Eur. J. Cancer 2016, 60, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Puri, D.R.; Meyers, P.A.; Kraus, D.H.; Laquaglia, M.P.; Wexler, L.H.; Wolden, S.L. Radiotherapy in the multimodal treatment of extrarenal extracranial malignant rhabdoid tumors. Pediatr. Blood Cancer 2008, 50, 167–169. [Google Scholar] [CrossRef] [PubMed]
- Muscal, J.A.; Thompson, P.A.; Horton, T.M.; Ingle, A.M.; Ahern, C.H.; McGovern, R.M.; Reid, J.M.; Ames, M.M.; Espinoza-Delgado, I.; Weigel, B.J.; et al. A phase I trial of vorinostat and bortezomib in children with refractory or recurrent solid tumors: A Children’s Oncology Group phase I consortium study (ADVL0916). Pediatr. Blood Cancer 2013, 60, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Knutson, S.K.; Warholic, N.M.; Wigle, T.J.; Klaus, C.R.; Allain, C.J.; Raimondi, A.; Porter Scott, M.; Chesworth, R.; Moyer, M.P.; Copeland, R.A.; et al. Durable tumor regression in genetically altered malignant rhabdoid tumors by inhibition of methyltransferase EZH2. Proc. Natl. Acad. Sci. USA 2013, 110, 7922–7927. [Google Scholar] [CrossRef]
| Case | Age at Diagnosis (Months) | Gender (M/F) | AFP Level (ng/mL) | Specimen Type | Morphology on Biopsy | Initial Diagnosis | GPC-3 | Hepatocellular Markers | INI1 | CCCP | Subsequent Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 9 | M | 14.2 | B and R | Small cell | SCUD-HB | − | − | Loss | SMARCB1 del | MRT |
| 2 | 11 | F | 90 | B | Small cell | SCUD-HB | + | − | Loss | SMARCB1 del | MRT |
| 3 | 3 | F | 33.8 | B and R | Rhabdoid | MRT | − | − | Loss | SMARCB1 del | MRT |
| 4 | 12 | F | 69.8 | B and R | Small cell * | SCUD-HB | + | − | Loss | SMARCB1 del | MRT |
| 5 | 10 | M | 13.6 | B | Small cell | SCUD-HB | − | − | Loss | SMARCB1 del | MRT |
| 6 | 24 | M | 3.4 | B and R | Small cell | MRT | − | − | Loss | SMARCB1 del | MRT |
| Case | Tumor Stage (Evans) | PRETEXT Stage | Preoperative Chemotherapy | Response RECIST | Resection | Site of Metastasis | Radiotherapy | Postoperative/Retrieval Chemotherapy | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | I | PRETEXT 2 | none | No | R0 | Yes Records not available | vincristine, doxorubicin, cyclophosphamide, cisplatin, ifosfamide, etoposide, irinotecan, temozolomide | DOD | |
| 2 | IV | PRETEXT 3 | cisplatin, doxorubicin | No | None | Lung, Brain | No | irinotecan, vincristine | DOD |
| 3 | IV | PRETEXT 3M | vincristine, cisplatin, doxorubicin | Yes CR-lung PR- liver | R0 | Lung | Yes 1050cGy to whole lung 1050cGy to abdomen | carboplatin, cyclophosphamide, etoposide | Alive at 8 years after diagnosis |
| 4 | IV | PRETEXT 2 | vincristine, irinotecan, cisplatin, doxorubicin, 5FU | Yes PR- liver PR-lung | R0 | Lung | Yes 1050cGy to whole lung 1200cGy to abdomen 14.5Gy to cavity intra-op after recurrence | ifosfamide, carboplatin, vincristine, cyclophosphamide, doxorubicin HD chemotherapy with autologous SCT Second surgical resection | DOD |
| 5 | III | PRETEXT 2 | cisplatin, doxorubicin | No | None | Lung | No | pazopanib | DOD |
| 6 | III | PRETEXT 3 | vincristine, doxorubicin, cyclophosphamide | Yes PR-liver | R1 margin | Yes Proton beam 3000cGy to abdomen | HD chemotherapy with autologous SCT | Alive at 1.5 years after diagnosis |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fazlollahi, L.; Hsiao, S.J.; Kochhar, M.; Mansukhani, M.M.; Yamashiro, D.J.; Remotti, H.E. Malignant Rhabdoid Tumor, an Aggressive Tumor Often Misclassified as Small Cell Variant of Hepatoblastoma. Cancers 2019, 11, 1992. https://doi.org/10.3390/cancers11121992
Fazlollahi L, Hsiao SJ, Kochhar M, Mansukhani MM, Yamashiro DJ, Remotti HE. Malignant Rhabdoid Tumor, an Aggressive Tumor Often Misclassified as Small Cell Variant of Hepatoblastoma. Cancers. 2019; 11(12):1992. https://doi.org/10.3390/cancers11121992
Chicago/Turabian StyleFazlollahi, Ladan, Susan J. Hsiao, Manpreet Kochhar, Mahesh M. Mansukhani, Darrell J. Yamashiro, and Helen E. Remotti. 2019. "Malignant Rhabdoid Tumor, an Aggressive Tumor Often Misclassified as Small Cell Variant of Hepatoblastoma" Cancers 11, no. 12: 1992. https://doi.org/10.3390/cancers11121992
APA StyleFazlollahi, L., Hsiao, S. J., Kochhar, M., Mansukhani, M. M., Yamashiro, D. J., & Remotti, H. E. (2019). Malignant Rhabdoid Tumor, an Aggressive Tumor Often Misclassified as Small Cell Variant of Hepatoblastoma. Cancers, 11(12), 1992. https://doi.org/10.3390/cancers11121992




