Mangiferin-Loaded Polymeric Nanoparticles: Optical Characterization, Effect of Anti-topoisomerase I, and Cytotoxicity
Abstract
1. Introduction
2. Results and Discussion
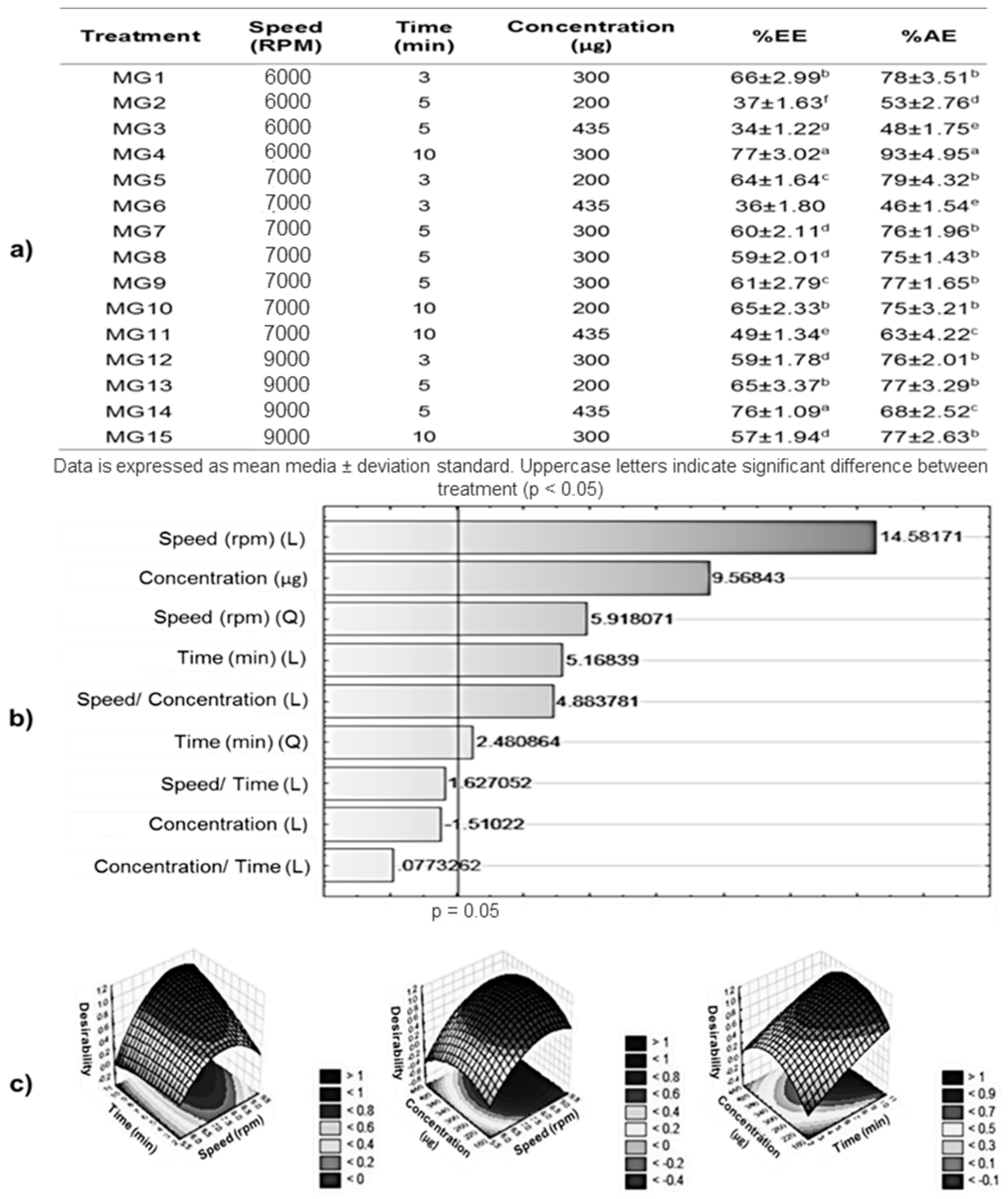
2.1. Encapsulation Efficiency (EE%) and Entrapment Efficiency (AE%)
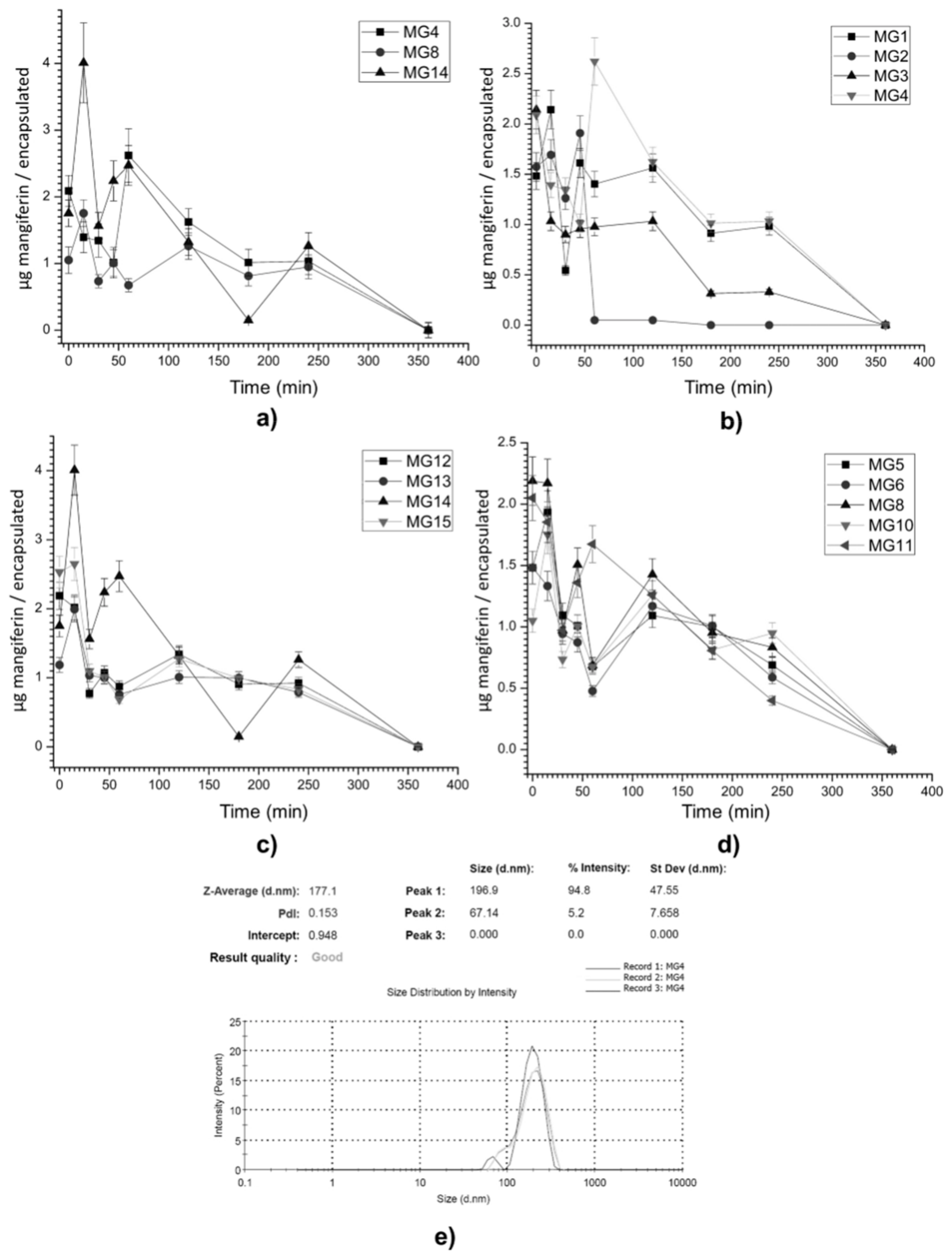
2.2. Mangiferin Release Profile
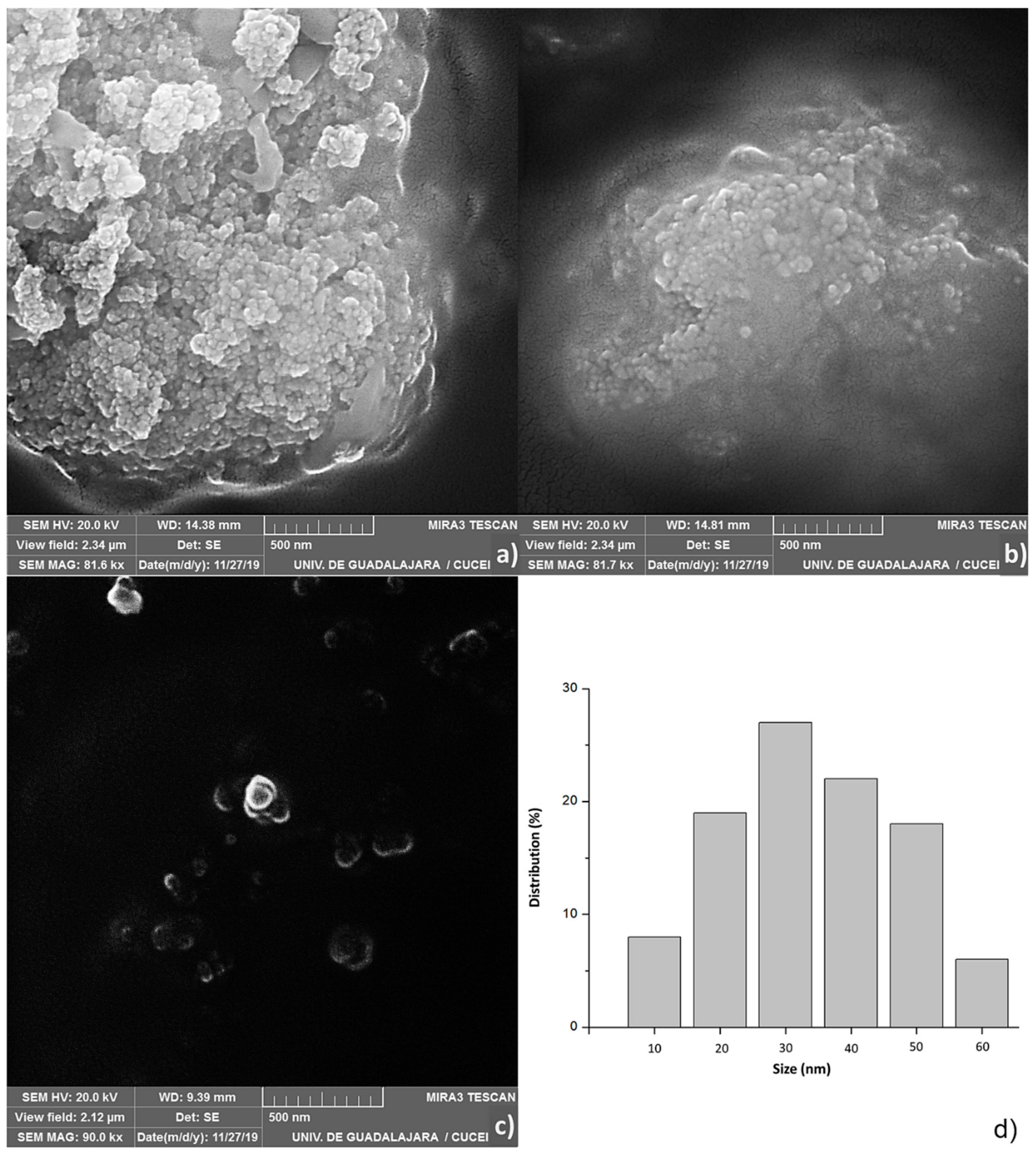
2.3. Scanning Electron Microscopy (SEM)
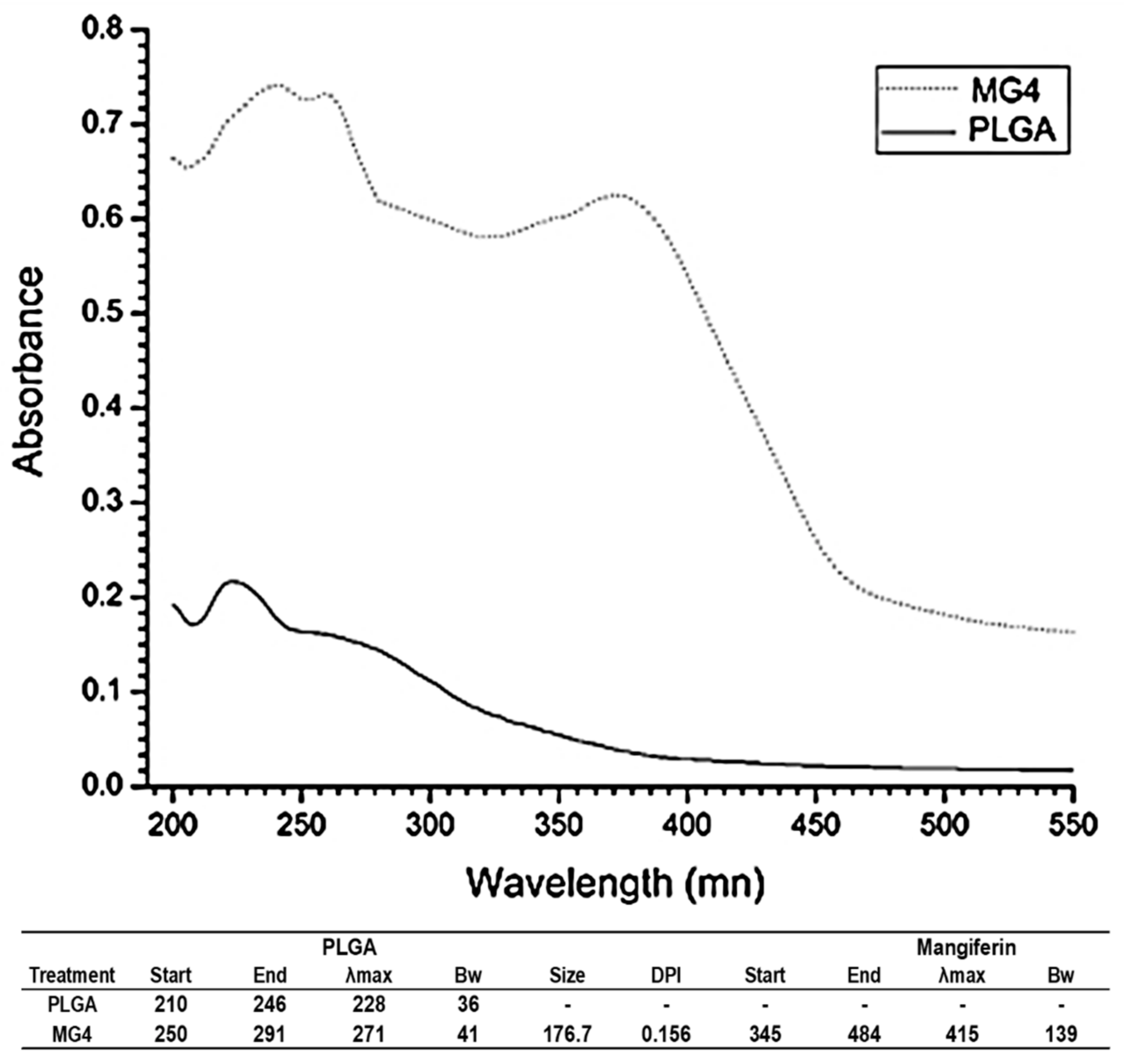
2.4. UV-Visible Spectroscopy
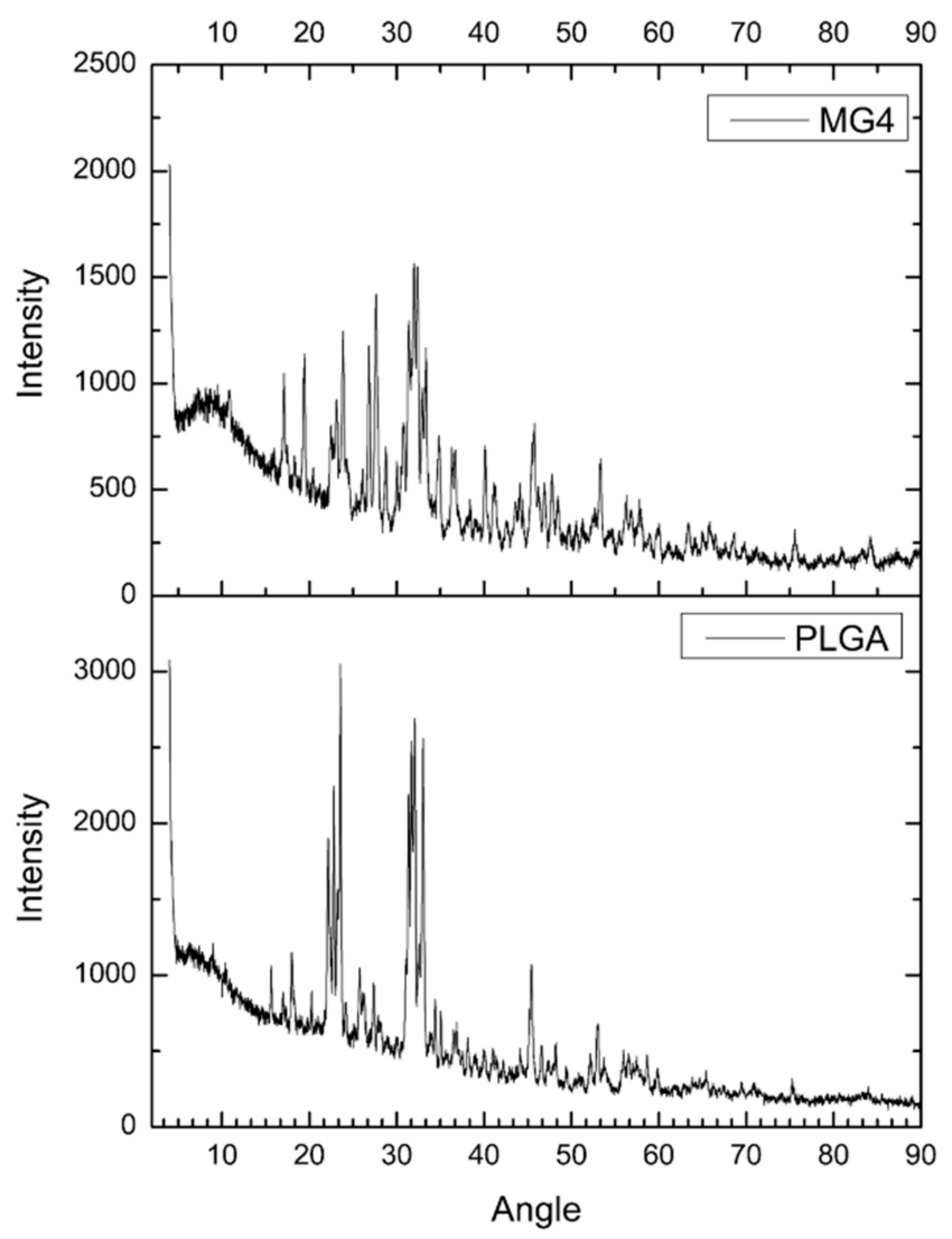
2.5. Powder X-ray Diffraction (XRD)
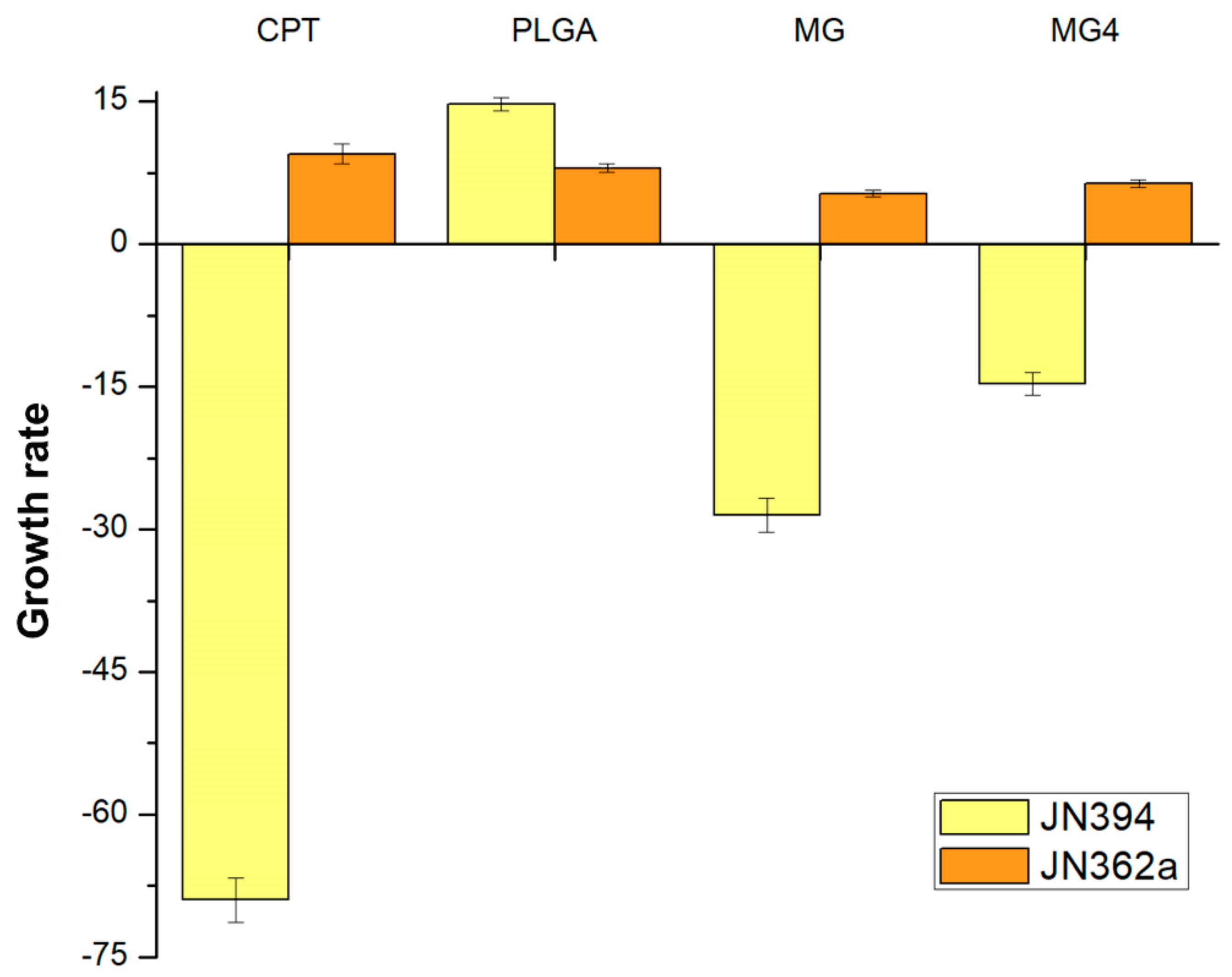
2.6. Anti-Topoisomerase Activity
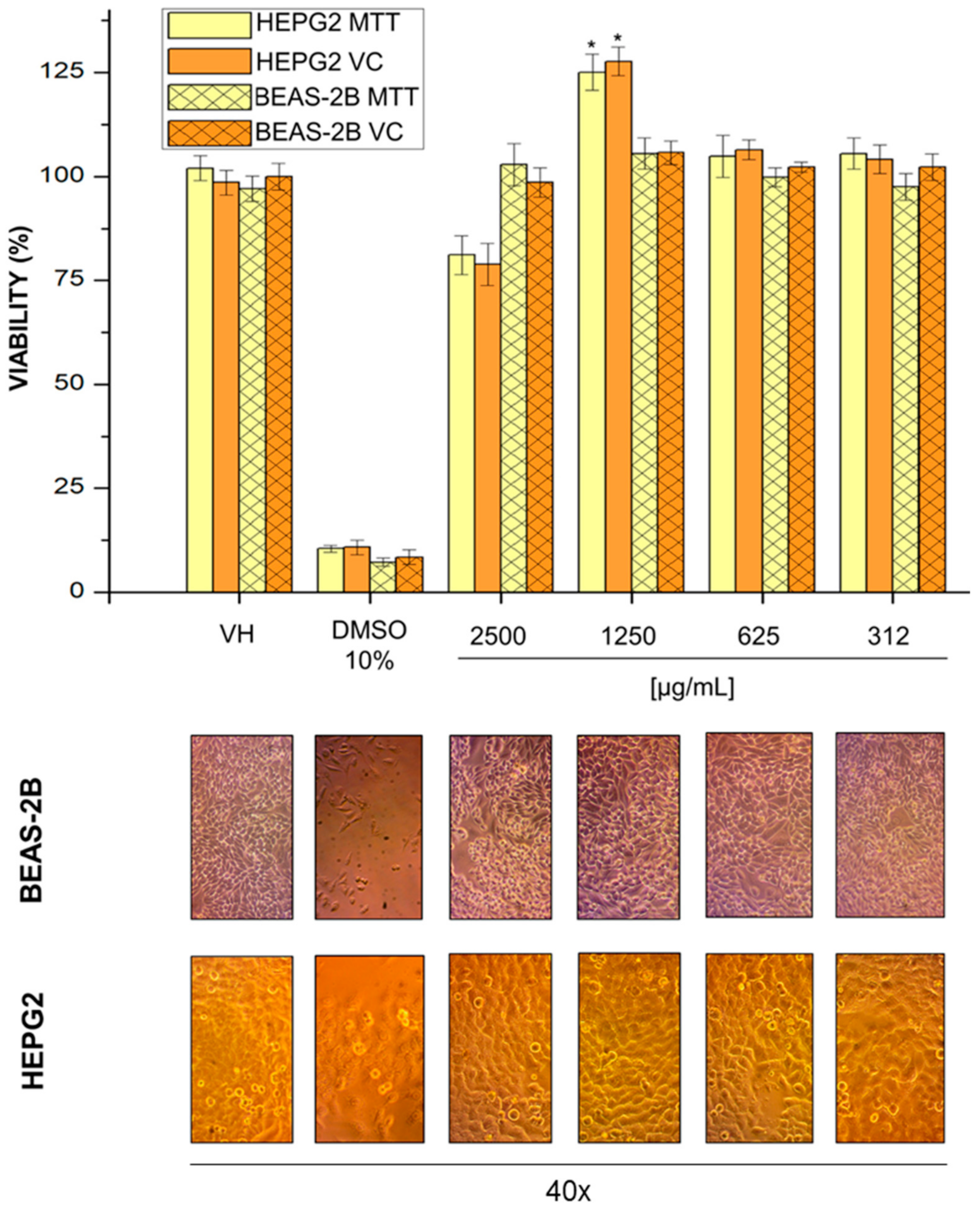
2.7. Cell Viability
3. Materials and Methods
3.1. Reactives
3.2. Preparation of Nanoparticles (NPs)
3.3. Experimental Design
3.4. Evaluation of Mangiferin Encapsulation Efficiency (EE%) and Entrapment Efficiency (AE%)
Optimization of Data Using Response Surface Methodology (RSM)
3.5. Mangiferin Release Profile in NPs
3.6. Optical Characterization
3.6.1. Size Distribution of Mangiferin NPs
3.6.2. Evaluation Morphology by Scanning Electron Microscopy (SEM)
3.6.3. UV-Visible Spectroscopy
3.6.4. Surface Composition of the Np´s by X-ray Diffraction (XRD)
3.7. Biological Material
3.8. Yeast Anti-Topoisomerase Assay
3.9. Cell Line Culture
3.10. Cell Viability Assay
3.10.1. Staining with Violet Crystal
3.10.2. MTT Tetrazolium Assay
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Vyas, A.; Syeda, K.; Ahmad, A.; Padhye, S.; Sarkar, F.H. Perspective on medical properties of mangiferin. Mini Rev. Med. Chem. 2012, 12, 412–425. [Google Scholar] [CrossRef] [PubMed]
- Nunez Selles, A.J.; Velez Castro, H.T.; Aguero-Aguero, J.; Gonzalez-Gonzalez, J.; Naddeo, F.; De Simone, F.; Rastrelli, L. Isolation and quantitative analysis of phenolic antioxidants, free sugars, and polyols from mango (Mangifera indica L.) stem bark aqueous decoction used in Cuba as a nutritional supplement. J. Agric. Food Chem. 2002, 50, 762–766. [Google Scholar] [CrossRef] [PubMed]
- Nunez Selles, A.J.; Daglia, M.; Rastrelli, L. The potential role of mangiferin in cancer treatment through its immunomodulatory, anti-angiogenic, apoptopic, and gene regulatory effects. Biofactors 2016, 42, 475–491. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Wang, K.; Tang, Y.; Sun, Z.; Jian, L.; Li, Z.; Wu, B.; Huang, C. Structure elucidation of in vivo and in vitro metabolites of mangiferin. J. Pharm. Biomed. Anal. 2011, 55, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- Leiro, J.; Arranz, J.A.; Yanez, M.; Ubeira, F.M.; Sanmartin, M.L.; Orallo, F. Expression profiles of genes involved in the mouse nuclear factor-kappa B signal transduction pathway are modulated by mangiferin. Int. Immunopharmacol. 2004, 4, 763–778. [Google Scholar] [CrossRef]
- Takeda, T.; Tsubaki, M.; Kino, T.; Yamagishi, M.; Iida, M.; Itoh, T.; Imano, M.; Tanabe, G.; Muraoka, O.; Satou, T.; et al. Mangiferin induces apoptosis in multiple myeloma cell lines by suppressing the activation of nuclear factor kappa B-inducing kinase. Chem. Biol. Interact. 2016, 251, 26–33. [Google Scholar] [CrossRef]
- Takeda, T.; Tsubaki, M.; Sakamoto, K.; Ichimura, E.; Enomoto, A.; Suzuki, Y.; Itoh, T.; Imano, M.; Tanabe, G.; Muraoka, O.; et al. Mangiferin, a novel nuclear factor kappa B-inducing kinase inhibitor, suppresses metastasis and tumor growth in a mouse metastatic melanoma model. Toxicol. Appl. Pharmacol. 2016, 306, 105–112. [Google Scholar] [CrossRef]
- Garrido, G.; Delgado, R.; Lemus, Y.; Rodriguez, J.; Garcia, D.; Nunez-Selles, A.J. Protection against septic shock and suppression of tumor necrosis factor alpha and nitric oxide production on macrophages and microglia by a standard aqueous extract of Mangifera indica L. (VIMANG). Role of mangiferin isolated from the extract. Pharmacol. Res. 2004, 50, 165–172. [Google Scholar] [CrossRef]
- Bhatia, H.S.; Candelario-Jalil, E.; de Oliveira, A.C.; Olajide, O.A.; Martinez-Sanchez, G.; Fiebich, B.L. Mangiferin inhibits cyclooxygenase-2 expression and prostaglandin E2 production in activated rat microglial cells. Arch. Biochem. Biophys. 2008, 477, 253–258. [Google Scholar] [CrossRef]
- Ariyarathna, I.R.; Karunaratne, D.N. Microencapsulation stabilizes curcumin for efficient delivery in food applications. Food Packag. Shelf Life 2016, 10, 79–86. [Google Scholar] [CrossRef]
- Rodríguez, J.; Martín, M.J.; Ruiz, M.A.; Clares, B. Current encapsulation strategies for bioactive oils: From alimentary to pharmaceutical perspectives. Food Res. Int. 2016, 83, 41–59. [Google Scholar] [CrossRef]
- Esfanjani, A.F.; Jafari, S.M. Biopolymer nano-particles and natural nanocarriers for nano-encapsulation of phenolic compounds. Colloids Surf. B Biointerfaces 2016, 146, 532–543. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Yan, H.; Puligundla, P.; Gao, X.; Zhou, Y.; Wan, X. Applications of chitosan nanoparticles to enhance absorption and bioavailability of tea polyphenols: A review. Food Hydrocolloids 2017, 69, 286–292. [Google Scholar] [CrossRef]
- Anwer, M.K.; Mohammad, M.; Ezzeldin, E.; Fatima, F.; Alalaiwe, A.; Iqbal, M. Preparation of sustained release apremilast-loaded PLGA nanoparticles: In vitro characterization and in vivo pharmacokinetic study in rats. Int. J. Nanomed. 2019, 14, 1587. [Google Scholar] [CrossRef] [PubMed]
- Benitez, S.; Benoit, J.P.; Puisioux, F.; Thies, C. Characterization of drug loaded poly (d,l-lactide) microespheres. J. Pharmacol. Sci. 1994, 732, 1721–1728. [Google Scholar]
- Fernandez, D.M.; Gómez, M.; Núñez, L.; Ramos, D.; Moya, A.; Chang, A. Características físico-químicas de las microesferas obtenidas con diferentes polímeros y la liberación del principio activo. Rev. Cuba. Farm. 2005, 37, 5–9. [Google Scholar]
- Busatto, C.A.; Helbling, I.; Casis, N.; Luna, N.; Estenoz, D.A. Microesferas biodegradables de PLGA para la liberación controlada de progesterona. In Proceedings of the 13st Congresso da Sociedade Latino Americana de Biomateriais, Orgãos Artificiais e Engenharia de Tecidos—SLABO, Foz do Iguaçu, Brazil, 24–27 August 2016. [Google Scholar]
- Gracia, E.; García, M.T.; Rodríguez, J.F.; de Lucas, A.; Gracia, I. Improvement of PLGA loading and release of curcumin by supercritical technology. J. Supercrit. Fluids 2018, 141, 60–67. [Google Scholar] [CrossRef]
- Varga, N.; Hornok, V.; Janovák, L.; Dékány, I.; Csapó, E. The effect of synthesis conditions and tunable hydrophilicity on the drug encapsulation capability of PLA and PLGA nanoparticles. Colloids Surf. B Biointerfaces 2019, 176, 212–218. [Google Scholar] [CrossRef]
- Mahapatro, A.; Singh, D.K. Biodegradable nanoparticles are excellent vehicle for site directed in-vivo delivery of drugs and vaccines. J. Nanobiotechnol. 2011, 9, 2–11. [Google Scholar] [CrossRef]
- Souza, J.R.; Feitosa, J.P.; De Carvalho, J.I.; Trevisan, M.T.; De Paula, H.C.; Nágila, M.P. Chitosan-coated pectin beads: Characterization and in vitro release of mangiferin. Food Hydrocoll. 2009, 23, 2278–2286. [Google Scholar] [CrossRef]
- Owen, R.W. Spray-drying encapsulation of mangiferin using natural polymers. Food Hydrocoll. 2013, 33, 10–18. [Google Scholar]
- Dhand, V.; Soumya, L.; Bharadwaj, S.; Chakra, S.; Bhatt, D.; Sreedhar, B. Green synthesis of silver nanoparticles using Coffea arabica seed extract and its antibacterial activity. Mater. Sci. Eng. C 2016, 58, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Venugopal, N.; Mitra, A. Influence of temperature dependent morphology on localized surface plasmon resonance in ultra-thin silver island films. Appl. Surf. Sci. 2013, 85, 357–372. [Google Scholar] [CrossRef]
- Pool, H.; Quintanar, D.; Figueroa, J.D.; Mano, C.; Bechara, H.; Godínez, L.A.; Mendoza, S. Antioxidant effects of quercetin and catechin encapsulated into PLGA nanoparticles. J. Nanomater. 2012, 2012, 1–12. [Google Scholar] [CrossRef]
- Patra, N.; Dehury, N.; Pal, A.; Behera, A.; Patra, S. Preparation and mechanistic aspect of natural xanthone functionalized gold nanoparticle. Mater. Sci. Eng. C 2018, 90, 439–445. [Google Scholar] [CrossRef]
- Engelbrekt, C.; Sørensen, K.H.; Zhang, J.; Welinder, A.C.; Jensen, P.S.; Ulstrup, J. Green synthesis of gold nanoparticles with starch–glucose and application in bioelectrochemistry. J. Mater. Chem. 2009, 42, 7839–7847. [Google Scholar] [CrossRef]
- Pereira, M.C.; Oliveira, D.A.; Hill, L.E.; Zambiazi, R.C.; Borges, C.D.; Vizzotto, M.; Mertens-Talcott, S.; Talcott, S.; Gomes, C.L. Effect of nanoencapsulation using PLGA on antioxidant and antimicrobial activities of guabiroba fruit phenolic extract. Food Chem. 2018, 240, 396–404. [Google Scholar] [CrossRef]
- Kumawat, M.K.; Thakur, M.; Gurung, R.B.; Srivastava, R. Graphene Quantum Dots from Mangifera indica: Application in Near-Infrared Bioimaging and Intracellular Nanothermometry. ACS Sustain. Chem. Eng. 2017, 5, 1382–1391. [Google Scholar] [CrossRef]
- Kim, K.; Luu, Y.K.; Chang, C.; Fang, D.; Hsiao, B.S.; Chu, B.; Hadjiargyrou, M. Incorporation and controlled release of a hydrophilicantibiotic using poly(lactide-co-glycolide)-based electrospun nanofibrous scaffolds. J. Controll. Release 2004, 98, 47–56. [Google Scholar] [CrossRef]
- Chaitanya, K. Molecular structure, vibrational spectroscopic (FT-IR, FT-Raman), UV–vis spectra, first order hyperpolarizability, NBO analysis, HOMO and LUMO analysis, thermodynamic properties of benzophenone 2,4-dicarboxylic acid by ab initio HF and density functional method. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2012, 86, 159–173. [Google Scholar]
- Thomas, M. Ultraviolet and Visible Spectroscopy, 2nd ed.; John Wiley & Sons: New York, NY, USA, 1996; p. 172. [Google Scholar]
- Pearson, R.G. Absolute electronegativity and hardness correlated with molecular orbital theory. Proc. Natl. Acad. Sci. USA 1986, 83, 8440–8441. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhao, Y.; Chen, Y.; Liao, X.; Gao, C.; Xiao, D.; Qin, Q.; Yi, D.; Yang, B. Host–guest inclusion system of mangiferin with β-cyclodextrin and its derivatives. Mater. Sci. Eng. C 2013, 33, 2386–2391. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Liu, Z.; Zhang, C.; Zhang, B. Nanostructured Lipid Carriers As Novel Ophthalmic Delivery System for Mangiferin: Improving In Vivo Ocular Bioavailability. J. Pharm. Sci. 2012, 101, 3833–3844. [Google Scholar] [CrossRef] [PubMed]
- Sangeetha, G.; Rajeshwari, S.; Venckatesh, R. Green synthesis of zinc oxide nanoparticles by aloe barbadensis miller leaf extract: Structure and optical properties. Mater. Res. Bull. 2011, 46, 2560–2566. [Google Scholar] [CrossRef]
- Pona, A.; Cline, A.; Kolli, S.S.; Taylor, S.L.; Feldman, S.R. Review of future insights of Dragon’s Blood in dermatology. Dermatol. Ther. 2019, 32, 1–20. [Google Scholar] [CrossRef]
- Arunkumar, J.; Rajarajan, S. A Study on the in vitro Cytotoxicity and Anti- HSV-2 Activity of Lyophilized Extracts of Terminalia Catappa Lin., Mangifera Indica Lin.and Phytochemical Compound Mangiferin. Int. J. Med. Pharm. Virol. 2015, 2, 22–26. [Google Scholar]
- Nitiss, J.; Wang, J.C. DNA topoisomerase-targeting antitumor drugs can be studied in yeast. Proc. Natl. Acad. Sci. USA 1988, 85, 7501–7505. [Google Scholar] [CrossRef]
- Ramírez-Mares, M.V.; Sánchez-Burgos, J.A.; Hernández-Carlos, B. Antioxidant, antimicrobial and antitopoisomerase screening of the stem bark extracts of Ardisia compressa. Pak. J. Nutr. 2010, 9, 307–313. [Google Scholar]
- Qin, J.L.; Deng, S.P.; Zhang, Y.L.; Yuan, T.; Li, Y.B.; Han, H.H.; Chen, Z.F. Water soluble copper (II) and zinc (II) complexes of mangiferin: Synthesis, antitumour activity and DNA binding studies. J. Chem. Res. 2016, 40, 659–663. [Google Scholar] [CrossRef]
- Zhang, B.P.; Zhao, J.; Li, S.S.; Yang, L.J.; Zeng, L.L.; Chen, Y.; Fang, J. Mangiferin activates Nrf2-antioxidant response element signaling without reducing the sensitivity to etoposide of human myeloid leukemia cells in vitro. Acta Pharmacol. Sin. 2014, 35, 257. [Google Scholar] [CrossRef]
- Villamizar, G.; Parra-Monroy, M.L. Uso de Nanopartículas de plata en el control de microorganismos patógenos presentes en alimentos. Nano Cienc. Tecnol. 2015, 13, 54–59. [Google Scholar]
- Broderick, L.; Yost, S.; Li, D.; McGeough, M.D.; Booshehri, L.M.; Guaderrama, M.; Hakonarson, H. Mutations in topoisomerase IIβ result in a B cell immunodeficiency. Nat. Commun. 2019, 10, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Souza, L.G.; Silva, E.J.; Martins, A.L.L.; Mota, M.F.; Braga, R.C.; Lima, E.M.; Marreto, R.N. Development of topotecan loaded lipid nanoparticles for chemical stabilization and prolonged release. Eur. J. Pharm. Biopharm. 2011, 79, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Bahadar, H.; Maqbool, F.; Niaz, K.; Abdollahi, M. Toxicity of Nanoparticles and an Overview of Current Experimental Models. Iran. Biomed. J. 2016, 20, 1–11. [Google Scholar]
- Chatterjee, N.; Yang, J.; Kim, H.M.; Jo, E.; Kim, P.J.; Choi, K.; Choi, J. Potential toxicity of differential functionalized multiwalled carbon nanotubes (MWCNT) in human cell line (BEAS2B) and Caenorhabditis elegans. J. Toxicol. Environ. Health Part A 2014, 77, 1399–1408. [Google Scholar] [CrossRef]
- Chatterjee, N.; Yang, J.S.; Park, K.; Oh, S.M.; Park, J.; Choi, J. Screening of toxic potential of graphene family nanomaterials using in vitro and alternative in vivo toxicity testing systems. Environ. Health Toxicol. 2015, 15, 1–7. [Google Scholar] [CrossRef]
- Wang, C.; Jian-Dong, J.; Wei, W.; Wei-Jia, K. The Compound of Mangiferin-Berberine Salt Has Potent Activities in Modulating Lipid and Glucose Metabolisms in HepG2 Cell. BioMed Res. Int. 2016, 2016, 1–15. [Google Scholar] [CrossRef]
- Ahmed, A.; Rabou, A.; Hanaa, H. CS-PEG decorated PLGA nano-prototype for delivery of bioactive compounds: A novel approach for induction of apoptosis in HepG2 cell line. Adv. Med. Sci. 2017, 207, 1–11. [Google Scholar]
- Amararathana, M.; Johnston, M.R.; Vasantha-Rupasinghe, H.P. Plant Polyphenols as Chemopreventive Agents For Lung Cancer. Int. J. Mol. Sci. 2016, 17, 1352. [Google Scholar] [CrossRef]
- Grauzdyté, D.; Raudoniuté, J.; Kulvinskiené, I.; Bagdonas, E.; Stasiulaitiené, I.; Martuzevicius, D.; Bironaite, D.; Aldonyte, R.; Venskutonis, P.R. Cytoprotective Effects of Mangiferin and Z-Ligustilide in PAH-Exposed Human Airway Epithelium in Vitro. Nutrients 2019, 11, 218. [Google Scholar] [CrossRef]
- Venugopal, V.; Kumar, K.J.; Muralidharan, S.; Parasuraman, S.; Raj, P.V.; Kumar, K.V. Optimization and in-vivo evaluation of isradipine nanoparticles using Box-Behnken design surface response methodology. OpenNano 2016, 1, 1–15. [Google Scholar] [CrossRef]
- Gomes, C.; Moreira, R.G.; Castell-Perez, E. Poly (DL-lactide-co-glycolide) (PLGA) nanoparticles with entrapped trans-cinnamaldehyde and eugenol for antimicrobial delivery applications. J. Food Sci. 2011, 76, N16–N24. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.M.; Moraes, T.C.M.; De Camargo, L.E.A.; Khalil, L.F.; Dalmolin, N.M.; Mainardes, R.M. Poly(L-lactide) nanoparticles reduce Amphotericin B cytotoxicity and maintain its in vitro antifungal activity. J. Nanosci. Nanotechnol. 2014, 15, 848–854. [Google Scholar] [CrossRef]
- Alves, A.C.S.; Minardes, R.M.; Khalil, N.M. Nanoencapsulation of gallic acid and evaluation of its cytotoxicity and antioxidant activity. Mater. Sci. Eng. C 2016, 60, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Ritger, P.L.; Peppas, N.A. Simple equation for description of solute release II. Fickian and anomalous release from swellable devices. J. Controll. Release 1987, 5, 37–42. [Google Scholar] [CrossRef]
- Siepmann, J.; Peppas, N.A. Modeling of drug release from delivery systems based on hydroxypropyl methylcellulose (HPMC). Adv. Drug Deliv. Rev. 2001, 64, 163–174. [Google Scholar] [CrossRef]
- Nitiss, J.L.; Nitiss, K.C. Yeast systems for demonstrating the targets of antitopoisomerase II agents. Methods Mol. Biol. 2001, 95, 315–327. [Google Scholar]
- Kizhedath, A.; Wilkinson, S.; Glassey, J. Assessment of hepatotoxicity and dermal toxicity of butyl paraben and methyl paraben using HepG2 and HDFn in vitro models. Toxicol. Vitro 2019, 55, 108–115. [Google Scholar] [CrossRef]
- Kim, Y.J.; Haribalan, P.; Castro-Aceituno, V.; Kim, D.; Markus, J.; Lee, S.; Kim, S.; Liu, Y.; Chun-Yang, D. Photoluminescent And Self-Assembled Hyaluronic Acid-Zinc Oxide-Ginsenoside Rh2 Nanoparticles And Their Potential Caspase-9 Apoptotic Mechanism Towards Cancer Cell Lines. Int. J. Nanomed. 2019, 14, 8195–8208. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Razura-Carmona, F.F.; Pérez-Larios, A.; González-Silva, N.; Herrera-Martínez, M.; Medina-Torres, L.; Sáyago-Ayerdi, S.G.; Sánchez-Burgos, J.A. Mangiferin-Loaded Polymeric Nanoparticles: Optical Characterization, Effect of Anti-topoisomerase I, and Cytotoxicity. Cancers 2019, 11, 1965. https://doi.org/10.3390/cancers11121965
Razura-Carmona FF, Pérez-Larios A, González-Silva N, Herrera-Martínez M, Medina-Torres L, Sáyago-Ayerdi SG, Sánchez-Burgos JA. Mangiferin-Loaded Polymeric Nanoparticles: Optical Characterization, Effect of Anti-topoisomerase I, and Cytotoxicity. Cancers. 2019; 11(12):1965. https://doi.org/10.3390/cancers11121965
Chicago/Turabian StyleRazura-Carmona, Francisco Fabian, Alejandro Pérez-Larios, Napoleón González-Silva, Mayra Herrera-Martínez, Luis Medina-Torres, Sonia Guadalupe Sáyago-Ayerdi, and Jorge Alberto Sánchez-Burgos. 2019. "Mangiferin-Loaded Polymeric Nanoparticles: Optical Characterization, Effect of Anti-topoisomerase I, and Cytotoxicity" Cancers 11, no. 12: 1965. https://doi.org/10.3390/cancers11121965
APA StyleRazura-Carmona, F. F., Pérez-Larios, A., González-Silva, N., Herrera-Martínez, M., Medina-Torres, L., Sáyago-Ayerdi, S. G., & Sánchez-Burgos, J. A. (2019). Mangiferin-Loaded Polymeric Nanoparticles: Optical Characterization, Effect of Anti-topoisomerase I, and Cytotoxicity. Cancers, 11(12), 1965. https://doi.org/10.3390/cancers11121965