Three-Dimensional Conformal Radiotherapy-Based or Intensity-Modulated Radiotherapy-Based Concurrent Chemoradiotherapy in Patients with Thoracic Esophageal Squamous Cell Carcinoma
Abstract
1. Introduction
2. Patients and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations Lis
| RT | radiotherapy |
| IMRT | intensity-modulated radiotherapy |
| ICD-9-CM | International Classification of Diseases, Ninth Revision, Clinical Modification |
| CCRT | concurrent chemoradiotherapy |
| AJCC | American Joint Committee on Cancer |
| HR | hazard ratio |
| CI | confidence interval |
| CCI | Charlson comorbidity index |
| TESCC | thoracic esophageal squamous cell carcinoma |
| ESCC | esophageal squamous cell carcinoma |
| SCC | squamous cell carcinoma |
| 3D-CRT | three-dimensional conformal radiation therapy |
| NCCN | National Comprehensive Cancer Network |
| TCRD | Taiwan Cancer Registry Database |
References
- National Health Insurance Administration. Ministry of Health and Welfare: Taipei, China (2015). 2017. Available online: http://nhird.nhri.org.tw/en/Data_Subsets.html#S3 and http://nhis.nhri.org.tw/point.html. (accessed on 31 December 2016).
- Lin, W.C.; Ding, Y.F.; Hsu, H.L.; Chang, J.H.; Yuan, K.S.; Wu, A.T.H.; Chow, J.M.; Chang, C.L.; Chen, S.U.; Wu, S.Y. Value and application of trimodality therapy or definitive concurrent chemoradiotherapy in thoracic esophageal squamous cell carcinoma. Cancer 2017, 123, 3904–3915. [Google Scholar] [CrossRef] [PubMed]
- Yen, Y.C.; Chang, J.H.; Lin, W.C.; Chiou, J.F.; Chang, Y.C.; Chang, C.L.; Hsu, H.L.; Chow, J.M.; Yuan, K.S.; Wu, A.T.H.; et al. Effectiveness of esophagectomy in patients with thoracic esophageal squamous cell carcinoma receiving definitive radiotherapy or concurrent chemoradiotherapy through intensity-modulated radiation therapy techniques. Cancer 2017, 123, 2043–2053. [Google Scholar] [CrossRef]
- Chang, C.L.; Tsai, H.C.; Lin, W.C.; Chang, J.H.; Hsu, H.L.; Chow, J.M.; Yuan, K.S.; Wu, A.T.H.; Wu, S.Y. Dose escalation intensity-modulated radiotherapy-based concurrent chemoradiotherapy is effective for advanced-stage thoracic esophageal squamous cell carcinoma. Radiother. Oncol. 2017, 125, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Pennathur, A.; Gibson, M.K.; Jobe, B.A.; Luketich, J.D. Oesophageal carcinoma. Lancet 2013, 12, 381–400. [Google Scholar] [CrossRef]
- Domper Arnal, M.J.; Ferrandez Arenas, A.; Lanas Arbeloa, A. Esophageal cancer: Risk factors, screening and endoscopic treatment in Western and Eastern countries. World J. Gastroenterol. 2015, 21, 7933–7943. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology; NCCN: Plymouth Meeting, PA, USA, 2019. [Google Scholar]
- Minsky, B.D.; Pajak, T.F.; Ginsberg, R.J.; Pisansky, T.M.; Martenson, J.; Komaki, R.; Okawara, G.; Rosenthal, S.A.; Kelsen, D.P. INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: High-dose versus standard-dose radiation therapy. J. Clin. Oncol. 2002, 20, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, A.; Shibamoto, Y.; Miyakawa, A.; Murai, T.; Otsuka, S.; Iwaya, H.; Sugie, C.; Yanggi, t.; Ogino, H.; Ishikura, S. Definitive Concurrent Chemotherapy and High-dose (60-70 Gy) Radiotherapy for Esophageal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, S325. [Google Scholar] [CrossRef]
- Kondo, T.; Shibamoto, Y.; Hayashi, A.; Takaoka, T.; Murai, T.; Miyakawa, A.; Sugie, C.; Yanagi, T.; Matsuo, M. Definitive Concurrent Chemotherapy and High Dose (60-70Gy) Radiation Therapy for Esophageal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2015, 93, E131–E132. [Google Scholar] [CrossRef]
- Lieberman, M.D.; Shriver, C.D.; Bleckner, S.; Burt, M. Carcinoma of the esophagus. Carcinoma of the esophagus. Prognostic significance of histologic type. J. Thorac. Cardiovasc. Surg. 1995, 109, 130–139. [Google Scholar] [CrossRef]
- Siewert, J.R.; Ott, K. Are squamous and adenocarcinomas of the esophagus the same disease? Semin. Radiat. Oncol. 2007, 17, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Bollschweiler, E.; Metzger, R.; Drebber, U.; Baldus, S.; Vallbohmer, D.; Kocher, M.; Holscher, A.H. Histological type of esophageal cancer might affect response to neo-adjuvant radiochemotherapy and subsequent prognosis. Ann. Oncol. 2009, 20, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Hölscher, A.H.; Bollschweiler, E.; Schneider, P.M.; Siewert, J.R. Prognosis of early esophageal cancer. Comparison between adeno-and squamous cell carcinoma. Cancer 1995, 76, 178–816. [Google Scholar] [CrossRef]
- Siewert, J.R.; Stein, H.J.; Feith, M.; Bruecher, B.L.; Bartels, H.; Fink, U. Histologic tumor type is an independent prognostic parameter in esophageal cancer: Lessons from more than 1,000 consecutive resections at a single center in the Western world. Ann. Surg. 2001, 234, 360. [Google Scholar] [CrossRef] [PubMed]
- Hermanto, U.; Frija, E.K.; Lii, M.J.; Chang, E.L.; Mahajan, A.; Woo, S.Y. Intensity-modulated radiotherapy (IMRT) and conventional three-dimensional conformal radiotherapy for high-grade gliomas: Does IMRT increase the integral dose to normal brain? Int. J. Radiat. Oncol. Biol. Phys. 2007, 67, 1135–1144. [Google Scholar] [CrossRef] [PubMed]
- Boyle, J.; Ackerson, B.; Gu, L.; Kelsey, C.R. Dosimetric advantages of intensity modulated radiation therapy in locally advanced lung cancer. Adv. Radiat. Oncol. 2017, 2, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Bakiu, E.; Telhaj, E.; Kozma, E.; Ruci, F.; Malkaj, P. Comparison of 3D CRT and IMRT Tratment Plans. Acta Inform. Med. 2013, 21, 211. [Google Scholar] [CrossRef] [PubMed]
- Haefner, M.F.; Lang, K.; Verma, V.; Koerber, S.A.; Uhlmann, L.; Debus, J.; Sterzing, F. Intensity-modulated versus 3-dimensional conformal radiotherapy in the definitive treatment of esophageal cancer: Comparison of outcomes and acute toxicity. Radiat. Oncol. 2017, 12, 131. [Google Scholar] [CrossRef]
- Aoyama, H.; Westerly, D.C.; Mackie, T.R.; Olivera, G.H.; Bentzen, S.M.; Patel, R.R.; Jaradat, H.; Tome, W.A.; Ritter, M.A.; Mehta, M.P. Integral radiation dose to normal structures with conformal external beam radiation. Int. J. Radiat. Oncol. Biol. Phys. 2006, 64, 962–967. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.J.; Wuu, C.S. Radiation-induced second cancers: The impact of 3D-CRT and IMRT. Int. J. Radiat. Oncol. Biol. Phys. 2003, 56, 83–88. [Google Scholar] [CrossRef]
- Hsu, F.M.; Lee, Y.C.; Lee, J.M.; Hsu, C.H.; Lin, C.C.; Tsai, Y.C.; Wu, J.K.; Cheng, J.C. Association of clinical and dosimetric factors with postoperative pulmonary complications in esophageal cancer patients receiving intensity-modulated radiation therapy and concurrent chemotherapy followed by thoracic esophagectomy. Ann. Surg. Oncol. 2009, 16, 1669–1677. [Google Scholar] [CrossRef]
- Yaremko, B.P.; Palma, D.A.; Erickson, A.L.; Pierce, G.; Malthaner, R.A.; Inculet, R.I.; Dar, A.R.; Rodrigues, G.B.; Yu, E. Adjuvant concurrent chemoradiation using intensity-modulated radiotherapy and simultaneous integrated boost for resected high-risk adenocarcinoma of the distal esophagus and gastro-esophageal junction. Radiat. Oncol. 2013, 8, 33. [Google Scholar] [CrossRef] [PubMed]
- Jain, V.; Berman, A.T. Radiation Pneumonitis: Old Problem, New Tricks. Cancers 2018, 10, 222. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, S.; Chang, B.W. Current strategies in chemoradiation for esophageal cancer. J. Gastrointest. Oncol. 2014, 5, 156–165. [Google Scholar] [PubMed]
- Macomber, M.W.; Bowen, S.R.; Gopan, O.; Yeung, R.; Apisarnthanarax, S.; Zeng, J.; Patel, S. Heart Dose and Outcomes in Radiation Treatment for Esophageal Cancer. Cureus 2018, 10, e2378. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Liao, Z.; Chen, Y.; Chang, J.Y.; Jeter, M.; Guerrero, T.; Ajani, J.; Phan, A.; Swisher, S.; Allen, P.; et al. Esophageal cancer located at the neck and upper thorax treated with concurrent chemoradiation: A single-institution experience. J. Thorac. Oncol. 2006, 1, 252–259. [Google Scholar] [CrossRef]
- Hoeben, A.; Polak, J.; Van De Voorde, L.; Hoebers, F.; Grabsch, H.I.; de Vos-Geelen, J. Cervical esophageal cancer: A gap in cancer knowledge. Ann. Oncol. 2016, 27, 1664–1674. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.; Xia, P.; Quivey, J.M.; Sultanem, K.; Poon, I.; Akazawa, C.; Akazawa, P.; Weinberg, V.; Fu, K.K. Intensity-modulated radiotherapy in the treatment of nasopharyngeal carcinoma: An update of the UCSF experience. Int. J. Radiat. Oncol. Biol. Phys. 2002, 53, 12–22. [Google Scholar] [CrossRef]
- Nutting, C.M.; Morden, J.P.; Harrington, K.J.; Urbano, T.G.; Bhide, S.A.; Clark, C.; Miles, E.A.; Miah, A.B.; Newbold, K.; Tanay, M.; et al. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): A phase 3 multicentre randomised controlled trial. Lancet Oncol. 2011, 12, 127–136. [Google Scholar] [CrossRef]
- Chen, J.H.; Yen, Y.C.; Chen, T.M.; Yuan, K.S.; Lee, F.P.; Lin, K.C.; Lai, M.T.; Wu, C.C.; Chang, C.L.; Wu, S.Y. Survival prognostic factors for metachronous second primary head and neck squamous cell carcinoma. Cancer Med. 2017, 6, 142–153. [Google Scholar] [CrossRef]
- Chen, T.M.; Lin, K.C.; Yuan, K.S.; Chang, C.L.; Chow, J.M.; Wu, S.Y. Treatment of advanced nasopharyngeal cancer using low-or high-dose concurrent chemoradiotherapy with intensity-modulated radiotherapy: A propensity score-matched, nationwide, population-based cohort study. Radiother. Oncol. 2017, 123, 23–29. [Google Scholar] [CrossRef]
- Lin, Y.K.; Hsieh, M.C.; Chang, C.L.; Chow, J.M.; Yuan, K.S.; Wu, A.T.H.; Wu, S.Y. Intensity-modulated radiotherapy with systemic chemotherapy improves survival in patients with nonmetastatic unresectable pancreatic adenocarcinoma: A propensity score-matched, nationwide, population-based cohort study. Radiother. Oncol. 2018, 129, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.J.; Bosch, W.R.; Chang, D.T.; Hong, T.S.; Jabbour, S.K.; Kleinberg, L.R.; Mamon, H.J.; Thomas, C.R., Jr.; Goodman, K.A. Expert Consensus Contouring Guidelines for Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2015, 92, 911–920. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurance Administration. Ministry of Health and Welfare, Taiwan, R.O.C. (2014)., National Health Insurance Annual Report 2014–2015. 2016. Available online: http://tcr.cph.ntu.edu.tw/main.php?Page=A6 (accessed on 4 March 2019).
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Chen, J.H.; Yen, Y.C.; Yang, H.C.; Liu, S.H.; Yuan, S.P.; Wu, L.L.; Lee, F.P.; Lin, K.C.; Lai, M.T.; Wu, C.C.; et al. Curative-Intent Aggressive Treatment Improves Survival in Elderly Patients with Locally Advanced Head and Neck Squamous Cell Carcinoma and High Comorbidity Index. Medicine 2016, 95, e3268. [Google Scholar] [CrossRef] [PubMed]
- Darby, S.C.; Ewertz, M.; McGale, P.; Bennet, A.M.; Blom-Goldman, U.; Bronnum, D.; Correa, C.; Cutter, D.; Gagliardi, G.; Gigante, B.; et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N. Engl. J. Med. 2013, 368, 987–998. [Google Scholar] [CrossRef] [PubMed]
- Byhardt, R.W.; Martin, L.; Pajak, T.F.; Shin, K.H.; Emami, B.; Cox, J.D. The influence of field size and other treatment factors on pulmonary toxicity following hyperfractionated irradiation for inoperable non-small cell lung cancer (NSCLC)-analysis of a Radiation Therapy Oncology Group (RTOG) protocol. Int. J. Radiat. Oncol. Biol. Phys. 1993, 27, 537–544. [Google Scholar] [CrossRef]
- Lin, S.H.; Wang, L.; Myles, B.; Thall, P.F.; Hofstetter, W.L.; Swisher, S.G.; Ajani, J.A.; Cox, J.D.; Komaki, R.; Liao, Z. Propensity score-based comparison of long-term outcomes with 3-dimensional conformal radiotherapy vs. intensity-modulated radiotherapy for esophageal cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 1078–1085. [Google Scholar] [CrossRef] [PubMed]
- Zenda, S.; Kojima, T.; Kato, K.; Izumi, S.; Ozawa, T.; Kiyota, N.; Katada, C.; Tsushima, T.; Ito, Y.; Akimoto, T.; et al. Multicenter Phase 2 Study of Cisplatin and 5-Fluorouracil With Concurrent Radiation Therapy as an Organ Preservation Approach in Patients With Squamous Cell Carcinoma of the Cervical Esophagus. Int. J. Radiat. Oncol. Biol. Phys. 2016, 96, 976–984. [Google Scholar] [CrossRef]
- Cao, C.N.; Luo, J.W.; Gao, L.; Xu, G.Z.; Yi, J.L.; Huang, X.D.; Li, S.Y.; Xiao, J.P.; Liu, S.Y.; Xu, Z.G.; et al. Primary radiotherapy compared with primary surgery in cervical esophageal cancer. JAMA Otolaryngol. Head Neck Surg. 2014, 140, 918–926. [Google Scholar] [CrossRef]
- Zhang, P.; Xi, M.; Zhao, L.; Qiu, B.; Liu, H.; Hu, Y.H.; Liu, M.Z. Clinical efficacy and failure pattern in patients with cervical esophageal cancer treated with definitive chemoradiotherapy. Radiother. Oncol. 2015, 116, 257–261. [Google Scholar] [CrossRef]
- Cunningham, D.; Allum, W.H.; Stenning, S.P.; Thompson, J.N.; Van de Velde, C.J.; Nicolson, M.; Scarffe, J.H.; Lofts, F.J.; Falk, S.J.; Iveson, T.J.; et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N. Engl. J. Med. 2006, 355, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Sjoquist, K.M.; Burmeister, B.H.; Smithers, B.M.; Zalcberg, J.R.; Simes, R.J.; Barbour, A.; Gebski, V. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: An updated meta-analysis. Lancet Oncol. 2011, 12, 681–692. [Google Scholar] [CrossRef]
- Fenkell, L.; Kaminsky, I.; Breen, S.; Huang, S.; Van Prooijen, M.; Ringash, J. Dosimetric comparison of IMRT vs. 3D conformal radiotherapy in the treatment of cancer of the cervical esophagus. Radiother. Oncol. 2008, 89, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Chandra, A.; Guerrero, T.M.; Liu, H.H.; Tucker, S.L.; Liao, Z.; Wang, X.; Murshed, H.; Bonnen, M.D.; Garg, A.K.; Stevens, C.W.; et al. Feasibility of using intensity-modulated radiotherapy to improve lung sparing in treatment planning for distal esophageal cancer. Radiother. Oncol. 2005, 77, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Nicolini, G.; Ghosh-Laskar, S.; Shrivastava, S.K.; Banerjee, S.; Chaudhary, S.; Agarwal, J.P.; Munshi, A.; Clivio, A.; Fogliata, A.; Mancosu, P.; et al. Volumetric modulation arc radiotherapy with flattening filter-free beams compared with static gantry IMRT and 3D conformal radiotherapy for advanced esophageal cancer: A feasibility study. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 553–560. [Google Scholar] [CrossRef]
- Wu, V.W.; Kwong, D.L.; Sham, J.S. Target dose conformity in 3-dimensional conformal radiotherapy and intensity modulated radiotherapy. Radiother. Oncol. 2004, 71, 201–206. [Google Scholar] [CrossRef]
- Wang, D.; Yang, Y.; Zhu, J.; Li, B.; Chen, J.; Yin, Y. 3D-conformal RT, fixed-field IMRT and RapidArc, which one is better for esophageal carcinoma treated with elective nodal irradiation. Technol. Cancer Res. Treat. 2011, 10, 487–494. [Google Scholar] [CrossRef]
- Graham, M.V.; Purdy, J.A.; Emami, B.; Harms, W.; Bosch, W.; Lockett, M.A.; Perez, C.A. Clinical dose-volume histogram analysis for pneumonitis after 3D treatment for non-small cell lung cancer (NSCLC). Int. J. Radiat. Oncol. Biol. Phys. 1999, 45, 323–329. [Google Scholar] [CrossRef]
- Hernando, M.L.; Marks, L.B.; Bentel, G.C.; Zhou, S.M.; Hollis, D.; Das, S.K.; Fan, M.; Munley, M.T.; Shafman, T.D.; Anscher, M.S.; et al. Radiation-induced pulmonary toxicity: A dose-volume histogram analysis in 201 patients with lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2001, 51, 650–659. [Google Scholar] [CrossRef]
- Kwa, S.L.; Lebesque, J.V.; Theuws, J.C.; Marks, L.B.; Munley, M.T.; Bentel, G.; Oetzel, D.; Spahn, U.; Graham, M.V.; Drzymala, R.E.; et al. Radiation pneumonitis as a function of mean lung dose: An analysis of pooled data of 540 patients. Int. J. Radiat. Oncol. Biol. Phys. 1998, 42, 1–9. [Google Scholar] [CrossRef]
- Seppenwoolde, Y.; Lebesque, J.V.; de Jaeger, K.; Belderbos, J.S.; Boersma, L.J.; Schilstra, C.; Henning, G.T.; Hayman, J.A.; Martel, M.K.; Ten Haken, R.K. Comparing different NTCP models that predict the incidence of radiation pneumonitis. Normal tissue complication probability. Int. J. Radiat. Oncol. Biol. Phys. 2003, 55, 724–735. [Google Scholar] [CrossRef]
- Chen, Y.J.; Liu, A.; Han, C.; Tsai, P.T.; Schultheiss, T.E.; Pezner, R.D.; Vora, N.; Lim, D.; Shibata, S.; Kernstine, K.H.; et al. Helical tomotherapy for radiotherapy in esophageal cancer: A preferred plan with better conformal target coverage and more homogeneous dose distribution. Med. Dosim. 2007, 32, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Kwa, S.L.; Theuws, J.C.; Wagenaar, A.; Damen, E.M.; Boersma, L.J.; Baas, P.; Muller, S.H.; Lebesque, J.V. Evaluation of two dose-volume histogram reduction models for the prediction of radiation pneumonitis. Radiother. Oncol. 1998, 48, 61–69. [Google Scholar] [CrossRef]
- Kole, T.P.; Aghayere, O.; Kwah, J.; Yorke, E.D.; Goodman, K.A. Comparison of heart and coronary artery doses associated with intensity-modulated radiotherapy versus three-dimensional conformal radiotherapy for distal esophageal cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, 1580–1586. [Google Scholar] [CrossRef]
- Kinsman, K.J.; DeGregorio, B.T.; Katon, R.M.; Morrison, K.; Saxon, R.R.; Keller, F.S.; Rosch, J. Prior radiation and chemotherapy increase the risk of life-threatening complications after insertion of metallic stents for esophagogastric malignancy. Gastrointest. Endosc. 1996, 43, 196–203. [Google Scholar] [CrossRef]
- Zhou, Z.G.; Zhen, C.J.; Bai, W.W.; Zhang, P.; Qiao, X.Y.; Liang, J.L.; Gao, X.S.; Wang, S.S. Salvage radiotherapy in patients with local recurrent esophageal cancer after radical radiochemotherapy. Radiat. Oncol. 2015, 10, 54. [Google Scholar] [CrossRef]
- Hsu, P.K.; Wu, Y.C.; Chou, T.Y.; Huang, C.S.; Hsu, W.H. Comparison of the 6th and 7th editions of the American Joint Committee on Cancer tumor-node-metastasis staging system in patients with resected esophageal carcinoma. Ann. Thorac. Surg. 2010, 89, 1024–1031. [Google Scholar] [CrossRef]
- Cheng, Y.F.; Chen, H.S.; Wu, S.C.; Chen, H.C.; Hung, W.H.; Lin, C.H.; Wang, B.Y. Esophageal squamous cell carcinoma and prognosis in Taiwan. Cancer Med. 2018, 7, 4193–4201. [Google Scholar] [CrossRef]
- Berry, S.D.; Ngo, L.; Samelson, E.J.; Kiel, D.P. Competing risk of death: An important consideration in studies of older adults. J. Am. Geriatr. Soc. 2010, 58, 783–787. [Google Scholar] [CrossRef]
| Variable | All | IMRT | 3D-CRT | ||||
|---|---|---|---|---|---|---|---|
| n = 2062 | (%) | n = 1524 | (%) | n = 538 | (%) | p Value | |
| Age | |||||||
| SD | 57.92 | 11.00 | 57.85 | 10.86 | 58.44 | 11.37 | 0.1342 |
| 0.5096 | |||||||
| 20–29 | 6 | (0.29) | 4 | (0.26) | 2 | (0.37) | |
| 30–39 | 55 | (2.67) | 40 | (2.62) | 15 | (2.79) | |
| 40–49 | 472 | (23.09) | 345 | (22.64) | 127 | (23.61) | |
| 50–59 | 714 | (34.82) | 545 | (35.76) | 169 | (31.41) | |
| 60–69 | 500 | (23.97) | 367 | (24.08) | 133 | (24.72) | |
| 70–79 | 240 | (11.45) | 168 | (11.02) | 72 | (13.38) | |
| 80–89 | 72 | (3.52) | 52 | (3.41) | 20 | (3.72) | |
| 90–100 | 3 | (0.14) | 3 | (0.20) | 0 | (0.00) | |
| Sex | 0.4189 | ||||||
| Male | 1960 | (95.05) | 1447 | (94.95) | 513 | (95.35) | |
| Female | 102 | (4.95) | 77 | (5.05) | 25 | (4.65) | |
| Follow-up time (year) | 0.1848 | ||||||
| Median, IQR | 2.02 | 1.15 | 2.02 | 1.15 | 2.00 | 1.14 | |
| (q1, q3) | (0.92, | 2.77) | (0.93, | 2.78) | (0.99, | 2.74) | |
| (min, max) | (0.09, | 7.29) | (0.09, | 7.29) | (0.12, | 6.96) | |
| CCI score | |||||||
| SD | 1.25 | 1.39 | 1.25 | 1.40 | 1.29 | 1.34 | 0.4568 |
| 0 | 697 | (34.03) | 533 | (34.97) | 164 | (30.48) | 0.2443 |
| 1 | 721 | (35.10) | 525 | (34.45) | 196 | (36.43) | |
| 2 | 353 | (16.78) | 253 | (16.60) | 100 | (18.59) | |
| >3 | 291 | (14.09) | 213 | (13.98) | 78 | (14.50) | |
| Radiation dose (Gy) | 0.9617 | ||||||
| Median, IQR | 50.40 | 0.30 | 50.40 | 0.31 | 50.40 | 0.22 | |
| Cumulative cisplatin dose (mg/m2) | 0.1152 | ||||||
| Mean (SD) | 255.57 | 57.65 | 255.57 | 58.61 | 253.56 | 59.16 | |
| AJCC clinical stages | 0.0017 | ||||||
| Early stage (IA-IIB) | 336 | (16.78) | 232 | (15.22) | 104 | (19.33) | |
| Advanced stage (IIIA-IIIC) | 1726 | (83.22) | 1292 | (84.78) | 434 | (80.67) | |
| AJCC clinical stages | <0.0001 | ||||||
| IA | 5 | (0.42) | 5 | (0.33) | 0 | (0.00) | |
| IB | 31 | (1.62) | 24 | (1.57) | 7 | (1.30) | |
| IIA | 126 | (6.31) | 79 | (5.18) | 47 | (8.74) | |
| IIB | 174 | (8.44) | 124 | (8.14) | 50 | (9.29) | |
| IIIA | 397 | (19.19) | 319 | (20.93) | 78 | (14.50) | |
| IIIB | 661 | (31.80) | 439 | (28.81) | 219 | (40.71) | |
| IIIC | 671 | (32.22) | 534 | (35.04) | 137 | (25.46) | |
| Year of diagnosis | <0.0001 | ||||||
| 2006–2010 | 798 | (39.08) | 450 | (29.53) | 348 | (64.68) | |
| 2011–2014 | 1264 | (60.92) | 1074 | (70.47) | 190 | (35.32) | |
| Toxicity profile | 0.5687 | ||||||
| Major heart events | 58 | (2.81) | 41 | (2.69) | 17 | (3.16) | |
| Radiation pneumonitis grade 2 | 465 | (22.55 | 334 | (21.92) | 122 | (22.67) | |
| Death | <0.0001 | ||||||
| No | 454 | (21.84) | 372 | (24.41) | 82 | (15.24) | |
| Yes | 1608 | (78.16) | 1152 | (75.59) | 456 | (84.76) | |
| Variable | Univariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | aHR * | 95% CI | p | |||
| RT Modalities | ||||||||
| 3D-CRT (ref) | 1 | 1 | ||||||
| IMRT | 0.89 | (0.80, | 0.99) | 0.0372 | 0.88 | (0.78, | 0.98) | 0.0223 |
| Sex | ||||||||
| Female (ref) | 1 | 1 | ||||||
| Male | 1.12 | (0.89, | 1.40) | 0.3378 | 1.06 | (0.84, | 1.33) | 0.6274 |
| Age | ||||||||
| 20–29 (ref) | 1 | 1 | ||||||
| 30–39 | 2.07 | (0.29, | 14.86) | 0.4680 | 2.30 | (0.32, | 16.71) | 0.4098 |
| 40–49 | 2.25 | (0.32, | 15.88) | 0.4149 | 2.44 | (0.34, | 17.42) | 0.3735 |
| 50–59 | 1.79 | (0.25, | 12.59) | 0.5600 | 1.98 | (0.28, | 14.12) | 0.4958 |
| 60–69 | 1.65 | (0.23, | 11.65) | 0.6141 | 1.78 | (0.25, | 12.72) | 0.5649 |
| 70–79 | 1.62 | (0.23, | 11.42) | 0.6311 | 1.89 | (0.26, | 13.57) | 0.5251 |
| 80–89 | 1.92 | (0.27, | 13.76) | 0.5144 | 2.17 | (0.30, | 15.73) | 0.4433 |
| 90– | 2.14 | (0.23, | 20.44) | 0.5075 | 3.09 | (0.32, | 29.79) | 0.3295 |
| CCI score | ||||||||
| 0 (ref) | 1 | 1 | ||||||
| 1 | 0.98 | (0.87, | 1.11) | 0.7628 | 1.02 | (0.91, | 1.15) | 0.7646 |
| 2 | 0.94 | (0.81, | 1.08) | 0.3725 | 1.02 | (0.88, | 1.18) | 0.7948 |
| >3 | 0.96 | (0.83, | 1.12) | 0.6291 | 1.14 | (0.97, | 1.33) | 0.1176 |
| Year of diagnosis | ||||||||
| 2006–2010 (ref) | 1 | 1 | ||||||
| 2011–2014 | 0.96 | (0.87, | 1.07) | 0.4678 | 0.96 | (0.87, | 1.07) | 0.4741 |
| AJCC clinical stages | ||||||||
| Early stage (ref) | 1 | 1 | ||||||
| Advanced stage | 1.84 | (1.59, | 2.12) | <0.0001 | 1.89 | (1.63, | 2.19) | <.0001 |
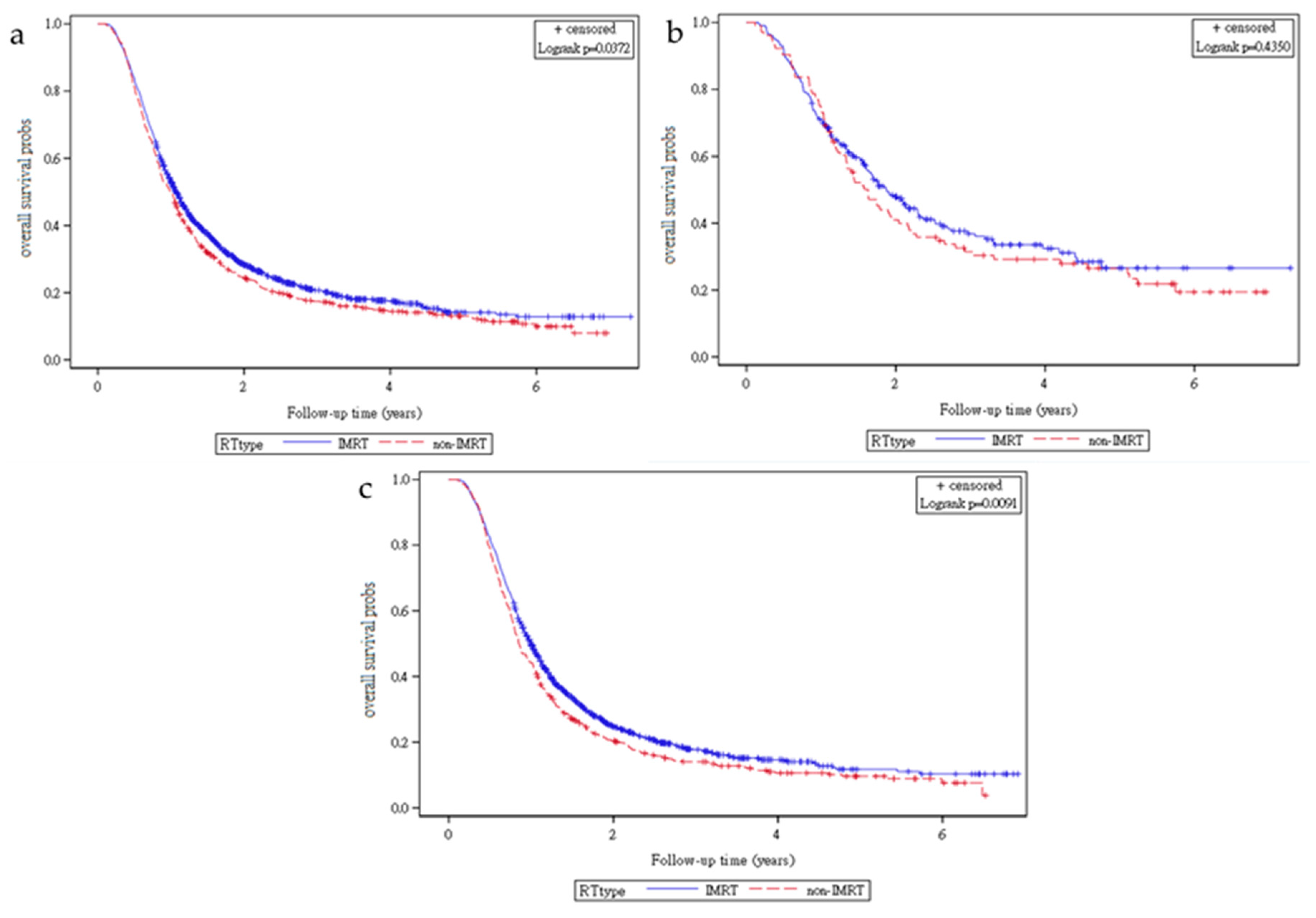
| Treatment | n | Death | Death Rate (%) | Univariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p Value | aHR * | 95% CI | p Value | ||||||
| All stage | 2062 | 1608 | |||||||||
| 3D-CRT | 538 | 456 | 84.76 | 1 | 1 | ||||||
| IMRT | 1524 | 1152 | 75.59 | 0.89 | (0.80, | 0.99) | 0.0372 | 0.88 | (0.78, | 0.98) | 0.0223 |
| Early stage (IA~IIB) | 336 | 218 | |||||||||
| 3D-CRT | 104 | 77 | 74.04 | 1 | 1 | ||||||
| IMRT | 232 | 141 | 60.78 | 0.89 | (0.68, | 1.18) | 0.4344 | 0.91 | (0.67, | 1.25) | 0.5746 |
| Advanced stage (IIIA-IIIC) | 1726 | 1390 | |||||||||
| 3D-CRT | 434 | 379 | 87.33 | 1 | 1 | ||||||
| IMRT | 1292 | 1011 | 78.25 | 0.85 | (0.76, | 0.96) | 0.0091 | 0.88 | (0.77, | 0.99) | 0.0368 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, W.-C.; Chang, C.-L.; Hsu, H.-L.; Yuan, K.S.-P.; Wu, A.T.H.; Wu, S.-Y. Three-Dimensional Conformal Radiotherapy-Based or Intensity-Modulated Radiotherapy-Based Concurrent Chemoradiotherapy in Patients with Thoracic Esophageal Squamous Cell Carcinoma. Cancers 2019, 11, 1529. https://doi.org/10.3390/cancers11101529
Lin W-C, Chang C-L, Hsu H-L, Yuan KS-P, Wu ATH, Wu S-Y. Three-Dimensional Conformal Radiotherapy-Based or Intensity-Modulated Radiotherapy-Based Concurrent Chemoradiotherapy in Patients with Thoracic Esophageal Squamous Cell Carcinoma. Cancers. 2019; 11(10):1529. https://doi.org/10.3390/cancers11101529
Chicago/Turabian StyleLin, Wei-Cheng, Chia-Lun Chang, Han-Lin Hsu, Kevin Sheng-Po Yuan, Alexander T. H. Wu, and Szu-Yuan Wu. 2019. "Three-Dimensional Conformal Radiotherapy-Based or Intensity-Modulated Radiotherapy-Based Concurrent Chemoradiotherapy in Patients with Thoracic Esophageal Squamous Cell Carcinoma" Cancers 11, no. 10: 1529. https://doi.org/10.3390/cancers11101529
APA StyleLin, W.-C., Chang, C.-L., Hsu, H.-L., Yuan, K. S.-P., Wu, A. T. H., & Wu, S.-Y. (2019). Three-Dimensional Conformal Radiotherapy-Based or Intensity-Modulated Radiotherapy-Based Concurrent Chemoradiotherapy in Patients with Thoracic Esophageal Squamous Cell Carcinoma. Cancers, 11(10), 1529. https://doi.org/10.3390/cancers11101529






