Osmotically Enabled Wearable Patch for Sweat Harvesting and Lactate Quantification
Abstract
:1. Introduction
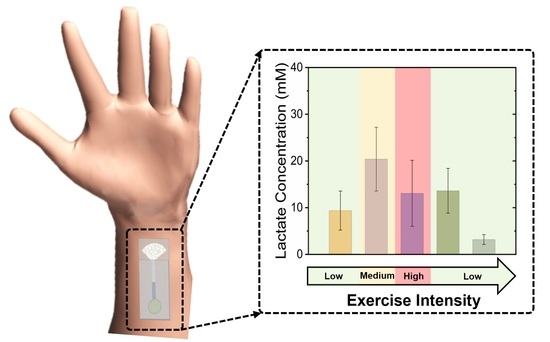
2. Experimental Section
2.1. Materials
2.2. Patch Fabrication
2.3. Hydrogel Synthesis and PDMS Disk Fabrication
2.4. On-Skin (In Vivo) Sweat Analysis
2.5. Statistical Analysis
3. Results and Discussion
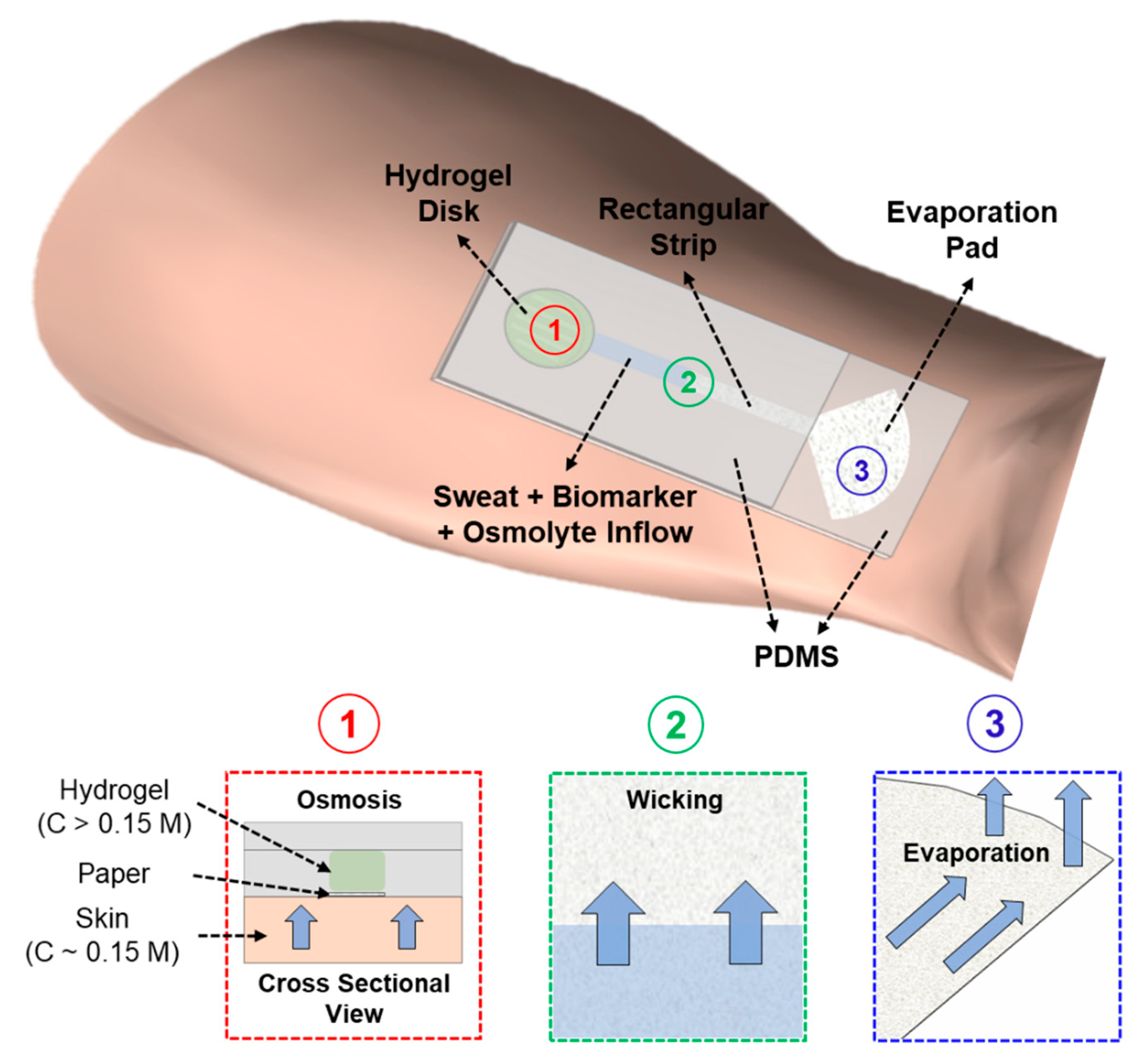
3.1. Sweat Sampling Mechanism of the Wearable Patch
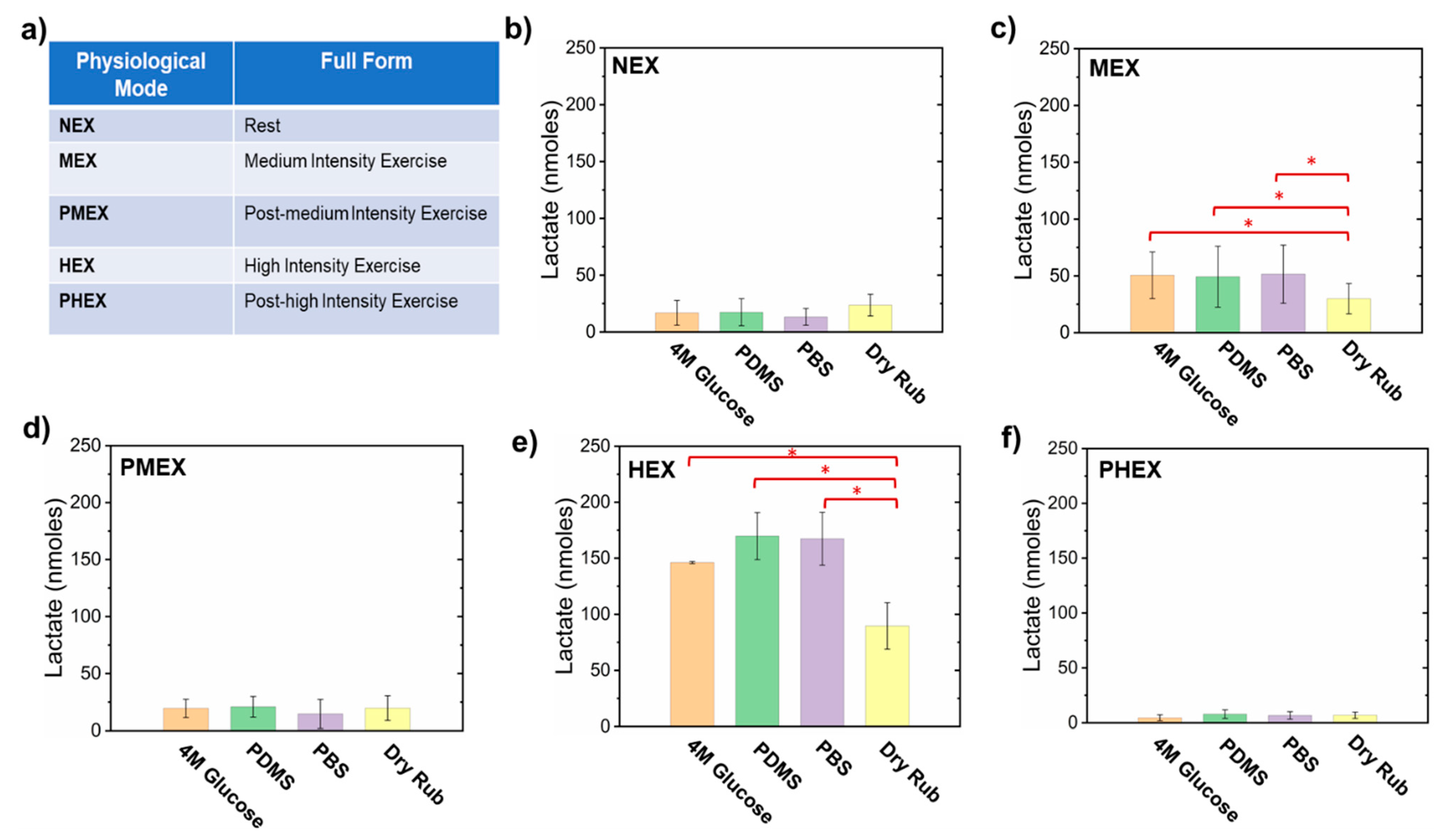
3.2. Sampling of Sweat Lactate Using Different Pumping Materials in the Patch
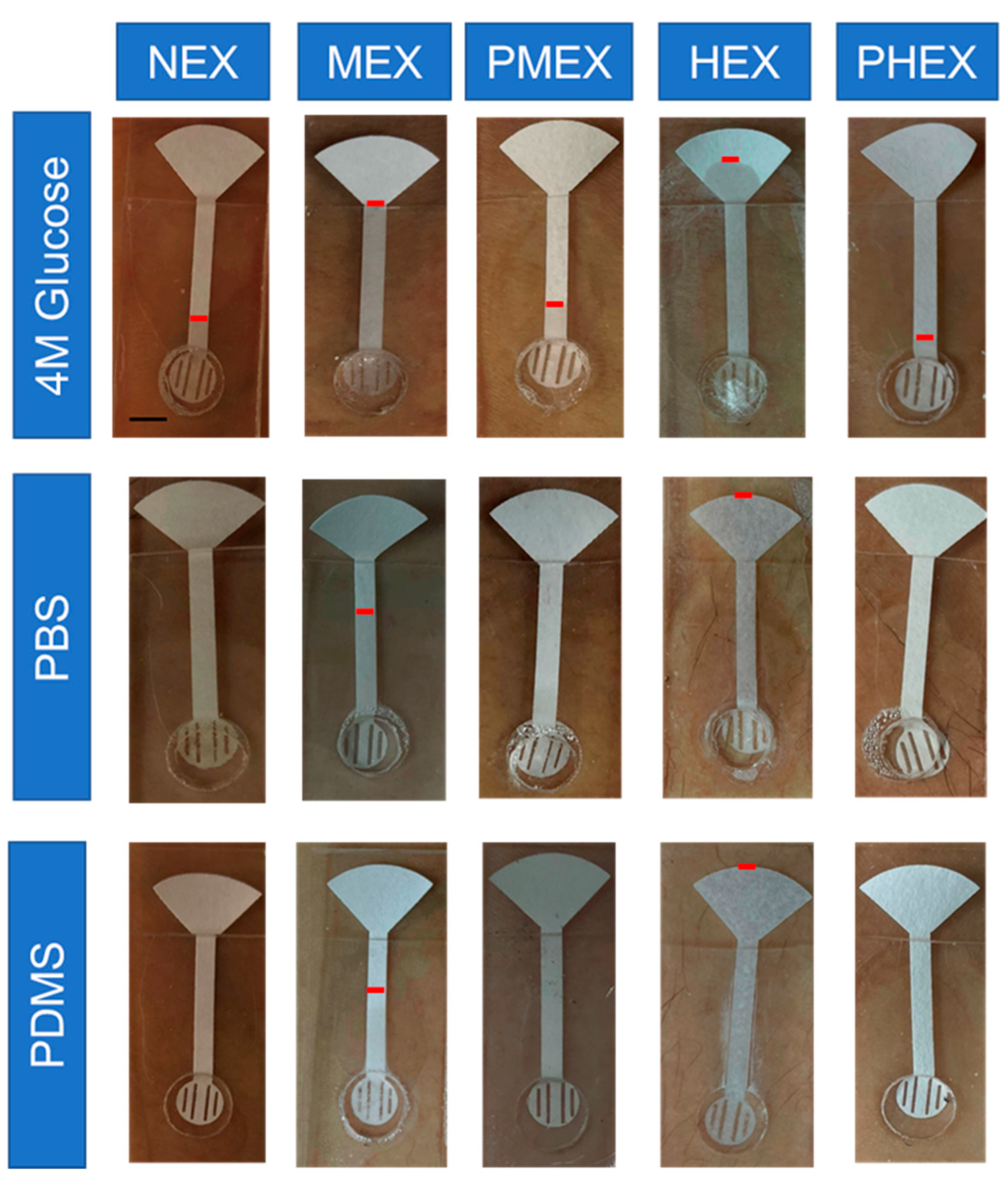
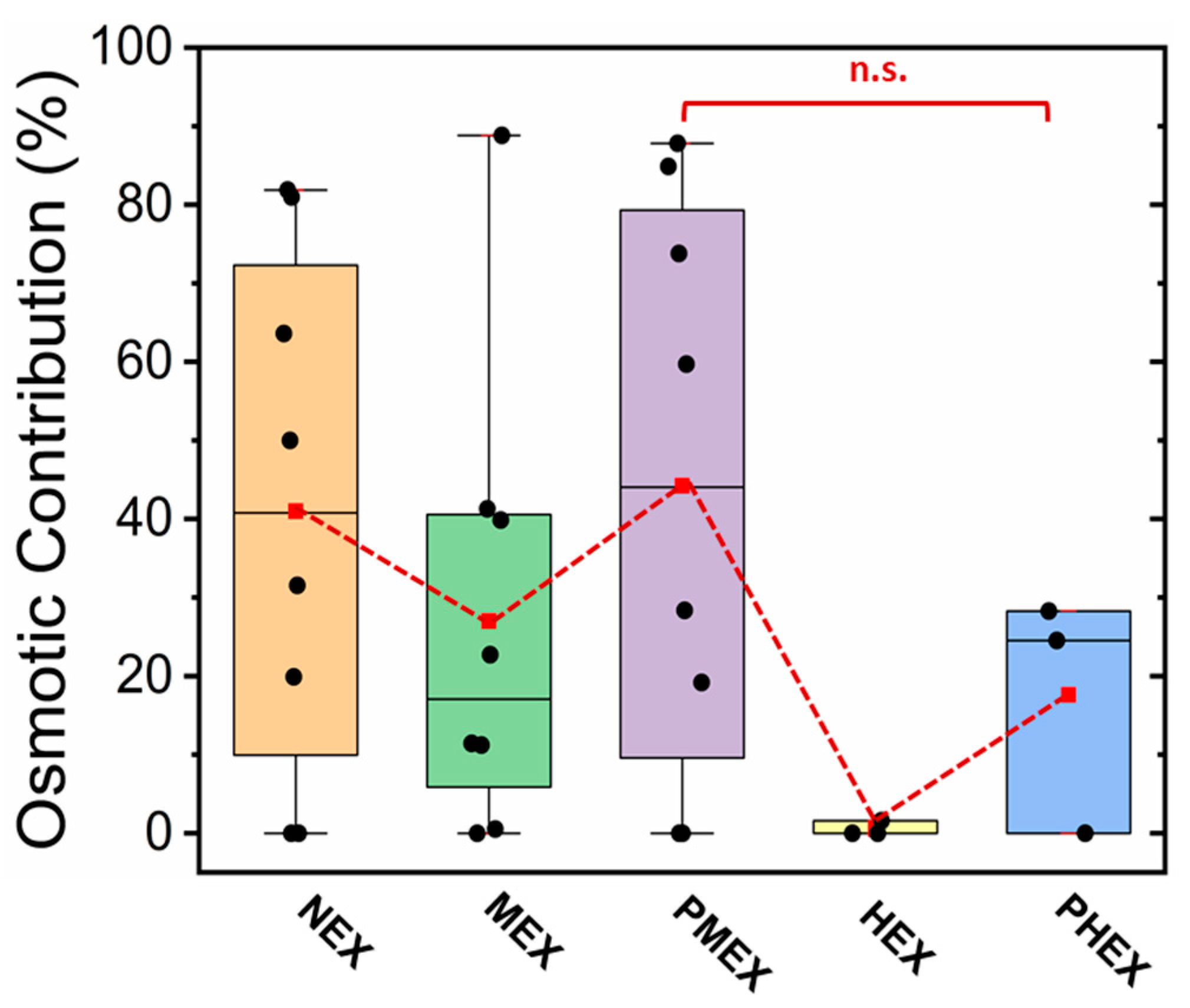
3.3. Working Mechanism of Different Pumping Materials on-skin toward the Sampling of Sweat Lactate
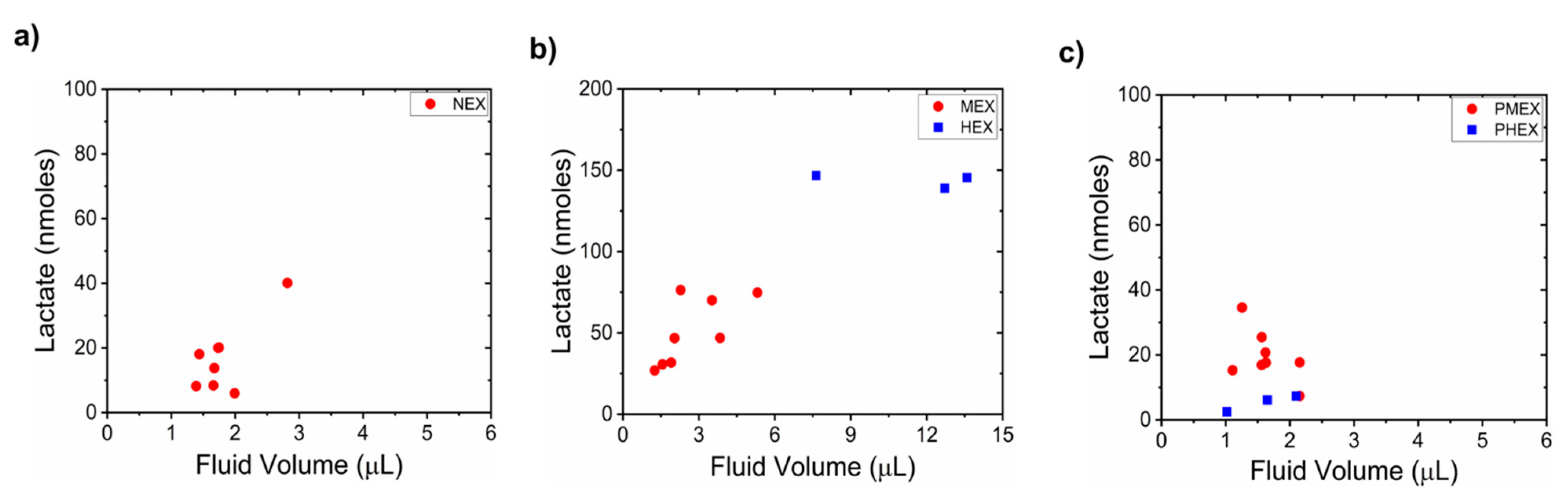
3.4. Relationship between Sweat Lactate and Sweat Volume
3.5. Estimation of Sweat Lactate Concentration and Its Relationship with Blood Lactate
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Karpova, E.V.; Laptev, A.I.; Andreev, E.A.; Karyakina, E.E.; Karyakin, A.A. Relationship Between Sweat and Blood Lactate Levels During Exhaustive Physical Exercise. ChemElectroChem 2020, 7, 191–194. [Google Scholar] [CrossRef]
- Bakker, J.; Nijsten, M.W.N.; Jansen, T.C. Clinical Use of Lactate Monitoring in Critically Ill Patients. Ann. Intensive Care 2013, 3, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alam, F.; RoyChoudhury, S.; Jalal, A.H.; Umasankar, Y.; Forouzanfar, S.; Akter, N.; Bhansali, S.; Pala, N. Lactate Biosensing: The Emerging Point-of-Care and Personal Health Monitoring. Biosens. Bioelectron. 2018, 117, 818–829. [Google Scholar] [CrossRef]
- Pundir, C.S.; Narwal, V.; Batra, B. Determination of Urea with Special Emphasis on Biosensors: A Review. Biosens. Bioelectron. 2016, 86, 777–790. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B. Physiology of Sweat Gland Function: The Roles of Sweating and Sweat Composition in Human Health. Temperature 2019, 6, 211–259. [Google Scholar] [CrossRef] [Green Version]
- Sonner, Z.; Wilder, E.; Heikenfeld, J.; Kasting, G.; Beyette, F.; Swaile, D.; Sherman, F.; Joyce, J.; Hagen, J.; Kelley-Loughnane, N.; et al. The Microfluidics of the Eccrine Sweat Gland, Including Biomarker Partitioning, Transport, and Biosensing Implications. Biomicrofluidics 2015, 9, 031301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, N.; Lähdesmäki, I.; Parviz, B.A. A Contact Lens with an Integrated Lactate Sensor. Sens. Actuators B Chem. 2012, 162, 128–134. [Google Scholar] [CrossRef]
- Kim, J.; Valdés-Ramírez, G.; Bandodkar, A.J.; Jia, W.; Martinez, A.G.; Ramírez, J.; Mercier, P.; Wang, J. Non-Invasive Mouthguard Biosensor for Continuous Salivary Monitoring of Metabolites. Analyst 2014, 139, 1632–1636. [Google Scholar] [CrossRef]
- Walenta, S.; Wetterling, M.; Lehrke, M.; Schwickert, G.; Sundfør, K.; Rofstad, E.K.; Mueller-Klieser, W. High Lactate Levels Predict Likelihood of Metastases, Tumor Recurrence, and Restricted Patient Survival in Human Cervical Cancers. Cancer Res. 2000, 60, 916–921. [Google Scholar] [PubMed]
- Cureton, E.L.; Kwan, R.O.; Dozier, K.C.; Sadjadi, J.; Pal, J.D.; Victorino, G.P. A Different View of Lactate in Trauma Patients: Protecting the Injured Brain. J. Surg. Res. 2010, 159, 468–473. [Google Scholar] [CrossRef]
- Derbyshire, P.J.; Barr, H.; Davis, F.; Higson, S.P.J. Lactate in Human Sweat: A Critical Review of Research to the Present Day. J. Physiol. Sci. 2012, 62, 429–440. [Google Scholar] [CrossRef]
- Anastasova, S.; Crewther, B.; Bembnowicz, P.; Curto, V.; Ip, H.M.; Rosa, B.; Yang, G. A Wearable Multisensing Patch for Continuous Sweat Monitoring. Biosens. Bioelectron. 2017, 93, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Mitsubayashi, K.; Suzuki, M.; Tamiya, E.; Karube, I. Analysis of Metabolites in Sweat as a Measure of Physical Condition. Anal. Chim. Acta 1994, 289, 27–34. [Google Scholar] [CrossRef]
- Saha, T.; Fang, J.; Mukherjee, S.; Dickey, M.D.; Velev, O.D. Wearable Osmotic-Capillary Patch for Prolonged Sweat Harvesting and Sensing. ACS Appl. Mater. Interfaces 2021, 13, 8071–8081. [Google Scholar] [CrossRef] [PubMed]
- Meyer, F.; Laitano, O.; Bar-Or, O.; McDougall, D.; Heingenhauser, G.J.F. Effect of Age and Gender on Sweat Lactate and Ammonia Concentrations during Exercise in the Heat. Braz. J. Med. Biol. Res. 2007, 40, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Fellmann, N.; Grizard, G.; Coudert, J. Human Frontal Sweat Rate and Lactate Concentration during Heat Exposure and Exercise. J. Appl. Physiol. 1983, 54, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Buono, M.J.; Lee, N.V.L.; Miller, P.W. The Relationship between Exercise Intensity and the Sweat Lactate Excretion Rate. J. Physiol. Sci. 2010, 60, 103–107. [Google Scholar] [CrossRef]
- Green, J.M.; Bishop, P.A.; Muir, I.H.; Lomax, R.G. Gender Differences in Sweat Lactate. Eur. J. Appl. Physiol. 2000, 82, 0230. [Google Scholar] [CrossRef]
- Patterson, M.J.; Galloway, S.D.R.; Nimmo, M.A. Variations in Regional Sweat Composition in Normal Human Males. Exp. Physiol. 2000, 85, 869–875. [Google Scholar] [CrossRef]
- Sakharov, D.A.; Shkurnikov, M.U.; Vagin, M.Y.; Yashina, E.I.; Karyakin, A.A.; Tonevitsky, A.G. Relationship between Lactate Concentrations in Active Muscle Sweat and Whole Blood. Bull. Exp. Biol. Med. 2010, 150, 83–85. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, M.L.; Harris, J.E.; Hernández, A.; Gladden, L.B. Blood Lactate Measurements and Analysis during Exercise: A Guide for Clinicians. J. Diabetes Sci. Technol. 2007, 1, 558–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koh, A.; Kang, D.; Xue, Y.; Lee, S.; Pielak, R.M.; Kim, J.; Hwang, T.; Min, S.; Banks, A.; Bastien, P.; et al. A Soft, Wearable Microfluidic Device for the Capture, Storage, and Colorimetric Sensing of Sweat. Sci. Transl. Med. 2016, 8, 366ra165. [Google Scholar] [CrossRef] [Green Version]
- Choi, J.; Kang, D.; Han, S.; Kim, S.B.; Rogers, J.A. Thin, Soft, Skin-Mounted Microfluidic Networks with Capillary Bursting Valves for Chrono-Sampling of Sweat. Adv. Healthc. Mater. 2017, 6, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Bandodkar, A.J.; Reeder, J.T.; Ray, T.R.; Turnquist, A.; Kim, S.B.; Nyberg, N.; Hourlier-Fargette, A.; Model, J.B.; Aranyosi, A.J.; et al. Soft, Skin-Integrated Multifunctional Microfluidic Systems for Accurate Colorimetric Analysis of Sweat Biomarkers and Temperature. ACS Sensors 2019, 4, 379–388. [Google Scholar] [CrossRef] [PubMed]
- Baysal, G.; Önder, S.; Göcek, İ.; Trabzon, L.; Kızıl, H.; Kök, F.N.; Kayaoğlu, B.K. Microfluidic Device on a Nonwoven Fabric: A Potential Biosensor for Lactate Detection. Text. Res. J. 2014, 84, 1729–1741. [Google Scholar] [CrossRef]
- Ashley, B.K.; Brown, M.S.; Park, Y.; Kuan, S.; Koh, A. Skin-Inspired, Open Mesh Electrochemical Sensors for Lactate and Oxygen Monitoring. Biosens. Bioelectron. 2019, 132, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Zhang, W.; Wang, Y.; Guan, R.; Liu, B.; Wang, X.; Sun, Z.; Xing, L.; Chen, S.; Xue, X. Self-Powered Wearable Athletics Monitoring Nanodevice Based on ZnO Nanowire Piezoelectric-Biosensing Unit Arrays. Sci. Adv. Mater. 2019, 11, 351–359. [Google Scholar] [CrossRef]
- Enomoto, K.; Shimizu, R.; Kudo, H. Real-Time Skin Lactic Acid Monitoring System for Assessment of Training Intensity. Electron. Commun. Japan 2018, 101, 41–46. [Google Scholar] [CrossRef]
- Payne, M.E.; Zamarayeva, A.; Pister, V.I.; Yamamoto, N.A.D.; Arias, A.C. Printed, Flexible Lactate Sensors: Design Considerations Before Performing On-Body Measurements. Sci. Rep. 2019, 9, 13720. [Google Scholar] [CrossRef]
- Onor, M.; Gufoni, S.; Lomonaco, T.; Ghimenti, S.; Salvo, P.; Sorrentino, F.; Bramanti, E. Potentiometric Sensor for Non Invasive Lactate Determination in Human Sweat. Anal. Chim. Acta 2017, 989, 80–87. [Google Scholar] [CrossRef]
- Weltin, A.; Kieninger, J.; Enderle, B.; Gellner, A.K.; Fritsch, B.; Urban, G.A. Polymer-Based, Flexible Glutamate and Lactate Microsensors for in Vivo Applications. Biosens. Bioelectron. 2014, 61, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Meyerhoff, C.; Bischof, F.; Mennel, F.J.; Sternberg, F.; Bican, J.; Pfeiffer, E.F. On Line Continuous Monitoring of Blood Lactate in Men by a Wearable Device Based upon an Enzymatic Amperometric Lactate Sensor. Biosens. Bioelectron. 1993, 8, 409–414. [Google Scholar] [CrossRef]
- Tur-García, E.L.; Davis, F.; Collyer, S.D.; Holmes, J.L.; Barr, H.; Higson, S.P.J. Novel Flexible Enzyme Laminate-Based Sensor for Analysis of Lactate in Sweat. Sens. Actuators B Chem. 2017, 242, 502–510. [Google Scholar] [CrossRef]
- Nagamine, K.; Mano, T.; Nomura, A.; Ichimura, Y.; Izawa, R.; Furusawa, H.; Matsui, H.; Kumaki, D.; Tokito, S. Noninvasive Sweat-Lactate Biosensor Emplsoying a Hydrogel-Based Touch Pad. Sci. Rep. 2019, 9, 10102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pribil, M.M.; Laptev, G.U.; Karyakina, E.E.; Karyakin, A.A. Noninvasive Hypoxia Monitor Based on Gene-Free Engineering of Lactate Oxidase for Analysis of Undiluted Sweat. Anal. Chem. 2014, 86, 5215–5219. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Wang, B.; Zhao, Y.; Shih, R.; Cheng, X.; Yu, W.; Hojaiji, H.; Lin, H.; Hoffman, C.; Ly, D.; et al. Natural Perspiration Sampling and in Situ Electrochemical Analysis with Hydrogel Micropatches for User-Identifiable and Wireless Chemo/Biosensing. ACS Sens. 2020, 5, 93–102. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Sempionatto, J.R.; Kim, J.; Jeong, Y.; Gu, J.; Wang, J.; Park, I. Microscale Biosensor Array Based on Flexible Polymeric Platform toward Lab-on-a-Needle: Real-Time Multiparameter Biomedical Assays on Curved Needle Surfaces. ACS Sens. 2020, 1–31. [Google Scholar] [CrossRef]
- Bariya, M.; Nyein, H.Y.Y.; Javey, A. Wearable Sweat Sensors. Nat. Electron. 2018, 1, 160–171. [Google Scholar] [CrossRef]
- Nie, Z.; Deiss, F.; Liu, X.; Akbulut, O.; Whitesides, G.M. Integration of Paper-Based Microfluidic Devices with Commercial Electrochemical Readers. Lab Chip 2010, 10, 3163–3169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, W.; Wang, C.; Wang, H.; Jian, M.; Lu, W.; Liang, X.; Zhang, X.; Yang, F.; Zhang, Y. Integrated Textile Sensor Patch for Real-Time and Multiplex Sweat Analysis. Sci. Adv. 2019, 5, eaax0649. [Google Scholar] [CrossRef] [Green Version]
- Sempionatto, J.R.; Nakagawa, T.; Pavinatto, A.; Mensah, S.T.; Imani, S.; Mercier, P.; Wang, J. Eyeglasses Based Wireless Electrolyte and Metabolite Sensor Platform. Lab Chip 2017, 17, 1834–1842. [Google Scholar] [CrossRef] [PubMed]
- Martín, A.; Kim, J.; Kurniawan, J.F.; Sempionatto, J.R.; Moreto, J.R.; Tang, G.; Campbell, A.S.; Shin, A.; Lee, M.Y.; Liu, X.; et al. Epidermal Microfluidic Electrochemical Detection System: Enhanced Sweat Sampling and Metabolite Detection. ACS Sens. 2017, 2, 1860–1868. [Google Scholar] [CrossRef] [PubMed]
- Bhide, A.; Cheeran, S.; Muthukumar, S.; Prasad, S. Enzymatic Low Volume Passive Sweat Based Assays for Multi-Biomarker Detection. Biosensors 2019, 9, 13. [Google Scholar] [CrossRef] [Green Version]
- Jia, W.; Bandodkar, A.J.; Valde, G.; Windmiller, J.R.; Yang, Z.; Ram, J.; Chan, G.; Wang, J. Electrochemical Tattoo Biosensors for Real-Time Noninvasive Lactate Monitoring in Human Perspiration. Anal. Chem. 2013, 85, 6553–6560. [Google Scholar] [CrossRef] [PubMed]
- Lamas-Ardisana, P.J.; Loaiza, O.A.; Añorga, L.; Jubete, E.; Borghei, M.; Ruiz, V.; Ochoteco, E.; Cabañero, G.; Grande, H.J. Disposable Amperometric Biosensor Based on Lactate Oxidase Immobilised on Platinum Nanoparticle-Decorated Carbon Nanofiber and Poly(Diallyldimethylammonium Chloride) Films. Biosens. Bioelectron. 2014, 56, 345–351. [Google Scholar] [CrossRef]
- Abrar, M.A.; Dong, Y.; Lee, P.K.; Kim, W.S. Bendable Electro-Chemical Lactate Sensor Printed with Silver Nano-Particles. Sci. Rep. 2016, 6, 30565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imani, S.; Bandodkar, A.J.; Mohan, A.M.V.; Kumar, R.; Yu, S.; Wang, J.; Mercier, P.P. A Wearable Chemical-Electrophysiological Hybrid Biosensing System for Real-Time Health and Fitness Monitoring. Nat. Commun. 2016, 7, 11650. [Google Scholar] [CrossRef] [PubMed]
- Guan, H.; Zhong, T.; He, H.; Zhao, T.; Xing, L.; Zhang, Y.; Xue, X. A Self-Powered Wearable Sweat-Evaporation-Biosensing Analyzer for Building Sports Big Data. Nano Energy 2019, 59, 754–761. [Google Scholar] [CrossRef]
- Rathee, K.; Dhull, V.; Dhull, R.; Singh, S. Biosensors Based on Electrochemical Lactate Detection: A Comprehensive Review. Biochem. Biophys. Rep. 2016, 5, 35–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, W.; Emaminejad, S.; Nyein, H.Y.Y.; Challa, S.; Chen, K.; Peck, A.; Fahad, H.M.; Ota, H.; Shiraki, H.; Kiriya, D.; et al. Fully Integrated Wearable Sensor Arrays for Multiplexed in Situ Perspiration Analysis. Nature 2016, 529, 509–514. [Google Scholar] [CrossRef] [Green Version]
- Luo, X.; Guo, L.; Liu, Y.; Shi, W.; Gai, W.; Cui, Y. Wearable Tape-Based Smart Biosensing Systems for Lactate and Glucose. IEEE Sens. J. 2020, 20, 3757–3765. [Google Scholar] [CrossRef]
- Roda, A.; Guardigli, M.; Calabria, D.; Maddalena Calabretta, M.; Cevenini, L.; Michelini, E. A 3D-Printed Device for a Smartphone-Based Chemiluminescence Biosensor for Lactate in Oral Fluid and Sweat. Analyst 2014, 139, 6494–6501. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-M.; Cheng, S.-B.; Ji, K.; Gao, J.; Liu, Y.-L.; Wen, W.; Zhang, X.; Wang, S.; Huang, W.-H. Construction of a Flexible Electrochemiluminescence Platform for Sweat Detection. Chem. Sci. 2019, 10, 6295–6303. [Google Scholar] [CrossRef] [Green Version]
- Yokus, M.A.; Songkakul, T.; Pozdin, V.A.; Bozkurt, A.; Daniele, M.A. Wearable Multiplexed Biosensor System toward Continuous Monitoring of Metabolites. Biosens. Bioelectron. 2020, 153, 112038. [Google Scholar] [CrossRef]
- Biagi, S.; Ghimenti, S.; Onor, M.; Bramanti, E. Simultaneous Determination of Lactate and Pyruvate in Human Sweat Using Reversed-Phase High-Performance Liquid Chromatography: A Noninvasive Approach. Biomed. Chromatogr. 2012, 26, 1408–1415. [Google Scholar] [CrossRef]
- Zhang, Y.; Tao, T.H. A Bioinspired Wireless Epidermal Photoreceptor for Artificial Skin Vision. Adv. Funct. Mater. 2020, 30, 2000381. [Google Scholar] [CrossRef]
- Souza, S.L.; Graça, G.; Oliva, A. Characterization of Sweat Induced with Pilocarpine, Physical Exercise, and Collected Passively by Metabolomic Analysis. Ski. Res. Technol. 2018, 24, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Bhide, A.; Lin, K.; Muthukumar, S.; Prasad, S. On-Demand Lactate Monitoring towards Assessing Physiological Responses in Sedentary Populations. Analyst 2021, 146, 3482–3492. [Google Scholar] [CrossRef] [PubMed]
- Shay, T.; Saha, T.; Dickey, M.D.; Velev, O.D. Principles of Long-Term Fluids Handling in Paper-Based Wearables with Capillary–Evaporative Transport. Biomicrofluidics 2020, 14, 034112. [Google Scholar] [CrossRef] [PubMed]
- Yokus, M.A.; Saha, T.; Fang, J.; Dickey, M.D.; Velev, O.D.; Daniele, M.A. Towards Wearable Electrochemical Lactate Sensing Using Osmotic-Capillary Microfluidic Pumping. In Proceedings of the 2019 IEEE Sensors, Montreal, QC, Canada, 27–30 October 2019; pp. 1–4. [Google Scholar]
- Klous, L.; de Ruiter, C.J.; Scherrer, S.; Gerrett, N.; Daanen, H.A.M. The (in)Dependency of Blood and Sweat Sodium, Chloride, Potassium, Ammonia, Lactate and Glucose Concentrations during Submaximal Exercise. Eur. J. Appl. Physiol. 2021, 121, 803–816. [Google Scholar] [CrossRef]
- Zhao, C.; Li, X.; Wu, Q.; Liu, X. A Thread-Based Wearable Sweat Nanobiosensor. Biosens. Bioelectron. 2021, 188, 113270. [Google Scholar] [CrossRef] [PubMed]
- Xuan, X.; Pérez-Ràfols, C.; Chen, C.; Cuartero, M.; Crespo, G.A. Lactate Biosensing for Reliable On-Body Sweat Analysis. ACS Sens. 2021, 6, 2763–2771. [Google Scholar] [CrossRef] [PubMed]
- Vinoth, R.; Nakagawa, T.; Mathiyarasu, J.; Mohan, A.M.V. Fully Printed Wearable Microfluidic Devices for High-Throughput Sweat Sampling and Multiplexed Electrochemical Analysis. ACS Sens. 2021, 6, 1174–1186. [Google Scholar] [CrossRef] [PubMed]
- Anderson, G.S.; Rhodes, E.C. A Review of Blood Lactate and Ventilatory Methods of Detecting Transition Thresholds. Sports Med. 1989, 8, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Green, J.M.; Pritchett, R.C.; Crews, T.R.; McLester, J.R.; Tucker, D.C. Sweat Lactate Response between Males with High and Low Aerobic Fitness. Eur. J. Appl. Physiol. 2004, 91, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Broskey, N.T.; Pories, W.J.; Jones, T.E.; Tanner, C.J.; Zheng, D.; Cortright, R.N.; Yang, Z.W.; Khang, N.; Yang, J.; Houmard, J.A.; et al. The Association between Lactate and Muscle Aerobic Substrate Oxidation: Is Lactate an Early Marker for Metabolic Disease in Healthy Subjects? Physiol. Rep. 2021, 9, e14729. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saha, T.; Fang, J.; Mukherjee, S.; Knisely, C.T.; Dickey, M.D.; Velev, O.D. Osmotically Enabled Wearable Patch for Sweat Harvesting and Lactate Quantification. Micromachines 2021, 12, 1513. https://doi.org/10.3390/mi12121513
Saha T, Fang J, Mukherjee S, Knisely CT, Dickey MD, Velev OD. Osmotically Enabled Wearable Patch for Sweat Harvesting and Lactate Quantification. Micromachines. 2021; 12(12):1513. https://doi.org/10.3390/mi12121513
Chicago/Turabian StyleSaha, Tamoghna, Jennifer Fang, Sneha Mukherjee, Charles T. Knisely, Michael D. Dickey, and Orlin D. Velev. 2021. "Osmotically Enabled Wearable Patch for Sweat Harvesting and Lactate Quantification" Micromachines 12, no. 12: 1513. https://doi.org/10.3390/mi12121513
APA StyleSaha, T., Fang, J., Mukherjee, S., Knisely, C. T., Dickey, M. D., & Velev, O. D. (2021). Osmotically Enabled Wearable Patch for Sweat Harvesting and Lactate Quantification. Micromachines, 12(12), 1513. https://doi.org/10.3390/mi12121513