Serum Magnesium Concentrations in the Canadian Population and Associations with Diabetes, Glycemic Regulation, and Insulin Resistance
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Design
2.2. Biochemical Measurements
2.3. Collection of Demographic Information
2.4. Calculations
2.5. Statistical Analyses
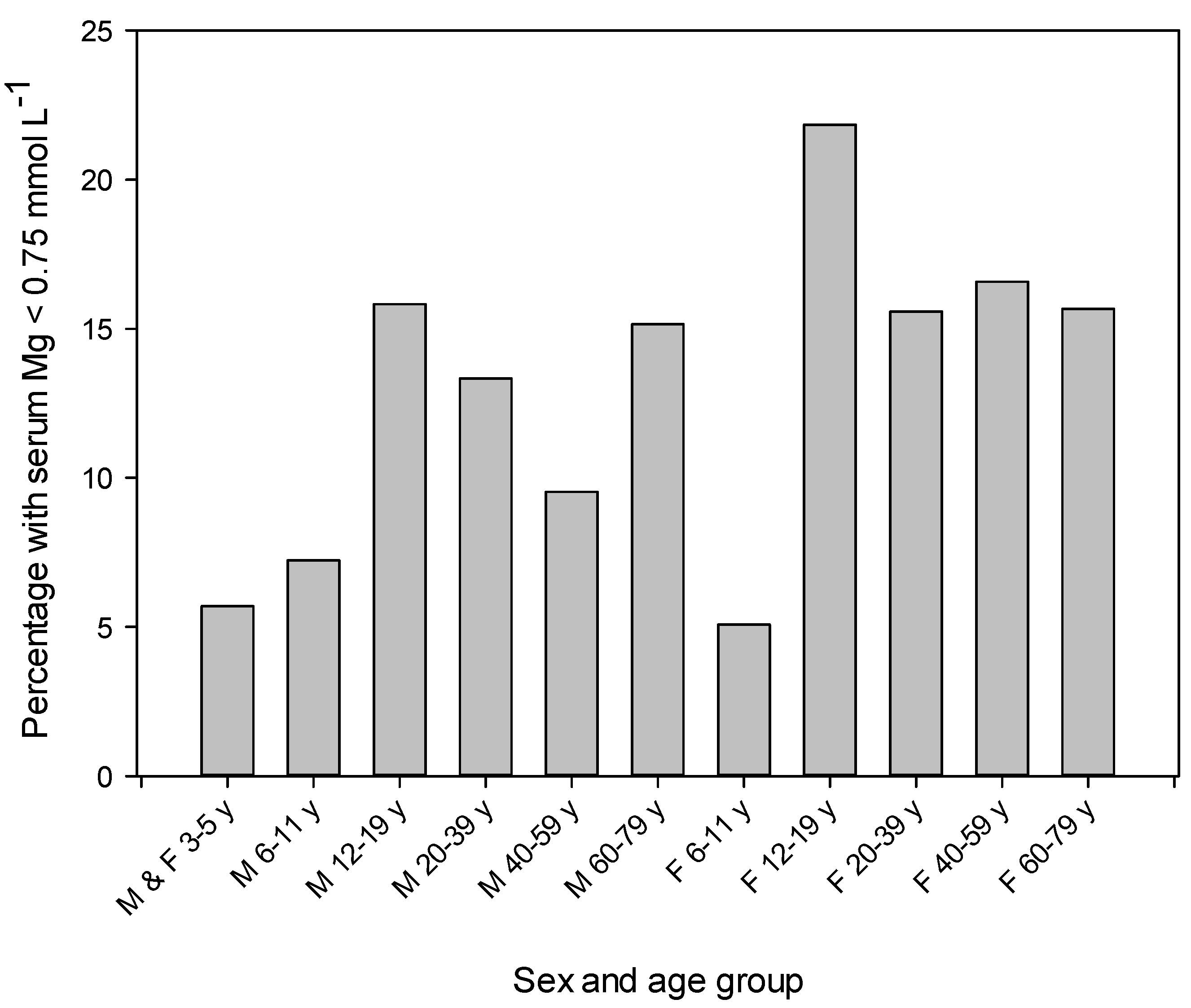
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Swaminathan, R. Magnesium metabolism and its disorders. Clin. Biochem. Rev. 2003, 24, 47–66. [Google Scholar] [PubMed]
- Volpe, S.L. Magnesium in disease prevention and overall health. Adv. Nutr. 2013, 4, 378S–383S. [Google Scholar] [CrossRef] [PubMed]
- Elin, R.J. Magnesium: The fifth but forgotten electrolyte. Am. J. Clin. Pathol. 1994, 102, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Wolf, F.I.; Cittadini, A. Magnesium in cell proliferation and differentiation. Front. Biosci. 1999, 4, D607–D617. [Google Scholar] [CrossRef] [PubMed]
- Moshfegh, A.; Goldman, J.D.; Ahuja, J.; Rhodes, D.; LaComb, R. What We Eat in America, NHANES 2005–2006: Usual Nutrient Intakes from Food and Water Compared to 1997 Dietary Reference Intakes for Vitamin D, Calcium, Phosphorus, and Magnesium; U.S. Department of Agriculture, Agriculture Research Service: Washington, DC, USA, 2009. [Google Scholar]
- Health Canada. Do Canadian Adults Meet Their Nutrient Requirements through Food Intake Alone? Available online: http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/art-nutr-adult-eng.php (accessed on 23 February 2017).
- Ford, E.S.; Mokdad, A.H. Dietary magnesium intake in a national sample of US adults. J. Nutr. 2003, 133, 2879–2882. [Google Scholar] [PubMed]
- Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride; National Academy Press: Washington, DC, USA, 1997; pp. 190–249. [Google Scholar]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific opinion on dietary reference values for magnesium. EFSA J. 2015, 13, 4186. [Google Scholar]
- Joint FAO/WHO Expert Consultation. Vitamin and Mineral Requirements in Human Nutrition: Report of a Joint FAO/WHO Expert Consultation, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Arnaud, M.J. Update on the assessment of magnesium status. Br. J. Nutr. 2008, 99, S24–S36. [Google Scholar] [CrossRef] [PubMed]
- Elin, R.J. Assessment of magnesium status for diagnosis and therapy. Magnes. Res. 2010, 23, S194–S198. [Google Scholar] [PubMed]
- Zhang, X.; Del Gobbo, L.C.; Hruby, A.; Rosanoff, A.; He, K.; Dai, Q.; Costello, R.B.; Zhang, W.; Song, Y. The circulating concentration and 24-h urine excretion of magnesium dose- and time-dependently respond to oral magnesium supplementation in a meta-analysis of randomized controlled trials. J. Nutr. 2016, 146, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Lowenstein, F.W.; Stanton, M.F. Serum magnesium levels in the United States, 1971–1974. J. Am. Coll. Nutr. 1986, 5, 399–414. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Folsom, A.R.; Melnick, S.L.; Eckfeldt, J.H.; Sharrett, A.R.; Nabulsi, A.A.; Hutchinson, R.G.; Metcalf, P.A. Associations of serum and dietary magnesium with cardiovascular disease, hypertension, diabetes, insulin, and carotid arterial wall thickness: The ARIC study. Atherosclerosis Risk in Communities Study. J. Clin. Epidemiol. 1995, 48, 927–940. [Google Scholar] [CrossRef]
- Zhang, X.; Li, Y.; Del Gobbo, L.C.; Rosanoff, A.; Wang, J.; Zhang, W.; Song, Y. Effects of magnesium supplementation on blood pressure: A meta-analysis of randomized double-blind placebo-controlled trials. Hypertension 2016, 68, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Kieboom, B.C.; Niemeijer, M.N.; Leening, M.J.; van den Berg, M.E.; Franco, O.H.; Deckers, J.W.; Hofman, A.; Zietse, R.; Stricker, B.H.; Hoorn, E.J. Serum magnesium and the risk of death from coronary heart disease and sudden cardiac death. J. Am. Heart Assoc. 2016, 5, e002707. [Google Scholar] [CrossRef] [PubMed]
- Peacock, J.M.; Ohira, T.; Post, W.; Sotoodehnia, N.; Rosamond, W.; Folsom, A.R. Serum magnesium and risk of sudden cardiac death in the Atherosclerosis Risk in Communities (ARIC) Study. Am. Heart J. 2010, 160, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Orchard, T.S.; Larson, J.C.; Alghothani, N.; Bout-Tabaku, S.; Cauley, J.A.; Chen, Z.; LaCroix, A.Z.; Wactawski-Wende, J.; Jackson, R.D. Magnesium intake, bone mineral density, and fractures: Results from the Women’s Health Initiative Observational study. Am. J. Clin. Nutr. 2014, 99, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Del Gobbo, L.C.; Imamura, F.; Wu, J.H.; de Oliveira Otto, M.C.; Chiuve, S.E.; Mozaffarian, D. Circulating and dietary magnesium and risk of cardiovascular disease: A systematic review and meta-analysis of prospective studies. Am. J. Clin. Nutr. 2013, 98, 160–173. [Google Scholar] [CrossRef] [PubMed]
- Qu, X.; Jin, F.; Hao, Y.; Li, H.; Tang, T.; Wang, H.; Yan, W.; Dai, K. Magnesium and the risk of cardiovascular events: A meta-analysis of prospective cohort studies. PLoS ONE 2013, 8, e57720. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.C.; Pang, Z.; Liu, Q.F. Magnesium intake and risk of colorectal cancer: A meta-analysis of prospective studies. Eur. J. Clin. Nutr. 2012, 66, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Qu, X.; Jin, F.; Hao, Y.; Zhu, Z.; Li, H.; Tang, T.; Dai, K. Nonlinear association between magnesium intake and the risk of colorectal cancer. Eur. J. Gastroenterol. Hepatol. 2013, 25, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Bertinato, J.; Lavergne, C.; Rahimi, S.; Rachid, H.; Vu, N.A.; Plouffe, L.J.; Swist, E. Moderately low magnesium intake impairs growth of lean body mass in obese-prone and obese-resistant rats fed a high-energy diet. Nutrients 2016, 8, 253. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Berton, L.; Carraro, S.; Bolzetta, F.; De Rui, M.; Perissinotto, E.; Toffanello, E.D.; Bano, G.; Pizzato, S.; Miotto, F.; et al. Effect of oral magnesium supplementation on physical performance in healthy elderly women involved in a weekly exercise program: A randomized controlled trial. Am. J. Clin. Nutr. 2014, 100, 974–981. [Google Scholar] [CrossRef] [PubMed]
- De Valk, H.W. Magnesium in diabetes mellitus. Neth. J. Med. 1999, 54, 139–146. [Google Scholar] [CrossRef]
- Pham, P.C.; Pham, P.M.; Pham, S.V.; Miller, J.M.; Pham, P.T. Hypomagnesemia in patients with type 2 diabetes. Clin. J. Am. Soc. Nephrol. 2007, 2, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Kao, W.H.; Folsom, A.R.; Nieto, F.J.; Mo, J.P.; Watson, R.L.; Brancati, F.L. Serum and dietary magnesium and the risk for type 2 diabetes mellitus: The Atherosclerosis Risk in Communities Study. Arch. Intern. Med. 1999, 159, 2151–2159. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Wolk, A. Magnesium intake and risk of type 2 diabetes: A meta-analysis. J. Intern. Med. 2007, 262, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Weng, L.C.; Lee, N.J.; Yeh, W.T.; Ho, L.T.; Pan, W.H. Lower intake of magnesium and dietary fiber increases the incidence of type 2 diabetes in Taiwanese. J. Formos. Med. Assoc. 2012, 111, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Gommers, L.M.; Hoenderop, J.G.; Bindels, R.J.; de Baaij, J.H. Hypomagnesemia in type 2 diabetes: A vicious circle? Diabetes 2016, 65, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Bertinato, J.; Xiao, C.W.; Ratnayake, W.M.; Fernandez, L.; Lavergne, C.; Wood, C.; Swist, E. Lower serum magnesium concentration is associated with diabetes, insulin resistance, and obesity in South Asian and white Canadian women but not men. Food Nutr. Res. 2015, 59, 25974. [Google Scholar] [CrossRef] [PubMed]
- Arpaci, D.; Tocoglu, A.G.; Ergenc, H.; Korkmaz, S.; Ucar, A.; Tamer, A. Associations of serum magnesium levels with diabetes mellitus and diabetic complications. Hippokratia 2015, 19, 153–157. [Google Scholar] [PubMed]
- Sinha, S.; Sen, S. Status of zinc and magnesium levels in type 2 diabetes mellitus and its relationship with glycemic status. Int. J. Diabetes Dev. Ctries. 2014, 34, 220–223. [Google Scholar] [CrossRef]
- Kim, D.J.; Xun, P.; Liu, K.; Loria, C.; Yokota, K.; Jacobs, D.R., Jr.; He, K. Magnesium intake in relation to systemic inflammation, insulin resistance, and the incidence of diabetes. Diabetes Care 2010, 33, 2604–2610. [Google Scholar] [CrossRef] [PubMed]
- Shields, M.; Carroll, M.D.; Ogden, C.L. Adult obesity prevalence in Canada and the United States. NCHS Data Brief 2011, 56, 1–8. [Google Scholar]
- Public Health Agency of Canada. Diabetes in Canada: Facts and Figures from a Public Health Perspective. Available online: http://www.phac-aspc.gc.ca/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres-2011/index-eng.php (accessed on 23 February 2017).
- Statistics Canada. Canadian Health Measures Survey (CHMS). Available online: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=136652 (accessed on 23 February 2017).
- Giroux, S. Canadian Health Measures Survey: Sampling strategy overview. Health Rep. 2007, 18, S31–S36. [Google Scholar]
- Statistics Canada. Canadian Health Measures Survey (CHMS) Data User Guide: Cycle 1. Available online: http://www23.statcan.gc.ca/imdb-bmdi/document/5071_D2_T1_V1-eng.htm (accessed on 23 February 2017).
- Kroll, M.H.; Elin, R.J. Relationships between magnesium and protein concentrations in serum. Clin. Chem. 1985, 31, 244–246. [Google Scholar] [PubMed]
- Seelig, M.S.; Preuss, H.G. Magnesium metabolism and perturbations in the elderly. Geriatr. Nephrol. Urol. 1994, 4, 101–111. [Google Scholar] [CrossRef]
- Barbagallo, M.; Belvedere, M.; Dominguez, L.J. Magnesium homeostasis and aging. Magnes. Res. 2009, 22, 235–246. [Google Scholar] [PubMed]
- DeFronzo, R.A.; Tobin, J.D.; Andres, R. Glucose clamp technique: A method for quantifying insulin secretion and resistance. Am. J. Physiol. 1979, 237, E214–E223. [Google Scholar] [PubMed]
- Singh, B.; Saxena, A. Surrogate markers of insulin resistance: A review. World J. Diabetes 2010, 1, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Olefsky, J.; Farquhar, J.W.; Reaven, G. Relationship between fasting plasma insulin level and resistance to insulin-mediated glucose uptake in normal and diabetic subjects. Diabetes 1973, 22, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Gutch, M.; Kumar, S.; Razi, S.M.; Gupta, K.K.; Gupta, A. Assessment of insulin sensitivity/resistance. Indian J. Endocrinol. Metab. 2015, 19, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Simental-Mendia, L.E.; Sahebkar, A.; Rodriguez-Moran, M.; Guerrero-Romero, F. A systematic review and meta-analysis of randomized controlled trials on the effects of magnesium supplementation on insulin sensitivity and glucose control. Pharmacol. Res. 2016, 111, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Watutantrige-Fernando, S.; Luchini, C.; Solmi, M.; Sartore, G.; Sergi, G.; Manzato, E.; Barbagallo, M.; Maggi, S.; Stubbs, B. Effect of magnesium supplementation on glucose metabolism in people with or at risk of diabetes: A systematic review and meta-analysis of double-blind randomized controlled trials. Eur. J. Clin. Nutr. 2016, 70, 1354–1359. [Google Scholar] [CrossRef] [PubMed]
- Zheltova, A.A.; Kharitonova, M.V.; Iezhitsa, I.N.; Spasov, A.A. Magnesium deficiency and oxidative stress: an update. BioMedicine 2016, 6, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Barbagallo, M.; Dominguez, L.J. Magnesium and type 2 diabetes. World J. Diabetes 2015, 6, 1152–1157. [Google Scholar] [CrossRef] [PubMed]
- Instructions for Use. VITROS Chemistry Products Mg Slides. Available online: https://www.cmmc.org/cmmclab/IFU/Mg_MP2-47_EN_I.pdf (accessed on 23 February 2017).
- Lakshmanan, F.L.; Rao, R.B.; Kim, W.W.; Kelsay, J.L. Magnesium intakes, balances, and blood levels of adults consuming self-selected diets. Am. J. Clin. Nutr. 1984, 40, 1380–1389. [Google Scholar] [PubMed]
- Misialek, J.R.; Lopez, F.L.; Lutsey, P.L.; Huxley, R.R.; Peacock, J.M.; Chen, L.Y.; Soliman, E.Z.; Agarwal, S.K.; Alonso, A. Serum and dietary magnesium and incidence of atrial fibrillation in whites and in African Americans: Atherosclerosis Risk in Communities (ARIC) Study. Circ. J. 2013, 77, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Bertinato, J.; Lavergne, C.; Plouffe, L.J.; El Niaj, H.A. Small increases in dietary calcium above normal requirements exacerbate magnesium deficiency in rats fed a low magnesium diet. Magnes. Res. 2014, 27, 35–47. [Google Scholar] [PubMed]
- Bertinato, J.; Plouffe, L.J.; Lavergne, C.; Ly, C. Bioavailability of magnesium from inorganic and organic compounds is similar in rats fed a high phytic acid diet. Magnes. Res. 2014, 27, 175–185. [Google Scholar] [PubMed]
- Klevay, L.M.; Milne, D.B. Low dietary magnesium increases supraventricular ectopy. Am. J. Clin. Nutr. 2002, 75, 550–554. [Google Scholar] [PubMed]
- Witkowski, M.; Hubert, J.; Mazur, A. Methods of assessment of magnesium status in humans: A systematic review. Magnes. Res. 2011, 24, 163–180. [Google Scholar] [PubMed]
- Song, Y.; He, K.; Levitan, E.B.; Manson, J.E.; Liu, S. Effects of oral magnesium supplementation on glycaemic control in type 2 diabetes: A meta-analysis of randomized double-blind controlled trials. Diabet. Med. 2006, 23, 1050–1056. [Google Scholar] [CrossRef] [PubMed]
- Costello, R.B.; Elin, R.J.; Rosanoff, A.; Wallace, T.C.; Guerrero-Romero, F.; Hruby, A.; Lutsey, P.L.; Nielsen, F.H.; Rodriguez-Moran, M.; Song, Y.; et al. Perspective: The case for an evidence-based reference interval for serum magnesium: the time has come. Adv. Nutr. 2016, 7, 977–993. [Google Scholar] [CrossRef] [PubMed]
| Sex and Age | n | Serum Magnesium | Distribution of Serum Magnesium Concentrations | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5th | 10th | 25th | 50th | 75th | 90th | 95th | |||||||||||
| Arithmetic Mean 1 | 95% CI | Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | ||
| mmol·L−1 | |||||||||||||||||
| All 2 | |||||||||||||||||
| 3–5 years | 505 | 0.83 | 0.82, 0.84 | 0.74 | 0.72, 0.76 | 0.76 | 0.74, 0.77 | 0.78 | 0.77, 0.80 | 0.82 | 0.80, 0.84 | 0.86 | 0.84, 0.88 | 0.90 | 0.87, 0.93 | 0.92 | 0.90, 0.95 |
| Male 3 | |||||||||||||||||
| 6–11 years | 493 | 0.83 a,* | 0.82, 0.84 | 0.73 | 0.71, 0.76 | 0.76 | 0.73, 0.78 | 0.79 | 0.78, 0.81 | 0.83 | 0.82, 0.84 | 0.86 | 0.85, 0.88 | 0.88 | 0.86, 0.91 | 0.91 | 0.88, 0.94 |
| 12–19 years | 490 | 0.80 c | 0.78, 0.81 | 0.71 | 0.68, 0.74 | 0.73 | 0.70, 0.75 | 0.76 | 0.72, 0.79 | 0.79 | 0.77, 0.81 | 0.83 | 0.80, 0.85 | 0.87 | 0.84, 0.89 | 0.88 | 0.87, 0.90 |
| 20–39 years | 510 | 0.81 b,c,* | 0.80, 0.82 | 0.69 | 0.64, 0.74 | 0.73 | 0.70, 0.76 | 0.77 | 0.74, 0.79 | 0.80 | 0.79, 0.82 | 0.84 | 0.83, 0.86 | 0.87 | 0.86, 0.89 | 0.90 | 0.87, 0.92 |
| 40–59 years | 538 | 0.82 a,b,* | 0.81, 0.83 | 0.71 | 0.68, 0.73 | 0.74 | 0.71, 0.77 | 0.78 | 0.76, 0.80 | 0.82 | 0.80, 0.84 | 0.86 | 0.84, 0.88 | 0.90 | 0.88, 0.92 | 0.91 | 0.88, 0.94 |
| 60–79 years | 509 | 0.81 b | 0.81, 0.82 | 0.69 | 0.67, 0.71 | 0.72 | 0.71, 0.74 | 0.77 | 0.75, 0.79 | 0.82 | 0.80, 0.84 | 0.86 | 0.84, 0.87 | 0.89 | 0.88, 0.91 | 0.91 | 0.89, 0.93 |
| Female 3 | |||||||||||||||||
| 6–11 years | 455 | 0.82 a | 0.81, 0.83 | 0.74 | 0.72, 0.76 | 0.75 | 0.73, 0.78 | 0.78 | 0.77, 0.80 | 0.82 | 0.80, 0.84 | 0.85 | 0.83, 0.86 | 0.88 | 0.86, 0.89 | 0.89 | 0.88, 0.90 |
| 12–19 years | 486 | 0.79 d | 0.78, 0.80 | 0.70 | 0.68, 0.72 | 0.72 | 0.70, 0.73 | 0.75 | 0.73, 0.77 | 0.78 | 0.77, 0.80 | 0.82 | 0.80, 0.83 | 0.86 | 0.84, 0.87 | 0.88 | 0.86, 0.90 |
| 20–39 years | 511 | 0.80 c,d | 0.79, 0.80 | 0.71 | 0.70, 0.72 | 0.73 | 0.71, 0.75 | 0.76 | 0.74, 0.78 | 0.79 | 0.77, 0.80 | 0.82 | 0.80, 0.84 | 0.85 | 0.82, 0.88 | 0.87 | 0.85, 0.89 |
| 40–59 years | 532 | 0.81 b,c | 0.80, 0.82 | 0.69 | 0.64, 0.74 | 0.72 | 0.69, 0.76 | 0.76 | 0.74, 0.78 | 0.81 | 0.79, 0.82 | 0.85 | 0.83, 0.87 | 0.88 | 0.86, 0.89 | 0.89 | 0.87, 0.92 |
| 60–79 years | 532 | 0.82 a,b | 0.81, 0.83 | 0.67 | 0.65, 0.69 | 0.71 | 0.69, 0.73 | 0.77 | 0.75, 0.79 | 0.82 | 0.80, 0.83 | 0.86 | 0.84, 0.88 | 0.90 | 0.88, 0.92 | 0.93 | 0.90, 0.97 |
| IV | Estimate (95% CI) 2,3 | Estimate (95% CI) 3,4 | p | Distribution of Continuous IV | |
|---|---|---|---|---|---|
| mmol·L−1 | 5th (95% CI ) | 95th (95% CI ) | |||
| Male 5 | 0.01 (0.00, 0.01) | - | <0.01 | - | - |
| White race 6 | −0.01 (−0.02, −0.00) | - | <0.001 | - | - |
| Diabetes 7 | −0.04 (−0.05, −0.02) | - | <0.001 | - | - |
| Age, year | 0.01 (0.01, 0.01) | 0.05 (0.04, 0.05) | <0.001 | 21.1 (18.3, 23.9) | 71.7 (70.1, 73.3) |
| BMI, kg·m−2 | −0.002 (−0.002, −0.001) | −0.03 (−0.03, −0.02) | <0.001 | 19.7 (19.1, 20.3) | 36.3 (34.7, 38.0) |
| Household income, K | 0.0005 (0.0001, 0.0008) | 0.01 (0.00, 0.01) | <0.01 | 15.0 (11.5, 18.5) | 196.7 (166.2, 227.2) |
| Serum albumin, g·L−1 | 0.002 (0.001, 0.003) | 0.02 (0.01, 0.03) | <0.001 | 37.8 (36.3, 39.3) | 48.9 (47.4, 50.5) |
| HbA1c, % | −0.01 (−0.02, −0.01 ) | −0.02 (−0.03, −0.02) | <0.001 | 4.8 (4.6, 5.0) | 6.5 (6.1, 6.9) |
| IV | Estimate (95% CI) 2,3 | Estimate (95% CI) 3,4 | p | Distribution of Continuous IV | |
|---|---|---|---|---|---|
| mmol·L−1 | 5th (95% CI ) | 95th (95% CI ) | |||
| Diabetes 5 | −0.06 (−0.07, −0.04) | - | <0.001 | - | - |
| Age, year | 0.01 (0.01, 0.01) | 0.04 (0.03, 0.05) | <0.001 | 20.6 (17.9, 23.3) | 70.8 (69.1, 72.4) |
| Household income, K | 0.0008 (0.0004, 0.0012) | 0.02 (0.01, 0.02) | <0.001 | 14.5 (10.3, 18.7) | 199.0 (162.5, 235.6) |
| Serum glucose, mmol·L−1 | −0.01 (−0.01, −0.00) | −0.01 (−0.02, −0.01) | <0.001 | 4.3 (4.1, 4.4) | 6.6 (5.9, 7.4) |
| Serum insulin, pmol·L−1 | −0.00008 (−0.00013, −0.00004) | −0.01 (−0.02, −0.00) | <0.001 | 25.1 (21.9, 28.2) | 180.1 (156.7, 203.4) |
| IV | Estimate (95% CI) 2,3 | Estimate (95% CI) 3,4 | p | Distribution of Continuous IV | |
|---|---|---|---|---|---|
| mmol·L−1 | 5th (95% CI ) | 95th (95% CI ) | |||
| Diabetes 5 | −0.07 (−0.08, −0.06) | - | <0.001 | - | - |
| Age, year | 0.01 (0.01, 0.01) | 0.04 (0.03, 0.05) | <0.001 | 20.6 (18.0, 23.3) | 70.8 (69.1, 72.5) |
| Household income, K | 0.0008 (0.0004, 0.0012) | 0.02 (0.01, 0.02) | <0.001 | 14.5 (10.3, 18.7) | 199.0 (162.0, 236.0) |
| HOMA-IR | −0.003 (−0.004, −0.002) | −0.02 (−0.02, −0.01) | <0.001 | 0.80 (0.67, 0.93) | 6.99 (6.34, 7.65) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertinato, J.; Wang, K.C.; Hayward, S. Serum Magnesium Concentrations in the Canadian Population and Associations with Diabetes, Glycemic Regulation, and Insulin Resistance. Nutrients 2017, 9, 296. https://doi.org/10.3390/nu9030296
Bertinato J, Wang KC, Hayward S. Serum Magnesium Concentrations in the Canadian Population and Associations with Diabetes, Glycemic Regulation, and Insulin Resistance. Nutrients. 2017; 9(3):296. https://doi.org/10.3390/nu9030296
Chicago/Turabian StyleBertinato, Jesse, Kuan Chiao Wang, and Stephen Hayward. 2017. "Serum Magnesium Concentrations in the Canadian Population and Associations with Diabetes, Glycemic Regulation, and Insulin Resistance" Nutrients 9, no. 3: 296. https://doi.org/10.3390/nu9030296
APA StyleBertinato, J., Wang, K. C., & Hayward, S. (2017). Serum Magnesium Concentrations in the Canadian Population and Associations with Diabetes, Glycemic Regulation, and Insulin Resistance. Nutrients, 9(3), 296. https://doi.org/10.3390/nu9030296




