Adding Agnus Castus and Magnolia to Soy Isoflavones Relieves Sleep Disturbances Besides Postmenopausal Vasomotor Symptoms-Long Term Safety and Effectiveness
Abstract
:1. Introduction
2. Materials and Methods
- Group 1: the ESP group (100 women) received one tablet/day containing SI 60 mg, Lactobacillus sporogenes 109 spores, Magnolia officinalis extract 50 mg, Vitex agnus-castus extract 40 mg and vitamin D 35 μg. This combination is commercially available in one tablet.
- Group 2: the C group (80 women) received one tablet/day containing only isoflavones 60 mg.
- (a)
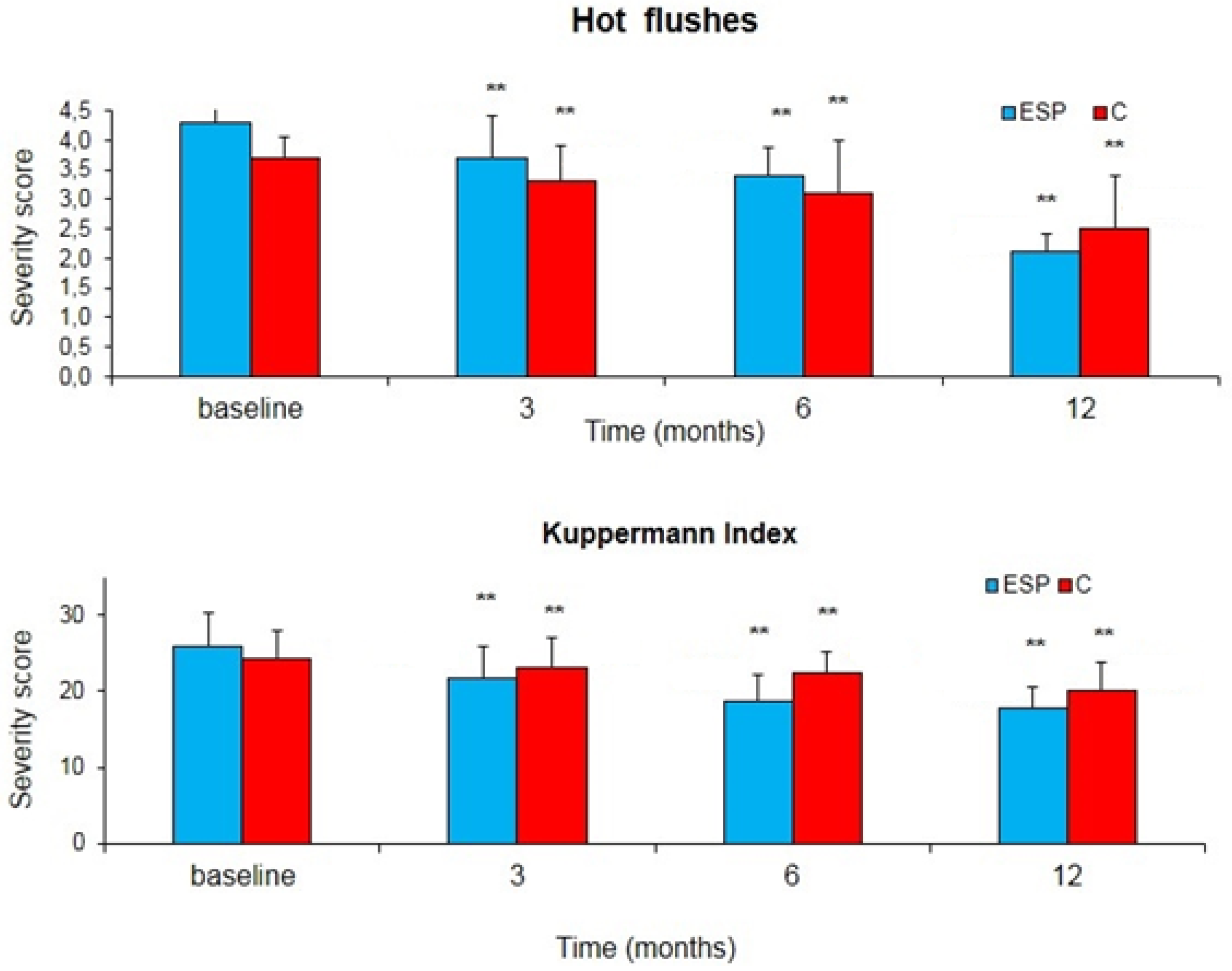
- The Kupperman index. The score is the result of a self-completed questionnaire that evaluates frequency and subjective intensity of 11 among the most frequent vasomotor symptoms in postmenopausal women (hot flushes, insomnia, irritability, sweating, musculoskeletal pains, headache, palpitations, fatigue, paresthesia). The symptoms were rated as mild (score 15–20), moderate (20–35), severe (>35). Number and daily intensity of hot flushes were recorded on a self-completed diary (0 = absent; 1 = mild; 2 = moderate; 3 = severe; 4 = very severe).
- (b)
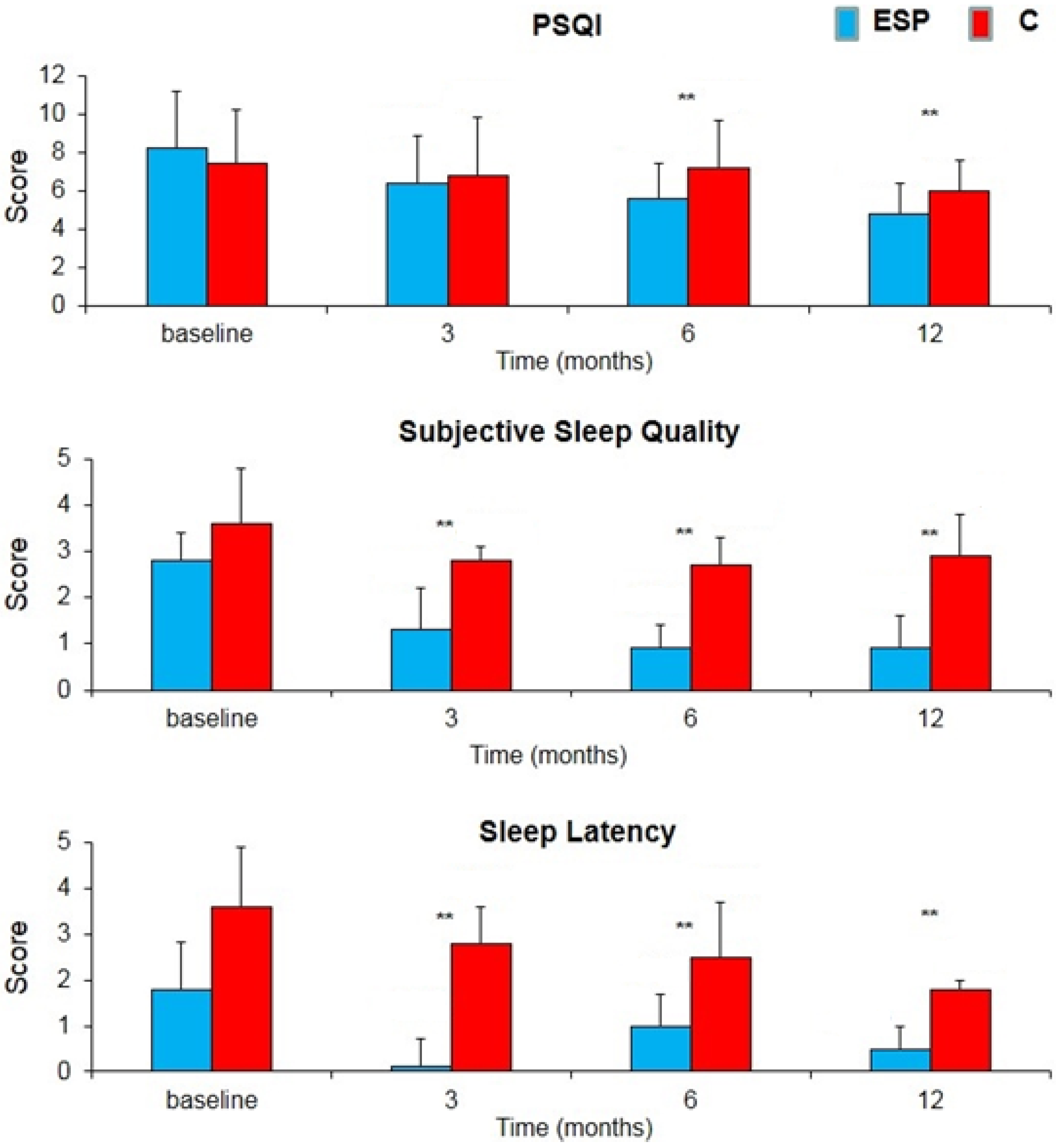
- The Pittsburgh Sleep Quality Index (PSQI) test for the evaluation of sleep disorders. It is a 19-item questionnaire regarding the last month’s symptomatology. The questionnaire generates seven composite scores, on a scale from 0 to 3; so the PSQI global score is from 0 to 21. Higher scores reflect more severe sleep disorders (the cut-off for sleep disturbances is a score of >5). The results give numbers in seven categories: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction (26).
- (c)
- Short Form 36 (SF-36). It is a test submitted at baseline and after one year to evaluate the psycho-physics wellness parameters. The SF-36 health survey consists of 36 questions evaluating functioning and well-being. Each of the questionnaire items refers to one of the following eight different health indicators: physical functioning; physical-role, referred to the limitations in performing relevant life roles due to physical health; bodily pain; general health; vitality; social functioning; limitations in performing relevant life roles due to emotional problems; mental health, referring to the absence of anxiety and depression. The test gives results in eight composite scores and a total score on a scale from 0 to 100. Lower scores show more severe impairment of psychophysics wellness parameters.
3. Results
4. Discussion
Author Contributions
Conflicts of Interest
References
- Bruyneel, M. Sleep disturbances in menopausal women: Aetiology and practical aspects. Maturitas 2015, 81, 406–409. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Lang, C.P. Examining the relationship between subjective sleep disturbance and menopause: A systematic review and meta-analysis. Menopause 2014, 21, 1301–1318. [Google Scholar] [CrossRef] [PubMed]
- North American Menopause Society. Estrogen and progestogen use in postmenopausal women: 2010 position statement of the North American Menopause Society. Menopause 2010, 17, 242–255. [Google Scholar]
- Nonhormonal management of menopause-associated vasomotor symptoms: 2015 position statement of the North American Menopause Society. Menopause 2015, 22, 1155.
- Rabin, D.S.; Cipparrone, N.; Linn, E.S.; Moen, M. Why menopausal women do not want to take hormone replacement therapy. Menopause 1999, 6, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Panay, N. Integrating phytoestrogens with prescription medicines—A conservative clinical approach to vasomotor symptom management. Maturitas 2007, 57, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Lethaby, A.; Marjoribanks, J.; Kronenberg, F.; Roberts, H.; Eden, J.; Brown, J. Phytoestrogens for vasomotor menopausal symptoms. Cochrane Database Syst. Rev. 2013, 12, CD001395. [Google Scholar] [CrossRef]
- Pino, A.M.; Valladares, L.E.; Palma, M.A.; Mancilla, A.M.; Yanez, M.; Albala, C. Dietary isoflavones affect sex hormone-binding globulin levels in postmenopausal women. J. Clin. Endocrinol. Metab. 2000, 85, 2797–2800. [Google Scholar] [CrossRef] [PubMed]
- Colacurci, N.; De Franciscis, P.; Atlante, M.; Mancino, P.; Monti, M.; Volpini, G.; Benvenuti, C. Endometrial, breast and liver safety of soy isoflavones plus Lactobacillus sporogenes in post-menopausal women. Gynecol. Endocrinol. 2013, 29, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.H.; Doerge, D.R.; Woodling, K.A.; Hartman, J.A.; Kwak, J.; Helferich, W.G. Dietary genistein negates the inhibitory effect of letrozole on the growth of aromatase-expressing estrogendependent human breast cancer cells (MCF-7Ca) in vivo. Carcinogenesis 2008, 29, 2162–2168. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.H.; Doerge, D.R.; Allred, K.F.; Allred, C.D.; Helferich, W.G. Dietary genistein negates the inhibitory effect of tamoxifen on growth of estrogen-dependent human breast cancer (MCF-7) cells implanted in athymic mice. Cancer Res. 2002, 62, 2474–2477. [Google Scholar] [PubMed]
- Eichling, P.S.; Sahni, J. Menopause related sleep disorders. J. Clin. Sleep Med. 2005, 1, 293–300. [Google Scholar]
- Owens, J.F.; Matthews, K.A. Sleep disturbance in healthy middle-aged women. Maturitas 1998, 30, 41–50. [Google Scholar] [CrossRef]
- Boulet, M.J.; Oddens, B.J.; Lehert, P.; Vemer, H.M.; Visser, A. Climacteric and menopause in seven South-east Asian countries. Maturitas 1994, 19, 157–176. [Google Scholar] [CrossRef]
- Jacobs, A.; Wegewitz, U.; Sommerfeld, C.; Grossklaus, R.; Lampen, A. Efficacy of isoflavones in relieving vasomotor menopausal symptoms—A systematic review. Mol. Nutr. Food Res. 2009, 53, 1084–1097. [Google Scholar] [CrossRef] [PubMed]
- Hachul, H.; Brandao, L.C.; D’Almeida, V.; Bittencourt, L.R.; Baracat, E.C.; Tufik, S. Isoflavones decrease insomnia in postmenopause. Menopause 2011, 18, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Schellenberg, R. Treatment for the premenstrual syndrome with agnus castus fruit extract: Prospective, randomised, placebo controlled study. BMJ 2001, 322, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Yamasaki, T.; Konoshita, M.; Ikeda, T.; Okawa, M.; Kinjo, J.; Yoshimitsu, H.; Nohara, T. Five new diterpenoids, viteagnusins A-E, from the fruit of Vitex agnus-castus. Chem. Pharm. Bull. 2008, 56, 1621–1624. [Google Scholar] [CrossRef] [PubMed]
- Costa, M.R.; Ribeiro, C.G.; Santos-Filho, S.D.; Neves, R.F.; Fonseca, A.S.; Bernardo-Filho, M.; de Almeida Catanho, M.T.J. An aqueous extract of Vitex agnus-castus alters the labeling of blood constituents with Technetium-99m. Braz. Arch. Biol. Technol. 2007, 50, 183–188. [Google Scholar] [CrossRef]
- Azarnia, M.; Ejtemaei-Mehr, S.; Shakoor, A.; Ansari, A. Effects of Vitex agnus-castus on mice fetus development. Acta Med. Iran. 2007, 45, 264–270. [Google Scholar]
- Carmichael, A.R. Can Vitex agnus-castus be used for the treatment of mastalgia? What is the current evidence? Evid. Based Complement. Altern. Med. 2008, 5, 247–250. [Google Scholar] [CrossRef] [PubMed]
- Dugoua, J.J.; Seely, D.; Perri, D.; Koren, G.; Mills, E. Safety and efficacy of chaste tree (Vitex agnus-castus) during pregnancy and lactation. Can. J. Clin. Pharmacol. 2008, 15, e74–e79. [Google Scholar] [PubMed]
- Zeraati, F.; Shobeiri, F.; Nazari, M.; Araghchian, M.; Bekhradi, R. Comparative evaluation of the efficacy of herbal drugs (fennelin and vitagnus) and mefenamic acid in the treatment of primary dysmenorrhea. Iran. J. Nurs. Midwifery Res. 2014, 19, 581–584. [Google Scholar] [PubMed]
- Golian Tehrani, S.; Bazzazian, S.; Bakhtiarian, A.; Ghobadzadeh, M. Effects of calci soya balance and vitagnus on menopausal symptoms. Iran. Red Crescent Med. J. 2014, 16, 13651. [Google Scholar] [CrossRef] [PubMed]
- Kuribara, H.; Kishi, E.; Hattori, N.; Okada, M.; Maruyana, Y. The anxiolytic effect of two oriental herbal drugs in japan attributed to honokiol from magnolia bark. J. Pharm. Pharmacol. 2000, 52, 1425–1429. [Google Scholar] [CrossRef] [PubMed]
- Mucci, M.; Carraro, C.; Mancino, P.; Monti, M.; Papadia, L.S.; Volpini, G.; Benvenuti, C. Soy isoflavones, lactobacilli, Magnolia bark extract, Vitamin D3 and calcium. Controlled clinical study in menopause. Minerva Ginecol. 2006, 58, 323–334. [Google Scholar] [PubMed]
- Van Die, M.D.; Burger, H.G.; Teede, H.J.; Bone, K.M. Vitex agnus-castus (Chaste-Tree/Berry) in the treatment of menopause-related complaints. J. Altern. Complement. Med. 2009, 15, 853–862. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, P.J.; Roca, C.A.; Bloch, M.; Rubinow, D.R. The perimenopause and affective disorders. Semin. Reprod. Endocrinol. 1997, 15, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Kuribara, H.; Stavinoha, W.B.; Maruyama, Y. Behavioural pharmacological characteristics of honokiol, an anxiolytic agent present in extracts of Magnolia bark, evaluated by an elevated plus-maze test in mice. J. Pharm. Pharmacol. 1998, 50, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Kuribara, H.; Stavinoha, W.B.; Maruyama, Y. Honokiol, a putative anxiolytic agent extracted from magnolia bark, has no diazepam-like side-effects in mice. J. Pharm. Pharmacol. 1999, 51, 97–103. [Google Scholar] [PubMed]
- Rekha, C.R.; Vijayalakshmi, G. Isoflavone phytoestrogens in soymilk fermented with β-glucosidase producing probiotic lactic acid bacteria. Int. J. Food Sci. Nutr. 2011, 62, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.K.; Shah, N.P. Enhancing the biotransformation of isoflavones in soymilk supplemented with lactose using probiotic bacteria during extended fermentation. J. Food Sci. 2010, 75, M140–M149. [Google Scholar] [CrossRef] [PubMed]
- Izumi, T.; Pistula, M.K.; Osawa, S.; Obata, A.; Tobe, K.; Saito, M.; Kataoka, S.; Kubota, Y.; Kikuchi, M. Soy isoflavonesaglycones are absorbed faster and in higher amounts than their glucosides in humans. J. Nutr. 2000, 130, 1695–1699. [Google Scholar] [PubMed]
- Boriello, S.P.; Setchell, K.D.R.; Axelson, M.; Lawson, A.M. Production and metabolism of lignans by the human faecal flora. J. Appl. Bacteriol. 1985, 58, 37–43. [Google Scholar] [CrossRef]
- Messina, M. Investigating the optimal soy protein and isoflavone intakes for women: A perspective. Womens Health 2008, 4, 337–356. [Google Scholar] [CrossRef] [PubMed]
- Nettleton, J.A.; Greany, K.A.; Thomas, W.; Wangen, K.E.; Adlercreutz, H.; Kurzer, M.S. The effect of soy consumption on the urinary 2:16-hydroxyestrone ratio in postmenopausal women depends on equol production status but is not influenced by probiotic consumption. J. Nutr. 2005, 135, 603–608. [Google Scholar] [PubMed]
| ESP Group | C Group | |
|---|---|---|
| Age (Years) | 55.0 ± 6.4 | 56.0 ± 5.8 |
| BMI | 24.9 ± 2.9 | 25.7 ± 4.3 |
| Period of Amenorrhea (Years) | 3.2 ± 0.8 | 2.6 ± 0.4 |
| Group ESP (n = 100) | Group C (n = 80) | |||
|---|---|---|---|---|
| Baseline | 12 Months | Baseline | 12 Months | |
| Mammographic density (%) | 1.80 ± 0.7 * | 1.86 ± 0.8 ** | 1.75 ± 0.7 * | 1.79 ± 0.6 ** |
| Endometrial thickness (mm) | 3.4 ± 0.9 * | 3.2 ± 0.6 ** | 3.8 ± 1.2 * | 3.3 ± 1.1 ** |
| ALT (UI/L) | 18.7 ± 6.5 * | 20.2 ± 4.2 ** | 19.7 ± 2.6 * | 21.3 ± 3.8 ** |
| AST (UI/L) | 21.4 ± 5.3 * | 20.3 ± 6.2 ** | 19.2 ± 4.6 * | 19.8 ± 3.4 ** |
| γGT (UI/L) | 24.3 ± 15.6 * | 22.6 ± 19.3 ** | 20.4 ± 17.3 * | 24.8 ± 18.2 ** |
| Bilirubin (mg/dL) | 0.46 ± 0.22 * | 0.40 ± 0.26 ** | 0.48 ± 0.34 * | 0.42 ± 0.23 ** |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Franciscis, P.; Grauso, F.; Luisi, A.; Schettino, M.T.; Torella, M.; Colacurci, N. Adding Agnus Castus and Magnolia to Soy Isoflavones Relieves Sleep Disturbances Besides Postmenopausal Vasomotor Symptoms-Long Term Safety and Effectiveness. Nutrients 2017, 9, 129. https://doi.org/10.3390/nu9020129
De Franciscis P, Grauso F, Luisi A, Schettino MT, Torella M, Colacurci N. Adding Agnus Castus and Magnolia to Soy Isoflavones Relieves Sleep Disturbances Besides Postmenopausal Vasomotor Symptoms-Long Term Safety and Effectiveness. Nutrients. 2017; 9(2):129. https://doi.org/10.3390/nu9020129
Chicago/Turabian StyleDe Franciscis, Pasquale, Flavio Grauso, Anna Luisi, Maria Teresa Schettino, Marco Torella, and Nicola Colacurci. 2017. "Adding Agnus Castus and Magnolia to Soy Isoflavones Relieves Sleep Disturbances Besides Postmenopausal Vasomotor Symptoms-Long Term Safety and Effectiveness" Nutrients 9, no. 2: 129. https://doi.org/10.3390/nu9020129
APA StyleDe Franciscis, P., Grauso, F., Luisi, A., Schettino, M. T., Torella, M., & Colacurci, N. (2017). Adding Agnus Castus and Magnolia to Soy Isoflavones Relieves Sleep Disturbances Besides Postmenopausal Vasomotor Symptoms-Long Term Safety and Effectiveness. Nutrients, 9(2), 129. https://doi.org/10.3390/nu9020129





