Maternal Iodine Intake and Offspring Attention-Deficit/Hyperactivity Disorder: Results from a Large Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
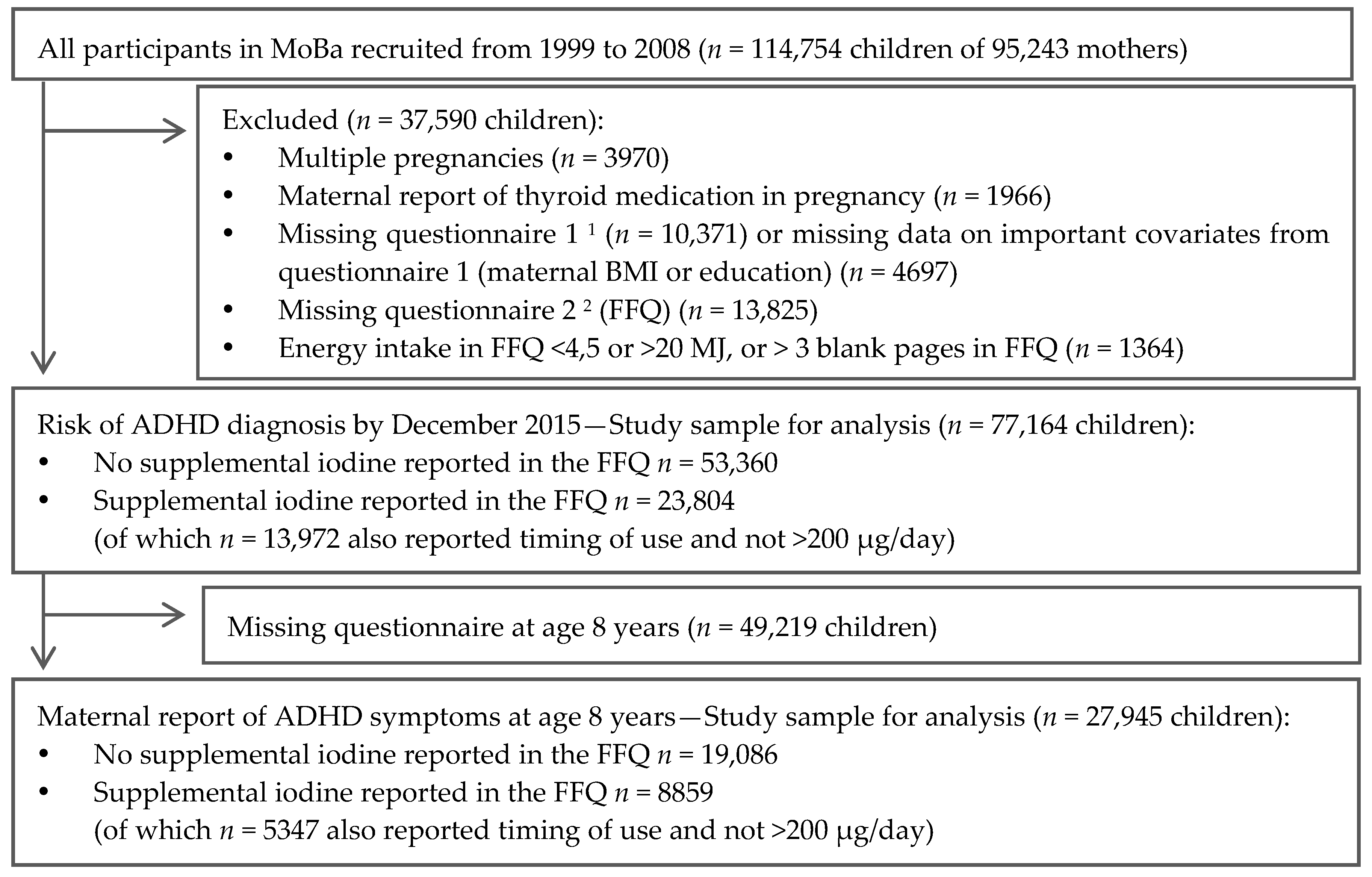
2.1. Subjects and Design
2.2. Exposure Variables—Iodine Intake from Food and Supplements
2.3. ADHD Diagnosis
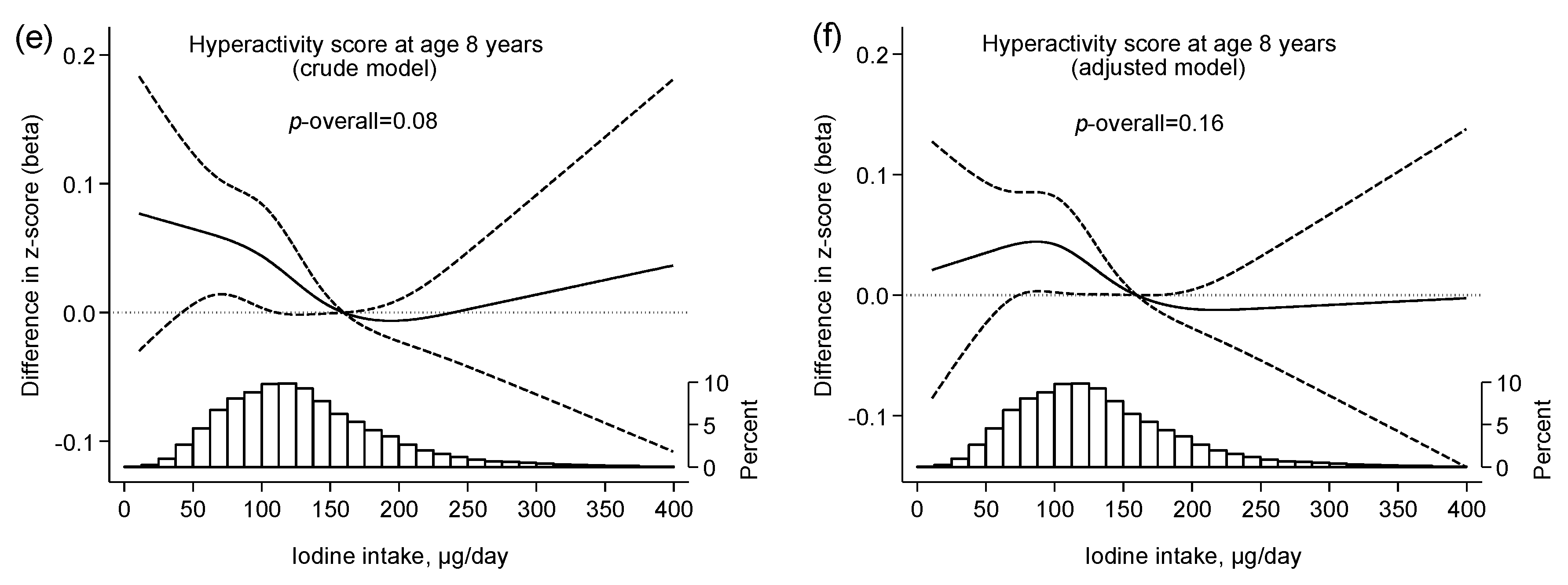
2.4. ADHD Symptom Score
2.5. Covariates
2.6. Ethics
2.7. Statistics
3. Results
3.1. Background Characteristics
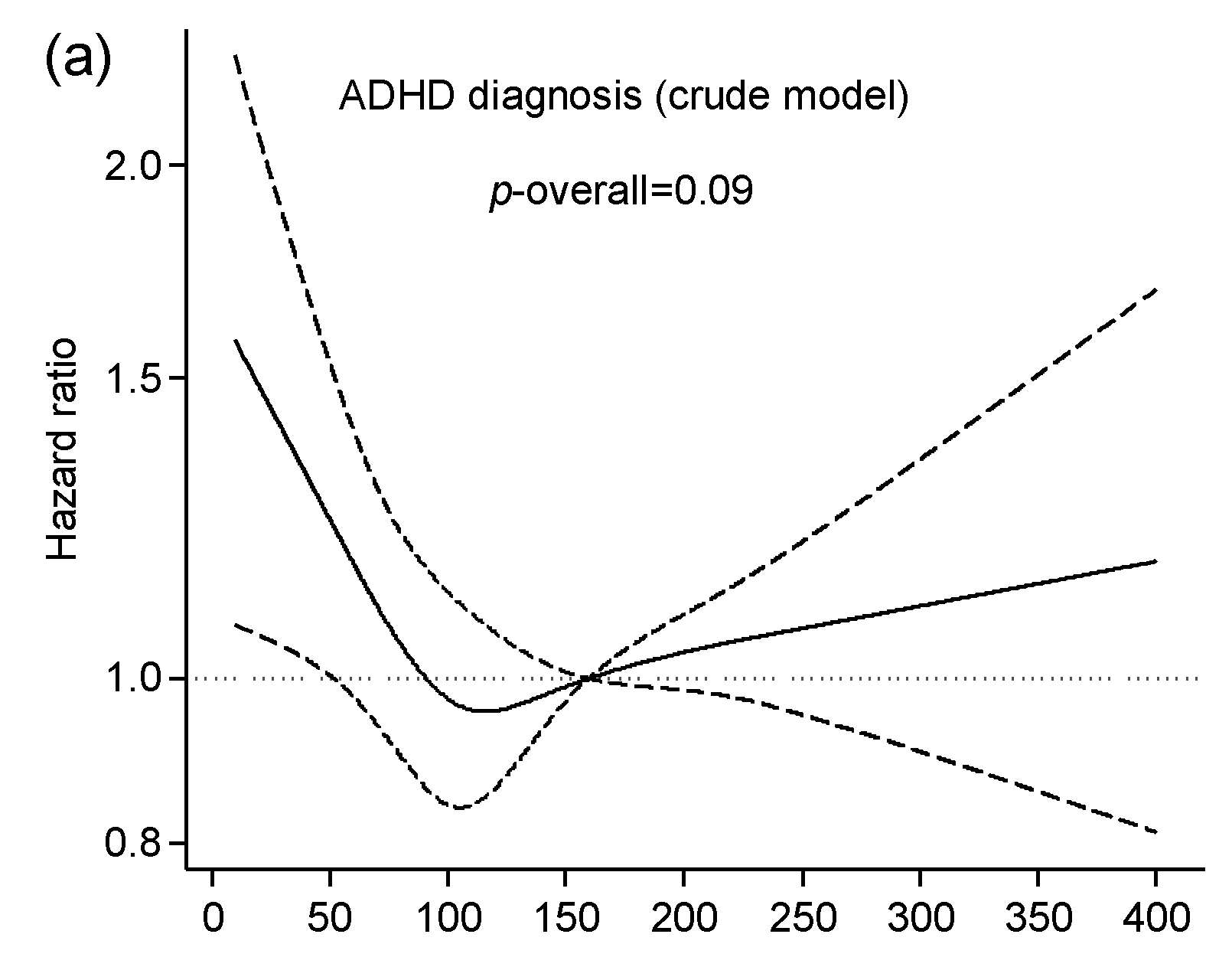
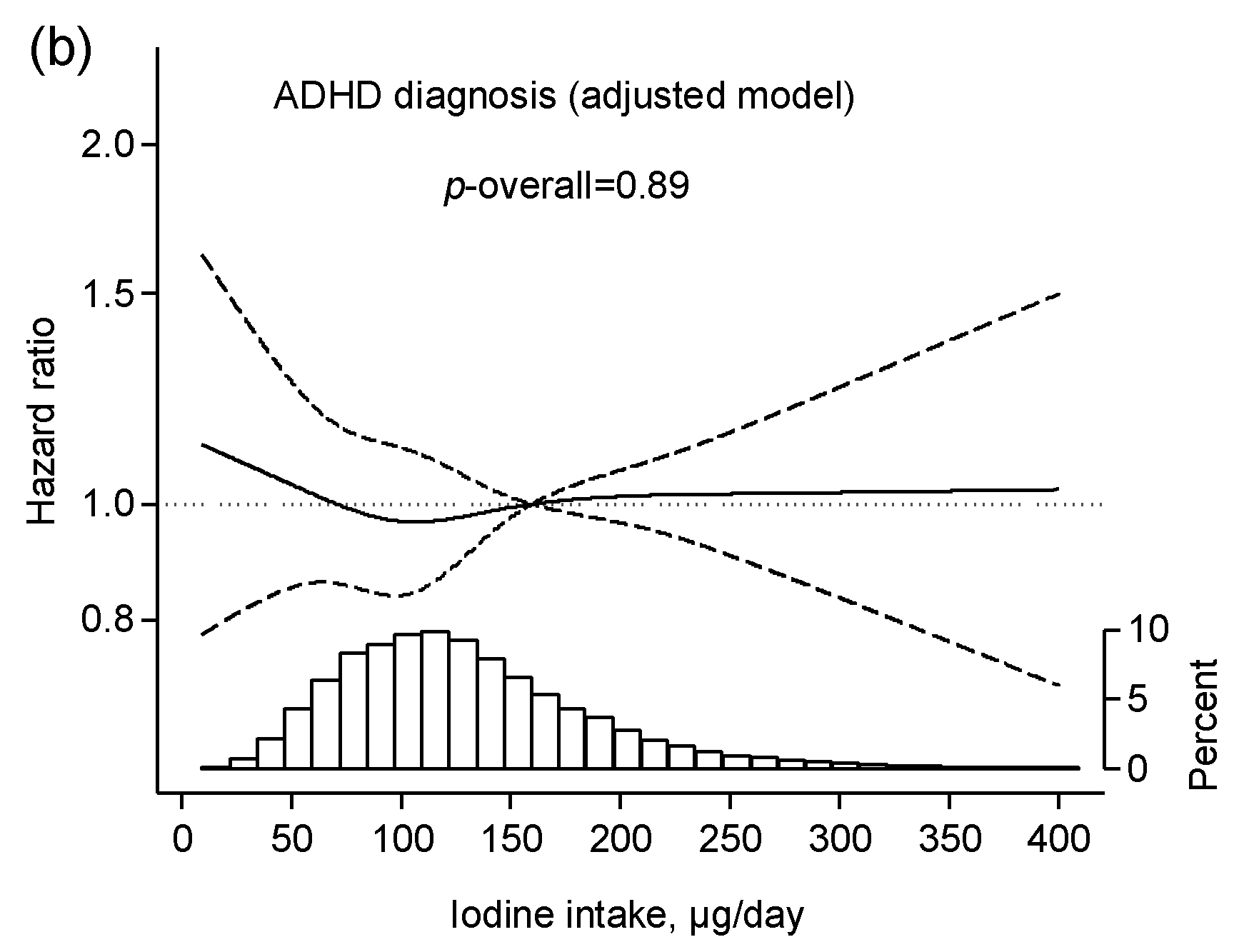
3.2. Iodine Intake from Food and Risk of ADHD
3.3. Iodine Intake from Supplements and Risk of ADHD
4. Discussion
4.1. Iodine from Food and ADHD
4.2. Iodine from Supplements and ADHD
4.3. Strengths and Limitations
4.4. Clinical Relevance and Implications
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ADHD | Attention-deficit/hyperactivity disorder |
| DSM | The diagnostic and statistical manual of mental disorders |
| EAR | Estimated average requirement |
| FFQ | Food frequency questionnaire |
| GW | Gestational week |
| HKD | Hyperkinetic disorder |
| ICD | International Classification of Disease |
| ID | Iodine deficiency |
| IQ | Intelligence quotient |
| MoBa | The Norwegian Mother and Child Cohort Study |
| NPR | Norwegian Patient Registry |
| UIC | Urinary iodine concentration |
References
- World Health Organization; United Nations Children’s Fund; International Council for Control of Iodine Deficiency Disorders. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Redman, K.; Ruffman, T.; Fitzgerald, P.; Skeaff, S. Iodine deficiency and the brain: Effects and mechanisms. Crit. Rev. Food Sci. Nutr. 2016, 56, 2695–2713. [Google Scholar] [CrossRef] [PubMed]
- Pearce, E.N.; Lazarus, J.H.; Moreno-Reyes, R.; Zimmermann, M.B. Consequences of iodine deficiency and excess in pregnant women: An overview of current knowns and unknowns. Am. J. Clin. Nutr. 2016, 104, 918S–923S. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.; Sanders, S.; Doust, J.; Beller, E.; Glasziou, P. Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics 2015, 135, e994–e1001. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Spencer, T.J.; Biederman, J.; Mick, E. Attention-deficit/hyperactivity disorder: Diagnosis, lifespan, comorbidities, and neurobiology. Ambul. Pediatr. 2007, 7, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Thapar, A.; Cooper, M.; Eyre, O.; Langley, K. Practitioner review: What have we learnt about the causes of ADHD? J. Child Psychol. Psychiatry 2013, 54, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Larsson, H.; Chang, Z.; D’Onofrio, B.M.; Lichtenstein, P. The heritability of clinically diagnosed attention deficit hyperactivity disorder across the lifespan. Psychol. Med. 2014, 44, 2223–2229. [Google Scholar] [CrossRef] [PubMed]
- Vermiglio, F.; Lo Presti, V.P.; Moleti, M.; Sidoti, M.; Tortorella, G.; Scaffidi, G.; Castagna, M.G.; Mattina, F.; Violi, M.A.; Crisa, A.; et al. Attention deficit and hyperactivity disorders in the offspring of mothers exposed to mild-moderate iodine deficiency: A possible novel iodine deficiency disorder in developed countries. J. Clin. Endocrinol. Metab. 2004, 89, 6054–6060. [Google Scholar] [CrossRef] [PubMed]
- Van Mil, N.H.; Tiemeier, H.; Bongers-Schokking, J.J.; Ghassabian, A.; Hofman, A.; Hooijkaas, H.; Jaddoe, V.W.; de Muinck Keizer-Schrama, S.M.; Steegers, E.A.; Visser, T.J.; et al. Low urinary iodine excretion during early pregnancy is associated with alterations in executive functioning in children. J. Nutr. 2012, 142, 2167–2174. [Google Scholar] [CrossRef] [PubMed]
- Zhukov, A.O. Mental development disorders and attention-deficit syndrome caused by iodine deficiency: A clinical and epidemiological study. Zh. Nevrol. Psikhiatr. Im. S. S. Korsakova 2007, 107, 4–16. [Google Scholar] [PubMed]
- Abel, M.H.; Caspersen, I.H.; Meltzer, H.M.; Haugen, M.; Brandlistuen, R.E.; Aase, H.; Alexander, J.; Torheim, L.E.; Brantsaeter, A.L. Suboptimal maternal iodine intake is associated with impaired child neurodevelopment at 3 years of age in the Norwegian mother and child cohort study. J. Nutr. 2017, 147, 1314–1324. [Google Scholar] [CrossRef] [PubMed]
- Magnus, P.; Birke, C.; Vejrup, K.; Haugan, A.; Alsaker, E.; Daltveit, A.K.; Handal, M.; Haugen, M.; Hoiseth, G.; Knudsen, G.P.; et al. Cohort profile update: The Norwegian mother and child cohort study (Moba). Int. J. Epidemiol. 2016, 45, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Irgens, L.M. The medical birth registry of Norway. Epidemiological research and surveillance throughout 30 years. Acta Obstet. Gynecol. Scand. 2000, 79, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, H.M.; Brantsaeter, A.L.; Ydersbond, T.A.; Alexander, J.; Haugen, M. Methodological challenges when monitoring the diet of pregnant women in a large study: Experiences from the Norwegian mother and child cohort study (Moba). Matern. Child Nutr. 2008, 4, 14–27. [Google Scholar] [CrossRef] [PubMed]
- Norwegian Institute of Public Health Website. MoBa Food Frequency Questionnaire (English Translation). Available online: http://www.webcitation.org/6u5JMPcZg (accessed on 9 October 2017).
- Dahl, L.; Johansson, L.; Julshamn, K.; Meltzer, H.M. The iodine content of Norwegian foods and diets. Public Health Nutr. 2004, 7, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Dahl, L.; Opsahl, J.A.; Meltzer, H.M.; Julshamn, K. Iodine concentration in Norwegian milk and dairy products. Br. J. Nutr. 2003, 90, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Haugen, M.; Brantsaeter, A.L.; Alexander, J.; Meltzer, H.M. Dietary supplements contribute substantially to the total nutrient intake in pregnant Norwegian women. Ann. Nutr. Metab. 2008, 52, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Brantsaeter, A.L.; Haugen, M.; Alexander, J.; Meltzer, H.M. Validity of a new food frequency questionnaire for pregnant women in the Norwegian mother and child cohort study (Moba). Matern. Child Nutr. 2008, 4, 28–43. [Google Scholar] [CrossRef] [PubMed]
- Brantsaeter, A.L.; Haugen, M.; Hagve, T.A.; Aksnes, L.; Rasmussen, S.E.; Julshamn, K.; Alexander, J.; Meltzer, H.M. Self-reported dietary supplement use is confirmed by biological markers in the Norwegian mother and child cohort study (Moba). Ann. Nutr. Metab. 2007, 51, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Brantsaeter, A.L.; Haugen, M.; Julshamn, K.; Alexander, J.; Meltzer, H.M. Evaluation of urinary iodine excretion as a biomarker for intake of milk and dairy products in pregnant women in the Norwegian mother and child cohort study (Moba). Eur. J. Clin. Nutr. 2009, 63, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Abel, M.H.; Korevaar, T.I.M.; Caspersen, I.H.; Villanger, G.D.; Meltzer, H.M.; Torheim, L.E.; Alexander, J.; Arohonka, P.; Erlund, I.; Brantsæter, A.L. Iodine intake and thyroid function in pregnancy. Unpublished work. 2018. [Google Scholar]
- Norwegian Institute of Public Health. Norwegian Prescription Database. Available online: www.norpd.no (accessed on 1 June 2016).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Polanczyk, G.V.; Willcutt, E.G.; Salum, G.A.; Kieling, C.; Rohde, L.A. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int. J. Epidemiol. 2014, 43, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Sonuga-Barke, E.J.S.; Taylor, E. Adhd and hyperkinetic disorder. In Rutter’s Child and Adolescent Psychiatry, 6th ed.; Thapar, A., Pine, D.S., Leckman, J.F., Scott, S., Snowling, M.J., Taylor, E., Eds.; John Wiley and Sons Ltd.: Chichester, UK, 2015; pp. 738–756. [Google Scholar]
- Taylor, E.; Schachar, R.; Thorley, G.; Wieselberg, H.M.; Everitt, B.; Rutter, M. Which boys respond to stimulant medication? A controlled trial of methylphenidate in boys with disruptive behaviour. Psychol. Med. 1987, 17, 121–143. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.R.; Alpert, M.; Pouget, E.; Silva, V.; Trosper, S.; Reyes, K.; Dummit, S. A rating scale for disruptive behavior disorders, based on the DSM-IV item pool. Psychiatr. Q. 2005, 76, 327–339. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.; Goetz, T.; Glenn, T.; Whybrow, P.C. The thyroid-brain interaction in thyroid disorders and mood disorders. J. Neuroendocrinol. 2008, 20, 1101–1114. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Iodine. In Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc; The National Academies Press: Washington, DC, USA, 2001; pp. 258–289. [Google Scholar] [CrossRef]
- Orsini, N.; Greenland, S. A procedure to tabulate and plot results after flexible modeling of a quantitative covariate. Stata J. 2011, 11, 1–29. [Google Scholar]
- Moleti, M.; Di Bella, B.; Giorgianni, G.; Mancuso, A.; De Vivo, A.; Alibrandi, A.; Trimarchi, F.; Vermiglio, F. Maternal thyroid function in different conditions of iodine nutrition in pregnant women exposed to mild-moderate iodine deficiency: An observational study. Clin. Endocrinol. (Oxf.) 2011, 74, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Andersson, M.; de Benoist, B.; Delange, F.; Zupan, J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: Conclusions and recommendations of the technical consultation. Public Health Nutr. 2007, 10, 1606–1611. [Google Scholar] [CrossRef] [PubMed]
- Oerbeck, B.; Overgaard, K.R.; Aspenes, S.T.; Pripp, A.H.; Mordre, M.; Aase, H.; Reichborn-Kjennerud, T.; Zeiner, P. Adhd, comorbid disorders and psychosocial functioning: How representative is a child cohort study? Findings from a national patient registry. BMC Psychiatry 2017, 17, 23. [Google Scholar] [CrossRef] [PubMed]
- Suren, P.; Bakken, I.J.; Aase, H.; Chin, R.; Gunnes, N.; Lie, K.K.; Magnus, P.; Reichborn-Kjennerud, T.; Schjolberg, S.; Oyen, A.S.; et al. Autism spectrum disorder, ADHD, epilepsy, and cerebral palsy in Norwegian children. Pediatrics 2012, 130, e152–e158. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Han, C.; Li, C.; Mao, J.; Wang, W.; Xie, X.; Li, C.; Xu, B.; Meng, T.; Du, J.; et al. Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: A cross-sectional study of 7190 pregnant women in China. J. Clin. Endocrinol. Metab. 2015, 100, 1630–1638. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Boelaert, K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 2015, 3, 286–295. [Google Scholar] [CrossRef]
- Roman, G.C. Autism: Transient in utero hypothyroxinemia related to maternal flavonoid ingestion during pregnancy and to other environmental antithyroid agents. J. Neurol. Sci. 2007, 262, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Hauser, P.; Zametkin, A.J.; Martinez, P.; Vitiello, B.; Matochik, J.A.; Mixson, A.J.; Weintraub, B.D. Attention deficit-hyperactivity disorder in people with generalized resistance to thyroid hormone. N. Engl. J. Med. 1993, 328, 997–1001. [Google Scholar] [CrossRef] [PubMed]
- Ghassabian, A.; Henrichs, J.; Tiemeier, H. Impact of mild thyroid hormone deficiency in pregnancy on cognitive function in children: Lessons from the Generation R Study. Best Pract. Res. Clin. Endocrinol. Metab. 2014, 28, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Modesto, T.; Tiemeier, H.; Peeters, R.P.; Jaddoe, V.W.; Hofman, A.; Verhulst, F.C.; Ghassabian, A. Maternal mild thyroid hormone insufficiency in early pregnancy and attention-deficit/hyperactivity disorder symptoms in children. JAMA Pediatr. 2015, 169, 838–845. [Google Scholar] [CrossRef] [PubMed]
- Ghassabian, A.; Bongers-Schokking, J.J.; de Rijke, Y.B.; van Mil, N.; Jaddoe, V.W.; de Muinck Keizer-Schrama, S.M.; Hooijkaas, H.; Hofman, A.; Visser, W.; Roman, G.C.; et al. Maternal thyroid autoimmunity during pregnancy and the risk of attention deficit/hyperactivity problems in children: The generation r study. Thyroid 2012, 22, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.L.; Laurberg, P.; Wu, C.S.; Olsen, J. Attention deficit hyperactivity disorder and autism spectrum disorder in children born to mothers with thyroid dysfunction: A Danish nationwide cohort study. BJOG 2014, 121, 1365–1374. [Google Scholar] [CrossRef] [PubMed]
- Harding, K.B.; Pena-Rosas, J.P.; Webster, A.C.; Yap, C.M.; Payne, B.A.; Ota, E.; De-Regil, L.M. Iodine supplementation for women during the preconception, pregnancy and postpartum period. Cochrane Database Syst. Rev. 2017, 3, CD011761. [Google Scholar] [CrossRef] [PubMed]
- Gowachirapant, S.; Jaiswal, N.; Melse-Boonstra, A.; Galetti, V.; Stinca, S.; Mackenzie, I.; Thomas, S.; Thomas, T.; Winichagoon, P.; Srinivasan, K.; et al. Effect of iodine supplementation in pregnant women on child neurodevelopment: A randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2017, 5, 853–863. [Google Scholar] [CrossRef]
- Garnweidner-Holme, L.; Aakre, I.; Lilleengen, A.M.; Brantsaeter, A.L.; Henjum, S. Knowledge about iodine in pregnant and lactating women in the Oslo area, Norway. Nutrients 2017, 9, 493. [Google Scholar] [CrossRef] [PubMed]
- Ystrom, E.; Vollrath, M.E.; Nordeng, H. Effects of personality on use of medications, alcohol, and cigarettes during pregnancy. Eur. J. Clin. Pharmacol. 2012, 68, 845–851. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, R.M.; Vollset, S.E.; Gjessing, H.K.; Skjaerven, R.; Melve, K.K.; Schreuder, P.; Alsaker, E.R.; Haug, K.; Daltveit, A.K.; Magnus, P. Self-selection and bias in a large prospective pregnancy cohort in Norway. Paediatr. Perinat. Epidemiol. 2009, 23, 597–608. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, R.M.; Suren, P.; Gunnes, N.; Alsaker, E.R.; Bresnahan, M.; Hirtz, D.; Hornig, M.; Lie, K.K.; Lipkin, W.I.; Reichborn-Kjennerud, T.; et al. Analysis of self-selection bias in a population-based cohort study of autism spectrum disorders. Paediatr. Perinat. Epidemiol. 2013, 27, 553–563. [Google Scholar] [CrossRef] [PubMed]
| Iodine Intake from Food (µg/Day) | Supplemental Iodine (µg/Day) | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| <100 | 100–159.9 | 160–250 | >250 | 0 | 1–200 | >200 | ||
| Mother-child pairs, n (%) | 25,637 (33.2) | 31,688 (41.1) | 16,322 (21.1) | 3517 (4.6) | 53,360 (69.2) | 21,940 (28.4) | 1864 (2.4) | 77,164 (100) |
| Maternal age at delivery, years | 30.1 (4.5) | 30.4 (4.4) | 30.1 (4.6) | 29.4 (4.9) | 30.1 (4.6) | 30.3 (4.4) | 30.0 (4.8) | 30.2 (4.5) |
| Pre-pregnancy BMI, kg/m2 | 24.2 (4.4) | 23.9 (4.2) | 24.0 (4.2) | 24.4 (4.6) | 24.1 (4.3) | 23.9 (4.2) | 23.9 (4.3) | 24.0 (4.3) |
| Parity, % | ||||||||
| 0 | 49.9 | 46.2 | 45.3 | 48.4 | 44.7 | 52.7 | 58.2 | 47.3 |
| 1 | 34.9 | 36.3 | 35.8 | 32.4 | 36.7 | 33.4 | 31.0 | 35.6 |
| 2 or more | 15.2 | 17.4 | 18.9 | 19.2 | 18.6 | 13.9 | 10.8 | 17.1 |
| Maternal education | ||||||||
| ≤12 years | 31.1 | 27.9 | 32.1 | 41.7 | 32.2 | 26.4 | 30.3 | 30.5 |
| 13–16 years | 42.4 | 43.9 | 43.3 | 39.0 | 42.3 | 44.9 | 42.9 | 43.1 |
| >16 years | 26.5 | 28.2 | 24.6 | 19.3 | 25.5 | 28.7 | 26.8 | 26.5 |
| Married/cohabitant | 96.7 | 97.0 | 96.6 | 94.9 | 96.7 | 96.8 | 95.9 | 96.7 |
| Smoking in pregnancy | ||||||||
| No | 77.8 | 79.8 | 78.5 | 74.0 | 78.1 | 79.8 | 78.2 | 78.6 |
| Occasionally | 16.2 | 14.9 | 15.1 | 16.5 | 15.5 | 15.2 | 16.1 | 15.5 |
| Daily | 6.0 | 5.3 | 6.4 | 9.5 | 6.4 | 5.0 | 5.7 | 5.9 |
| Chronic illness | 11.6 | 9.5 | 9.3 | 10.5 | 9.8 | 11.0 | 12.0 | 10.2 |
| Parents’ income | ||||||||
| Low | 25.1 | 25.1 | 29.0 | 33.4 | 27.1 | 24.7 | 23.5 | 26.3 |
| Medium | 40.7 | 41.2 | 42.0 | 42.6 | 41.4 | 40.9 | 41.3 | 41.3 |
| High | 31.8 | 31.2 | 26.0 | 19.8 | 28.7 | 32.1 | 32.5 | 29.8 |
| Missing | 2.4 | 2.5 | 3.0 | 4.3 | 2.8 | 2.4 | 2.7 | 2.6 |
| Child sex | ||||||||
| Boys | 51.2 | 51.2 | 51.0 | 51.6 | 51.5 | 50.5 | 51.2 | 51.2 |
| Girls | 48.8 | 48.8 | 49.0 | 48.4 | 48.5 | 49.5 | 48.8 | 48.8 |
| Bilingual parent(s) | 10.7 | 10.3 | 8.9 | 9.3 | 9.8 | 10.6 | 12.8 | 10.1 |
| ADHD diagnosis by December 2015 | 2.1 | 2.1 | 2.6 | 3.4 | 2.2 | 2.3 | 2.1 | 2.2 |
| Iodine Intake from Food | Supplemental Iodine | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| <100 | 100–159.9 | 160–250 | >250 | 0 | 1–200 | >200 | ||
| Energy intake, MJ/day | 8.2 (2.0) | 9.7 (2.1) | 11.3 (2.4) | 13.5 (2.8) | 9.7 (2.6) | 9.7 (2.6) | 9.9 (2.6) | 9.7 (2.6) |
| Iodine from food, µg/day | 74 (18) | 127 (17) | 193 (24) | 304 (55) | 132 (61) | 131 (61) | 133 (64) | 132 (61) |
| Food intake, g/day | ||||||||
| Milk/yoghurt | 162 (123) | 411 (168) | 756 (246) | 1435 (443) | 447 (360) | 448 (362) | 463 (386) | 448 (362) |
| Fish, lean | 16 (11) | 22 (13) | 25 (15) | 28 (18) | 21 (14) | 20 (13) | 21 (15) | 21 (14) |
| Fish, fatty | 9 (9) | 12 (13) | 16 (18) | 19 (23) | 12 (14) | 12 (14) | 12 (12) | 12 (14) |
| Eggs | 9 (9) | 12 (12) | 13 (14) | 15 (17) | 11 (12) | 12 (13) | 12 (13) | 11 (12) |
| Fruits and vegetables | 388 (217) | 453 (246) | 502 (280) | 559 (344) | 443 (253) | 451 (254) | 489 (308) | 447 (255) |
| Nutrient intake, g/day | ||||||||
| Protein | 71 (14) | 86 (14) | 104 (16) | 132 (21) | 87 (21) | 87 (21) | 89 (22) | 87 (21) |
| Sugar | 55 (37) | 60 (36) | 70 (40) | 84 (50) | 62 (39) | 62 (37) | 62 (37) | 62 (38) |
| Fiber | 27 (9) | 31 (10) | 35 (11) | 39 (13) | 31 (10) | 31 (11) | 33 (12) | 31 (10) |
| Alcohol | 0.1 (0.6) | 0.1 (0.7) | 0.1 (0.5) | 0.1 (0.7) | 0.1 (0.6) | 0.1 (0.7) | 0.1 (0.3) | 0.1 (0.6) |
| Iodine from source, µg/day | ||||||||
| Milk including yoghurt | 20 (16) | 56 (23) | 107 (35) | 206 (64) | 62 (52) | 61 (52) | 63 (55) | 62 (52) |
| Fish | 16 (11) | 24 (14) | 30 (19) | 35 (27) | 23 (16) | 23 (16) | 22 (16) | 23 (16) |
| Eggs | 4 (4) | 5 (6) | 6 (6) | 7 (8) | 5 (5) | 5 (6) | 5 (6) | 5 (6) |
| Supplements | 35 (72) | 35 (72) | 35 (71) | 37 (77) | - | 95 (51) | 336 (135) | 35 (72) |
| Iodine supplement | ||||||||
| 0 µg/day | 69.0 | 69.1 | 69.4 | 69.3 | 100 | - | - | 69.2 |
| 1–99 µg/day | 15.8 | 15.1 | 14.8 | 14.8 | - | 53.7 | - | 15.3 |
| 100–199 µg/day | 12.6 | 13.4 | 13.4 | 13.1 | - | 46.3 | - | 13.2 |
| ≥200 µg/day | 2.5 | 2.3 | 2.4 | 2.8 | - | - | 100 | 2.4 |
| n-3 FA supplement 2 | 64.9 | 69.7 | 69.7 | 66.4 | 63.4 | 77.4 | 86.0 | 68.0 |
| Folic acid supplement 3 | 73.9 | 73.9 | 71.0 | 66.3 | 68.6 | 82.6 | 84.5 | 72.9 |
| Any supplement (in FFQ) | 83.8 | 86.7 | 86.3 | 83.7 | 79.1 | 100 | 100 | 85.5 |
| ADHD Diagnosis | ||||
|---|---|---|---|---|
| n | Crude Model | Adjusted Model 2 | Adjusted Model 2 | |
| Matched Controls | ||||
| Iodine from food <160 µg/day | ||||
| Iodine from supplement: | ||||
| No (reference) | 39,597 (11,057 3) | 1 | 1 | 1 |
| 1–200 µg/day | 16,355 | 1.03 (0.91, 1.17) | 1.13 (0.99, 1.28) | 1.01 (0.86, 1.20) |
| >200 µg/day | 1373 | 1.05 (0.71, 1.55) | 1.07 (0.72, 1.59) | 0.95 (0.63, 1.43) |
| First report of iodine 4 | ||||
| Before pregnancy 5 | 4018 | 1.02 (0.81, 1.28) | 1.24 (0.99, 1.56) | 1.11 (0.86, 1.43) |
| Gestational week 0–12 | 2970 | 1.34 (1.07, 1.68) | 1.47 (1.17, 1.85) | 1.29 (1.00, 1.67) |
| Gestational week ≥13 | 3402 | 1.04 (0.82, 1.32) | 1.11 (0.87, 1.41) | 0.98 (0.75, 1.27) |
| Iodine from food ≥160 µg/day | ||||
| Iodine from supplement: | ||||
| No (reference) | 13,763 (4152 3) | 1 | 1 | 1 |
| 1–200 µg/day | 5585 | 1.11 (0.92, 1.34) | 1.18 (0.98, 1.43) | 1.08 (0.84, 1.37) |
| >200 µg/day | 491 | 1.15 (0.66, 2.00) | 1.16 (0.66, 2.01) | 1.03 (0.58, 1.83) |
| First report of iodine 4 | ||||
| Before pregnancy 5 | 1460 | 0.97 (0.69, 1.37) | 1.21 (0.85, 1.71) | 1.09 (0.74, 1.59) |
| Gestational week 0–12 | 1020 | 1.40 (1.01, 1.95) | 1.50 (1.07, 2.10) | 1.35 (0.93, 1.96) |
| Gestational week ≥13 | 1102 | 0.99 (0.68, 1.44) | 1.04 (0.71, 1.52) | 0.93 (0.61, 1.40) |
| N | ADHD Score | Inattention Score | Hyperactivity Score | |||||
|---|---|---|---|---|---|---|---|---|
| Crude Model | Adjusted Model | Adjusted Model | Crude Model | Adjusted Model | Crude Model | Adjusted Model | ||
| Matched Controls 2 | ||||||||
| Iodine from food <160 µg/day | ||||||||
| Iodine from supplement: | ||||||||
| No (reference) | 14,089 (4133) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1–200 µg/day | 6115 | 0.06 (0.04, 0.09) | 0.05 (0.03, 0.08) | 0.02 (−0.01, 0.05) | 0.06 (0.03, 0.08) | 0.05 (0.02, 0.07) | 0.06 (0.03, 0.10) | 0.06 (0.03, 0.10) |
| >200 µg/day | 457 | 0.07 (−0.00, 0.15) | 0.06 (−0.02, 0.13) | 0.02 (−0.06, 0.10) | 0.07 (−0.00, 0.15) | 0.06 (−0.02, 0.13) | 0.07 (−0.03, 0.17) | 0.06 (−0.03, 0.16) |
| First report of iodine supplement 3: | ||||||||
| Before pregnancy 4 | 1650 | 0.04 (0.00, 0.09) | 0.04 (0.00, 0.08) | 0.01 (−0.04, 0.05) | 0.06 (0.02, 0.10) | 0.05 (0.01, 0.09) | 0.02 (−0.03, 0.08) | 0.03 (−0.02, 0.08) |
| Gestational week 0–12 | 1203 | 0.12 (0.07, 0.17) | 0.10 (0.05, 0.15) | 0.06 (0.01, 0.11) | 0.11 (0.06, 0.15) | 0.07 (0.03, 0.12) | 0.14 (0.08, 0.20) | 0.13 (0.07, 0.19) |
| Gestational week ≥13 | 1264 | 0.06 (0.01, 0.11) | 0.05 (0.00, 0.10) | 0.01 (−0.04, 0.07) | 0.05 (0.01, 0.10) | 0.04 (−0.01, 0.09) | 0.07 (0.01, 0.14) | 0.07 (0.01, 0.13) |
| Iodine from food ≥160 µg/day | ||||||||
| Iodine from supplement: | ||||||||
| No (reference) | 4997 (1593) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1–200 µg/day | 2133 | 0.02 (−0.02, 0.06) | 0.02 (−0.02, 0.07) | 0.02 (−0.04, 0.07) | 0.02 (−0.02, 0.07) | 0.02 (−0.02, 0.06) | 0.02 (−0.04, 0.07) | 0.02 (−0.03, 0.08) |
| >200 µg/day | 154 | 0.00 (−0.13, 0.14) | 0.01 (−0.11, 0.13) | 0.01 (−0.11, 0.13) | 0.02 (−0.11, 0.15) | 0.05 (−0.07, 0.17) | −0.02 (−0.20, 0.17) | −0.04 (−0.21, 0.13) |
| First report of iodine supplement 3: | ||||||||
| Before pregnancy 4 | 611 | 0.06 (−0.02, 0.13) | 0.08 (0.00, 0.15) | 0.07 (−0.02, 0.15) | 0.05 (−0.02, 0.13) | 0.06 (−0.01, 0.14) | 0.06 (−0.03, 0.16) | 0.09 (−0.00, 0.19) |
| Gestational week 0–12 | 397 | 0.03 (−0.05, 0.12) | 0.02 (−0.07, 0.10) | 0.00 (−0.09, 0.10) | 0.04 (−0.04, 0.13) | 0.02 (−0.06, 0.10) | 0.02 (−0.09, 0.13) | 0.02 (−0.09, 0.13) |
| Gestational week ≥13 | 439 | 0.02 (−0.07, 0.10) | 0.01 (−0.07, 0.09) | 0.00 (−0.09, 0.09) | 0.01 (−0.07, 0.09) | 0.00 (−0.08, 0.08) | 0.03 (−0.08, 0.14) | 0.02 (−0.09, 0.13) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abel, M.H.; Ystrom, E.; Caspersen, I.H.; Meltzer, H.M.; Aase, H.; Torheim, L.E.; Askeland, R.B.; Reichborn-Kjennerud, T.; Brantsæter, A.L. Maternal Iodine Intake and Offspring Attention-Deficit/Hyperactivity Disorder: Results from a Large Prospective Cohort Study. Nutrients 2017, 9, 1239. https://doi.org/10.3390/nu9111239
Abel MH, Ystrom E, Caspersen IH, Meltzer HM, Aase H, Torheim LE, Askeland RB, Reichborn-Kjennerud T, Brantsæter AL. Maternal Iodine Intake and Offspring Attention-Deficit/Hyperactivity Disorder: Results from a Large Prospective Cohort Study. Nutrients. 2017; 9(11):1239. https://doi.org/10.3390/nu9111239
Chicago/Turabian StyleAbel, Marianne Hope, Eivind Ystrom, Ida Henriette Caspersen, Helle Margrete Meltzer, Heidi Aase, Liv Elin Torheim, Ragna Bugge Askeland, Ted Reichborn-Kjennerud, and Anne Lise Brantsæter. 2017. "Maternal Iodine Intake and Offspring Attention-Deficit/Hyperactivity Disorder: Results from a Large Prospective Cohort Study" Nutrients 9, no. 11: 1239. https://doi.org/10.3390/nu9111239
APA StyleAbel, M. H., Ystrom, E., Caspersen, I. H., Meltzer, H. M., Aase, H., Torheim, L. E., Askeland, R. B., Reichborn-Kjennerud, T., & Brantsæter, A. L. (2017). Maternal Iodine Intake and Offspring Attention-Deficit/Hyperactivity Disorder: Results from a Large Prospective Cohort Study. Nutrients, 9(11), 1239. https://doi.org/10.3390/nu9111239






