A Study of the Effects of Latent Iron Deficiency on Measures of Cognition: A Pilot Randomised Controlled Trial of Iron Supplementation in Young Women
Abstract
:1. Introduction
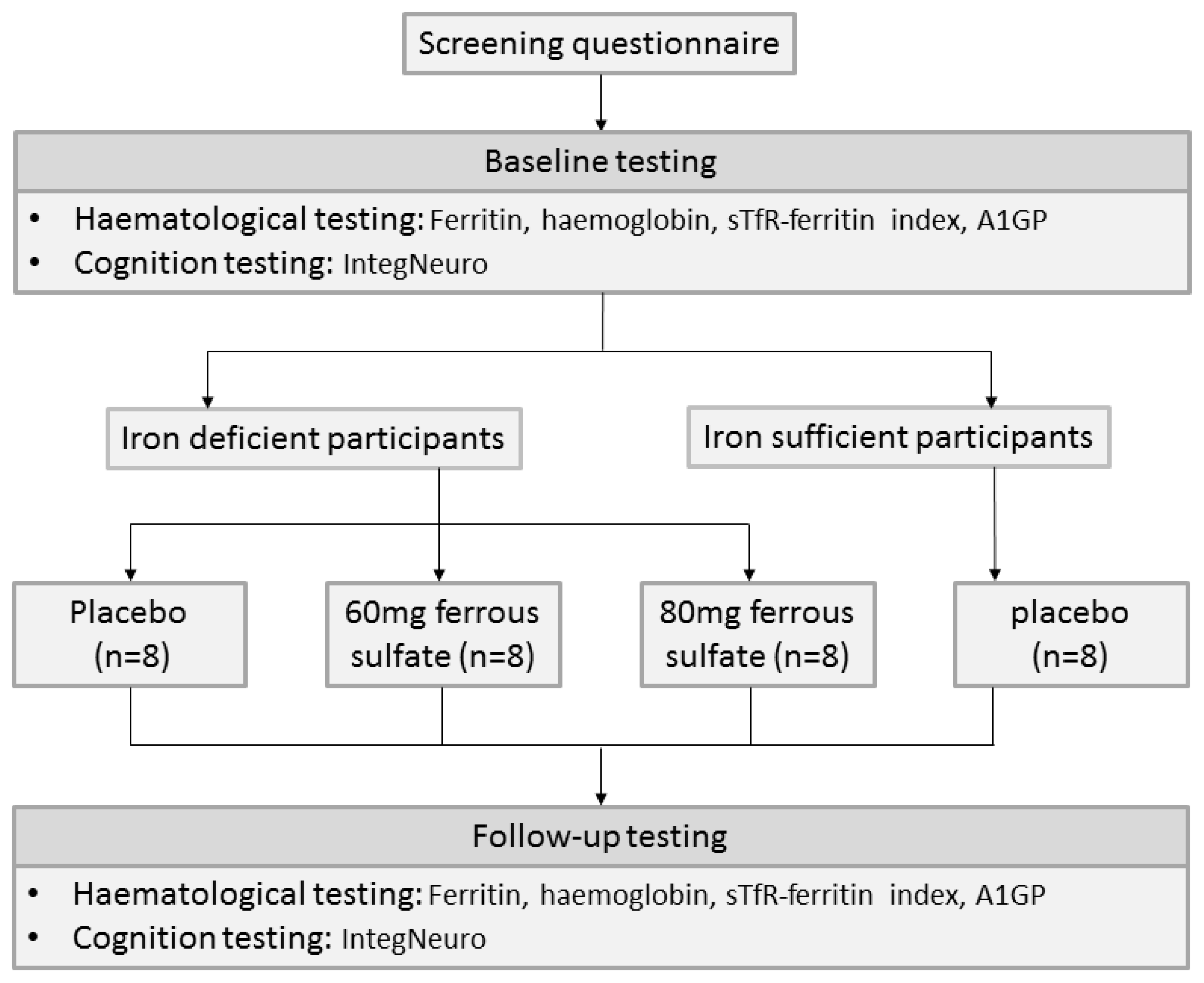
2. Experimental Section
2.1. Haematological Testing
2.2. Cognitive Testing
2.3. Treatment Randomisation
2.4. Treatment Blinding
2.5. Required Sample Size for an Adequately Powered RCT
2.6. Statistical Analysis
3. Results
3.1. Participants
3.2. Iron Status
3.3. Cognitive Scores
| Cognitive domain | 60 mg Iron (n = 7) | 80 mg Iron (n = 6) | Placebo (n = 6) | Control ( n = 6) | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Memory | 6.00 (6.0–7.0) | 6.50 (6.5–8.0) | 4.25 (3.5–5.0) | 4.25 (4.0–5.0) | 6.75 (5.0–7.5) | 6.50 (4.5–7.5) | 7.00 (3.0–8.0) | 6.75 (5.0–7.5) |
| Response Speed | 4.50 (3.0–6.0) | 6.50 (2.0–7.5) | 6.00 (5.0–6.5) | 4.00 (3.5–4.5) | 5.50 (3.0–7.0) | 6.50 (2.0–7.0) | 6.00 (4.5–6.5) | 6.25 (6.0–6.5) |
| Impulsivity | 6.50 (5.0–7.5) | 8.50 (4.0–9.0) | 4.75 (4.0–8.0) | 6.25 (4.5–9.0) | 6.00 (4.5–8.5) | 6.50 (5.0–8.5) | 7.00 (4.5–9.0) | 5.00 (3.5–6.5) |
| Attention | 4.50 (2.5–6.5) | 5.00 (3.0–7.0) | 4.25 (1.0–8.0) | 7.50 (3.5–9.5) | 7.25 (4.0–7.5) | 5.75 (4.0–7.5) | 7.50 (6.0–8.0) | 7.00 (4.0–8.0) |
| Information Processing | 6.00 (4.5–9.0) | 8.00 (6.0–9.0) | 4.50 (4.5–6.0) | 6.50 (4.5–8.0) | 7.00 (5.0–7.5) | 6.50 (6.0–7.0) | 7.75 (6.5–8.0) | 6.50 (6.5–6.5) |
| Executive Function | 8.00 (7.5–9.0) | 7.50 (6.5–8.0) | 4.50 (3.0–7.0) | 7.00 (6.5–7.5) | 7.50 (4.5–8.5) | 7.50 (7.0–8.0) | 7.50 (7.5–8.5) | 7.75 (5.0–10.0) |
| Emotion Identification | 6.50 (3.0–7.5) | 4.00 (1.5–8.0) | 6.00 (5.0–8.0) | 5.75 (4.5–7.0) | 6.00 (3.0–6.5) | 7.00 (4.0–8.0) | 4.00 (1.0–6.5) | 4.25 (4.0–6.5) |
3.3.1. Baseline Comparison of Iron-deficient Groups (combined) vs. Iron-sufficient Group
3.3.2. Baseline Comparison of Iron-Deficient Groups
3.3.3. Cognitive Change Scores
| Cognitive change Sten score | Iron treatment groups (n = 13) (Mean ± SD) | No treatment groups (n = 12) (Mean ± SD) | p Value |
|---|---|---|---|
| Memory | 0.67 ± 0.78 | 0.08 ± 1.76 | 0.210 |
| Response speed | −0.27 ± 2.21 | −0.46 ± 2.15 | 0.512 |
| Impulsivity | 0.62 ± 1.83 | −0.88 ± 2.42 | 0.047 * |
| Attention | 1.31 ± 2.80 | −0.54 ± 2.36 | 0.085 |
| Information Processing | 1.00 ± 1.86 | −0.21 ± 2.48 | 0.107 |
| Executive Function | 0.62 ± 2.48 | 0.58 ± 1.43 | 0.805 |
| Emotion Identification | −0.50 ± 2.16 | 0.96 ± 1.67 | 0.105 |
3.3.3.1. Analysis of Cognitive Scores in Ferritin Improvers and Non-Improvers
| Cognitive change Sten score | Ferritin improvers (n = 17) | Ferritin non-improvers (n = 8) | p Value |
|---|---|---|---|
| Memory | 0.69 ± 0.95 | −0.25 ± 1.87 | 0.071 |
| Response Speed | 0.15 ± 2.49 | −0.06 ± 1.40 | 0.930 |
| Impulsivity | 0.74 ± 2.07 | −1.88 ± 1.36 | 0.004 * |
| Attention | 1.24 ± 2.49 | −1.31 ± 2.43 | 0.026 * |
| Information Processing | 0.62 ± 1.91 | 0.00 ± 2.88 | 0.334 |
| Executive Function | 0.74 ± 2.21 | 0.31 ± 1.56 | 0.681 |
| Emotion Identification | −0.44 ± 2.05 | 1.56 ± 1.24 | 0.022 * |
3.3.3.2. Analysis of Cognitive Scores in Haemoglobin Improvers and Non-Improvers
| Cognitive change Sten score | Haemoglobin improvers (n = 10) | Haemoglobin non-improvers (n = 15) | p Value |
|---|---|---|---|
| Memory | 0.61 ± 1.50 | 0.23 ± 1.31 | 0.741 |
| Response Speed | 0.30 ± 1.75 | −0.07 ± 2.46 | 0.521 |
| Impulsivity | 0.05 ± 2.23 | −0.20 ± 2.29 | 0.739 |
| Attention | 0.75 ± 2.47 | 0.20 ± 2.92 | 0.802 |
| Information Processing | 1.35 ± 2.56 | −0.20 ± 1.79 | 0.112 |
| Executive Function | 0.65 ± 2.12 | 0.57 ± 1.99 | 0.538 |
| Emotion Identification | 0.50 ± 1.43 | 0.00 ± 2.39 | 0.780 |
3.4. Effect of Guessing Treatment Allocation on Cognitive Change
3.5. Required Sample Size for an Adequately Powered RCT
4. Discussion
4.1. Suitability of IntegNeuro for Iron Deficiency Research
4.2. Required Sample Size for an Adequately Powered RCT
4.3. Effect of Iron Deficiency on Cognition at Baseline and after Iron Treatment
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- The Prevalence of Anaemia in Women: A Tabulation of Available Information, 1992. Available online: http://whqlibdoc.who.int/hq/1992/WHO_MCH_MSM_92.2.pdf (accessed on 20 June 2013).
- Iron Deficiency Anaemia: Assessment, Prevention, and Control. A Guide for Programme Managers. Available online: http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf (accessed on 18 September 2013).
- Scrimshaw, N.S. Iron deficiency. Sci. Am. 1991, 265, 46–52. [Google Scholar] [CrossRef]
- Falkingham, M.; Abdelhamid, A.; Curtis, P.; Fairweather-Tait, S.; Dye, L.; Hooper, L. The effects of oral iron supplementation on cognition in older children and adults: A systematic review and meta-analysis. Nutr. J. 2010, 9, 4. [Google Scholar] [CrossRef]
- Lozoff, B.; Brittenham, G.; Viteri, F.; Wolf, A.; Urrutia, J. Developmental deficits in iron-deficient infants: Effects of age and severity of iron lack. J. Pediatr. 1982, 101, 948–952. [Google Scholar] [CrossRef]
- Oski, F.A.; Honig, A.S.; Helu, B.; Howanitz, P. Effect of iron therapy on behavior performance in nonanemic, iron-deficient infants. Pediatrics 1983, 71, 877–880. [Google Scholar]
- Pollitt, E.; Hathirat, P.; Kotchabhakdi, N.J.; Missell, L.; Valyasevi, A. Iron-deficiency and educational-achievement in Thailand. Am. J. Clin. Nutr. 1989, 50, 687–697. [Google Scholar]
- Walter, T.; Kovalskys, J.; Stekel, A. Effect of mild iron-deficiency on infant mental-development scores. J. Pediatr. 1983, 102, 519–522. [Google Scholar] [CrossRef]
- Webb, T.E.; Oski, F.A. Iron-deficiency anaemia and scholastic achievement in young adolescents. J. Pediatr. 1973, 82, 827–830. [Google Scholar] [CrossRef]
- Tucker, D.M.; Sandstead, H.H.; Penland, J.G.; Dawson, J.G.; Milne, D.B. Iron status and brain-function serum ferritin levels associated with asymmetries of cortical electrophysiology and cognitive performance. Am. J. Clin. Nutr. 1984, 39, 105–113. [Google Scholar]
- Beard, J.L. Iron deficiency alters brain development and functioning. J. Nutr. 2003, 133, 1468S–1472S. [Google Scholar]
- Grantham-McGregor, S.; Ani, C. A review of studies on the effect of iron deficiency on cognitive development in children. J. Nutr. 2001, 131, 649S–666S. [Google Scholar]
- Lozoff, B.; Brittenham, G.M.; Viteri, F.E.; Wolf, A.W.; Urrutia, J.J. The effects of short-term oral iron therapy on developmental deficits in iron-deficient anemic infants. J. Pediatr. 1982, 100, 351–357. [Google Scholar] [CrossRef]
- Lozoff, B.; Beard, J.; Connor, J.; Felt, B.; Georgieff, M.; Schallert, T. Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr. Rev. 2006, 64, S34–S43. [Google Scholar] [CrossRef]
- Khedr, E.; Hamed, S.A.; Elbeih, E.; El-Shereef, H.; Ahmad, Y.; Ahmed, S. Iron states and cognitive abilities in young adults: Neuropsychological and neurophysiological assessment. Eur. Arch. Psychiatry Clin. Neurosci. 2008, 258, 489–496. [Google Scholar] [CrossRef]
- Murray-Kolb, L.E.; Beard, J.L. Iron treatment normalizes cognitive functioning in young women. Am. J. Clin. Nutr. 2007, 85, 778–787. [Google Scholar]
- Patterson, A.J. Iron Deficiency in Australian Women: Development, Implications and Treatment. Ph.D. Thesis, The University of Newcastle, Newcastle, Australia, 1999. [Google Scholar]
- Groner, J.A.; Holtzman, N.A.; Charney, E.; Mellits, E.D. A randomized trial of oral iron on tests of short-term memory and attention span in young pregnant-women. J. Adolesc. Health 1986, 7, 44–48. [Google Scholar] [CrossRef]
- Kretsch, M.J.; Fong, A.K.; Green, M.W.; Johnson, H.L. Cognitive function, iron status, and hemoglobin concentration in obese dieting women. Eur. J. Clin. Nutr. 1998, 52, 512–518. [Google Scholar]
- Ballin, A.; Berar, M.; Rubinstein, U.; Kleter, Y.; Hershkovitz, A.; Meytes, D. Iron state in females adolescents. Am. J. Dis. Child. 1992, 146, 803–805. [Google Scholar]
- Bruner, A.B.; Joffe, A.; Duggan, A.K.; Casella, J.F.; Brandt, J. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet 1996, 348, 992–996. [Google Scholar]
- Elwood, P.C.; Hughes, D. Clinical trial of iron therapy on psychomotor function in anaemic women. Br. Med. J. 1970, 3, 254–255. [Google Scholar] [CrossRef]
- Greig, A.J; Patterson, A.J; Collins, C.E; Chalmers, K.A. Iron deficiency, cognition, mental health and fatigue in women of childbearing age: A systematic review. J. Nutr. Sci. 2013, 2. [Google Scholar] [CrossRef]
- Blanton, C. Improvements in iron status and cognitive function in young women consuming beef or non-beef lunches. Nutrients 2013, 6, 90–110. [Google Scholar] [CrossRef]
- Paul, R.H.; Lawrence, J.; Williams, L.M.; Richard, C.C.; Cooper, N.; Gordon, E. Preliminary validity of “IntegNeuro (TM)”: A new computerized battery of neurocognitive tests. Int. J. Neurosci. 2005, 115, 1549–1567. [Google Scholar] [CrossRef]
- Clark, C.R.; Paul, R.H.; Williams, L.M.; Arns, M.; Fallahpour, K.; Handmer, C.; Gordon, E. Standardized assessment of cognitive functioning during development and aging using an automated touchscreen battery. Arch. Clin. Neuropsychol. 2006, 21, 449–467. [Google Scholar] [CrossRef]
- Ahmed, F.; Coyne, T.; Dobson, A.; McClintock, C. Iron status among Australian adults: Findings of a population based study in Queensland, Australia. Asia Pac. J. Clin. Nutr. 2008, 17, 40–47. [Google Scholar]
- Leonard, A.J.; Patterson, A.J.; Collins, C.E.; Chalmers, K.A. Is soluble transferrin receptor a useful marker in early stage iron deficiency. e-SPEN J. 2013, 8, e210–e212. [Google Scholar] [CrossRef]
- Suominen, P.; Punnonen, K.; Rajamaki, A.; Irjala, K. Serum transferrin receptor and transferrin receptor-ferritin index identify healthy subjects with subclinical iron deficits. Blood 1998, 92, 2934–2939. [Google Scholar]
- Larsson, A.; Hansson, L.O.; Palm, M.; Basu, S.; Axelsson, O. Reference values for a1-acid glycoprotein, a1-antitrypsin, albumin, haptoglobin, C-reactive protein, IgA, IgG and IgM during pregnancy. Acta Obstet. Gynecol. Scand. 2008, 87, 1084–1088. [Google Scholar] [CrossRef]
- Malope, B.I.; MacPhail, A.P.; Alberts, M.; Hiss, D.C. The ratio of serum transferrin receptor and serum ferritin in the diagnosis of iron status. Br. J. Haematol. 2001, 115, 84–89. [Google Scholar] [CrossRef]
- Borel, M.J.; Smith, S.M.; Derr, J.; Beard, J.L. Day-to-day variation in iron-status indexes in healthy-men and women. Am. J. Clin. Nutr. 1991, 54, 729–735. [Google Scholar]
- Cooper, M.J.; Zlotkin, S.H. Day-to-day variation of transferrin receptor and ferritin in healthy men and women. Am. J. Clin. Nutr. 1996, 64, 738–742. [Google Scholar]
- Stupnicki, R.; Malczewska, J.; Milde, K.; Hackney, A.C. Day to day variability in the transferrin receptor/ferritin index in female athletes. Br. J. Sport. Med. 2003, 37, 267–269. [Google Scholar] [CrossRef]
- Brain Resource Company. Brain Resource BRISC and IntegNeuro Assessment Manual; Brain Resource Company: San Francisco, CA, USA, 2011. [Google Scholar]
- Psychometric Success. Standard Scores, Percentiles and Norming. Available online: http://www.psychometric-success.com/aptitude-tests/percentiles-and-norming.htm (accessed on 17 January 2014).
- Leonard, A.J.; Chalmers, K.A.; Collins, C.E.; Patterson, A.J. Comparison of two doses of elemental iron in the treatment of latent iron deficiency: Efficacy, side effects and blinding capabilities. Nutrients 2014, 6, 1394–1405. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software; StataCorp LP: College Station, TX, USA, 2013. [Google Scholar]
- Beard, J.L.; Hendricks, M.K.; Perez, E.M.; Murray-Kolb, L.E.; Berg, A.; Vernon-Feagans, L.; Irlam, J.; Isaacs, W.; Sive, A.; Tomlinson, M. Maternal iron deficiency anemia affects postpartum emotions and cognition. J. Nutr. 2005, 135, 267–272. [Google Scholar]
- Mansson, J.; Johansson, G.; Wiklund, M.; Baigi, A.; Marklund, B. Symptom panorama in upper secondary school students and symptoms related to iron deficiency. Screening with laboratory tests, questionnaire and interventional treatment with iron. Scand. J. Prim. Health Care 2005, 23, 28–33. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2011, 9, 672–677. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Leonard, A.J.; Chalmers, K.A.; Collins, C.E.; Patterson, A.J. A Study of the Effects of Latent Iron Deficiency on Measures of Cognition: A Pilot Randomised Controlled Trial of Iron Supplementation in Young Women. Nutrients 2014, 6, 2419-2435. https://doi.org/10.3390/nu6062419
Leonard AJ, Chalmers KA, Collins CE, Patterson AJ. A Study of the Effects of Latent Iron Deficiency on Measures of Cognition: A Pilot Randomised Controlled Trial of Iron Supplementation in Young Women. Nutrients. 2014; 6(6):2419-2435. https://doi.org/10.3390/nu6062419
Chicago/Turabian StyleLeonard, Alecia J., Kerry A. Chalmers, Clare E. Collins, and Amanda J. Patterson. 2014. "A Study of the Effects of Latent Iron Deficiency on Measures of Cognition: A Pilot Randomised Controlled Trial of Iron Supplementation in Young Women" Nutrients 6, no. 6: 2419-2435. https://doi.org/10.3390/nu6062419
APA StyleLeonard, A. J., Chalmers, K. A., Collins, C. E., & Patterson, A. J. (2014). A Study of the Effects of Latent Iron Deficiency on Measures of Cognition: A Pilot Randomised Controlled Trial of Iron Supplementation in Young Women. Nutrients, 6(6), 2419-2435. https://doi.org/10.3390/nu6062419






