Magnesium and Zinc Are Associated with Sleep Quality in Saudi Adults: Evidence from a Cross-Sectional Study
Abstract
1. Introduction
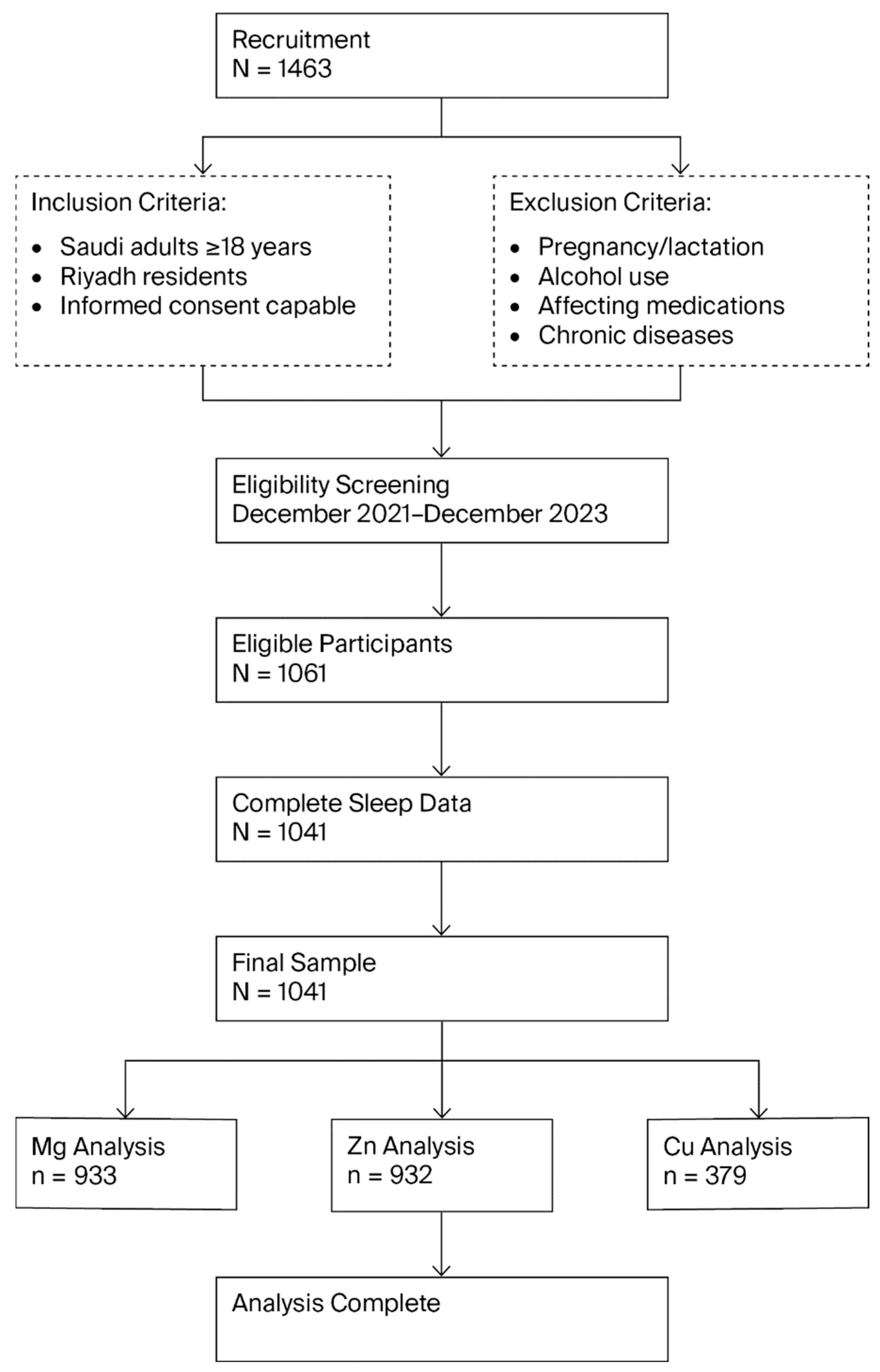
2. Materials and Methods
2.1. Study Design and Settings
2.2. Study Population
2.3. Sample Size and Sampling Method
2.4. Data Collection
2.4.1. Socio-Demographics and Anthropometric Measurements
2.4.2. Biochemical Blood Analysis
2.4.3. Sleep Quality Assessment
2.4.4. Dietary Assessment
2.4.5. Physical Activity Assessment
2.4.6. Statistical Analysis
3. Results
3.1. General Characteristics of Study Subjects
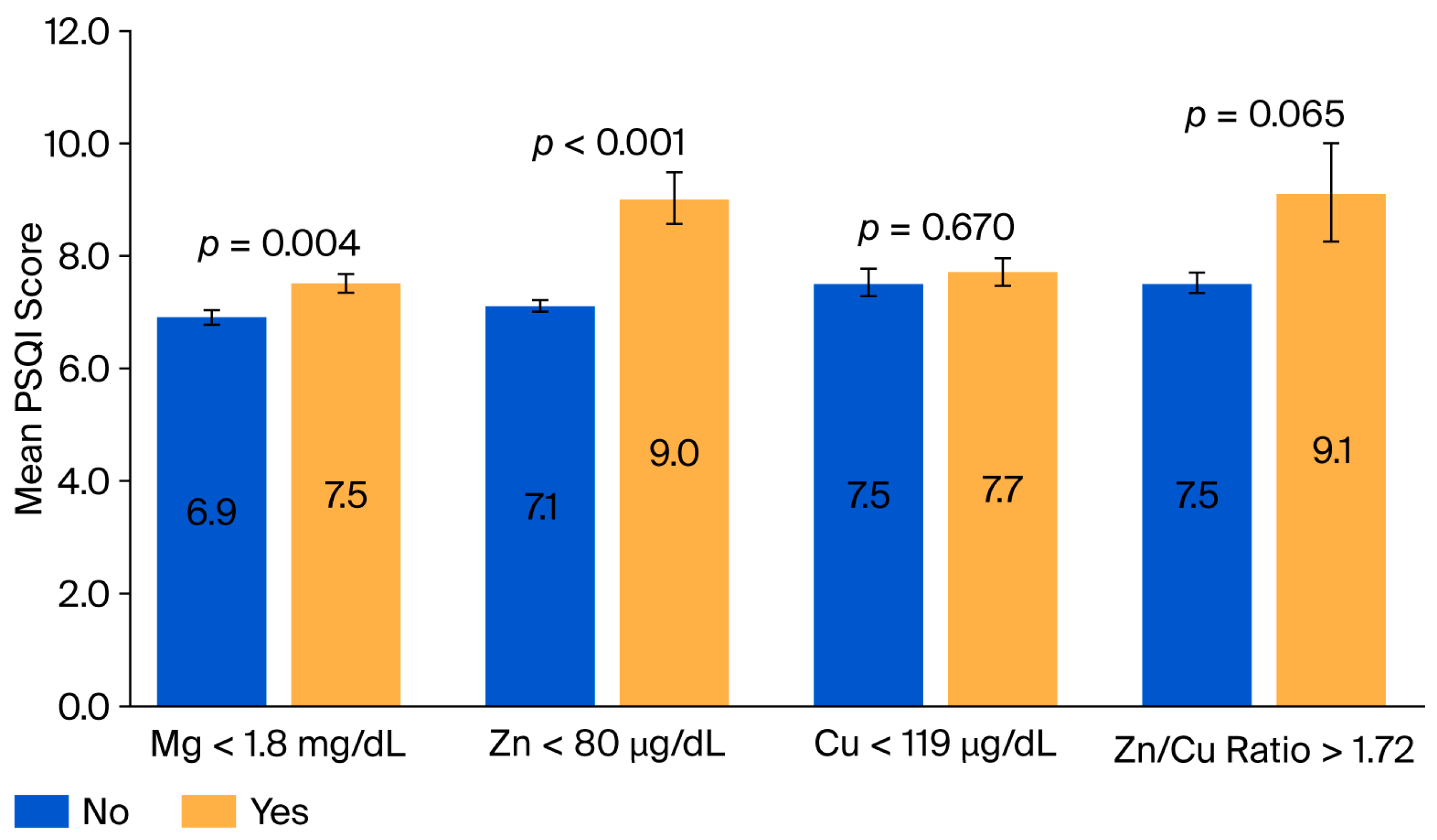
3.2. Lower Serum Mg and Zn Levels Are Associated with Poor Sleep Quality
3.3. Highest Tertiles of Serum Zn and Cu Levels Are Associated with Lower Odds of Poor Sleep Quality
3.4. Serum Zn and Mg Deficiencies Are Associated with Higher Odds of Poor Sleep Quality
3.5. Sex-Related Differences in the Association Between Serum Zn and Mg Deficiency States and Odds of Poor Sleep Quality
3.6. Age-Related Differences in the Association Between Serum Zn and Mg Deficiency States and Higher Odds of Poor Sleep Quality
3.7. Lower Dietary Mg Intake Is Associated with Odds of Poor Sleep Quality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Ramar, K.; Malhotra, R.K.; Carden, K.A.; Martin, J.L.; Abbasi-Feinberg, F.; Aurora, R.N.; Kapur, V.K.; Olson, E.J.; Rosen, C.L.; Rowley, J.A.; et al. Sleep is essential to health: An American Academy of Sleep Medicine position statement. J. Clin. Sleep Med. 2021, 17, 2115–2119. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015, 38, 843–844. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Adams Hillard, P.J.; Katz, E.S.; et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef]
- Canever, J.B.; Zurman, G.; Vogel, F.; Sutil, D.V.; Diz, J.B.M.; Danielewicz, A.L.; Moreira, B.d.S.; Cimarosti, H.I.; de Avelar, N.C.P. Worldwide prevalence of sleep problems in community-dwelling older adults: A systematic review and meta-analysis. Sleep Med. 2024, 119, 118–134. [Google Scholar] [CrossRef]
- Madrid-Valero, J.J.; Martínez-Selva, J.M.; Couto, B.R.d.; Sánchez-Romera, J.F.; Ordoñana, J.R. Age and gender effects on the prevalence of poor sleep quality in the adult population. Gac. Sanit. 2017, 31, 18–22. [Google Scholar] [CrossRef]
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med. Rev. 2017, 34, 70–81. [Google Scholar] [CrossRef]
- Luckhaupt, S.E.; Tak, S.; Calvert, G.M. The prevalence of short sleep duration by industry and occupation in the National Health Interview Survey. Sleep 2010, 33, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Pankowska, M.M.; Lu, H.; Wheaton, A.G.; Liu, Y.; Lee, B.; Greenlund, K.J.; Carlson, S.A. Prevalence and geographic patterns of self-reported short sleep duration among US adults, 2020. Prev. Chronic Dis. 2023, 20, E53. [Google Scholar] [CrossRef]
- Thalib, H.I.; Ali, S.H.; Hanin, A.; Jamal, A.M.; Bajri, R.O.; Ikram, H.N. Prevalence of poor sleep quality among adults in Jeddah, Saudi Arabia. Med. Sci. 2024, 28, e133ms3456. [Google Scholar]
- Alwhaibi, M.; Al Aloola, N.A. Associations between Stress, Anxiety, Depression and Sleep Quality among Healthcare Students. J. Clin. Med. 2023, 12, 4340. [Google Scholar] [CrossRef]
- AlSaif, H.I. Prevalence of and risk factors for poor sleep quality among residents in training in KSA. J. Taibah Univ. Med. Sci. 2019, 14, 52–59. [Google Scholar] [CrossRef]
- Alharbi, A.S.; Alshahrani, S.M.; Alsaadi, M.M.; Al-Jahdali, H.H.; Wali, S.O.; BaHammam, A.S. Sleep quality and insomnia during the COVID-19 lockdown among the Saudi public: A cross-sectional study. Saudi Med. J. 2021, 42, 384–390. [Google Scholar] [CrossRef]
- Del Brutto, O.H.; Mera, R.M.; Rumbea, D.A.; Sedler, M.J.; Castillo, P.R. Poor sleep quality increases mortality risk: A population-based longitudinal prospective study in community-dwelling middle-aged and older adults. Sleep Health 2024, 10, 144–148. [Google Scholar] [CrossRef]
- Onyegbule, C.J.; Muoghalu, C.G.; Ofoegbu, C.C.; Ezeorah, F. The Impact of Poor Sleep Quality on Cardiovascular Risk Factors and Quality of Life. Cureus 2025, 17, e77397. [Google Scholar] [CrossRef]
- Lee, J.A.; Sunwoo, S.; Kim, Y.S.; Yu, B.Y.; Park, H.K.; Jeon, T.H.; Yoo, B.W. The Effect of Sleep Quality on the Development of Type 2 Diabetes in Primary Care Patients. J. Korean Med. Sci. 2016, 31, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Zhang, R.; Wang, C.; Fu, R.; Song, W.; Dou, K.; Wang, S. Sleep quality and risk of cancer: Findings from the English longitudinal study of aging. Sleep 2021, 44, zsaa192. [Google Scholar] [CrossRef]
- Pearson, O.; Uglik-Marucha, N.; Miskowiak, K.W.; Cairney, S.A.; Rosenzweig, I.; Young, A.H.; Stokes, P.R. The relationship between sleep disturbance and cognitive impairment in mood disorders: A systematic review. J. Affect. Disord. 2023, 327, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, J.; McDaniel, K.; DiBlanda, A. Association Between Insufficient Sleep, Depressive Symptoms, and Suicidality Among Florida High School Students. Prev. Chronic Dis. 2023, 20, E59. [Google Scholar] [CrossRef] [PubMed]
- Tuna, M.K.; Işık, A.C.; Madenci, Ö.; Kaya, K.S. Obesity effects on sleep quality with anthropometric and metabolic changes. Rev. Assoc. Med. Bras. 2022, 68, 574–578. [Google Scholar] [CrossRef]
- Watson, E.J.; Coates, A.M.; Kohler, M.; Banks, S. Caffeine Consumption and Sleep Quality in Australian Adults. Nutrients 2016, 8, 479. [Google Scholar] [CrossRef]
- Reut, G.; Lana, B. Lifestyle factors that affect youth’s sleep and strategies for guiding patients and families toward healthy sleeping. J. Sleep Disorders Ther. 2013, 2, 1000130. [Google Scholar] [CrossRef]
- Honarmand, K.; Rafay, H.; Le, J.; Mohan, S.; Rochwerg, B.; Devlin, J.W.; Skrobik, Y.; Weinhouse, G.L.; Drouot, X.; Watson, P.L.; et al. A systematic review of risk factors for sleep disruption in critically ill adults. Crit. Care Med. 2020, 48, 1066–1074. [Google Scholar] [CrossRef]
- Ikonte, C.J.; Mun, J.G.; Reider, C.A.; Grant, R.W.; Mitmesser, S.H. Micronutrient Inadequacy in Short Sleep: Analysis of the NHANES 2005-2016. Nutrients 2019, 11, 2335. [Google Scholar] [CrossRef] [PubMed]
- Ji, X.; Grandner, M.A.; Liu, J. The relationship between micronutrient status and sleep patterns: A systematic review. Public Health Nutr. 2017, 20, 687–701. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Wang, B.; Chen, X.; Xu, J.; Yang, Y.; Yuan, M. The Mechanisms of Magnesium in Sleep Disorders. Nat. Sci. Sleep 2025, 17, 2639–2656. [Google Scholar] [CrossRef] [PubMed]
- Cherasse, Y.; Urade, Y. Dietary Zinc Acts as a Sleep Modulator. Int. J. Mol. Sci. 2017, 18, 2334. [Google Scholar] [CrossRef]
- Hajianfar, H.; Mollaghasemi, N.; Tavakoly, R.; Campbell, M.S.; Mohtashamrad, M.; Arab, A. The association between dietary zinc intake and health status, including mental health and sleep quality, among Iranian female students. Biol. Trace Elem. Res. 2021, 199, 1754–1761. [Google Scholar] [CrossRef]
- Deng, M.-G.; Liu, F.; Liang, Y.; Chen, Y.; Nie, J.-Q.; Chai, C.; Wang, K. Associations of serum zinc, copper, and selenium with sleep disorders in the American adults: Data from NHANES 2011–2016. J. Affect. Disord. 2023, 323, 378–385. [Google Scholar] [CrossRef]
- Lu, Y.; Liu, Q.; Zhang, T.; Cai, J.; Xu, T.; Wei, Y.; Mo, X.; Huang, S.; Lin, Y.; Li, Y.; et al. Association between multiple metals exposure and sleep disorders in a Chinese population: A mixture-based approach. Chemosphere 2023, 343, 140213. [Google Scholar] [CrossRef]
- Jia, Y.; Sun, J.; Chen, L.; Xue, Y. Associations of Serum Zinc, Copper, and Zinc/Copper Ratio with Sleep Duration in Adults. Biol. Trace Elem. Res. 2021, 200, 2651–2659. [Google Scholar] [CrossRef]
- Aşker, S.; Asker, M.; Yeltekin, A.Ç.; Aslan, M.; Demir, H. Serum levels of trace minerals and heavy metals in severe obstructive sleep apnea patients: Correlates and clinical implications. Sleep Breath. 2015, 19, 547–552. [Google Scholar] [CrossRef]
- Hashimoto, A.; Inoue, H.; Kuwano, T. Low energy intake and dietary quality are associated with low objective sleep quality in young Japanese women. Nutr. Res. 2020, 80, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Ji, X.; Compher, C.W.; Irving, S.Y.; Kim, J.; Dinges, D.F.; Liu, J. Serum micronutrient status, sleep quality and neurobehavioural function among early adolescents. Public Health Nutr. 2021, 24, 5815–5825. [Google Scholar] [CrossRef]
- Song, C.-H.; Kim, Y.H.; Jung, K.I. Associations of Zinc and Copper Levels in Serum and Hair with Sleep Duration in Adult Women. Biol. Trace Elem. Res. 2012, 149, 16–21. [Google Scholar] [CrossRef]
- Zhu, Z.; Wang, Y.; Wang, Y.; Fu, M.; Luo, X.; Wang, G.; Zhang, J.; Yang, X.; Shan, W.; Li, C.; et al. The association of mixed multi-metal exposure with sleep duration and self-reported sleep disorder: A subgroup analysis from the National Health and Nutrition Examination Survey (NHANES). Environ. Pollut. 2024, 361, 124798. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, C.; Lu, L.; Knutson, K.L.; Carnethon, M.R.; Fly, A.D.; Luo, J.; Haas, D.M.; Shikany, J.M.; Kahe, K. Association of magnesium intake with sleep duration and sleep quality: Findings from the CARDIA study. Sleep 2021, 45, zsab276. [Google Scholar] [CrossRef] [PubMed]
- Luojus, M.K.; Lehto, S.M.; Tolmunen, T.; Elomaa, A.-P.; Kauhanen, J. Serum copper, zinc and high-sensitivity C-reactive protein in short and long sleep duration in ageing men. J. Trace Elem. Med. Biol. Organ Soc. Miner. Trace Elem. 2015, 32, 177–182. [Google Scholar] [CrossRef]
- Audina, N.E.; Hatsu, I.E.; Robinette, L.M.; Johnstone, J.M.; Leung, B.M.Y.; Ast, H.K.; Arnold, L.E. Baseline Micronutrients Status and Sleep Quality in Children With Attention Deficit/Hyperactivity Disorder (ADHD): Secondary Analysis of MADDY RCT. Curr. Dev. Nutr. 2024, 8, 103180. [Google Scholar] [CrossRef]
- Azadi, N.A.; Nakhaee, S.; Hassan, N.E.; Mansouri, B.; Ariyaee, M. Role of toxic and essential elements in sleep duration of patients with cardiovascular diseases. Sci. Rep. 2025, 15, 2392. [Google Scholar] [CrossRef]
- Tunc, M.; Soysal, P.; Pasin, O.; Smith, L.; Rahmati, M.; Yigitalp, V.; Sahin, S.; Dramé, M. Hypomagnesemia Is Associated with Excessive Daytime Sleepiness, but Not Insomnia, in Older Adults. Nutrients 2023, 15, 2467. [Google Scholar] [CrossRef]
- Ersan, B.; Özgen Özkaya, Ş. Is there a relationship between sleep quality, dietary intake and weight gain in Turkish pregnant women? BMC Pregnancy Childbirth 2025, 25, 808. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Prevention CfDCa. Adult BMI Categories: Centers for Disease Control and Prevention. 2024. Available online: https://www.cdc.gov/bmi/adult-calculator/bmi-categories.html (accessed on 13 November 2025).
- Negrea, L.; DeLozier, S.J.; Janes, J.L.; Rahman, M.; Dobre, M. Serum Magnesium and Cardiovascular Outcomes and Mortality in CKD: The Chronic Renal Insufficiency Cohort (CRIC). Kidney Med. 2021, 3, 183–192.e1. [Google Scholar] [CrossRef]
- Yokokawa, H.; Morita, Y.; Hamada, I.; Ohta, Y.; Fukui, N.; Makino, N.; Ohata, E.; Naito, T. Demographic and clinical characteristics of patients with zinc deficiency: Analysis of a nationwide Japanese medical claims database. Sci. Rep. 2024, 14, 2791. [Google Scholar] [CrossRef] [PubMed]
- Dìez, M.; Cerdàn, F.J.; Arroyo, M.; Balibrea, J.L. Use of the copper/zinc ratio in the diagnosis of lung cancer. Cancer 1989, 63, 726–730. [Google Scholar] [CrossRef]
- Suleiman, K.H.; Yates, B.C.; Berger, A.M.; Pozehl, B.; Meza, J. Translating the Pittsburgh Sleep Quality Index into Arabic. West. J. Nurs. Res. 2010, 32, 250–268. [Google Scholar] [CrossRef]
- Institute of Medicine Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. The National Academies Collection: Reports funded by National Institutes of Health. In Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride; National Academies Press (US): Washington, DC, USA, 1997. [Google Scholar]
- Doyle, C.; Khan, A.; Burton, N. Reliability and validity of a self-administered Arabic version of the Global Physical Activity Questionnaire (GPAQ-A). J. Sports Med. Phys. Fitness 2019, 59, 1221–1228. [Google Scholar] [CrossRef]
- Alqahtani, B.A. Association between Physical Frailty and Sleep Quality among Saudi Older Adults: A Community-Based, Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 12741. [Google Scholar] [CrossRef] [PubMed]
- Alhoqail, A.A.; Aburisheh, K.H.; Alammar, A.M.; Bin Mugren, M.A.; Shadid, A.M.; Aldakhil, I.K.; Enabi, H.M.K.; Alotaibi, F.N. Sleep Quality Assessment and Its Predictors Among Saudi Adults with Type 1 and Type 2 Diabetes: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2024, 21, 1437. [Google Scholar] [CrossRef] [PubMed]
- Wali, S.O.; Alghamdi, L.; Alsubhi, L.; Alghamdi, R.; Aljahdaly, N.; Barashid, M.; Wazira, L.A.; Batawi, G.A.; Manzar, M.D.; Alshumrani, R.A.; et al. Prevalence of poor sleep quality among physicians and nurses in a tertiary health care center. Chest 2023, 164, A6278. [Google Scholar] [CrossRef]
- Mahfouz, M.S.; Ali, S.A.; Bahari, A.Y.; Ajeebi, R.E.; Sabei, H.J.; Somaily, S.Y.; Madkhali, Y.A.; Hrooby, R.H.; Shook, R.N. Association between sleep quality and physical activity in Saudi Arabian University students. Nat. Sci. Sleep 2020, 12, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Tang, M.; Wei, X.; Peng, Y. Association between magnesium deficiency score and sleep quality in adults: A population-based cross-sectional study. J. Affect. Disord. 2024, 358, 105–112. [Google Scholar] [CrossRef]
- Ji, X.; Liu, J. Associations between blood zinc concentrations and sleep quality in childhood: A cohort study. Nutrients 2015, 7, 5684–5696. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Nakayama, A.; Kanbe, H.; Kato, M.; Saito, Y.; Adachi, M.; Kondon, N.; Iida, T. A knowledge about the relationship between dietary habits and sleep quality. J. Anal. Bio-Sci. 2013, 36, 181–185. [Google Scholar]
- Malavolta, M.; Piacenza, F.; Basso, A.; Giacconi, R.; Costarelli, L.; Mocchegiani, E. Serum copper to zinc ratio: Relationship with aging and health status. Mech. Ageing Dev. 2015, 151, 93–100. [Google Scholar] [CrossRef]
| Parameters | PSQI-G (PSQI ≤ 5) | PSQI-P (PSQI > 5) | p-Value ⁂ | p-Value (B. Adj.) |
|---|---|---|---|---|
| N | 351 | 690 | ||
| Age (years) | 32.7 ± 12.8 | 31.3 ± 11.9 | 0.082 | -- |
| BMI (kg/m2) | 26.1 ± 5.8 | 27.2 ± 6.3 | 0.012 | -- |
| Male/Female | 155/196 | 242/448 | 0.004 | -- |
| Fat (%) | 33.6 ± 10.5 | 35.4 ± 10.6 | 0.007 | 0.237 |
| SBP (mmHg) | 112.4 ± 15.3 | 111.1 ± 15.9 | 0.216 | 0.597 |
| DBP (mmHg) | 73.6 ± 10.5 | 75.3 ± 10.9 | 0.020 | 0.005 * |
| Serum Mg (mg/dL) | 1.8 ± 0.5 | 1.7 ± 0.4 | 0.007 | 0.015 * (0.036) |
| Serum Zn (µg/dL) | 116.4 ± 26.4 | 112.2 ± 26.0 | 0.019 | 0.058 (0.232) |
| Serum Cu (µg/dL) | 117.1 ± 18.9 | 116.7 ± 18.4 | 0.835 | 0.311 (1.00) |
| Serum Cu/Zn Ratio | 1.2 ± 0.2 | 1.2 ± 0.3 | 0.154 | 0.730 (1.00) |
| Dietary Mg (per 1000 Kcal) | 108.7 (89.3–136.5) | 104.4 (84.4–129.3) | 0.015 | 0.005 * (0.015) |
| Dietary Zn (per 1000 Kcal) | 3.8 (3.0–4.7) | 3.6 (2.9–4.5) | 0.066 | 0.716 (1.00) |
| Dietary Cu (per 1000 Kcal) | 0.5 (0.4–0.7) | 0.5 (0.4–0.6) | 0.059 | 0.123 (0.369) |
| GPAQ Score | 199 (56.7) | 366 (53.0) | 0.264 | 0.477 |
| Smoking (Yes, %) | 41 (11.7) | 105 (15.2) | 0.120 | 0.024 |
| Prescription Medication Use (Not Sleep Aid) (Yes, %) | 17 (4.8) | 48 (7.0) | 0.183 | 0.024 |
| Multivitamin Supplement Intake (Yes, %) | 81 (23.1) | 181 (26.2) | 0.267 | 0.195 |
| Mineral/Index | Tertile/Quantile | Tertile/Quantile (B. Adj.) | Tertile/Quantile (B. Adj.) | |
|---|---|---|---|---|
| Mg | Mean Serum Level (mg/dL) | 1.2 ± 0.4 | 1.9 ± 0.1 | 2.1 ± 0.2 |
| OR for PSQI-P (95% CI) | -- | 1.2 (0.7–2.0) | 0.7 (0.4–1.2) | |
| p-value (B. Adj.) | -- | 0.569 (1.000) | 0.226 (1.000) | |
| Zn | Mean Serum Level (µg/dL) | 90.6 ± 10.5 | 109.1 ± 4.4 | 141.8 ± 24.0 |
| OR for PSQI-P (95% CI) | -- | 1.0 (0.7–1.4) | 0.6 (0.4–0.9) | |
| p-Value (B. Adj.) | -- | 0.901 (1.000) | 0.006 (0.040) | |
| Cu | Mean Serum Level (µg/dL) | 95.1 ± 9.3 | 119.5 ± 6.0 | 137.1 ± 5.9 |
| OR for PSQI-P (95% CI) | -- | 0.9 (0.6–1.3) | 0.7 (0.5–0.8) | |
| p-Value (B. Adj.) | -- | 0.554 (1.000) | 0.036 (0.280) | |
| Cu/Zn ratio | Mean Serum Level | 0.9 ± 0.1 | 1.2 ± 0.1 | 1.5 ± 0.2 |
| OR for PSQI-P (95% CI) | -- | 1.3 (0.8–2.3) | 1.3 (0.7–2.2) | |
| p-Value (B. Adj.) | -- | 0.315 (1.000) | 0.343 (1.000) | |
| Mineral/Index | Deficient | Crude | Model 1 | Model 2 | |||
|---|---|---|---|---|---|---|---|
| N (%) | OR (95% CI) | p-Value (B. Adj.) | OR (95% CI) | p-Value (B. Adj.) | OR (95% CI) | p-Value (B. Adj.) | |
| Mg deficiency (<1.8 mg/dL) | 360 (38.6) | 1.3 (1.0–1.7) | 0.048 * (0.065) | 1.3 (1.0–1.7) | 0.081 (0.324) | 1.2 (0.9–1.6) | 0.147 (0.588) |
| Zn deficiency (<80 µg/dL) | 42 (4.5) | 3.3 (1.4–8.0) | 0.007 * (0.028) | 3.1 (1.3–7.5) | 0.011 * (0.044) | 2.8 (1.1–6.8) | 0.024 * (0.043) |
| Cu deficiency (<119 µg/dL) | 182 (48.0) | 1.0 (0.7–1.6) | 0.868 (1.000) | 1.0 (0.7–1.6) | 0.892 (1.000) | 1.2 (0.7–1.9) | 0.461 (1.000) |
| Cu/Zn ratio (>1.72 µg/dL) | 15 (4.0) | 6.3 (0.8–48.5) | 0.077 (0.308) | 6.3 (0.8–49.2) | 0.078 (0.312) | 5.0 (0.6–40.3) | 0.131 (0.524) |
| Dietary Mg < DRI | 981 (94.2) | 2.2 (1.3–3.7) | 0.003 (0.009) | 1.9 (1.1–3.2) | 0.025 (0.075) | 1.8 (1.0–3.1) | 0.04 (0.120) |
| Dietary Zn < DRI | 774 (74.4) | 1.2 (0.9–1.6) | 0.178 (0.534) | 1.0 (0.7–1.4) | 0.914 (1.000) | 1.1 (0.8–1.5) | 0.67 (1.000) |
| Dietary Cu < DRI | 398 (38.2) | 1.1 (0.8–1.4) | 0.57 (1.000) | 1.0 (0.8–1.3) | 0.911 (1.000) | 1.0 (0.8–1.3) | 0.57 (1.000) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Al-Musharaf, S.; Aldhwayan, M.M.; Mazi, T.A.; Abujabir, O.; Alfawaz, W.; Aljuraiban, G.S. Magnesium and Zinc Are Associated with Sleep Quality in Saudi Adults: Evidence from a Cross-Sectional Study. Nutrients 2026, 18, 114. https://doi.org/10.3390/nu18010114
Al-Musharaf S, Aldhwayan MM, Mazi TA, Abujabir O, Alfawaz W, Aljuraiban GS. Magnesium and Zinc Are Associated with Sleep Quality in Saudi Adults: Evidence from a Cross-Sectional Study. Nutrients. 2026; 18(1):114. https://doi.org/10.3390/nu18010114
Chicago/Turabian StyleAl-Musharaf, Sara, Madhawi M. Aldhwayan, Tagreed A. Mazi, Ohud Abujabir, Waad Alfawaz, and Ghadeer S. Aljuraiban. 2026. "Magnesium and Zinc Are Associated with Sleep Quality in Saudi Adults: Evidence from a Cross-Sectional Study" Nutrients 18, no. 1: 114. https://doi.org/10.3390/nu18010114
APA StyleAl-Musharaf, S., Aldhwayan, M. M., Mazi, T. A., Abujabir, O., Alfawaz, W., & Aljuraiban, G. S. (2026). Magnesium and Zinc Are Associated with Sleep Quality in Saudi Adults: Evidence from a Cross-Sectional Study. Nutrients, 18(1), 114. https://doi.org/10.3390/nu18010114





