The Design and Impact of Teaching Kitchens and Hands-On Cooking Strategies on Diverse Populations: Increasing Evidence of Positive Effects and Proposed Future Directions
1. Introduction
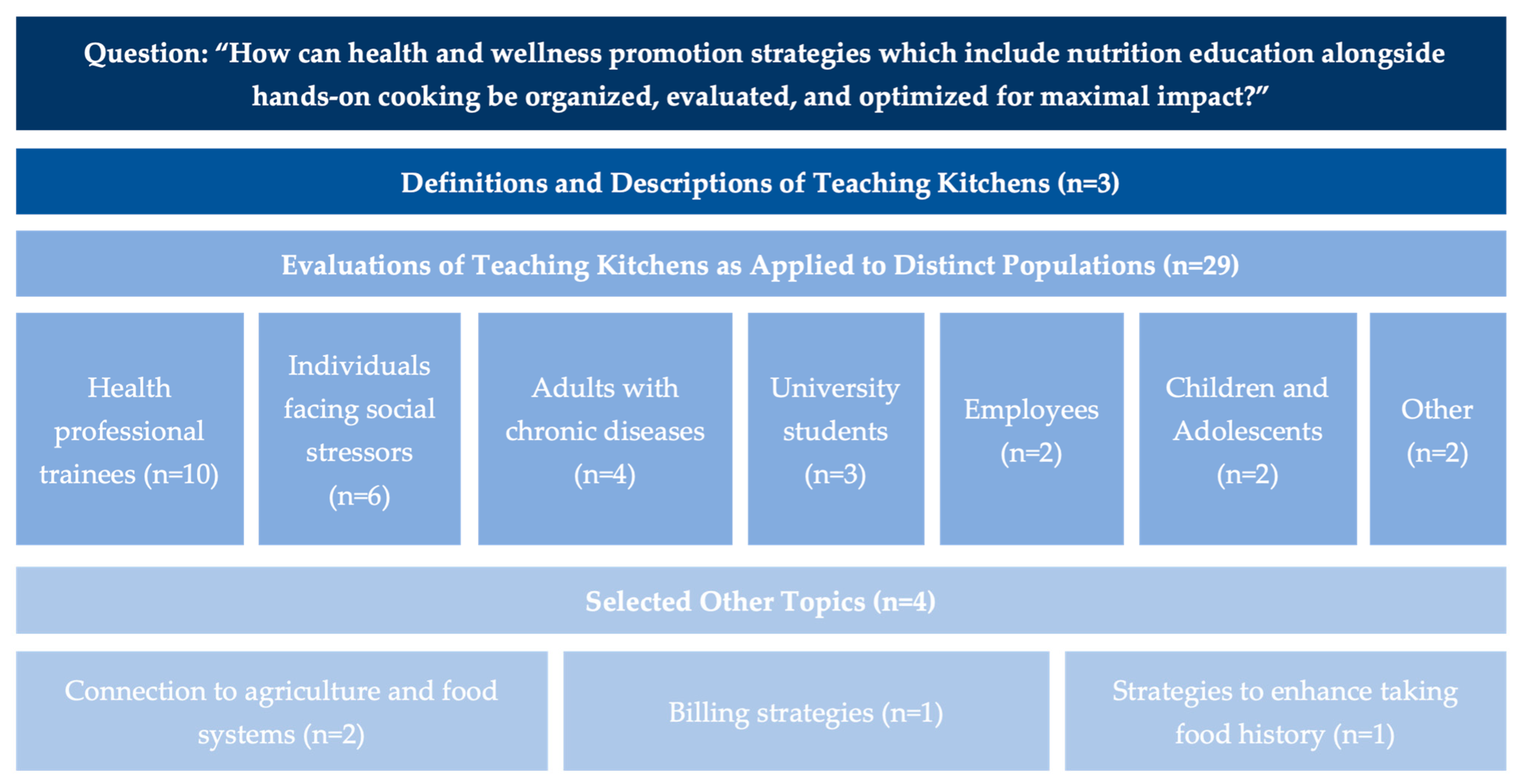
2. Descriptions of Nutrients Special Issue Articles
3. Selected Articles
3.1. Perspective: Teaching Kitchens: Conceptual Origins, Applications and Potential for Impact Within Food Is Medicine Research [2]
3.2. Characteristics of Current Teaching Kitchens: Findings from Recent Surveys of the Teaching Kitchen Collaborative [3]
3.3. “Zoom”ing to the Kitchen: A Novel Approach to Virtual Nutrition Education for Medical Trainees [12]
3.4. Impact of Culinary Medicine Course on Confidence and Competence in Diet and Lifestyle Counseling, Interprofessional Communication, and Health Behaviors and Advocacy [13]
3.5. Assessing Acceptability: The Role of Understanding Participant, Neighborhood, and Community Contextual Factors in Designing a Community-Tailored Cooking Intervention [20]
3.6. Promoting Nutrition and Food Sustainability Knowledge in Apprentice Chefs: An Intervention Study at the School of Italian Culinary Arts—ALMA [26]
3.7. University Students as Change Agents for Health and Sustainability: A Pilot Study on the Effects of a Teaching Kitchen-Based Planetary Health Diet Curriculum [27]
3.8. Effect of the Emory Healthy Kitchen Collaborative on Employee Health Habits and Body Weight: A 12-Month Workplace Wellness Trial [29]
3.9. The Role of Agricultural Systems in Teaching Kitchens: An Integrative Review and Thoughts for the Future [35]
3.10. Culinary Medicine eConsults Pair Nutrition and Medicine: A Feasibility Pilot [36]
3.11. Standard Patient History Can Be Augmented Using Ethnographic Foodlife Questions [37]
4. Discussion
5. Future Research and Educational Opportunities
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FIM | Food is Medicine |
| US | United States |
| MAHA | Make America Healthy Again |
| GLP | Glucagon-like peptide |
| NIH | National Institutes of Health |
| ONR | Office of Nutrition Research |
References
- Eisenberg, D.M. Special Issue: How Can Health and Wellness Promotion Strategies Which Include Nutrition Education alongside Hands-On Cooking Be Organized, Evaluated, and Optimized for Maximal Impact. Nutrients 2023. Available online: https://www.mdpi.com/journal/nutrients/special_issues/F62DAN81H6 (accessed on 11 October 2025).
- Eisenberg, D.M.; Pacheco, L.S.; McClure, A.C.; McWhorter, J.W.; Janisch, K.; Massa, J. Perspective: Teaching Kitchens: Conceptual Origins, Applications and Potential for Impact within Food Is Medicine Research. Nutrients 2023, 15, 2859. [Google Scholar] [CrossRef]
- Badaracco, C.; Thomas, O.W.; Massa, J.; Bartlett, R.; Eisenberg, D.M. Characteristics of Current Teaching Kitchens: Findings from Recent Surveys of the Teaching Kitchen Collaborative. Nutrients 2023, 15, 4326. [Google Scholar] [CrossRef]
- Croxford, S.; Stirling, E.; MacLaren, J.; McWhorter, J.W.; Frederick, L.; Thomas, O.W. Culinary Medicine or Culinary Nutrition? Defining Terms for Use in Education and Practice. Nutrients 2024, 16, 603. [Google Scholar] [CrossRef]
- Lindsay, K.L.; Kennedy, J.; Kim, D.; Kalra, A.; Parekh, N.K. Development of a Culinary Medicine Curriculum to Support Nutrition Knowledge for Gastroenterology Fellows and Faculty. Nutrients 2024, 16, 404. [Google Scholar] [CrossRef]
- Thircuir, S.; Chen, N.N.; Madsen, K.A. Addressing the Gap of Nutrition in Medical Education: Experiences and Expectations of Medical Students and Residents in France and the United States. Nutrients 2023, 15, 5054. [Google Scholar] [CrossRef]
- Donovan, K.; Thomas, O.W.; Sweeney, T.; Ryan, T.J.; Kytomaa, S.; Zhao, M.; Zhong, W.; Long, M.; Rajendran, I.; Sarfaty, S.; et al. Eat to Treat: The Methods and Assessments of a Culinary Medicine Seminar for Future Physicians and Practicing Clinicians. Nutrients 2023, 15, 4819. [Google Scholar] [CrossRef]
- Böttcher, S.; Schonebeck, L.J.; Drösch, L.; Plogmann, A.M.; Leineweber, C.G.; Puderbach, S.; Buhre, C.; Schmöcker, C.; Neumann, U.; Ellrott, T. Comparison of Effectiveness regarding a Culinary Medicine Elective for Medical Students in Germany Delivered Virtually versus In-Person. Nutrients 2023, 15, 4281. [Google Scholar] [CrossRef]
- Ring, M.; Ai, D.; Maker-Clark, G.; Sarazen, R. Cooking up Change: DEIB Principles as Key Ingredients in Nutrition and Culinary Medicine Education. Nutrients 2023, 15, 4257. [Google Scholar] [CrossRef] [PubMed]
- Thang, C.K.; Guerrero, A.D.; Garell, C.L.; Leader, J.K.; Lee, E.; Ziehl, K.; Carpenter, C.L.; Boyce, S.; Slusser, W. Impact of a Teaching Kitchen Curriculum for Health Professional Trainees in Nutrition Knowledge, Confidence, and Skills to Advance Obesity Prevention and Management in Clinical Practice. Nutrients 2023, 15, 4240. [Google Scholar] [CrossRef] [PubMed]
- Maker-Clark, G.; McHugh, A.; Shireman, H.; Hernandez, V.; Prasad, M.; Xie, T.; Parkhideh, A.; Lockwood, C.; Oyola, S. Empowering Future Physicians and Communities on Chicago’s South Side through a 3-Arm Culinary Medicine Program. Nutrients 2023, 15, 4212. [Google Scholar] [CrossRef] [PubMed]
- Charles, J.A.; Wood, N.I.; Neary, S.; Moreno, J.O.; Scierka, L.; Brink, B.; Zhao, X.; Gielissen, K.A. “Zoom”ing to the Kitchen: A Novel Approach to Virtual Nutrition Education for Medical Trainees. Nutrients 2023, 15, 4166. [Google Scholar] [CrossRef]
- Brennan, B.R.; Beals, K.A.; Burns, R.D.; Chow, C.J.; Locke, A.B.; Petzold, M.P.; Dvorak, T.E. Impact of Culinary Medicine Course on Confidence and Competence in Diet and Lifestyle Counseling, Interprofessional Communication, and Health Behaviors and Advocacy. Nutrients 2023, 15, 4157. [Google Scholar] [CrossRef] [PubMed]
- Shafto, K.; Vandenburgh, N.; Wang, Q.; Breen, J. Experiential Culinary, Nutrition and Food Systems Education Improves Knowledge and Confidence in Future Health Professionals. Nutrients 2023, 15, 3994. [Google Scholar] [CrossRef] [PubMed]
- Domper, J.; Gayoso, L.; Goni, L.; Perezábad, L.; Razquin, C.; de la O, V.; Etxeberria, U.; Ruiz-Canela, M. An Intensive Culinary Intervention Programme to Promote Healthy Ageing: The SUKALMENA-InAge Feasibility Pilot Study. Nutrients 2024, 16, 1735. [Google Scholar] [CrossRef]
- Huang, S.; Riccardi, D.; Pflanzer, S.; Redwine, L.S.; Gray, H.L.; Carson, T.L.; McDowell, M.; Thompson, Z.; Hubbard, J.J.; Pabbathi, S. Survivors Overcoming and Achieving Resiliency (SOAR): Mindful Eating Practice for Breast Cancer Survivors in a Virtual Teaching Kitchen. Nutrients 2023, 15, 4205. [Google Scholar] [CrossRef]
- Tanumihardjo, J.P.; Davis, H.; Zhu, M.; On, H.; Guillory, K.K.; Christensen, J. Enhancing Chronic-Disease Education through Integrated Medical and Social Care: Exploring the Beneficial Role of a Community Teaching Kitchen in Oregon. Nutrients 2023, 15, 4368. [Google Scholar] [CrossRef]
- McGuire, M.F.; Chen, P.M.; Smith-Morris, C.; Albin, J.; Siler, M.D.; Lopez, M.A.; Pruitt, S.L.; Merrill, V.C.; Bowen, M.E. Redesigning Recruitment and Engagement Strategies for Virtual Culinary Medicine and Medical Nutrition Interventions in a Randomized Trial of Patients with Uncontrolled Type 2 Diabetes. Nutrients 2023, 15, 4124. [Google Scholar] [CrossRef] [PubMed]
- French, M.L.; Christensen, J.T.; Estabrooks, P.A.; Hernandez, A.M.; Metos, J.M.; Marcus, R.L.; Thorpe, A.; Dvorak, T.E.; Jordan, K.C. Evaluation of the Effectiveness of a Bilingual Nutrition Education Program in Partnership with a Mobile Health Unit. Nutrients 2024, 16, 618. [Google Scholar] [CrossRef]
- Farmer, N.; Tuason, R.; Middleton, K.R.; Ude, A.; Tataw-Ayuketah, G.; Flynn, S.; Kazmi, N.; Baginski, A.; Mitchell, V.; Powell-Wiley, T.M.; et al. Assessing Acceptability: The Role of Understanding Participant, Neighborhood, and Community Contextual Factors in Designing a Community-Tailored Cooking Intervention. Nutrients 2024, 16, 463. [Google Scholar] [CrossRef]
- Wetherill, M.S.; Caywood, L.T.; Hollman, N.; Carter, V.P.; Gentges, J.; Sims, A.; Henderson, C.V. Food Is Medicine for Individuals Affected by Homelessness: Findings from a Participatory Soup Kitchen Menu Redesign. Nutrients 2023, 15, 4417. [Google Scholar] [CrossRef]
- Herman, D.R.; Kimmel, R.; Shodahl, S.; Vargas, J.H. Examination of an Online Cooking Education Program to Improve Shopping Skills, Attitudes toward Cooking, and Cooking Confidence among WIC Participants. Nutrients 2023, 15, 4177. [Google Scholar] [CrossRef]
- Ylitalo, K.R.; Janda, K.M.; Clavon, R.; Raleigh-Yearby, S.; Kaliszewski, C.; Rumminger, J.; Hess, B.; Walter, K.; Cox, W. Cross-Sector Partnerships for Improved Cooking Skills, Dietary Behaviors, and Belonging: Findings from a Produce Prescription and Cooking Education Pilot Program at a Federally Qualified Health Center. Nutrients 2023, 15, 4098. [Google Scholar] [CrossRef]
- Temelkova, S.; Lofton, S.; Lo, E.; Wise, J.; McDonald, E.K. Nourishing Conversations: Using Motivational Interviewing in a Community Teaching Kitchen to Promote Healthy Eating via a Food as Medicine Intervention. Nutrients 2024, 16, 960. [Google Scholar] [CrossRef] [PubMed]
- French, C.D.; Gomez-Lara, A.; Hee, A.; Shankar, A.; Song, N.; Campos, M.; McCoin, M.; Matias, S.L. Impact of a Food Skills Course with a Teaching Kitchen on Dietary and Cooking Self-Efficacy and Behaviors among College Students. Nutrients 2024, 16, 585. [Google Scholar] [CrossRef]
- Franchini, C.; Biasini, B.; Giopp, F.; Rosi, A.; Scazzina, F. Promoting Nutrition and Food Sustainability Knowledge in Apprentice Chefs: An Intervention Study at The School of Italian Culinary Arts—ALMA. Nutrients 2024, 16, 537. [Google Scholar] [CrossRef] [PubMed]
- Rosenau, N.; Neumann, U.; Hamblett, S.; Ellrott, T. University Students as Change Agents for Health and Sustainability: A Pilot Study on the Effects of a Teaching Kitchen-Based Planetary Health Diet Curriculum. Nutrients 2024, 16, 521. [Google Scholar] [CrossRef] [PubMed]
- Daker, R.; Challamel, G.; Hanson, C.; Upritchard, J. Cultivating Healthier Habits: The Impact of Workplace Teaching Kitchens on Employee Food Literacy. Nutrients 2024, 16, 865. [Google Scholar] [CrossRef]
- Bergquist, S.H.; Wang, D.; Fall, R.; Bonnet, J.P.; Morgan, K.R.; Munroe, D.; Moore, M.A. Effect of the Emory Healthy Kitchen Collaborative on Employee Health Habits and Body Weight: A 12-Month Workplace Wellness Trial. Nutrients 2024, 16, 517. [Google Scholar] [CrossRef]
- Marconi, S.; Covolo, L.; Marullo, M.; Zanini, B.; Viola, G.C.V.; Gelatti, U.; Maroldi, R.; Latronico, N.; Castellano, M. Cooking Skills, Eating Habits and Nutrition Knowledge among Italian Adolescents during COVID-19 Pandemic: Sub-Analysis from the Online Survey COALESCENT (Change amOng ItAlian adoLESCENTs). Nutrients 2023, 15, 4143. [Google Scholar] [CrossRef]
- Rivera, N.; Nguyen, K.; Kalami, V.; Qin, F.; Mathur, M.B.; Blankenburg, R.; Yeh, A.M. A Specific Carbohydrate Diet Virtual Teaching Kitchen Curriculum Promotes Knowledge and Confidence in Caregivers of Pediatric Patients with Inflammatory Bowel Disease. Nutrients 2023, 15, 3999. [Google Scholar] [CrossRef]
- Moore, S.G.; Kundra, A.; Ho, P.; Bissell, E.; Apekey, T. Feasibility of a Community Healthy Eating and Cooking Intervention Featuring Traditional African Caribbean Foods from Participant and Staff Perspectives. Nutrients 2023, 15, 3758. [Google Scholar] [CrossRef]
- Polak, R.; Finkelstein, A.; Budd, M.A.; Gray, B.E.; Robinson, H.; Silver, J.K.; Faries, M.D.; Tirosh, A. Expectations from a Home Cooking Program: Qualitative Analyses of Perceptions from Participants in “Action” and “Contemplation” Stages of Change, before Entering a Bi-Center Randomized Controlled Trial. Nutrients 2023, 15, 2082. [Google Scholar] [CrossRef] [PubMed]
- Fals, A.M.; Brennan, A.M. Teaching Kitchens and Culinary Gardens as Integral Components of Healthcare Facilities Providing Whole Person Care: A Commentary. Nutrients 2023, 15, 4162. [Google Scholar] [CrossRef]
- Cole, A.; Pethan, J.; Evans, J. The Role of Agricultural Systems in Teaching Kitchens: An Integrative Review and Thoughts for the Future. Nutrients 2023, 15, 4045. [Google Scholar] [CrossRef] [PubMed]
- Albin, J.L.; Siler, M.; Kitzman, H. Culinary Medicine eConsults Pair Nutrition and Medicine: A Feasibility Pilot. Nutrients 2023, 15, 2816. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; McWhorter, J.W.; Bryant, G.; Zisser, H.; Eisenberg, D.M. Standard Patient History Can Be Augmented Using Ethnographic Foodlife Questions. Nutrients 2023, 15, 4272. [Google Scholar] [CrossRef]
- Albin, J.; Wong, W.; Siler, M.; Bowen, M.E.; Kitzman, H. A Novel Culinary Medicine Service Line: Practical Strategy for Food as Medicine. NEJM Catal. Innov. Care Deliv. 2025, 6, CAT-24. [Google Scholar] [CrossRef]
- Vanderweele, T.J. On the promotion of human flourishing. Proc. Natl. Acad. Sci. USA 2017, 114, 8148–8156. [Google Scholar] [CrossRef]
- Maurana, C.A.; Fritz, J.D.; Witten, A.A.; Williams, S.E.; Ellefson, K.A. Advancing flourishing as the north star of medical education: A call for personal and professional development as key to becoming physicians. Med. Teach. 2024, 46, 1539–1543. [Google Scholar] [CrossRef]
- Haramati, A. Importance of Mind-Body Medicine and Human Flourishing in the Training of Physicians. Marshall J. Med. 2024, 10, 1. [Google Scholar] [CrossRef]
- Teaching Kitchen Preps Families for a Feast—The Children’s Inn at NIH. Available online: https://childrensinn.org/stories/teaching-kitchen/ (accessed on 6 September 2025).
- National Institutes of Health. Office of Nutrition Research Strategic Plan, Fiscal Years 2026–2030. Available online: https://dpcpsi.nih.gov/onr/onr-strategic-plan (accessed on 6 September 2025).
- Lynch, C.J. A Concept for Comprehensive Food is Medicine Networks or Centers of Excellence. Am. J. Clin. Nutr. 2023, 118, 10–12. [Google Scholar] [CrossRef]
- HHS Demands Nutrition Education Reforms in Medical Schools | Nutrition | JAMA | JAMA Network. Available online: https://jamanetwork.com/journals/jama/article-abstract/2839214 (accessed on 11 October 2025).
- Secretaries Kennedy, McMahon Demand Comprehensive Nutrition Education Reforms|HHS.gov. U.S. Department of Health and Human Services. 27 August 2025. Available online: https://www.hhs.gov/press-room/hhs-education-nutrition-medical-training-reforms.html (accessed on 11 October 2025).
- Kennedy, R.F., Jr. RFK Jr.: An Apple a Day Is a Good Prescription. Wall Street Journal. 27 August 2025. Available online: https://www.wsj.com/opinion/an-apple-a-day-is-a-good-prescription-kennedy-hhs-diet-health-73227a67 (accessed on 16 October 2025).
- Pang, B.; Memel, Z.; Diamant, C.; Clarke, E.; Chou, S.; Gregory, H. Culinary medicine and community partnership: Hands-on culinary skills training to empower medical students to provide patient-centered nutrition education. Med. Educ. Online 2019, 24, 1630238. [Google Scholar] [CrossRef] [PubMed]
- Magallanes, E.; Sen, A.; Siler, M.; Albin, J. Nutrition from the kitchen: Culinary medicine impacts students’ counseling confidence. BMC Med. Educ. 2021, 21, 88. [Google Scholar] [CrossRef]
- Wood, N.I.; Fussell, M.; Benghiat, E.; Silver, L.; Goldstein, M.; Ralph, A.; Mastroianni, L.; Spatz, E.; Small, D.; Fisher, R.; et al. A Randomized Controlled Trial of a Culinary Medicine Intervention in a Virtual Teaching Kitchen for Primary Care Residents. J. Gen. Intern. Med. 2025, 40, 2668–2678. [Google Scholar] [CrossRef]
- Razavi, A.C.; Latoff, A.; Dyer, A.; Albin, J.L.; Artz, K.; Babcock, A.; Cimino, F.; Daghigh, F.; Dollinger, B.; Fiellin, M.; et al. Virtual teaching kitchen classes and cardiovascular disease prevention counselling among medical trainees. BMJ Nutr. Prev. Health. 2023, 6, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Ricanati, E.H.; Golubić, M.; Yang, D.; Saager, L.; Mascha, E.J.; Roizen, M.F. Mitigating preventable chronic disease: Progress report of the Cleveland Clinic’s Lifestyle 180 program. Nutr. Metab. 2011, 8, 83. [Google Scholar] [CrossRef]
- Dasgupta, K.; Hajna, S.; Joseph, L.; Da Costa, D.; Christopoulos, S.; Gougeon, R. Effects of meal preparation training on body weight, glycemia, and blood pressure: Results of a phase 2 trial in type 2 diabetes. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 125. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.V.; McWhorter, J.W.; Chow, J.; Danho, M.P.; Weston, S.R.; Chavez, F.; Moore, L.S.; Almohamad, M.; Gonzalez, J.; Liew, E.; et al. Impact of a Virtual Culinary Medicine Curriculum on Biometric Outcomes, Dietary Habits, and Related Psychosocial Factors among Patients with Diabetes Participating in a Food Prescription Program. Nutrients 2021, 13, 4492. [Google Scholar] [CrossRef]
- Schlueter, R.; Calhoun, B.; Harned, E.; Gore, S. A VA Health Care Innovation: Healthier Kidneys Through Your Kitchen—Earlier Nutrition Intervention for Chronic Kidney Disease. J. Ren. Nutr. 2021, 31, 35–38. [Google Scholar] [CrossRef]
- Pritlove, C.; Capone, G.; Kita, H.; Gladman, S.; Maganti, M.; Jones, J.M. Cooking for Vitality: Pilot Study of an Innovative Culinary Nutrition Intervention for Cancer-Related Fatigue in Cancer Survivors. Nutrients 2020, 12, 2760. [Google Scholar] [CrossRef]
- Krenek, A.M.; Aggarwal, M.; Chung, S.T.; Courville, A.B.; Farmer, N.; Guo, J.; Mathews, A. Influence of a Virtual Plant-Based Culinary Medicine Intervention on Mood, Stress, and Quality of Life Among Patients at Risk for Cardiovascular Disease. Nutrients 2025, 17, 1357. [Google Scholar] [CrossRef]
- Pooler, J.A.; Morgan, R.E.; Wong, K.; Wilkin, M.K.; Blitstein, J.L. Cooking Matters for Adults Improves Food Resource Management Skills and Self-confidence Among Low-Income Participants. J. Nutr. Educ. Behav. 2017, 49, 545–553.e1. [Google Scholar] [CrossRef]
- Eisenberg, D.M.; Righter, A.C.; Matthews, B.; Zhang, W.; Willett, W.C.; Massa, J. Feasibility Pilot Study of a Teaching Kitchen and Self-Care Curriculum in a Workplace Setting. Am. J. Lifestyle Med. 2017, 13, 319–330. [Google Scholar] [CrossRef]
- A Culinary-Based Intensive Lifestyle Program for Patients with Obesity: The Teaching Kitchen Collaborative Curriculum (TKCC) Pilot Study—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/40507123/ (accessed on 11 October 2025).
- Novotny, D.; Urich, S.M.; Roberts, H.L. Effectiveness of a Teaching Kitchen Intervention on Dietary Intake, Cooking Self-Efficacy, and Psychosocial Health. Am. J. Health Educ. 2023, 54, 38–49. [Google Scholar] [CrossRef]
- Moore, M.; Wang, D.; Berquist, S.; Bonnet, J.; Rastorguieva, K. Dietary, Cooking, and Eating Pattern Outcomes from the Emory Healthy Kitchen Collaborative. Ann. Fam. Med. 2023, 21 (Suppl. S1), 3761. [Google Scholar] [CrossRef]
- Moore, M.A.; Cousineau, B.A.; Rastorguieva, K.; Bonnet, J.P.; Bergquist, S.H. A Teaching Kitchen Program Improves Employee Micronutrient and Healthy Dietary Consumption. Nutr. Metab. Insights 2023, 16, 11786388231159192. [Google Scholar] [CrossRef] [PubMed]
- Razavi, A.C.; Sapin, A.; Monlezun, D.J.; McCormack, I.G.; Latoff, A.; Pedroza, K.; McCullough, C.; Sarris, L.; Schlag, E.; Dyer, A.; et al. Effect of culinary education curriculum on Mediterranean diet adherence and food cost savings in families: A randomised controlled trial. Public Health Nutr. 2021, 24, 2297–2303. [Google Scholar] [CrossRef] [PubMed]
- Galyean, S.; Alcorn, M.; Chavez, J.; Niraula, S.R.; Childress, A. The effect of culinary medicine to enhance protein intake on muscle quality in older adults: A randomized controlled trial. Aging Clin. Exp. Res. 2025, 37, 171. [Google Scholar] [CrossRef] [PubMed]
| Articles by Core Category | Brief Summary |
|---|---|
| Definitions | |
| Perspective: Teaching Kitchens: Conceptual Origins, Applications and Potential for Impact within Food Is Medicine Research [2] Eisenberg DM, Pacheco LS, McClure AC, McWhorter JW, Janisch K, Massa J | This paper describes the fundamental principles of teaching kitchens, their conceptual origins, and the growing body of evidence demonstrating their effectiveness for various patient populations. Further, it summarizes their anticipated growth trajectory, relevance to other food- and nutrition-related fields of study, variations in teaching kitchen design, and thoughts for future research and practice. |
| Characteristics of Current Teaching Kitchens: Findings from Recent Surveys of the Teaching Kitchen Collaborative [3] Badaracco C, Thomas OW, Massa J, Bartlett R, Eisenberg DM | This paper describes the settings, participants, models, functions, personnel, and funding sources of dozens of existing teaching kitchens and makes recommendations for the continued improvement, expansion, and long-term sustainability of teaching kitchen programs. |
| Culinary Medicine or Culinary Nutrition? Defining Terms for Use in Education and Practice [4] Croxford S, Stirling E, MacLaren J, McWhorter JW, Frederick L, Thomas OW | This paper proposes an introductory model demonstrating the interrelationship between culinary nutrition terms and indicates that multidisciplinary collaboration amongst individuals trained in culinary arts, nutrition, health, and education underpins deployment of effective culinary nutrition interventions. |
| Populations | |
| Health professional trainees | |
| Development of a Culinary Medicine Curriculum to Support Nutrition Knowledge for Gastroenterology Fellows and Faculty [5] Lindsay KL, Kennedy J, Kim D, Kalra A, Parekh NK | This study presents positive findings on the acceptability and relevance of a tailored four-module culinary medicine curriculum delivered through a virtual platform by a chef and registered dietitian for gastroenterology fellows and faculty. |
| Addressing the Gap of Nutrition in Medical Education: Experiences and Expectations of Medical Students and Residents in France and the United States [6] Thircuir S, Chen NN, Madsen KA | This study illustrates the importance of integrating interdisciplinary and systems-based perspectives in nutrition and hands-on culinary teaching to bridge the gap between current medical school training and students’ perceived need to receive enhanced nutrition education in medical training. |
| Eat to Treat: The Methods and Assessments of a Culinary Medicine Seminar for Future Physicians and Practicing Clinicians [7] Donovan K, Thomas OW, Sweeney T, et al. | This study highlights the effectiveness of a six-module hands-on culinary medicine program facilitated by a registered dietitian to improve medical students’ and practicing clinicians’ nutrition knowledge, self-efficacy, and practice-based confidence. |
| Comparison of Effectiveness regarding a Culinary Medicine Elective for Medical Students in Germany Delivered Virtually versus In-Person [8] Böttcher S, Schonebeck LJ, Drösch L, et al. | This study describes a seven-module culinary medicine elective and demonstrates that virtual and in-person teaching kitchen programs are equally effective modalities by which to deliver nutrition education and culinary training to medical students. |
| Cooking up Change: DEIB Principles as Key Ingredients in Nutrition and Culinary Medicine Education [9] Ring M, Ai D, Maker-Clark G, Sarazen R | This paper investigates the current landscape of the topics of diversity, equity, inclusion, and belonging in existing food, nutrition, and health training programs, and proposes a three-tier “Checklist for Culturally Competent Education in Nutrition.” |
| Impact of a Teaching Kitchen Curriculum for Health Professional Trainees in Nutrition Knowledge, Confidence, and Skills to Advance Obesity Prevention and Management in Clinical Practice [10] Thang CK, Guerrero AD, Garell CL, et al. | This paper demonstrates that the Upstream Obesity Solutions curriculum delivered to a variety of health professional trainees—medical students, dental students, nursing students, and pediatric residents—over varying course durations is effective in improving confidence in counseling, nutrition knowledge and literacy, and cooking skills. |
| Empowering Future Physicians and Communities on Chicago’s South Side through a 3-Arm Culinary Medicine Program [11] Maker-Clark G, McHugh A, Shireman H, et al. | This study demonstrates that an eight-session culinary medicine elective improves fourth-year medical students’ confidence in nutrition counseling and personal dietary habits, improves community members’ confidence in chronic disease management and cooking skills, and is well-perceived by middle school participants. |
| “Zoom”ing to the Kitchen: A Novel Approach to Virtual Nutrition Education for Medical Trainees [12] Charles JA, Wood NI, Neary S, et al. | This study presents findings from a three-hour interactive virtual culinary medicine curriculum for first-year physician assistant students and demonstrates effectiveness in improving knowledge, attitudes, and confidence in nutrition counseling. |
| Impact of Culinary Medicine Course on Confidence and Competence in Diet and Lifestyle Counseling, Interprofessional Communication, and Health Behaviors and Advocacy [13] Brennan BR, Beals KA, Burns RD, et al. | This study highlights the effectiveness of an eight-week culinary medicine elective on improving medical and health professional students’ confidence in diet and lifestyle counseling, interprofessional communication, and healthy meal preparation, and demonstrates that these findings are uniform across both in-person and virtual teaching environments. |
| Experiential Culinary, Nutrition and Food Systems Education Improves Knowledge and Confidence in Future Health Professionals [14] Shafto K, Vandenburgh N, Wang Q, Breen J | This study demonstrates that a six-week experiential food systems and culinary nutrition course for health sciences graduate students improves knowledge and attitudes about food skills, food systems, and chronic disease conditions as they relate to basic nutrition concepts. |
| Adults with chronic diseases | |
| An Intensive Culinary Intervention Programme to Promote Healthy Ageing: The SUKALMENA-InAge Feasibility Pilot Study [15] Domper J, Gayoso L, Goni L, et al. | This study suggests that a four-week culinary intervention for older adults with overweight or obesity leads to improvements in Mediterranean diet adherence, cooking confidence, weight, BMI, and waist and hip circumference compared to a nutrition education intervention alone. |
| Survivors Overcoming and Achieving Resiliency (SOAR): Mindful Eating Practice for Breast Cancer Survivors in a Virtual Teaching Kitchen [16] Huang S, Riccardi D, Pflanzer S, et al. | This study demonstrates that a nine-week virtual teaching kitchen intervention delivered by a multidisciplinary team leads to improvements in mindful eating behaviors for survivors of breast cancer. |
| Enhancing Chronic-Disease Education through Integrated Medical and Social Care: Exploring the Beneficial Role of a Community Teaching Kitchen in Oregon [17] Tanumihardjo JP, Davis H, Zhu M, On H, Guillory KK, Christensen J | This study highlights that a community teaching kitchen designed for actively engaged adult patients with one or more chronic diseases may lead to significant clinical improvements such as blood sugar and blood pressure control and help address unmet social needs, including reducing barriers to food access. |
| Redesigning Recruitment and Engagement Strategies for Virtual Culinary Medicine and Medical Nutrition Interventions in a Randomized Trial of Patients with Uncontrolled Type 2 Diabetes [18] McGuire MF, Chen PM, Smith-Morris C, et al. | This study describes barriers and facilitators to patient engagement in virtually delivered culinary medicine and medical nutrition therapy interventions for patients with uncontrolled type 2 diabetes and food insecurity. |
| Individuals facing social stressors | |
| Evaluation of the Effectiveness of a Bilingual Nutrition Education Program in Partnership with a Mobile Health Unit [19] French ML, Christensen JT, Estabrooks PA, et al. | This study reports on a bilingual nutrition education program with a mobile health unit designed for low-income and underserved community residents and indicates that this program achieved effectiveness in improving health and behavioral outcomes, especially for those most at risk. |
| Assessing Acceptability: The Role of Understanding Participant, Neighborhood, and Community Contextual Factors in Designing a Community-Tailored Cooking Intervention [20] Farmer N, Tuason R, Middleton KR, et al. | This study demonstrates that engaging participant perspectives—African American adults with cardiovascular disease risk factors and low food access—increases understanding of the barriers, motivators, environmental factors, and acceptability of health-focused interventions in community-based participatory research. |
| Food Is Medicine for Individuals Affected by Homelessness: Findings from a Participatory Soup Kitchen Menu Redesign [21] Wetherill MS, Caywood LT, Hollman N, et al. | This study describes a participatory-based approach to redesign a food shelter menu for individuals experiencing homelessness by assessing participant nutritional needs and taste preferences and responding with strategic menu guidelines. |
| Examination of an Online Cooking Education Program to Improve Shopping Skills, Attitudes toward Cooking, and Cooking Confidence among WIC Participants [22] Herman DR, Kimmel R, Shodahl S, Vargas JH | This study highlights that a cooking education curriculum delivered virtually to WIC participants leads to improvements in attitudes towards and confidence in cooking skills and cooking healthfully on a budget. |
| Cross-Sector Partnerships for Improved Cooking Skills, Dietary Behaviors, and Belonging: Findings from a Produce Prescription and Cooking Education Pilot Program at a Federally Qualified Health Center [23] Ylitalo KR, Janda KM, Clavon R, et al. | This study demonstrates that a six-week ‘food as medicine’ produce prescription program combined with hands-on cooking education for patients of a federally qualified health center leads to improvements in cooking self-efficacy, diet-related disease management, and daily vegetable intake. |
| Nourishing Conversations: Using Motivational Interviewing in a Community Teaching Kitchen to Promote Healthy Eating via a Food as Medicine Intervention [24] Temelkova S, Lofton S, Lo E, Wise J, McDonald EK 4th | This paper describes the benefits of motivational interviewing techniques in both individual and group settings to drive behavior change for low-income individuals in the context of a six-week cooking and nutrition course. |
| University students | |
| Impact of a Food Skills Course with a Teaching Kitchen on Dietary and Cooking Self-Efficacy and Behaviors among College Students [25] French CD, Gomez-Lara A, Hee A, et al. | This study demonstrates that a 14-week food skills course which includes both didactic and hands-on teaching delivered to college students leads to improvements in healthy cooking and eating behaviors and self-efficacy compared to a control group. |
| Promoting Nutrition and Food Sustainability Knowledge in Apprentice Chefs: An Intervention Study at The School of Italian Culinary Arts—ALMA [26] Franchini C, Biasini B, Giopp F, Rosi A, Scazzina F | This study describes an education intervention on nutrition and food sustainability knowledge for culinary students and demonstrates that the curriculum is effective in improving students’ knowledge and translation to menu design. |
| University Students as Change Agents for Health and Sustainability: A Pilot Study on the Effects of a Teaching Kitchen-Based Planetary Health Diet Curriculum [27] Rosenau N, Neumann U, Hamblett S, Ellrott T | This study indicates that a seven-week planetary health diet elective delivered through a teaching kitchen setting to university students is feasible, well-regarded by participants, and leads to improvements in planetary health diet literacy. |
| Employees | |
| Cultivating Healthier Habits: The Impact of Workplace Teaching Kitchens on Employee Food Literacy [28] Daker R, Challamel G, Hanson C, Upritchard J | This study reports on the impact of an in-person and virtual workplace teaching kitchen on improving food literacy for employees at a multinational technology company and describes engagement strategies for increasing teaching kitchen participation. |
| Effect of the Emory Healthy Kitchen Collaborative on Employee Health Habits and Body Weight: A 12-Month Workplace Wellness Trial [29] Bergquist SH, Wang D, Fall R, et al. | This study presents findings that a 12-month employer-based teaching kitchen program delivered by a multidisciplinary team leads to significant improvements in healthy eating behaviors and cooking confidence for employees at risk of or experiencing chronic diseases. |
| Children and Adolescents | |
| Cooking Skills, Eating Habits and Nutrition Knowledge among Italian Adolescents during COVID-19 Pandemic: Sub-Analysis from the Online Survey COALESCENT (Change amOng ItAlian adoLESCENTs) [30] Marconi S, Covolo L, Marullo M, et al. | This study demonstrates the positive correlation between cooking skills, nutrition knowledge, and healthy eating behaviors—especially reduced consumption of ultra-processed foods—in Italian adolescents. |
| A Specific Carbohydrate Diet Virtual Teaching Kitchen Curriculum Promotes Knowledge and Confidence in Caregivers of Pediatric Patients with Inflammatory Bowel Disease [31] Rivera N, Nguyen K, Kalami V, et al. | This study describes a 90 min virtual teaching kitchen session for caregivers of pediatric patients with inflammatory bowel disease and suggests that hands-on teaching may improve knowledge and attitudes toward a specific carbohydrate diet. |
| Others | |
| Feasibility of a Community Healthy Eating and Cooking Intervention Featuring Traditional African Caribbean Foods from Participant and Staff Perspectives [32] Moore SG, Kundra A, Ho P, Bissell E, Apekey T | This study explores the benefits of integrating participant perspectives—individuals with African Caribbean backgrounds—during program design to develop culturally adapted nutrition interventions which may help increase familiarity and acceptability of the foods offered. |
| Expectations from a Home Cooking Program: Qualitative Analyses of Perceptions from Participants in “Action” and “Contemplation” Stages of Change, before Entering a Bi-Center Randomized Controlled Trial [33] Polak R, Finkelstein A, Budd MA, et al. | This study delineates between “action” and “contemplation” stages of change related to home cooking behaviors for individuals with overweight and describes differences in concerns and expectations about health and lifestyle goals. |
| Others | |
| Connection to agriculture and food systems | |
| Teaching Kitchens and Culinary Gardens as Integral Components of Healthcare Facilities Providing Whole Person Care: A Commentary [34] Fals AM, Brennan AM | This paper explores the potential value of embedding culinary gardens within clinical practice, especially in the context of pediatric obesity management, and presents directions for incorporating teaching kitchens and culinary gardens within both in-person and virtual shared medical appointments to advance value-based care. |
| The Role of Agricultural Systems in Teaching Kitchens: An Integrative Review and Thoughts for the Future [35] Cole A, Pethan J, Evans J | This paper highlights synergies between health practitioners, chefs, and farmers and presents case studies wherein multidisciplinary teams collaborate to advance individual and community health, food is medicine initiatives, and broader planetary health objectives. |
| Billing strategies | |
| Culinary Medicine eConsults Pair Nutrition and Medicine: A Feasibility Pilot [36] Albin JL, Siler M, Kitzman H | This study describes how innovations in clinical workflows can facilitate referrals to a multidisciplinary culinary medicine team, enhancing the delivery of personalized nutrition guidance to patients and strategies for which these services can be routinely billed. |
| Collecting food history | |
| Standard Patient History Can Be Augmented Using Ethnographic Foodlife Questions [37] Lee JJ, McWhorter JW, Bryant G, Zisser H, Eisenberg DM | This paper proposes a novel methodology by which to collect a patient’s food history to increase patient engagement, improve provider understanding, and enhance patient–provider trust. |
| Health Professionals and Trainees | Adults with Chronic Diseases | Individuals Facing Social Stressors | Students | Employees and Others | Children and Adolescents |
|---|---|---|---|---|---|
| Residents Fellows Practicing physicians Registered dietitians Medical students Nursing students Physician assistant students Dental students | Patients experiencing overweight or obesity Patients with type 2 diabetes Breast cancer survivors Patients with kidney disease | WIC recipients Low-income individuals Patients in underserved areas Individuals experiencing food insecurity Individuals experiencing housing instability Veterans | College students Culinary students Health professional graduate students | Professional chefs Community-based leaders Workplace employees Families Older adults | Pediatric patients with inflammatory bowel disease Middle school students High school students |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eisenberg, D.M.; Cole, A.; Pacheco, L.S.; Massa, J.; Haramati, A.; Bremer, A.A. The Design and Impact of Teaching Kitchens and Hands-On Cooking Strategies on Diverse Populations: Increasing Evidence of Positive Effects and Proposed Future Directions. Nutrients 2025, 17, 3638. https://doi.org/10.3390/nu17233638
Eisenberg DM, Cole A, Pacheco LS, Massa J, Haramati A, Bremer AA. The Design and Impact of Teaching Kitchens and Hands-On Cooking Strategies on Diverse Populations: Increasing Evidence of Positive Effects and Proposed Future Directions. Nutrients. 2025; 17(23):3638. https://doi.org/10.3390/nu17233638
Chicago/Turabian StyleEisenberg, David M., Alexis Cole, Lorena S. Pacheco, Jennifer Massa, Aviad Haramati, and Andrew A. Bremer. 2025. "The Design and Impact of Teaching Kitchens and Hands-On Cooking Strategies on Diverse Populations: Increasing Evidence of Positive Effects and Proposed Future Directions" Nutrients 17, no. 23: 3638. https://doi.org/10.3390/nu17233638
APA StyleEisenberg, D. M., Cole, A., Pacheco, L. S., Massa, J., Haramati, A., & Bremer, A. A. (2025). The Design and Impact of Teaching Kitchens and Hands-On Cooking Strategies on Diverse Populations: Increasing Evidence of Positive Effects and Proposed Future Directions. Nutrients, 17(23), 3638. https://doi.org/10.3390/nu17233638





