Health State Utility Associated with Parenteral Nutrition Requirement in Patients with Short Bowel Syndrome and Intestinal Failure in Korea: A Vignette-Based Approach
Abstract
1. Introduction
2. Methods
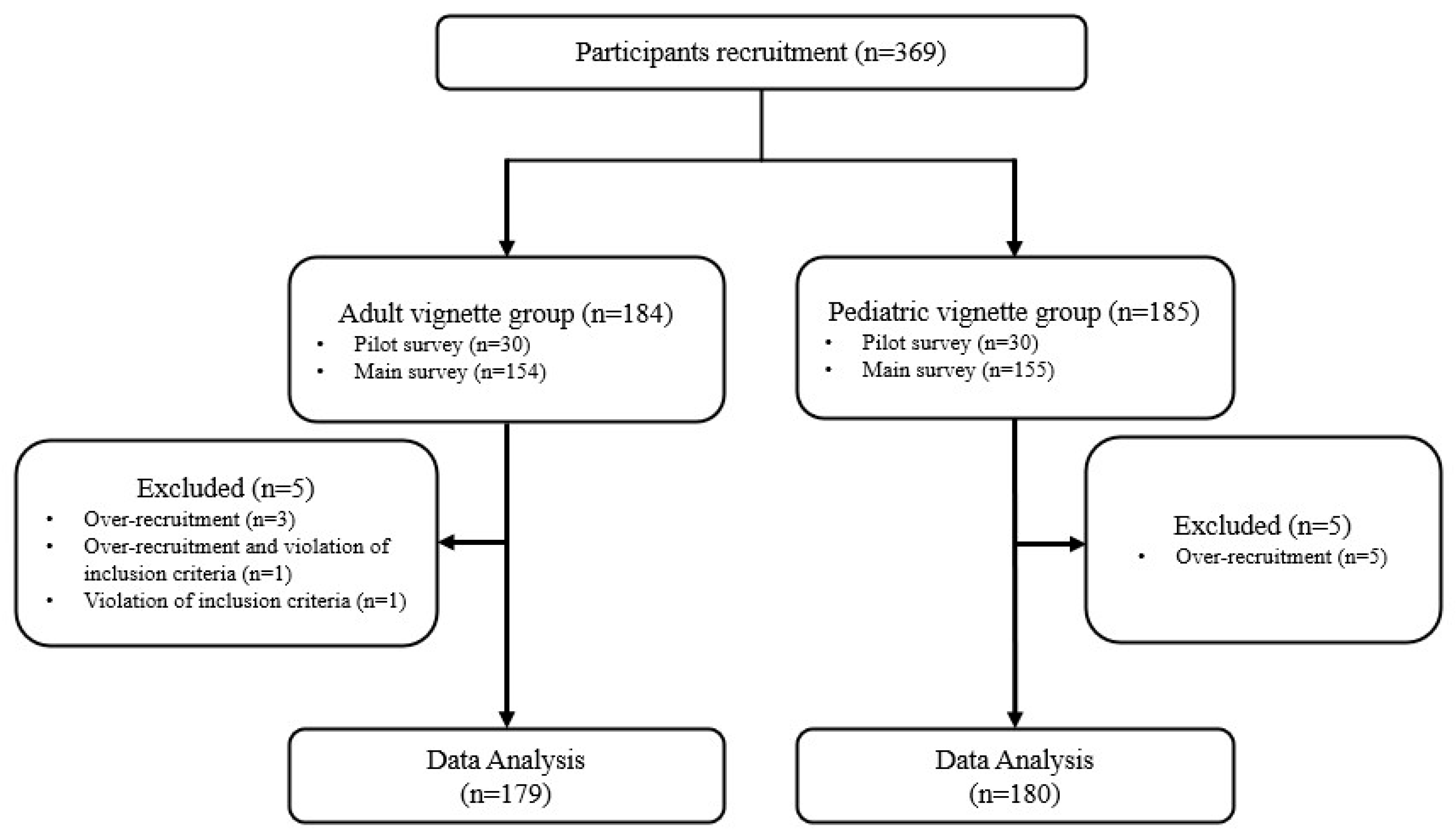
2.1. Sample and Procedures
2.2. Health States Development
2.3. Health State Valuation
2.3.1. EQ-5D-5L
2.3.2. VAS
2.3.3. TTO
2.4. Statistical Analysis
3. Results
3.1. Survey Participants
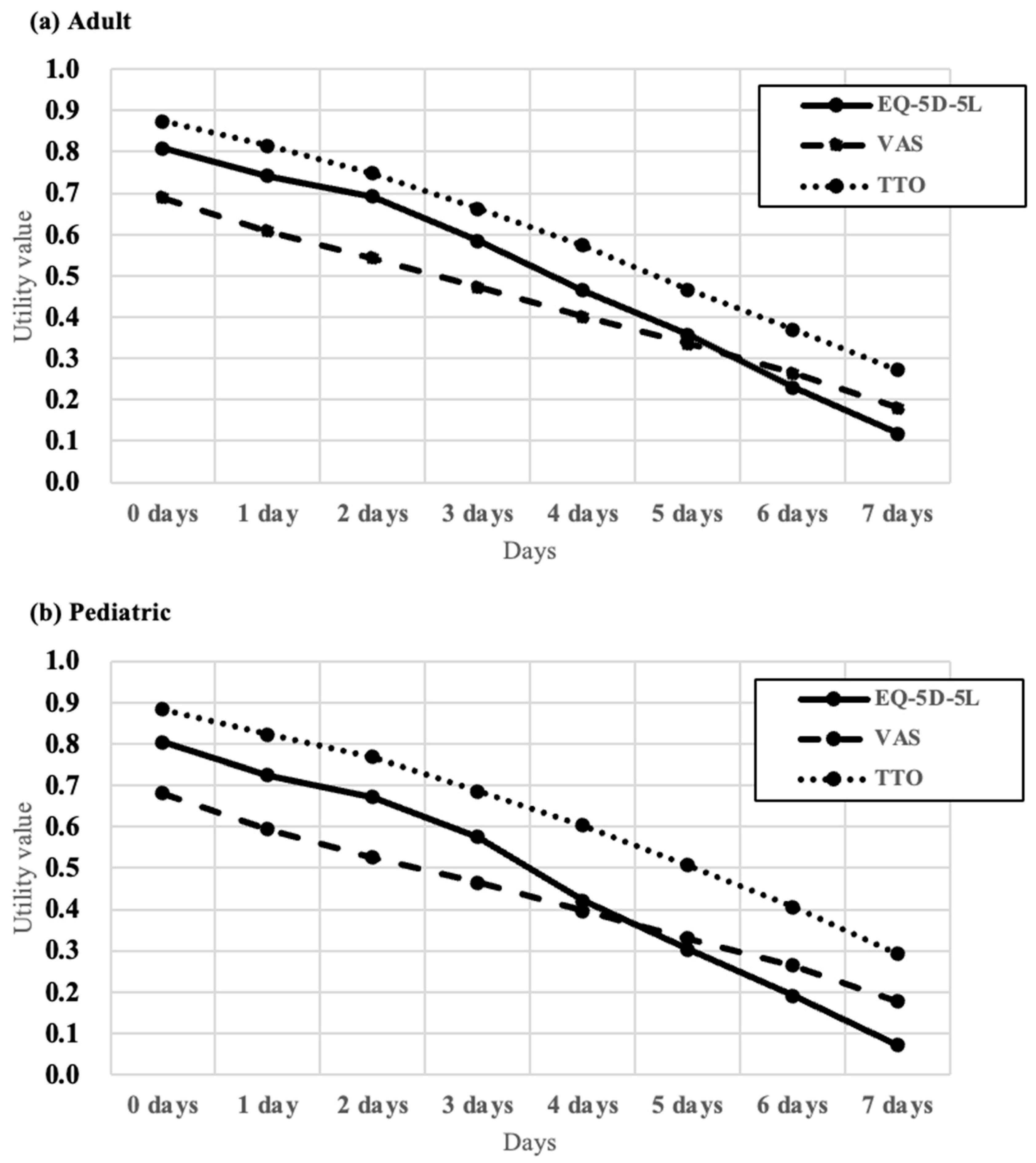
3.2. Health State Utilities
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| −2LL | −2 Log Likelihood |
| AIC | Akaike Information Criterion |
| AICc | Corrected AIC |
| BIC | Bayesian Information Criterion |
| EQ-5D | EuroQol 5-Dimension |
| EQ-5D-5L | 5-level EQ-5D |
| HRQoL | Health-related quality of life |
| ICCs | Intra-class correlation coefficients |
| IF | Intestinal failure |
| KRW | South Korean Won |
| NHI | National Health Insurance |
| PN | Parenteral nutrition |
| QoL | Quality of life |
| SBS | Short bowel syndrome |
| SD | Standard deviation |
| TTO | Time trade-off |
| VAS | Visual analog scale |
References
- Billiauws, L.; Maggiori, L.; Joly, F.; Panis, Y. Medical and surgical management of short bowel syndrome. J. Visc. Surg. 2018, 155, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Amiot, A.; Messing, B.; Corcos, O.; Panis, Y.; Joly, F. Determinants of home parenteral nutrition dependence and survival of 268 patients with non-malignant short bowel syndrome. Clin. Nutr. 2013, 32, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Sigalet, D.L. Short bowel syndrome in infants and children: An overview. Semin. Pediatr. Surg. 2001, 10, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Massironi, S.; Cavalcoli, F.; Rausa, E.; Invernizzi, P.; Braga, M.; Vecchi, M. Understanding short bowel syndrome: Current status and future perspectives. Dig. Liver Dis. 2020, 52, 253–261. [Google Scholar] [CrossRef]
- Lee, T.; Cho, Y.; Park, K. Prevalence and disease burden of patients with short bowel syndrome in Korea. Health Insur. Rev. Assess. Serv. 2018, 2, 34–37. [Google Scholar]
- Nightingale, J.; Woodward, J.M. Guidelines for management of patients with a short bowel. Gut 2006, 55 (Suppl. 4), iv1–iv12. [Google Scholar] [CrossRef]
- Pironi, L.; Steiger, E.; Joly, F.; Jeppesen, P.B.; Wanten, G.; Sasdelli, A.S.; Chambrier, C.; Aimasso, U.; Mundi, M.S.; Szczepanek, K.; et al. Characteristics of adult patients with chronic intestinal failure due to short bowel syndrome: An international multicenter survey. Clin. Nutr. ESPEN 2021, 45, 433–441. [Google Scholar] [CrossRef]
- Woods, A.; Lal, S. Intestinal failure and short bowel syndrome. Medicine 2024, 52, 181–185. [Google Scholar] [CrossRef]
- O’Keefe, S.J.; Buchman, A.L.; Fishbein, T.M.; Jeejeebhoy, K.N.; Jeppesen, P.B.; Shaffer, J. Short bowel syndrome and intestinal failure: Consensus definitions and overview. Clin. Gastroenterol. Hepatol. 2006, 4, 6–10. [Google Scholar] [CrossRef]
- Vugrinec Mamić, M.; Hojsak, I.; Mišak, Z.; Kerman, V.; Kolaček, S. Treatment in a Tertiary Intestinal Rehabilitation Center Improves Outcome for Children With Short Bowel Syndrome. Gastroenterol. Nurs. 2019, 42, 165–168. [Google Scholar] [CrossRef]
- Baxter, J.P.; Fayers, P.M.; McKinlay, A.W. The clinical and psychometric validation of a questionnaire to assess the quality of life of adult patients treated with long-term parenteral nutrition. JPEN J. Parenter. Enter. Nutr. 2010, 34, 131–142. [Google Scholar] [CrossRef]
- Winkler, M.F.; Smith, C.E. Clinical, social, and economic impacts of home parenteral nutrition dependence in short bowel syndrome. JPEN J. Parenter. Enter. Nutr. 2014, 38, 32s–37s. [Google Scholar] [CrossRef]
- Huisman-de Waal, G.; Bazelmans, E.; van Achterberg, T.; Jansen, J.; Sauerwein, H.; Wanten, G.; Schoonhoven, L. Predicting fatigue in patients using home parenteral nutrition: A longitudinal study. Int. J. Behav. Med. 2011, 18, 268–276. [Google Scholar] [CrossRef]
- Jeppesen, P.B.; Langholz, E.; Mortensen, P.B. Quality of life in patients receiving home parenteral nutrition. Gut 1999, 44, 844–852. [Google Scholar] [CrossRef]
- Persoon, A.; Huisman-de Waal, G.; Naber, T.A.; Schoonhoven, L.; Tas, T.; Sauerwein, H.; van Achterberg, T. Impact of long-term HPN on daily life in adults. Clin. Nutr. 2005, 24, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Ballinger, R.; Macey, J.; Lloyd, A.; Brazier, J.; Ablett, J.; Burden, S.; Lal, S. Measurement of Utilities Associated with Parenteral Support Requirement in Patients with Short Bowel Syndrome and Intestinal Failure. Clin. Ther. 2018, 40, 1878–1893.e1871. [Google Scholar] [CrossRef] [PubMed]
- Matza, L.S.; Stewart, K.D.; Lloyd, A.J.; Rowen, D.; Brazier, J.E. Vignette-Based Utilities: Usefulness, Limitations, and Methodological Recommendations. Value Health 2021, 24, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L. Definitions of intestinal failure and the short bowel syndrome. Best. Pract. Res. Clin. Gastroenterol. 2016, 30, 173–185. [Google Scholar] [CrossRef]
- Bae, E.Y.; Hong, J.; Bae, S.; Hahn, S.; An, H.; Hwang, E.J.; Lee, S.M.; Lee, T.J. Korean Guidelines for Pharmacoeconomic Evaluations: Updates in the Third Version. Appl. Health Econ. Health Policy 2022, 20, 467–477. [Google Scholar] [CrossRef]
- Ha, B. Gang Survey. In How to Investigate Ads.; Communication Books: Seoul, Republic of Korea, 2013; pp. 31–39. [Google Scholar]
- Hennink, M.; Kaiser, B.N. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc. Sci. Med. 2022, 292, 114523. [Google Scholar] [CrossRef]
- Torrance, G.W. Utility approach to measuring health-related quality of life. J. Chronic Dis. 1987, 40, 593–603. [Google Scholar] [CrossRef]
- Klose, K.; Kreimeier, S.; Tangermann, U.; Aumann, I.; Damm, K. Patient- and person-reports on healthcare: Preferences, outcomes, experiences, and satisfaction—An essay. Health Econ. Rev. 2016, 6, 18. [Google Scholar] [CrossRef]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Kim, S.H.; Ahn, J.; Ock, M.; Shin, S.; Park, J.; Luo, N.; Jo, M.W. The EQ-5D-5L valuation study in Korea. Qual. Life Res. 2016, 25, 1845–1852. [Google Scholar] [CrossRef]
- Parkin, D.; Devlin, N. Is there a case for using visual analogue scale valuations in cost-utility analysis? Health Econ. 2006, 15, 653–664. [Google Scholar] [CrossRef] [PubMed]
- Song, H.J.; Park, H.; Park, S.Y.; Lee, E.K.; Ha, S.Y.; Park, S.Y.; Bae, E.J.; Ku, H. Estimation of Health Utilities Based on the Response to Treatment in Atopic Dermatitis: A Population-based Study. Clin. Ther. 2019, 41, 700–713. [Google Scholar] [CrossRef] [PubMed]
- Torrance, G.W.; Thomas, W.H.; Sackett, D.L. A utility maximization model for evaluation of health care programs. Health Serv. Res. 1972, 7, 118–133. [Google Scholar]
- Lugnér, A.K.; Krabbe, P.F.M. An overview of the time trade-off method: Concept, foundation, and the evaluation of distorting factors in putting a value on health. Expert. Rev. Pharmacoecon Outcomes Res. 2020, 20, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Attema, A.E.; Edelaar-Peeters, Y.; Versteegh, M.M.; Stolk, E.A. Time trade-off: One methodology, different methods. Eur. J. Health Econ. 2013, 14 (Suppl. 1), S53–S64. [Google Scholar] [CrossRef]
- van Nooten, F.E.; Koolman, X.; Brouwer, W.B.F. The influence of subjective life expectancy on health state valuations using a 10 year TTO. Health Econ. 2009, 18, 549–558. [Google Scholar] [CrossRef]
- Carey, S.; Tu, W.; Hyde-Jones, L.; Koh, C. Assessing Patient Preferences for Intestinal Failure Management Using the Time Trade-Off Methodology. JPEN J. Parenter. Enter. Nutr. 2019, 43, 912–917. [Google Scholar] [CrossRef]
- Muhammad, L.N. Guidelines for repeated measures statistical analysis approaches with basic science research considerations. J. Clin. Investig. 2023, 133, 1–3. [Google Scholar] [CrossRef]
- Chang, Y.H.; Buras, M.R.; Davis, J.M., 3rd; Crowson, C.S. Avoiding Blunders When Analyzing Correlated Data, Clustered Data, or Repeated Measures. J. Rheumatol. 2023, 50, 1269–1272. [Google Scholar] [CrossRef]
- Feeny, D. Preference-Based Measures: Utility And Quality-Adjusted Life Years. In Assessing Quality of Life in Clinical Trials: Methods and Practice; Fayers, P., Hays, R., Eds.; Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Choi, H.S.; Yang, D.W.; Rhee, C.K.; Yoon, H.K.; Lee, J.H.; Lim, S.Y.; Kim, Y.I.; Yoo, K.H.; Hwang, Y.I.; Lee, S.H.; et al. The health-related quality-of-life of chronic obstructive pulmonary disease patients and disease-related indirect burdens. Korean J. Intern. Med. 2020, 35, 1136–1144. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.H.; Lee, J.Y.; Park, S.K.; Nam, J.H.; Song, H.J.; Park, S.Y.; Lee, E.K. The Utility of 5 Hypothetical Health States in Heart Failure Using Time Trade-Off (TTO) and EQ-5D-5L in Korea. Clin. Drug Investig. 2018, 38, 727–736. [Google Scholar] [CrossRef] [PubMed]
- Sera, L.; Miyoung, O.; Seonghee, K.; Hyunah, K. Analysis of Adverse Reactions Associated with Parenteral Nutrition Use in Korea. J. Clin. Nutr. 2017, 9, 16–20. [Google Scholar] [CrossRef]
- Pironi, L.; Goulet, O.; Buchman, A.; Messing, B.; Gabe, S.; Candusso, M.; Bond, G.; Gupte, G.; Pertkiewicz, M.; Steiger, E.; et al. Outcome on home parenteral nutrition for benign intestinal failure: A review of the literature and benchmarking with the European prospective survey of ESPEN. Clin. Nutr. 2012, 31, 831–845. [Google Scholar] [CrossRef]
- Abbas, E.M.; Harshavardhan, R.; Mohammed, H.; Loona, V.; Faseeh, K.M. An assessment of quality of life in ESRD patients undergoing hemodialysis. Egypt. J. Intern. Med. 2024, 36, 104. [Google Scholar] [CrossRef]
- Jeppesen, P.B.; Pertkiewicz, M.; Forbes, A.; Pironi, L.; Gabe, S.M.; Joly, F.; Messing, B.; Loth, S.; Youssef, N.N.; Heinze, H.; et al. Quality of life in patients with short bowel syndrome treated with the new glucagon-like peptide-2 analogue teduglutide--analyses from a randomised, placebo-controlled study. Clin. Nutr. 2013, 32, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Mu, F.; Xie, J.; Kelkar, S.S.; Olivier, C.; Signorovitch, J.; Jeppesen, P.B. Impact of Teduglutide on Quality of Life Among Patients With Short Bowel Syndrome and Intestinal Failure. JPEN J. Parenter. Enter. Nutr. 2020, 44, 119–128. [Google Scholar] [CrossRef]
- Mazzuoli, S.; Regano, N.; Lamacchia, S.; Silvestri, A.; Guglielmi, F.W. Forty-eight months outcomes of teduglutide treatment in adult stable patients with short bowel syndrome and home parenteral nutrition dependence: A real-world Italian single-center observational cohort study. Nutrition 2025, 131, 112640. [Google Scholar] [CrossRef] [PubMed]
- Jurewitsch, B.; Peters, C.; Okamoto, C. Quality of life and lived experience of patients with short bowel syndrome treated with teduglutide and weaning off home parenteral nutrition: A qualitative analysis of patient diaries. BMJ Open Gastroenterol. 2025, 12, e001818. [Google Scholar] [CrossRef]
- Burden, S.T.; Jones, D.J.; Gittins, M.; Ablett, J.; Taylor, M.; Mountford, C.; Tyrrell-Price, J.; Donnellan, C.; Leslie, F.; Bowling, T.; et al. Needs-based quality of life in adults dependent on home parenteral nutrition. Clin. Nutr. 2019, 38, 1433–1438. [Google Scholar] [CrossRef]
- Stanner, H.; Zelig, R.; Rigassio Radler, D. Impact of infusion frequency on quality of life in patients receiving home parenteral nutrition. JPEN J. Parenter. Enter. Nutr. 2022, 46, 757–770. [Google Scholar] [CrossRef]
- Ramos-Goñi, J.M.; Oppe, M.; Stolk, E.; Shah, K.; Kreimeier, S.; Rivero-Arias, O.; Devlin, N. International Valuation Protocol for the EQ-5D-Y-3L. Pharmacoeconomics 2020, 38, 653–663. [Google Scholar] [CrossRef]
- Arnold, D.; Girling, A.; Stevens, A.; Lilford, R. Comparison of direct and indirect methods of estimating health state utilities for resource allocation: Review and empirical analysis. BMJ 2009, 339, b2688. [Google Scholar] [CrossRef]
- Jo, M.W.; Ahn, J.H.; Kim, S.H. The Valuation of EQ-5D-5L Health States in Korea; National Evidence-based Collaborating Agency (NECA): Seoul, Republic of Korea, 2014; pp. 1–120. [Google Scholar]
- Janssen, M.F.; Birnie, E.; Haagsma, J.A.; Bonsel, G.J. Comparing the standard EQ-5D three-level system with a five-level version. Value Health 2008, 11, 275–284. [Google Scholar] [CrossRef]
- Janssen, M.F.; Pickard, A.S.; Golicki, D.; Gudex, C.; Niewada, M.; Scalone, L.; Swinburn, P.; Busschbach, J. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: A multi-country study. Qual. Life Res. 2013, 22, 1717–1727. [Google Scholar] [CrossRef] [PubMed]
- Brazier, J.; Rowen, D. NICE Decision Support Unit Technical Support Documents. In NICE DSU Technical Support Document 11: Alternatives to EQ-5D for Generating Health State Utility Values; National Institute for Health and Care Excellence (NICE): London, UK, 2011. [Google Scholar]
- Im, K.M.; Chung, J.H. Intestinal Rehabilitation Program for Adult Patients with Intestinal Failure: A 20-Year Analysis of Outcomes in the Single-Center Experience at a Tertiary Hospital. Dig. Dis. Sci. 2024, 69, 1770–1777. [Google Scholar] [CrossRef]
- Kinberg, S.; Verma, T.; Kaura, D.; Mercer, D.F. Optimizing transition from pediatric to adult care in short bowel syndrome and intestinal failure. JPEN J. Parenter. Enter. Nutr. 2023, 47, 718–728. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.J.; Lee, K.J.; Choi, J.S.; Yang, H.R.; Moon, J.S.; Chang, J.Y.; Ko, J.S. Poor Prognostic Factors in Patients with Parenteral Nutrition-Dependent Pediatric Intestinal Failure. Pediatr. Gastroenterol. Hepatol. Nutr. 2016, 19, 44–53. [Google Scholar] [CrossRef]
- Radetic, M.; Kamel, A.; Lahey, M.; Brown, M.; Sharma, A. Management of Short Bowel Syndrome (SBS) and Intestinal Failure. Dig. Dis. Sci. 2023, 68, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Vara-Luiz, F.; Glória, L.; Mendes, I.; Carlos, S.; Guerra, P.; Nunes, G.; Oliveira, C.S.; Ferreira, A.; Santos, A.P.; Fonseca, J. Chronic Intestinal Failure and Short Bowel Syndrome in Adults: The State of the Art. GE Port. J. Gastroenterol. 2024, 31, 388–400. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; An, D.; Lee, D.; Woo, H. An Overview and Future Challenges of the WHO International Classification of Disease ICD-11. J. Health Info Stat. 2022, 47, 241–249. [Google Scholar] [CrossRef]
| Characteristics | Adult Vignettes (n = 179) | Pediatric Vignettes (n = 180) |
|---|---|---|
| Age (years), n (%) | ||
| 19–29 | 47 (26.3%) | 48 (26.7%) |
| 30–39 | 44 (24.6%) | 44 (24.4%) |
| 40–49 | 47 (26.3%) | 49 (27.2%) |
| 50–59 | 41 (22.9%) | 39 (21.7%) |
| Sex, n (%) | ||
| Male | 74 (41.3%) | 75 (41.7%) |
| Female | 105 (58.7%) | 105 (58.3%) |
| Education, n (%) | ||
| High school graduate or lower | 11 (6.1%) | 6 (3.3%) |
| University attendance or higher | 168 (93.9%) | 174 (96.7%) |
| Monthly household income (KRW), n (%) | ||
| ≤5 million | 56 (31.3%) | 57 (31.7%) |
| >5 million | 123 (68.7%) | 123 (68.3%) |
| Employment status, n (%) | ||
| Employed | 118 (65.9%) | 138 (76.7%) |
| Student/homemaker | 59 (33.0%) | 39 (21.7%) |
| Unemployed | 2 (1.1%) | 3 (1.7%) |
| Health insurance, n (%) | ||
| NHI district subscriber | 51 (28.5%) | 38 (21.1%) |
| NHI employee subscriber | 119 (66.5%) | 134 (74.4%) |
| Medical aid | 6 (3.4%) | 3 (1.7%) |
| Don’t know | 3 (1.7%) | 5 (2.8%) |
| Disease (self or family/acquaintances) *, n (%) | ||
| Short Bowel Syndrome | 0 (0%) | 1 (0.6%) |
| Other intestinal malabsorption disorders | 5 (2.8%) | 2 (1.1%) |
| None | 174 (97.2%) | 177 (98.3%) |
| Current health status, n (%) | ||
| Normal or improved | 164 (91.6%) | 170 (94.4%) |
| Poor or declined | 15 (8.4%) | 10 (5.6%) |
| EQ-5D-5L, mean (SD) | 0.86 ± 0.05 | 0.86 ± 0.05 |
| VAS, mean (SD) | 0.82 ± 0.11 | 0.82 ± 0.13 |
| PN Days | Adult Vignettes | Pediatric Vignettes | ||||
|---|---|---|---|---|---|---|
| EQ-5D-5L | VAS | TTO | EQ-5D-5L | VAS | TTO | |
| 0 days | 0.808 (0.062) | 0.689 (0.130) | 0.874 (0.111) | 0.804 (0.059) | 0.680 (0.146) | 0.883 (0.120) |
| 1 day | 0.742 (0.073) | 0.607 (0.130) | 0.814 (0.127) | 0.724 (0.091) | 0.593 (0.148) | 0.822 (0.127) |
| 2 days | 0.691 (0.098) | 0.543 (0.123) | 0.748 (0.141) | 0.672 (0.108) | 0.525 (0.144) | 0.767 (0.134) |
| 3 days | 0.584 (0.146) | 0.472 (0.121) | 0.663 (0.157) | 0.575 (0.147) | 0.464 (0.143) | 0.686 (0.145) |
| 4 days | 0.464 (0.176) | 0.400 (0.120) | 0.574 (0.175) | 0.421 (0.169) | 0.397 (0.138) | 0.603 (0.155) |
| 5 days | 0.357 (0.161) | 0.336 (0.123) | 0.467 (0.191) | 0.302 (0.137) | 0.330 (0.132) | 0.506 (0.174) |
| 6 days | 0.230 (0.172) | 0.263 (0.121) | 0.369 (0.201) | 0.191 (0.144) | 0.264 (0.128) | 0.406 (0.184) |
| 7 days | 0.117 (0.170) | 0.180 (0.119) | 0.272 (0.209) | 0.070 (0.134) | 0.178 (0.119) | 0.291 (0.190) |
| Variable | Adult Vignettes | Pediatric Vignettes | ||
|---|---|---|---|---|
| Coefficient | p | Coefficient | p | |
| Constant | 0.7911 | <0.0001 | 0.8331 | <0.0001 |
| 0 days on PN (weaned off) | ||||
| 1 day on PN | −0.0665 | <0.0001 | −0.0800 | <0.0001 |
| 2 days on PN | −0.1173 | <0.0001 | −0.1327 | <0.0001 |
| 3 days on PN | −0.2242 | <0.0001 | −0.2287 | <0.0001 |
| 4 days on PN | −0.3442 | <0.0001 | −0.3834 | <0.0001 |
| 5 days on PN | −0.4511 | <0.0001 | −0.5019 | <0.0001 |
| 6 days on PN | −0.5782 | <0.0001 | −0.6128 | <0.0001 |
| 7 days on PN | −0.6908 | <0.0001 | −0.7338 | <0.0001 |
| Age | 0.0004 | 0.4325 | 0.0005 | 0.2256 |
| Sex (Male) | ||||
| Female | −0.0015 | 0.8805 | −0.0004 | 0.9634 |
| Education (High school graduate or lower) | ||||
| University attendance or higher | −0.0016 | 0.9329 | −0.0384 | 0.1096 |
| Monthly household income (≤5 million KRW) | ||||
| >5 million KRW | 0.0113 | 0.2606 | −0.0120 | 0.2230 |
| Employment status (Unemployed/Student/Homemaker) | ||||
| Employed | −0.0046 | 0.6599 | −0.0032 | 0.7630 |
| Health insurance (National Health Insurance) | ||||
| Medical aid | 0.0272 | 0.2867 | −0.0238 | 0.4724 |
| Don’t know | 0.0308 | 0.3966 | −0.0017 | 0.9511 |
| Disease (No) | ||||
| Yes | −0.0260 | 0.3375 | −0.0228 | 0.4890 |
| Difference of Least square means | Differences | p | Differences | p |
| Between PN days | ||||
| 0 days vs. 1 day | 0.0665 | <0.0001 | 0.0800 | <0.0001 |
| 1 day vs. 2 days | 0.0508 | <0.0001 | 0.0527 | <0.0001 |
| 2 days vs. 3 days | 0.1069 | <0.0001 | 0.0960 | <0.0001 |
| 3 days vs. 4 days | 0.1200 | <0.0001 | 0.1547 | <0.0001 |
| 4 days vs. 5 days | 0.1070 | <0.0001 | 0.1185 | <0.0001 |
| 5 days vs. 6 days | 0.1271 | <0.0001 | 0.1109 | <0.0001 |
| 6 days vs. 7 days | 0.1126 | <0.0001 | 0.1210 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sim, H.; Moon, J.S.; Park, Y.S.; Heo, E.; Chun, Y.S.; Choi, S.; Ku, H.; Chung, J.H. Health State Utility Associated with Parenteral Nutrition Requirement in Patients with Short Bowel Syndrome and Intestinal Failure in Korea: A Vignette-Based Approach. Nutrients 2025, 17, 3551. https://doi.org/10.3390/nu17223551
Sim H, Moon JS, Park YS, Heo E, Chun YS, Choi S, Ku H, Chung JH. Health State Utility Associated with Parenteral Nutrition Requirement in Patients with Short Bowel Syndrome and Intestinal Failure in Korea: A Vignette-Based Approach. Nutrients. 2025; 17(22):3551. https://doi.org/10.3390/nu17223551
Chicago/Turabian StyleSim, Hyewon, Jin Soo Moon, Young Suk Park, Eunji Heo, Yoon Soo Chun, Songhwa Choi, Hyemin Ku, and Jae Hee Chung. 2025. "Health State Utility Associated with Parenteral Nutrition Requirement in Patients with Short Bowel Syndrome and Intestinal Failure in Korea: A Vignette-Based Approach" Nutrients 17, no. 22: 3551. https://doi.org/10.3390/nu17223551
APA StyleSim, H., Moon, J. S., Park, Y. S., Heo, E., Chun, Y. S., Choi, S., Ku, H., & Chung, J. H. (2025). Health State Utility Associated with Parenteral Nutrition Requirement in Patients with Short Bowel Syndrome and Intestinal Failure in Korea: A Vignette-Based Approach. Nutrients, 17(22), 3551. https://doi.org/10.3390/nu17223551






