Association Between Exclusive Breastfeeding, Nutritional Status and Eating Behavior, in Chilean Schoolchildren: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Subjects
2.2. Exclusive Breastfeeding
2.3. Anthropometric Measurements
2.4. Eating Behavior Assessment
2.5. Statistical Analysis
2.6. Ethical Considerations
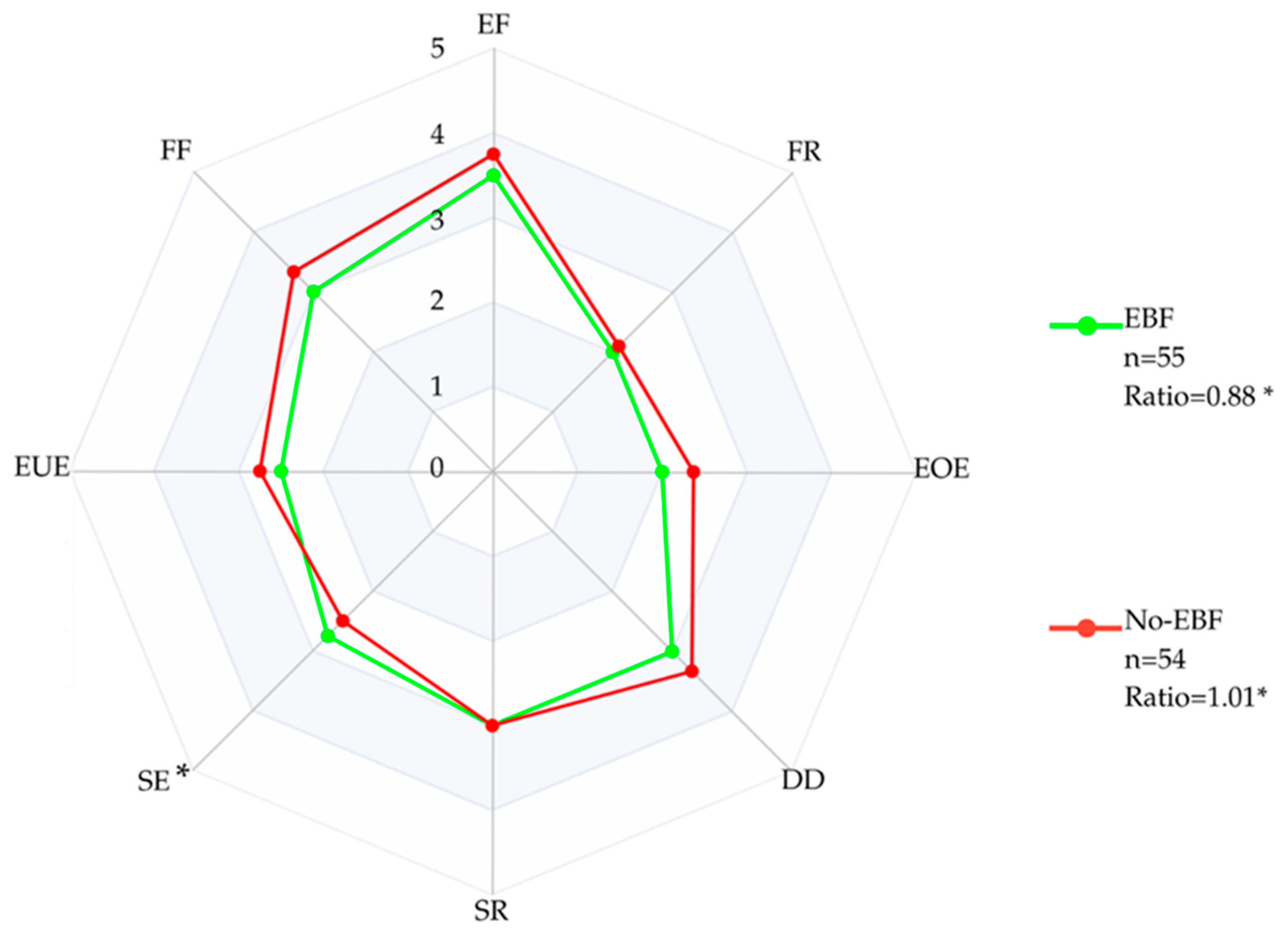
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization (WHO). Breastfeeding. Available online: https://www.who.int/health-topics/breastfeeding (accessed on 11 August 2025).
- Ministerio de Salud de Chile. Manual de Lactancia Materna: Contenidos Técnicos para Profesionales de la Salud, 2nd ed.; Ministerio de Salud: Santiago, Chile, 2010; Available online: https://diprece.minsal.cl/wrdprss_minsal/wp-content/uploads/2015/10/2010_Manual-de-Lactancia-Materna.pdf (accessed on 11 August 2025).
- Rochat, T.J.; Houle, B.; Stein, A.; Coovadia, H.; Coutsoudis, A.; Desmond, C.; Newell, M.-L.; Bland, R.M. Exclusive Breastfeeding and Cognition, Executive Function, and Behavioural Disorders in Primary School-Aged Children in Rural South Africa: A Cohort Analysis. PLoS Med. 2016, 13, e1002044. [Google Scholar] [CrossRef] [PubMed]
- Pang, W.W.; McCrickerd, K.; Quah, P.L.; Fogel, A.; Aris, I.M.; Yuan, W.L.; Fok, D.; Chua, M.C.; Lim, S.B.; Shek, L.P.; et al. Is breastfeeding associated with later child eating behaviours? Appetite 2020, 150, 104653. [Google Scholar] [CrossRef]
- Ergang, B.C.; da Silva, C.H.; Goldani, M.Z.; Hagen, M.E.K.; Bernardi, J.R. Is the duration of breastfeeding associated with eating behavior in early childhood? Physiol. Behav. 2021, 242, 113607. [Google Scholar] [CrossRef]
- Oyarce Merino, K.; Valladares Vega, M.; Elizondo-Vega, R.; Obregón, A.M. Conducta alimentaria en niños. Nutr. Hosp. 2016, 33, 1461–1469. [Google Scholar] [CrossRef] [PubMed]
- De Cosmi, V.; Scaglioni, S.; Agostoni, C. Early Taste Experiences and Later Food Choices. Nutrients 2017, 9, 107. [Google Scholar] [CrossRef] [PubMed]
- Lasserre-Laso, N.; Inostroza-Saelzer, V.; Petermann-Rocha, F.; Martínez-Sanguinetti, M.A.; Leiva-Ordoñez, A.M.; Lanuza, F.; Troncoso-Pantoja, C.; Villagrán, M.; Mardones, L.; Diaz, F.; et al. Lactancia materna y su asociación con obesidad: Mecanismos que podrían explicar el rol protector en la infancia. Rev. Chil. Nutr. 2021, 48, 955–964. [Google Scholar] [CrossRef]
- Mennella, J.A.; Jagnow, C.P.; Beauchamp, G.K. Prenatal and Postnatal Flavor Learning by Human Infants. Pediatrics 2001, 107, e88. [Google Scholar] [CrossRef]
- Mennella, J.A.; Daniels, L.M.; Reiter, A.R. Learning to like vegetables during breastfeeding: A randomized clinical trial of lactating mothers and infants. Am. J. Clin. Nutr. 2017, 106, 67–76. [Google Scholar] [CrossRef]
- Scott, J.; Chih, T.; Oddy, W. Food Variety at 2 Years of Age is Related to Duration of Breastfeeding. Nutrients 2012, 4, 1464–1474. [Google Scholar] [CrossRef]
- de Lauzon-Guillain, B.; Jones, L.; Oliveira, A.; Moschonis, G.; Betoko, A.; Lopes, C.; Moreira, P.; Manios, Y.; Papadopoulos, N.G.; Emmett, P.; et al. The influence of early feeding practices on fruit and vegetable intake among preschool children in 4 European birth cohorts. Am. J. Clin. Nutr. 2013, 98, 804–812. [Google Scholar] [CrossRef]
- Perrine, C.G.; Galuska, D.A.; Thompson, F.E.; Scanlon, K.S. Breastfeeding Duration Is Associated With Child Diet at 6 Years. Pediatrics 2014, 134 (Suppl. 1), S50–S55. [Google Scholar] [CrossRef] [PubMed]
- Möller, L.M.; De Hoog, M.L.A.; Van Eijsden, M.; Gemke, R.J.B.J.; Vrijkotte, T.G.M. Infant nutrition in relation to eating behaviour and fruit and vegetable intake at age 5 years. Br. J. Nutr. 2013, 109, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.L.; Blissett, J. Breastfeeding duration and its relation to weight gain, eating behaviours and positive maternal feeding practices in infancy. Appetite 2017, 108, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Borkhoff, C.M.; Dai, D.W.H.; A Jairam, J.; Wong, P.D.; Cox, K.A.; Maguire, J.L.; Birken, C.S.; Macarthur, C.; Parkin, P.C. Breastfeeding to 12 mo and beyond: Nutrition outcomes at 3 to 5 y of age. Am. J. Clin. Nutr. 2018, 108, 354–362. [Google Scholar] [CrossRef]
- Yelverton, C.A.; Geraghty, A.A.; O’bRien, E.C.; Killeen, S.L.; Horan, M.K.; Donnelly, J.M.; Larkin, E.; Mehegan, J.; McAuliffe, F.M. Breastfeeding and maternal eating behaviours are associated with child eating behaviours: Findings from the ROLO Kids Study. Eur. J. Clin. Nutr. 2021, 75, 670–679. [Google Scholar] [CrossRef]
- Calderón García, A.; Alaminos-Torres, A.; Pedrero Tomé, R.; Prado Martínez, C.; Martínez Álvarez, J.R.; Villarino Marín, A.; Marrodán Serrano, M.D. Eating Behavior and Obesity in a Sample of Spanish Schoolchildren. Int. J. Environ. Res. Public Health 2023, 20, 4186. [Google Scholar] [CrossRef]
- Henríquez Konings, F.P.; Lanuza Rilling, F.I.; Bustos Medina, L.H.; González San Martín, A.; Hazbún Game, J.I. Association between eating behavior and nutritional status in Chilean preschoolers. Nutr. Hosp. 2018, 35, 1049–1053. [Google Scholar] [CrossRef]
- ScienceDirect. Convenience Sampling—An Overview | ScienceDirect Topics. 2018. Available online: https://www.sciencedirect.com/topics/computer-science/convenience-sampling (accessed on 11 August 2025).
- Rito, A.I.; Buoncristiano, M.; Spinelli, A.; Salanave, B.; Kunešová, M.; Hejgaard, T.; García Solano, M.; Fijałkowska, A.; Sturua, L.; Hyska, J.; et al. Association between Characteristics at Birth, Breastfeeding and Obesity in 22 Countries: The WHO European Childhood Obesity Surveillance Initiative—COSI 2015/2017. Obes. Facts 2019, 12, 226–243. [Google Scholar] [CrossRef]
- Ministerio de Salud Chile (MINSAL). Norma Técnica Para la Supervisión de Salud Integral de Niños y Niñas de 0 a 9 Años en Atención Primaria en Salud. Available online: https://www.minsal.cl/ministerio-de-salud-presenta-actualizacion-de-norma-tecnica-para-la-supervision-de-salud-integral-de-ninos-y-ninas-de-0-a-9-anos-en-aps/ (accessed on 11 August 2025).
- Ministerio de Salud Chile (MINSAL). Patrones de Crecimiento Para la Evaluación Nutricional de Niños, Niñas y Adolescentes, Desde el Nacimiento Hasta los 19 Años de Edad. 2018. Available online: http://www.bibliotecaminsal.cl/wp/wp-content/uploads/2018/03/2018.03.16-Patrones-de-crecimiento-para-la-evaluaci%C3%B3n-nutricional-de-ni%C3%B1os-ni%C3%B1as-y-adolescentes-2018.pdf (accessed on 11 August 2025).
- Valle-Leal, J.; Abundis-Castro, L.; Hernández-Escareño, J.; Flores-Rubio, S. Índice cintura-estatura como indicador de riesgo metabólico en niños. Rev. Chil. Pediatr. 2016, 87, 180–185. [Google Scholar] [CrossRef]
- Wardle, J.; Guthrie, C.A.; Sanderson, S.; Rapoport, L. Development of the Children’s Eating Behaviour Questionnaire. J. Child Psychol. Psychiatry 2001, 42, 963–970. [Google Scholar] [CrossRef]
- Santos, M.J.L.; González, A. Adaptación y aplicación del cuestionario de conducta de alimentación infantil CEBQ. In Fundamentos de Nutrición y Dietética. Bases Metodológicas y Aplicaciones, 1st ed.; Martínez, A., Portillo, M., Eds.; Editorial Médica Panamericana: Madrid, Spain, 2011; pp. 339–344. [Google Scholar]
- Santos, J.L.; A Ho-Urriola, J.; González, A.; Smalley, S.V.; Domínguez-Vásquez, P.; Cataldo, R.; Obregón, A.M.; Amador, P.; Weisstaub, G.; Hodgson, M.I. Association between eating behavior scores and obesity in Chilean children. Nutr. J. 2011, 10, 108. [Google Scholar] [CrossRef] [PubMed]
- Sweetman, C.; Wardle, J.; Cooke, L. Soft drinks and «desire to drink» in preschoolers. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 60. [Google Scholar] [CrossRef] [PubMed]
- Mou, J.; Zhou, H.; Huang, S.; Feng, Z. Factorial validation of the children’s eating behavior questionnaire and the association between the eating behaviors assessed and BMI Z score in Chinese preschoolers aged 2–5 years. J. Health Popul. Nutr. 2024, 43, 145. [Google Scholar] [CrossRef] [PubMed]
- Mosli, R.H.; Kutbi, H.A. The association of early feeding practices with eating behaviors and maternal indulgent feeding behaviors among Saudi preschoolers. Front. Psychol. 2023, 14, 1126687. [Google Scholar] [CrossRef]
- Ashcroft, J.; Semmler, C.; Carnell, S.; van Jaarsveld, C.H.M.; Wardle, J. Continuity and stability of eating behaviour traits in children. Eur. J. Clin. Nutr. 2008, 62, 985–990. [Google Scholar] [CrossRef]
- García, A.C.; Pedrero-Tomé, R.; Alaminos-Torres, A.; López-Ejeda, N.; Álvarez, M.S.; Martínez, C.P.; Álvarez, J.R.M.; Serrano, M.D.M. Evaluation of the reliability and internal consistency of the child eating behavior questionnaire (CEBQ) in spanish schoolchildren and its association with obesity. Brain Behav. 2025, 15, e70343. [Google Scholar] [CrossRef]
- Peuckert, M.Z.; Ayala, C.O.; Mattiello, R.; Viola, T.W.; Walker, M.S.; Feoli, A.M.P.; Costa, C.A.D. Validation Evidence for the Children’s Eating Behaviour Questionnaire (CEBQ) in Brazil: A Cross-Sectional Study. Nutrients 2025, 17, 851. [Google Scholar] [CrossRef]
- Santos, F.G.C.D.; Godoy-Leite, M.; Penido, E.A.R.; Ribeiro, K.A.; da Gloria Rodrigues-Machado, M.; Rezende, B.A. Eating behaviour, quality of life and cardiovascular risk in obese and overweight children and adolescents: A cross-sectional study. BMC Pediatr. 2023, 23, 299. [Google Scholar] [CrossRef]
- Freitas, A.; Albuquerque, G.; Silva, C.; Oliveira, A. Appetite-Related Eating Behaviours: An Overview of Assessment Methods, Determinants and Effects on Children’s Weight. Ann. Nutr. Metab. 2018, 73, 19–29. [Google Scholar] [CrossRef]
- Papaioannou, M.A.; Micheli, N.; Power, T.G.; Fisher, J.O.; Hughes, S.O. Associations Between Independent Assessments of Child Appetite Self-Regulation: A Narrative Review. Front. Nutr. 2021, 8, 810912. [Google Scholar] [CrossRef]
- Ochoa Sangrador, C.; Ochoa-Brezmes, J. Waist-to-height ratio as a risk marker for metabolic syndrome in childhood. A meta-analysis. Pediatr. Obes. 2018, 13, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Lichtenauer, M.; Wheatley, S.D.; James, M.M.-S.; Duncan, M.J.; Cobayashi, F.; Berg, G.; Musso, C.; Graffigna, M.; Soutelo, J.; Bovet, P.; et al. Efficacy of anthropometric measures for identifying cardiovascular disease risk in adolescents: Review and meta-analysis. Minerva Pediatr. 2018, 70, 371–382. [Google Scholar] [CrossRef] [PubMed]
- Taxová Braunerová, R.; Kunešová, M.; Heinen, M.M.; Rutter, H.; Hassapidou, M.; Duleva, V.; Pudule, I.; Petrauskienė, A.; Sjöberg, A.; Lissner, L.; et al. Waist circumference and waist-to-height ratio in 7-year-old children-WHO Childhood Obesity Surveillance Initiative. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2021, 22 (Suppl. 6), e13208. [Google Scholar] [CrossRef] [PubMed]
- Ochiai, H.; Shirasawa, T.; Nanri, H.; Nishimura, R.; Matoba, M.; Hoshino, H.; Kokaze, A. Eating quickly is associated with waist-to-height ratio among Japanese adolescents: A cross-sectional survey. Arch. Public Health Arch. Belg. Sante Publique 2016, 74, 18. [Google Scholar] [CrossRef]
- Braet, C.; Van Strien, T. Assessment of emotional, externally induced and restrained eating behaviour in nine to twelve-year-old obese and non-obese children. Behav. Res. Ther. 1997, 35, 863–873. [Google Scholar] [CrossRef]
- Bertacchi, V.; Daiy, K.; Vesi, L.; Faaselele-Savusa, K.; Duckham, R.L.; Naseri, T.; Soti-Ulberg, C.; Abraham, J.; Bribiescas, R.G.; Hawley, N.L. Associations between maternal and infant body composition, feeding practices, and perceived infant eating behaviour in Samoan mother–infant dyads aged 1–4 months. Ann. Hum. Biol. 2025, 52, 2534349. [Google Scholar] [CrossRef]
- Brahm, P.; Valdés, V. Beneficios de la lactancia materna y riesgos de no amamantar. Rev. Chil. Pediatr. 2017, 88, 07–14. [Google Scholar] [CrossRef]
- Bartok, C.J.; Ventura, A.K. Mechanisms underlying the association between breastfeeding and obesity. Int. J. Pediatr. Obes. 2009, 4, 196–204. [Google Scholar] [CrossRef]
- Spahn, J.M.; Callahan, E.H.; Spill, M.K.; Wong, Y.P.; E Benjamin-Neelon, S.; Birch, L.; Black, M.M.; Cook, J.T.; Faith, M.S.; A Mennella, J.; et al. Influence of maternal diet on flavor transfer to amniotic fluid and breast milk and children’s responses: A systematic review. Am. J. Clin. Nutr. 2019, 109, 1003S–1026S. [Google Scholar] [CrossRef]
- de Carvalho, C.A.; Viola, P.C.D.A.F.; da Silva Magalhães, E.I.; Machado, S.P.; Matijasevich, A.; Menezes, A.M.B.; Tovo-Rodrigues, L.; Santos, I.S.; Goncalves, H.; Wehrmeister, F.C.; et al. Association between breast feeding and food consumption according to the degree of processing in Brazil: A cohort study. BMJ Open 2024, 14, e083871. [Google Scholar] [CrossRef]
- Ergang, B.C.; Caprara, G.L.; Machado, M.B.; Moreira, P.R.; Hagen, M.E.K.; Bernardi, J.R. Breastfeeding duration and eating behavior in early childhood: A systematic review. Rev. Bras. Saúde Materno Infant. 2023, 23, e20220074. [Google Scholar] [CrossRef]
- Specht, I.O.; Rohde, J.F.; Olsen, N.J.; Heitmann, B.L. Duration of exclusive breastfeeding may be related to eating behaviour and dietary intake in obesity prone normal weight young children. PLoS ONE 2018, 13, e0200388. [Google Scholar] [CrossRef]
- DiSantis, K.I.; Hodges, E.A.; Johnson, S.L.; Fisher, J.O. The role of responsive feeding in overweight during infancy and toddlerhood: A systematic review. Int. J. Obes. 2011, 35, 480–492. [Google Scholar] [CrossRef]
- Petermann-Rocha, F.; Martínez-Sanguinetti, M.A.; Villagrán, M.; Ulloa, N.; Nazar, G.; Troncoso-Pantoja, C.; Garrido-Méndez, A.; Mardones, L.; Lanuza, F.; Leiva, A.M.; et al. Desde una mirada global al contexto chileno: ¿Qué factores han repercutido en el desarrollo de obesidad en Chile? (Parte 1). Rev. Chil. Nutr. 2020, 47, 299–306. [Google Scholar] [CrossRef]
- Marseglia, L.; Manti, S.; D’aNgelo, G.; Cuppari, C.; Salpietro, V.; Filippelli, M.; Trovato, A.; Gitto, E.; Salpietro, C.; Arrigo, T. Obesity and breastfeeding: The strength of association. Women Birth J. Aust. Coll. Midwives 2015, 28, 81–86. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic Characteristics | ||
|---|---|---|
| n | % | |
| City of residence | ||
| Los Ángeles | 61 | 56.0 |
| Temuco | 18 | 16.5 |
| Iquique | 30 | 27.5 |
| Gender | ||
| Female | 58 | 53.2 |
| Male | 51 | 46.8 |
| Anthropometric Characteristics | ||
| Weight (kg) (X ± SD) | 26.22 | 5.70 |
| Height (cm) (X ± SD) | 119.94 | 6.69 |
| BMI (kg/m2) (X ± SD) | 18.06 | 2.61 |
| Waist circumference (cm) (X ± SD) | 59.87 | 7.74 |
| Waist-to-height ratio (X ± SD) | 0.49 | 0.05 |
| Nutritional Status | ||
| Normal | 45 | 41.7 |
| Overweight | 39 | 36.1 |
| Obese | 24 | 22.2 |
| Waist circumference classification | ||
| Normal | 55 | 50.5 |
| Risk of abdominal obesity | 34 | 31.2 |
| Abdominal obesity | 20 | 18.3 |
| Waist-to-Height Ratio Classification | ||
| Normal | 53 | 48.6 |
| Cardiometabolic risk | 56 | 51.4 |
| Breastfeeding Characteristics | ||
| Duration of breastfeeding (months) (X ± SD) | 17.40 | 12.62 |
| Exclusive Breastfeeding | ||
| EBF | 55 | 50.5 |
| Non-EBP | 54 | 49.5 |
| Age of introduction to infant formula (months) (X ± SD) | 10.60 | 9.94 |
| Age of introduction to complementary feeding (months) (X ± SD) | 5.82 | 0.61 |
| EBF | Non-EBF | |||||||
|---|---|---|---|---|---|---|---|---|
| N n = 24 | OW n = 21 | OB n = 9 | p-Value | N n = 21 | OW n = 18 | OB n = 15 | p-Value | |
| Enjoyment of food | 3.25 [2.87–3.75] | 3.5 [2.75–4.0] | 3.5 [2.75–4.0] | 0.78 | 3.5 [2.75–4.0] a | 3.5 [3.0–4.0] a,b | 4.25 [4.0–4.75] c | 0.00 * |
| Food responsiveness | 1.7 [1.4–2.2] | 2.0 [1.2–2.6] | 2.0 [1.6–3.0] | 0.77 | 1.4 [1.0–2.0] a | 2.1 [1.2–2.6] a,b | 3.2 [2.4–3.4] c | 0.00 * |
| Emotional over-eating | 1.87 [1.25–2.25] | 2.25 [1.5–3.25] | 2.0 [1.5–2.75] | 0.18 | 1.5 [1.0–2.5] a | 2.37 [1.25–3.0] a,b | 3.25 [2.75–3.75] c | 0.00 * |
| Desire to drink | 3.0 [2.0–4.0] | 2.33 [1.66–4.0] | 4.0 [2.0–4.0] | 0.64 | 3.0 [2.0–4.0] | 4.0 [3.0–4.6] | 3.33 [2.0–5.0] | 0.38 |
| Satiety responsiveness | 3.1 [2.9–3.6] a | 2.8 [2.6–3.4] a,b | 2.4 [2.2–2.8] b | 0.00 * | 3.0 [2.6–3.6] | 2.8 [2.4–3.2] | 2.8 [2.2–3.2] | 0.28 |
| Slowness in eating | 3.0 [2.62–4.25] | 2.75 [2.0–3.75] | 2.5 [2.5–3.0] | 0.14 | 3.0 [2.25–4.0] a | 2.5 [2.0–3.5] a,b | 2.5 [1.75–2.5] b | 0.03 * |
| Emotional under-eating | 2.75 [2.0–3.0] | 2.75 [2.0–3.0] | 2.25 [2.0–2.75] | 0.48 | 2.75 [2.0–3.0] | 2.75 [2.25–3.25] | 2.5 [1.5–3.25] | 0.65 |
| Food fussiness | 2.83 [2.66–3.5] | 3.0 [2.5–4.16] | 3.0 [2.33–3.16] | 0.66 | 3.33 [2.83–3.83] | 3.0 [2.6–3.5] | 3.5 [3.16–4.16] | 0.09 |
| Ratio | 0.79 [0.65–0.95] a | 0.9 [0.81–1.06] a,b | 1.0 [0.91–1.13] b | 0.02 * | 0.91 [0.74–1.01] a | 1.02 [0.78–1.18] a,b | 1.24 [1.03–1.47] b | 0.00 * |
| EBF | Non-EBF | |||||||
|---|---|---|---|---|---|---|---|---|
| N n = 29 | RAO n = 18 | AO n = 8 | p-Value | N n = 26 | RAO n = 16 | AO n = 12 | p-Value | |
| Enjoyment of food | 3.25 [3.0–3.5] | 3.75 [3.0–4.0] | 3.25 [2.62–4.25] | 0.526 | 3.37 [2.75–4.0] a | 3.87 [3.37–4.37] a,b | 4.25 [4.0–4.62] b | 0.001 * |
| Food responsiveness | 1.6 [1.4–2.0] | 2.5 [1.2–3.0] | 2.0 [1.4–3.0] | 0.410 | 1.5 [1.0–2.6] a | 2.2 [1.2–3.2] a,b | 3.2 [2.4–3.4] b | 0.008 * |
| Emotional over-eating | 2.0 [1.25–2.25] | 2.75 [1.25–3.25] | 2.12 [1.5–2.75] | 0.174 | 1.62 [1.25–2.5] a | 3.0 [1.25–3.25] a,b | 3.12 [2.5–3.37] b | 0.005 * |
| Desire to drink | 3.0 [2.0–4.0] | 3.3 [2.0–4.6] | 2.0 [1.5–4.16] | 0.507 | 3.5 [2.0–4.66] | 3.83 [3.0–4.33] | 3.0 [2.0–3.3] | 0.387 |
| Satiety responsiveness | 3.0 [2.8–3.6] a | 2.9 [2.6–3.4] a,b | 2.4 [2.2–2.7] b | 0.014 * | 3.0 [2.6–3.4] | 2.8 [2.4–3.2] | 2.9 [2.3–3.2] | 0.577 |
| Slowness in eating | 3.0 [2.75–4.25] | 2.5 [2.0–4.0] | 2.62 [2.25–3.12] | 0.127 | 2.87 [2.25–4.0] a | 2.5 [2.0–3.0] a,b | 2.25 [1.75–2.5] b | 0.020 * |
| Emotional under-eating | 2.75 [2.0–3.0] | 2.6 [2.0–3.2] | 2.25 [2.12–2.62] | 0.487 | 2.75 [2.0–3.0] | 2.62 [2.0–3.12] | 2.75 [2.12–3.25] | 0.891 |
| Food fussiness | 3.0 [2.6–3.6] | 2.9 [2.5–4.1 | 2.75 [2.25–3.25] | 0.435 | 3.08 [2.66–3.66] | 3.33 [3.08–3.66] | 3.41 [3.16–4.0] | 0.373 |
| Ratio | 0.80 [0.70–0.95] | 0.95 [0.84–0.95] | 0.96 [0.78–1.15] | 0.059 | 0.91 [0.74–1.02] a | 1.12 [0.83–1.33] a,b | 1.22 [1.00–1.29] b | 0.011 * |
| EBF | Non-EBF | |||||
|---|---|---|---|---|---|---|
| No-CR n = 27 | CR n = 28 | p-Value | No-CR n = 29 | CR n = 25 | p-Value | |
| Enjoyment of food | 3.25 [2.75–3.75] | 3.63 [2.75–4.0] | 0.253 | 3.5 [2.75–4.0] | 4.0 [3.75–4.25] | 0.020 * |
| Food responsiveness | 1.8 [1.2–2.2] | 2.0 [1.2–2.9] | 0.365 | 1.4 [1.0–2.6] | 2.6 [2.2–3.2] | 0.003 * |
| Emotional over-eating | 2.0 [1.25–2.25] | 2.25 [1.37–3.0] | 0.152 | 1.75 [1.25–2.75] | 3.0 [2.25–3.25] | 0.009 * |
| Desire to drink | 3.0 [2.0–4.0] | 2.33 [1.5–4.3] | 0.330 | 4.0 [2.0–2.4] | 3.33 [2.33–4.33] | 0.800 |
| Satiety responsiveness | 3.0 [2.8–3.6] | 2.8 [2.4–3.2] | 0.013 * | 3.0 [2.6–3.4] | 2.8 [2.6–3.2] | 0.373 |
| Slowness in eating | 3.5 [2.75–4.5] | 2.5 [2.12–3.12] | 0.001 * | 3.0 [2.25–4.0] | 2.5 [2.0–2.5] | 0.013 * |
| Emotional under-eating | 2.5 [2.0–3.0] | 2.62 [2.12–3.0] | 0.609 | 2.75 [2.0–3.0] | 2.75 [2.0–3.25] | 0.800 |
| Food fussiness | 3.16 [2.66–4.0] | 2.75 [2.33–3.25] | 0.074 | 3.16 [2.66–3.66] | 3.33 [3.16–3.66] | 0.316 |
| Ratio | 0.82 [0.60–1.01] | 0.94 [0.78–1.13] | 0.041 * | 0.91 [0.76–1.11] | 1.13 [0.98–1.30] | 0.009 * |
| OB | AO | CR | |||||||
|---|---|---|---|---|---|---|---|---|---|
| EBF | Non-EBF | p-Value | EBF | Non-EBF | p-Value | EBF | Non-EBF | p-Value | |
| Enjoyment of food | 3.5 [2.75–4.0] | 4.25 [4.0–4.75] | 0.011 * | 3.25 [2.62–4.25] | 4.25 [4.0–4.62] | 0.031 * | 3.63 [2.75–4.0] | 4.0 [3.75–4.25] | 0.036 * |
| Food responsiveness | 2.0 [1.6–3.0] | 3.2 [2.4–3.4] | 0.067 | 2.0 [1.4–3.0] | 3.2 [2.4–3.4] | 0.111 | 2.0 [1.2–2.9] | 2.6 [2.2–3.2] | 0.091 |
| Emotional over-eating | 2.0 [1.5–2.75] | 3.25 [2.75–3.75] | 0.008 * | 2.12 [1.5–2.75] | 3.12 [2.5–3.37] | 0.017 * | 2.25 [1.37–3.0] | 3.0 [2.25–3.25] | 0.049 * |
| Desire to drink | 4.0 [2.0–4.0] | 3.33 [2.0–5.0] | 0.880 | 2.0 [1.5–4.16] | 3.0 [2.0–3.3] | 0.433 | 2.33 [1.5–4.3] | 3.33 [2.33–4.33] | 0.130 |
| Satiety responsiveness | 2.4 [2.2–2.8] | 2.8 [2.2–3.2] | 0.367 | 2.4 [2.2–2.7] | 2.9 [2.3–3.2] | 0.295 | 2.8 [2.4–3.2] | 2.8 [2.6–3.2] | 0.886 |
| Slowness in eating | 2.5 [2.5–3.0] | 2.5 [1.75–2.5] | 0.068 | 2.62 [2.25–3.12] | 2.25 [1.75–2.5] | 0.077 | 2.5 [2.12–3.12] | 2.5 [2.0–2.5] | 0.222 |
| Emotional under-eating | 2.25 [2.0–2.75] | 2.5 [1.5–3.25] | 0.810 | 2.25 [2.12–2.62] | 2.75 [2.12–3.25] | 0.243 | 2.62 [2.12–3.0] | 2.75 [2.0–3.25] | 0.726 |
| Food fussiness | 3.0 [2.33–3.16] | 3.5 [3.16–4.16] | 0.009 * | 2.75 [2.25–3.25] | 3.41 [3.16–4.0] | 0.017 * | 2.75 [2.33–3.25] | 3.33 [3.16–3.66] | 0.017 * |
| Ratio | 1.0 [0.91–1.13] | 1.24 [1.03–1.47] | 0.052 | 0.96 [0.78–1.15] | 1.22 [1.00–1.29] | 0.105 | 0.94 [0.78–1.13] | 1.13 [0.98–1.30] | 0.038 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lasserre-Laso, N.; Leiva-Manzor, G.; Bustos-Arriagada, E.; Etchegaray-Armijo, K. Association Between Exclusive Breastfeeding, Nutritional Status and Eating Behavior, in Chilean Schoolchildren: A Cross-Sectional Study. Nutrients 2025, 17, 3444. https://doi.org/10.3390/nu17213444
Lasserre-Laso N, Leiva-Manzor G, Bustos-Arriagada E, Etchegaray-Armijo K. Association Between Exclusive Breastfeeding, Nutritional Status and Eating Behavior, in Chilean Schoolchildren: A Cross-Sectional Study. Nutrients. 2025; 17(21):3444. https://doi.org/10.3390/nu17213444
Chicago/Turabian StyleLasserre-Laso, Nicole, Guillermo Leiva-Manzor, Edson Bustos-Arriagada, and Karina Etchegaray-Armijo. 2025. "Association Between Exclusive Breastfeeding, Nutritional Status and Eating Behavior, in Chilean Schoolchildren: A Cross-Sectional Study" Nutrients 17, no. 21: 3444. https://doi.org/10.3390/nu17213444
APA StyleLasserre-Laso, N., Leiva-Manzor, G., Bustos-Arriagada, E., & Etchegaray-Armijo, K. (2025). Association Between Exclusive Breastfeeding, Nutritional Status and Eating Behavior, in Chilean Schoolchildren: A Cross-Sectional Study. Nutrients, 17(21), 3444. https://doi.org/10.3390/nu17213444






