Clustering of Unhealthy Lifestyle Behaviours and Its Contextual Determinants in Adolescents: A Multilevel Analysis of School-Based Surveys in 45 Countries
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Study Outcome
2.3. Contextual Factors
2.4. Statistical Analysis
2.4.1. Data Preparation and Descriptive Analyses of Clusters of Lifestyle Behaviours
2.4.2. Multilevel Logistic Regression Analyses
3. Results
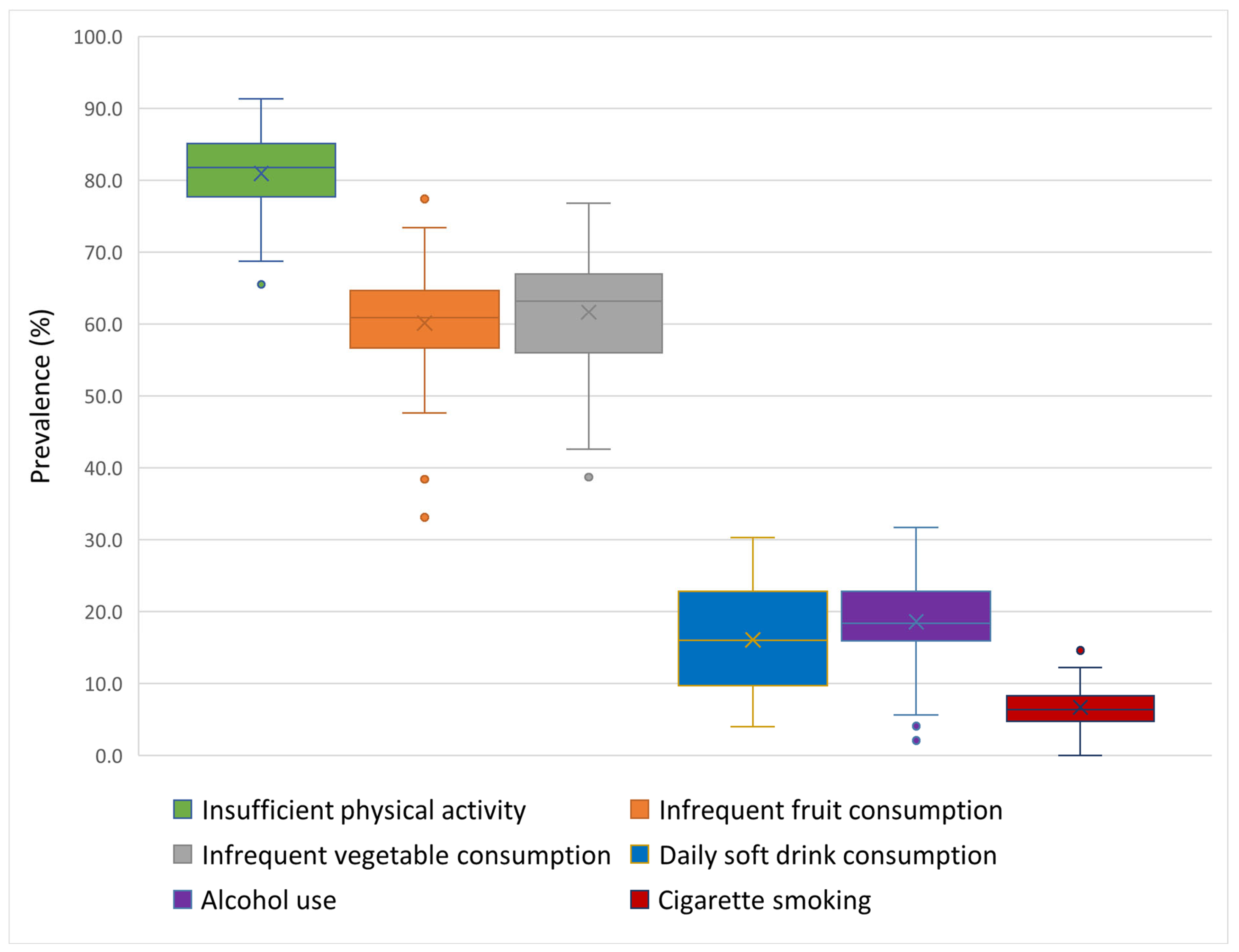
3.1. Prevalence of Individual Unhealthy Lifestyle Behaviours
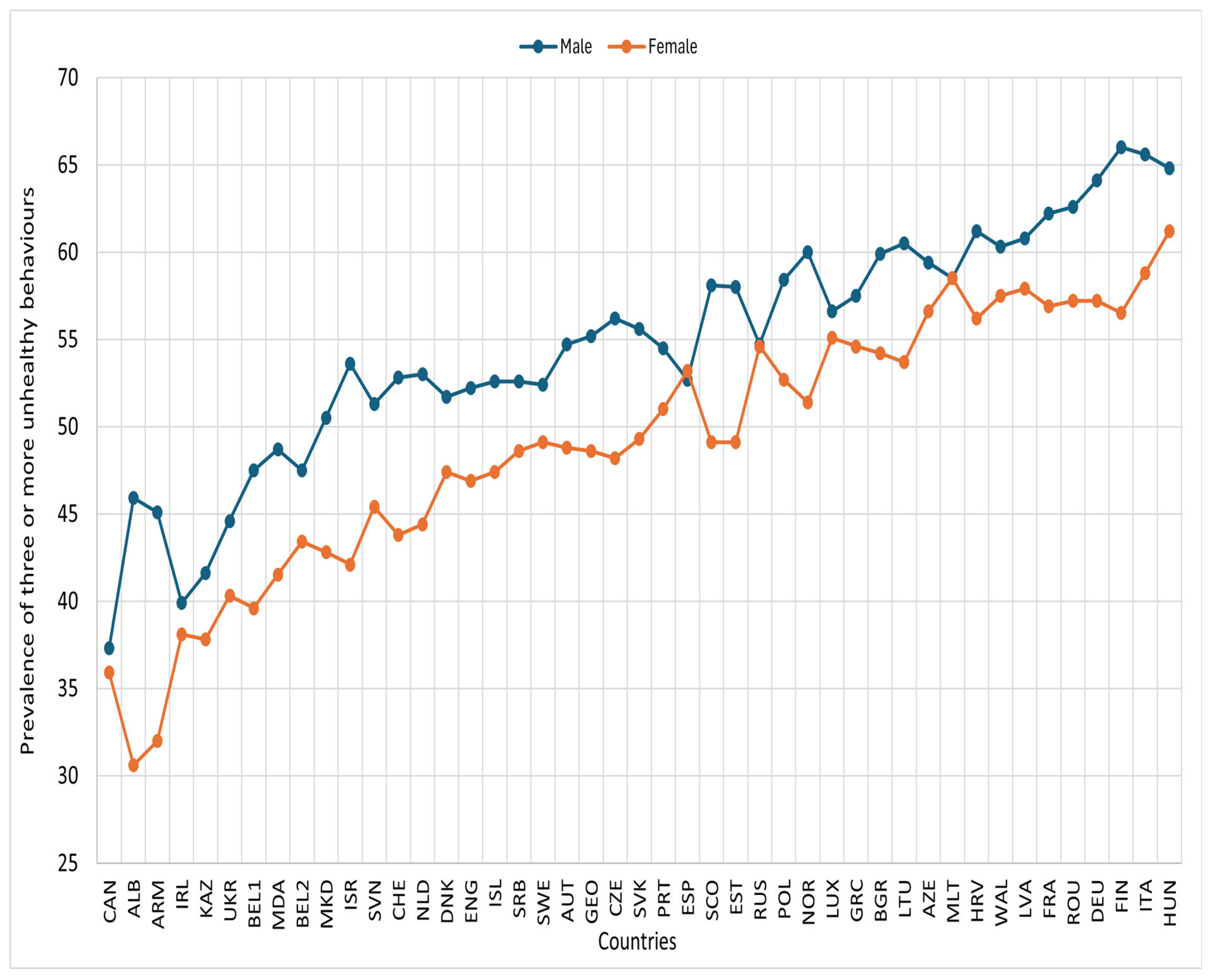
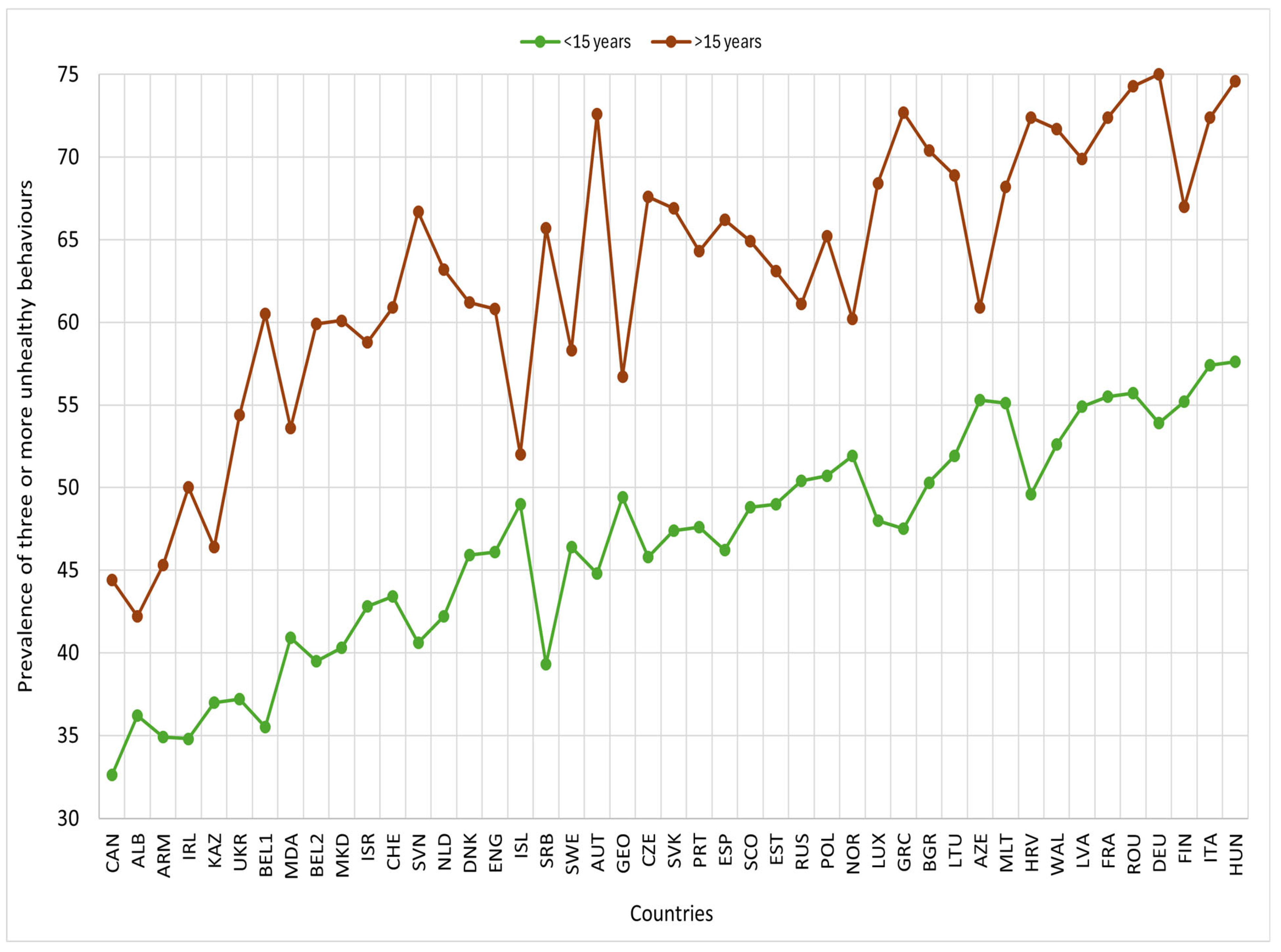
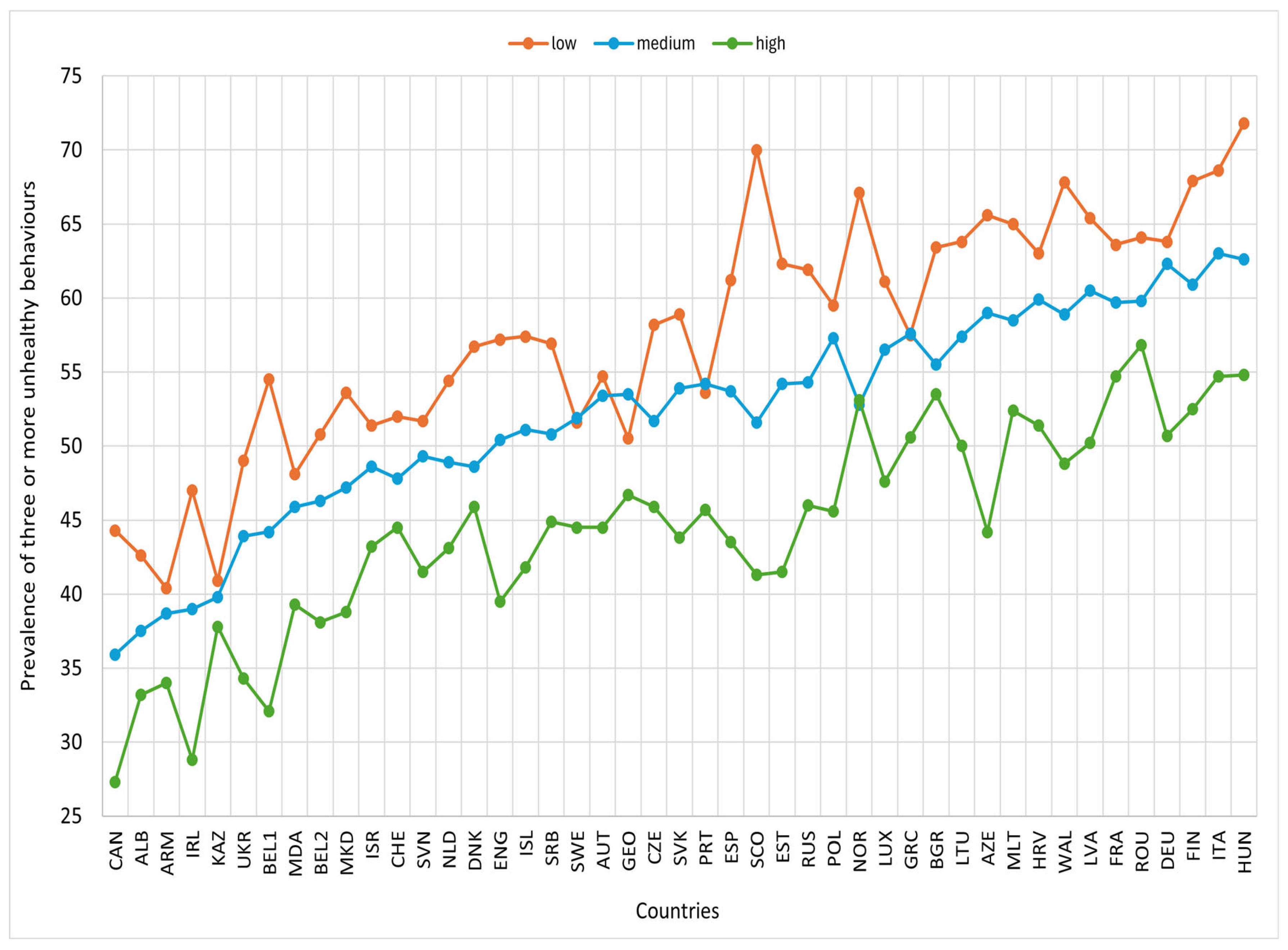
3.2. Clustering of Unhealthy Lifestyle Behaviours
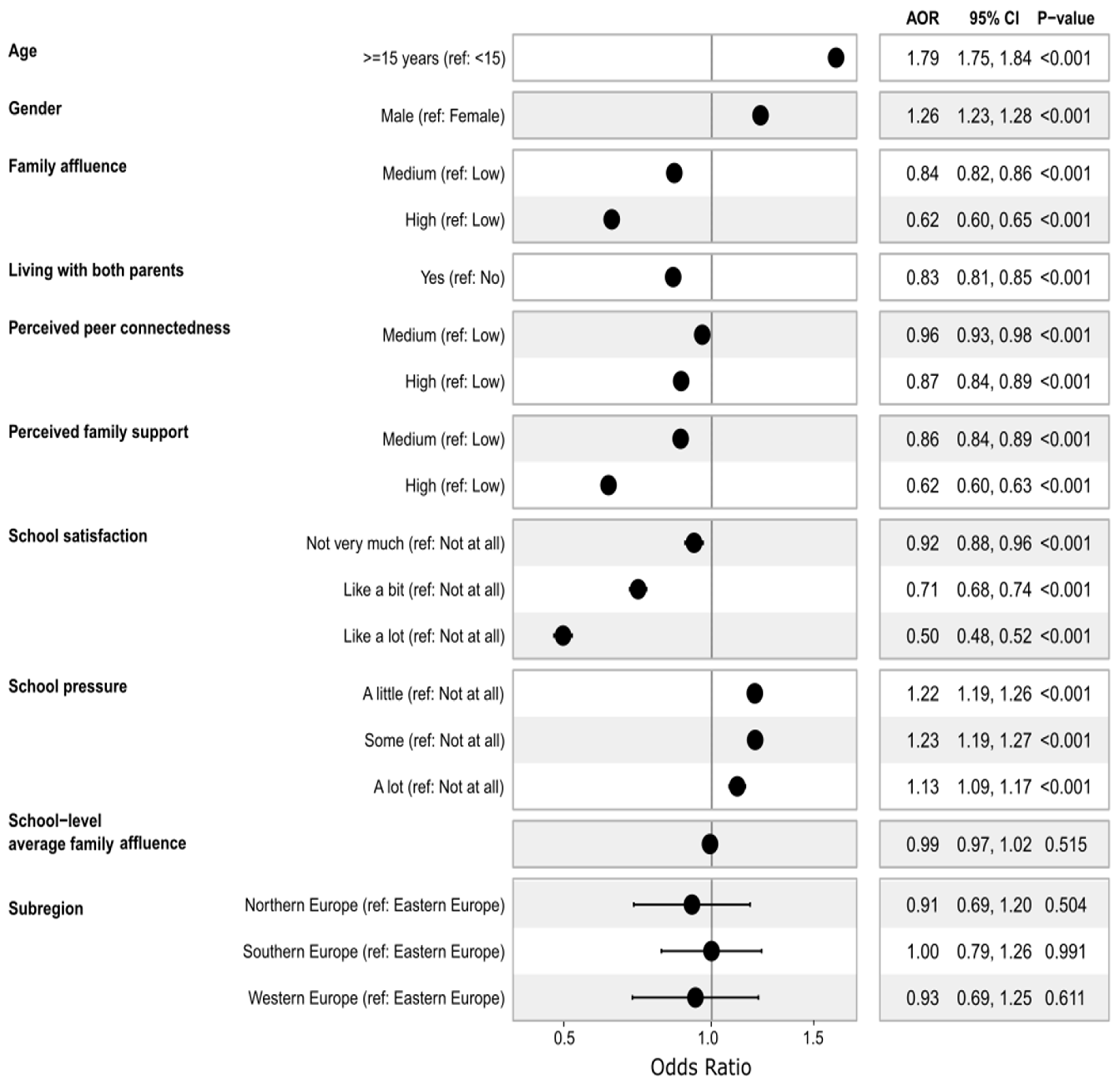
3.3. Association Between Multilevel Contextual Factors and Clustering of Unhealthy Behaviours
3.3.1. Multilevel (Random Effects) Results
3.3.2. Fixed Effects Analysis Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Patton, G.C.; Sawyer, S.M.; Santelli, J.S.; Ross, D.A.; Afifi, R.; Allen, N.B.; Arora, M.; Azzopardi, P.; Baldwin, W.; Bonell, C.; et al. Our future: A commission on adolescent health and wellbeing. Lancet 2016, 387, 2423–2478. [Google Scholar] [CrossRef]
- Sawyer, S.M.; Afifi, R.A.; Bearinger, L.H.; Blakemore, S.J.; Dick, B.; Ezeh, A.C.; Patton, G.C. Adolescence: A foundation for future health. Lancet 2012, 379, 1630–1640. [Google Scholar] [CrossRef]
- Tohi, M.; Bay, J.L.; Tu’akoi, S.; Vickers, M.H. The Developmental Origins of Health and Disease: Adolescence as a Critical Lifecourse Period to Break the Transgenerational Cycle of NCDs-A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 6024. [Google Scholar] [CrossRef]
- Heidari-Beni, M. Early life nutrition and non communicable disease. In Primordial Prevention of Non Communicable Disease; Springer: Berlin/Heidelberg, Germany, 2019; pp. 33–40. [Google Scholar]
- Barker, D.J.P. The developmental origins of adult disease. J. Am. Coll. Nutr. 2004, 23, 588S–595S. [Google Scholar] [CrossRef]
- Biswas, T.; Townsend, N.; Huda, M.M.; Maravilla, J.; Begum, T.; Pervin, S.; Ghosh, A.; Mahumud, R.A.; Islam, S.; Anwar, N.; et al. Prevalence of multiple non-communicable diseases risk factors among adolescents in 140 countries: A population-based study. Eclinicalmedicine 2022, 52, 101591. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Xi, B.; Li, Z.; Wu, H.; Zhao, M.; Liang, Y.; Bovet, P. Prevalence and trends in tobacco use among adolescents aged 13–15 years in 143 countries, 1999–2018: Findings from the Global Youth Tobacco Surveys. Lancet Child Adolesc. Health 2021, 5, 245–255. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Uddin, R.; Lee, E.Y.; Khan, S.R.; Tremblay, M.S.; Khan, A. Clustering of lifestyle risk factors for non-communicable diseases in 304,779 adolescents from 89 countries: A global perspective. Prev. Med. 2020, 131, 105955. [Google Scholar] [CrossRef] [PubMed]
- Efa, Y.T.; Roder, D.; Shi, Z.M.; Li, M. Clustering Patterns of Unhealthy Lifestyle Behaviours Among Adolescents: A Multilevel Analysis of a Nationally Representative School-Based Survey from 73 Countries. Nutrients 2025, 17, 609. [Google Scholar] [CrossRef]
- Efa, Y.T.; Lathief, S.; Roder, D.; Shi, Z.M.; Li, M. Clustering of Lifestyle Habits and Association with Depressive Symptoms and Suicidal Behaviors in Adolescents: A Systematic Review and Meta-Analysis. Adolesc. Res. Rev. 2024, 10, 381–401. [Google Scholar] [CrossRef]
- Kvaavik, E.; Batty, G.D.; Ursin, G.; Huxley, R.; Gale, C.R. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: The United Kingdom health and lifestyle survey. Arch. Intern. Med. 2010, 170, 711–718. [Google Scholar] [CrossRef]
- Li, Y.; Fan, X.; Wei, L.; Yang, K.; Jiao, M. The impact of high-risk lifestyle factors on all-cause mortality in the US non-communicable disease population. BMC Public Health 2023, 23, 422. [Google Scholar] [CrossRef]
- Loewen, O.K.; Maximova, K.; Ekwaru, J.P.; Faught, E.L.; Asbridge, M.; Ohinmaa, A.; Veugelers, P.J. Lifestyle Behavior and Mental Health in Early Adolescence. Pediatrics 2019, 143, e20183307. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Liu, J.; Zhao, Y.; Gong, L.; Chen, Q.; Jiang, X.; Zhang, J.; Hao, Y.; Zhou, H.; Lou, X.; et al. Unhealthy lifestyles and clusters status among 3637 adolescents aged 11–23 years: A school-based cross-sectional study in China. BMC Public Health 2023, 23, 1279. [Google Scholar] [CrossRef] [PubMed]
- Ricardo, C.Z.; Azeredo, C.M.; Machado de Rezende, L.F.; Levy, R.B. Co-occurrence and clustering of the four major non-communicable disease risk factors in Brazilian adolescents: Analysis of a national school-based survey. PLoS ONE 2019, 14, e0219370. [Google Scholar] [CrossRef] [PubMed]
- Mayne, S.L.; Virudachalam, S.; Fiks, A.G. Clustering of unhealthy behaviors in a nationally representative sample of U.S. children and adolescents. Prev. Med. 2020, 130, 105892. [Google Scholar] [CrossRef]
- Lisboa, T.; Silva, W.R.D.; Silva, D.A.S.; Felden, E.P.G.; Pelegrini, A.; Lopes, J.J.D.; Beltrame, T.S. Social support from family and friends for physical activity in adolescence: Analysis with structural equation modeling. Cad. Saude Publica 2021, 37, e00196819. [Google Scholar] [CrossRef]
- Haidar, A.; Ranjit, N.; Archer, N.; Hoelscher, D.M. Parental and peer social support is associated with healthier physical activity behaviors in adolescents: A cross-sectional analysis of Texas School Physical Activity and Nutrition (TX SPAN) data. BMC Public Health 2019, 19, 640. [Google Scholar] [CrossRef]
- Glozah, F.N.; Pevalin, D.J. Perceived social support and parental education as determinants of adolescents’ physical activity and eating behaviour: A cross-sectional survey. Int. J. Adolesc. Med. Health 2015, 27, 253–259. [Google Scholar] [CrossRef]
- Draper, C.E.; Grobler, L.; Micklesfield, L.K.; Norris, S.A. Impact of social norms and social support on diet, physical activity and sedentary behaviour of adolescents: A scoping review. Child Care Health Dev. 2015, 41, 654–667. [Google Scholar] [CrossRef]
- Broyles, S.T.; Denstel, K.D.; Church, T.S.; Chaput, J.P.; Fogelholm, M.; Hu, G.; Kuriyan, R.; Kurpad, A.; Lambert, E.V.; Maher, C.; et al. The epidemiological transition and the global childhood obesity epidemic. Int. J. Obes. Suppl. 2015, 5, S3–S8. [Google Scholar] [CrossRef]
- Chavez-Ugalde, I.Y.; de Vocht, F.; Jago, R.; Adams, J.; Ong, K.K.; Forouhi, N.G.; Colombet, Z.; Ricardo, L.I.C.; van Sluijs, E.; Toumpakari, Z. Ultra-processed food consumption in UK adolescents: Distribution, trends, and sociodemographic correlates using the National Diet and Nutrition Survey 2008/09 to 2018/19. Eur. J. Nutr. 2024, 63, 2709–2723. [Google Scholar] [CrossRef] [PubMed]
- de Vet, E.; de Wit, J.B.; Luszczynska, A.; Stok, F.M.; Gaspar, T.; Pratt, M.; Wardle, J.; de Ridder, D.T. Access to excess: How do adolescents deal with unhealthy foods in their environment? Eur. J. Public Health 2013, 23, 752–756. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Popkin, B.M. The nutrition transition: New trends in the global diet. Nutr. Rev. 1997, 55, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Mason, C. The physical activity transition. J. Phys. Act. Health 2009, 6, 269–280. [Google Scholar] [CrossRef]
- Schunk, D.H.; DiBenedetto, M.K. Learning from a social cognitive theory perspective. In International Encyclopedia of Education, 4th ed.; Tierney, R.J., Rizvi, F., Ercikan, K., Eds.; Elsevier: Oxford, UK, 2023; pp. 22–35. [Google Scholar]
- Inchley, J.; Currie, D.; Cosma, A.; Samdal, O. (Eds.) Health Behaviour in School-Aged Children (HBSC) Study Protocol: Background, Methodology and Mandatory Items for the 2017/18 Survey; CAHRU: St Andrews, UK, 2018. [Google Scholar]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Hu, H.; Song, J.; MacGregor, G.A.; He, F.J. Consumption of Soft Drinks and Overweight and Obesity Among Adolescents in 107 Countries and Regions. JAMA Netw. Open 2023, 6, e2325158. [Google Scholar] [CrossRef]
- Bross, I.D.J. How to use ridit analysis. Biometrics 1958, 14, 18–38. [Google Scholar] [CrossRef]
- Torsheim, T. HBSC Family Affluence Scale Coding Guidance (V1): HBSC Methods Note 1; HBSC data Management Centre, University of Bergen: Bergen, Norway, 2019. [Google Scholar]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Vereecken, C.A.; Inchley, J.; Subramanian, S.V.; Hublet, A.; Maes, L. The relative influence of individual and contextual socio-economic status on consumption of fruit and soft drinks among adolescents in Europe. Eur. J. Public Health 2005, 15, 224–232. [Google Scholar] [CrossRef]
- R Core Team. A Language and Environment for Statistical Computing; Foundation for Statistical Computing: Vienna, Austria, 2024; Available online: https://www.R-project.org/ (accessed on 23 May 2024).
- StataCorp. Stata Statistical Software: Release 18; StataCorp LLC: College Station, TX, USA, 2023. [Google Scholar]
- Cox, N.J.; Morris, T.P. Speaking Stata: The joy of sets: Graphical alternatives to Euler and Venn diagrams. Stata J. 2024, 24, 329–361. [Google Scholar] [CrossRef]
- Merlo, J.; Chaix, B.; Ohlsson, H.; Beckman, A.; Johnell, K.; Hjerpe, P.; Rastam, L.; Larsen, K. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J. Epidemiol. Community Health 2006, 60, 290–297. [Google Scholar] [CrossRef]
- Kim, J.H. Multicollinearity and misleading statistical results. Korean J. Anesthesiol. 2019, 72, 558–569. [Google Scholar] [CrossRef]
- McCoach, D.B.; Newton, S.D.; Gambino, A.J. Multilevel model selection: Balancing model fit and adequacy. In Methodology for Multilevel Modeling in Educational Research: Concepts and Applications; Springer: Berlin/Heidelberg, Germany, 2022; pp. 29–48. [Google Scholar]
- Li, X.; Dessie, Y.; Mwanyika-Sando, M.; Assefa, N.; Millogo, O.; Manu, A.; Chukwu, A.; Bukenya, J.; Patil, R.; Zou, S.Y.; et al. Co-occurrence of and factors associated with health risk behaviors among adolescents: A multi-center study in sub-Saharan Africa, China, and India. Eclinicalmedicine 2024, 70, 102525. [Google Scholar] [CrossRef]
- Velicer, W.F.; Redding, C.A.; Paiva, A.L.; Mauriello, L.M.; Blissmer, B.; Oatley, K.; Meier, K.S.; Babbin, S.F.; McGee, H.; Prochaska, J.O.; et al. Multiple behavior interventions to prevent substance abuse and increase energy balance behaviors in middle school students. Transl. Behav. Med. 2013, 3, 82–93. [Google Scholar] [CrossRef]
- Dabravolskaj, J.; Montemurro, G.; Ekwaru, J.P.; Wu, X.Y.; Storey, K.; Campbell, S.; Veugelers, P.J.; Ohinmaa, A. Effectiveness of school-based health promotion interventions prioritized by stakeholders from health and education sectors: A systematic review and meta-analysis. Prev. Med. Rep. 2020, 19, 101138. [Google Scholar] [CrossRef]
- Champion, K.E.; Parmenter, B.; McGowan, C.; Spring, B.; Wafford, Q.E.; Gardner, L.A.; Thornton, L.; McBride, N.; Barrett, E.L.; Teesson, M.; et al. Effectiveness of school-based eHealth interventions to prevent multiple lifestyle risk behaviours among adolescents: A systematic review and meta-analysis. Lancet Digit. Health 2019, 1, E206–E221. [Google Scholar] [CrossRef]
- O’Dean, S.; Smout, S.; Sunderland, M.; Slade, T.; Gardner, L.A.; Chapman, C.; Thornton, L.; Osman, B.; Hunter, E.; Egan, L.; et al. Adolescent behavioural intentions: Secondary outcomes from a cluster randomized controlled trial of the Health4Life school-based lifestyle modification intervention. Can. J. Public Health 2024, 116, 432–445. [Google Scholar] [CrossRef]
- Alamian, A.; Paradis, G. Clustering of chronic disease behavioral risk factors in Canadian children and adolescents. Prev. Med. 2009, 48, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, A.; Norman, G.J.; Sallis, J.F.; Calfas, K.J.; Cella, J.; Patrick, K. Patterns and correlates of physical activity and nutrition behaviors in adolescents. Am. J. Prev. Med. 2007, 32, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Olson, J.S.; Hummer, R.A.; Harris, K.M. Gender and Health Behavior Clustering among US Young Adults. Biodemography Soc. Biol. 2017, 63, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Matias, T.S.; de Oliveira Araujo, R.H.; Tassitano, R.M.; Ramirez-Velez, R.; Sadarangani, K.P.; Ywgne, J.; Gaia, J.W.P.; de Jesus, G.M.; da Silva, D.R.P. Clustering of obesogenic behaviours amongst 140 052 South American adolescents: A harmonized meta-analysis of national health surveys. J. Public Health 2025, 47, 654–667. [Google Scholar] [CrossRef]
- Murphy, J.J.; MacDonncha, C.; Murphy, M.H.; Murphy, N.; Timperio, A.; Leech, R.M.; Woods, C.B. Identification of health-related behavioural clusters and their association with demographic characteristics in Irish university students. BMC Public Health 2019, 19, 121. [Google Scholar] [CrossRef] [PubMed]
- Silva, K.S.; Barbosa Filho, V.C.; Del Duca, G.F.; de Anselmo Peres, M.A.; Mota, J.; Lopes Ada, S.; Nahas, M.V. Gender differences in the clustering patterns of risk behaviours associated with non-communicable diseases in Brazilian adolescents. Prev. Med. 2014, 65, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Hanson, M.D.; Chen, E. Socioeconomic status and health behaviors in adolescence: A review of the literature. J. Behav. Med. 2007, 30, 263–285. [Google Scholar] [CrossRef] [PubMed]
- Gautam, N.; Dessie, G.; Rahman, M.M.; Khanam, R. Socioeconomic status and health behavior in children and adolescents: A systematic literature review. Front. Public Health 2023, 11, 1228632. [Google Scholar] [CrossRef]
- Seiger, E.; Ouda, R.; Ruto, N.; Dianga, P.; Lytle, L.; Meyer, K.; Ammerman, A.; Voruganti, S.; Nandoya, E.; Omala, H. “We just eat this food because of hunger or because we cannot afford other foods”: Drivers of Adolescent Food Choice from the Perspectives of Adolescents and Influential Adults. Curr. Dev. Nutr. 2022, 6, 603. [Google Scholar] [CrossRef]
- Poonawalla, I.B.; Kendzor, D.E.; Owen, M.T.; Caughy, M.O. Family income trajectory during childhood is associated with adolescent cigarette smoking and alcohol use. Addict. Behav. 2014, 39, 1383–1388. [Google Scholar] [CrossRef]
- Humbert, M.L.; Chad, K.E.; Spink, K.S.; Muhajarine, N.; Anderson, K.D.; Bruner, M.W.; Girolami, T.M.; Odnokon, P.; Gryba, C.R. Factors that influence physical activity participation among high- and low-SES youth. Qual. Health Res. 2006, 16, 467–483. [Google Scholar] [CrossRef]
- Ke, Y.Z.; Shi, L.J.; Peng, L.Q.; Chen, S.T.; Hong, J.T.; Liu, Y. Associations between socioeconomic status and physical activity: A cross-sectional analysis of Chinese children and adolescents. Front. Psychol. 2022, 13, 904506. [Google Scholar] [CrossRef]
- Svendsen, M.T.; Bak, C.K.; Sorensen, K.; Pelikan, J.; Riddersholm, S.J.; Skals, R.K.; Mortensen, R.N.; Maindal, H.T.; Boggild, H.; Nielsen, G.; et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: A large national population-based survey among Danish adults. BMC Public Health 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Todd, J.; Smith, R.; Levin, K.A.; Inchley, J.C.; Currie, D.B.; Currie, C. Family Structure and Relationships and Health Among Schoolchildren; The University of Edinburgh: Edinburgh, UK, 2007. [Google Scholar]
- Chen, M.Y.; Shiao, Y.C.; Gau, Y.M. Comparison of adolescent health-related behavior in different family structures. J. Nurs. Res. 2007, 15, 1–10. [Google Scholar] [CrossRef]
- Theodorakis, Y.; Papaioannou, A.; Karastogianidou, K. Relations between family structure and students’ health-related attitudes and behaviors. Psychol. Rep. 2004, 95, 851–858. [Google Scholar] [CrossRef]
- Yelick, A. The Effects of Family Structure on Consumption and Exercise Patterns for Adolescent Youth. Child Adolesc. Soc. Work J. 2017, 34, 381–395. [Google Scholar] [CrossRef]
- Zaborskis, A.; Kavaliauskiene, A.; Eriksson, C.; Klemera, E.; Dimitrova, E.; Melkumova, M.; Husarova, D. Family Support as Smoking Prevention during Transition from Early to Late Adolescence: A Study in 42 Countries. Int. J. Environ. Res. Public Health 2021, 18, 12739. [Google Scholar] [CrossRef]
- Lawman, H.G.; Wilson, D.K. A review of family and environmental correlates of health behaviors in high-risk youth. Obesity 2012, 20, 1142–1157. [Google Scholar] [CrossRef]
- Beets, M.W.; Vogel, R.; Forlaw, L.; Pitetti, K.H.; Cardinal, B.J. Social support and youth physical activity: The role of provider and type. Am. J. Health Behav. 2006, 30, 278–289. [Google Scholar] [CrossRef] [PubMed]
- Kahn, N.F.; Graham, R. Promoting Positive Adolescent Health Behaviors and Outcomes: Thriving in the 21st Century; The National Academies Press: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Noor, Z.; Khaliq, M.; Khan, A.U.; Ali, M.A.; Tahir, S.K.; Khaliq, K. Academic stress and adolescent health: Exploring eating patterns, dietary preferences, and sleep duration in Pakistan’s youth. Appetite 2025, 209, 107962. [Google Scholar] [CrossRef] [PubMed]
- Han, W.; Altalbe, A.; Rehman, N.; Rehman, S.; Sharma, S. Exploring the longitudinal impacts of academic stress and lifestyle factors among Chinese students. J. Pharm. Policy Pract. 2024, 17, 2398706. [Google Scholar] [CrossRef] [PubMed]
- Thompson, F.E.; Subar, A.F. Dietary assessment methodology. In Nutrition in the Prevention and Treatment of Disease; Elsevier: Amsterdam, The Netherlands, 2017; pp. 5–48. [Google Scholar] [CrossRef]

| Countries | Overall Mean (SD) | Age | Sex | Family Affluence (FAS) | ||||
|---|---|---|---|---|---|---|---|---|
| <15 Years | >=15 Years | Male | Female | Low | Medium | High | ||
| Non-European | ||||||||
| Canada | 1.94 (1.2) | 1.79 | 2.26 *** | 1.95 | 1.94 * | 2.17 | 1.93 *** | 1.66 *** |
| Israel | 2.37 (1.2) | 2.22 | 2.69 *** | 2.50 | 2.24 *** | 2.53 | 2.39 | 2.21 * |
| Kazakhstan | 2.06 (1.1) | 2.00 | 2.21 *** | 2.11 | 2.01 ** | 2.12 | 2.07 | 1.99 ** |
| Eastern Europe | ||||||||
| Armenia | 2.16 (1.1) | 2.04 | 2.41 *** | 2.35 | 1.99 *** | 2.21 | 2.18 | 2.04 ** |
| Azerbaijan | 2.41 (1.0) | 2.36 | 2.46 | 2.48 | 2.34 ** | 2.54 | 2.42 * | 2.20 *** |
| Bulgaria | 2.72 (1.3) | 2.49 | 3.20 *** | 2.76 | 2.69 | 2.94 | 2.68 *** | 2.63 *** |
| Czech Republic | 2.46 (1.3) | 2.22 | 3.02 *** | 2.55 | 2.37 *** | 2.60 | 2.45 *** | 2.32 *** |
| Georgia | 2.51 (1.1) | 2.44 | 2.65 | 2.62 | 2.40 *** | 2.51 | 2.54 | 2.39 |
| Hungary | 2.75 (1.3) | 2.53 | 3.27 *** | 2.80 | 2.72 * | 2.96 | 2.75 ** | 2.56 ** |
| Poland | 2.51 (1.2) | 2.33 | 2.88 *** | 2.58 | 2.45 *** | 2.60 | 2.57 | 2.23 *** |
| Republic of Moldova | 2.26 (1.1) | 2.13 | 2.52 *** | 2.38 | 2.14 *** | 2.31 | 2.28 | 2.13 ** |
| Romania | 2.69 (1.2) | 2.55 | 3.17 *** | 2.77 | 2.60 *** | 2.82 | 2.67 ** | 2.60 ** |
| Russia | 2.39 (1.1) | 2.26 | 2.59 *** | 2.40 | 2.38 | 2.58 | 2.37 *** | 2.18 *** |
| Slovakia | 2.47 (1.3) | 2.29 | 2.97 *** | 2.56 | 2.37 *** | 2.60 | 2.49 | 2.27 *** |
| Ukraine | 2.17 (1.2) | 2.01 | 2.55 *** | 2.23 | 2.12 ** | 2.34 | 2.21 * | 1.94 *** |
| Northern Europe | ||||||||
| Denmark | 2.39 (1.2) | 2.22 | 2.93 *** | 2.44 | 2.34 ** | 2.58 | 2.37 *** | 2.25 *** |
| England | 2.34 (1.2) | 2.21 | 2.75 *** | 2.38 | 2.29 | 2.54 | 2.37 * | 2.04 *** |
| Estonia | 2.41 (1.2) | 2.25 | 2.74 *** | 2.51 | 2.31 *** | 2.61 | 2.43 *** | 2.11 *** |
| Finland | 2.67 (1.2) | 2.44 | 2.92 *** | 2.80 | 2.55 *** | 2.78 | 2.66 * | 2.56 |
| Iceland | 2.18 (1.1) | 2.14 | 2.27 *** | 2.24 | 2.12 ** | 2.35 | 2.22 *** | 1.95 *** |
| Ireland | 2.04 (1.2) | 1.89 | 2.42 *** | 2.06 | 2.02 * | 2.29 | 2.02 *** | 1.77 *** |
| Latvia | 2.63 (1.1) | 2.46 | 3.05 *** | 2.65 | 2.62 | 2.78 | 2.66 * | 2.43 *** |
| Lithuania | 2.55 (1.2) | 2.36 | 2.98 *** | 2.65 | 2.45 *** | 2.71 | 2.56 | 2.37 *** |
| Norway | 2.44 (1.1) | 2.30 | 2.61 | 2.55 | 2.34 ** | 2.69 | 2.39 *** | 2.40 * |
| Scotland | 2.49 (1.2) | 2.31 | 2.95 *** | 2.61 | 2.39 *** | 2.89 | 2.46 *** | 2.17 *** |
| Sweden | 2.39 (1.1) | 2.24 | 2.65 *** | 2.40 | 2.37 | 2.42 | 2.42 | 2.21 ** |
| Wales | 2.64 (1.2) | 2.39 | 3.14 *** | 2.66 | 2.62 | 2.88 | 2.63 *** | 2.37 *** |
| Southern Europe | ||||||||
| Albania | 2.12 (1.2) | 2.06 | 2.38 * | 2.33 | 1.95 *** | 2.22 | 2.13 | 2.02 |
| Croatia | 2.68 (1.3) | 2.36 | 3.17 *** | 2.75 | 2.62 ** | 2.8 | 2.72 | 2.47 ** |
| Greece | 2.62 (1.2) | 2.36 | 3.14 *** | 2.67 | 2.58 * | 2.66 | 2.67 | 2.47 |
| Italy | 2.75 (1.1) | 2.56 | 3.17 *** | 2.83 | 2.69 *** | 2.92 | 2.77 * | 2.57 *** |
| Macedonia | 2.30 (1.3) | 2.08 | 2.78 *** | 2.42 | 2.19 *** | 2.52 | 2.31 ** | 2.10 *** |
| Malta | 2.67 (1.2) | 2.53 | 3.09 *** | 2.67 | 2.67 | 2.83 | 2.67 ** | 2.49 *** |
| Portugal | 2.49 (1.1) | 2.32 | 2.86 *** | 2.52 | 2.46 * | 2.51 | 2.52 | 2.33 *** |
| Serbia | 2.46 (1.4) | 2.06 | 3.01 *** | 2.52 | 2.40 | 2.64 | 2.46 ** | 2.31 *** |
| Slovenia | 2.32 (1.2) | 2.07 | 2.91 *** | 2.40 | 2.24 *** | 2.39 | 2.34 | 2.16 *** |
| Spain | 2.52 (1.2) | 2.30 | 2.95 *** | 2.50 | 2.54 | 2.73 | 2.52 ** | 2.33 *** |
| Western Europe | ||||||||
| Austria | 2.46 (1.2) | 2.23 | 3.17 *** | 2.53 | 2.40 *** | 2.52 | 2.51 | 2.28 ** |
| Belgium (Flemish) | 2.31 (1.2) | 2.07 | 2.83 *** | 2.40 | 2.22 *** | 2.56 | 2.34 ** | 2.01 *** |
| Belgium (French) | 2.36 (1.2) | 2.17 | 2.82 *** | 2.42 | 2.30 * | 2.49 | 2.39 * | 2.17 *** |
| France | 2.68 (1.2) | 2.53 | 3.15 *** | 2.73 | 2.63 *** | 2.73 | 2.69 | 2.58 ** |
| Germany | 2.67 (1.2) | 2.43 | 3.20 *** | 2.76 | 2.6 *** | 2.68 | 2.74 | 2.44 * |
| Luxembourg | 2.57 (1.2) | 2.30 | 2.95 *** | 2.61 | 2.53 ** | 2.70 | 2.59 | 2.36 ** |
| Netherlands | 2.43 (1.2) | 2.23 | 2.87 *** | 2.53 | 2.32 *** | 2.57 | 2.42 * | 2.30 ** |
| Switzerland | 2.38 (1.2) | 2.20 | 2.86 *** | 2.50 | 2.27 *** | 2.46 | 2.38 | 2.26 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Efa, Y.T.; Roder, D.; Shi, Z.; Li, M. Clustering of Unhealthy Lifestyle Behaviours and Its Contextual Determinants in Adolescents: A Multilevel Analysis of School-Based Surveys in 45 Countries. Nutrients 2025, 17, 3388. https://doi.org/10.3390/nu17213388
Efa YT, Roder D, Shi Z, Li M. Clustering of Unhealthy Lifestyle Behaviours and Its Contextual Determinants in Adolescents: A Multilevel Analysis of School-Based Surveys in 45 Countries. Nutrients. 2025; 17(21):3388. https://doi.org/10.3390/nu17213388
Chicago/Turabian StyleEfa, Yohannes Tekalegn, David Roder, Zumin Shi, and Ming Li. 2025. "Clustering of Unhealthy Lifestyle Behaviours and Its Contextual Determinants in Adolescents: A Multilevel Analysis of School-Based Surveys in 45 Countries" Nutrients 17, no. 21: 3388. https://doi.org/10.3390/nu17213388
APA StyleEfa, Y. T., Roder, D., Shi, Z., & Li, M. (2025). Clustering of Unhealthy Lifestyle Behaviours and Its Contextual Determinants in Adolescents: A Multilevel Analysis of School-Based Surveys in 45 Countries. Nutrients, 17(21), 3388. https://doi.org/10.3390/nu17213388








