Magnitudes of Various Forms of Undernutrition Among Children from the Composite Index of Anthropometric Failure in Sub-Saharan Africa: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Searching Strategies and Screening
2.2. Eligibility Criteria and Data Extraction
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Included Study and Quality Appraisal Score

| Author (Year) | Country | Sub-Region | Age Group (M) | Study Design | Sample Size | Year of Data Collection | Sampling Techniques | Prevalence (%) by Undernutrition Categories | JBI Score |
|---|---|---|---|---|---|---|---|---|---|
| Alarape et al. (2022) [21] | Nigeria | West Africa | 0 to 59 | Cross-sectional | 19,471 | 2018 | Stratified-cluster sampling | Wasting only = 1.4 Underweight only = 1.8 WU = 2.4 | 9 |
| Endris N et al. (2017) [29] | Ethiopia | East Africa | 0 to 59 | Cross-sectional | 3095 | 2014 | Stratified-cluster sampling | CIAF = 48.2 Stunting only = 18.2 Wasting only = 3.3 Underweight only = 1.3 SU = 19.4 WU = 2.8 SWU = 3.7 | 9 |
| Amusa et al. (2023) [23] | Nigeria | West Africa | 0 to 59 | Cross-sectional | 10,962 | 2018 | Stratified-cluster sampling | CIAF = 41.3 Stunting only = 36.2 Wasting only = 6.8 Underweight only = 21.7 SU = 14.8 WU = 2.1 SWU = 3 | 9 |
| Odei Obeng-Amoako et al. (2020) [39]. | Uganda | East Africa | 6 to 59 | Cross-sectional | 32,962 | 2015–2018 | Two-stage cluster sampling | SWU = 4.96 | 9 |
| Gonete AT, et al. (2021) [32] | Ethiopia | East Africa | Newborn | Cross-sectional | 394 | 2020 | Simple random sampling | SWU = 2.5 | 6 |
| Bidira K et al. (2021) [27] | Ethiopia | East Africa | 24 to 59 | Cross-sectional | 588 | 2019 | Systematic random sampling | CIAF = 50.8 Stunting only = 22.5 Wasting only = 0.4 Underweight only = 4.9 SU = 11.1 WU = 3.7 SWU = 8.3 | 7 |
| Roba A et al. (2021) [41] | Ethiopia | East Africa | 6 to 59 | Cross-sectional | 993 | 2019 | Simple random sampling | SWU = 5.8 | 9 |
| Addo I et al. (2023) [19] | Benin | West Africa | 0 to 59 | Cross-sectional | 13,589 | 2017–2018 | Two-stage cluster sampling | CIAF = 14.95 | 9 |
| M. Pomati, S. Nandy (2019) [37] | - | West & Central Africa | 0 to 59 | Cross-sectional | 183,000 | 2008–2012 | Two-stage cluster sampling | CIAF = 48 Stunting only = 21 Wasting only = 4 Underweight only = 1 SU = 14 WU = 4 SWU = 4 | 9 |
| B. O. Olusanya et al. (2010) [40] | Nigeria | West Africa | 0 to 3 | Cross-sectional | 5888 | 2005–2006 | Two-stage cluster sampling | CIAF = 38.8 Stunting only = 21.5 Wasting only = 3.3 Underweight only = 1.2 SU = 6.1 WU = 3.4 SWU = 3.3 | 6 |
| Fenta H et al. (2021) [30] | Ethiopia | East Africa | 0 to 59 | Cross-sectional | 29,599 | 2000–2016 | Two-stage cluster sampling | CIAF = 53.78 | 9 |
| Asoba et al. (2019) [25] | Cameroon | West Africa | 0 to 59 | Cross-sectional | 1227 | 2018 | A multistage cluster sampling | CIAF = 32.6 | 9 |
| Berra W (2020) [26] | Ethiopia | East Africa | 6 to 23 | Cross-sectional | 525 | 2016 | Systematic random sampling | CIAF = 21.3 | 5 |
| Ziba and Kalimbiraba et al. (2018) [16] | Malawi | South Africa | 0 to 59 | Cross-sectional | 4586 | 2010 | Stratified-cluster sampling | CIAF = 50.6 Stunting only = 36.2 Wasting only = 1.7 Underweight only = 0.7 SU = 9.6 WU = 1.1 SWU = 1.3 | 9 |
| Sahiledengle B et al. (2023) [42] | Ethiopia | East Africa | 0 to 59 | Cross-sectional | 33,650 | 2000–2016 | Two-stage cluster sampling | SWU = 4.7 | 9 |
| Workie and Tesfaw (2021) [43] | Ethiopia | East Africa | 0 to 59 | Cross-sectional | 9411 | 2016 | Two-stage cluster sampling | Rural CIAF = 48.06 Urban CIAF = 33.26 | 9 |
| Indris A (2021) [20] | Ethiopia | East Africa | 6 to 23 | Cross-sectional | 245 | 2019 | Simple random sampling | Wasting only = 6.12 Underweight only = 4.48 WU = 2.44 | 4 |
| Asmare and Agmas (2022) [24] | Gambia | West Africa | 0 to 59 | Cross-sectional | 2399 | 2019–2020 | Two-stage cluster sampling | CIAF = 24.55 Stunting only = 4.96 Wasting only = 0.92 Underweight only = 6.54 SU = 7.13 WU = 3.58 SWU = 1.42 | 9 |
| Shiferaw and Regassa (2023) [38] | Ethiopia | East Africa | 0 to 59 | Cross-sectional | 48,782 | 2000–2019 | Two-stage cluster sampling | CIAF = 50.71 | 9 |
| Chikhungu L (2022) [28] | Malawi | South Africa | 0 to 59 | Cross-sectional | 5127 | 2015 | Two-stage cluster sampling | CIAF = 38.7 Stunting only = 26.8 Wasting only = 1 Underweight only = 0.4 SU = 8.8 WU = 0.8 SWU = 0.9 | 9 |
| N. Fentahun et al. (2016) [31] | Ethiopia | East Africa | 0 to 59 | Cross-sectional | 674 | 2015 | Stratified-cluster sampling | CIAF = 46.4 Stunting only = 14.5 Wasting only = 1.5 Underweight only = 2.7 SU = 23.2 WU = 2.8 SWU = 1.8 | 8 |
| Khamis et al. (2020) [34] | Tanzania | East Africa | 0 to 59 | Cross-sectional | 6774 | 2010–2011 | Two-stage cluster sampling | CIAF = 38.2 Stunting only = 23.2 Wasting only = 1.6 Underweight only = 0.9 SU = 9.7 WU = 1.3 SWU = 1.5 | 9 |
| 8913 | 2014/15 | CIAF = 45.9 Stunting only = 28.8 Wasting only = 1.3 Underweight only = 0.9 SU = 11.4 WU = 1.7 SWU = 1.8 | |||||||
| Kuwornu et al. (2022) [35] | Ghana | West Africa | 6 to 59 | Cross-sectional | 6532 | 2011 | Two-stage cluster sampling | CIAF = 30 Stunting only = 14.5 Wasting only = 1.5 Underweight only = 1.5 SU = 8.4 WU = 2.4 SWU = 1.6 | 9 |
| 2141 | 2008 | CIAF = 37 Stunting only = 19.5 Wasting only = 3.20 Underweight only = 0.8 SU = 8.5 WU = 3.4 SWU = 1.7 | |||||||
| 1608 | 2009/10 | CIAF = 45 Stunting only = 18.4 Wasting only = 4.2 Underweight only = 0.8 SU = 7.6 WU = 9 SWU = 5.6 | |||||||
| Menalu et al. (2022) [36] | Ethiopia | East Africa | 0 to 59 | Cross-sectional | 355 | 2019–2020 | Systematic random sampling | CIAF = 15.8 | 4 |
| Kassie and Workie (2019) [33] | Ethiopia | East Africa | 0 to 59 | Cross-sectional | 8768 | 2016 | Two-stage cluster sampling | CIAF = 45.96 Stunting only = 16.86 Wasting only = 4.22 Underweight only = 1.43 SU = 15.58 WU = 3.98 SWU = 3.89 | 9 |
| Amadu I, et al. (2021) [22] | - | West Africa | 0 to 59 | Cross-sectional | 127,487 | 2010–2019 | Two-stage cluster sampling | SWU = 3.11 | 9 |
| East Africa | |||||||||
| SWU = 2.43 | |||||||||
| Central Africa | SWU = 2.83 | ||||||||
| SWU = 0.88 | |||||||||
| South Africa |
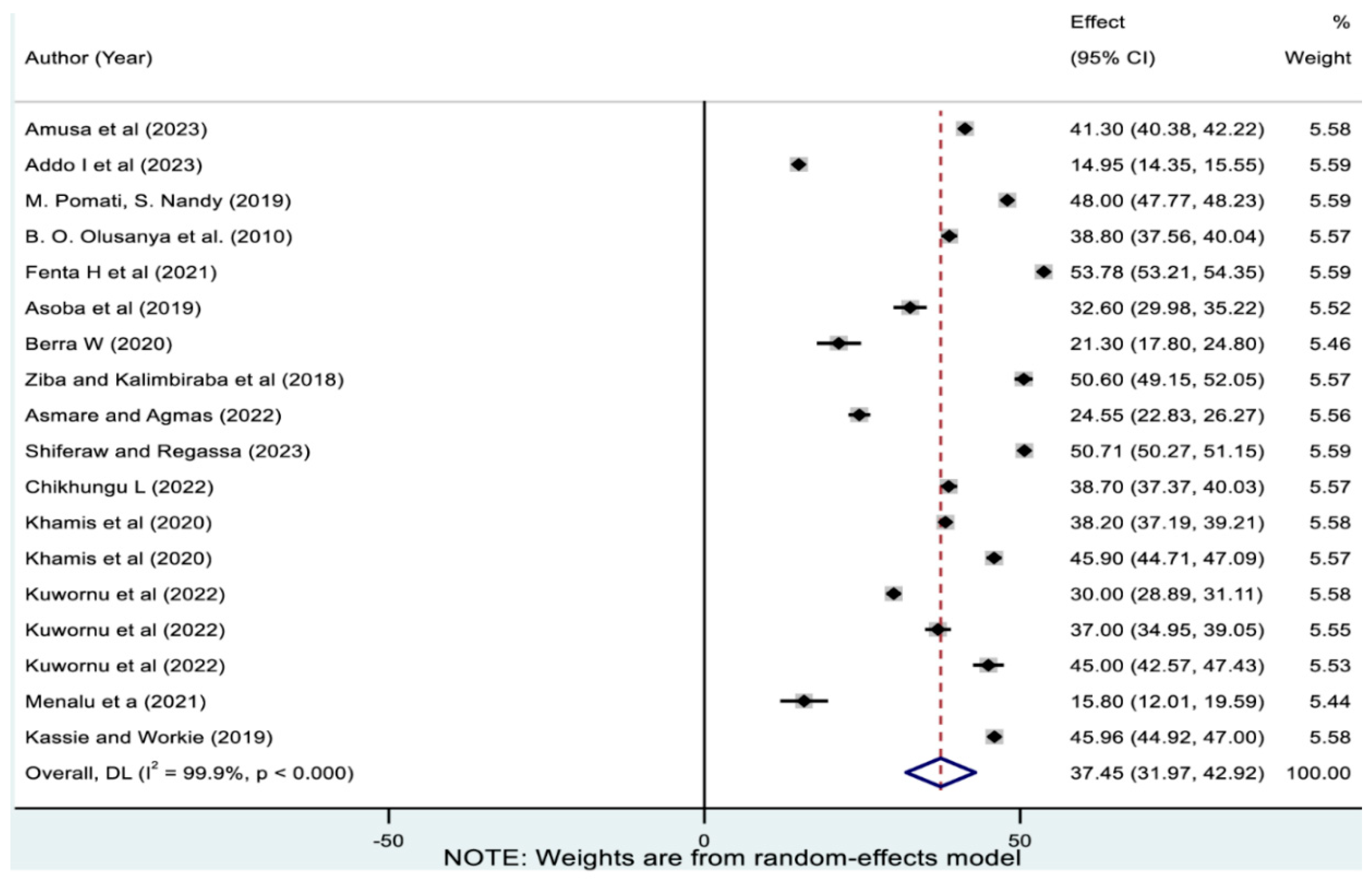
3.2. Pooled Prevalence of Overall Magnitude of Undernutrition
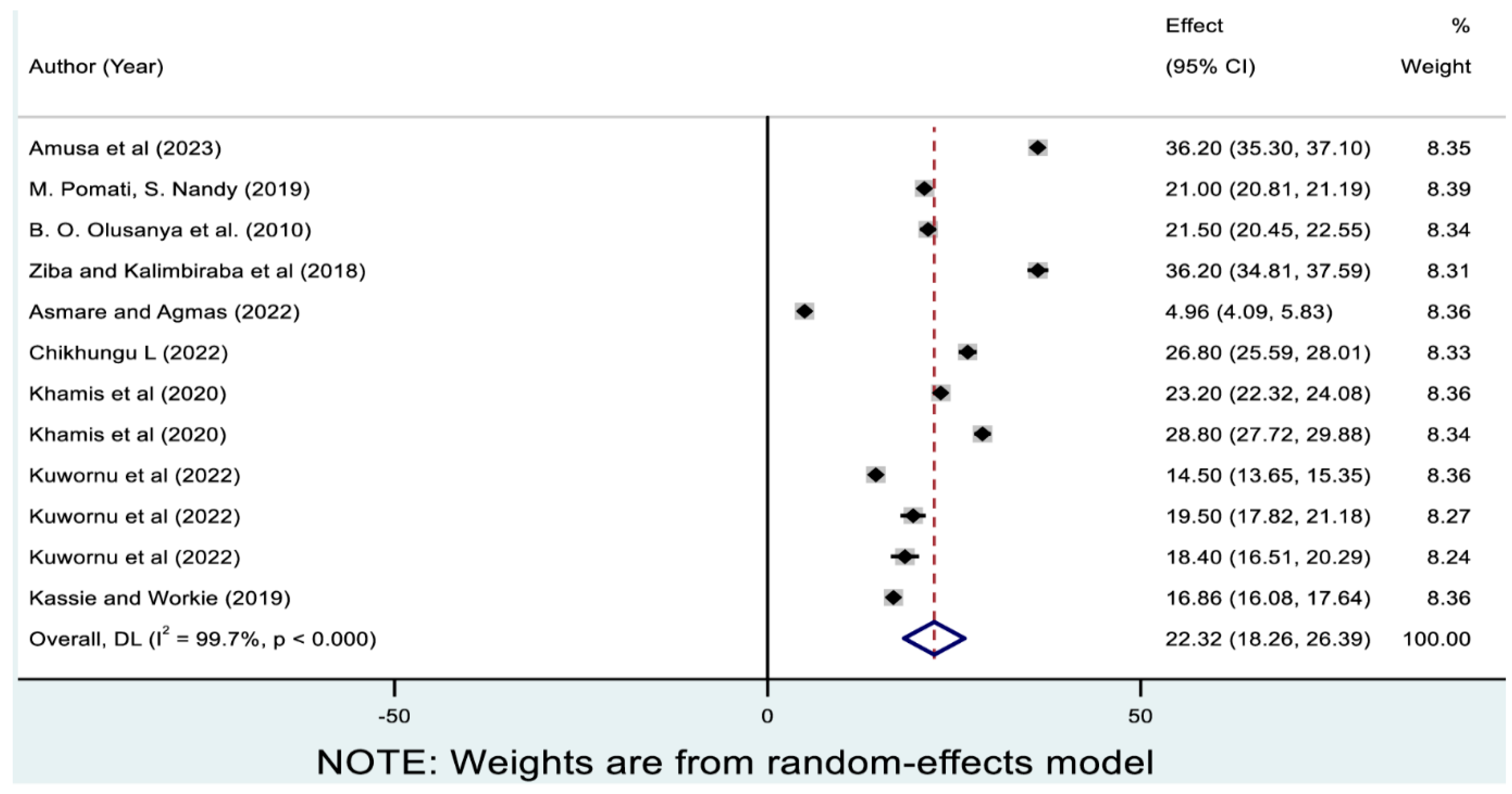
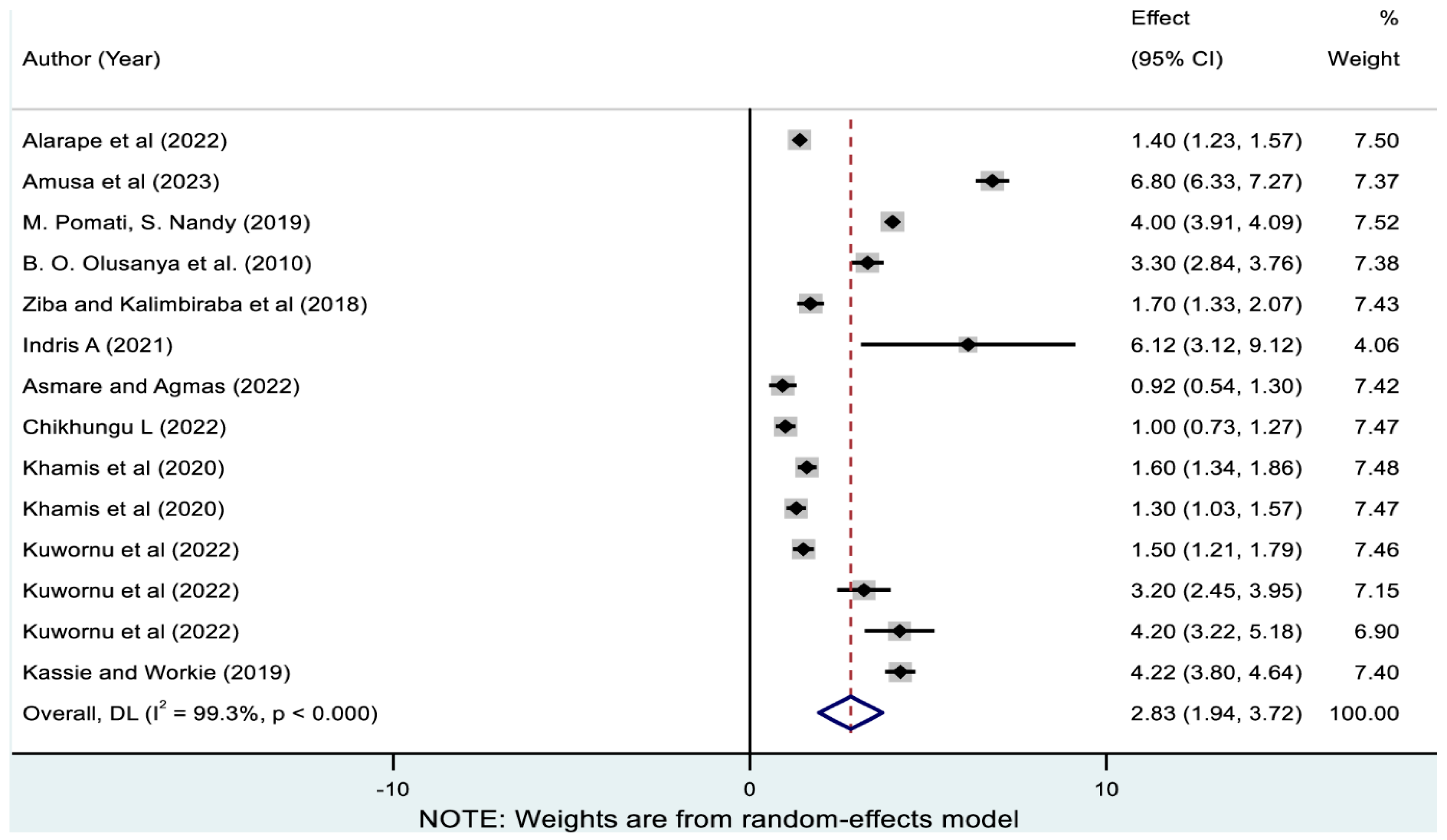
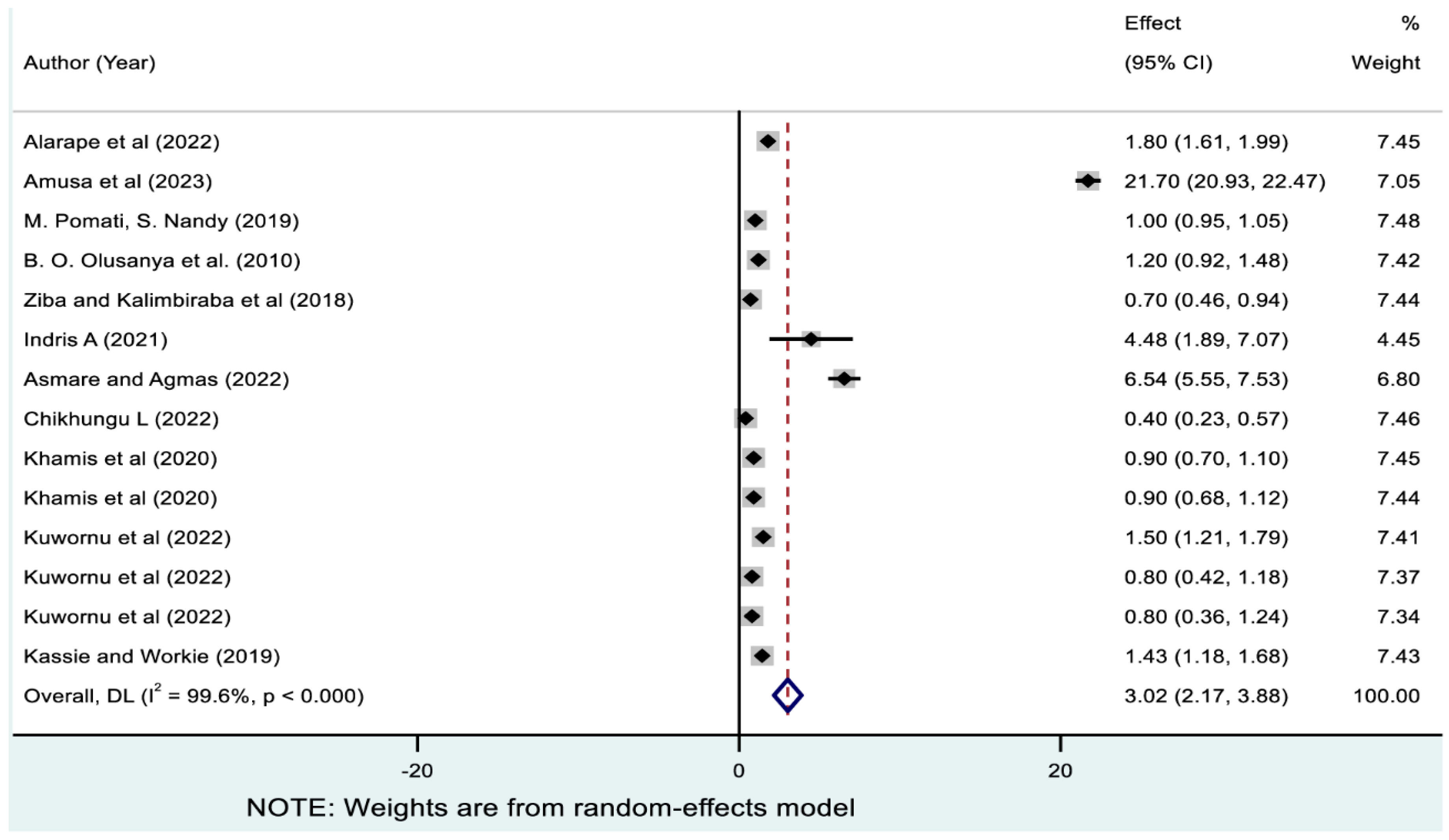
3.3. Pooled Prevalences of Single Forms of Undernutrition
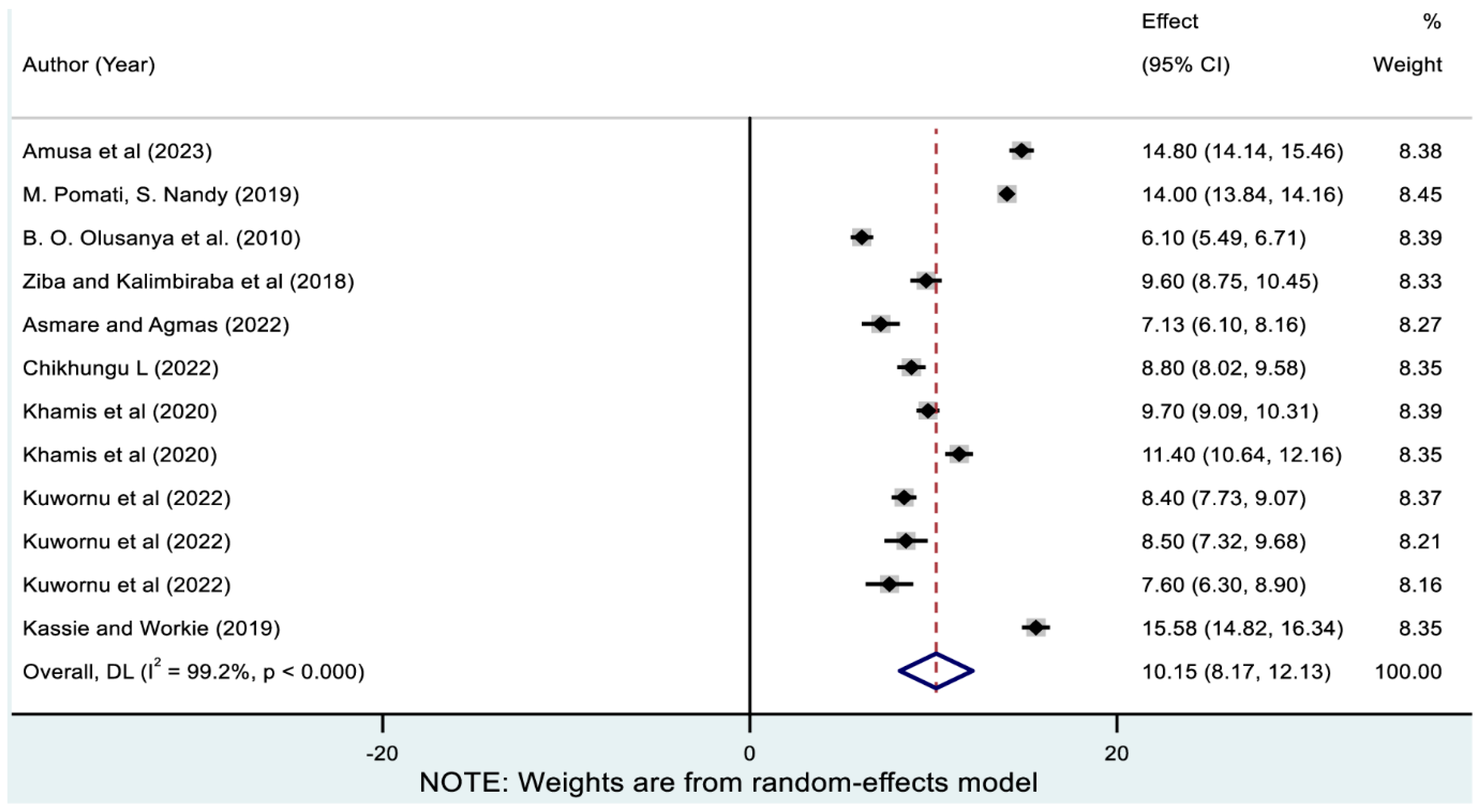
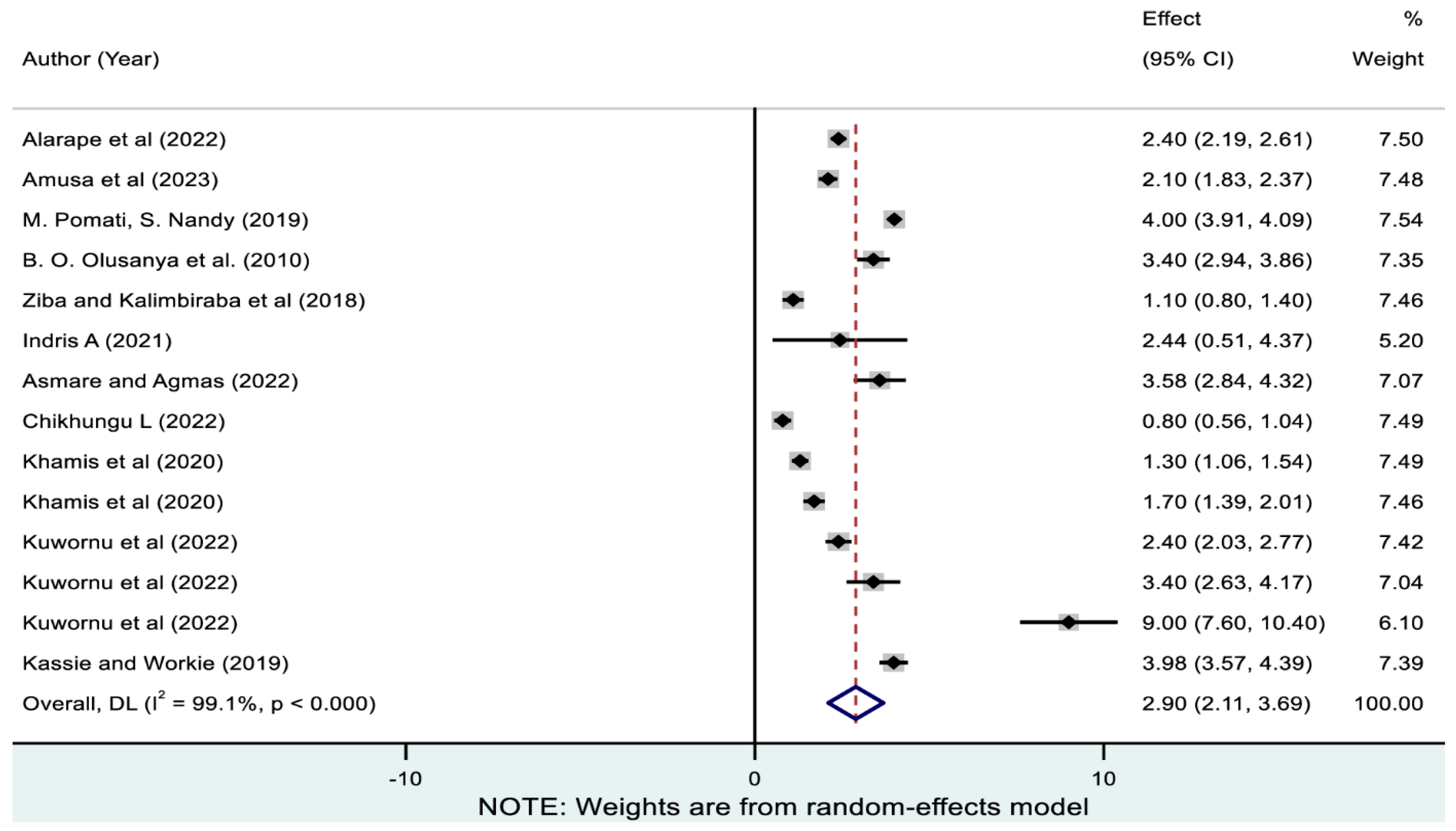
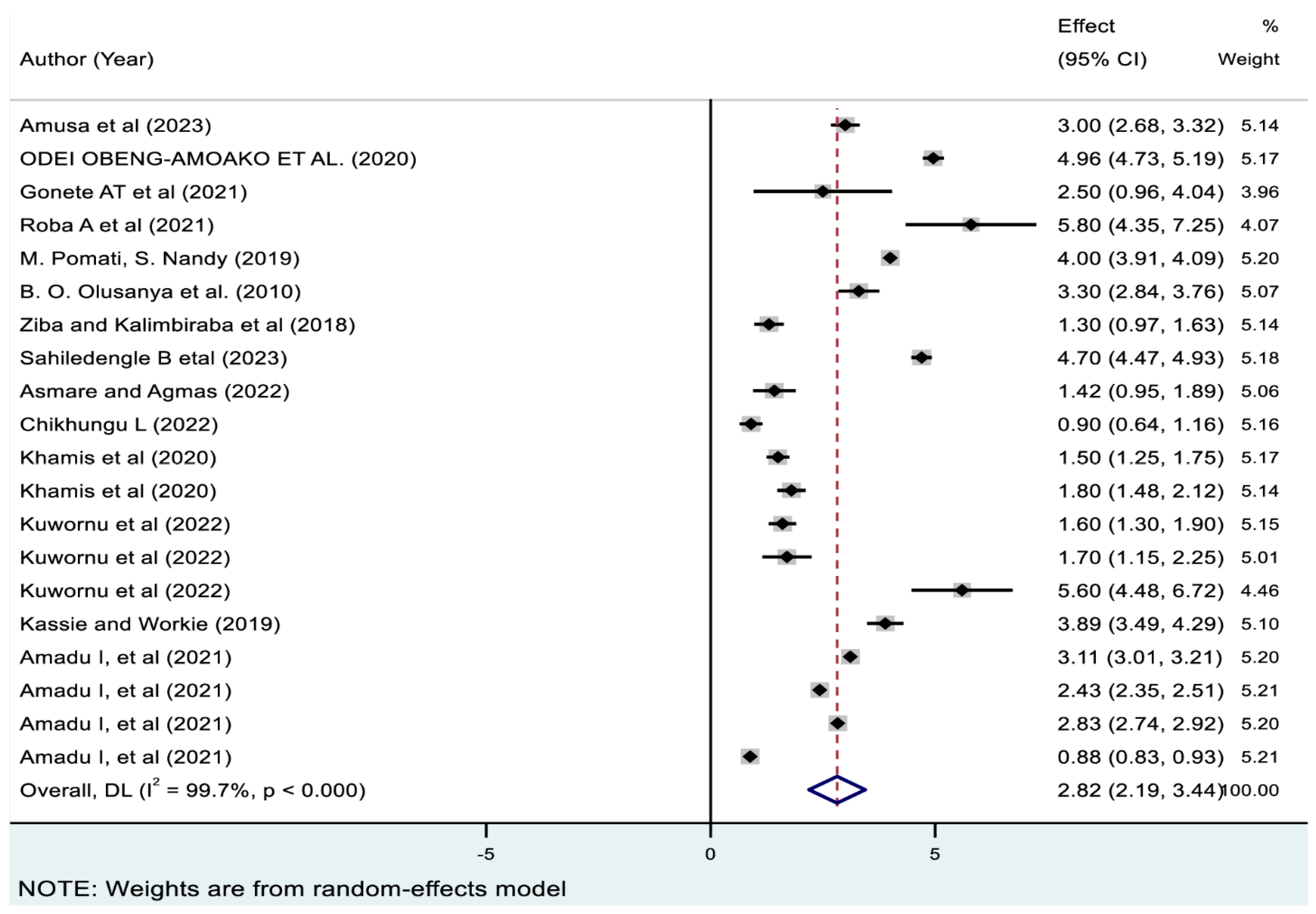
3.4. Pooled Prevalences of Coexisting Forms of Undernutrition
3.5. Meta-Regression Analysis
3.6. Publication Bias and Sensitivity Analysis
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Vassilakou, T. Childhood Malnutrition: Time for Action. Children 2021, 8, 103. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.; Kim, R.; Subramanian, S. Multiple anthropometric failures and early child development in 34 low-and middle-income countries. J. Glob. Health Sci. 2019, 1, e42. [Google Scholar] [CrossRef]
- Svedberg, P. The Composite Index of Anthropometric Failure: Empirical Applications. Ann. Pediatr. Child Health 2024, 12, 1328. [Google Scholar] [CrossRef]
- Agho, K.E.; Akombi, B.J.; Ferdous, A.J.; Mbugua, I.; Kamara, J.K. Childhood undernutrition in three disadvantaged East African Districts: A multinomial analysis. BMC Pediatr. 2019, 19, 118. [Google Scholar] [CrossRef]
- Akombi, B.J.; Agho, K.E.; Hall, J.J.; Merom, D.; Astell-Burt, T.; Renzaho, A.M. Stunting and severe stunting among children under-5 years in Nigeria: A multilevel analysis. BMC Pediatr. 2017, 17, 15. [Google Scholar] [CrossRef]
- Boah, M.; Azupogo, F.; Amporfro, D.A.; Abada, L.A. The epidemiology of undernutrition and its determinants in children under five years in Ghana. PLoS ONE 2019, 14, e0219665. [Google Scholar] [CrossRef]
- Chawla, S.; Gupta, V.; Singh, A.; Grover, K.; Panika, R.K.; Kaushal, P.; Kumar, A. Undernutrition and associated factors among children 1–5 years of age in rural area of Haryana, India: A community based cross-sectional study. J. Fam. Med. Prim. Care 2020, 9, 4240. [Google Scholar]
- Wells, J.C.; Briend, A.; Boyd, E.M.; Berkely, J.A.; Hall, A.; Isanaka, S.; Webb, P.; Khara, T.; Dolan, C. Beyond wasted and stunted—A major shift to fight child undernutrition. Lancet Child Adolesc. Health 2019, 3, 831–834. [Google Scholar] [CrossRef]
- Kundan, I.; Nair, R.; Kulkarni, S.; Deshpande, A.; Jotkar, R.; Phadke, M. Assessment, outcomes and implications of multiple anthropometric deficits in children. BMJ Nutr. Prev. Health 2021, 4, 267. [Google Scholar] [CrossRef]
- Akhade, K.S. Measuring malnutrition: Needs a comprehensive indicator. Int. J. Community Med. Public Health 2017, 5, 258–261. [Google Scholar] [CrossRef][Green Version]
- Sachdev, H. Assessing child malnutrition: Some basic issues. Bull. Nutr. Found. India 1995, 16, 1–5. [Google Scholar]
- Svedberg, P. Poverty and Undernutrition: Theory, Measurement, and Policy; Clarendon Press: Oxford, UK, 2000. [Google Scholar]
- Nandy, S.; Irving, M.; Gordon, D.; Subramanian, S.V.; Smith, G.D. Poverty, child undernutrition and morbidity: New evidence from India. Bull. World Health Organ. 2005, 83, 210–216. [Google Scholar]
- Nandy, S.; Svedberg, P. The Composite Index of Anthropometric Failure (CIAF): An alternative indicator for malnutrition in young children. In Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease; Springer: New York, NY, USA, 2012; pp. 127–137. [Google Scholar]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2015. [Google Scholar]
- Ziba, M.; Kalimbira, A.A.; Kalumikiza, Z. Estimated burden of aggregate anthropometric failure among Malawian children. S. Afr. J. Clin. Nutr. 2018, 31, 20–23. [Google Scholar] [CrossRef]
- Schulzke, S. Assessing and Exploring Heterogeneity. In Principles and Practice of Systematic Reviews and Meta-Analysis; Patole, S., Ed.; Springer International Publishing: Cham, Switzerland, 2021; pp. 33–41. [Google Scholar] [CrossRef]
- Khalil, H.; Bennett, M.; Godfrey, C.; McInerney, P.; Munn, Z.; Peters, M. Evaluation of the JBI scoping reviews methodology by current users. JBI Evid. Implement. 2020, 18, 95–100. [Google Scholar] [CrossRef]
- Addo, I.Y.; Boadu, E.F.; Osei Bonsu, E.; Boadi, C.; Dadzie, F.A. Prevalence and factors associated with undernutrition among children under the age of five years in Benin. PLoS ONE 2023, 18, e0289933. [Google Scholar] [CrossRef]
- Indris, A.; Shaleka, D.; Ashenafi, M. Child nutritional status, mothers’ nutritional knowledge and practice and Household food security status in Tehuledere Woreda, South Wollo, Ethiopia. SIN Ethiop. J. Sci. 2021, 44, 161–171. [Google Scholar] [CrossRef]
- Alarape, K.; Yusuf, O.; Akinyemi, J.; Samuel, F.; Morhason-Bello, I.; Salami, K.; Obisesan, O.; Ilori, T.; Aderinto, A.; Alada, A. Prevalence and patterns of anthropometric failure among under-five children in Nigeria: Evidence from the National nutrition and health survey, 2018. Afr. J. Reprod. Health 2022, 26, 54–61. [Google Scholar] [PubMed]
- Amadu, I.; Seidu, A.-A.; Duku, E.; Frimpong, J.B.; Jnr, J.E.H.; Aboagye, R.G.; Ampah, B.; Adu, C.; Ahinkorah, B.O. Risk factors associated with the coexistence of stunting, underweight, and wasting in children under 5 from 31 sub-Saharan African countries. BMJ Open 2021, 11, e052267. [Google Scholar] [CrossRef]
- Amusa, L.B.; Yahya, W.B.; Bengesai, A.V. Spatial variations and determinants of malnutrition among under-five children in Nigeria: A population-based cross-sectional study. PLoS ONE 2023, 18, e0284270. [Google Scholar] [CrossRef]
- Asmare, A.A.; Agmas, Y.A. Determinants of coexistence of stunting, wasting, and underweight among children under five years in the Gambia; evidence from 2019/20 Gambian demographic health survey: Application of multivariate binary logistic regression model. BMC Public Health 2022, 22, 1621. [Google Scholar] [CrossRef]
- Asoba, G.N.; Sumbele, I.U.N.; Anchang-Kimbi, J.K.; Metuge, S.; Teh, R.N. Influence of infant feeding practices on the occurrence of malnutrition, malaria and anaemia in children≤ 5 years in the Mount Cameroon area: A cross sectional study. PLoS ONE 2019, 14, e0219386. [Google Scholar] [CrossRef] [PubMed]
- Berra, W.G. Household food insecurity predicts childhood undernutrition: A cross-sectional study in West Oromia (Ethiopia). J. Environ. Public Health 2020, 2020, 5871980. [Google Scholar] [CrossRef] [PubMed]
- Bidira, K.; Tamiru, D.; Belachew, T. Anthropometric failures and its associated factors among preschool-aged children in a rural community in southwest Ethiopia. PLoS ONE 2021, 16, e0260368. [Google Scholar] [CrossRef]
- Chikhungu, L.C. Trends and patterns of stunted only and stunted underweight children in Malawi: A confirmation for child nutrition practitioners to continue focusing on stunting. Malawi Med. J. 2022, 34, 111–117. [Google Scholar] [CrossRef]
- Endris, N.; Asefa, H.; Dube, L. Prevalence of malnutrition and associated factors among children in rural Ethiopia. BioMed Res. Int. 2017, 2017, 6587853. [Google Scholar] [CrossRef]
- Fenta, H.M.; Zewotir, T.; Muluneh, E.K. Disparities in childhood composite index of anthropometric failure prevalence and determinants across Ethiopian administrative zones. PLoS ONE 2021, 16, e0256726. [Google Scholar] [CrossRef]
- Fentahun, N.; Belachew, T.; Lachat, C. Determinants and morbidities of multiple anthropometric deficits in southwest rural Ethiopia. Nutrition 2016, 32, 1243–1249. [Google Scholar] [CrossRef] [PubMed]
- Gonete, A.T.; Alemu, T.G.; Mekonnen, E.G.; Takele, W.W. Malnutrition and contributing factors among newborns delivered at the University of Gondar Hospital, Northwest Ethiopia: A cross-sectional study. BMJ Open 2021, 11, e053577. [Google Scholar] [CrossRef]
- Kassie, G.W.; Workie, D.L. Exploring the association of anthropometric indicators for under-five children in Ethiopia. BMC Public Health 2019, 19, 764. [Google Scholar] [CrossRef]
- Khamis, A.G.; Mwanri, A.W.; Kreppel, K.; Kwesigabo, G. The burden and correlates of childhood undernutrition in Tanzania according to composite index of anthropometric failure. BMC Nutr. 2020, 6, 39. [Google Scholar] [CrossRef]
- Kuwornu, J.P.; Amoyaw, J.; Manyanga, T.; Cooper, E.J.; Donkoh, E.; Nkrumah, A. Measuring the overall burden of early childhood malnutrition in Ghana: A comparison of estimates from multiple data sources. Int. J. Health Policy Manag. 2022, 11, 1035–1046. [Google Scholar] [CrossRef] [PubMed]
- Menalu, M.M.; Bayleyegn, A.D.; Tizazu, M.A.; Amare, N.S. Assessment of prevalence and factors associated with malnutrition among under-five children in Debre Berhan town, Ethiopia. Int. J. Gen. Med. 2021, 14, 1683–1697. [Google Scholar] [CrossRef]
- Pomati, M.; Nandy, S. Assessing progress towards SDG2: Trends and patterns of multiple malnutrition in young children under 5 in West and Central Africa. Child Indic. Res. 2020, 13, 1847–1873. [Google Scholar] [CrossRef]
- Shiferaw, N.; Regassa, N. Levels and trends in key socioeconomic inequalities in childhood undernutrition in Ethiopia: Evidence from Ethiopia demographic and health surveys 2000–2019. Discov. Soc. Sci. Health 2023, 3, 5. [Google Scholar] [CrossRef]
- Odei Obeng-Amoako, G.A.; Myatt, M.; Conkle, J.; Muwaga, B.K.; Aryeetey, R.; Okwi, A.L.; Okullo, I.; Mupere, E.; Wamani, H.; Briend, A. Concurrently wasted and stunted children 6–59 months in Karamoja, Uganda: Prevalence and case detection. Matern. Child Nutr. 2020, 16, e13000. [Google Scholar] [CrossRef]
- Olusanya, B.O.; Wirz, S.L.; Renner, J.K. Prevalence, pattern and risk factors for undernutrition in early infancy using the WHO Multicentre Growth Reference: A community-based study. Paediatr. Perinat. Epidemiol. 2010, 24, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Roba, A.A.; Assefa, N.; Dessie, Y.; Tolera, A.; Teji, K.; Elena, H.; Bliznashka, L.; Fawzi, W. Prevalence and determinants of concurrent wasting and stunting and other indicators of malnutrition among children 6–59 months old in Kersa, Ethiopia. Matern. Child Nutr. 2021, 17, e13172. [Google Scholar] [CrossRef]
- Sahiledengle, B.; Agho, K.E.; Petrucka, P.; Kumie, A.; Beressa, G.; Atlaw, D.; Tekalegn, Y.; Zenbaba, D.; Desta, F.; Mwanri, L. Concurrent wasting and stunting among under-five children in the context of Ethiopia: A generalised mixed-effects modelling. Matern. Child Nutr. 2023, 19, e13483. [Google Scholar] [CrossRef]
- Workie, D.L.; Tesfaw, L.M. Bivariate binary analysis on composite index of anthropometric failure of under-five children and household wealth-index. BMC Pediatr. 2021, 21, 332. [Google Scholar] [CrossRef]
- Khaliq, A.; Wraith, D.; Miller, Y.; Nambiar-Mann, S. Prevalence, trends, and socioeconomic determinants of coexisting forms of malnutrition amongst children under five years of age in Pakistan. Nutrients 2021, 13, 4566. [Google Scholar] [CrossRef]
- Elmighrabi, N.F.; Fleming, C.A.; Dhami, M.V.; Elmabsout, A.A.; Agho, K.E. A systematic review and meta-analysis of the prevalence of childhood undernutrition in North Africa. PLoS ONE 2023, 18, e0283685. [Google Scholar] [CrossRef]
- Gupta, G.; Sharma, A.K.; Choudhary, T.S. Assessment of undernutrition among children below 5, using Composite Index of Anthropometric Failure (CIAF). Indian J. Community Health 2017, 29, 108–113. [Google Scholar] [CrossRef]
- Khanra, P.; Biswas, S.; Bose, K. Nutritional Assessment by Composite Index of Anthropometric Failure among School Going Children of Purba Medinipur, West Bengal, India. Hum. Biol. Rev. 2019, 8, 66–76. [Google Scholar]
- Takele, B.A.; Gezie, L.D.; Alamneh, T.S. Pooled prevalence of stunting and associated factors among children aged 6–59 months in Sub-Saharan Africa countries: A Bayesian multilevel approach. PLoS ONE 2022, 17, e0275889. [Google Scholar] [CrossRef]
- Permatasari, T.A.E.; Chadirin, Y. Assessment of undernutrition using the composite index of anthropometric failure (CIAF) and its determinants: A cross-sectional study in the rural area of the Bogor District in Indonesia. BMC Nutr. 2022, 8, 133. [Google Scholar] [CrossRef]
- Sen, J.; Mondal, N. Socio-economic and demographic factors affecting the Composite Index of Anthropometric Failure (CIAF). Ann. Hum. Biol. 2012, 39, 129–136. [Google Scholar] [CrossRef]
- Islam, M.S.; Biswas, T. Prevalence and correlates of the composite index of anthropometric failure among children under 5 years old in Bangladesh. Matern. Child Nutr. 2020, 16, e12930. [Google Scholar] [CrossRef]
- Al-Sadeeq, A.H.; Bukair, A.Z.; Al-Saqladi, A.-W.M. Assessment of undernutrition using Composite Index of Anthropo-metric Failure among children aged< 5 years in rural Yemen. East. Mediterr. Health J. 2018, 24, 1119–1126. [Google Scholar]
- Khara, T. The Relationship Between Wasting and Stunting: Policy, Programming and Research Implications; Field Exchange 50; Emergency Nutrition Network (ENN): Kidlington, UK, 2016; p. 23. [Google Scholar]
- Florêncio, T.M.d.M.T.; Ferreira, H.d.S.; França, A.P.T.d.; Cavalcante, J.C.; Sawaya, A.L. Obesity and undernutrition in a very-low-income population in the city of Maceió, northeastern Brazil. Br. J. Nutr. 2001, 86, 277–283. [Google Scholar] [CrossRef]
- Zhang, Y.-Q.; Li, H.; Wu, H.-H.; Zong, X.-N. Stunting, wasting, overweight and their coexistence among children under 7 years in the context of the social rapidly developing: Findings from a population-based survey in nine cities of China in 2016. PLoS ONE 2021, 16, e0245455. [Google Scholar] [CrossRef]
- Rasheed, W.; Jeyakumar, A. Magnitude and severity of anthropometric failure among children under two years using Composite Index of Anthropometric Failure (CIAF) and WHO standards. Int. J. Pediatr. Adolesc. Med. 2018, 5, 24–27. [Google Scholar] [CrossRef]
- Khaliq, A.; Wraith, D.; Nambiar, S.; Miller, Y. A review of the prevalence, trends, and determinants of coexisting forms of malnutrition in neonates, infants, and children. BMC Public Health 2022, 22, 879. [Google Scholar] [CrossRef]
- Ferreira, H.d.S. Anthropometric assessment of children’s nutritional status: A new approach based on an adaptation of Waterlow’s classification. BMC Pediatr. 2020, 20, 65. [Google Scholar] [CrossRef]
- Fongar, A.; Gödecke, T.; Qaim, M. Various forms of double burden of malnutrition problems exist in rural Kenya. BMC Public Health 2019, 19, 1543. [Google Scholar] [CrossRef]
- Zhang, N.; Becares, L.; Chandola, T. Patterns and determinants of double-burden of malnutrition among rural children: Evidence from China. PLoS ONE 2016, 11, e0158119. [Google Scholar] [CrossRef]
- Rahman, A.; Rahman, M.S. Rural-urban differentials of childhood malnutrition in Bangladesh. Int. J. Child Health Nutr. 2019, 8, 35–42. [Google Scholar] [CrossRef]
- Anik, A.I.; Chowdhury, M.R.K.; Khan, H.T.; Mondal, M.N.I.; Perera, N.K.; Kader, M. Urban-rural differences in the associated factors of severe under-5 child undernutrition based on the composite index of severe anthropometric failure (CISAF) in Bangladesh. BMC Public Health 2021, 21, 2147. [Google Scholar] [CrossRef]
- Adler, N.E.; Ostrove, J.M. Socioeconomic status and health: What we know and what we don’t. Ann. N. Y. Acad. Sci. 1999, 896, 3–15. [Google Scholar] [CrossRef]
- McDonald, C.M.; Olofin, I.; Flaxman, S.; Fawzi, W.W.; Spiegelman, D.; Caulfield, L.E.; Black, R.E.; Ezzati, M.; Danaei, G. The effect of multiple anthropometric deficits on child mortality: Meta-analysis of individual data in 10 prospective studies from developing countries. Am. J. Clin. Nutr. 2013, 97, 896–901. [Google Scholar] [CrossRef]
| CIAF Categories | Wasted | Stunted | Underweight |
|---|---|---|---|
| No failure | No | No | No |
| Stunting only | No | Yes | No |
| Wasting only | Yes | No | No |
| Underweight only | No | No | Yes |
| Stunted and underweight | No | Yes | Yes |
| Wasted and underweight | Yes | No | Yes |
| Wasted, stunted, and underweight | Yes | Yes | Yes |
| Categories | Overall Magnitude of Undernutrition | Single Forms of Undernutrition | Coexisting Forms of Undernutrition | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CIAF | Stunting Only | Wasting Only | Underweight Only | SU | WU | SWU | ||||||||
| N | Prevalence (%) 95%CI | N | Prevalence (%) | N | Prevalence (%) | N | Prevalence (%) | N | Prevalence (%) | N | Prevalence (%) | N | Prevalence (%) | |
| Overall | 18 | 37.45 (31.97–42.92) | 11 | 22.32 (18.26–26.39) | 14 | 2.83 (1.94–3.72) | 14 | 3.02 (2.17–3.88) | 12 | 10.15 (8.17–12.13) | 14 | 2.90 (2.11–3.69) | 20 | 2.82 (2.19–3.44) |
| Country | ||||||||||||||
| Ethiopia | 5 | 38.15 (32.62–43.66) | 1 | 16.86 (16.07–17.64) | 2 | 4.57 (3.13–6.00) | 2 | 2.67 (0.27–5.61) | 1 | 15.58 (14.82–16.34) | 2 | 3.51 (2.12–4.90) | 4 | 4.28 (3.49–5.06) |
| Ghana | 3 | 37.28 (28.67–45.89) | 3 | 17.4 (13.93–20.87) | 3 | 2.92 (1.25–4.59) | 3 | 1.05 (0.55–1.55) | 3 | 8.28 (7.75–8.82) | 3 | 4.84 (2.06–7.62) | 3 | 2.85 (1.27–4.42) |
| Tanzania | 2 | 42.04 (34.49–49.58) | 2 | 25.99 (20.50–31.48) | 2 | 1.45 (1.16–1.75) | 2 | 0.9 (0.75–1.05) | 2 | 10.54 (8.87–12.20) | 2 | 1.49 (1.10–1.88) | 2 | 1.63 (1.34–1.93) |
| Nigeria | 2 | 40.09 (37.64–42.53) | 2 | 28.85 (14.45–43.26) | 3 | 3.83 (0.65–7.00) | 3 | 8.21 (1.79–14.63) | 2 | 10.45 (1.92–18.97) | 3 | 2.6 (2.02–3.17) | 2 | 3.10 (2.82–3.38) |
| Malawi | 2 | 44.65 (32.98–56.31) | 2 | 31.49 (22.28–40.71) | 2 | 1.34 (0.65–2.02) | 2 | 0.54 (0.24–0.83) | 2 | 9.18 (8.40–9.96) | 2 | 0.94 (0.64–1.23) | 2 | 1.09 (0.7–1.48) |
| Gambia | 1 | 24.55 (22.83–26.27) | 1 | 4.96 (4.09–5.82) | 1 | 0.92 (0.53–1.30) | 1 | 6.54 (5.55–7.52) | 1 | 7.13 (6.10–8.16) | 1 | 3.58 (2.83–4.32) | 1 | 1.42 (0.94–1.89) |
| Uganda | - | - | - | - | - | - | - | - | - | - | - | 1 | 4.96 (4.72–5.19) | |
| Benin | 1 | 14.95 (14.35–15.55) | - | - | - | - | - | - | - | - | - | - | - | |
| Cameroon | 1 | 33.6 (29.98, 35.22) | - | - | - | - | - | - | - | - | - | - | - | |
| Overall, DL | I2 = 99.9%, p < 0.000 | I2 = 99.7%, p < 0.000 | I2 = 98.4%, p < 0.000 | I2 = 99.6%, p < 0.000 | I2 = 98.5%, p < 0.000 | I2 = 97.2%, p < 0.000 | I2 = 98.8%, p < 0.000 | |||||||
| Subregion | ||||||||||||||
| West Africa | 8 | 33.01 (23.77–42.26) | 6 | 19.18 (9.31–29.04) | 7 | 3.03 (1.68–4.38) | 7 | 4.88 (2.11–7.65) | 6 | 8.76 (5.76–11.77) | 7 | 3.46 (2.75–4.17) | 7 | 2.72 (2.05–3.38) |
| West-central Africa | 1 | 48 (47.77–48.22) | 1 | 21 (20.81–21.18) | 1 | 4 (3.91–4.09) | 1 | 1 (0.95–1.04) | 1 | 14 (13.84–14.15) | 1 | 4 (3.91–4.09) | 1 | 4.00 (3.91–4.00) |
| South Africa | 2 | 44.65 (32.98–56.31) | 2 | 31.49 (22.28–40.71) | 2 | 1.34 (0.65–2.02) | 2 | 0.54 (0.24–0.83) | 2 | 9.18 (8.40–9.96) | 2 | 0.94 (0.64–1.23) | 3 | 0.98 (0.77–1.19) |
| East Africa | 7 | 39.20 (34.06–44.34) | 3 | 22.95 (16.30–29.59) | 4 | 2.84 (1.43–4.26) | 4 | 1.14 (0.76–1.53) | 3 | 12.22 (8.79–15.65) | 4 | 2.34 (1.06–3.61) | 8 | 3.41 (2.40–4.42) |
| Central Africa | - | - | - | 1 | 2.83 (2.74–2.92) | |||||||||
| Overall, DL | I2 = 99.9%, p < 0.000 | I2 = 99.7%, p < 0.000 | I2 = 99.3%, p < 0.000 | I2 = 99.6%, p < 0.000 | I2 = 99.2%, p < 0.000 | I2 = 99.1%, p < 0.000 | I2 = 99.7%, p < 0.000 | |||||||
| Age group | ||||||||||||||
| 0 to 3 | 1 | 38.8 (37.55–40.04) | 1 | 21.5 (20.45–22.54) | 1 | 3.3 (2.84–3.75) | 1 | 1.2 (0.92–1.47) | 1 | 6.1 (5.48–6.71) | 1 | 3.4 (2.93–3.86) | 1 | 3.3 (2.84–3.75) |
| 6 to 23 | 1 | 21.3 (17.79–24.8) | NA | 1 | 6.12 (3.11, 9.12) | 1 | 4.48 (1.89–7.07) | 1 | 2.44 (0.50–4.37) | - | ||||
| 6 to 59 | 3 | 33.45 (32.55–34.36) | 3 | 15.92 (15.22–16.63) | 3 | 1.9 (1.64–2.17) | 3 | 1.13 (0.93–1.34) | 3 | 8.28 (7.75–8.81) | 3 | 2.94 (2.61–3.26) | 5 | 3.58 (3.41–3.75) |
| 0 to 59 | 13 | 45.24 (45.07–45.41) | 8 | 21.33 (21.16–21.50) | 9 | 2.97 (2.91–3.04) | 9 | 1.06 (1.02–1.10) | 8 | 13.37 (13.23–13.51) | 9 | 3.01 (2.94–3.08) | 13 | 2.15 (2.11–2.18) |
| 0 | - | 1 | 2.5 (0.96, 4.04) | |||||||||||
| Overall DL | I2 = 99.9%, p < 0.000 | I2 = 99.7%, p < 0.000 | I2 = 99.3%, p < 0.000 | I2 = 99.6%, p < 0.000 | I2 = 99.2%, p < 0.000 | I2 = 99.1%, p < 0.000 | ||||||||
| Quality level | ||||||||||||||
| Medium | 3 | 25.37 (9.60–41.15) | 1 | 21.5 (20.45–22.55) | 2 | 4.30 (1.66–6.95) | 2 | 2.58 (−0.60–5.75) | 1 | 6.1 (5.48–6.71) | 2 | 3.35 (2.90–3.80) | 2 | 3.24 (2.80–3.67) |
| High | 15 | 39.82 (33.82–45.83) | 11 | 22.40 (17.98–26.82) | 12 | 2.64 (1.67–3.60) | 12 | 3.11 (2.17–4.05) | 11 | 10.52 (8.71–12.33) | 12 | 2.88 (2.02–3.74) | 18 | 2.80 (2.15–3.46) |
| Overall, DL | I2 = 99.9%, p < 0.000 | I2 = 99.7%, p < 0.000 | I2 = 99.3%, p < 0.000 | I2 = 99.6%, p < 0.000 | I2 = 99.2%, p < 0.000 | I2 = 99.1%, p < 0.000 | I2 = 99.7%, p < 0.000 | |||||||
| Data sources | ||||||||||||||
| Primary | 4 | 27.23 (16.94–37.52) | 1 | 21.5 (20.45–22.54) | 2 | 4.30 (1.66–6.95) | 2 | 2.58 (−0.60–5.75) | 1 | 6.01 (5.48–6.71) | 2 | 3.35 (2.90–3.80) | 3 | 3.83 (2.22–5.43) |
| Secondary | 14 | 40.33 (34.12–46.55) | 11 | 22.4 (17.98–26.82) | 12 | 2.64 (1.67–3.60) | 12 | 3.11 (2.17–4.05) | 11 | 10.52 (8.71–12.33) | 12 | 2.88 (2.02–3.74) | 17 | 2.66 (1.99–3.34) |
| Overall, DL | I2 = 99.9%, p < 0.000 | I2 = 99.7%, p < 0.000 | I2 = 99.3%, p < 0.000 | I2 = 99.6%, p < 0.000 | I2 = 99.2%, p < 0.000 | I2 = 99.1%, p < 0.000 | I2 = 99.7%, p < 0.000 | |||||||
| Covariates | Pooled Prevalence(95%CI) | Meta-Regression Coefficient | Std. Err | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| CIAF(%) | SWU(%) | CIAF | SWU | CIAF | SWU | CIAF | SWU | ||
| Residence | Urban | 33.52 (32.43, 34.60) | 2.07 (1.31, 2.83) | - | - | - | - | - | - |
| Rural | 49.70 (45.95, 53.45) | 4.04 (2.92, 5.15) | 16.37 (10.16, 22.60) | 2.085 (−2.2, 7.57) | 2.42 | 1.67 | 0.001 | 0.26 | |
| Sex | Female | 37.38 (19.18, 55.57) | 3.07 (1.69, 4.44) | - | - | - | - | - | - |
| Male | 31.74% (17.39, 46.09) | 6.03 (3.50, 8.50) | −5.68 (−35.22, 23.85) | 2.81 (−1.79, 7.43) | 12.07 | 1.66 | 0.65 | 0.16 | |
| Coefficient | se | t | p-Value | 95%CI | ||
|---|---|---|---|---|---|---|
| CIAF | Slope | 49.10 | 3.46 | 14.20 | 0.00 | 41.77, 56.43 |
| Bias | −16.55 | 9.76 | −1.69 | 0.11 | −37.26, 4.16 | |
| Stunting only | Slope | 20.48 | 2.21 | 9.26 | 0.000 | 15.55, 25.41 |
| Bias | 2.85 | 7.83 | 0.36 | 0.724 | −14.60, 20.29 | |
| Wasting only | Slope | 3.42 | 0.64 | 5.38 | 0.000 | 2.04, 4.81 |
| Bias | −5.19 | 5.23 | −0.99 | 0.34 | −16.59, 6.20 | |
| Underweight only | Slope | 0.67 | 0.39 | 1.69 | 0.12 | −0.192, 1.52 |
| Bias | 8.04 | 5.30 | 1.52 | 0.16 | −3.52, 19.59 | |
| SU | Slope | 14.89 | 0.86 | 17.23 | 0.000 | 12.97, 16.82 |
| Bias | −12.19 | 3.73 | −3.27 | 0.008 | −20.50, 3.88 | |
| WU | Slope | 3.59 | 0.54 | 6.62 | 0.00 | 2.41, 4.77 |
| Bias | −5.82 | 4.38 | −1.33 | 0.21 | −15.37, 3.72 | |
| SWU | Slope | 1.81 | 0.41 | 4.38 | 0.00 | 0.944, 2.68 |
| Bias | 7.32 | 5.76 | 1.27 | 0.22 | −4.78, 19.42 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Worku, M.G.; Mohanty, I.; Mengesha, Z.; Niyonsenga, T. Magnitudes of Various Forms of Undernutrition Among Children from the Composite Index of Anthropometric Failure in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Nutrients 2025, 17, 1818. https://doi.org/10.3390/nu17111818
Worku MG, Mohanty I, Mengesha Z, Niyonsenga T. Magnitudes of Various Forms of Undernutrition Among Children from the Composite Index of Anthropometric Failure in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Nutrients. 2025; 17(11):1818. https://doi.org/10.3390/nu17111818
Chicago/Turabian StyleWorku, Misganaw Gebrie, Itismita Mohanty, Zelalem Mengesha, and Theo Niyonsenga. 2025. "Magnitudes of Various Forms of Undernutrition Among Children from the Composite Index of Anthropometric Failure in Sub-Saharan Africa: A Systematic Review and Meta-Analysis" Nutrients 17, no. 11: 1818. https://doi.org/10.3390/nu17111818
APA StyleWorku, M. G., Mohanty, I., Mengesha, Z., & Niyonsenga, T. (2025). Magnitudes of Various Forms of Undernutrition Among Children from the Composite Index of Anthropometric Failure in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Nutrients, 17(11), 1818. https://doi.org/10.3390/nu17111818





