Biological Age Acceleration Associated with the Progression Trajectory of Cardio-Renal–Metabolic Multimorbidity: A Prospective Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Study Population
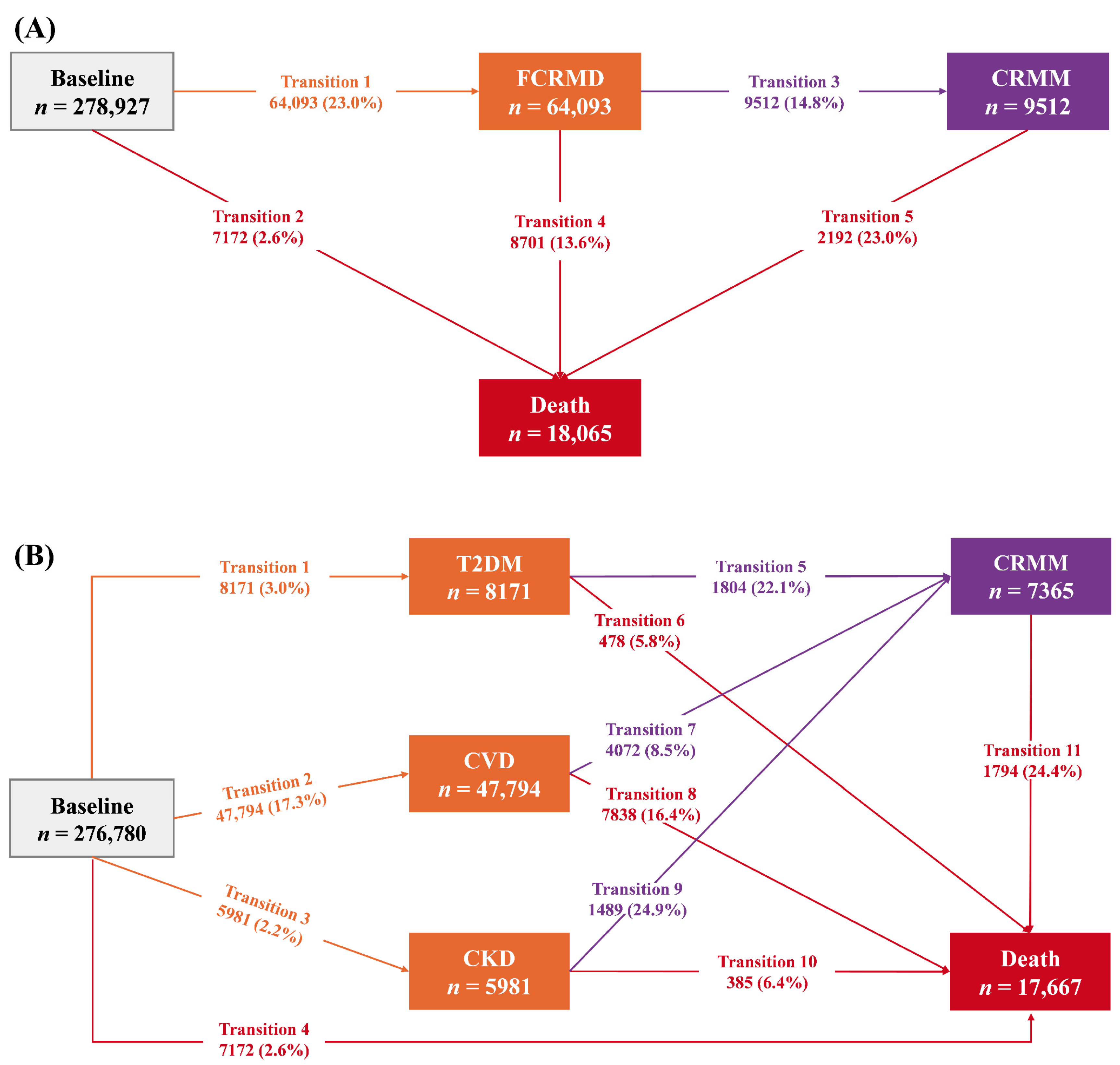
2.2. Follow-Up for Cardio-Renal–Metabolic Diseases and Death
2.3. Assessment of Biological Age
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Descriptive Analysis
3.2. BA Acceleration, CRMM and Mortality
3.3. BA Acceleration and Life Expectancy
3.4. Subgroup Analyses
3.5. Sensitivity Analyses
4. Discussion
4.1. Principal Findings
4.2. Comparison with Previous Studies
4.3. Mechanism
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Ndumele, C.E.; Rangaswami, J.; Chow, S.L.; Neeland, I.J.; Tuttle, K.R.; Khan, S.S.; Coresh, J.; Mathew, R.O.; Baker-Smith, C.M.; Carnethon, M.R.; et al. Cardiovascular-Kidney-Metabolic Health: A Presidential Advisory From the American Heart Association. Circulation 2023, 148, 1606–1635. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Liu, X.; Wang, L.; Zhang, Y.; Xiang, Y.; Cai, J.; Xu, H.; Xiao, X.; Zhao, X. Lifestyle factors and their relative contributions to longitudinal progression of cardio-renal-metabolic multimorbidity: A prospective cohort study. Cardiovasc. Diabetol. 2024, 23, 265. [Google Scholar] [CrossRef] [PubMed]
- Marassi, M.; Fadini, G.P. The cardio-renal-metabolic connection: A review of the evidence. Cardiovasc. Diabetol. 2023, 22, 195. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, R.; Ostrominski, J.W.; Vaduganathan, M. Prevalence of Cardiovascular-Kidney-Metabolic Syndrome Stages in US Adults, 2011-2020. JAMA 2024, 331, 1858–1860. [Google Scholar] [CrossRef]
- Tang, H.; Huang, J.; Zhang, X.; Chen, X.; Yang, Q.; Luo, N.; Lin, H.; Hong, J.; Wu, S.; Tian, C.; et al. Association between triglyceride glucose-body mass index and the trajectory of cardio-renal-metabolic multimorbidity: Insights from multi-state modelling. Cardiovasc. Diabetol. 2025, 24, 133. [Google Scholar] [CrossRef]
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Li, N.; Li, Y.; Cui, L.; Shu, R.; Song, H.; Wang, J.; Chen, S.; Liu, B.; Shi, H.; Gao, H.; et al. Association between different stages of cardiovascular-kidney-metabolic syndrome and the risk of all-cause mortality. Atherosclerosis 2024, 397, 118585. [Google Scholar] [CrossRef]
- Chen, L.; Zhang, Y.; Yu, C.; Guo, Y.; Sun, D.; Pang, Y.; Pei, P.; Yang, L.; Millwood, I.Y.; Walters, R.G.; et al. Modeling biological age using blood biomarkers and physical measurements in Chinese adults. eBioMedicine 2023, 89, 104458. [Google Scholar] [CrossRef]
- Khan, S.S.; Singer, B.D.; Vaughan, D.E. Molecular and physiological manifestations and measurement of aging in humans. Aging Cell 2017, 16, 624–633. [Google Scholar] [CrossRef]
- Mao, R.; Wang, F.; Zhong, Y.; Meng, X.; Zhang, T.; Li, J. Association of biological age acceleration with cardiac morphology, function, and incident heart failure: Insights from UK Biobank participants. Eur. Heart J.-Cardiovasc. Imaging 2024, 25, 1315–1323. [Google Scholar] [CrossRef] [PubMed]
- Belsky, D.W.; Moffitt, T.E.; Cohen, A.A.; Corcoran, D.L.; Levine, M.E.; Prinz, J.A.; Schaefer, J.; Sugden, K.; Williams, B.; Poulton, R.; et al. Eleven Telomere, Epigenetic Clock, and Biomarker-Composite Quantifications of Biological Aging: Do They Measure the Same Thing? Am. J. Epidemiol. 2018, 187, 1220–1230. [Google Scholar] [CrossRef]
- Liu, Z.; Kuo, P.L.; Horvath, S.; Crimmins, E.; Ferrucci, L.; Levine, M. A new aging measure captures morbidity and mortality risk across diverse subpopulations from NHANES IV: A cohort study. PLoS Med. 2018, 15, e1002718. [Google Scholar] [CrossRef]
- Klemera, P.; Doubal, S. A new approach to the concept and computation of biological age. Mech. Ageing Dev. 2006, 127, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Graf, G.H.; Crowe, C.L.; Kothari, M.; Kwon, D.; Manly, J.J.; Turney, I.C.; Valeri, L.; Belsky, D.W. Testing Black-White Disparities in Biological Aging Among Older Adults in the United States: Analysis of DNA-Methylation and Blood-Chemistry Methods. Am. J. Epidemiol. 2022, 191, 613–625. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.L.; Pilling, L.C.; Liu, Z.; Atkins, J.L.; Levine, M.E. Genetic associations for two biological age measures point to distinct aging phenotypes. Aging Cell 2021, 20, e13376. [Google Scholar] [CrossRef]
- Chen, Z.; Chen, Z.; Jin, X. Mendelian randomization supports causality between overweight status and accelerated aging. Aging Cell 2023, 22, e13899. [Google Scholar] [CrossRef]
- Li, X.; Li, C.; Zhang, W.; Wang, Y.; Qian, P.; Huang, H. Inflammation and aging: Signaling pathways and intervention therapies. Signal Transduct. Target. Ther. 2023, 8, 239. [Google Scholar] [CrossRef]
- Vatner, S.F.; Zhang, J.; Oydanich, M.; Berkman, T.; Naftalovich, R.; Vatner, D.E. Healthful aging mediated by inhibition of oxidative stress. Ageing Res. Rev. 2020, 64, 101194. [Google Scholar] [CrossRef]
- Li, X.; Wang, J.; Zhang, M.; Li, X.; Fan, Y.; Zhou, X.; Sun, Y.; Qiu, Z. Biological aging mediates the associations of metabolic score for insulin resistance with all-cause and cardiovascular disease mortality among US adults: A nationwide cohort study. Diabetes Obes. Metab. 2024, 26, 3552–3564. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, J.; Yu, B.; Sun, Y.; Chen, Y.; Lu, Y.; Wang, N.; Xia, F. Accelerated biological aging, mediating amino acids, and risk of incident type 2 diabetes: A prospective cohort study. J. Endocrinol. Investig. 2025, 48, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.G.; Suh, E.; Lee, J.W.; Kim, D.W.; Cho, K.H.; Bae, C.Y. Biological age as a health index for mortality and major age-related disease incidence in Koreans: National Health Insurance Service—Health screening 11-year follow-up study. Clin. Interv. Aging. 2018, 13, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Zhang, X.; Li, Y.; Wang, W.; Lai, W.; Zhang, W.; Kang, K.; Zhong, X.; Guo, L. Associations of combined accelerated biological aging and genetic susceptibility with incidence of heart failure in a population-based cohort study. Aging Cell 2024, 24, e14430. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Yan, H.; Zhang, Y.; Zhou, Q.; Meng, X.; Lin, J.; Jiang, Y.; Pan, Y.; Wang, Y. Accelerated biological aging increases the risk of short- and long-term stroke prognosis in patients with ischemic stroke or TIA. eBioMedicine 2025, 111, 105494. [Google Scholar] [CrossRef]
- Zheng, G.; Chang, Q.; Zhang, Y.; Liu, Y.; Ji, C.; Yang, H.; Chen, L.; Xia, Y.; Zhao, Y. Associations of clinical parameter-based accelerated aging, genetic predisposition with risk of chronic kidney disease and associated life expectancy: A prospective cohort study. Aging Cell 2025, 24, e14453. [Google Scholar] [CrossRef]
- Sudlow, C.; Gallacher, J.; Allen, N.; Beral, V.; Burton, P.; Danesh, J.; Downey, P.; Elliott, P.; Green, J.; Landray, M.; et al. UK biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015, 12, e1001779. [Google Scholar] [CrossRef]
- Zou, X.; Zhao, J.; Feng, A.; Chan, K.H.K.; Wu, W.C.; Manson, J.E.; Liu, S.; Li, J. Adversities in childhood and young adulthood and incident cardiovascular diseases: A prospective cohort study. eClinicalMedicine 2024, 69, 102458. [Google Scholar] [CrossRef]
- Ostrominski, J.W.; Arnold, S.V.; Butler, J.; Fonarow, G.C.; Hirsch, J.S.; Palli, S.R.; Donato, B.M.K.; Parrinello, C.M.; O’Connell, T.; Collins, E.B.; et al. Prevalence and Overlap of Cardiac, Renal, and Metabolic Conditions in US Adults, 1999-2020. JAMA Cardiol. 2023, 8, 1050–1060. [Google Scholar] [CrossRef]
- Jiang, M.; Tian, S.; Liu, S.; Wang, Y.; Guo, X.; Huang, T.; Lin, X.; Belsky, D.W.; Baccarelli, A.A.; Gao, X. Accelerated biological aging elevates the risk of cardiometabolic multimorbidity and mortality. Nat. Cardiovasc. Res. 2024, 3, 332–342. [Google Scholar] [CrossRef]
- Kwon, D.; Belsky, D.W. A toolkit for quantification of biological age from blood chemistry and organ function test data: BioAge. Geroscience 2021, 43, 2795–2808. [Google Scholar] [CrossRef]
- Zhang, Y.B.; Chen, C.; Pan, X.F.; Guo, J.; Li, Y.; Franco, O.H.; Liu, G.; Pan, A. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: Two prospective cohort studies. BMJ 2021, 373, n604. [Google Scholar] [CrossRef] [PubMed]
- Putter, H.; Fiocco, M.; Geskus, R.B. Tutorial in biostatistics: Competing risks and multi-state models. Stat. Med. 2007, 26, 2389–2430. [Google Scholar] [CrossRef] [PubMed]
- de Wreede, L.C.; Fiocco, M.; Putter, H. The mstate package for estimation and prediction in non- and semi-parametric multi-state and competing risks models. Comput. Methods Programs Biomed. 2010, 99, 261–274. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Zhang, Q.; Yu, K.; Meng, X.; Kan, H.; Chen, R. Long-term exposure to ambient air pollution is a risk factor for trajectory of cardiometabolic multimorbidity: A prospective study in the UK Biobank. eBioMedicine 2022, 84, 104282. [Google Scholar] [CrossRef]
- Chen, Y.; Yang, H.; Li, D.; Zhou, L.; Lin, J.; Yin, X.; Yang, W.; Gao, Y.; Zhang, Q.; Leng, S.X.; et al. Association of cardiorespiratory fitness with the incidence and progression trajectory of cardiometabolic multimorbidity. Br. J. Sports Med. 2025, 59, 306–315. [Google Scholar] [CrossRef]
- van den Hout, A.; Sum Chan, M.; Matthews, F. Estimation of life expectancies using continuous-time multi-state models. Comput. Methods Programs Biomed. 2019, 178, 11–18. [Google Scholar] [CrossRef]
- Xia, X.; Qiu, C.; Rizzuto, D.; Grande, G.; Laukka, E.J.; Fratiglioni, L.; Guo, J.; Vetrano, D.L. The age-dependent association of Life’s Simple 7 with transitions across cognitive states after age 60. J. Intern. Med. 2023, 294, 191–202. [Google Scholar] [CrossRef]
- Davies, L.E.; Mercer, S.W.; Brittain, K.; Jagger, C.; Robinson, L.; Kingston, A. The association between multimorbidity and mobility disability-free life expectancy in adults aged 85 years and over: A modelling study in the Newcastle 85+ cohort. PLoS Med. 2022, 19, e1004130. [Google Scholar] [CrossRef]
- Inker, L.A.; Eneanya, N.D.; Coresh, J.; Tighiouart, H.; Wang, D.; Sang, Y.; Crews, D.C.; Doria, A.; Estrella, M.M.; Froissart, M.; et al. New Creatinine- and Cystatin C-Based Equations to Estimate GFR without Race. N. Engl. J. Med. 2021, 385, 1737–1749. [Google Scholar] [CrossRef]
- Xiang, H.; Huang, Y.; Zhang, Y.; He, P.; Ye, Z.; Yang, S.; Zhang, Y.; Gan, X.; Hou, F.F.; Qin, X. Clinical biomarker-based biological ageing and the risk of adverse outcomes in patients with chronic kidney disease. Age Ageing 2024, 53, afae245. [Google Scholar] [CrossRef]
- Li, W.J.; Chen, X.M.; Nie, X.Y.; Zhang, J.; Cheng, Y.J.; Lin, X.X.; Wu, S.H. Cardiac troponin and C-reactive protein for predicting all-cause and cardiovascular mortality in patients with chronic kidney disease: A meta-analysis. Clinics 2015, 70, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Tian, R.; Tian, M.; Wang, L.; Qian, H.; Zhang, S.; Pang, H.; Liu, Z.; Fang, L.; Shen, Z. C-reactive protein for predicting cardiovascular and all-cause mortality in type 2 diabetic patients: A meta-analysis. Cytokine 2019, 117, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.A.; Milot, E.; Yong, J.; Seplaki, C.L.; Fülöp, T.; Bandeen-Roche, K.; Fried, L.P. A novel statistical approach shows evidence for multi-system physiological dysregulation during aging. Mech. Ageing Dev. 2013, 134, 110–117. [Google Scholar] [CrossRef]
- Zhu, R.; Wang, R.; He, J.; Wang, L.; Chen, H.; Niu, X.; Sun, Y.; Guan, Y.; Gong, Y.; Zhang, L.; et al. Prevalence of Cardiovascular-Kidney-Metabolic Syndrome Stages by Social Determinants of Health. JAMA Netw. Open. 2024, 7, e2445309. [Google Scholar] [CrossRef]
- Chowdhury, S.R.; Chandra Das, D.; Sunna, T.C.; Beyene, J.; Hossain, A. Global and regional prevalence of multimorbidity in the adult population in community settings: A systematic review and meta-analysis. eClinicalMedicine 2023, 57, 101860. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Hou, R.; Zhao, J.; Wang, X.; Wei, J.; Pan, X.; Zhu, X. Lifestyle effects on aging and CVD: A spotlight on the nutrient-sensing network. Ageing Res. Rev. 2023, 92, 102121. [Google Scholar] [CrossRef]
- Frølich, A.; Ghith, N.; Schiøtz, M.; Jacobsen, R.; Stockmarr, A. Multimorbidity, healthcare utilization and socioeconomic status: A register-based study in Denmark. PLoS ONE 2019, 14, e0214183. [Google Scholar] [CrossRef]
- Havranek, E.P. Epidemiology of heart disease: The influence of socioeconomic position. Trends Cardiovasc. Med. 2019, 29, 298–303. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Baumer, Y.; Baah, F.O.; Baez, A.S.; Farmer, N.; Mahlobo, C.T.; Pita, M.A.; Potharaju, K.A.; Tamura, K.; Wallen, G.R. Social Determinants of Cardiovascular Disease. Circ. Res. 2022, 130, 782–799. [Google Scholar] [CrossRef]
- Ndumele, C.E.; Neeland, I.J.; Tuttle, K.R.; Chow, S.L.; Mathew, R.O.; Khan, S.S.; Coresh, J.; Baker-Smith, C.M.; Carnethon, M.R.; Després, J.-P.; et al. A Synopsis of the Evidence for the Science and Clinical Management of Cardiovascular-Kidney-Metabolic (CKM) Syndrome: A Scientific Statement From the American Heart Association. Circulation 2023, 148, 1636–1664. [Google Scholar] [CrossRef]
- Sheng, X.; Qiu, C.; Liu, H.; Gluck, C.; Hsu, J.Y.; He, J.; Hsu, C.Y.; Sha, D.; Weir, M.R.; Isakova, T.; et al. Systematic integrated analysis of genetic and epigenetic variation in diabetic kidney disease. Proc. Natl. Acad. Sci. USA 2020, 117, 29013–29024. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.C.; Brownlee, M.; Susztak, K.; Sharma, K.; Jandeleit-Dahm, K.A.; Zoungas, S.; Rossing, P.; Groop, P.H.; Cooper, M.E. Diabetic kidney disease. Nat. Rev. Dis. Primers. 2015, 1, 15018. [Google Scholar] [CrossRef] [PubMed]
- Ajoolabady, A.; Pratico, D.; Vinciguerra, M.; Lip, G.Y.H.; Franceschi, C.; Ren, J. Inflammaging: Mechanisms and role in the cardiac and vasculature. Trends Endocrinol. Metab. 2023, 34, 373–387. [Google Scholar] [CrossRef] [PubMed]
- Adamo, L.; Rocha-Resende, C.; Prabhu, S.D.; Mann, D.L. Reappraising the role of inflammation in heart failure. Nat. Rev. Cardiol. 2020, 17, 269–285. [Google Scholar] [CrossRef]


| Characteristics a | Total (n = 278,927) | Free of CRMD (n = 214,834) | Incident FCRMD (n = 54,581) | Incident CRMM (n = 9512) |
|---|---|---|---|---|
| Age (years) | 55.69 (8.10) | 54.62 (8.02) | 58.98 (7.35) | 60.93 (6.73) |
| Sex (male) | 122,796 (44.0) | 88,785 (41.3) | 28,753 (52.7) | 5258 (55.3) |
| Ethnicity (White) | 265,381 (95.1) | 204,287 (95.1) | 52,184 (95.6) | 8910 (93.7) |
| Townsend deprivation index (>median) | 139,730 (50.1) | 106,664 (49.6) | 27,728 (50.8) | 5338 (56.1) |
| Educational level (high) | 136,707 (49.0) | 109,100 (50.8) | 24,189 (44.3) | 3418 (35.9) |
| Body mass index (kg·m−2) | 27.01(4.50) | 26.67 (4.32) | 27.88 (4.73) | 29.86 (5.34) |
| Smoking status | ||||
| Never | 158,072 (56.7) | 125,926 (58.6) | 27,839 (51.0) | 4307 (45.3) |
| Former | 92,457 (33.1) | 68,569 (31.9) | 20,122 (36.9) | 3766 (39.6) |
| Current | 28,398 (10.2) | 20,339 (9.5) | 6620 (12.1) | 1439 (15.1) |
| Alcohol consumption | ||||
| None | 64,576 (23.1) | 47,707 (22.2) | 13,728 (25.1) | 3141 (33.0) |
| Moderate | 139,097 (49.9) | 108,772 (50.6) | 26,125 (47.9) | 4200 (44.2) |
| Heavy | 75,254 (27.0) | 58,355 (27.2) | 14,728 (27.0) | 2171 (22.8) |
| Physical activity | ||||
| Low | 49,745 (17.8) | 37,573 (17.5) | 10,068 (18.4) | 2104(22.1) |
| Moderate | 113,783(40.8) | 88,041 (41.0) | 21,877 (40.1) | 3865 (40.7) |
| High | 115,399(41.4) | 89,220 (41.5) | 22,636 (41.5) | 3543 (37.2) |
| Dietary behaviors (healthy) | 45,823 (16.4) | 35,098 (16.3) | 9307 (17.1) | 1418 (14.9) |
| Biological age measures | ||||
| PhenoAge (years) | 49.18 (9.07) | 47.84 (8.79) | 53.12 (8.41) | 56.92 (8.34) |
| PhenoAge acceleration (years) | −6.51 (4.26) | −6.78 (4.09) | −5.86 (4.50) | −4.01 (5.26) |
| KDMAge (years) | 52.38 (12.41) | 50.82 (12.08) | 56.69 (11.87) | 62.92 (11.88) |
| KDMAge acceleration (years) | −3.31 (9.76) | −3.80 (9.48) | −2.29 (10.27) | 2.00 (10.86) |
| Components of biological age measures | ||||
| Lymphocyte (%) b | 29.15 (7.36) | 29.30 (7.28) | 28.74 (7.59) | 28.22 (7.71) |
| Mean cell volume (fL) b | 82.82 (5.26) | 82.78 (5.20) | 83.03 (5.43) | 82.60 (5.49) |
| Serum glucose (mmol/L) b | 4.99 (0.84) | 4.95 (0.72) | 5.09 (1.04) | 5.45 (1.68) |
| Red cell distribution width (%) b | 13.45 (0.94) | 13.42 (0.94) | 13.51 (0.94) | 13.64 (1.05) |
| White blood cell count (1000 cells/uL) b | 6.78 (1.86) | 6.71 (1.79) | 6.96 (2.02) | 7.39 (2.10) |
| Albumin (g/dL) b,c | 4.53 (0.26) | 4.54 (0.26) | 4.50 (0.26) | 4.47 (0.27) |
| Creatinine (mg/dL) b,c | 0.81 (0.16) | 0.80 (0.15) | 0.83 (0.17) | 0.90 (0.23) |
| C-reactive protein (mg/dL) b,c | 0.24 (0.40) | 0.22 (0.37) | 0.29 (0.45) | 0.40 (0.54) |
| Alkaline phosphatase (U/L) b,c | 82.53 (25.25) | 81.37 (24.50) | 85.74 (27.00) | 90.19 (28.40) |
| FEV1 (L) c | 2.77 (0.78) | 2.81 (0.77) | 2.70 (0.79) | 2.51 (0.76) |
| SBP (mm Hg) c | 137.15 (18.20) | 135.53 (17.80) | 142.02 (18.36) | 145.86 (18.60) |
| Total cholesterol (mg/dL) c | 225.41 (41.79) | 225.21 (41.30) | 226.77 (42.99) | 222.24 (45.34) |
| Glycated hemoglobin (%) c | 5.36 (0.43) | 5.32 (0.36) | 5.45 (0.52) | 5.75 (0.79) |
| Blood urea nitrogen (mg/dL) c | 14.90 (3.52) | 14.71 (3.38) | 15.35 (3.69) | 16.54 (4.62) |
| Transition | Cases | PhenoAge Acceleration | KDMAge Acceleration | ||||
|---|---|---|---|---|---|---|---|
| Biologically Younger | Biologically Older | Per 1 SD | Biologically Younger | Biologically Older | Per 1 SD | ||
| Baseline to FCRMD | 64,093 | Reference | 1.64 (1.59, 1.68) | 1.18 (1.17, 1.19) | Reference | 1.37 (1.35, 1.39) | 1.22 (1.21, 1.23) |
| Baseline to death | 7172 | Reference | 1.95 (1.80, 2.10) | 1.25 (1.22, 1.27) | Reference | 1.24 (1.18, 1.30) | 1.16 (1.13, 1.19) |
| FCRMD to CRMM | 9512 | Reference | 1.67 (1.58, 1.77) | 1.24 (1.22, 1.26) | Reference | 1.55 (1.49, 1.62) | 1.33 (1.30, 1.35) |
| FCRMD to death | 8701 | Reference | 1.42 (1.34, 1.51) | 1.13 (1.11, 1.15) | Reference | 1.06 (1.02, 1.11) | 1.05 (1.02, 1.07) |
| CRMM to death | 2192 | Reference | 1.33 (1.20, 1.47) | 1.09 (1.06, 1.12) | Reference | 1.11 (1.01, 1.21) | 1.04 (1.00, 1.08) |
| Transition | Cases | PhenoAge Acceleration | KDMAge Acceleration | ||||
|---|---|---|---|---|---|---|---|
| Biologically Younger | Biologically Older | Per 1 SD | Biologically Younger | Biologically Older | Per 1 SD | ||
| Baseline to T2DM | 8171 | Reference | 1.87 (1.75, 1.99) | 1.27 (1.24, 1.29) | Reference | 1.92 (1.83, 2.01) | 1.50 (1.47, 1.53) |
| Baseline to CVD | 47,794 | Reference | 1.41 (1.36, 1.45) | 1.11 (1.10, 1.12) | Reference | 1.23 (1.21, 1.26) | 1.13 (1.12, 1.14) |
| Baseline to CKD | 5981 | Reference | 2.77 (2.58, 2.98) | 1.40 (1.38, 1.42) | Reference | 1.88 (1.78, 1.98) | 1.59 (1.55, 1.63) |
| Baseline to death | 7172 | Reference | 1.97 (1.83, 2.12) | 1.25 (1.23, 1.27) | Reference | 1.25 (1.19, 1.31) | 1.17 (1.14, 1.20) |
| T2DM to CRMM | 1804 | Reference | 1.31 (1.16, 1.47) | 1.14 (1.10, 1.19) | Reference | 1.20 (1.09, 1.32) | 1.15 (1.10, 1.20) |
| T2DM to death | 478 | Reference | 1.50 (1.20, 1.88) | 1.10 (1.02, 1.18) | Reference | 0.97 (0.81, 1.17) | 0.96 (0.88, 1.05) |
| CVD to CRMM | 4072 | Reference | 1.71 (1.56, 1.86) | 1.26 (1.23, 1.29) | Reference | 1.60 (1.49, 1.70) | 1.34 (1.30, 1.38) |
| CVD to death | 7838 | Reference | 1.57 (1.47, 1.68) | 1.17 (1.15, 1.20) | Reference | 1.15 (1.10, 1.21) | 1.10 (1.08, 1.13) |
| CKD to CRMM | 1489 | Reference | 1.58 (1.39, 1.80) | 1.15 (1.10, 1.20) | Reference | 1.28 (1.15, 1.42) | 1.20 (1.15, 1.26) |
| CKD to death | 385 | Reference | 1.27 (0.97, 1.65) | 1.12 (1.03, 1.22) | Reference | 0.85 (0.70, 1.05) | 0.94 (0.86, 1.04) |
| CRMM to death | 8171 | Reference | 1.29 (1.15, 1.44) | 1.07 (1.04, 1.11) | Reference | 1.13 (1.02, 1.24) | 1.03 (0.99, 1.07) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tian, Y.; Wang, J.; Zhu, T.; Li, X.; Zhang, H.; Zhao, X.; Yang, X.; Luo, Y.; Tao, L.; Wu, Z.; et al. Biological Age Acceleration Associated with the Progression Trajectory of Cardio-Renal–Metabolic Multimorbidity: A Prospective Cohort Study. Nutrients 2025, 17, 1783. https://doi.org/10.3390/nu17111783
Tian Y, Wang J, Zhu T, Li X, Zhang H, Zhao X, Yang X, Luo Y, Tao L, Wu Z, et al. Biological Age Acceleration Associated with the Progression Trajectory of Cardio-Renal–Metabolic Multimorbidity: A Prospective Cohort Study. Nutrients. 2025; 17(11):1783. https://doi.org/10.3390/nu17111783
Chicago/Turabian StyleTian, Yixing, Jinqi Wang, Tianyu Zhu, Xia Li, Haiping Zhang, Xiaoyu Zhao, Xinghua Yang, Yanxia Luo, Lixin Tao, Zhiyuan Wu, and et al. 2025. "Biological Age Acceleration Associated with the Progression Trajectory of Cardio-Renal–Metabolic Multimorbidity: A Prospective Cohort Study" Nutrients 17, no. 11: 1783. https://doi.org/10.3390/nu17111783
APA StyleTian, Y., Wang, J., Zhu, T., Li, X., Zhang, H., Zhao, X., Yang, X., Luo, Y., Tao, L., Wu, Z., & Guo, X. (2025). Biological Age Acceleration Associated with the Progression Trajectory of Cardio-Renal–Metabolic Multimorbidity: A Prospective Cohort Study. Nutrients, 17(11), 1783. https://doi.org/10.3390/nu17111783






