Associations of Academic Study- and Non-Study-Related Sedentary Behaviors with Incident Obesity in Children and Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Exposure Variables
2.3. Outcomes
2.4. Potential Confounders
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Associations of Sedentary Behaviors and SSB Consumption with Overweight/Obesity Incidence and BMI
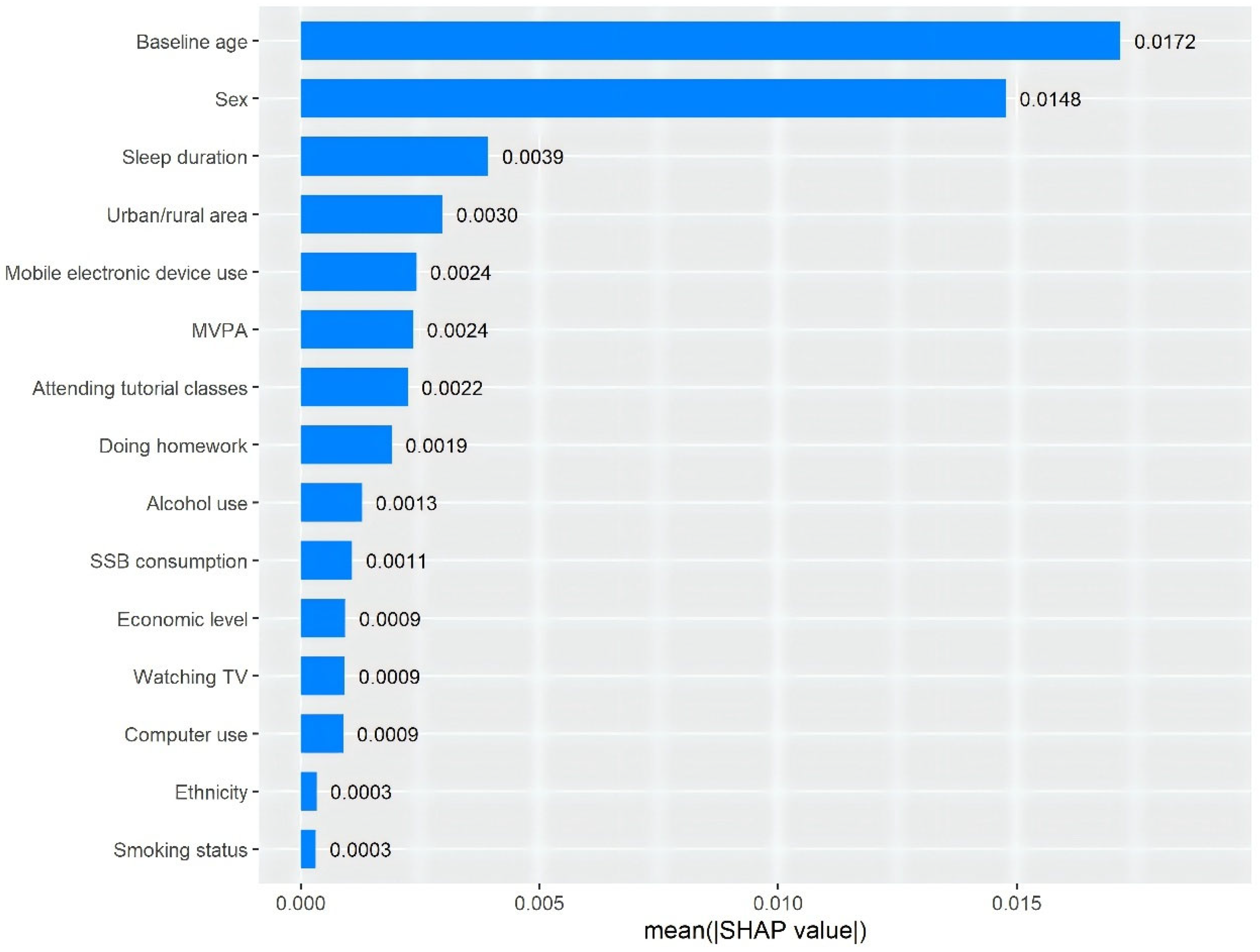
3.3. Mutually Adjusted Results and the Importance Ranking of Five Specific Sedentary Behaviors
3.4. Joint Associations of Total Sedentary Time and SSB Consumption with Overweight/Obesity Incidence and BMI
3.5. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Facts About Overweight and Obesity. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 28 March 2024).
- Pan, X.F.; Wang, L.; Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021, 9, 373–392. [Google Scholar] [CrossRef]
- Dobbie, L.J.; Pittam, B.; Zhao, S.S.; Alam, U.; Hydes, T.J.; Barber, T.M.; Cuthbertson, D.J. Childhood, adolescent, and adulthood adiposity are associated with risk of PCOS: A Mendelian randomization study with meta-analysis. Hum. Reprod. 2023, 38, 1168–1182. [Google Scholar] [CrossRef]
- Lindberg, L.; Hagman, E.; Danielsson, P.; Marcus, C.; Persson, M. Anxiety and depression in children and adolescents with obesity: A nationwide study in Sweden. BMC Med. 2020, 18, 30. [Google Scholar] [CrossRef]
- Chen, D.R.; Lu, H.H. Social alienation of adolescents with obesity in classrooms: A multilevel approach. J. Adolesc. 2022, 94, 81–91. [Google Scholar] [CrossRef]
- Umer, A.; Kelley, G.A.; Cottrell, L.E.; Giacobbi, P., Jr.; Innes, K.E.; Lilly, C.L. Childhood obesity and adult cardiovascular disease risk factors: A systematic review with meta-analysis. BMC Public Health 2017, 17, 683. [Google Scholar] [CrossRef]
- Fang, X.; Zuo, J.; Zhou, J.; Cai, J.; Chen, C.; Xiang, E.; Li, H.; Cheng, X.; Chen, P. Childhood obesity leads to adult type 2 diabetes and coronary artery diseases: A 2-sample mendelian randomization study. Medicine 2019, 98, e16825. [Google Scholar] [CrossRef]
- Nguyen, M.; Jarvis, S.E.; Tinajero, M.G.; Yu, J.; Chiavaroli, L.; Mejia, S.B.; Khan, T.A.; Tobias, D.K.; Willett, W.C.; Hu, F.B.; et al. Sugar-sweetened beverage consumption and weight gain in children and adults: A systematic review and meta-analysis of prospective cohort studies and randomized controlled trials. Am. J. Clin. Nutr. 2023, 117, 160–174. [Google Scholar] [CrossRef]
- Shao, T.; Wang, L.; Chen, H. Association Between Sedentary Behavior and Obesity in School-age Children in China: A Systematic Review of Evidence. Curr. Pharm. Des. 2020, 26, 5012–5020. [Google Scholar] [CrossRef]
- Rey-López, J.P.; Vicente-Rodríguez, G.; Biosca, M.; Moreno, L.A. Sedentary behaviour and obesity development in children and adolescents. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 242–251. [Google Scholar] [CrossRef] [PubMed]
- Barnett, T.A.; Kelly, A.S.; Young, D.R.; Perry, C.K.; Pratt, C.A.; Edwards, N.M.; Rao, G.; Vos, M.B. Sedentary Behaviors in Today’s Youth: Approaches to the Prevention and Management of Childhood Obesity: A Scientific Statement From the American Heart Association. Circulation 2018, 138, e142–e159. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Adolescent Mental Health: A UNICEF Priority For 2021–2025. Available online: https://www.unicef.cn/en/reports/adolescent-mental-health (accessed on 28 May 2024).
- Bertuol, C.; da Silveira, M.H.C.; Krug, R.R.; Kupske, J.W.; Mielke, G.I.; Del Duca, G.F. Use of electronic devices in leisure time modifies the prevalence and factors associated with sedentary behavior derived exclusively from excessive television viewing among Brazilian adults. BMC Public Health 2023, 23, 1602. [Google Scholar] [CrossRef]
- Moradell, A.; Santaliestra-Pasías, A.M.; Aparicio-Ugarriza, R.; Huybrechts, I.; Bertalanné Szommer, A.; Forsner, M.; González-Gross, M.; Kafatos, A.; Androutsos, O.; Michels, N.; et al. Are Physical Activity and Sedentary Screen Time Levels Associated With Food Consumption in European Adolescents? The HELENA Study. J. Am. Nutr. Assoc. 2023, 42, 55–66. [Google Scholar] [CrossRef]
- Kanellopoulou, A.; Diamantis, D.V.; Notara, V.; Panagiotakos, D.B. Extracurricular Sports Participation and Sedentary Behavior in Association with Dietary Habits and Obesity Risk in Children and Adolescents and the Role of Family Structure: A Literature Review. Curr. Nutr. Rep. 2021, 10, 1–11. [Google Scholar] [CrossRef]
- Kremers, S.P.; Visscher, T.L.; Seidell, J.C.; van Mechelen, W.; Brug, J. Cognitive determinants of energy balance-related behaviours: Measurement issues. Sports Med. 2005, 35, 923–933. [Google Scholar] [CrossRef]
- Dong, Z.; Lu, Z.; Song, X.; Song, Z.; Liu, J.; Zhang, Y.; Jiang, J.; Wang, R.; Yuan, W.; Qin, Y.; et al. Epidemiological characteristics and related factors of multimorbidity of wasting and spinal curvature abnormalities among children and adolescents aged 6–18 years in Inner Mongolia Autonomous Region. Chin. J. Prev. Med. 2025, 59, 151–159. [Google Scholar] [CrossRef]
- Ji, C.; Ma, G.; Zhang, L.; Chen, T.; Ma, J.; Li, Y.; Zhang, Y.; Du, S.; Zhu, G.; Ji, H. Screening for Overweight and Obesity Among School-Age Children and Adolescents. Available online: https://www.chinesestandard.net/PDF/English.aspx/WST586-2018 (accessed on 25 March 2024).
- de Menezes, M.C.; Duran, A.C.; Langellier, B.; Pérez-Ferrer, C.; Barnoya, J.; Mayén, A.L. Socioeconomic Position, Pre-Obesity and Obesity in Latin American Cities: A Systematic Review. Int. J. Soc. Determinants Health Health Serv. 2024, 54, 224–232. [Google Scholar] [CrossRef]
- Guo, H.; Phung, D.; Chu, C. Sociodemographic, lifestyle, behavioral, and parental factors associated with sugar-sweetened beverage consumption in children in China. PLoS ONE 2021, 16, e0261199. [Google Scholar] [CrossRef]
- Yepez, C.E.; Anderson, C.E.; Frost, E.; Whaley, S.E.; Koleilat, M. Sleep Duration Is Associated with Household Food Insecurity and Sugar-Sweetened Beverage Intake Among Women, Infants and Children Participating Children Ages 0–5. Am. J. Health Promot. 2024, 38, 492–502. [Google Scholar] [CrossRef]
- Gao, G.; Liu, Y.; Dong, Z.; He, J.; Wang, C.; Chen, X.; Chen, W. Investigation of obesity and its related factors among Chinese medical staff: A cross-sectional pilot study. Eat. Weight. Disord. 2024, 29, 15. [Google Scholar] [CrossRef]
- Carrasquilla, G.D.; García-Ureña, M.; Romero-Lado, M.J.; Kilpeläinen, T.O. Estimating causality between smoking and abdominal obesity by Mendelian randomization. Addiction 2024, 119, 1024–1034. [Google Scholar] [CrossRef]
- Zou, G. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 2004, 159, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Torlay, L.; Perrone-Bertolotti, M.; Thomas, E.; Baciu, M. Machine learning-XGBoost analysis of language networks to classify patients with epilepsy. Brain Inform. 2017, 4, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Zhang, Y.; Shi, X.; Almpanidis, G.; Fan, G.; Shen, X. On Incremental Learning for Gradient Boosting Decision Trees. Neural Process. Lett. 2019, 50, 957–987. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Lee, S.-I. A unified approach to interpreting model predictions. In Proceedings of the 31st International Conference on Neural Information Processing Systems—NIPS’17, Long Beach, CA, USA, 4–9 December 2017; pp. 4768–4777. [Google Scholar]
- Xu, S.; Sun, M. The interpretable machine learning model associated with metal mixtures to identify hypertension via EMR mining method. J. Clin. Hypertens 2024, 26, 187–196. [Google Scholar] [CrossRef]
- Yu, J.; Huang, F.; Zhang, X.; Xue, H.; Ni, X.; Yang, J.; Zou, Z.; Du, W. Association of Sugar-Sweetened Beverage Consumption and Moderate-to-Vigorous Physical Activity with Childhood and Adolescent Overweight/Obesity: Findings from a Surveillance Project in Jiangsu Province of China. Nutrients 2023, 15, 4164. [Google Scholar] [CrossRef]
- Kabali, H.K.; Irigoyen, M.M.; Nunez-Davis, R.; Budacki, J.G.; Mohanty, S.H.; Leister, K.P.; Bonner, R.L., Jr. Exposure and Use of Mobile Media Devices by Young Children. Pediatrics 2015, 136, 1044–1050. [Google Scholar] [CrossRef]
- Wang, D.; Xiong, R.; Zhang, J.; Han, X.; Jin, L.; Liu, W.; Qu, Y.; Chen, Q.; Chen, S.; Chen, X.; et al. Effect of Extracurricular After-School Physical Activities on Academic Performance of Schoolchildren: A Cluster Randomized Clinical Trial. JAMA Pediatr. 2023, 177, 1141–1148. [Google Scholar] [CrossRef]
- Godakanda, I.; Abeysena, C.; Lokubalasooriya, A. Sedentary behavior during leisure time, physical activity and dietary habits as risk factors of overweight among school children aged 14–15 years: Case control study. BMC Res. Notes 2018, 11, 186. [Google Scholar] [CrossRef]
- Ren, H.; Zhou, Z.; Liu, W.K.; Wang, X.; Yin, Z. Excessive homework, inadequate sleep, physical inactivity and screen viewing time are major contributors to high paediatric obesity. Acta Paediatr. 2017, 106, 120–127. [Google Scholar] [CrossRef]
- Zhang, T.; Cai, L.; Ma, L.; Jing, J.; Chen, Y.; Ma, J. The prevalence of obesity and influence of early life and behavioral factors on obesity in Chinese children in Guangzhou. BMC Public Health 2016, 16, 954. [Google Scholar] [CrossRef]
- Xue, H.; Tian, G.; Duan, R.; Quan, L.; Zhao, L.; Yang, M.; Libuda, L.; Muckelbauer, R.; Cheng, G. Sedentary Behavior Is Independently Related to Fat Mass among Children and Adolescents in South China. Nutrients 2016, 8, 667. [Google Scholar] [CrossRef] [PubMed]
- Michaud, I.; Chaput, J.P.; O’Loughlin, J.; Tremblay, A.; Mathieu, M.E. Long duration of stressful homework as a potential obesogenic factor in children: A QUALITY study. Obesity 2015, 23, 815–822. [Google Scholar] [CrossRef]
- Su, Y.; Li, X.; Li, H.; Xu, J.; Xiang, M. Association between Sedentary Behavior during Leisure Time and Excessive Weight in Chinese Children, Adolescents, and Adults. Nutrients 2023, 15, 424. [Google Scholar] [CrossRef]
- Sun, X.; Zhao, B.; Liu, J.; Wang, Y.; Xu, F.; Wang, Y.; Xue, H. A 3-year longitudinal study of the association of physical activity and sedentary behaviours with childhood obesity in China: The childhood obesity study in China mega-cities. Pediatr. Obes. 2021, 16, e12753. [Google Scholar] [CrossRef]
- Dowda, M.; Saunders, R.P.; Dishman, R.K.; Pate, R.R. Association of physical activity, sedentary behavior, diet quality with adiposity: A longitudinal analysis in children categorized by baseline weight status. Int. J. Obes. 2024, 48, 240–246. [Google Scholar] [CrossRef]
- Woo, S.; Yang, H.; Kim, Y.; Lim, H.; Song, H.J.; Park, K.H. Sedentary Time and Fast-Food Consumption Associated With Weight Gain During COVID-19 Lockdown in Children and Adolescents With Overweight or Obesity. J. Korean Med. Sci. 2022, 37, e103. [Google Scholar] [CrossRef]
- Mo, Z.; Wang, H.; Zhang, B.; Ding, G.; Popkin, B.M.; Du, S. The Effects of Physical Activity and Sedentary Behaviors on Overweight and Obesity among Boys may Differ from those among Girls in China: An Open Cohort Study. J. Nutr. 2022, 152, 1274–1282. [Google Scholar] [CrossRef]
- Liu, H.; Bi, C.; Lin, H.; Ma, W.; Zhang, J.; Hu, Y.Y.; Liu, J.Z. Compared with dietary behavior and physical activity risk, sedentary behavior risk is an important factor in overweight and obesity: Evidence from a study of children and adolescents aged 13–18 years in Xinjiang, China. BMC Pediatr. 2022, 22, 582. [Google Scholar] [CrossRef]
- Micklesfield, L.K.; Hanson, S.K.; Lobelo, F.; Cunningham, S.A.; Hartman, T.J.; Norris, S.A.; Stein, A.D. Adolescent physical activity, sedentary behavior and sleep in relation to body composition at age 18 years in urban South Africa, Birth-to-Twenty+ Cohort. BMC Pediatr. 2021, 21, 30. [Google Scholar] [CrossRef]
- Mahumud, R.A.; Sahle, B.W.; Owusu-Addo, E.; Chen, W.; Morton, R.L.; Renzaho, A.M.N. Association of dietary intake, physical activity, and sedentary behaviours with overweight and obesity among 282,213 adolescents in 89 low and middle income to high-income countries. Int. J. Obes. 2021, 45, 2404–2418. [Google Scholar] [CrossRef]
- Heinonen, I. Clinical and physiological advances in sedentary behavior research. Front. Physiol. 2024, 15, 1348122. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Sun, X.; Zhang, E.; Li, H.; Ge, X.; Hu, F.; Cai, Y.; Xiang, M. Association between Types of Screen Time and Weight Status during the COVID-19 Pandemic: A Longitudinal Study in Children and Adolescents. Nutrients 2023, 15, 2055. [Google Scholar] [CrossRef] [PubMed]
- Van Dyck, D.; Barnett, A.; Cerin, E.; Conway, T.L.; Esteban-Cornejo, I.; Hinckson, E.; Rubín, L.; Rush, E.; Baron-Epel, O.; Cain, K.L.; et al. Associations of accelerometer measured school- and non-school based physical activity and sedentary time with body mass index: IPEN Adolescent study. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 85. [Google Scholar] [CrossRef] [PubMed]
- Dolwick, A.P.; Persky, S. Parental reward-based eating drive predicts parents’ feeding behaviors and Children’s ultra-processed food intake. Appetite 2021, 164, 105241. [Google Scholar] [CrossRef]
- Chen, L.; Li, Q.; Song, Y.; Ma, J.; Wang, H.J. Association of physical activities, sedentary behaviors with overweight/obesity in 9-11 year-old Chinese primary school students. Beijing Da Xue Xue Bao Yi Xue Ban 2016, 48, 436–441. [Google Scholar]
- Bredella, M.A. Sex Differences in Body Composition. In Sex and Gender Factors Affecting Metabolic Homeostasis, Diabetes and Obesity; Mauvais-Jarvis, F., Ed.; Springer International Publishing: Cham, Switzerland, 2017; pp. 9–27. [Google Scholar] [CrossRef]
- Dietz, W.H. Critical periods in childhood for the development of obesity. Am. J. Clin. Nutr. 1994, 59, 955–959. [Google Scholar] [CrossRef]
| Overall | Follow-Up Overweight/Obesity Status | p Value | ||
|---|---|---|---|---|
| No | Yes | |||
| Number of participants, N (%) | 47,148 (100.00) | 44,197 (93.74) | 2951 (6.26) | - |
| Age, years, mean (SD) | 12.39 (2.86) | 12.44 (2.84) | 11.62 (2.98) | <0.001 |
| Sex, % | <0.001 | |||
| Men | 49.20 | 48.29 | 62.83 | |
| Women | 50.80 | 51.71 | 37.17 | |
| Ethnicity, % | 0.559 | |||
| Han | 98.17 | 98.18 | 98.03 | |
| Others | 1.83 | 1.82 | 1.97 | |
| Area, % | <0.001 | |||
| Urban | 55.04 | 54.81 | 58.52 | |
| Rural | 44.96 | 45.19 | 41.48 | |
| Economic level, % | 0.475 | |||
| Low | 31.44 | 31.38 | 32.29 | |
| Middle | 31.60 | 31.60 | 31.68 | |
| High | 36.96 | 37.02 | 36.02 | |
| Smoking status, % | 0.411 | |||
| Never | 95.34 | 95.35 | 95.15 | |
| Former | 3.98 | 3.95 | 4.31 | |
| Current | 0.68 | 0.69 | 0.54 | |
| Alcohol use, % | 0.561 | |||
| No | 81.75 | 81.78 | 81.35 | |
| Yes | 18.25 | 18.22 | 18.65 | |
| MVPA frequency, day/week | <0.001 | |||
| 0–1 | 29.35 | 29.57 | 25.95 | |
| 2–3 | 34.31 | 34.29 | 34.53 | |
| 4–5 | 18.20 | 18.18 | 18.49 | |
| 6–7 | 18.15 | 17.95 | 21.03 | |
| Diabetes, % | 0.891 | |||
| No | 99.97 | 99.97 | 99.97 | |
| Yes | 0.03 | 0.03 | 0.03 | |
| Hypertension, % | 0.073 | |||
| No | 99.98 | 99.98 | 99.93 | |
| Yes | 0.02 | 0.02 | 0.07 | |
| Cardiovascular disease, % | 0.592 | |||
| No | 99.90 | 99.90 | 99.93 | |
| Yes | 0.10 | 0.10 | 0.07 | |
| Sleep duration, hour/day, mean (SD) | 8.27 (1.83) | 8.27 (1.82) | 8.36 (1.90) | 0.010 |
| BMI, kg/m2, mean (SD) | 17.28 (2.37) | 17.16 (2.32) | 19.00 (2.48) | <0.001 |
| Participants with Overweight/Obesity, N (%) | Overweight/Obesity, RR (95% CI) | |||
|---|---|---|---|---|
| Crude Model | Model 1 | Model 2 | ||
| Doing homework (x), hour/day | ||||
| 0 ≤ x < 1 | 635 (6.59) | 1.00 | 1.00 | 1.00 |
| 1 ≤ x < 2 | 1198 (6.74) | 1.02 (0.93, 1.12) | 1.10 (1.01, 1.21) * | 1.10 (1.00, 1.21) |
| 2 ≤ x < 3 | 689 (5.73) | 0.87 (0.78, 0.97) ** | 1.04 (0.94, 1.16) | 1.04 (0.93, 1.16) |
| x ≥ 3 | 549 (5.79) | 0.88 (0.79, 0.98) * | 1.14 (1.02, 1.28) * | 1.13 (1.00, 1.27) * |
| Attending tutorial classes (x), hour/week | ||||
| 0 ≤ x < 1 | 1998 (5.90) | 1.00 | 1.00 | 1.00 |
| 1 ≤ x < 2 | 458 (7.15) | 1.21 (1.10, 1.34) *** | 1.08 (0.98, 1.20) | 1.08 (0.97, 1.19) |
| 2 ≤ x < 3 | 303 (6.77) | 1.15 (1.02, 1.29) * | 1.04 (0.92, 1.17) | 1.04 (0.93, 1.18) |
| x ≥ 3 | 351 (7.30) | 1.24 (1.11, 1.38) *** | 1.17 (1.05, 1.31) ** | 1.16 (1.04, 1.31) * |
| Watching TV (x), hour/day | ||||
| 0 | 554 (5.91) | 1.00 | 1.00 | 1.00 |
| 0 < x < 1 | 1332 (6.37) | 1.08 (0.98, 1.19) | 1.01 (0.92, 1.11) | 0.99 (0.89, 1.09) |
| 1 ≤ x < 2 | 771 (6.21) | 1.05 (0.94, 1.17) | 0.99 (0.89, 1.10) | 0.93 (0.83, 1.05) |
| x ≥ 2 | 567 (6.48) | 1.10 (0.98, 1.23) | 1.04 (0.93, 1.17) | 0.97 (0.85, 1.10) |
| Computer use (x), hour/day | ||||
| 0 | 1466 (6.09) | 1.00 | 1.00 | 1.00 |
| 0 < x < 1 | 1034 (6.28) | 1.03 (0.96, 1.11) | 1.05 (0.97, 1.13) | 1.03 (0.95, 1.12) |
| 1 ≤ x < 2 | 408 (6.69) | 1.10 (0.99, 1.22) | 1.11 (1.00, 1.24) | 1.04 (0.92, 1.17) |
| x ≥ 2 | 317 (6.57) | 1.08 (0.96, 1.21) | 1.06 (0.94, 1.20) | 0.99 (0.87, 1.13) |
| Mobile electronic device use (x), hour/day | ||||
| 0 | 767 (6.36) | 1.00 | 1.00 | 1.00 |
| 0 < x < 1 | 685 (6.35) | 1.00 (0.90, 1.10) | 1.02 (0.92, 1.13) | 1.00 (0.90, 1.11) |
| 1 ≤ x < 2 | 856 (6.47) | 1.02 (0.93, 1.12) | 1.09 (0.99, 1.20) | 1.08 (0.97, 1.20) |
| x ≥ 2 | 908 (5.96) | 0.94 (0.85, 1.03) | 1.20 (1.08, 1.33) *** | 1.20 (1.07, 1.34) ** |
| Screen-related sedentary time, hour/day | ||||
| Per hour increment | 3197 (6.25) | 1.00 (0.99, 1.01) | 1.01 (1.00, 1.03) * | 1.01 (1.00, 1.02) * |
| Academic study-related sedentary time, hour/day | ||||
| Per hour increment | 2979 (6.27) | 1.02 (0.99, 1.04) | 1.03 (1.01, 1.06) ** | 1.03 (1.01, 1.06) ** |
| Total sedentary time, hour/day | ||||
| Per hour increment | 2951 (6.26) | 0.99 (0.98, 1.01) | 1.02 (1.01, 1.03) ** | 1.02 (1.01, 1.03) ** |
| SSB consumption (x), time/day | ||||
| 0 | 571 (6.18) | 1.00 | 1.00 | 1.00 |
| 0 < x < 1 | 2351 (6.23) | 1.01 (0.92, 1.10) | 1.09 (0.93, 1.29) | 1.10 (0.93, 1.30) |
| x ≥ 1 | 300 (6.70) | 1.08 (0.95, 1.24) | 1.23 (0.98, 1.53) | 1.11 (0.88, 1.41) |
| Number of Participants, N (%) | BMI, kg/m2, β (95% CI) | |||
|---|---|---|---|---|
| Crude Model | Model 1 | Model 2 | ||
| Doing homework (x), hour/day | ||||
| 0 ≤ x < 1 | 11,765 (19.60) | 0.00 | 0.00 | 0.00 |
| 1 ≤ x < 2 | 21,902 (36.48) | 0.44 (0.36, 0.52) *** | 0.20 (0.12, 0.27) *** | 0.17 (0.09, 0.25) *** |
| 2 ≤ x < 3 | 14,829 (24.70) | 0.98 (0.89, 1.07) *** | 0.35 (0.27, 0.44) *** | 0.29 (0.20, 0.38) *** |
| x ≥ 3 | 11,539 (19.22) | 1.28 (1.19, 1.38) *** | 0.35 (0.25, 0.44) *** | 0.27 (0.18, 0.37) *** |
| Attending tutorial classes (x), hour/week | ||||
| 0 ≤ x < 1 | 40,924 (67.31) | 0.00 | 0.00 | 0.00 |
| 1 ≤ x < 2 | 7988 (13.14) | −0.24 (−0.33, −0.15) *** | 0.12 (0.03, 0.20) ** | 0.11 (0.03, 0.20) * |
| 2 ≤ x < 3 | 5693 (9.36) | 0.01 (−0.09, 0.11) | 0.24 (0.14, 0.33) *** | 0.19 (0.09, 0.29) *** |
| x ≥ 3 | 6194 (10.19) | 0.50 (0.40, 0.60) *** | 0.43 (0.34, 0.53) *** | 0.39 (0.29, 0.49) *** |
| Watching TV (x), hour/day | ||||
| 0 | 11,432 (18.12) | 0.00 | 0.00 | 0.00 |
| 0 < x < 1 | 25,281 (40.07) | −0.46 (−0.54, −0.38) *** | −0.07 (−0.15, 0.01) | −0.12 (−0.20, −0.03) ** |
| 1 ≤ x < 2 | 15,383 (24.38) | −0.15 (−0.24, −0.06) ** | 0.06 (−0.03, 0.14) | −0.03 (−0.12, 0.06) |
| x ≥ 2 | 11,000 (17.43) | 0.12 (0.02, 0.21) * | 0.18 (0.08, 0.27) *** | 0.06 (−0.05, 0.16) |
| Computer use (x), hour/day | ||||
| 0 | 29,311 (46.45) | 0.00 | 0.00 | 0.00 |
| 0 < x < 1 | 20,059 (31.79) | 0.25 (0.19, 0.32) *** | 0.02 (−0.04, 0.08) | 0.01 (−0.05, 0.08) |
| 1 ≤ x < 2 | 7614 (12.07) | 0.66 (0.56, 0.75) *** | 0.17 (0.08, 0.26) *** | 0.10 (0.00, 0.19) * |
| x ≥ 2 | 6118 (9.70) | 0.71 (0.61, 0.81) *** | 0.20 (0.10, 0.30) *** | 0.09 (−0.02, 0.20) |
| Mobile electronic device use (x), hour/day | ||||
| 0 | 14,672 (23.32) | 0.00 | 0.00 | 0.00 |
| 0 < x < 1 | 13,279 (21.10) | 0.29 (0.21, 0.38) *** | 0.10 (0.02, 0.19) * | 0.08 (−0.01, 0.17) |
| 1 ≤ x < 2 | 16,317 (25.93) | 0.56 (0.47, 0.64) *** | 0.18 (0.10, 0.26) *** | 0.14 (0.05, 0.23) ** |
| x ≥ 2 | 18,653 (29.65) | 1.35 (1.27, 1.42) *** | 0.23 (0.15, 0.31) *** | 0.14 (0.05, 0.23) ** |
| Screen-related sedentary time, hour/day | ||||
| Per hour increment | 62,702 (100.00) | 0.13 (0.12, 0.14) *** | 0.03 (0.02, 0.04) *** | 0.02 (0.01, 0.03) *** |
| Academic study-related sedentary time, hour/day | ||||
| Per hour increment | 58,318 (100.00) | 0.22 (0.20, 0.24) *** | 0.12 (0.10, 0.14) *** | 0.11 (0.10, 0.13) *** |
| Total sedentary time, hour/day | ||||
| Per hour increment | 57,885 (100.00) | 0.17 (0.16, 0.18) *** | 0.04 (0.03, 0.05) *** | 0.04 (0.03, 0.05) *** |
| SSB consumption (x), time/day | ||||
| 0 | 11,155 (17.68) | 0.00 | 0.00 | 0.00 |
| 0 < x < 1 | 46,288 (73.36) | 0.76 (0.69, 0.84) *** | 0.30 (0.17, 0.42) *** | 0.26 (0.13, 0.39) *** |
| x ≥ 1 | 5652 (8.96) | 1.27 (1.15, 1.38) *** | 0.58 (0.41, 0.76) *** | 0.51 (0.32, 0.69) *** |
| Sex | p for Interaction | Age | p for Interaction | |||
|---|---|---|---|---|---|---|
| Men | Women | <12 Years | 12+ Years | |||
| Overweight/obesity status, RR (95% CI) a | ||||||
| Screen-related sedentary time, hour/day | 0.063 | 0.004 | ||||
| Per hour increment | 1.01 (0.99, 1.02) | 1.03 (1.01, 1.05) ** | 1.03 (1.01, 1.05) *** | 0.99 (0.98, 1.01) | ||
| Academic study-related sedentary time, hour/day | 0.341 | <0.001 | ||||
| Per hour increment | 1.03 (1.00, 1.06) | 1.05 (1.01, 1.09) * | 0.99 (0.96, 1.02) | 1.09 (1.05, 1.13) *** | ||
| Total sedentary time, hour/day | 0.085 | 0.030 | ||||
| Per hour increment | 1.01 (1.00, 1.03) | 1.03 (1.01, 1.05) ** | 1.03 (1.01, 1.05) ** | 1.00 (0.98, 1.02) | ||
| SSB consumption (x), time/day | 0.351 | 0.516 | ||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | ||
| 0 < x < 1 | 1.10 (0.90, 1.36) | 1.07 (0.82, 1.39) | 0.92 (0.73, 1.15) | 1.28 (1.01, 1.62) * | ||
| x ≥ 1 | 1.10 (0.84, 1.45) | 1.48 (1.02, 2.13) * | 0.99 (0.69, 1.41) | 1.46 (1.09, 1.96) * | ||
| BMI, kg/m2, β (95% CI) b | ||||||
| Screen-related sedentary time, hour/day | 0.042 | <0.001 | ||||
| Per hour increment | 0.02 (0.01, 0.03) ** | 0.04 (0.02, 0.05) *** | 0.08 (0.07, 0.10) *** | 0.02 (0.01, 0.03) ** | ||
| Academic study-related sedentary time, hour/day | 0.199 | 0.009 | ||||
| Per hour increment | 0.12 (0.09, 0.15) *** | 0.11 (0.08, 0.13) *** | 0.08 (0.05, 0.11) *** | 0.12 (0.10, 0.15) *** | ||
| Total sedentary time, hour/day | 0.087 | <0.001 | ||||
| Per hour increment | 0.03 (0.02, 0.05) *** | 0.05 (0.04, 0.06) *** | 0.09 (0.08, 0.11) *** | 0.03 (0.02, 0.04) *** | ||
| SSB consumption (x), time/day | 0.651 | 0.808 | ||||
| 0 | 0.00 | 0.00 | 0.00 | 0.00 | ||
| 0 < x < 1 | 0.36 (0.17, 0.55) *** | 0.22 (0.07, 0.38) ** | 0.26 (0.06, 0.45) * | 0.28 (0.12, 0.44) ** | ||
| x ≥ 1 | 0.66 (0.41, 0.92) *** | 0.49 (0.26, 0.72) *** | 0.39 (0.07, 0.72) * | 0.63 (0.42, 0.85) *** | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, T.; Li, M.; Zhang, R.; Li, R.; Shen, S.; Chen, Q.; Liu, R.; Wang, J.; Qu, Y.; Xu, L. Associations of Academic Study- and Non-Study-Related Sedentary Behaviors with Incident Obesity in Children and Adolescents. Nutrients 2025, 17, 1633. https://doi.org/10.3390/nu17101633
Lu T, Li M, Zhang R, Li R, Shen S, Chen Q, Liu R, Wang J, Qu Y, Xu L. Associations of Academic Study- and Non-Study-Related Sedentary Behaviors with Incident Obesity in Children and Adolescents. Nutrients. 2025; 17(10):1633. https://doi.org/10.3390/nu17101633
Chicago/Turabian StyleLu, Tingyu, Meng Li, Ruihang Zhang, Ruiqiang Li, Shaojun Shen, Qiuxia Chen, Rong Liu, Jiao Wang, Yabin Qu, and Lin Xu. 2025. "Associations of Academic Study- and Non-Study-Related Sedentary Behaviors with Incident Obesity in Children and Adolescents" Nutrients 17, no. 10: 1633. https://doi.org/10.3390/nu17101633
APA StyleLu, T., Li, M., Zhang, R., Li, R., Shen, S., Chen, Q., Liu, R., Wang, J., Qu, Y., & Xu, L. (2025). Associations of Academic Study- and Non-Study-Related Sedentary Behaviors with Incident Obesity in Children and Adolescents. Nutrients, 17(10), 1633. https://doi.org/10.3390/nu17101633







