Socioeconomic Patterning of Stunting and Overweight Among Iranian Children Aged 2–5 Years: A National Cross-Sectional Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Outcome
2.3. Explanatory Variables
2.4. Mediation Variable
2.5. Statistical Analysis
3. Results
3.1. Sample Description and Univariate Statistics
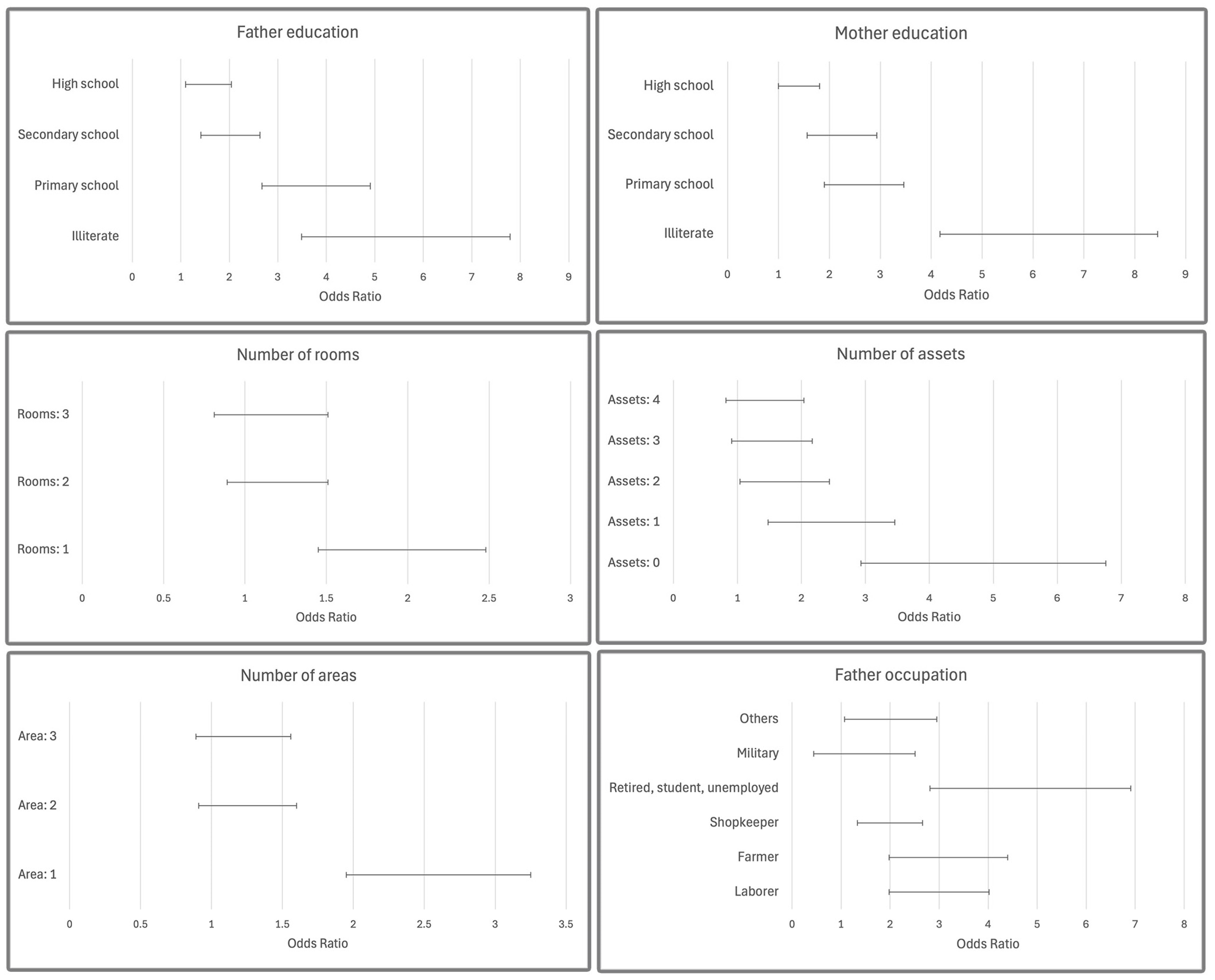
3.2. Multivariate Regression
3.3. Mediation Analysis
4. Discussion
4.1. Stunting
4.1.1. Parental Education
4.1.2. Parental Occupation
4.1.3. Housing and Assets
4.1.4. Diet Quality
4.2. Overweight
4.3. Limitations and Strengths of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DHS | Demography and Health Survey |
| MICS | Multiple Indicator Cluster Survey |
| SES | Socioeconomic status |
| WHO | World Health Organization |
| CDC | Centers for Disease Control and Prevention |
| HAZ | Height-for-age Z-score |
| WHZ | Weight-for-height Z-score |
| DDS | Dietary diversity score |
References
- Bi, J.; Liu, C.; Li, S.; He, Z.; Chen, K.; Luo, R.; Wang, Z.; Yu, Y.; Xu, H. Dietary diversity among preschoolers: A cross-sectional study in poor, rural, and ethnic minority areas of central south china. Nutrients 2019, 11, 558. [Google Scholar] [CrossRef] [PubMed]
- Rambe, N.L.; Hutabarat, E.N.; Hafifah, R. The Effect of Stunting on Children’s Cognitive Development: Systematic Review. Contag. Sci. Period. J. Public Health Coast. Health 2023, 5, 360–372. [Google Scholar] [CrossRef]
- Fajar, N.A.; Zulkarnain, M.; Taqwa, R.; Sulaningsi, K.; Ananingsih, E.S.; Rachmayanti, R.D.; Sin, S.C. Family roles and support in preventing stunting: A systematic review. J. Promosi Kesehat. Indones. 2023, 19, 50–57. [Google Scholar] [CrossRef]
- Soliman, A.; De Sanctis, V.; Alaaraj, N.; Ahmed, S.; Alyafei, F.; Hamed, N.; Soliman, N. Early and long-term consequences of nutritional stunting: From childhood to adulthood. Acta Bio Medica Atenei Parm. 2021, 92, e2021168. [Google Scholar]
- World Health Organization. The State of Food Security and Nutrition in the World 2022: Repurposing Food and Agricultural Policies to Make Healthy Diets More Affordable; Food & Agriculture Organization: Rome, Italy, 2022; Volume 2022. [Google Scholar]
- Khateri, S.; Moradi, Y.; Khazaei, Z.; Mirzaei, H.; Hanis, S.M.; Aliabadi, M.A.; Ranjbaran, M.; Varse, F.; Parang, S. Prevalence of obesity and overweight in Iranian children aged less than 5 years: A systematic review and meta-analysis. Korean J. Pediatr. 2019, 62, 206. [Google Scholar]
- Kia, A.A.; Rezapour, A.; Khosravi, A.; Abarghouei, V.A. Socioeconomic inequality in malnutrition in under-5 children in Iran: Evidence from the multiple indicator demographic and health survey, 2010. J. Prev. Med. Public Health 2017, 50, 201. [Google Scholar]
- Mansori, K.; Shadmani, F.K.; Mirzaei, H.; Azad, R.V.; Khateri, S.; Hanis, S.M.; Moradi, Y. Prevalence of stunting in Iranian children under five years of age: Systematic review and meta-analysis. Med. J. Islam. Repub. Iran 2018, 32, 103. [Google Scholar] [CrossRef]
- Belardinelli, P.; Torbica, A.; Fattore, G. Longitudinal associations between different measures of socioeconomic status and health behavior among adolescents. Data from a wealthy Italian region. Prev. Med. 2022, 160, 107092. [Google Scholar] [CrossRef]
- Karney, B.R. Socioeconomic status and intimate relationships. Annu. Rev. Psychol. 2021, 72, 391–414. [Google Scholar] [CrossRef]
- Akombi, B.J.; Agho, K.E.; Renzaho, A.M.; Hall, J.J.; Merom, D.R. Trends in socioeconomic inequalities in child undernutrition: Evidence from Nigeria Demographic and Health Survey (2003–2013). PLoS ONE 2019, 14, e0211883. [Google Scholar] [CrossRef]
- Rah, J.H.; Akhter, N.; Semba, R.D.; De Pee, S.; Bloem, M.W.; Campbell, A.A.; Moench-Pfanner, R.; Sun, K.; Badham, J.; Kraemer, K. Low dietary diversity is a predictor of child stunting in rural Bangladesh. Eur. J. Clin. Nutr. 2010, 64, 1393–1398. [Google Scholar] [CrossRef] [PubMed]
- Sk, R.; Banerjee, A.; Rana, M.J. Nutritional status and concomitant factors of stunting among pre-school children in Malda, India: A micro-level study using a multilevel approach. BMC Public Health 2021, 21, 1690. [Google Scholar] [CrossRef] [PubMed]
- Kien, V.D.; Lee, H.-Y.; Nam, Y.-S.; Oh, J.; Giang, K.B.; Minh, H.V. Trends in socioeconomic inequalities in child malnutrition in Vietnam: Findings from the Multiple Indicator Cluster Surveys, 2000–2011. Glob. Health Action 2016, 9, 29263. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi, M.B.H.; Abdollahi, Z.; Salehi Mazandarani, F.; Houshiarrad, A. Children Anthropomerty, Nutrition and Development Survey 2017, CANDS_IR96; Ministry of Health: Ghom, Iran, 2021. [Google Scholar]
- Rutstein, S.O.; Rojas, G. Guide to DHS Statistics; ORC Macro: Calverton, MD, USA, 2006; Volume 38, p. 78. [Google Scholar]
- Khan, S.; Hancioglu, A. Multiple indicator cluster surveys: Delivering robust data on children and women across the globe. Stud. Fam. Plan. 2019, 50, 279–286. [Google Scholar] [CrossRef]
- Akram, R.; Sultana, M.; Ali, N.; Sheikh, N.; Sarker, A.R. Prevalence and determinants of stunting among preschool children and its urban–rural disparities in Bangladesh. Food Nutr. Bull. 2018, 39, 521–535. [Google Scholar] [CrossRef]
- Vilcins, D.; Sly, P.D.; Jagals, P. Environmental risk factors associated with child stunting: A systematic review of the literature. Ann. Glob. Health 2018, 84, 551. [Google Scholar] [CrossRef]
- Hidayati, A.A.; Gunawan, I.M.A.; Paramashanti, B.A. Stunting was not associated with overweight among children aged 24–59 months. J. Gizi Dan Diet. Indones. (Indones. J. Nutr. Diet.) 2018, 5, 113–118. [Google Scholar] [CrossRef]
- Mahfouz, E.M.; Mohammed, E.S.; Alkilany, S.F.; Rahman, T.A.A. The relationship between dietary intake and stunting among pre-school children in Upper Egypt. Public Health Nutr. 2022, 25, 2179–2187. [Google Scholar] [CrossRef]
- Ali, P.Z.; Sayed, T.M.; Qureshi, M.A.; Tahir, H.; Shaikh, G.; Imran, M. Epidemiological Study on Overweight and Obesity among Adolescent Boys and Girls. Pak. J. Med. Health Sci. 2021, 15, 3430–3433. [Google Scholar]
- Chowdhury, T.R.; Chakrabarty, S.; Rakib, M.; Afrin, S.; Saltmarsh, S.; Winn, S. Factors associated with stunting and wasting in children under 2 years in Bangladesh. Heliyon 2020, 6, e04849. [Google Scholar] [CrossRef]
- Pham, B.N.; Silas, V.D.; Okely, A.D.; Pomat, W. Measuring wasting and stunting prevalence among children under 5 years of age and associated risk factors in Papua New Guinea: New evidence from the Comprehensive Health and Epidemiological Surveillance System. Front. Nutr. 2021, 8, 622660. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.B.; Tahsina, T.; Hoque, D.M.E.; Hasan, M.M.; Iqbal, A.; Huda, T.M.; El Arifeen, S. Association of food security and other socio-economic factors with dietary diversity and nutritional statuses of children aged 6–59 months in rural Bangladesh. PLoS ONE 2019, 14, e0221929. [Google Scholar] [CrossRef] [PubMed]
- Musheiguza, E.; Mahande, M.J.; Malamala, E.; Msuya, S.E.; Charles, F.; Philemon, R.; Mgongo, M. Inequalities in stunting among under-five children in Tanzania: Decomposing the concentration indexes using demographic health surveys from 2004/5 to 2015/6. Int. J. Equity Health 2021, 20, 46. [Google Scholar] [CrossRef] [PubMed]
- Ezeh, O.K.; Abir, T.; Zainol, N.R.; Al Mamun, A.; Milton, A.H.; Haque, M.R.; Agho, K.E. Trends of stunting prevalence and its associated factors among nigerian children aged 0–59 months residing in the northern nigeria, 2008–2018. Nutrients 2021, 13, 4312. [Google Scholar] [CrossRef]
- Alissa, E.M.; Algarni, S.A.; Khaffji, A.J.; Al Mansouri, N.M. Association of diet diversity score with visceral adiposity in women with polycystic ovarian syndrome. Hum. Nutr. Metab. 2021, 23, 200116. [Google Scholar] [CrossRef]
- Habte, T.-Y.; Krawinkel, M. Dietary diversity score: A measure of nutritional adequacy or an indicator of healthy diet? J. Nutr. Health Sci. 2016, 3, 1–9. [Google Scholar]
- Chowdhury, T.R.; Chakrabarty, S.; Rakib, M.; Winn, S.; Bennie, J. Risk factors for child stunting in Bangladesh: An analysis using MICS 2019 data. Arch. Public Health 2022, 80, 126. [Google Scholar] [CrossRef]
- Rehan, A.; Kishore, S.; Singh, M.; Jain, B.; Reddy, N.K.K.; Kumar, D.; Usha, P.; Parveen, R. A study to assess undernutrition and its sociodemographic correlates in under-five children in urban and rural areas of Rishikesh, Uttarakhand. J. Fam. Med. Prim. Care 2020, 9, 4980. [Google Scholar]
- Mutiarasari, D.; Miranti, M.; Fitriana, Y.; Pakaya, D.; Sari, P.; Bohari, B.; Sabir, M.; Wahyuni, R.D.; Ryzqa, R.; Hadju, V. A determinant analysis of stunting prevalence on under 5-year-old children to establish stunting management policy. Open Access Maced. J. Med. Sci. 2021, 9, 79–84. [Google Scholar] [CrossRef]
- Widyaningsih, V.; Mulyaningsih, T.; Nur Rahmawati, F.; Adhitya, D. Determinants of socioeconomic and rural-urban disparities in stunting: Evidence from Indonesia. Rural Remote Health 2022, 22, 1–10. [Google Scholar] [CrossRef]
- Keino, S.; Plasqui, G.; Ettyang, G.; van den Borne, B. Determinants of stunting and overweight among young children and adolescents in sub-Saharan Africa. Food Nutr. Bull. 2014, 35, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Yefri, R.; Lipoeto, N.I.; Putra, A.E.; Kadim, M. Parental Sociodemographic Factors Associated with Stunted Children below 5 Years of Age in Kampar Indonesia. Open Access Maced. J. Med. Sci. 2022, 10, 1889–1893. [Google Scholar] [CrossRef]
- Nshimyiryo, A.; Hedt-Gauthier, B.; Mutaganzwa, C.; Kirk, C.M.; Beck, K.; Ndayisaba, A.; Mubiligi, J.; Kateera, F.; El-Khatib, Z. Risk factors for stunting among children under five years: A cross-sectional population-based study in Rwanda using the 2015 Demographic and Health Survey. BMC Public Health 2019, 19, 175. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, S.H.; Muhammad, F.; Pakzad, R.; Alizadeh, S. Socioeconomic inequality in stunting among under-5 children in Ethiopia: A decomposition analysis. BMC Res. Notes 2019, 12, 184. [Google Scholar] [CrossRef]
- Khan, S.; Zaheer, S.; Safdar, N.F. Determinants of stunting, underweight and wasting among children< 5 years of age: Evidence from 2012-2013 Pakistan demographic and health survey. BMC Public Health 2019, 19, 358. [Google Scholar]
- Fantay Gebru, K.; Mekonnen Haileselassie, W.; Haftom Temesgen, A.; Oumer Seid, A.; Afework Mulugeta, B. Determinants of stunting among under-five children in Ethiopia: A multilevel mixed-effects analysis of 2016 Ethiopian demographic and health survey data. BMC Pediatr. 2019, 19, 176. [Google Scholar] [CrossRef]
- Bustami, B.; Ampera, M. The identification of modeling causes of stunting children aged 2–5 years in Aceh province, Indonesia (Data analysis of nutritional status monitoring 2015). Open Access Maced. J. Med. Sci. 2020, 8, 657–663. [Google Scholar] [CrossRef]
- Zamanimoghadam, M. Empowerment of female heads of households in Iran: A systematic review. Soc. Welf. Q. 2021, 21, 45–80. [Google Scholar]
- Gassara, G.; Lin, Q.; Deng, J.; Zhang, Y.; Wei, J.; Chen, J. Dietary Diversity, Household Food Insecurity and Stunting among Children Aged 12 to 59 Months in N’Djamena—Chad. Nutrients 2023, 15, 573. [Google Scholar] [CrossRef]
- Chowdhury, M.R.K.; Khan, H.T.; Rashid, M.; Kabir, R.; Islam, S.; Islam, M.S.; Kader, M. Differences in risk factors associated with single and multiple concurrent forms of undernutrition (stunting, wasting or underweight) among children under 5 in Bangladesh: A nationally representative cross-sectional study. BMJ Open 2021, 11, e052814. [Google Scholar] [CrossRef]
- Suratri, M.A.L.; Putro, G.; Rachmat, B.; Nurhayati; Ristrini; Pracoyo, N.E.; Yulianto, A.; Suryatma, A.; Samsudin, M.; Raharni. Risk Factors for Stunting among Children under Five Years in the Province of East Nusa Tenggara (NTT), Indonesia. Int. J. Environ. Res. Public Health 2023, 20, 1640. [Google Scholar] [CrossRef] [PubMed]
- Nahar, M.Z.; Zahangir, M.S. The role of parental education and occupation on undernutrition among children under five in Bangladesh: A rural-urban comparison. PLoS ONE 2024, 19, e0307257. [Google Scholar] [CrossRef] [PubMed]
- Gaidhane, A.; Dhakate, P.; Patil, M.; Zahiruddin, Q.S.; Khatib, N.; Gaidhane, S.; Choudhary, S. Determinants of stunting and wasting among the children under five years of age in rural India. Int. J. Curr. Res. Rev. 2021, 13, 18–26. [Google Scholar] [CrossRef]
- Mansur, M.; Afiaz, A.; Hossain, M.S. Sociodemographic risk factors of under-five stunting in Bangladesh: Assessing the role of interactions using a machine learning method. PLoS ONE 2021, 16, e0256729. [Google Scholar] [CrossRef]
- Ding, X.; Li, J.; Zhao, L.y.; Yang, Z.y.; Zhao, W. Long maternal working hours were linked to obesity, underweight and stunting in children under age 5 in China. Int. J. Soc. Welf. 2023, 32, 320–333. [Google Scholar] [CrossRef]
- Permatasari, T.A.E.; Chairunnisa, C.; Djarir, H.; Herlina, L.; Fauziah, M.; Andriyani, A.; Chadirin, Y. The Determinants of Stunting in the Under-five in Three Municipalities in the Special Capital Region of Jakarta. Kesmas J. Kesehat. Masy. Nas. (Natl. Public Health J.) 2023, 18, 32–40. [Google Scholar] [CrossRef]
- Asuman, D.; Ackah, C.G.; Fenny, A.P.; Agyire-Tettey, F. Assessing socioeconomic inequalities in the reduction of child stunting in sub-Saharan Africa. J. Public Health 2020, 28, 563–573. [Google Scholar] [CrossRef]
- Curi-Quinto, K.; Ortiz-Panozo, E.; De Romaña, D.L. Malnutrition in all its forms and socio-economic disparities in children under 5 years of age and women of reproductive age in Peru. Public Health Nutr. 2020, 23 (Suppl. S1), s89–s100. [Google Scholar] [CrossRef]
- Ernawati, F.; Syauqy, A.; Arifin, A.Y.; Soekatri, M.Y.; Sandjaja, S. Micronutrient deficiencies and stunting were associated with socioeconomic status in Indonesian children aged 6–59 months. Nutrients 2021, 13, 1802. [Google Scholar] [CrossRef]
- Syihab, S.F.; Stephani, M.R.; Kumalasari, I.; Suherman, A. Socioeconomic Status in Relation to Stunting and Motor Skill Development of Toddlers in Urban and Rural Areas. J. KEMAS 2021, 16, 340–347. [Google Scholar] [CrossRef]
- Azupogo, F.; Chapirah, J.; Halidu, R. The association between dietary diversity and anthropometric indices of children aged 24-59 months: A cross-sectional study in northern Ghana. Afr. J. Food Agric. Nutr. Dev. 2022, 22, 20829–20848. [Google Scholar] [CrossRef]
- Hein, A.K.; Hong, S.A.; Puckpinyo, A.; Tejativaddhana, P. Dietary diversity, social support and stunting among children aged 6–59 months in an internally displaced persons camp in Kayin state, Myanmar. Clin. Nutr. Res. 2019, 8, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Gassara, G.; Chen, J. Household food insecurity, dietary diversity, and stunting in sub-saharan africa: A systematic review. Nutrients 2021, 13, 4401. [Google Scholar] [CrossRef] [PubMed]
- Jelenkovic, A.; Sund, R.; Hur, Y.-M.; Yokoyama, Y.; Hjelmborg, J.v.B.; Möller, S.; Honda, C.; Magnusson, P.K.; Pedersen, N.L.; Ooki, S. Genetic and environmental influences on height from infancy to early adulthood: An individual-based pooled analysis of 45 twin cohorts. Sci. Rep. 2016, 6, 28496. [Google Scholar] [CrossRef]
- Ismawati, R.; Soeyonoa, R.D.; Romadhoni, I.F.; Dwijayanti, I. Nutrition intake and causative factor of stunting among children aged under-5 years in Lamongan city. Enferm. Clin. 2020, 30, 71–74. [Google Scholar] [CrossRef]
- Hossain, F.B.; Shawon, M.S.R.; Al-Abid, M.S.U.; Mahmood, S.; Adhikary, G.; Bulbul, M.M.I. Double burden of malnutrition in children aged 24 to 59 months by socioeconomic status in five South Asian countries: Evidence from demographic and health surveys. BMJ Open 2020, 10, e032866. [Google Scholar] [CrossRef]
- Ekholuenetale, M.; Tudeme, G.; Onikan, A.; Ekholuenetale, C.E. Socioeconomic inequalities in hidden hunger, undernutrition, and overweight among under-five children in 35 sub-Saharan Africa countries. J. Egypt. Public Health Assoc. 2020, 95, 9. [Google Scholar] [CrossRef]
- Diallo, R.; Baguiya, A.; Balde, M.D.; Camara, S.; Diallo, A.; Camara, B.S.; Toure, A.O.; Soumah, A.M.; Kouanda, S.; Compaore, E. Prevalence and factors associated with overweight in children under 5 years in West African countries. J. Public Health Res. 2023, 12, 22799036231181845. [Google Scholar] [CrossRef]
- Wang, Y.; Lim, H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int. Rev. Psychiatry 2012, 24, 176–188. [Google Scholar] [CrossRef]
- Dogui, D.; Doggui, R.; El Ati, J.; El Ati-Hellal, M. Association between overweight and diet diversity score: A cross-sectional study conducted among tunisian children. Children 2021, 8, 536. [Google Scholar] [CrossRef]
- Lioret, S.; Touvier, M.; Dubuisson, C.; Dufour, A.; Calamassi-Tran, G.; Lafay, L.; Volatier, J.L.; Maire, B. Trends in child overweight rates and energy intake in France from 1999 to 2007: Relationships with socioeconomic status. Obesity 2009, 17, 1092–1100. [Google Scholar] [CrossRef] [PubMed]
- Larson, R.B. Controlling social desirability bias. Int. J. Mark. Res. 2019, 61, 534–547. [Google Scholar] [CrossRef]
- Nouri Saeidlou, S.; Babaei, F.; Ayremlou, P. Malnutrition, overweight, and obesity among urban and rural children in north of west Azerbijan, Iran. J. Obes. 2014, 2014, 541213. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef] [PubMed]
| Age (Month) | 24–35 | 36–47 | 48–59 | Total | |
|---|---|---|---|---|---|
| Sex n (%) | Female | 1970 (49.2) | 1773 (48.1) | 1732 (50.0) | 5475 (49.1) |
| Male | 2033 (50.7) | 1909 (51.8) | 1730 (49.9) | 5672 (50.9) |
| Stunting (HAZ) < −2 | |||||
|---|---|---|---|---|---|
| Characteristics | Total n (%) | Stunting n (%) | Adjusted OR without Diet Quality (95% CI) | Adjusted OR with Diet Quality (95% CI) | |
| Education (father) | Illiterate | 387 (3.4) | 47 (12.2) | 1.70 * (1.01–2.88) | 1.69 (0.99–2.86) |
| Primary school | 1976 (17.7) | 174 (8.8) | 1.73 * (1.14–2.64) | 1.72 * (1.13–2.62) | |
| Secondary school | 2885 (25.9) | 142 (4.9) | 1.16 (0.77–1.74) | 1.16 (0.77–1.74) | |
| High school | 3690 (33.1) | 144 (3.9) | 1.09 (0.75–1.59) | 1.08 (0.74–1.58) | |
| Higher education | 2190 (19.6) | 58 (2.7) | Ref | Ref | |
| Education (mother) | Illiterate | 511 (4.6) | 74 (14.4) | 2.07 * (1.30–3.29) | 2.07 * (1.30–3.30) |
| Primary school | 2326 (21.0) | 158 (6.8) | 1.21 (0.82–1.79) | 1.21 (0.82–1.79) | |
| Secondary school | 2049 (18.5) | 119 (5.8) | 1.32 (0.90–1.93) | 1.32 (0.91–1.93) | |
| High school | 3974 (35.9) | 149 (3.8) | 1.02 (0.72–1.43) | 1.02 (0.72–1.43) | |
| Higher education | 2180 (19.7) | 62 (2.8) | Ref | Ref | |
| Occupation (father) | Employee | 1572 (14.2) | 38 (2.4) | Ref | Ref |
| Laborer | 2604 (23.5) | 171 (6.6) | 1.42 (0.92–2.21) | 1.22 (0.79–1.87) | |
| Farmer | 1016 (9.1) | 70 (6.9) | 1.35 (0.83–2.20) | 1.16 (0.72–1.87) | |
| Shopkeeper | 4535 (41.0) | 205 (4.5) | 1.36 (0.90–2.06) | 1.17 (0.76–1.78) | |
| Retired, student, or unemployed | 423 (3.8) | 41 (9.6) | 1.69 (1.00–2.87) | 1.26 (0.42–3.78) | |
| Military | 232 (2.1) | 6 (2.6) | 1.10 (0.46–2.66) | 0.94 (0.37–2.37) | |
| Others | 664 (6.0) | 30 (4.5) | 1.17 (0.67–2.03) | 0.85 (0.49–1.48) | |
| Occupation (mother) | Working 1 | 952 (8.5) | 34 (3.5) | Ref | Ref |
| Nonworking | 10,168 (91.4) | 528 (5.1) | 0.98 (0.69–1.39) | 1.03 (0.72–1.45) | |
| Rooms/family size (quartiles) | 1 | 2489 (22.5) | 179 (7.2) | 1.06 (0.79–1.43) | 1.06 (0.78–1.43) |
| 2 | 4508 (40.9) | 204 (4.5) | 0.93 (0.71–1.23) | 0.93 (0.71–1.23) | |
| 3 | 1967 (17.8) | 86 (4.4) | 1.07 (0.78–1.47) | 1.06 (0.77–1.45) | |
| 4 | 2054 (18.6) | 81 (4.0) | Ref | Ref | |
| Areas/family size (quartiles) | 1 | 2742 (24.6) | 231 (8.4) | 1.51 * (1.12–2.04) | 1.50 * (1.11–2.03) |
| 2 | 2868 (25.7) | 120 (4.2) | 0.91 (0.66–1.25) | 0.90 (0.66–1.24) | |
| 3 | 3134 (28.1) | 129 (4.1) | 1.08 (0.80–1.45) | 1.08 (0.80–1.45) | |
| 4 | 2382 (21.4) | 84 (3.5) | Ref | Ref | |
| Assets (score = sum of assets) | 0 | 1393 (12.4) | 156 (11.2) | 2.06 * (1.27–3.35) | 2.01 * (1.23–3.27) |
| 1 | 1939 (17.3) | 117 (6.0) | 1.35 (0.84–2.17) | 1.33 (0.83–2.15) | |
| 2 | 2479 (22.2) | 105 (4.2) | 1.14 (0.72–1.83) | 1.13 (0.71–1.81) | |
| 3 | 2294 (20.5) | 86 (3.7) | 1.14 (0.71–1.82) | 1.13 (0.71–1.80) | |
| 4 | 1818 (16.3) | 70 (3.8) | 1.24 (0.77–2.00) | 1.23 (0.77–1.98) | |
| 5 | 983 (8.8) | 24 (2.4) | Ref | Ref | |
| Diet Diversity Score (DDS) | 11,127 | 563 (5.1) | 0.92 (0.74–1.13) | ||
| Overweight (WHZ) > +2 | ||||||
|---|---|---|---|---|---|---|
| Characteristics | Total n (%) | Overweight n (%) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | Adjusted OR with Diet Quality (95% CI) | |
| Education (father) | Illiterate | 387 (3.4) | 12 (3.1) | 1.05 (0.56–1.96) | 2.05 (0.92–4.58) | 2.18 (0.97–4.87) |
| Primary school | 1976 (17.7) | 33 (1.7) | 0.56 * (0.37–0.85) | 0.83 (0.47–1.46) | 0.85 (0.48–1.50) | |
| Secondary school | 2885 (25.9) | 49 (1.7) | 0.57 * (0.39–0.83) | 0.67 (0.41–1.10) | 0.69 (0.42–1.13) | |
| High school | 3690 (33.1) | 108 (2.9) | 1.01 (0.74–1.38) | 1.12 (0.75–1.66) | 1.14 (0.77–1.70) | |
| Higher education | 2190 (19.6) | 64 (2.9) | Ref | Ref | Ref | |
| Education (mother) | Illiterate | 511 (4.6) | 11 (2.2) | 0.75 (0.39–1.44) | 1.37 (0.60–3.09) | 1.36 (0.60–3.07) |
| Primary school | 2326 (21.0) | 37 (1.6) | 0.55 * (0.37–0.83) | 0.95 (0.56–1.62) | 0.96 (0.56–1.63) | |
| Secondary school | 2049 (18.5) | 46 (2.2) | 0.79 (0.54–1.16) | 1.24 (0.77–1.98) | 1.24 (0.77–1.98) | |
| High school | 3974 (35.9) | 109 (2.8) | 0.98 (0.72–1.35) | 1.29 (0.89–1.86) | 1.28 (0.88–1.86) | |
| Higher education | 2180 (19.7) | 61 (2.8) | Ref | Ref | Ref | |
| Occupation (father) | Employee | 1572 (14.2) | 44 (2.8) | Ref | Ref | Ref |
| Laborer | 2604 (23.5) | 48 (1.9) | 0.66 (0.44–1.00) | 0.80 (0.48–1.33) | 1.25 (0.64–2.47) | |
| Farmer | 1016 (9.1) | 16 (1.6) | 0.56 * (0.31–0.99) | 0.71 (0.37–1.37) | 0.97 (0.51–1.87) | |
| Shopkeeper | 4535 (41.0) | 132 (2.9) | 1.05 (0.74–1.48) | 1.17 (0.77–1.77) | 0.87 (0.40–1.87) | |
| Retired, student, or unemployed | 423 (3.8) | 2 (2.3) | 0.25 * (0.08–0.80) | 0.29 * (0.09–0.99) | 1.44 (0.79–2.62) | |
| Military | 232 (2.1) | 7 (3.0) | 1.10 (0.49–2.46) | 1.08 (0.48–2.45) | 1.12 (0.24–5.14) | |
| Others | 664 (6.0) | 13 (2.0) | 0.70 (0.37–1.33) | 0.82 (0.41–1.61) | 0.15 (0.02–1.20) | |
| Occupation (mother) | Working 1 | 952 (8.5) | 32 (3.3) | Ref | Ref | Ref |
| Nonworking | 10,168 (91.4) | 232 (2.2) | 1.37 (0.72–1.86) | 0.75 (0.50–1.13) | 1.32 (0.88–1.97) | |
| Rooms/family size (quartiles) | 1 | 2489 (22.5) | 57 (2.3) | 0.72 (0.50–1.03) | 1.10 (0.73–1.67) | 1.12 (0.74–1.70) |
| 2 | 4508 (40.9) | 89 (2.0) | 0.62 * (0.45–0.86) | 0.77 (0.55–01.09) | 0.78 (0.55–1.10) | |
| 3 | 1967 (17.8) | 50 (2.5) | 0.81 (0.56–1.17) | 0.86 (0.58–1.26) | 0.86 (0.58–1.25) | |
| 4 | 2054 (18.6) | 65 (3.2) | Ref | Ref | Ref | |
| Areas/family size (quartiles) | 1 | 2742 (24.6) | 53 (1.9) | 0.63 * (0.44–0.91) | 0.75 (0.50–1.14) | 0.75 (0.50–1.14) |
| 2 | 2868 (25.7) | 55 (1.9) | 0.62 * (0.44–0.89) | 0.71 (0.47–1.05) | 0.70 (0.47–1.04) | |
| 3 | 3134 (28.1) | 87 (2.8) | 0.92 (0.67–1.26) | 0.98 (0.70–1.37) | 0.98 (0.70–1.36) | |
| 4 | 2382 (21.4) | 71 (3.0) | Ref | Ref | Ref | |
| Assets (score = sum of assets) | 0 | 1393 (12.4) | 19 (1.4) | 0.39 * (0.22–0.69) | 0.62 (0.32–1.20) | 0.66 (0.34–1.28) |
| 1 | 1939 (17.3) | 35 (1.8) | 0.60 * (0.38–0.96) | 0.90 (0.53–1.52) | 0.93 (0.55–1.58) | |
| 2 | 2479 (22.2) | 54 (2.2) | 0.67 (0.44–1.04) | 0.88 (0.54–1.42) | 0.90 (0.56–1.47) | |
| 3 | 2294 (20.5) | 72 (3.1) | 0.89 (0.58–1.35) | 1.05 (0.66–1.65) | 1.07 (0.68–1.69) | |
| 4 | 1818 (16.3) | 48 (2.6) | 0.75 (0.48–1.17) | 0.84 (0.52–1.35) | 0.85 (0.53–1.37) | |
| 5 | 983 (8.8) | 26 (2.7) | Ref | Ref | Ref | |
| Diet Diversity Score (DDS) | 11,127 | 265 (2.4) | 1.39 * (1.08–1.81) | 1.29 (0.99–1.69) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kasaii, M.S.; Rodrigues, S.; Abdollahi, M.; Houshiar-Rad, A.; Perelman, J. Socioeconomic Patterning of Stunting and Overweight Among Iranian Children Aged 2–5 Years: A National Cross-Sectional Analysis. Nutrients 2025, 17, 1631. https://doi.org/10.3390/nu17101631
Kasaii MS, Rodrigues S, Abdollahi M, Houshiar-Rad A, Perelman J. Socioeconomic Patterning of Stunting and Overweight Among Iranian Children Aged 2–5 Years: A National Cross-Sectional Analysis. Nutrients. 2025; 17(10):1631. https://doi.org/10.3390/nu17101631
Chicago/Turabian StyleKasaii, Maryam Sadat, Sara Rodrigues, Morteza Abdollahi, Anahita Houshiar-Rad, and Julian Perelman. 2025. "Socioeconomic Patterning of Stunting and Overweight Among Iranian Children Aged 2–5 Years: A National Cross-Sectional Analysis" Nutrients 17, no. 10: 1631. https://doi.org/10.3390/nu17101631
APA StyleKasaii, M. S., Rodrigues, S., Abdollahi, M., Houshiar-Rad, A., & Perelman, J. (2025). Socioeconomic Patterning of Stunting and Overweight Among Iranian Children Aged 2–5 Years: A National Cross-Sectional Analysis. Nutrients, 17(10), 1631. https://doi.org/10.3390/nu17101631







