Effect of Creatine Monohydrate Supplementation on Macro- and Microvascular Endothelial Function in Older Adults: A Pilot Study
Highlights
- Creatine offers many physiological benefits for performance and health, but the effects of creatine supplementation on macro- and microvasculature are scarcely investigated.
- We conducted a novel, randomized, crossover, pilot study to explore the impact of creatine supplementation on varied vascular measures versus placebo in healthy older adults who remain at risk of cardiovascular disease.
- Creatine supplementation led to improvements in flow-mediated dilation, microvascular reperfussion, fasting glucose and triglycerides versus placebo; however, pulse wave velocity and biomarkers of oxidative stress were not affected.
- The data support potential vascular-based benefits of creatine in older adults that require larger trials to expand upon these findings and explore their underlying mechanisms of action.
Abstract
1. Introduction
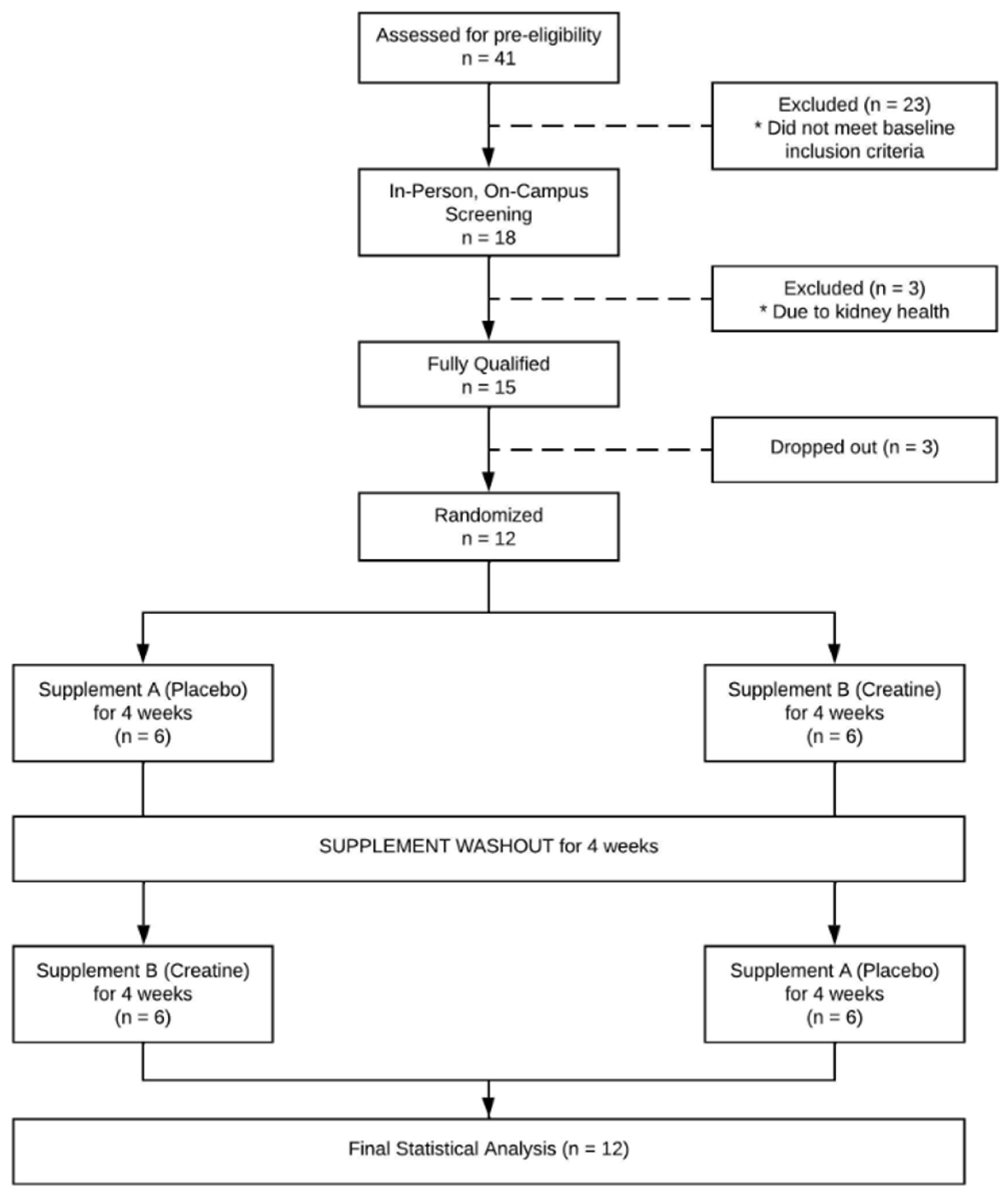
2. Methods
2.1. Study Participants
2.2. Study Design
2.3. Supplementation Protocol
2.4. Hemodynamic and Fluid Dynamic Assessments
2.5. Standardization of Vascular Assessments
2.6. Brachial Artery Flow-Mediated Dilation
2.7. Pulse Wave Analysis and Velocity Assessments
2.8. Near-Infrared Spectroscopy Microvascular Assessment
2.9. Blood Collection and Analyses
2.10. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Hemodynamics and Fluid Dynamics
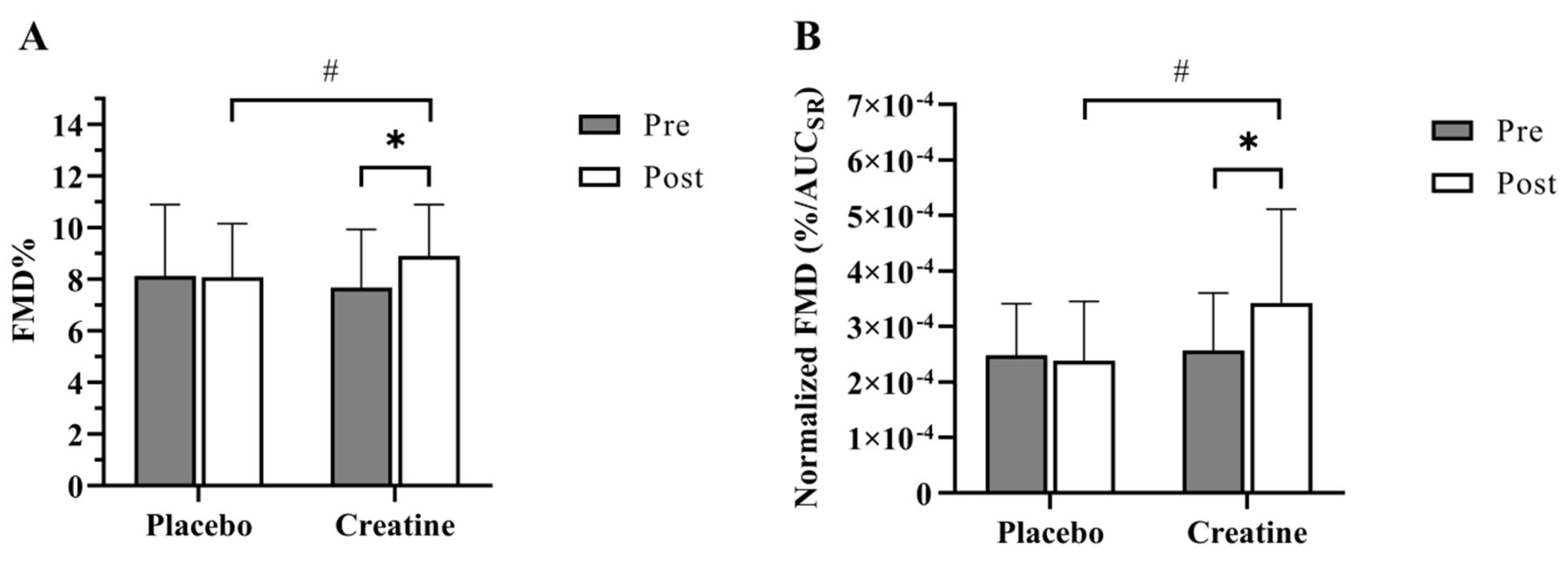
3.3. Flow-Mediated Dilation
3.4. Pulse Wave Analysis and Velocity
3.5. Near-Infrared Spectroscopy
3.6. Blood Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Center for Health Statistics. Multiple Cause of Death 2018–2022 on CDC WONDER Database. Available online: https://wonder.cdc.gov/mcd.html (accessed on 3 May 2024).
- Rodgers, J.L.; Jones, J.; Bolleddu, S.I.; Vanthenapalli, S.; Rodgers, L.E.; Shah, K.; Karia, K.; Panguluri, S.K. Cardiovascular Risks Associated with Gender and Aging. J. Cardiovasc. Dev. Dis. 2019, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Gkaliagkousi, E.; Lazaridis, A.; Dogan, S.; Fraenkel, E.; Tuna, B.G.; Mozos, I.; Vukicevic, M.; Yalcin, O.; Gopcevic, K. Theories and Molecular Basis of Vascular Aging: A Review of the Literature from VascAgeNet Group on Pathophysiological Mechanisms of Vascular Aging. Int. J. Mol. Sci. 2022, 23, 8672. [Google Scholar] [CrossRef]
- Del Buono, M.G.; Montone, R.A.; Camilli, M.; Carbone, S.; Narula, J.; Lavie, C.J.; Niccoli, G.; Crea, F. Coronary Microvascular Dysfunction Across the Spectrum of Cardiovascular Diseases: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 78, 1352–1371. [Google Scholar] [CrossRef]
- Matsue, Y.; Yoshida, K.; Nagahori, W.; Ohno, M.; Suzuki, M.; Matsumura, A.; Hashimoto, Y.; Yoshida, M. Peripheral microvascular dysfunction predicts residual risk in coronary artery disease patients on statin therapy. Atherosclerosis 2014, 232, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Kris-Etherton, P.M.; Lichtenstein, A.H.; Howard, B.V.; Steinberg, D.; Witztum, J.L. Antioxidant vitamin supplements and cardiovascular disease. Circulation 2004, 110, 637–641. [Google Scholar] [CrossRef] [PubMed]
- Wallimann, T.; Wyss, M.; Brdiczka, D.; Nicolay, K.; Eppenberger, H.M. Intracellular compartmentation, structure and function of creatine kinase isoenzymes in tissues with high and fluctuating energy demands: The ‘phosphocreatine circuit’ for cellular energy homeostasis. Biochem. J. 1992, 281 Pt 1, 21–40. [Google Scholar] [CrossRef]
- Wallimann, T.; Tokarska-Schlattner, M.; Schlattner, U. The creatine kinase system and pleiotropic effects of creatine. Amino Acids 2011, 40, 1271–1296. [Google Scholar] [CrossRef] [PubMed]
- Tarnopolsky, M.A.; Parise, G. Direct measurement of high-energy phosphate compounds in patients with neuromuscular disease. Muscle Nerve 1999, 22, 1228–1233. [Google Scholar] [CrossRef]
- Wyss, M.; Schulze, A. Health implications of creatine: Can oral creatine supplementation protect against neurological and atherosclerotic disease? Neuroscience 2002, 112, 243–260. [Google Scholar] [CrossRef]
- Gualano, B.; Painneli, V.D.S.; Roschel, H.; Artioli, G.G.; Manoel Neves, J.R.; Pinto, A.L.D.S.; Da Silva, M.E.R.; Cunha, M.R.; Otaduy, M.C.G.; Leite, C.D.C.; et al. Creatine in type 2 diabetes: A randomized, double-blind, placebo-controlled trial. Med. Sci. Sports Exerc. 2011, 43, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Gualano, B.; de Salles Painelli, V.; Roschel, H.; Lugaresi, R.; Dorea, E.; Artioli, G.G.; Lima, F.R.; da Silva, M.E.; Cunha, M.R.; Seguro, A.C.; et al. Creatine supplementation does not impair kidney function in type 2 diabetic patients: A randomized, double-blind, placebo-controlled, clinical trial. Eur. J. Appl. Physiol. 2011, 111, 749–756. [Google Scholar] [CrossRef]
- Schlattner, U.; Tokarska-Schlattner, M.; Wallimann, T. Mitochondrial creatine kinase in human health and disease. Biochim. Biophys. Acta 2006, 1762, 164–180. [Google Scholar] [CrossRef]
- Lawler, J.M.; Barnes, W.S.; Wu, G.; Song, W.; Demaree, S. Direct antioxidant properties of creatine. Biochem. Biophys. Res. Commun. 2002, 290, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Sestili, P.; Martinelli, C.; Colombo, E.; Barbieri, E.; Potenza, L.; Sartini, S.; Fimognari, C. Creatine as an antioxidant. Amino Acids 2011, 40, 1385–1396. [Google Scholar] [CrossRef] [PubMed]
- Nomura, A.; Zhang, M.; Sakamoto, T.; Ishii, Y.; Morishima, Y.; Mochizuki, M.; Kimura, T.; Uchida, Y.; Sekizawa, K. Anti-inflammatory activity of creatine supplementation in endothelial cells in vitro. Br. J. Pharmacol. 2003, 139, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Deminice, R.; Jordao, A.A. Creatine supplementation decreases plasma lipid peroxidation markers and enhances anaerobic performance in rats. Redox Rep. 2016, 21, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Decking, U.K.; Alves, C.; Wallimann, T.; Wyss, M.; Schrader, J. Functional aspects of creatine kinase isoenzymes in endothelial cells. Am. J. Physiol. Cell Physiol. 2001, 281, C320–C328. [Google Scholar] [CrossRef]
- Rossman, M.J.; LaRocca, T.J.; Martens, C.R.; Seals, D.R. Healthy lifestyle-based approaches for successful vascular aging. J. Appl. Physiol. 2018, 125, 1888–1900. [Google Scholar] [CrossRef] [PubMed]
- Kreider, R.B.; Jäger, R.; Purpura, M. Bioavailability, Efficacy, Safety, and Regulatory Status of Creatine and Related Compounds: A Critical Review. Nutrients 2022, 14, 1035. [Google Scholar] [CrossRef]
- Hultman, E.; Soderlund, K.; Timmons, J.A.; Cederblad, G.; Greenhaff, P.L. Muscle creatine loading in men. J. Appl. Physiol. 1996, 81, 232–237. [Google Scholar] [CrossRef]
- Harris, R.C.; Soderlund, K.; Hultman, E. Elevation of creatine in resting and exercised muscle of normal subjects by creatine supplementation. Clin. Sci. 1992, 83, 367–374. [Google Scholar] [CrossRef]
- Kreider, R.B.; Kalman, D.S.; Antonio, J.; Ziegenfuss, T.N.; Wildman, R.; Collins, R.; Candow, D.G.; Kleiner, S.M.; Almada, A.L.; Lopez, H.L. International Society of Sports Nutrition position stand: Safety and efficacy of creatine supplementation in exercise, sport, and medicine. J. Int. Soc. Sports Nutr. 2017, 14, 18. [Google Scholar] [CrossRef]
- Candow, D.G.; Forbes, S.C.; Chilibeck, P.D.; Cornish, S.M.; Antonio, J.; Kreider, R.B. Effectiveness of Creatine Supplementation on Aging Muscle and Bone: Focus on Falls Prevention and Inflammation. J. Clin. Med. 2019, 8, 488. [Google Scholar] [CrossRef] [PubMed]
- Persky, A.M.; Brazeau, G.A. Clinical pharmacology of the dietary supplement creatine monohydrate. Pharmacol. Rev. 2001, 53, 161–176. [Google Scholar] [PubMed]
- Persky, A.M.; Brazeau, G.A.; Hochhaus, G. Pharmacokinetics of the dietary supplement creatine. Clin. Pharmacokinet. 2003, 42, 557–574. [Google Scholar] [CrossRef] [PubMed]
- Vandenberghe, K.; Goris, M.; Van Hecke, P.; Van Leemputte, M.; Vangerven, L.; Hespel, P. Long-term creatine intake is beneficial to muscle performance during resistance training. J. Appl. Physiol. 1997, 83, 2055–2063. [Google Scholar] [CrossRef]
- Thijssen, D.H.; Black, M.A.; Pyke, K.E.; Padilla, J.; Atkinson, G.; Harris, R.A.; Parker, B.; Widlansky, M.E.; Tschakovsky, M.E.; Green, D.J. Assessment of flow-mediated dilation in humans: A methodological and physiological guideline. Am. J. Physiol. Heart Circ. Physiol. 2011, 300, H2–H12. [Google Scholar] [CrossRef]
- Harris, R.A.; Nishiyama, S.K.; Wray, D.W.; Richardson, R.S. Ultrasound assessment of flow-mediated dilation. Hypertension 2010, 55, 1075–1085. [Google Scholar] [CrossRef]
- Soares, R.N.; Somani, Y.B.; Proctor, D.N.; Murias, J.M. The association between near-infrared spectroscopy-derived and flow-mediated dilation assessment of vascular responsiveness in the arm. Microvasc. Res. 2019, 122, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Iannetta, D.; Inglis, E.C.; Soares, R.N.; McLay, K.M.; Pogliaghi, S.; Murias, J.M. Reliability of microvascular responsiveness measures derived from near-infrared spectroscopy across a variety of ischemic periods in young and older individuals. Microvasc. Res. 2019, 122, 117–124. [Google Scholar] [CrossRef]
- Jones, T.; Dunn, E.L.; Macdonald, J.H.; Kubis, H.P.; McMahon, N.; Sandoo, A. The Effects of Beetroot Juice on Blood Pressure, Microvascular Function and Large-Vessel Endothelial Function: A Randomized, Double-Blind, Placebo-Controlled Pilot Study in Healthy Older Adults. Nutrients 2019, 11, 1792. [Google Scholar] [CrossRef]
- Ahn, Y.; Aung, N.; Ahn, H.-S. A Comprehensive Review of Clinical Studies Applying Flow-Mediated Dilation. Diagnostics 2024, 14, 2499. [Google Scholar] [CrossRef] [PubMed]
- Ras, R.T.; Streppel, M.T.; Draijer, R.; Zock, P.L. Flow-mediated dilation and cardiovascular risk prediction: A systematic review with meta-analysis. Int. J. Cardiol. 2013, 168, 344–351. [Google Scholar] [CrossRef]
- Green, D.J.; Jones, H.; Thijssen, D.; Cable, N.T.; Atkinson, G. Flow-mediated dilation and cardiovascular event prediction: Does nitric oxide matter? Hypertension 2011, 57, 363–369. [Google Scholar] [CrossRef]
- Curtis, P.J.; Van Der Velpen, V.; Berends, L.; Jennings, A.; Feelisch, M.; Umpleby, A.M.; Evans, M.; Fernandez, B.O.; Meiss, M.S.; Minnion, M.; et al. Blueberries improve biomarkers of cardiometabolic function in participants with metabolic syndrome-results from a 6-month, double-blind, randomized controlled trial. Am. J. Clin. Nutr. 2019, 109, 1535–1545. [Google Scholar] [CrossRef]
- Sabbatinelli, J.; Orlando, P.; Galeazzi, R.; Silvestri, S.; Cirilli, I.; Marcheggiani, F.; Dludla, P.V.; Giuliani, A.; Bonfigli, A.R.; Mazzanti, L.; et al. Ubiquinol Ameliorates Endothelial Dysfunction in Subjects with Mild-to-Moderate Dyslipidemia: A Randomized Clinical Trial. Nutrients 2020, 12, 1098. [Google Scholar] [CrossRef]
- Mohler, E.R., III; Herrington, D.; Ouyang, P.; Mangano, C.; Ritter, S.; Davis, P.; Purkayastha, D.; Gatlin, M.; Vogel, R.A. A Randomized, Double-Blind Trial Comparing the Effects of Amlodipine Besylate/Benazepril HCl vs Amlodipine on Endothelial Function and Blood Pressure. J. Clin. Hypertens. 2006, 8, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Aron, A.; Landrum, E.J.; Schneider, A.D.; Via, M.; Evans, L.; Rawson, E.S. Effects of acute creatine supplementation on cardiac and vascular responses in older men; a randomized controlled trial. Clin. Nutr. 2024, 63, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Gonzalez, M.A.; Wieder, R.; Kim, J.S.; Vicil, F.; Figueroa, A. Creatine supplementation attenuates hemodynamic and arterial stiffness responses following an acute bout of isokinetic exercise. Eur. J. Appl. Physiol. 2011, 111, 1965–1971. [Google Scholar] [CrossRef] [PubMed]
- Mihic, S.; MacDonald, J.R.; McKenzie, S.; Tarnopolsky, M.A. Acute creatine loading increases fat-free mass, but does not affect blood pressure, plasma creatinine, or CK activity in men and women. Med. Sci. Sports Exerc. 2000, 32, 291. [Google Scholar] [CrossRef]
- Murphy, A.J.; Watsford, M.L.; Coutts, A.J.; Richards, D.A. Effects of creatine supplementation on aerobic power and cardiovascular structure and function. J. Sci. Med. Sport. 2005, 8, 305–313. [Google Scholar] [CrossRef]
- Kastello, G.M.; Asuncion, E.J.; Boyd, M.S.; Exsted, N. Creatine Monohydrate: Daily Blood Pressure Monitoring During the Loading Phase of Supplementation. In Medicine and Science in Sports and Exercise; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012; p. 606. [Google Scholar]
- Galvan, E.; Walker, D.K.; Simbo, S.Y.; Dalton, R.; Levers, K.; O’connor, A.; Goodenough, C.; Barringer, N.D.; Greenwood, M.; Rasmussen, C.; et al. Acute and chronic safety and efficacy of dose dependent creatine nitrate supplementation and exercise performance. J. Int. Soc. Sports Nutr. 2016, 13, 12. [Google Scholar] [CrossRef] [PubMed]
- Moraes, R.; Van Bavel, D.; Moraes, B.S.; Tibirica, E. Effects of dietary creatine supplementation on systemic microvascular density and reactivity in healthy young adults. Nutr. J. 2014, 13, 115. [Google Scholar] [CrossRef] [PubMed]
- Van Bavel, D.; de Moraes, R.; Tibirica, E. Effects of dietary supplementation with creatine on homocysteinemia and systemic microvascular endothelial function in individuals adhering to vegan diets. Fundam. Clin. Pharmacol. 2018, 33, 428–440. [Google Scholar] [CrossRef]
- Rahimi, R. Creatine supplementation decreases oxidative DNA damage and lipid peroxidation induced by a single bout of resistance exercise. J. Strength Cond. Res. 2011, 25, 3448–3455. [Google Scholar] [CrossRef] [PubMed]
- Ahsan, A.; Han, G.; Pan, J.; Liu, S.; Padhiar, A.A.; Chu, P.; Sun, Z.; Zhang, Z.; Sun, B.; Wu, J.; et al. Phosphocreatine protects endothelial cells from oxidized low-density lipoprotein-induced apoptosis by modulating the PI3K/Akt/eNOS pathway. Apoptosis 2015, 20, 1563–1576. [Google Scholar] [CrossRef] [PubMed]
- Chia, C.W.; Egan, J.M.; Ferrucci, L. Age-Related Changes in Glucose Metabolism, Hyperglycemia, and Cardiovascular Risk. Circ. Res. 2018, 123, 886–904. [Google Scholar] [CrossRef]
- Rocic, B.; Bajuk, N.B.; Rocic, P.; Weber, D.S.; Boras, J.; Lovrencic, M.V. Comparison of antihyperglycemic effects of creatine and metformin in type II diabetic patients. Clin. Investig. Med. 2009, 32, E322. [Google Scholar] [CrossRef] [PubMed]
- Ročić, B.; Znaor, A.; Ročić, P.; Weber, D.; Vučić Lovrenčić, M. Comparison of antihyperglycemic effects of creatine and glibenclamide in type II diabetic patients. Wien. Med. Wochenschr. 2011, 161, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Rooney, K.B.; Bryson, J.M.; Digney, A.L.; Rae, C.D.; Thompson, C.H. Creatine supplementation affects glucose homeostasis but not insulin secretion in humans. Ann. Nutr. Metab. 2003, 47, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Newman, J.E.; Hargreaves, M.; Garnham, A.; Snow, R.J. Effect of creatine ingestion on glucose tolerance and insulin sensitivity in men. Med. Sci. Sports Exerc. 2003, 35, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Earnest, C.P.; Almada, A.L.; Mitchell, T.L. High-performance capillary electrophoresis-pure creatine monohydrate reduces blood lipids in men and women. Clin. Sci. 1996, 91, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Bode-Böger, S.M.; Muke, J.; Surdacki, A.; Brabant, G.; Böger, R.H.; Frölich, J.C. Oral L-arginine improves endothelial function in healthy individuals older than 70 years. Vasc. Med. 2003, 8, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Yin, W.H.; Chen, J.W.; Tsai, C.; Chiang, M.C.; Young, M.S.; Lin, S.J. L-arginine improves endothelial function and reduces LDL oxidation in patients with stable coronary artery disease. Clin. Nutr. 2005, 24, 988–997. [Google Scholar] [CrossRef]
- Cracowski, J.-L.; Gaillard-Bigot, F.; Cracowski, C.; Sors, C.; Roustit, M.; Millet, C. Involvement of cytochrome epoxygenase metabolites in cutaneous postocclusive hyperemia in humans. J. Appl. Physiol. 2013, 114, 245–251. [Google Scholar] [CrossRef]
- Dzeja, P.P.; Terzic, A. Phosphotransfer reactions in the regulation of ATP-sensitive K+ channels. FASEB J. 1998, 12, 523–529. [Google Scholar] [CrossRef]
- Selivanov, V.A.; Alekseev, A.E.; Hodgson, D.M.; Dzeja, P.P.; Terzic, A. Nucleotide-gated KATP channels integrated with creatine and adenylate kinases: Amplification, tuning and sensing of energetic signals in the compartmentalized cellular environment. Mol. Cell Biochem. 2004, 256, 243–256. [Google Scholar] [CrossRef] [PubMed]
- Clarke, H.; Hickner, R.C.; Ormsbee, M.J. The Potential Role of Creatine in Vascular Health. Nutrients 2021, 13, 857. [Google Scholar] [CrossRef] [PubMed]
- Clarke, H.; Kim, D.-H.; Meza, C.A.; Ormsbee, M.J.; Hickner, R.C. The Evolving Applications of Creatine Supplementation: Could Creatine Improve Vascular Health? Nutrients 2020, 12, 2834. [Google Scholar] [CrossRef] [PubMed]

| Randomized Group Sequence | p Value | |||
|---|---|---|---|---|
| Overall | PL—CrM | CrM—PL | ||
| N (Male/Female) | 12 (6/6) | 6 (4/2) | 6 (2/4) | - |
| Age (years) | 58.3 ± 3.4 | 59 ± 2.7 | 57.5 ± 4.1 | 0.473 |
| Height (cm) | 171.1 ± 9.0 | 171.7 ± 8.2 | 170.5 ± 10.4 | 0.824 |
| Weight (kg) | 75.0 ± 17.8 | 75.6 ± 17.9 | 74.5 ± 19.4 | 0.917 |
| BMI (kg/m2) | 25.6 ± 5.6 | 25.7 ± 5.9 | 25.5 ± 5.9 | 0.962 |
| Variable | Placebo | Creatine | |
|---|---|---|---|
| Resting Diameter (mm) | |||
| Pre | 4.10 ± 0.73 | 4.21 ± 0.81 | |
| Post | 4.11 ± 0.8 | 4.18 ± 0.82 | |
| Δ | 0.01 ± 0.15 | −0.13 ± 0.13 | |
| Absolute Change (mm) * | |||
| Pre | 0.33 ± 0.11 | 0.33 ± 0.12 | |
| Post | 0.34 ± 0.11 | 0.38 ± 0.12 †‡ | |
| Δ | 0.003 ± 0.06 | 0.05 ± 0.04 ⁋ | |
| Time to Peak (sec) | |||
| Pre | 43.5 ± 7.73 | 38 ± 8.52 | |
| Post | 41.25 ± 11.87 | 41.5 ± 11.92 | |
| Δ | −2.25 ± 14.65 | 3.5 ± 13.71 | |
| FMD% * | |||
| Pre | 8.13 ± 2.76 | 7.68 ± 2.25 | |
| Post | 8.08 ± 2.07 | 8.9 ± 1.99 †‡ | |
| Δ | −0.05 ± 1.73 | 1.22 ± 0.87 ⁋ | |
| Shear Stress (AUC) | |||
| Pre | 35,579.73 ± 12549.4 | 32,087.04 ± 8209.87 | |
| Post | 35,675.45 ± 9752.13 | 30,650.48 ± 10,244.53 | |
| Δ | 95 ± 5881.29 | −1436.56 ± 4362.63 | |
| Normalized FMD (%/AUCSR) * | |||
| Pre | 2.48 × 10−4 ± 9.28 × 10−5 | 2.57 × 10−4 ± 1.03 × 10−4 | |
| Post | 2.38 × 10−4 ± 1.07 × 10−4 | 3.42 × 10−4 ± 1.69 × 10−4 †‡ | |
| Δ | −1.01 × 10−5 ± 4.60 × 10−5 | 8.44 × 10−5 ± 9.47 × 10−5 ⁋ | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clarke, H.E.; Akhavan, N.S.; Behl, T.A.; Ormsbee, M.J.; Hickner, R.C. Effect of Creatine Monohydrate Supplementation on Macro- and Microvascular Endothelial Function in Older Adults: A Pilot Study. Nutrients 2025, 17, 58. https://doi.org/10.3390/nu17010058
Clarke HE, Akhavan NS, Behl TA, Ormsbee MJ, Hickner RC. Effect of Creatine Monohydrate Supplementation on Macro- and Microvascular Endothelial Function in Older Adults: A Pilot Study. Nutrients. 2025; 17(1):58. https://doi.org/10.3390/nu17010058
Chicago/Turabian StyleClarke, Holly E., Neda S. Akhavan, Taylor A. Behl, Michael J. Ormsbee, and Robert C. Hickner. 2025. "Effect of Creatine Monohydrate Supplementation on Macro- and Microvascular Endothelial Function in Older Adults: A Pilot Study" Nutrients 17, no. 1: 58. https://doi.org/10.3390/nu17010058
APA StyleClarke, H. E., Akhavan, N. S., Behl, T. A., Ormsbee, M. J., & Hickner, R. C. (2025). Effect of Creatine Monohydrate Supplementation on Macro- and Microvascular Endothelial Function in Older Adults: A Pilot Study. Nutrients, 17(1), 58. https://doi.org/10.3390/nu17010058







