Tailored Meal-Type Food Provision for Diabetes Patients Can Improve Routine Blood Glucose Management in Patients with Type 2 Diabetes: A Crossover Study
Abstract
1. Introduction
2. Materials and Methods
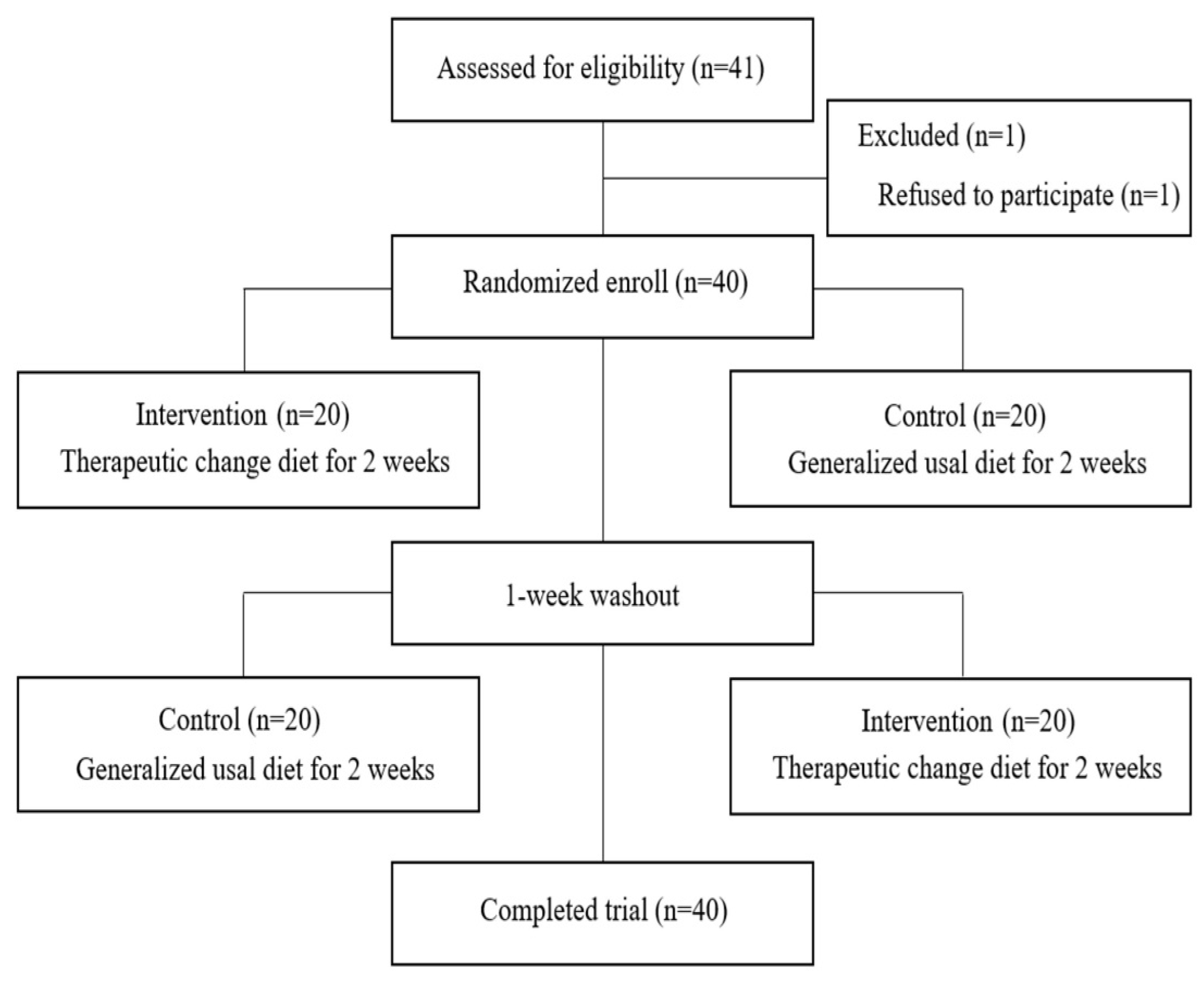
2.1. Study Design and Participants
2.2. Diet Composition and Provision
2.3. Participant Characteristics
2.4. Outcome Assessment
2.5. Nutrient Intake
2.6. Glycemic Control
2.7. Statistical Analyses
3. Results
3.1. General Characteristics
3.2. Comparison of Clinical Factors and Nutritional Status Changes
3.3. Changes in Nutrient Intake
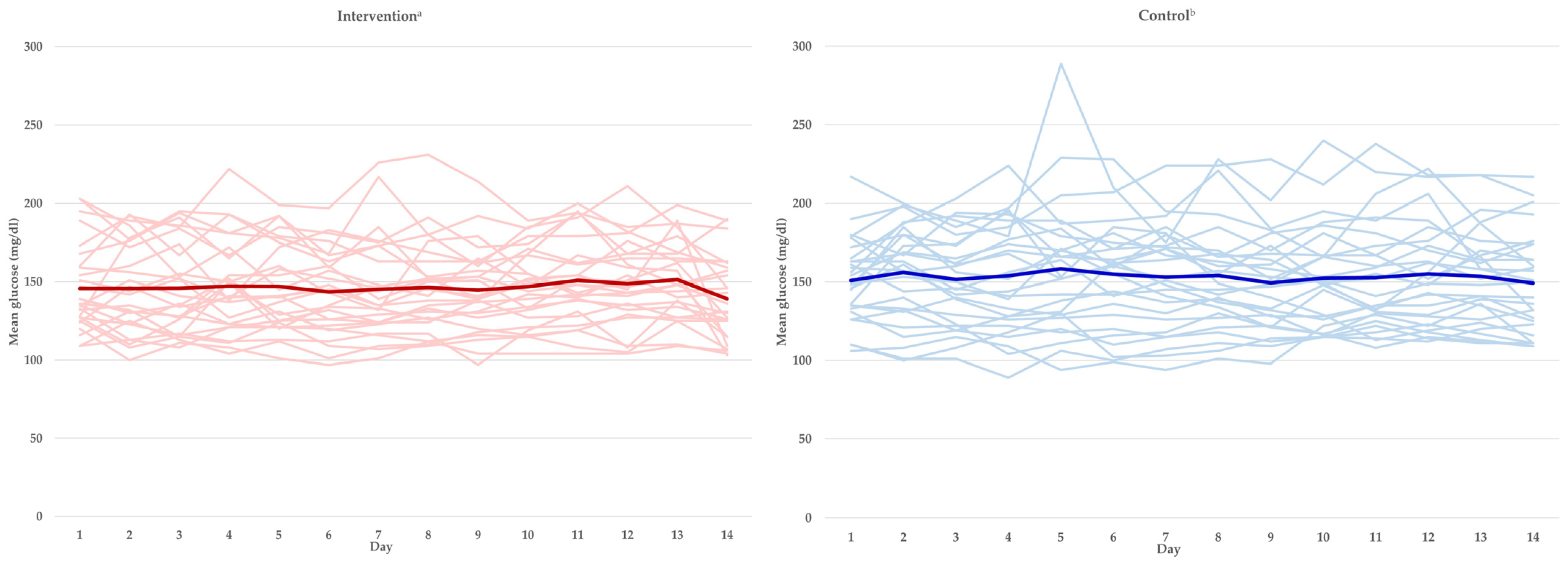
3.4. Analysis of Blood Glucose Index Changes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of type 2 diabetes—Global burden of disease and forecasted trends. J. Epidemiol. Glob. Health. 2020, 10, 107–111. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. Global Diabetes Data Report 2000–2045. Available online: https://diabetesatlas.org/data/en/world/ (accessed on 19 February 2024).
- Korean Diabetes Association. Diabetes Fact Sheet in Korea. 2022. Available online: https://www.diabetes.or.kr/bbs/?code=fact_sheet&mode=view&number=2500&page=1&code=fact_sheet (accessed on 19 February 2024).
- International Diabetes Federation. Diabetes Prevention. Available online: https://idf.org/about-diabetes/diabetes-prevention/ (accessed on 19 February 2024).
- Korean Diabetes Association. Clinical Practice Guidelines for Diabetes. Available online: https://www.diabetes.or.kr/bbs/?code=guide&mode=view&number=1284&page=1&code=guide (accessed on 19 February 2024).
- Lee, J.; Kim, J.H. Clinical utilities of continuous glucose monitoring and insulin pumps in pediatric patients with type 1 diabetes. Ewha Med. J. 2021, 44, 55–62. [Google Scholar] [CrossRef]
- American Diabetes Association. 7. Diabetes technology: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44 (Suppl. 1), S85–S99. [Google Scholar] [CrossRef] [PubMed]
- Price, D.A.; Deng, Q.; Kipnes, M.; Beck, S.E. Episodic real-time CGM use in adults with type 2 diabetes: Results of a pilot randomized controlled trial. Diabetes Ther. 2021, 12, 2089–2099. [Google Scholar] [CrossRef] [PubMed]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 5. Facilitating positive health behaviors and well-being to improve health outcomes: Standards of care in diabetes-2023. Diabetes Care 2023, 46 (Suppl. 1), S68–S96. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, K.B.; Ranjan, A.G.; McCarthy, O.M.; Bracken, R.M.; Nørgaard, K.; Schmidt, S. Sensor-based glucose metricsduring different diet compositions in type 1 diabetes-A randomized one-week crossover trial. Nutrients 2024, 16, 199. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Food and Drug Safety. Available online: https://www.mfds.go.kr/brd/m_211/view.do?seq=14817 (accessed on 19 February 2024).
- Lee, D.G.; Kang, I.G.; Kim, T.S.; Ahn, Y.; Lee, S.Y.; Ahn, H.J.; Park, Y.K. Efficacy of convenience meal-type foods designed for diabetes in the management of metabolic syndrome based on a 3-week trial. Nutrition 2024, 118, 112287. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.H.; Min, S.H.; Lim, K.H.; Shin, U.J.; Kim, M.S. Glucose-lowering effect of home-delivered therapeutic meals in patients with type 2 diabetes. Korean Diabetes J. 2020, 21, 46–54. [Google Scholar] [CrossRef]
- Gomes, J.M.G.; Costa, J.D.A.; Alfenas, R.C.G. Effect of increased calcium consumption from fat-free milk in an energy-restricted diet on the metabolic syndrome and cardiometabolic outcomes in adults with type 2 diabetes mellitus: A randomised cross-over clinical trial. Br. J. Nutr. 2018, 119, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Bjørnshave, A.; Holst, J.J.; Hermansen, K. Pre-meal effect of whey proteins on metabolic parameters in subjects with and without type 2 diabetes: A randomized, crossover trial. Nutrients 2018, 10, 122. [Google Scholar] [CrossRef]
- Lee, J.S.; Kim, H.Y.; Hwang, J.Y.; Kwon, S.; Chung, H.R.; Kwak, T.-K.; Kang, M.-H.; Choi, Y.-S. Development of nutrition quotient for Korean adults: Item selection and validation of factor structure. J. Nutr. Health. 2018, 51, 340–356. [Google Scholar] [CrossRef]
- Battelino, T.; Danne, T.; Bergenstal, R.M.; Amiel, S.A.; Beck, R.; Biester, T.; Bosi, E.; Buckingham, B.A.; Cefalu, W.T.; Close, K.L.; et al. Clinical targets for continuous glucose monitoring data interpretation: Recommendations from the international consensus on time in range. Diabetes Care 2019, 42, 1593–1603. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Keogh, J.B.; Clifton, P.M. Differential effects of red meat/refined grain diet and dairy/chicken/nuts/whole grain diet on glucose, insulin and triglyceride in a randomized crossover study. Nutrients 2016, 8, 687. [Google Scholar] [CrossRef] [PubMed]
- Mendez, I.; Lundeen, E.A.; Saunders, M.; Williams, A.; Saaddine, J.; Albright, A. Diabetes self-management education and association with diabetes self-care and clinical preventive care practices. Sci. Diabetes Self Manag. Care. 2022, 48, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Stolar, M.W.; Hoogwerf, B.J.; Gorshow, S.M.; Boyle, P.J.; Wales, D.O. Managing type 2 diabetes: Going beyond glycemic control. J. Manag. Care Pharm. 2008, 14 (Suppl. B), s2–s19. [Google Scholar] [CrossRef] [PubMed]
- Morton, J.I.; Lazzarini, P.A.; Polkinghorne, K.R.; Carstensen, B.; Magliano, D.J.; Shaw, J.E. The association of attained age, age at diagnosis, and duration of type 2 diabetes with the long-term risk for major diabetes-related complications. Diabetes Res. Clin. Pract. 2022, 190, 110022. [Google Scholar] [CrossRef] [PubMed]
- Zoungas, S.; for the ADVANCE Collaborative group; Woodward, M.; Li, Q.; Cooper, M.E.; Hamet, P.; Harrap, S.; Heller, S.; Marre, M.; Patel, A.; et al. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia 2014, 57, 2465–2474. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Wu, P.; Zhang, Y.; Lin, Y.; Shen, X.; Zhao, F.; Yan, S. Relationship between onset age of type 2 diabetes mellitus and vascular complications based on propensity score matching analysis. J. Diabetes Investig. 2022, 13, 1062–1072. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.S.; Kim, H.L.; Kim, S.H.; Moon, M.K.; Committee of Clinical Practice Guideline; Korean Diabetes Association and Clinical Practice Guideline Committee; Korean Society of Lipid and Atherosclerosis. lipid management in Korean people with type 2 diabetes mellitus: Korean diabetes association and Korean society of lipid and atherosclerosis consensus statement. J. Lipid Atheroscler. 2023, 12, 12–22. [Google Scholar] [CrossRef] [PubMed]
- The Korean Nutrition Society. Available online: https://www.kns.or.kr/fileroom/FileRoom_view.asp?mode=mod&restring=%252FFileRoom%252FFileRoom%252Easp%253Fxsearch%253D0%253D%253Dxrow%253D10%253D%253DBoardID%253DNq%253D%253Dpage%253D1&idx=103&page=1&BoardID=Nq&xsearch=1&cn_search= (accessed on 19 February 2024).
- Humardani, F.M.; Tanaya, L.T.A.; Mulyanata, L.T.; Kesuma, D.; Wijono, H.; Ikawaty, R.; Putra, S.E.D. The effect of high carbohydrate and high MSG intake on body weight and white adipose tissue. AIP Conf. Proc. 2023, 2606, 30010. [Google Scholar] [CrossRef]
- Martín, P.S.; Fito, M.; Castaner, O. Mediterranean diet effects on type 2 diabetes prevention, disease progression, and related mechanisms. A Review. Nutrients 2020, 12, 2236. [Google Scholar] [CrossRef] [PubMed]
- Sainsbury, E.; Kizirian, N.V.; Partridge, S.R.; Gill, T.; Colagiuri, S.; Gibson, A.A. Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2018, 139, 239–252. [Google Scholar] [CrossRef] [PubMed]
- Razaz, J.M.; Rahmani, J.; Varkaneh, H.K.; Thompson, J.; Clark, C.; Abdulazeem, H.M. The health effects of medical nutrition therapy by dietitians in patients with diabetes: A systematic review and meta-analysis: Nutrition therapy and diabetes. Prim. Care Diabetes. 2019, 13, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare; The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2020; Ministry of Health and Welfare: Sejong, Republic of Korea, 2020. [Google Scholar]
- Beck, R.W.; Bergenstal, R.M.; Cheng, P.; Kollman, C.; Carlson, A.L.; Johnson, M.L.; Rodbard, D. The relationships between time in range, hyperglycemia metrics, and HbA1c. J. Diabetes Sci. Technol. 2019, 13, 614–626. [Google Scholar] [CrossRef] [PubMed]
| Variables | Subjects (n = 40) |
|---|---|
| Gender | |
| Male | 22 (55.0%) |
| Female | 18 (45.0%) |
| Age (yrs) | 61.4 ± 10.4 |
| 40~64 | 22 (55.0%) |
| ≥65 | 18 (45.0%) |
| Married status | |
| Married | 29 (72.5%) |
| Bereavement | 7 (17.5%) |
| Divorce | 3 (7.5%) |
| Unmarried | 1 (2.5%) |
| Education level | |
| Elementary school | 2 (5.0%) |
| Middle school | 2 (5.0%) |
| High school | 13 (32.5%) |
| College | 23 (57.5%) |
| Average duration of DM a (yrs) | 7.1 ± 7.7 |
| Treatment | |
| Insulin | 1 (2.5%) |
| Oral hypoglycemic agent | 20 (50.0%) |
| Insulin + OHA b | 4 (10.0%) |
| Life habit management | 10 (25.0%) |
| Only diet therapy | 5 (12.5%) |
| Complications | |
| Cardiovascular | 1 (2.5%) |
| Retinal | 1 (2.5%) |
| Neurovascular | 1 (2.5%) |
| Hypertension | 2 (5.0%) |
| Smoking | |
| Smoker | 2 (5.0%) |
| Non-smoker | 28 (70.0%) |
| Ex-smoker | 10 (25.0%) |
| Drinking | |
| Drinker | 19 (47.5%) |
| Non-drinker | 15 (37.5%) |
| Ex- drinker | 6 (15.0%) |
| Exercise | |
| Regular | 28 (70.0%) |
| Irregular | 6 (15.0%) |
| None | 6 (15.0%) |
| Variables | Intervention (n = 40) | Control (n = 40) | ||||
|---|---|---|---|---|---|---|
| Pre | Post | p-Value | Pre | Post | p-Value | |
| Cardiovascular risk factors | ||||||
| Weight (kg) | 67.5 ± 13.7 | 67.6 ± 12.8 | 0.716 | 67.2 ± 13.3 | 68.9 ± 13.0 | <0.001 |
| Waist circumference (inch) | 86.7 ± 9.3 | 85.8 ± 9.0 | 0.023 | 86.7 ± 8.7 | 86.4 ± 9.6 | 0.627 |
| Body Fat (%) | 19.0 ± 7.2 | 17.2 ± 6.7 | <0.001 | 18.1 ± 7.1 | 17.6 ± 6.9 | 0.323 |
| Systolic Blood Pressure (mmHg) | 129.6 ± 13.0 | 130.4 ± 13.8 | 0.601 | 126.7 ± 11.5 | 134.5 ± 16.2 | 0.001 |
| Diastolic Blood Pressure (mmHg) | 76.0 ± 9.7 | 76.8 ± 9.3 | 0.363 | 75.5 ± 9.8 | 80.4 ± 10.8 | 0.001 |
| Total cholesterol (mg/dL) | 163.2 ± 33.9 | 157.6 ± 32.5 | 0.056 | 157.0 ± 33.5 | 163.2 ± 30.8 | 0.065 |
| LDL cholesterol (mg/dL) | 111.8 ± 35.0 | 102.5 ± 36.4 | 0.004 | 108.2 ± 34.3 | 114.2 ± 33.7 | 0.034 |
| HDL cholesterol (mg/dL) | 53.6 ± 12.5 | 52.7 ± 14.3 | 0.459 | 53.0 ± 13.3 | 54.9 ± 12.2 | 0.110 |
| Triglyceride (mg/dL) | 190.2 ± 71.2 | 174.7 ± 68.2 | 0.001 | 178.6 ± 80.4 | 184.6 ± 64.6 | 0.349 |
| SMBG a (mg/dL) | 178.1 ± 55.7 | 137.8 ± 22.2 | <0.001 | 183.6 ± 46.2 | 178.1 ± 55.7 | 0.572 |
| Nutritional status factors | ||||||
| Nutritional score | 63.9 ± 12.3 | 64.0 ± 11.8 | 0.897 | 62.4 ± 12.9 | 65.0 ± 11.8 | 0.026 |
| Balance | 52.5 ± 17.6 | 51.9 ± 16.9 | 0.745 | 50.3 ± 17.4 | 52.0 ± 17.4 | 0.283 |
| Moderation | 71.5 ± 14.6 | 73.2 ± 13.7 | 0.271 | 72.8 ± 15.0 | 73.9 ± 14.0 | 0.496 |
| Practice | 66.7 ± 17.2 | 66.1 ± 16.0 | 0.731 | 63.6 ± 17.9 | 68.1 ± 16.2 | 0.021 |
| Variables | Intervention (n = 40) | Control (n = 40) | ||||
|---|---|---|---|---|---|---|
| Pre | Post | p-Value | Pre | Post | p-Value | |
| Energy (kcal) | 1911.2 ± 328.2 | 1867.8 ± 247.0 | 0.506 | 1812.6 ± 382.9 | 1837.8 ± 310.6 | 0.658 |
| Carbohydrate (g) | 262.1 ± 54.0 | 258.6 ± 48.6 | 0.721 | 269.9 ± 45.8 | 266.5 ± 48.1 | 0.670 |
| Sugar (g) | 45.3 ± 11.8 | 40.1 ± 7.1 | 0.005 | 44.7 ± 14.8 | 41.7 ± 13.7 | 0.127 |
| Protein (g) | 89.5 ± 17.2 | 92.1 ± 16.3 | 0.459 | 75.3 ± 25.7 | 74.6 ± 20.4 | 0.857 |
| Fat (g) | 56.0 ± 14.9 | 56.3 ± 11.5 | 0.933 | 44.5 ± 18.1 | 47.5 ± 18.11 | 0.394 |
| Carbohydrate energy ratio (%) | 56.6 ± 4.2 | 53.6 ± 4.1 | 0.007 | 61.0 ± 9.0 | 59.0 ± 8.0 | 0.221 |
| Protein-energy ratio (%) | 18.7 ± 2.5 | 20.5 ± 3.8 | 0.047 | 16.0 ± 3.0 | 16.0 ± 3.0 | 0.587 |
| Fat energy ratio (%) | 24.7 ± 3.4 | 25.4 ± 2.2 | 0.312 | 22.0 ± 6.0 | 23.0 ± 7.0 | 0.365 |
| Variables | Target [17] | Intervention (n = 30) | Control (n = 30) | p-Value |
|---|---|---|---|---|
| Mean glucose (mg/dL) | - | 146.1 ± 28.9 | 157.5 ± 28.0 | 0.127 |
| Target range (70~180 mg/dL, %) | >70% | 80.2 ± 18.5 | 75.4 ± 19.5 | 0.336 |
| Above range (180~250 mg/dL, %) | <25% | 12.1 ± 9.2 | 18.0 ± 12.8 | 0.045 |
| Above range (≥250 mg/dL, %) | <5% | 4.3 ± 7.2 | 6.3 ± 8.7 | 0.342 |
| Mean glucose management indicator (GMI, %) | - | 6.7 ± 0.6 | 7.0 ± 0.7 | 0.100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, D.H.; Han, J.W.; Shin, H.; Lim, H.-S. Tailored Meal-Type Food Provision for Diabetes Patients Can Improve Routine Blood Glucose Management in Patients with Type 2 Diabetes: A Crossover Study. Nutrients 2024, 16, 1190. https://doi.org/10.3390/nu16081190
Jung DH, Han JW, Shin H, Lim H-S. Tailored Meal-Type Food Provision for Diabetes Patients Can Improve Routine Blood Glucose Management in Patients with Type 2 Diabetes: A Crossover Study. Nutrients. 2024; 16(8):1190. https://doi.org/10.3390/nu16081190
Chicago/Turabian StyleJung, Dong Hoon, Jae Won Han, Hyeri Shin, and Hee-Sook Lim. 2024. "Tailored Meal-Type Food Provision for Diabetes Patients Can Improve Routine Blood Glucose Management in Patients with Type 2 Diabetes: A Crossover Study" Nutrients 16, no. 8: 1190. https://doi.org/10.3390/nu16081190
APA StyleJung, D. H., Han, J. W., Shin, H., & Lim, H.-S. (2024). Tailored Meal-Type Food Provision for Diabetes Patients Can Improve Routine Blood Glucose Management in Patients with Type 2 Diabetes: A Crossover Study. Nutrients, 16(8), 1190. https://doi.org/10.3390/nu16081190






