Responsive Feeding Practices to Promote Healthy Diets: A Mixed Method Study among Low-Income Caregivers with Toddlers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Survey Procedures
2.2.1. Responsive Feeding and Conceptual Constructs of Environmental Influences and Child Influences
2.2.2. Intake Patterns for Food Groups to Create Healthy and Less Healthy Scores
2.3. Focus Group Procedures
2.4. Data Analysis
3. Results
3.1. Survey Results
3.1.1. Participant Characteristics
3.1.2. Intake Patterns Compared to Guidelines for Healthy Eating
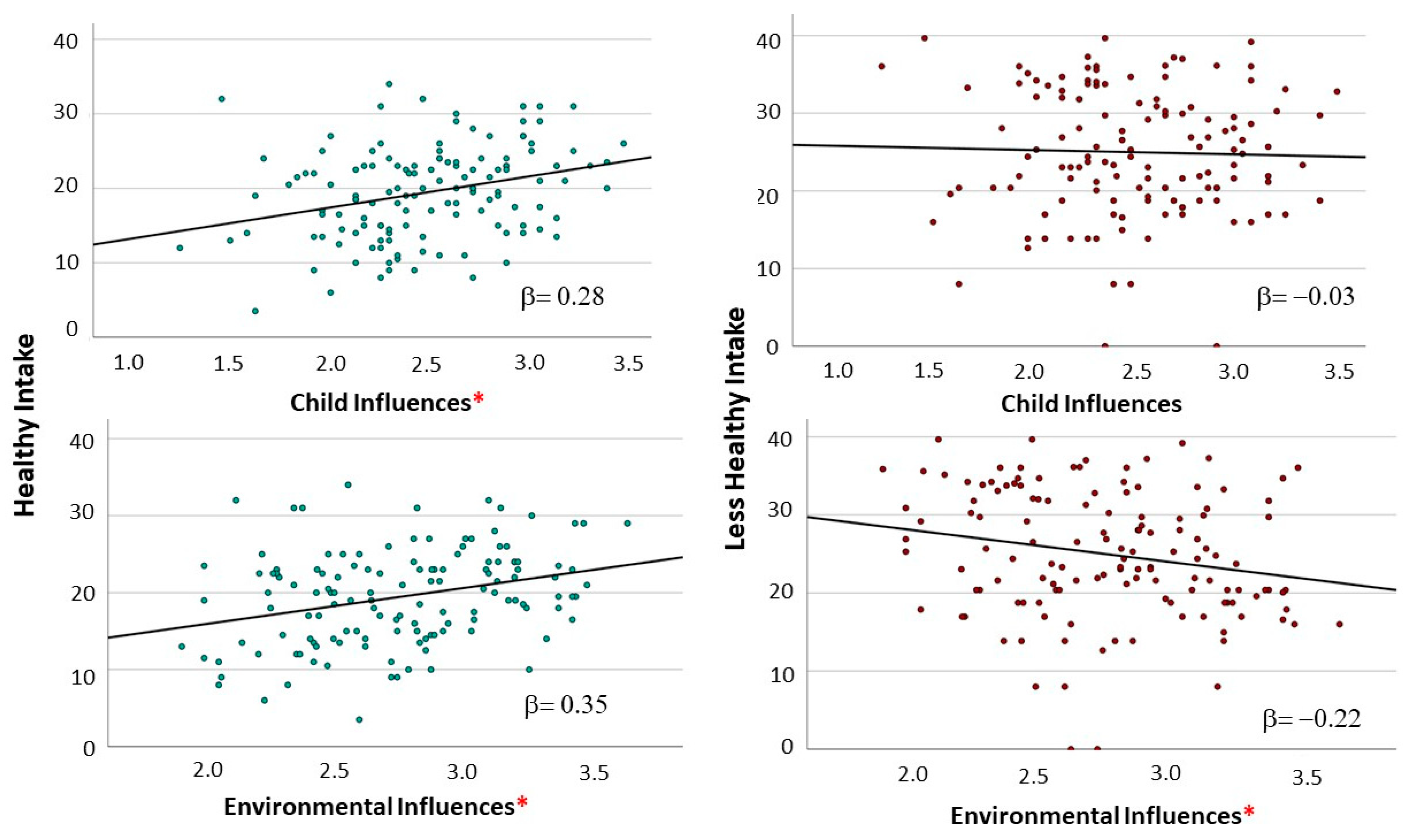
3.1.3. RF Variability and Association with Children’s Dietary Intake
3.2. Focus Group Results
3.2.1. Participants
3.2.2. Focus Group Themes
Lack of Trust in Child Hunger or Fullness Cues
Trust in Child Hunger or Fullness Cues
Using Force and Bribery to Ensure Children Eat Enough and a Variety of Foods
RF-Aligned Strategies to Encourage Children to Eat Non-Preferred Foods
3.3. Integration of Quantitative and Qualitative Findings
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bailey, R.L.; Catellier, D.J.; Jun, S.; Dwyer, J.T.; Jacquier, E.F.; Anater, A.S.; Eldridge, A.L. Total Usual Nutrient Intakes of US Children (Under 48 Months): Findings from the Feeding Infants and Toddlers Study (FITS) 2016. J. Nutr. 2018, 148 (Suppl. 3), 1557S–1566S. [Google Scholar] [CrossRef]
- Thomson, J.L.; Tussing-Humphreys, L.M.; Goodman, M.H.; Landry, A.S. Diet quality in a nationally representative sample of American children by sociodemographic characteristics. Am. J. Clin. Nutr. 2019, 109, 127–138. [Google Scholar] [CrossRef]
- Hennessy, Á.; McCarthy, E.K.; Chaoimh, C.N.; Murray, D.M.; Kiely, M.E. Poor Quality Diets Characterized by Low-Nutrient Density Foods Observed in One-Quarter of 2-Year-Olds in a High Resource Setting. J. Nutr. 2023, 153, 2678–2688. [Google Scholar] [CrossRef] [PubMed]
- Ayling, K.; Li, R.; Muhardi, L.; Melse-Boonstra, A.; Sun, Y.; Chen, W.; Kudla, U. Systematic Literature Review of the Nutrient Status, Intake, and Diet Quality of Chinese Children across Different Age Groups. Nutrients 2023, 15, 1536. [Google Scholar] [CrossRef] [PubMed]
- Koivuniemi, E.; Gustafsson, J.; Mäkelä, I.; Koivisto, V.J.; Vahlberg, T.; Schwab, U.; Niinikoski, H.; Laitinen, K. Parental and Child Factors Associated With 2- to 6-Year-Old Children’s Diet Quality in Finland. J. Acad. Nutr. Diet. 2022, 122, 129–138.e4. [Google Scholar] [CrossRef] [PubMed]
- Pabayo, R.; Spence, J.C.; Casey, L.; Storey, K. Food consumption patterns in preschool children. Can. J. Diet. Pract. Res. 2012, 73, 66–71. [Google Scholar] [CrossRef]
- Welker, E.B.; Jacquier, E.F.; Catellier, D.J.; Anater, A.S.; Story, M.T. Room for Improvement Remains in Food Consumption Patterns of Young Children Aged 2–4 Years. J. Nutr. 2018, 148, 1536s–1546s. [Google Scholar] [CrossRef] [PubMed]
- Olstad, D.L.; Nejatinamini, S.; Victorino, C.; Kirkpatrick, S.I.; Minaker, L.M.; McLaren, L. Trends in Socioeconomic Inequities in Diet Quality between 2004 and 2015 among a Nationally Representative Sample of Children in Canada. J. Nutr. 2021, 151, 3781–3794. [Google Scholar] [CrossRef] [PubMed]
- Jarman, M.; Edwards, K.; Blissett, J. Influences on the dietary intakes of preschool children: A systematic scoping review. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 20. [Google Scholar] [CrossRef]
- Harbron, J.; Booley, S. Responsive feeding: Establishing healthy eating behaviour early on in life. S. Afr. J. Clin. Nutr. 2013, 26, S141–S149. [Google Scholar]
- Pérez-Escamilla, R.; Segura-Pérez, S.; Lott, M. Feeding Guidelines for Infants and Young Toddlers: A Responsive Parenting Approach. Nutr. Today 2017, 52, 223–231. [Google Scholar] [CrossRef]
- Johnson, S.L. Developmental and Environmental Influences on Young Children’s Vegetable Preferences and Consumption. Adv. Nutr. 2016, 7, 220s–231s. [Google Scholar] [CrossRef]
- Holley, C.E.; Farrow, C.; Haycraft, E. A Systematic Review of Methods for Increasing Vegetable Consumption in Early Childhood. Curr. Nutr. Rep. 2017, 6, 157–170. [Google Scholar] [CrossRef]
- Burnett, A.J.; Lacy, K.E.; Russell, C.G.; Spence, A.C.; Worsley, A.; Lamb, K.E. Groups of mothers based on feeding practices and their associations with dietary quality of pre-school children: A latent profile analysis. Appetite 2022, 168, 105754. [Google Scholar] [CrossRef]
- Pérez-Escamilla, R.; Jimenez, E.Y.; Dewey, K.G. Responsive Feeding Recommendations: Harmonizing Integration into Dietary Guidelines for Infants and Young Children. Curr. Dev. Nutr. 2021, 5, nzab076. [Google Scholar] [CrossRef]
- Lim, E.X.; Forde, C.G.; Cheon, B.K. Low subjective socioeconomic status alters taste-based perceptual sensitivity to the energy density of beverages. Physiol. Behav. 2020, 223, 112989. [Google Scholar] [CrossRef]
- Laraia, B.A.; Leak, T.M.; Tester, J.M.; Leung, C.W. Biobehavioral Factors That Shape Nutrition in Low-Income Populations: A Narrative Review. Am. J. Prev. Med. 2017, 52, S118–S126. [Google Scholar] [CrossRef]
- Fisher, J.O.; Hughes, S.O.; Miller, A.L.; Horodynski, M.A.; Brophy-Herb, H.E.; Contreras, D.A.; Kaciroti, N.; Peterson, K.E.; Rosenblum, K.L.; Appugliese, D.; et al. Characteristics of eating behavior profiles among preschoolers with low-income backgrounds: A person-centered analysis. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 91. [Google Scholar] [CrossRef]
- Rummo, P.E.; Guilkey, D.K.; Ng, S.W.; Popkin, B.M.; Evenson, K.R.; Gordon-Larsen, P. Beyond Supermarkets: Food Outlet Location Selection in Four U.S. Cities Over Time. Am. J. Prev. Med. 2017, 52, 300–310. [Google Scholar] [CrossRef]
- Backholer, K.; Gupta, A.; Zorbas, C.; Bennett, R.; Huse, O.; Chung, A.; Isaacs, A.; Golds, G.; Kelly, B.; Peeters, A. Differential exposure to, and potential impact of, unhealthy advertising to children by socio-economic and ethnic groups: A systematic review of the evidence. Obes. Rev. 2021, 22, e13144. [Google Scholar] [CrossRef]
- Heller, R.L.; Chiero, J.D.; Puglisi, M.; Mobley, A.R. Feeding Infants and Toddlers: A Qualitative Study to Determine Parental Education Needs. Child. Obes. 2019, 15, 443–450. [Google Scholar] [CrossRef]
- Rosemond, T.N.; Blake, C.E.; Shapiro, C.J.; Burke, M.P.; Bernal, J.; Adams, E.J.; Frongillo, E.A. Disrupted Relationships, Chaos, and Altered Family Meals in Food-Insecure Households: Experiences of Caregivers and Children. J. Acad. Nutr. Diet. 2019, 119, 1644–1652. [Google Scholar] [CrossRef] [PubMed]
- Schuster, R.C.; Szpak, M.; Klein, E.; Sklar, K.; Dickin, K.L. “I try, I do”: Child feeding practices of motivated, low-income parents reflect trade-offs between psychosocial- and nutrition-oriented goals. Appetite 2019, 136, 114–123. [Google Scholar] [CrossRef]
- Agrawal, T.; Farrell, T.J.; Wethington, E.; Devine, C.M. Change and Continuity in Low-Income Working Mothers’ Food Practices for Young Children in Response to Life Events. Matern. Child Health J. 2019, 23, 1206–1212. [Google Scholar] [CrossRef]
- Beck, A.L.; Takayama, J.I.; Halpern-Felsher, B.; Badiner, N.; Barker, J.C. Understanding how Latino parents choose beverages to serve to infants and toddlers. Matern. Child Health J. 2014, 18, 1308–1315. [Google Scholar] [CrossRef]
- Savage, J.S.; Neshteruk, C.D.; Balantekin, K.N.; Birch, L.L. Low-Income Women’s Feeding Practices and Perceptions of Dietary Guidance: A Qualitative Study. Matern. Child Health J. 2016, 20, 2510–2517. [Google Scholar] [CrossRef]
- Choi, Y.Y.; Ludwig, A.; Harris, J.L. US toddler milk sales and associations with marketing practices. Public Health Nutr. 2020, 23, 1127–1135. [Google Scholar] [CrossRef] [PubMed]
- Romo-Palafox, M.; Pomeranz, J.L.; Harris, J.L. Infant formula and toddler milk marketing and caregiver’s provision to young children. Matern. Child Nutr. 2020, 16, e12962. [Google Scholar] [CrossRef]
- Harris, J.L.; Romo-Palafox, M.J.; Gershman, H.; Kagan, I.; Duffy, V. Healthy Snacks and Drinks for Toddlers: A Qualitative Study of Caregivers’ Understanding of Expert Recommendations and Perceived Barriers to Adherence. Nutrients 2023, 15, 1006. [Google Scholar] [CrossRef]
- Wasti, S.P.; Simkhada, P.; van Teijlingen, E.; Sathian, B.; Banerjee, I. The Growing Importance of Mixed-Methods Research in Health. Nepal J. Epidemiol. 2022, 12, 1175–1178. [Google Scholar] [CrossRef] [PubMed]
- McCrudden, M.T.; Marchand, G.; Schutz, P.A. Joint displays for mixed methods research in psychology. Methods Psychol. 2021, 5, 100067. [Google Scholar] [CrossRef]
- Creswell, J.W. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 4th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans 2020–2025; U.S. Department of Agriculture; U.S. Department of Health and Human Services: Washington, DC, USA, 2020.
- Fisher, J.; Lumeng, J.; Tovar, A.; Mendoza, J.A.; Berge, J.; Davison, K.K.; Rhee, K.; Francis, L.A.; Black, M.M.; Baskin, M.L.; et al. Evidence-Based Recommendations and Best Practices for Promoting Healthy Eating Behaviors in Children 2 to 8 Years; Healthy Eating Research: Durham, NC, USA, 2021. [Google Scholar]
- Fenn, L. The Development of an Online Survey and Screening Tool to Assess Toddler Feeding Behaviors in a Low-Income Connecticut Community. Master’s Thesis, University of Connecticut, Storrs, CT, USA, 2019. [Google Scholar]
- U.S. Census Bureau. QuickFacts. Available online: https://www.census.gov/quickfacts/ (accessed on 11 September 2023).
- Hager, E.R.; Quigg, A.M.; Black, M.M.; Coleman, S.M.; Heeren, T.; Rose-Jacobs, R.; Cook, J.T.; De Cuba, S.A.E.; Casey, P.H.; Chilton, M.; et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010, 126, 26. [Google Scholar] [CrossRef]
- Black, M.M.; Aboud, F.E. Responsive feeding is embedded in a theoretical framework of responsive parenting. J. Nutr. 2011, 141, 490–494. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Weinfield, N.S.; Borger, C.; Gola, A.A. Breastfeeding Duration in a Low-Income Sample Is Associated With Child Diet Quality at Age Three. J. Hum. Lact. 2021, 37, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Au, L.E.; Gurzo, K.; Paolicelli, C.; Whaley, S.E.; Weinfield, N.S.; Ritchie, L.D. Diet Quality of US Infants and Toddlers 7–24 Months Old in the WIC Infant and Toddler Feeding Practices Study-2. J. Nutr. 2018, 148, 1786–1793. [Google Scholar] [CrossRef] [PubMed]
- Jun, S.; E Cowan, A.; Dodd, K.W.; A Tooze, J.; Gahche, J.J.; A Eicher-Miller, H.; Guenther, P.M.; Dwyer, J.T.; Potischman, N.; Bhadra, A.; et al. Association of food insecurity with dietary intakes and nutritional biomarkers among US children, National Health and Nutrition Examination Survey (NHANES) 2011–2016. Am. J. Clin. Nutr. 2021, 114, 1059–1069. [Google Scholar] [CrossRef] [PubMed]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Pearson/Allyn & Bacon: Boston, MA, USA, 2007. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Machuca, H.; Arevalo, S.; Hackley, B.; Applebaum, J.; Mishkin, A.; Heo, M.; Shapiro, A. Well Baby Group Care: Evaluation of a Promising Intervention for Primary Obesity Prevention in Toddlers. Child. Obes. 2016, 12, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Tovar, A.; Fox, K.; Gans, K.M.; Risica, P.M.; Papandonatos, G.D.; Ramirez, A.; Gorin, A.A.; von Ash, T.; Jennings, E.; Bouchard, K.; et al. Results from the Strong Families Start at Home/Familias Fuertes Comienzan en Casa: Feasibility randomised control trial to improve the diet quality of low-income, predominantly Hispanic/Latinx children. Public Health Nutr. 2023, 26, 890–904. [Google Scholar] [CrossRef] [PubMed]
- Nix, R.L.; Francis, L.A.; Feinberg, M.E.; Gill, S.; Jones, D.E.; Hostetler, M.L.; Stifter, C.A. Improving Toddlers’ Healthy Eating Habits and Self-regulation: A Randomized Controlled Trial. Pediatrics 2021, 147, e20193326. [Google Scholar] [CrossRef]
- Redsell, S.A.; Slater, V.; Rose, J.; Olander, E.K.; Matvienko-Sikar, K. Barriers and enablers to caregivers’ responsive feeding behaviour: A systematic review to inform childhood obesity prevention. Obes. Rev. 2021, 22, e13228. [Google Scholar] [CrossRef]
- McCann, J.R.; Russell, C.G.; Woods, J.L. The Nutritional Profile and On-Pack Marketing of Toddler-Specific Food Products Launched in Australia between 1996 and 2020. Nutrients 2021, 14, 163. [Google Scholar] [CrossRef]
- Chau, S.; Oldman, S.; Smith, S.R.; Lin, C.A.; Ali, S.; Duffy, V.B. Online Behavioral Screener with Tailored Obesity Prevention Messages: Application to a Pediatric Clinical Setting. Nutrients 2021, 13, 223. [Google Scholar] [CrossRef] [PubMed]
- Heller, R.L.; Mobley, A.R. Development and Qualitative Pretesting of Child Feeding and Obesity Prevention Messages for Parents of Infants and Toddlers. J. Acad. Nutr. Diet. 2021, 121, 1528–1541.e1. [Google Scholar] [CrossRef] [PubMed]
- Mennella, J.A.; Reiter, A.R.; Daniels, L.M. Vegetable and Fruit Acceptance during Infancy: Impact of Ontogeny, Genetics, and Early Experiences. Adv. Nutr. 2016, 7, 211S–219S. [Google Scholar] [CrossRef] [PubMed]
- Goodell, L.S.; Johnson, S.L.; Antono, A.C.; Power, T.G.; Hughes, S.O. Strategies Low-Income Parents Use to Overcome Their Children’s Food Refusal. Matern. Child Health J. 2017, 21, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Harris, H.A.; Ria-Searle, B.; Jansen, E.; Thorpe, K. What’s the fuss about? Parent presentations of fussy eating to a parenting support helpline. Public Health Nutr. 2018, 21, 1520–1528. [Google Scholar] [CrossRef] [PubMed]
- Frankel, L.A.; Hughes, S.O.; Teresia, M.; O’Connor, T.M.; Power, T.G.; Fisher, J.O.; Hazen, N.L. Parental Influences on Children’s Self-Regulation of Energy Intake: Insights from Developmental Literature on Emotion Regulation. J. Obes. 2012, 2012, 327259. [Google Scholar] [CrossRef]
- Daniel, C. Economic constraints on taste formation and the true cost of healthy eating. Soc. Sci. Med. 2016, 148, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.C.; Momin, S.; Senn, M.; Hughes, S.O. Pediatric Eating Behaviors as the Intersection of Biology and Parenting: Lessons from the Birds and the Bees. Curr. Nutr. Rep. 2018, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.L.; Rosenblum, K.L.; Retzloff, L.B.; Lumeng, J.C. Observed Self-Regulation is Associated with Weight in Low-Income Toddlers. Appetite 2016, 105, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.L.; Doub, A.E. Learning to eat: Birth to age 2 y. Am. J. Clin. Nutr. 2014, 99, 723S–728S. [Google Scholar] [CrossRef] [PubMed]
- Power, T.G.; Hughes, S.O.; Goodell, L.S.; Johnson, S.L.; Duran, J.A.J.; Williams, K.; Beck, A.D. Feeding practices of low-income mothers: How do they compare to current recommendations? Int. J. Behav. Nutr. Phys. Act. 2015, 12, 34. [Google Scholar] [CrossRef] [PubMed]
- Gross, R.S.; Fierman, A.H.; Mendelsohn, A.L.; Chiasson, M.A.; Rosenberg, T.J.; Scheinmann, R.; Messito, M.J. Maternal perceptions of infant hunger, satiety, and pressuring feeding styles in an urban Latina WIC population. Acad. Pediatr. 2010, 10, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Seguin, R.A.; Aggarwal, A.; Vermeylen, F.; Drewnowski, A. Consumption Frequency of Foods Away from Home Linked with Higher Body Mass Index and Lower Fruit and Vegetable Intake among Adults: A Cross-Sectional Study. J. Environ. Public Health 2016, 2016, 3074241. [Google Scholar] [CrossRef] [PubMed]
- Pineros-Leano, M.; Tabb, K.; Liechty, J.; Castañeda, Y.; Williams, M. Feeding decision-making among first generation Latinas living in non-metropolitan and small metro areas. PLoS ONE 2019, 14, e0213442. [Google Scholar] [CrossRef] [PubMed]
- Savage, J.S.; Ruggiero, C.F.; Eagleton, S.G.; Marini, M.E.; Harris, H.A. The feeding to Manage Child Behavior Questionnaire: Development of a tool to measure’ non-nutritive feeding practices in low income families with preschool-aged children. Appetite 2022, 169, 105849. [Google Scholar] [CrossRef]
- Killion, K.; Harris, J.L.; Duffy, V.B. Caregiver perceptions of snacks for young children: A thematic synthesis of qualitative research. Appetite 2023, 188, 106628. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Agosti, M. Nutrition in the First 1000 Days: Ten Practices to Minimize Obesity Emerging from Published Science. Int. J. Environ. Res. Public Health 2017, 14, 1491. [Google Scholar] [CrossRef]
- Powell, E.M.; Frankel, L.A.; Hernandez, D.C. The mediating role of child self-regulation of eating in the relationship between parental use of food as a reward and child emotional overeating. Appetite 2017, 113, 78–83. [Google Scholar] [CrossRef]
- Verhage, C.L.; Gillebaart, M.; van der Veek, S.M.; Vereijken, C.M. The relation between family meals and health of infants and toddlers: A review. Appetite 2018, 127, 97–109. [Google Scholar] [CrossRef]
- Avery, A.; Anderson, C.; McCullough, F. Associations between children’s diet quality and watching television during meal or snack consumption: A systematic review. Matern. Child Nutr. 2017, 13, e12428. [Google Scholar] [CrossRef] [PubMed]
- Cox, R.; Skouteris, H.; Rutherford, L.; Fuller-Tyszkiewicz, M.; Dell, D.; Hardy, L.L. Television viewing, television content, food intake, physical activity and body mass index: A cross-sectional study of preschool children aged 2–6 years. Health Promot. J. Aust. 2012, 23, 58–62. [Google Scholar] [CrossRef]
- Domingues-Montanari, S. Clinical and psychological effects of excessive screen time on children. J. Paediatr. Child Health 2017, 53, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Dubois, L.; Farmer, A.; Girard, M.; Peterson, K. Social factors and television use during meals and snacks is associated with higher BMI among pre-school children. Public Health Nutr. 2008, 11, 1267–1279. [Google Scholar] [CrossRef] [PubMed]
- Duch, H.; Fisher, E.M.; Ensari, I.; Harrington, A. Screen time use in children under 3 years old: A systematic review of correlates. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 102. [Google Scholar] [CrossRef]
- Jensen, M.L.; Carpentier, F.R.D.; Corvalán, C.; Popkin, B.M.; Evenson, K.R.; Adair, L.; Taillie, L.S. Television viewing and using screens while eating: Associations with dietary intake in children and adolescents. Appetite 2022, 168, 105670. [Google Scholar] [CrossRef]
- Trofholz, A.C.; Tate, A.; Loth, K.; Neumark-Sztainer, D.; Berge, J.M. Watching Television while Eating: Associations with Dietary Intake and Weight Status among a Diverse Sample of Young Children. J. Acad. Nutr. Diet. 2019, 119, 1462–1469. [Google Scholar] [CrossRef]
- Mena, N.Z.; Gorman, K.; Dickin, K.; Greene, G.; Tovar, A. Contextual and Cultural Influences on Parental Feeding Practices and Involvement in Child Care Centers among Hispanic Parents. Child. Obes. 2015, 11, 347–354. [Google Scholar] [CrossRef]
- Heller, R.L.; Mobley, A.R. Instruments assessing parental responsive feeding in children ages birth to 5 years: A systematic review. Appetite 2019, 138, 23–51. [Google Scholar] [CrossRef]
- DiSantis, K.I.; A Hodges, E.; Johnson, S.L.; O Fisher, J. The role of responsive feeding in overweight during infancy and toddlerhood: A systematic review. Int. J. Obes. 2011, 35, 480–492. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, A.E.; Ward, D.S.; Fisher, J.O.; Faith, M.S.; Hughes, S.O.; Kremers, S.P.; Musher-Eizenman, D.R.; O’connor, T.M.; Patrick, H.; Power, T.G. Fundamental constructs in food parenting practices: A content map to guide future research. Nutr. Rev. 2016, 74, 98–117. [Google Scholar] [CrossRef] [PubMed]
- Bentley, M.E.; Wasser, H.M.; Creed-Kanashiro, H.M. Responsive feeding and child undernutrition in low- and middle-income countries. J. Nutr. 2011, 141, 502–507. [Google Scholar] [CrossRef] [PubMed]
| Conceptual Group | Survey Questions 1 |
|---|---|
| Environmental Influences | |
| Meal Environment |
|
| Food Offered and Caregiver Modeling |
|
| Caregiver Nutrition Beliefs |
|
| Child Influences | |
| Child Self-Regulation of Intake |
|
| Child Hunger and Satiety Cues |
|
| Food for Reward or Behavior |
|
| Child Food Acceptance |
|
| n (%) | |
|---|---|
| Household | |
| Number of children in home | |
| 1 | 41 (30.6) |
| 2 | 44 (32.8) |
| 3 | 24 (17.9) |
| 4 | 19 (14.2) |
| 5+ | 6 (4.5) |
| Number of children between 12 and 36 months | |
| 1 | 123 (91.8) |
| 2+ | 11 (8.2) |
| Food security | |
| Food Secure | 99 (73.9) |
| Food Insecure | 35 (26.1) |
| Participation in food assistance programs | |
| WIC | 111 (82.8) |
| SNAP | 66 (49.3) |
| Mobile food pantry | 14 (10.5) |
| Food pantry | 22 (16.4) |
| Caregiver | |
| Age (years) | |
| 18–24 | 16 (11.9) |
| 25–34 | 78 (58.2) |
| 35–44 | 33 (24.7) |
| 45+ | 7 (5.2) |
| Gender | |
| Male | 10 (7.5) |
| Female | 124 (92.5) |
| Other | 0 (0) |
| Race/ethnicity | |
| White | 26 (19.4) |
| Black/African American | 36 (26.9) |
| Hispanic/Latino | 43 (32.1) |
| American Indian/Alaska Native | 1 (0.7) |
| Asian/Pacific Islander | 5 (3.7) |
| More than one race/ethnicity | 19 (14.2) |
| Other | 4 (3.0) |
| Education | |
| Less than high school | 10 (7.4) |
| High school/GED | 35 (26.1) |
| Some college or trade school | 37 (27.6) |
| 2-year college | 17 (12.7) |
| 4-year college | 23 (17.2) |
| Master’s degree or higher | 12 (9.0) |
| Sampled Child 12–36 Months | |
| Age (months), Average (SD) | 22.8 (7.3) |
| Gender | |
| Male | 70 (52.2) |
| Female | 64 (47.8) |
| Other | 0 (0.0) |
| Race/ethnicity | |
| White | 17 (12.7) |
| Black/African American | 39 (29.1) |
| Hispanic/Latino | 36 (26.9) |
| American Indian/Alaska Native | 0 (0.0) |
| Asian/Pacific Islander | 3 (2.2) |
| More than one race/ethnicity | 36 (26.9) |
| Other | 3 (2.2) |
| Fruit | Vegetables | Juice | Sweetened | Snack Foods | Fast Food | |
|---|---|---|---|---|---|---|
| Beverages | ||||||
| None | 1 | 2 | 23 | 60 | 4 | 73 |
| (0.7%) | (1.5%) | (17.2%) | (44.8%) | (3.0%) | (54.5%) | |
| 1–2 times/week | 11 | 18 | 33 | 35 | 84 | 61 |
| (8.2%) | (13.4%) | (24.6%) | (26.1%) | (62.7%) | (45.5%) | |
| 3–4 times/week | 26 | 32 | 24 | 16 | 46 | |
| (19.4%) | (23.9%) | (17.9%) | (11.9%) | (34.3%) | ||
| 5–6 times/week | 19 | 20 | 14 | 8 | ||
| (14.2%) | (14.9%) | (10.4%) | (6.0%) | |||
| Daily | 77 | 62 | 40 | 15 | ||
| (57.5%) | (46.3%) | (29.9%) | (11.2%) |
| Theme | Quote |
|---|---|
| Lack of trust in child hunger or fullness cues | “Because they just keep eating. And they don’t know when to stop. And you can see her belly’s so full and you’re like, you need to stop eating. That’s not good. I don’t think they know”. “They see it there, they just keep eating. They see it there, they’ll just keep eating. Just keep eating and eating”. “Sometimes I feel like throughout today my granddaughter doesn’t get enough because either she doesn’t like it or she’s busy and she wants to play”. |
| Trust in child hunger or fullness cues | “She seems to know how much she wants to eat, because I can give her a little bag of snacks that I have in the bag and she will not eat it all. She knows automatically when she’s had enough”. “But if she doesn’t ask me to eat, I don’t give her anything. I don’t know, does that sound bad? But I figure, if she’s hungry, she’ll tell me. She’s old enough to”. “I think after a while, you feed them, you know how much they’re going to eat. You know what I’m trying to say? So if I know—if I have a piece of chicken and I’m cutting it up for her, I cut her just so much. And I know that’s what she’s going to eat”. |
| Using force and bribery to ensure children eat enough and a variety of foods | “And then we bribe her sometimes. We tell her, OK. You have two—not bribe her, but say, OK. You have to eat two more pieces of meat before you can have the mashed potatoes. And it usually works”. “So sometimes I go, and I’m like, [child name], you know, Mommy pays so much money for all this food. You have to eat. Eat so you be like Mommy. You’ll be big like Mommy”. “When they go to eat, they do not want to eat, then I take the tablet. And I tell you, until you eat you will not use the tablet”. “I could get them to do anything for a graham cracker and some fishies”. |
| RF-aligned strategies to encourage children to eat non-preferred foods | “I do try to schedule the meals and snacks. And the reason I do that is because I don’t want her to be hungry when I’m tied up doing something else” “So she’s sing all these little things. I’ll say ‘Try something new.’ We’ll do the little song, and then she’ll try it. And if she doesn’t like it, she doesn’t like it”. “What I heard about teaching children to eat more vegetables. Even if they don’t like it, you don’t force it. But you give them a small serving on their plate and they see you eat it. And then it takes a certain amount of time before they try it or what have you. I am desperately trying that”. “They won’t eat just plain broccoli, or they won’t eat just plain corn. They like their corn and their rice mixed in with stuff, like that. They’ll eat it like that”. |
| Quantitative Results | Qualitative Results | Exemplar Quote |
|---|---|---|
| Child influences score positively associated with healthy intake | Lack of trust in child hunger or fullness cues | “And she says sometimes she doesn’t want to finish it all. But sometimes she prefers—I see she prefers rice than the vegetables. And I say, OK. You can leave the rice, but eat the vegetables”. |
| Trust in child hunger or fullness cues | “He did not eat though, let’s say, for breakfast, so I give him fruits or something. I don’t force him”. | |
| Environmental influences score positively associated with healthy intake | RF-aligned strategies to encourage children to eat non-preferred foods | “Because I put the snacks always in the bag—a little bag for her. Like grapes, strawberries, carrots. The little baby carrots. And oranges in little pieces. So she has many choices”. “She likes the pasta. And sometimes when I give her pasta, I just put the sauce—homemade sauce. Not only tomato. I mix meat with vegetables and then put it on the top of the pasta”. |
| Environmental influences score negatively associated with less healthy intake | Using force and bribery to ensure children eat enough and a variety of foods | “One thing that I have failed on with her is because she’s so sweet tooth addicted that I say—and I have done this and I have to find a way to stop—is that I say if you eat your healthy dinner, you can have a bowl of ice cream”. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Killion, K.E.; Corcoran, A.; Romo-Palafox, M.J.; Harris, J.L.; Kagan, I.; Gilbert, L.; Duffy, V.B. Responsive Feeding Practices to Promote Healthy Diets: A Mixed Method Study among Low-Income Caregivers with Toddlers. Nutrients 2024, 16, 863. https://doi.org/10.3390/nu16060863
Killion KE, Corcoran A, Romo-Palafox MJ, Harris JL, Kagan I, Gilbert L, Duffy VB. Responsive Feeding Practices to Promote Healthy Diets: A Mixed Method Study among Low-Income Caregivers with Toddlers. Nutrients. 2024; 16(6):863. https://doi.org/10.3390/nu16060863
Chicago/Turabian StyleKillion, Kate E., Amy Corcoran, Maria J. Romo-Palafox, Jennifer L. Harris, Inna Kagan, Laura Gilbert, and Valerie B. Duffy. 2024. "Responsive Feeding Practices to Promote Healthy Diets: A Mixed Method Study among Low-Income Caregivers with Toddlers" Nutrients 16, no. 6: 863. https://doi.org/10.3390/nu16060863
APA StyleKillion, K. E., Corcoran, A., Romo-Palafox, M. J., Harris, J. L., Kagan, I., Gilbert, L., & Duffy, V. B. (2024). Responsive Feeding Practices to Promote Healthy Diets: A Mixed Method Study among Low-Income Caregivers with Toddlers. Nutrients, 16(6), 863. https://doi.org/10.3390/nu16060863







