The Cerebellar Response to Visual Portion Size Cues Is Associated with the Portion Size Effect in Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
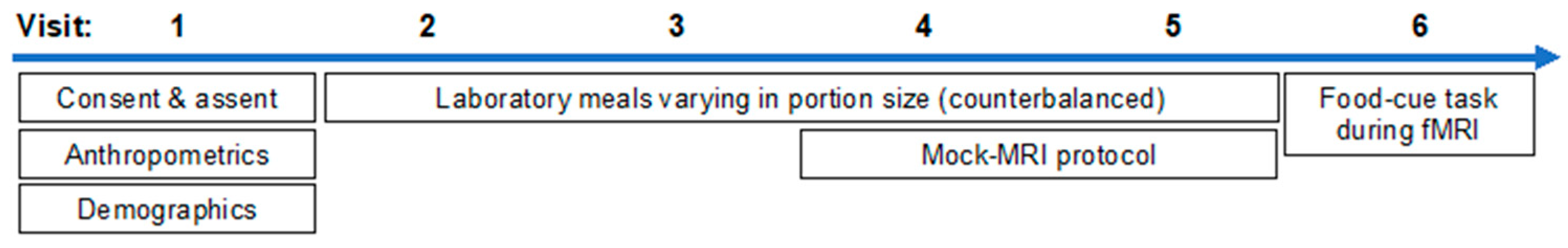
2.2. Data Collection
2.2.1. Demographics
2.2.2. Anthropometrics
2.2.3. Laboratory Portion Size Meals
2.2.4. Mock-MRI Protocol
2.2.5. fMRI Visit Protocol
2.2.6. MRI Data Acquisition
2.2.7. Food-Cue Task
2.3. fMRI Data Processing
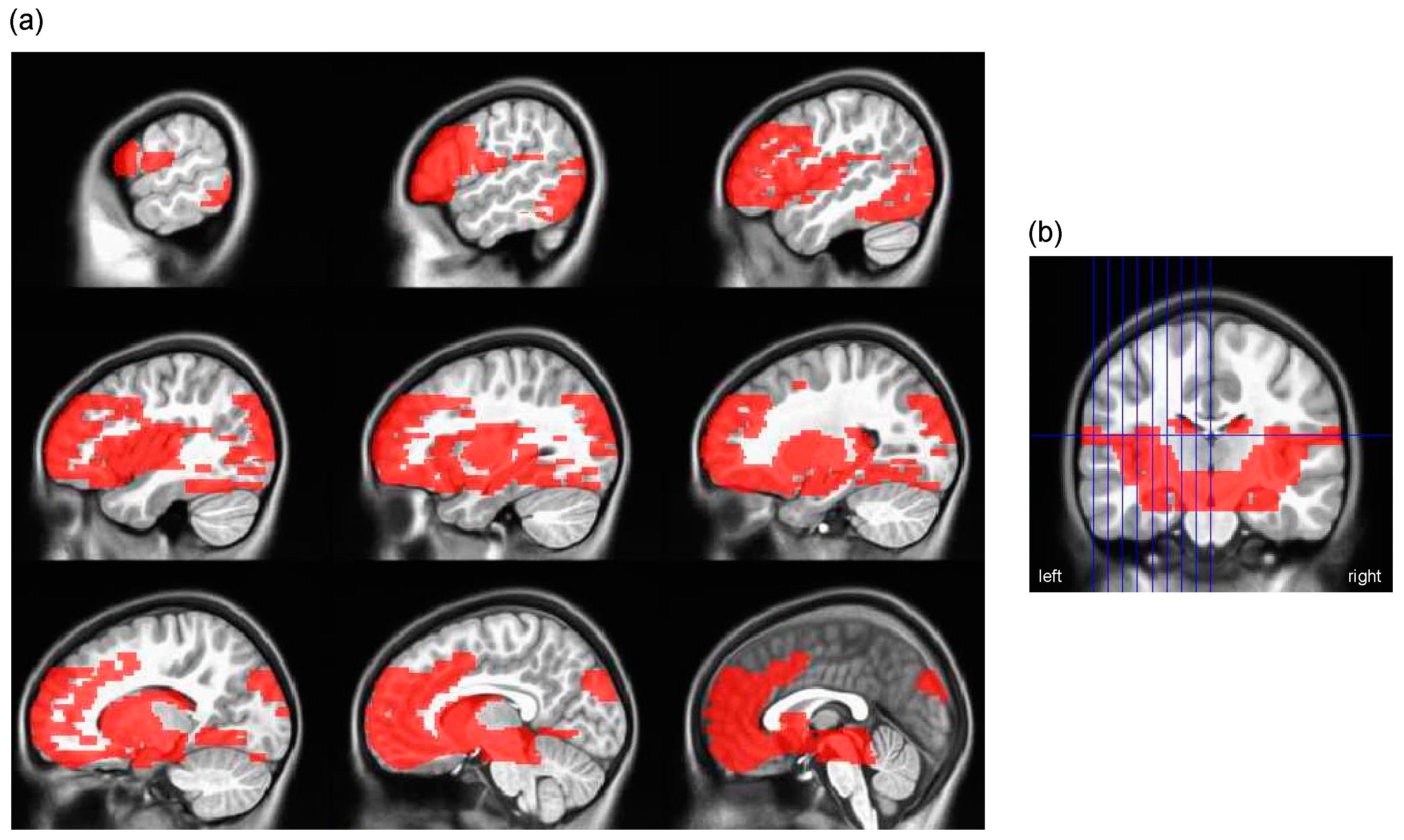
2.3.1. Masks
2.4. Group-Level Analyses
2.4.1. Analysis Sample
2.4.2. Estimation of Individual-Level Portion Size Slopes
2.4.3. Descriptive Statistics
2.4.4. Wanting Responses during the Food-Cue Task
2.4.5. Neural Responses to Portion Size and the PSE
3. Results
3.1. Participant Characteristics
3.2. Child-Specific Portion Size Curves
3.3. Behavioral Responses during the Food-Cue Task
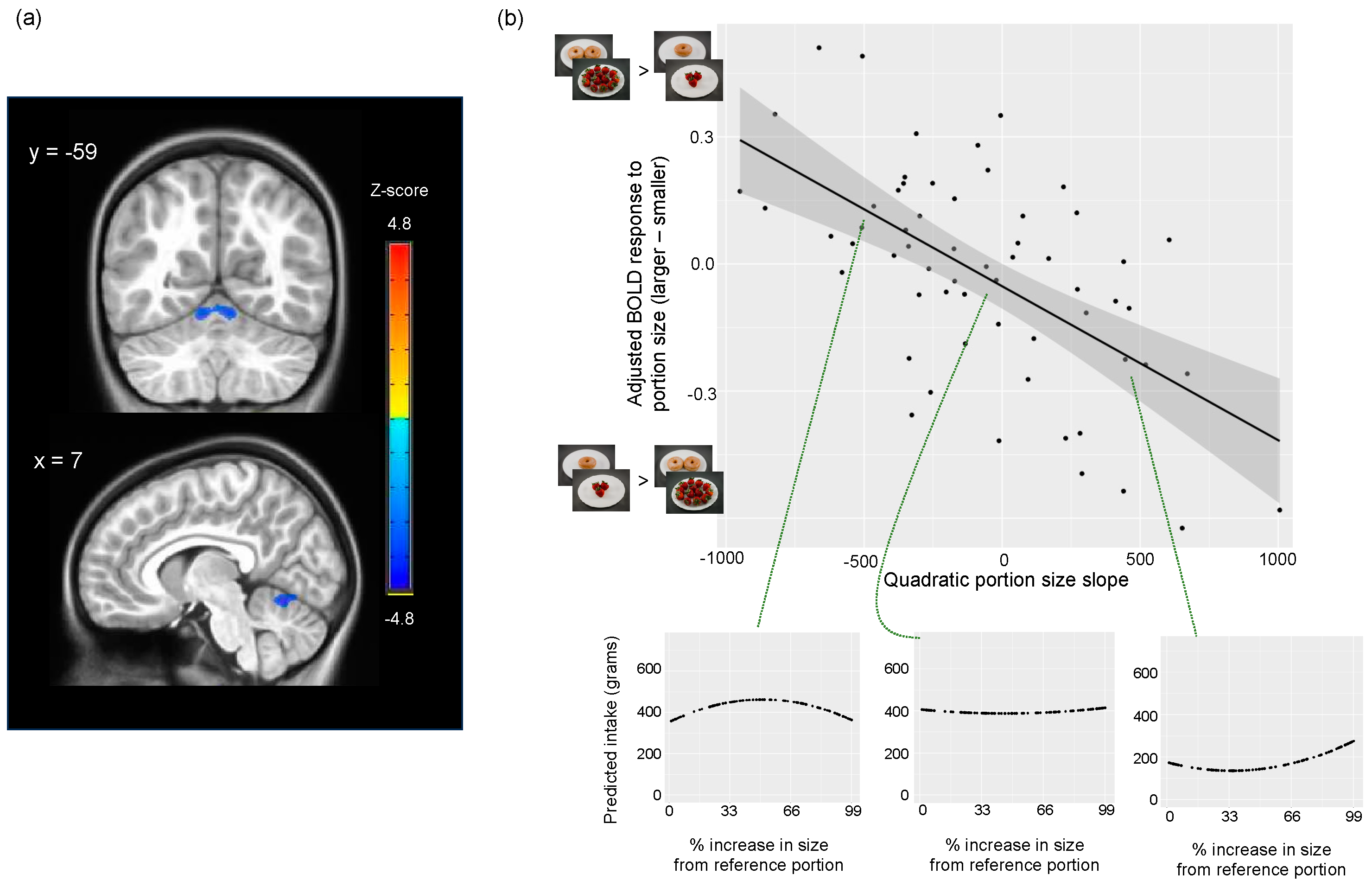
3.4. Associations between Neural Responses to Portion Size and the PSE
3.4.1. Appetitive Network Mask
3.4.2. Cerebellum Mask
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reale, S.; Hamilton, J.; Akparibo, R.; Hetherington, M.M.; Cecil, J.E.; Caton, S.J. The Effect of Food Type on the Portion Size Effect in Children Aged 2–12 Years: A Systematic Review and Meta-Analysis. Appetite 2019, 137, 47–61. [Google Scholar] [CrossRef]
- Diliberti, N.; Bordi, P.L.; Conklin, M.T.; Roe, L.S.; Rolls, B.J. Increased Portion Size Leads to Increased Energy Intake in a Restaurant Meal. Obes. Res. 2004, 12, 562–568. [Google Scholar] [CrossRef]
- Gough, T.; Haynes, A.; Clarke, K.; Hansell, A.; Kaimkhani, M.; Price, B.; Roberts, A.; Hardman, C.A.; Robinson, E. Out of the Lab and into the Wild: The Influence of Portion Size on Food Intake in Laboratory vs. Real-World Settings. Appetite 2021, 162, 105160. [Google Scholar] [CrossRef]
- Wood, C.T.; Skinner, A.C.; Yin, H.S.; Rothman, R.L.; Sanders, L.M.; Delamater, A.; Ravanbakht, S.N.; Perrin, E.M. Association Between Bottle Size and Formula Intake in 2 Month Old Infants. Acad. Pediatr. 2016, 16, 254–259. [Google Scholar] [CrossRef]
- Smethers, A.D.; Roe, L.S.; Sanchez, C.E.; Zuraikat, F.M.; Keller, K.L.; Kling, S.M.R.; Rolls, B.J. Portion Size Has Sustained Effects over 5 Days in Preschool Children: A Randomized Trial. Am. J. Clin. Nutr. 2019, 109, 1361–1372. [Google Scholar] [CrossRef]
- Han, J.C.; Rutledge, M.S.; Kozlosky, M.; Salaita, C.G.; Gustafson, J.K.; Keil, M.F.; Fleisch, A.F.; Roberts, M.D.; Ning, C.; Yanovski, J.A. Insulin Resistance, Hyperinsulinemia, and Energy Intake in Overweight Children. J. Pediatr. 2008, 152, 612–617.e1. [Google Scholar] [CrossRef]
- Romieu, I.; Dossus, L.; Barquera, S.; Blottière, H.M.; Franks, P.W.; Gunter, M.; Hwalla, N.; Hursting, S.D.; Leitzmann, M.; Margetts, B.; et al. Energy Balance and Obesity: What Are the Main Drivers? Cancer Causes Control 2017, 28, 247–258. [Google Scholar] [CrossRef]
- Berthoud, H.-R.; Münzberg, H.; Morrison, C.D. Blaming the Brain for Obesity: Integration of Hedonic and Homeostatic Mechanisms. Gastroenterology 2017, 152, 1728–1738. [Google Scholar] [CrossRef] [PubMed]
- Berthoud, H.-R.; Morrison, C. The Brain, Appetite, and Obesity. Annu. Rev. Psychol. 2008, 59, 55–92. [Google Scholar] [CrossRef]
- Dagher, A. Functional Brain Imaging of Appetite. Trends Endocrinol. Metab. 2012, 23, 250–260. [Google Scholar] [CrossRef]
- Giuliani, N.R.; Merchant, J.S.; Cosme, D.; Berkman, E.T. Neural Predictors of Eating Behavior and Dietary Change. Ann. N. Y. Acad. Sci. 2018, 1428, 208–220. [Google Scholar] [CrossRef] [PubMed]
- van Meer, F.; van der Laan, L.N.; Adan, R.A.H.; Viergever, M.A.; Smeets, P.A.M. What You See Is What You Eat: An ALE Meta-Analysis of the Neural Correlates of Food Viewing in Children and Adolescents. NeuroImage 2015, 104, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Masterson, T.D.; Stein, W.M.; Beidler, E.; Bermudez, M.; English, L.K.; Keller, K.L. Brain Response to Food Brands Correlates with Increased Intake from Branded Meals in Children: An fMRI Study. Brain Imaging Behav. 2019, 13, 1035–1048. [Google Scholar] [CrossRef] [PubMed]
- Keller, K.L.; English, L.K.; Fearnbach, S.N.; Lasschuijt, M.; Anderson, K.; Bermudez, M.; Fisher, J.O.; Rolls, B.J.; Wilson, S.J. Brain Response to Food Cues Varying in Portion Size Is Associated with Individual Differences in the Portion Size Effect in Children. Appetite 2018, 125, 139–151. [Google Scholar] [CrossRef]
- Cornier, M.-A.; Salzberg, A.K.; Endly, D.C.; Bessesen, D.H.; Tregellas, J.R. Sex-Based Differences in the Behavioral and Neuronal Responses to Food. Physiol. Behav. 2010, 99, 538–543. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Koike, S. Daily Fat Intake Is Associated with Basolateral Amygdala Response to High-Calorie Food Cues and Appetite for High-Calorie Food. Nutr. Neurosci. 2023, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Frankort, A.; Roefs, A.; Siep, N.; Roebroeck, A.; Havermans, R.; Jansen, A. Neural Predictors of Chocolate Intake Following Chocolate Exposure. Appetite 2015, 87, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Grodd, W.; Hülsmann, E.; Lotze, M.; Wildgruber, D.; Erb, M. Sensorimotor Mapping of the Human Cerebellum: fMRI Evidence of Somatotopic Organization. Hum. Brain Mapp. 2001, 13, 55–73. [Google Scholar] [CrossRef]
- Wagner, M.J.; Kim, T.H.; Savall, J.; Schnitzer, M.J.; Luo, L. Cerebellar Granule Cells Encode the Expectation of Reward. Nature 2017, 544, 96–100. [Google Scholar] [CrossRef]
- Kostadinov, D.; Häusser, M. Reward Signals in the Cerebellum: Origins, Targets, and Functional Implications. Neuron 2022, 110, 1290–1303. [Google Scholar] [CrossRef]
- Turner, B.M.; Paradiso, S.; Marvel, C.L.; Pierson, R.; Boles Ponto, L.L.; Hichwa, R.D.; Robinson, R.G. The Cerebellum and Emotional Experience. Neuropsychologia 2007, 45, 1331–1341. [Google Scholar] [CrossRef]
- Schmahmann, J.D. The Cerebellum and Cognition. Neurosci. Lett. 2019, 688, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Duan, L.; Ou, Y.; Ling, Q.; Cao, L.; Qian, H.; Zhang, J.; Wang, J.; Yuan, X. The Cerebellum and Cognitive Neural Networks. Front. Hum. Neurosci. 2023, 17, 1197459. [Google Scholar] [CrossRef] [PubMed]
- Berman, S.M.; Paz-Filho, G.; Wong, M.-L.; Kohno, M.; Licinio, J.; London, E.D. Effects of Leptin Deficiency and Replacement on Cerebellar Response to Food-Related Cues. Cerebellum 2013, 12, 59–67. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Marron, E.M.; Viejo-Sobera, R.; Cuatrecasas, G.; Redolar-Ripoll, D.; Lorda, P.G.; Datta, A.; Bikson, M.; Magerowski, G.; Alonso-Alonso, M. Prefronto-Cerebellar Neuromodulation Affects Appetite in Obesity. Int. J. Obes. 2019, 43, 2119–2124. [Google Scholar] [CrossRef]
- Mordel, J.; Karnas, D.; Pévet, P.; Isope, P.; Challet, E.; Meissl, H. The Output Signal of Purkinje Cells of the Cerebellum and Circadian Rhythmicity. PLoS ONE 2013, 8, e58457. [Google Scholar] [CrossRef]
- Mendoza, J.; Pévet, P.; Felder-Schmittbuhl, M.-P.; Bailly, Y.; Challet, E. The Cerebellum Harbors a Circadian Oscillator Involved in Food Anticipation. J. Neurosci. 2010, 30, 1894–1904. [Google Scholar] [CrossRef]
- Chen, E.Y.; Zeffiro, T.A. Hunger and BMI Modulate Neural Responses to Sweet Stimuli: fMRI Meta-Analysis. Int. J. Obes. 2020, 44, 1636–1652. [Google Scholar] [CrossRef]
- English, L.K.; Fearnbach, S.N.; Wilson, S.J.; Fisher, J.O.; Savage, J.S.; Rolls, B.J.; Keller, K.L. Food Portion Size and Energy Density Evoke Different Patterns of Brain Activation in Children. Am. J. Clin. Nutr. 2017, 105, 295–305. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Yokum, S.; Stice, E.; Harris, J.L.; Brownell, K.D. Relation of Obesity to Neural Activation in Response to Food Commercials. Soc. Cogn. Affect. Neurosci. 2014, 9, 932–938. [Google Scholar] [CrossRef]
- Yang, Y.; Wu, Q.; Morys, F. Brain Responses to High-Calorie Visual Food Cues in Individuals with Normal-Weight or Obesity: An Activation Likelihood Estimation Meta-Analysis. Brain Sci. 2021, 11, 1587. [Google Scholar] [CrossRef]
- Lundgren, J.D.; Patrician, T.M.; Breslin, F.J.; Martin, L.E.; Donnelly, J.E.; Savage, C.R. Evening Hyperphagia and Food Motivation: A Preliminary Study of Neural Mechanisms. Eat. Behav. 2013, 14, 447–450. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Low, A.Y.T.; Goldstein, N.; Gaunt, J.R.; Huang, K.-P.; Zainolabidin, N.; Yip, A.K.K.; Carty, J.R.E.; Choi, J.Y.; Miller, A.M.; Ho, H.S.T.; et al. Reverse-Translational Identification of a Cerebellar Satiation Network. Nature 2021, 600, 269–273. [Google Scholar] [CrossRef]
- Iosif, C.I.; Bashir, Z.I.; Apps, R.; Pickford, J. Cerebellar Prediction and Feeding Behaviour. Cerebellum 2022, 22, 1002–1019. [Google Scholar] [CrossRef] [PubMed]
- English, L.K.; Masterson, T.D.; Fearnbach, S.N.; Tanofsky-Kraff, M.; Fisher, J.; Wilson, S.J.; Rolls, B.J.; Keller, K.L. Increased Brain and Behavioural Susceptibility to Portion Size in Children with Loss of Control Eating. Pediatr. Obes. 2019, 14, e12436. [Google Scholar] [CrossRef]
- Meng, X.; Huang, D.; Ao, H.; Wang, X.; Gao, X. Food Cue Recruits Increased Reward Processing and Decreased Inhibitory Control Processing in the Obese/Overweight: An Activation Likelihood Estimation Meta-Analysis of fMRI Studies. Obes. Res. Clin. Pract. 2020, 14, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, B.A.; Pearce, A.L.; Rolls, B.J.; Wilson, S.J.; Rose, E.J.; Geier, C.F.; Keller, K.L. Does ‘portion size’ matter? Neural responses to food and non-food cues presented in varying amounts. Appetite 2024, in press. [Google Scholar] [CrossRef]
- Keller, K.L.; Pearce, A.L.; Fuchs, B.; Hallisky, K.; Rolls, B.J.; Wilson, S.J.; Geier, C.; Rose, E.J. Children with Lower Ratings of Executive Functions Have a Greater Response to the Portion Size Effect. Appetite 2023, 186, 106569. [Google Scholar] [CrossRef]
- Bradley, R.H.; Corwyn, R.F. Socioeconomic Status and Child Development. Annu. Rev. Psychol. 2002, 53, 371–399. [Google Scholar] [CrossRef]
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S.; Grummer-Strawn, L.M.; Flegal, K.M.; Mei, Z.; Wei, R.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. 2000 CDC Growth Charts for the United States: Methods and Development. Vital Health Stat. 2002, 11, 1–190. [Google Scholar]
- Smiciklas-Wright, H.; Mitchell, D.C.; Mickle, S.J.; Goldman, J.D.; Cook, A. Foods Commonly Eaten in the United States, 1989–1991 and 1994–1996: Are Portion Sizes Changing? J. Am. Diet. Assoc. 2003, 103, 41–47. [Google Scholar] [CrossRef]
- Kling, S.M.R.; Roe, L.S.; Keller, K.L.; Rolls, B.J. Double Trouble: Portion Size and Energy Density Combine to Increase Preschool Children’s Lunch Intake. Physiol. Behav. 2016, 162, 18–26. [Google Scholar] [CrossRef]
- English, L.K.; Fearnbach, S.N.; Lasschuijt, M.; Schlegel, A.; Anderson, K.; Harris, S.; Wilson, S.J.; Fisher, J.O.; Savage, J.S.; Rolls, B.J.; et al. Brain Regions Implicated in Inhibitory Control and Appetite Regulation Are Activated in Response to Food Portion Size and Energy Density in Children. Int. J. Obes. 2016, 40, 1515–1522. [Google Scholar] [CrossRef]
- Martens, M.; Born, J.; Lemmens, S.; Karhunen, L.; Heinecke, A.; Goebel, R.; Adam, T.; Westerterp-Plantenga, M. Increased Sensitivity to Food Cues in the Fasted State and Decreased Inhibitory Control in the Satiated State in the Overweight. Am. J. Clin. Nutr. 2013, 97, 471–479. [Google Scholar] [CrossRef]
- Keller, K.L.; Assur, S.A.; Torres, M.; Lofink, H.E.; Thornton, J.C.; Faith, M.S.; Kissileff, H.R. Potential of an Analog Scaling Device for Measuring Fullness in Children: Development and Preliminary Testing. Appetite 2006, 47, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Ersig, A.L.; Kleiber, C.; McCarthy, A.M.; Hanrahan, K. Validation of a Clinically Useful Measure of Children’s State Anxiety before Medical Procedures. J. Spec. Pediatr. Nurs. 2013, 18, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Kling, S.M.R.; Pearce, A.L.; Reynolds, M.L.; Garavan, H.; Geier, C.F.; Rolls, B.J.; Rose, E.J.; Wilson, S.J.; Keller, K.L. Development and Pilot Testing of Standardized Food Images for Studying Eating Behaviors in Children. Front. Psychol. 2020, 11, 1729. [Google Scholar] [CrossRef] [PubMed]
- Esteban, O.; Blair, R.; Markiewicz, C.J.; Berleant, S.L.; Moodie, C.; Ma, F.; Isik, A.I.; Erramuzpe, A.; Goncalves, M.; Poldrack, R.A.; et al. Poldracklab/Fmriprep: 1.0.0-Rc5 2017. Available online: https://zenodo.org/records/996169 (accessed on 20 December 2023).
- Fonov, V.; Evans, A.C.; Botteron, K.; Almli, C.R.; McKinstry, R.C.; Collins, D.L. Unbiased Average Age-Appropriate Atlases for Pediatric Studies. NeuroImage 2011, 54, 313–327. [Google Scholar] [CrossRef] [PubMed]
- Fonov, V.; Evans, A.; McKinstry, R.; Almli, C.; Collins, D. Unbiased Nonlinear Average Age-Appropriate Brain Templates from Birth to Adulthood. NeuroImage 2009, 47, S102. [Google Scholar] [CrossRef]
- Cox, R.W. AFNI: Software for Analysis and Visualization of Functional Magnetic Resonance Neuroimages. Comput. Biomed Res. 1996, 29, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Cox, R.W.; Hyde, J.S. Software Tools for Analysis and Visualization of fMRI Data. NMR Biomed 1997, 10, 171–178. [Google Scholar] [CrossRef]
- Power, J.D.; Mitra, A.; Laumann, T.O.; Snyder, A.Z.; Schlaggar, B.L.; Petersen, S.E. Methods to Detect, Characterize, and Remove Motion Artifact in Resting State fMRI. Neuroimage 2014, 84, 320–341. [Google Scholar] [CrossRef]
- Hagler, D.J.; Hatton, S.; Cornejo, M.D.; Makowski, C.; Fair, D.A.; Dick, A.S.; Sutherland, M.T.; Casey, B.J.; Barch, D.M.; Harms, M.P.; et al. Image Processing and Analysis Methods for the Adolescent Brain Cognitive Development Study. Neuroimage 2019, 202, 116091. [Google Scholar] [CrossRef]
- Ashburner, J.; Barnes, G.; Chen, C.-C.; Daunizeau, J.; Flandin, G.; Friston, K.; Gitelman, D.; Glauche, V.; Henson, R.; Hutton, C.; et al. SPM12 Manual; UCL Queen Square Institute of Neurology: London, UK, 2021. [Google Scholar]
- Kanoski, S.E.; Boutelle, K.N. Food Cue Reactivity: Neurobiological and Behavioral Underpinnings. Rev. Endocr. Metab Disord. 2022, 23, 683–696. [Google Scholar] [CrossRef]
- Carnell, S.; Thapaliya, G.; Jansen, E.; Chen, L. Biobehavioral Susceptibility for Obesity in Childhood: Behavioral, Genetic and Neuroimaging Studies of Appetite. Physiol. Behav. 2023, 271, 114313. [Google Scholar] [CrossRef] [PubMed]
- Zlatevska, N.; Dubelaar, C.; Holden, S.S. Sizing up the Effect of Portion Size on Consumption: A Meta-Analytic Review. J. Mark. 2014, 78, 140–154. [Google Scholar] [CrossRef]
- Robinson, E.; McFarland-Lesser, I.; Patel, Z.; Jones, A. Downsizing Food: A Systematic Review and Meta-Analysis Examining the Effect of Reducing Served Food Portion Sizes on Daily Energy Intake and Body Weight. Br. J. Nutr. 2023, 129, 888–903. [Google Scholar] [CrossRef] [PubMed]
- Rüttenauer, T.; Ludwig, V. Fixed Effects Individual Slopes: Accounting and Testing for Heterogeneous Effects in Panel Data or Other Multilevel Models. Sociol. Methods Res. 2019, 52, 43–84. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. J. Stat. Soft. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Cox, R.W.; Chen, G.; Glen, D.R.; Reynolds, R.C.; Taylor, P.A. fMRI Clustering and False-Positive Rates. Proc. Natl. Acad. Sci. USA 2017, 114, E3370–E3371. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-S. Meta-Analysis of Brain Mechanisms of Chewing and Clenching Movements. J. Oral Rehabil. 2018, 45, 627–639. [Google Scholar] [CrossRef] [PubMed]
- Ernst, T.M.; Brol, A.E.; Gratz, M.; Ritter, C.; Bingel, U.; Schlamann, M.; Maderwald, S.; Quick, H.H.; Merz, C.J.; Timmann, D. The Cerebellum Is Involved in Processing of Predictions and Prediction Errors in a Fear Conditioning Paradigm. eLife 2019, 8, e46831. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Li, M.; Zhang, Y.; Song, H.; von Deneen, K.M.; Shi, Y.; Liu, Y.; He, D. Intrinsic Brain Subsystem Associated with Dietary Restraint, Disinhibition and Hunger: An fMRI Study. Brain Imaging Behav. 2017, 11, 264–277. [Google Scholar] [CrossRef] [PubMed]
- Pearce, A.L.; Fuchs, B.; Adise, S.; Masterson, T.D.; Fearnbach, N.; English, L.; Keller, K.L. Loss of Control Eating in Children Is Associated with Altered Cortical and Subcortical Brain Structure. Front. Psychol. 2024, 14, 1237591. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J.; Dimitropoulos, A. Influence of Feeding State on Neurofunctional Differences between Individuals Who Are Obese and Normal Weight: A Meta-Analysis of Neuroimaging Studies. Appetite 2014, 75, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Carnell, S.; Benson, L.; Pantazatos, S.P.; Hirsch, J.; Geliebter, A. Amodal Brain Activation and Functional Connectivity in Response to High-Energy-Density Food Cues in Obesity: Amodal Brain Responses to Food Cues in Obesity. Obesity 2014, 22, 2370–2378. [Google Scholar] [CrossRef] [PubMed]
- Tomasi, D.; Wang, G.-J.; Wang, R.; Backus, W.; Geliebter, A.; Telang, F.; Jayne, M.C.; Wong, C.; Fowler, J.S.; Volkow, N.D. Association of Body Mass and Brain Activation during Gastric Distention: Implications for Obesity. PLoS ONE 2009, 4, e6847. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Thapaliya, G.; Papantoni, A.; Benson, L.; Carnell, S. Neural Correlates of Appetite in Adolescents. Appetite 2023, 191, 107076. [Google Scholar] [CrossRef] [PubMed]
- Moulton, E.A.; Elman, I.; Becerra, L.R.; Goldstein, R.Z.; Borsook, D. The Cerebellum and Addiction: Insights Gained from Neuroimaging Research. Addict. Biol. 2014, 19, 317–331. [Google Scholar] [CrossRef]
- D’Angelo, E.; Casali, S. Seeking a Unified Framework for Cerebellar Function and Dysfunction: From Circuit Operations to Cognition. Front. Neural Circuits 2012, 6, 116. [Google Scholar] [CrossRef]
- Koziol, L.F.; Budding, D.; Andreasen, N.; D’Arrigo, S.; Bulgheroni, S.; Imamizu, H.; Ito, M.; Manto, M.; Marvel, C.; Parker, K.; et al. Consensus Paper: The Cerebellum’s Role in Movement and Cognition. Cerebellum 2014, 13, 151–177. [Google Scholar] [CrossRef]
- Suzuki, M.; Asada, Y.; Ito, J.; Hayashi, K.; Inoue, H.; Kitano, H. Activation of Cerebellum and Basal Ganglia on Volitional Swallowing Detected by Functional Magnetic Resonance Imaging. Dysphagia 2003, 18, 71–77. [Google Scholar] [CrossRef]
- Onozuka, M.; Fujita, M.; Watanabe, K.; Hirano, Y.; Niwa, M.; Nishiyama, K.; Saito, S. Mapping Brain Region Activity during Chewing: A Functional Magnetic Resonance Imaging Study. J. Dent. Res. 2002, 81, 743–746. [Google Scholar] [CrossRef]
- Kheradmand, A.; Zee, D.S. Cerebellum and Ocular Motor Control. Front. Neurol 2011, 2, 53. [Google Scholar] [CrossRef]
- Frazier, M.R.; Hoffman, L.J.; Popal, H.; Sullivan-Toole, H.; Olino, T.M.; Olson, I.R. A Missing Link in Affect Regulation: The Cerebellum. Soc. Cogn. Affect. Neurosci. 2022, 17, 1068–1081. [Google Scholar] [CrossRef]
- Somerville, L.H.; Casey, B. Developmental Neurobiology of Cognitive Control and Motivational Systems. Curr. Opin. Neurobiol. 2010, 20, 236–241. [Google Scholar] [CrossRef]
- Burrows, T.L.; Martin, R.J.; Collins, C.E. A Systematic Review of the Validity of Dietary Assessment Methods in Children When Compared with the Method of Doubly Labeled Water. J. Am. Diet. Assoc. 2010, 110, 1501–1510. [Google Scholar] [CrossRef]
- Grady, C.L.; Rieck, J.R.; Nichol, D.; Rodrigue, K.M.; Kennedy, K.M. Influence of Sample Size and Analytic Approach on Stability and Interpretation of Brain-behavior Correlations in Task-related fMRI Data. Hum. Brain Mapp. 2020, 42, 204–219. [Google Scholar] [CrossRef]
- Minks, E.; Kopickova, M.; Marecek, R.; Streitova, H.; Bares, M. Transcranial Magnetic Stimulation of the Cerebellum. Biomed Pap. Med. Fac. Univ. Palacky Olomouc Czech Repub. 2010, 154, 133–139. [Google Scholar] [CrossRef]
- Santarnecchi, E.; Egiziano, E.; D’Arista, S.; Gardi, C.; Romanella, S.M.; Mencarelli, L.; Rossi, S.; Reda, M.; Rossi, A. Mindfulness-Based Stress Reduction Training Modulates Striatal and Cerebellar Connectivity. J. Neurosci. Res. 2021, 99, 1236–1252. [Google Scholar] [CrossRef]
- Hoekzema, E.; Carmona, S.; Tremols, V.; Gispert, J.D.; Guitart, M.; Fauquet, J.; Rovira, M.; Bielsa, A.; Soliva, J.C.; Tomas, X.; et al. Enhanced Neural Activity in Frontal and Cerebellar Circuits after Cognitive Training in Children with Attention-Deficit/Hyperactivity Disorder. Hum. Brain Mapp. 2010, 31, 1942–1950. [Google Scholar] [CrossRef]
- Moody, T.D.; Morfini, F.; Cheng, G.; Sheen, C.; Tadayonnejad, R.; Reggente, N.; O’Neill, J.; Feusner, J.D. Mechanisms of Cognitive-Behavioral Therapy for Obsessive-Compulsive Disorder Involve Robust and Extensive Increases in Brain Network Connectivity. Transl. Psychiatry 2017, 7, e1230. [Google Scholar] [CrossRef]
- Van Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Gulban, O.F.; Nielson, D.; Lee, J.; Poldrack, R.; Gorgolewski, C.; Vanessasaurus; Markiewicz, C. Poldracklab/pydeface: PyDeface v2.0.2. 2022. Available online: https://zenodo.org/records/6856482 (accessed on 20 December 2023).

| Region | Brodmann Area (s) |
|---|---|
| Dorsolateral prefrontal cortex | 9, 46 |
| Anterior prefrontal cortex | 10 |
| Orbitofrontal cortex | 11, 12 |
| Insula | 13, 14, 16 |
| Associative visual cortex | 19 |
| Subgenual area | 25 |
| Dorsal anterior cingulate cortex | 32 |
| Fusiform | 37 |
| Primary gustatory cortex | 43 |
| Inferior frontal gyrus | 44, 45, 47 |
| Hippocampus | - |
| Hypothalamus | - |
| Globus pallidus (lateral, medial) | - |
| Caudate (body, tail, head) | - |
| Putamen | - |
| Substantia nigra | - |
| Subthalamic nucleus | - |
| Amygdala | - |
| Midbrain | - |
| Included (N = 63) | Excluded (N = 25) | |
|---|---|---|
| Sex | ||
| Male | 30 (47.6%) | 15 (60.0%) |
| Female | 33 (52.4%) | 10 (40.0%) |
| Age, yrs | ||
| Mean (SD) | 7.82 (0.587) | 7.79 (0.595) |
| Min, Max | 7.00, 8.99 | 7.03, 8.81 |
| Family Income | ||
| <USD 51,000 | 9 (14.3%) | 2 (8.0%) |
| USD 51,000–USD 100,000 | 28 (44.4%) | 14 (56.0%) |
| >USD 100,000 | 24 (38.1%) | 8 (32.0%) |
| Missing | 2 (3.2%) | 1 (4.0%) |
| Maternal Education | ||
| <Bachelor’s Degree | 13 (20.6%) | 5 (20.0%) |
| Bachelor’s Degree | 30 (47.6%) | 11 (44.0%) |
| >Bachelor’s Degree | 19 (30.2%) | 9 (36.0%) |
| Missing | 1 (1.6%) | 0 (0%) |
| BMI Percentile | ||
| Mean (SD) | 47.0 (25.5) | 49.0 (24.2) |
| Min, Max | 3.91, 89.3 | 6.69, 89.5 |
| Pre-MRI Fullness | ||
| Mean (SD) | 71.3 (30.1) | 70.2 (33.2) |
| Min, Max | 4.00, 150 | 3.00, 139 |
| Missing | 1 (1.6%) | 0 (0%) |
| Pre-MRI Anxiety | ||
| Median [Q1, Q3] | 2.0 [0.0, 3.0] | 3.0 [0.75, 6.0] |
| Min, Max | 0, 10 | 0, 10 |
| Missing | 0 (0%) | 1 (4.0%) |
| Average Framewise Displacement | ||
| Median [Q1, Q3] | 0.30 [0.19, 0.38] | 1.52 [0.89, 1.67] |
| Min, Max | 0.0800, 1.29 | 0.500, 4.79 |
| Missing | 0 (0%) | 6 (24.0%) |
| Portion Size Slope | N | Mean (SD) | Min, Max |
|---|---|---|---|
| Linear portion size slope, g a | 63 | 58.0 (113) | −194, 370 |
| Linear portion size slope, kcal b | 63 | 124 (175) | −205, 647 |
| Quadratic portion size slope, g c | 60 | −66.8 (419) | −953, 1090 |
| Quadratic portion size slope, kcal d | 60 | −26.8 (628) | −1500, 1470 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuchs, B.A.; Pearce, A.L.; Rolls, B.J.; Wilson, S.J.; Rose, E.J.; Geier, C.F.; Garavan, H.; Keller, K.L. The Cerebellar Response to Visual Portion Size Cues Is Associated with the Portion Size Effect in Children. Nutrients 2024, 16, 738. https://doi.org/10.3390/nu16050738
Fuchs BA, Pearce AL, Rolls BJ, Wilson SJ, Rose EJ, Geier CF, Garavan H, Keller KL. The Cerebellar Response to Visual Portion Size Cues Is Associated with the Portion Size Effect in Children. Nutrients. 2024; 16(5):738. https://doi.org/10.3390/nu16050738
Chicago/Turabian StyleFuchs, Bari A., Alaina L. Pearce, Barbara J. Rolls, Stephen J. Wilson, Emma J. Rose, Charles F. Geier, Hugh Garavan, and Kathleen L. Keller. 2024. "The Cerebellar Response to Visual Portion Size Cues Is Associated with the Portion Size Effect in Children" Nutrients 16, no. 5: 738. https://doi.org/10.3390/nu16050738
APA StyleFuchs, B. A., Pearce, A. L., Rolls, B. J., Wilson, S. J., Rose, E. J., Geier, C. F., Garavan, H., & Keller, K. L. (2024). The Cerebellar Response to Visual Portion Size Cues Is Associated with the Portion Size Effect in Children. Nutrients, 16(5), 738. https://doi.org/10.3390/nu16050738






