Abstract
The Inuit population of Nunavik is faced with a significant rise in the prevalence of obesity [body mass index (BMI) ≥ 30 kg/m2], but the impact on cardiometabolic health is unclear. The aim of this study was to characterize adiposity phenotypes and explore their associations with cardiometabolic risk factors among Nunavimmiut men and women. We used data obtained from 1296 Inuit who participated in the Qanuilirpitaa? 2017 Nunavik Inuit Health survey. Collected information included demographics, anthropometric measurements including visceral fat level (VFL) measured using electrical bioimpedance, biomarkers, hemodynamics, medical history and medication list. Adjusted population-weighted linear regressions were conducted to assess associations between body fat distribution and cardiometabolic risk factors. The accuracy and cut-off points of anthropometric indices to detect cardiometabolic abnormalities was evaluated by area under the receiver operator characteristic curve (AUROC) and a maximum Youden index analysis. Among Nunavimmiut (mean age 38.8 years [95%CI: 38.4 to 39.3]), obesity was observed in 42.8% of women and 25.6% of men. Compared to men, women presented a higher prevalence of abdominal obesity (78.8% vs. 46.4% in men, p < 0.05) and elevated VFL (54.4% vs. 20.1% with an InBody level ≥ 13, p < 0.05). Indices of global fat distribution and abdominal adiposity including VFL provided poor to moderate ability to detect cardiometabolic abnormalities (AUROC between 0.64 and 0.79). This analysis revealed that despite a high prevalence of abdominal obesity, particularly among women, anthropometric measurements of adiposity are inconsistently associated cardio-metabolic risk factors in Inuit adults of Nunavik.
1. Introduction
Over recent decades, Canadian Indigenous communities have been faced with a significant and disproportionate rise in the prevalence of obesity [body mass index (BMI) ≥ 30 kg/m2] [1,2,3] and cardiovascular (CV) risk factors such as hypertension [4,5] and dyslipidemia [6]. Among other factors, the progressive impacts of colonization have contributed to a change in their traditional lifestyle behaviors and diet. This is associated with adverse effects on their CV health and promotes health disparities among Indigenous peoples across Canada [1]. Despite their younger average age, certain Indigenous peoples living in Canada (First Nations, Métis) present a higher prevalence of CV risk factors (insulin resistance, type 2 diabetes, hypertension, dyslipidemia) and exhibit higher CV morbidity and mortality compared to non-Indigenous Canadians [3]. However, reports over the last few decades tend to distinguish the Inuit population from other Indigenous populations in Canada, and suggest a differential effect of fat accumulation on cardiovascular risk factors, mainly insulin resistance and type 2 diabetes (T2D) [7].
The cardiometabolic risk profile of Inuit adults living in Nunavik has been previously described in two major health surveys (the Santé Québec Survey in 1992 and the Qanuippitaa? Inuit Health Survey in 2004) which included participants from all 14 communities of Nunavik. Results from those surveys have described an increase in the prevalence of obesity (from 19% in 1992 to 28% in 2004), which was encountered particularly in women (from 25 to 31%) [1]. This trend was also observed in Inuit living with severe obesity (BMI ≥ 35 kg/m2) [2]. We have previously shown that the prevalence of severe obesity had increased from 1.5% in 1992 to 5.5% in 2004, with women presenting a significant increase in waist circumference (WC) over time (from 103.9 to 121.5 cm), i.e., abdominal obesity [2].
Numerous studies have reported that abdominal obesity and more specifically abdominal visceral fat level (VFL) has an important prognostic role in obesity-related cardiometabolic complications [8,9]. Across the entire spectrum of BMI values, the presence of cardiometabolic conditions appears to be closely related to a predominantly visceral abdominal body fat deposition pattern, as well as ectopic fat accumulation in organs such as the liver and the heart [9]. Although abdominal obesity is now an established universal marker of cardiometabolic risk, the majority of studies supporting this hypothesis did not include Indigenous populations [10,11]. Moreover, despite a significant rise in the prevalence of obesity and abdominal obesity over recent decades, the prevalence of cardiometabolic risk factors (dyslipidemia, dysglycemia, insulin resistance, hypertension, liver steatosis, etc.) appears to be relatively stable in Inuit men and women, reinforcing the idea that the Inuit population would benefit from a more favorable cardiometabolic risk profile, independent of their degree of obesity [2]. Cross-sectional studies including Inuit of the central Canadian Arctic (434 participants, 54.1% women, mean BMI of 24.7 kg/m2 in men and 28.6 kg/m2 in women) [7] and Nunavimmiut (710 participants, 54.4% women, BMI of 27.1 kg/m2 in men and of 28.0 kg/m2 in women) [6] have reported a weaker association between anthropometric indices of abdominal obesity (WC) and cardiometabolic risk factors, compared to non-Indigenous populations. In a study using data from the Qanuilirpitaa? 2017 survey (1177 participants, 65.4% women and 32% of obesity), we reported that abdominal obesity (WC ≥ 88 cm in women and ≥102 cm in men) was a risk factor for hypertension, but this association was weaker in women compared to men, suggesting that metabolically healthy obesity might be more prevalent among Inuit women [4]. These results raise important questions about the generalization of pathophysiological concepts associating abdominal obesity and detrimental cardiometabolic health to Inuit populations. This also challenged the applicability of our current obesity public health policies and CV clinical guidelines [12,13,14] to the Inuit population of Nunavik.
This study is the first to explore the association between measured indices of body fat distribution including VFL level and cardiometabolic health using contemporary data in Inuit from Nunavik. The aim of this study was (1) to characterize adiposity phenotypes and the cardiometabolic risk profile among Inuit men and women from Nunavik; (2) to describe the association between anthropometric indices and cardiometabolic risk factors; and (3) to explore sex- and ethnic-specific cut-offs for global obesity and abdominal obesity in the Inuit population of Nunavik.
2. Methodology
2.1. Setting
The Qanuilirpitaa? 2017 Nunavik Inuit Health survey was conducted in partnership with Nunavik health organizations, the Institut National de Santé Publique du Québec (INSPQ) and research teams from different universities in Canada. It took place following a resolution adopted by the Nunavik Regional Board of Health and Social Services (NRBHSS), which requested updated information on the overall health of the Nunavik population. An Inuit-led Steering Committee oversaw the preparation, conduct, interpretation and dissemination of all survey results. The Data Management Committee of Qanuilirpitaa? 2017 evaluated the relevance of our research question for the Nunavik population, approved data and biological sample requests, made comments on this manuscript and approved its final version. The dissemination of the results presented in the present study was prepared according to the recent call for action on culturally safe research in Canadian Indigenous populations by Aziz et al. [15]. The Qanuilirpitaa? 2017 survey was also approved by the ethics committee of the Centre de Recherche du CHU de Québec—Université Laval (no. 2016-2499-21).
2.2. Study Population
Data collection for the Qanuilirpitaa? 2017 health survey took place in the 14 communities of Nunavik (Northern Quebec, Canada), from 19 August to 5 October 2017. Participants aged 16 years and older were invited aboard the Amundsen, a Canadian Coast Guard icebreaker, converted into a scientific research ship. Potential participants were selected from a proportional sampling of the Makivvik Corporation’s beneficiary list of Inuit living in Nunavik, stratified for age groups and communities. The Makivvik list is the most comprehensive available list to use as a sampling frame for research purposes. It is estimated that the majority of Inuit individuals living in Nunavik are on this list, and for this health survey, the most recent list (spring 2017) has been obtained. The overall participation rate was 36.5%; many individuals originally selected from the list could not be contacted as they were out of the community during the study period. The inclusion criterion was set at 16 years of age or older. This specific age threshold was established based on the community request to include youth for the purpose of assessing their overall health. The only pre-established exclusion criterion for this study was pregnancy (n = 30). A total of 1326 individuals were eligible and included in the Qanuilirpitaa? 2017 health survey, and 1296 were included in this specific study. Aboard the Amundsen, medical and lifestyle questionnaires were administered and clinical and laboratory tests were performed. Some information including medication lists (n = 1047) was obtained from participants’ medical records in local community-service centers with the participants’ authorization. The detailed methodology has been described elsewhere [16].
2.3. Clinical Assessment, Medical Review and Questionnaires
Weight and body composition measurements based on bioelectrical impedance were obtained using a validated InBody device (Model 570, Cerritos, CA, USA) [17]. BMI was calculated by dividing the weight in kilograms by the square of the height in meters (kg/m2), and classified according to the National Institute of Health’s scheme (BMI value 25.0–29.9 kg/m2 being overweight, 30.0–34.9 kg/m2 being obesity, and ≥35.0 kg/m2 being severe obesity) [18]. Visceral fat level (VFL) was provided by the InBody device and a high level of visceral fat was defined as per the manufacturer’s recommendations and previous validation studies (level ≥ 13) [17,19,20], which did not include Canadian Inuit populations. To estimate visceral fat level using the InBody device, participants had to stand on the monitor without shoes. A low and safe electrical signal is sent from the feet to the abdomen to produce body composition measurements. Height and WC were measured in centimeters and taken by nurses or trained interviewers and the waist-to-height ratio (WHtR) was calculated by dividing the participant’s WC by its height (in cm). Due to the lack of published data regarding Inuit people, abdominal obesity was defined using the current World Health Organization (WHO) recommended cut-offs of WC (≥88 cm in women and ≥102 cm in men) [21]; however, it is possibly not appropriate for non-Caucasian ethnic groups [22,23]. Resting blood pressure was measured with the ProBP 2400 Digital electronic device (Welch Allyn, Aurburn, NY, USA) according to the 2005 Canadian Hypertension Education Program recommendations. Participants first rested for 5 min in a seated position and the blood pressure cuff was placed on the supported bare arm at the heart level. Three measurements were taken for the same arm with the participant in the same position, but the first reading was discarded, and the blood pressure recorded was the mean of the two latter measures. Hypertension was defined as a systolic blood pressure ≥ 140 mm Hg or a diastolic blood pressure ≥ 90 mm Hg or if participants were on anti-hypertensive medications [24].
Blood samples were collected by trained nurses and processed by laboratory technicians within 90 min of collection. White blood cell count (WBC), platelet count (PLT) and hemoglobin (Hb) concentration were obtained using a DxH 500 hematology analyzer (Beckman Coulter). In addition, the following clinical biochemistry tests were conducted in collaborating hospital laboratories on samples stored at −80 °C: hepatic profile [albumin, aspartate transaminase (AST), alanine transaminase (ALT), gamma-glutamyl-transferase (GGT) and total bilirubin], renal function (creatinine, eGFR, urine micro-albuminuria), lipid profile [triglycerides (TG), low-density-lipoprotein cholesterol (LDL-C), total cholesterol (TC), high-density-lipoprotein cholesterol (HDL-C) and apolipoprotein-B (ApoB)], glycated hemoglobin (HbA1c) and high-sensitivity C-reactive protein (hs-CRP). When participants were fasting (n = 548), fasting glucose and fasting insulin were also measured. The Homeostatic Model Assessment was used to obtain a quantitative assessment of insulin resistance (HOMA-IR) [25]. Insulin resistance was defined as a HOMA-IR index > 2.0 according to previous results reported in a First Nation population of Northern Quebec (Eeyou Istchee Crees) [26].
T2D and pre-diabetes were defined using criteria from Diabetes Canada [27] or determined according to the participant’s medication (i.e., participants on glucose-lowering drugs were considered to be diagnosed with T2D). Dyslipidemia was diagnosed using the Canadian Cardiovascular Society’s recommendations or if participants were on lipid-lowering drugs [28] and stages of chronic kidney disease were reported as per the Kidney Disease: Improving Global Outcomes recommendations [29]. To estimate non-alcoholic fatty liver disease (NAFLD), the fatty liver index (FLI) was calculated using the formula elaborated by Bedogni and colleagues with recommended cut-offs [30], although this index has not been previously validated for Inuit populations. The FIB-4 score was also used to estimate the level of hepatic fibrosis and advanced fibrosis; scores > 2.67 have demonstrated a high positive predictive value for advanced liver fibrosis and this cut-off has been used previously in the Greenlandic Inuit population [31,32,33]. Standardized and culturally appropriate questionnaires were administered to participants to collect information on their lifestyle (smoking status and alcohol consumption).
2.4. Statistical Analysis
All statistical analyses were conducted using StataCorp 15.0. Normally distributed continuous variables were reported using mean and standard deviation (SD) and compared between sexes using Student’s t-tests. Categorical variables were reported as frequencies and compared with Chi-square tests. Associations between anthropometric measurements of fat distribution (weight, BMI, WC and WHtR) and measurements of fat distribution using electrical bio-impedance (estimated percentage of body fat, body fat mass and VFL) as well as cardio-metabolic risk factors were assessed using logistic and linear regression analyses, adjusted for age, gender, smoking status and BMI in the case of predictor variables WC and VFL, given the previously estimated collinearity. The data employed in the logistic and linear regression analyses underwent prior assessments to ensure normality and linearity, with all assumptions being satisfied. As no cut-off for indices of adiposity have been validated in the Inuit population, independent variables of body phenotypes (weight, BMI, WC and WHtR) were analyzed as continuous variables. Capacities of weight, BMI, WC, WHtR and VFL to predict cardiometabolic diseases were calculated using the area under the receiver operating characteristic curves (AUROCs). An AUC of 0.500 denoted no discriminatory power, 0.501–0.69 denoted poor discriminatory ability, 0.700–0.79 was considered acceptable discriminatory ability, 0.800–0.89 denoted excellent discriminatory ability, and 0.90–1 was considered outstanding discriminatory ability [34]. A Youden index analysis was used to determine the optimal cut-off for the AUROCs [35]. Two-sided p < 0.05 was considered statistically significant. Survey weights were applied in all analyses to consider the sampling methodology and nonresponse [16], and bootstrap weights (500) were used to compute the variance of all estimates.
3. Results
Baseline characteristics of participants are described in Table 1. A total of 843 (65.0%) women were included in this study, and the majority of participants were under 50 years old (79.9% of men and 82.7% of women), with a large proportion under 19 years old (30.0% of men and 26.6% of women). Mean BMI was 26.3 ± 5.7 kg/m2 in men and 28.0 ± 6.4 kg/m2 in women (p < 0.05). Obesity was noted in 116 men (25.6%) and 361 women (42.8%), among which 22 men (4.9%) and 144 women (17.1%) presented with severe obesity. Severe obesity was more prevalent among young Nunavimmiut women (between 16 to 44 years old) (Figure 1). Inuit women presented a higher prevalence of abdominal obesity (as defined by WHO cut-offs) compared to men (78.8 vs. 46.4%, p < 0.05). Furthermore, Nunavimmiut women also had higher levels of VFL (estimated using electrical bio-impedance) compared to men (54.4 vs. 20.1%, p < 0.05).

Table 1.
Population descriptive characteristics.
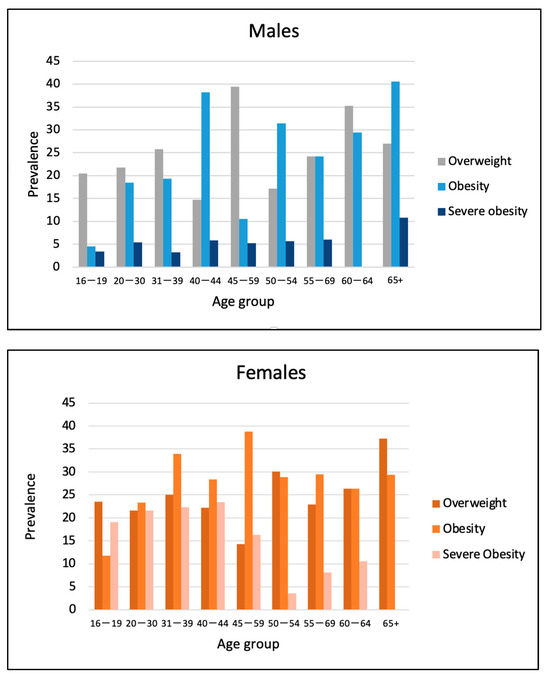
Figure 1.
Prevalence of overweight, obesity and severe obesity by sex among Nunavimmiut aged 16 and over, Qanuilirpitaa? 2017 Health Survey.
Prevalence of obesity-associated comorbidities are also displayed in Table 1. Nunavimmiut women presented a lower prevalence of hypertension and dyslipidemia compared to men (15.2 vs. 25.8% for hypertension and 29.5 vs. 36.2% for dyslipidemia, p < 0.05, respectively). Insulin resistance (estimated using HOMA-IR) was highly prevalent among men and women (55.4% of men and 67.3% of women, p = 0.09), but prevalence of prediabetes and T2D (diagnosed using fasting glucose and/or HbA1c) was relatively low for both sexes (9.1% of men and 10.0% of women had prediabetes, 6.0% of men and 7.3% of women had T2D, p < 0.05). Using the FLI score, only a small proportion of men and women were diagnosed with NAFLD (3.1 and 2.4%, p < 0.05, respectively) and only two participants [one man (0.22%) and one woman (0.12%), p < 0.05] were characterized with advanced hepatic fibrosis, defined with the FIB-4 score. Tobacco consumption was high in both sexes, with 64.5% of men and 70.2% of women reporting daily smoking.
Clinical biochemistry data are presented in Table 2. Overall, laboratory features of cardiometabolic risk factors were similar between sex, except for HbA1c, which was significantly higher in men compared to women (HbA1c of 5.56 ± 0.60% in men vs. 5.47 ± 0.74% in women, p < 0.05).

Table 2.
Biomarker profile among Nunavimmiut 16 years and over, Qanuilirpitaa? 2017 Health Survey.
Correlations between anthropometric parameters (BMI, WC, WHtR and VFL) were estimated using standardized linear regression analysis (adjusted for age and BMI in the case of WC and WHtR). Correlation factors with VFL were r = 0.90 for BMI, r = 0.87 for WC and r = 0.89 for WHtR (p-value <0.05 for all). Estimated predicted values of VFL using anthropometric measurement of adiposity are displayed in Figure 2. Anthropometric indices were all significantly correlated with VFL, with BMI being more strongly associated with VFL (standardized β-coefficient of 5.19, 95% CI: 5.04–5.29), compared to WC (standardized β-coefficient of 1.11, 95% CI: 0.84–1.39) and WHtR (standardized β-coefficient of 0.60, 95% CI: 0.31–0.90). For similar values of BMI and WC, women consistently presented a greater adjusted predicted VFL value compared to men. This trend was also noted for WHtR; the estimated VFL value was higher in women, but only up to a certain WHtR level (WHtR = 1.3).
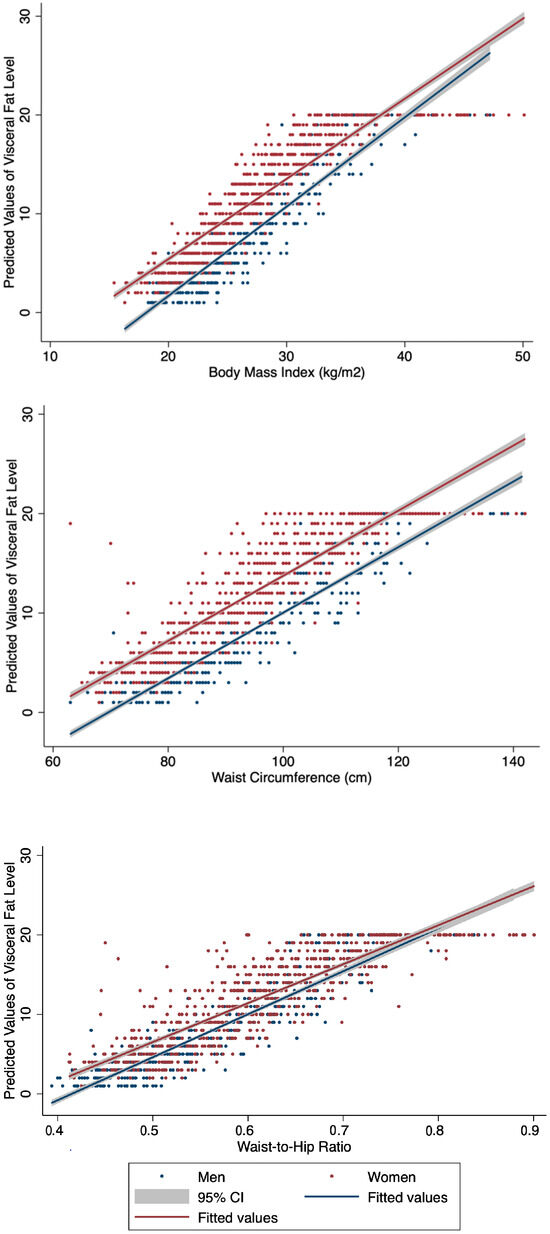
Figure 2.
Predictive capacities of anthropometric indices of body fat distribution for the identification of visceral adiposity by sex among Nunavimmiut aged 16 and over, Qanuilirpitaa? 2017 Health Survey.
Associations between the anthropometric features of obesity (weight, BMI, WC, WHtR and VFL) and cardiometabolic risk factors (TC/HDL ratio, LDL, HDL, TG, ApoB, HbA1c, fasting glucose and fasting insulin, HOMA-IR, systolic and diastolic blood pressure) are displayed in Supplementary Table S2, with subgroup analyses for men (Supplementary Table S3) and for premenopausal women (Supplementary Table S4). In men, BMI was associated with a detrimental increase in almost all cardiometabolic risk factors (decrease in case of HDL), but HbA1c. Men demonstrated no significant association between measurements of abdominal obesity and a detrimental cardiometabolic risk profile. Although VFL was associated with an abnormal lipid profile (higher TG and CHOL/HDL ratio) and a higher level of fasting glucose, it was neither significantly linked to an increase in LDL, ApoB, a decrease in HDL nor to higherHOMA-IR, HbA1c and systolic blood pressure values. Specifically looking at premenopausal women, WC and WHtR were negatively associated with insulin resistance and positively associated with dyslipidemia (high TG and ApoB levels). VFL was associated with an abnormal lipid profile and higher diastolic blood pressure but not with risk factors of insulin resistance or dysglycemia. Therefore, in premenopausal Nunavimmiut women, VFL was not associated with any cardiometabolic risk factors albeit accumulating more VFL than Nunavimmiut men. A subgroup analysis excluding participants under the age of 20 showed similar associations compared to the overall included population (Supplementary Table S5).
The predictive abilities of anthropometric measurements (weight, BMI, WC, WHtR) and VFL) to detect obesity-associated comorbidities were estimated using AUROC (Table 3). In men, all measurements of fat distribution demonstrated an acceptable capacity to predict hypertension, insulin resistance, prediabetes, T2D and dyslipidemia. However, in women, anthropometric measurements were generally poor predictors of cardiometabolic conditions, except for insulin resistance for which anthropometric indices of obesity showed an acceptable capacity.

Table 3.
Predictive capacities of anthropometric indices and VFL to detect cardiometabolic disorders among Nunavimmiut aged 16 and over by sex, Qanuilirpitaa? 2017 Health Survey.
The Youden Index analysis was used to determine the optimal sex-specific cut-offs for BMI and WC among Nunavimmiut (Supplementary Table S6). In men, optimal BMI cut-offs for cardiometabolic disorders ranged between 25.6 and 28.8 kg/m2, while in women, BMI cut-offs were estimated between 26.6 kg/m2 and 29.9 kg/m2. WC cut-offs for men ranged from 86.5 cm for dyslipidemia and hypertension to 100 cm for prediabetes and diabetes, while WC cut-offs for women ranged from 92.0 cm to 100 cm depending on the outcome. Cardiometabolic comorbidities were optimally detected at lower levels of VFL in men (from 6 to 10) compared to women (from 12 to 14).
4. Discussion
In this study, we report a very high prevalence of obesity, severe obesity and abdominal obesity, especially among Nunavimmiut women. Previous surveys from Canada [36] and other countries [37,38] have also described a higher prevalence of abdominal obesity in diverse ethnic female groups compared to males. Comparing our results to a recent study including data from a subgroup of 4662 participants of the Canadian Health Measures Survey Cycles 1 and 2 (mean age of 55.1 years for men and 55.8 years for women) [39], we also demonstrate that Inuit women, despite being younger, have a higher WHtR compared to their Canadian counterparts (0.61 ± 0.10 vs. 0.56 ± 0.10), whereas Inuit men had lower values (0.55 ± 0.10 vs. 0.57 ± 0.08). Our analysis also revealed that, despite being younger (median age [IQR] of 38 [25–63] years old), 12.8% of men and women were characterized by severe obesity, an increased proportion (more than double) compared to the prevalence reported in a weighted analysis from 2004 (5.5% of the total population, median age [IQR] of 48 [28–63] years old) and from 1992 (1.5% of participants, median age of 47 [28–61] years old) [2]. Our results also suggest that obesity prevalence is high in Nunavimmiut youth (16–44 years old). Obesity prevalence in the 16 to 44 years age group varies from 4.5 to 38.2% in men and from 11.8 to 38.8% in women, which is more than twice higher compared to their non-Indigenous counterparts. In comparison with young non-Indigenous Canadians of a similar age (<35 years old), between 7.2 and 15.9% of men and 5.5% to 13.3% of women were characterized with obesity in 2018 [40]. Abdominal obesity is found to be highly prevalent among Inuit men and even more so in Inuit women (46 and 79%, respectively), especially among youth. This trend is particularly worrisome from a long-term perspective, given the risk of morbidity and mortality associated with high-risk obesity observed in non-Inuit populations.
Differences in the association between obesity and cardiometabolic risk factors based on ethnic origin are increasingly noted in the scientific literature and could be partly explained by an ethnic-specific predisposition to store fat subcutaneously compared to viscerally [41,42,43]. A previous study comparing body fat distribution among different ethnic groups suggested that Greenlandic Inuit men and women might accumulate less VAT (measured using ultrasound) for a given level of BMI compared to European-descent populations [42]. However, in our study, we noted high levels of estimated VFL among women and observed a high correlation between anthropometric measurements of body fat (BMI, WC and WHtR) and VFL in both sexes. For a given BMI, WC or WHtR, women almost systematically present higher age-adjusted predicted values of VFL compared to Inuit men (Figure 2). Despite methodological limitations imposed by the use of bio-impedance VFL measurements, this trend is consistent with a previous study, which compared anthropometric measurements between the Greenlandic Inuit (3083 participants, 60.0% women and mean age of 42 years) and a European-descent Danish population (795, 56.4% woman participants and mean age of 47 years), which showed that Inuit women had the highest absolute values in BMI, WC, and VAT accumulation (estimated using standardized measures of ultrasonography) compared to Inuit men and individuals of European descents [41]. Menopausal status was not assessed in the Qanuilirpitaa? 2017 health survey but extending our analysis to a subgroup of women aged ≤ 55 years old, we report a similar proportion of women with a high level of VFL (47.1 vs. 54.4% of total women) and age-adjusted predictive values of VFL. If menopause plays a role, its impact on fat distribution among Inuit women remains unclear and will need to be assessed specifically.
Comparing our results to those of the Canadian Health Measures Survey Cycles 1 and 2 (2012–2013), we report that despite a high prevalence of obesity and abdominal obesity, Nunavimmiut have a slightly lower prevalence of dyslipidemia (36.2% in men and 29.5% in women vs. 38% in the Canadian population) [44] and T2D (5.9% in men, 7.3% in women vs. 7.9%) [45] and a higher prevalence of hypertension in men but lower in women (25.3% in men and 15.2% in women vs. 22.6%) compared to the general Canadian population [46]. Our results also indicate a significantly lower prevalence of estimated NAFLD (3.1% in men and 2.4% in women using FLI formula) compared to that reported in the Canadian population (20.8% of Canadians were projected to have a diagnosis of NAFLD in 2019 using a Markov model using historical trends in obesity prevalence and diagnosis of liver fibrosis, decompensated cirrhosis, hepatocellular carcinoma and liver transplantation) [47]. No Canadian data on NAFLD prevalence have been published yet.
It should be noted that the population included in Qanuilirpitaa? 2017 is younger than the general Canadian population. Rather than demonstrating a favorable ethnic-specific metabolic profile, our results might illustrate that Inuit men and women from Nunavik are currently characterized by a transient phenotype of obesity, with a short duration of fat accumulation and a preserved metabolic state. After performing analysis on a sub-group of adults 50 years of age and older (Supplementary Table S7), we report a prevalence of 28.8% of women with obesity and 75.1% with abdominal obesity, compared to 31.6% of men with obesity and 64.0% with elevated WC. Our analysis also demonstrates that some adiposity-associated comorbidities are more prevalent in this age group. Insulin resistance was diagnosed in the majority of participants (55.4% of men and 67.3% of women, p = 0.9). Longitudinal studies will be necessary to better understand how obesity will impact the cardiometabolic health of this group over the long term.
Recent imaging studies have shown that ethnicity could affect metabolic responses to obesity [48,49], and demonstrated that African Americans were less prone to developing a dysglycemic status compared to persons identifying as Hispanic or of European descent, despite a similar level of VAT [49]. Inuit have never been included in large standardized international imaging studies, but specific ethnic disparities could partly explain their low prevalence in cardiometabolic comorbidities, despite a high level of abdominal obesity. When extending our analysis to the effect of abdominal fat accumulation on the cardiometabolic profile of Inuit men and women, we observe a positive association between estimated VFL and risk factors for dyslipidemia and hypertension. However, VFL is not significantly associated with features of dysglycemia (for both sexes combined and in men and premenopausal women separately) and is found to be a poor predictor of pre-diabetes and T2D in Nunavimmiut women (AUROC of 0.69 for both). Similarly, WC was positively associated with certain cardiometabolic parameters (TG, CHOL/HDL, ApoB) but not others (LDL-C, HDL-C, HbA1c, fasting glucose, HOMA-IR, blood pressure) (Supplementary Table S2). Beyond body fat distribution, other factors seem to play a significant role in the complex physiological interactions connecting obesity and glucose homeostasis in the Inuit of Nunavik. Among other factors, the traditional diet of Nunavimmiut (low in glucose and rich in protein and long-chain n-3 polyunsaturated fatty acids) might afford protection against cardiometabolic disorders including T2D [50,51,52]. Significant differences in Inuit’s microbiota [53], physical activity level [11], exposure to persistent organic pollutants [52,54] and genetic variants [51] might also impact significantly on their cardiometabolic health. For example, a population-specific nonsense genetic variant in TBC1D4, which has a large impact on T2D risk, has recently been identified in Greenlandic, Canadian and Alaskan Inuit [51,55]. Mutations on TBC1D4 are associated with higher post-prandial glucose and insulin levels. In a recent study, Manousaki et al. have reported that the TBC1D4 mutation was present in 27% of Canadian and Alaskan Inuit (heterozygote or homozygote carriers) [55], which suggests that pre-diabetes and T2D might be underdiagnosed among Canadian Inuit, unless post-prandial values are tested. The prevalence of TBC1D4 mutations have not been yet reported among Nunavimmiut, and further studies examining the validity and diagnostic capacities of traditional screening methods to detect dysglycemia and T2D risk factors are needed in this population.
Although being the most recognized measurement to estimate the degree of obesity and predict associated cardiometabolic disorders, it has been previously suggested that BMI would be inadequate for the Canadian Inuit population [56,57]. Charbonneau-Roberts et al. have previously reported that Inuit men and women tend to have shorter legs and a relatively higher sitting height than other populations, which could lead to an over-estimation of obesity in this population [57]. In a cross-sectional study including 3083 Inuit from Greenland and 795 Europeans from Denmark, Ronn et al. reported a lower percentage of body fat in Greenlandic men and women, despite having higher anthropometric indices of obesity than Europeans [42]. In our study, we observed significant positive associations between BMI, WC, WHtR and estimates of body fat composition and fat distribution using electrical bio-impedance (percentage of body fat, body fat mass and VFL) (Supplementary Table S1). However, we also noted poor to moderate capacities of anthropometric indices of obesity to predict cardiometabolic abnormalities (AUROC between 0.60 and 0.77). This suggests that BMI, WC, WHtR and even VFL estimated using electrical bio-impedance are poor predictors of cardiovascular disorders in this population. However, the young age of our population, thus at lower risk for metabolic and cardiovascular disease, needs to be highlighted here and could partly explain these results.
Strengths and Limitations
This study is the first to extensively describe the cardiometabolic risk profile of Nunavimmiut. Because Nunavik is a remote region of northern Quebec, which is not easily accessible, inclusion of Nunavimmiut in clinical cardiometabolic trials has been limited. This study tentatively addresses the current gap in the scientific literature and provides new data on the metabolic and cardiovascular consequences of body fat accumulation in this population. However, our results need to be interpreted with caution due to certain limitations. First, although all models were adjusted for participants’ age, Nunavimmiut participants in this study were relatively young, which might have impacted on: (1) the prevalence of the cardiometabolic comorbidities observed, and (2) the association between body fat accumulation and cardiovascular and metabolic risk factors. Causal inference of the relationship between adiposity and cardiometabolic health should be examined further in longitudinal studies. Second, measurement of VFL using electrical bio-impedance is not considered the gold-standard and has never been validated in the Inuit population of Nunavik. To our knowledge, no previous studies have reported on VFL using an InBody device in this population, and validation studies will be necessary. Likewise, the cut-off values employed in this study for assessing abdominal obesity lack validation within the Inuit population. It is imperative to undertake more extensive in-community projects, specifically involving under-represented populations like Inuit, to validate commonly used indices and clinical tools for assessing cardiometabolic health. Finally, we employed the Makivvik Corporation’s beneficiary list as a sampling framework to randomly select Inuit participants residing in Nunavik. While it is believed that a significant portion of the population is registered on this list, we acknowledge the possibility that a selection bias may have been induced by the recruitment process.
5. Conclusions
In conclusion, Nunavimmiut have a high prevalence of potentially high-risk obesity (abdominal visceral obesity and severe obesity), especially among young women. Early detection and management of cardiometabolic risk factors remain paramount for improving CV health and potentially reducing premature CV mortality. Long-term effects of obesity at a younger age on CV morbidity and mortality risk later in life need to be explored with longitudinal cardiac and whole-body imaging technique studies. Public health actions are required to target this emergent epidemic, but further research is needed to better understand the complex interplays between body fat accumulation and cardiometabolic disorders, in order to develop specific and culturally-appropriate interventions for Nunavimmiut.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/nu16050725/s1, Table S1: Associations between anthropometric indices and body fat composition measures among Inuit; Table S2: Association between anthropometric indices and cardiometabolic risk factors among Inuit; Table S3: Subgroup analysis of the association between anthropometric indices and cardiometabolic risk factors in Inuit men; Table S4: Subgroup analysis of the association between anthropometric indices and cardiometabolic risk factors in Inuit premenopausal women (estimated by age under 55 years old); Table S5: Subgroup analysis of the association between anthropometric indices and cardiometabolic risk factors in Inuit aged 20 years old and more; Table S6: Ideal anthropometric indices cut-offs to detect cardiometabolic disorders among Inuit; Table S7: Obesity features and associated cardiometabolic comorbidities of Nunavimmiut men and women aged 50 years old and more.
Author Contributions
Conceptualization, F.L.-T., M.-E.P. and P.P.; methodology, F.L.-T. and M.-E.P.; software, F.L.-T.; validation, P.A.; formal analysis, F.L.-T.; investigation, P.A.; resources, P.A.; data curation, P.A.; writing—original draft preparation, F.L.-T.; writing—review and editing, F.L.-T., M.-E.P., P.P., A.T. and P.A.; supervision, M.-E.P., P.P. and P.A.; project administration, P.A.; funding acquisition, P.A. All authors have read and agreed to the published version of the manuscript.
Funding
The financial support of ArcticNet—a Network of Excellence of Canada—is gratefully acknowledged (project P 11).
Institutional Review Board Statement
Centre de Recherche du CHU de Québec—Université Laval (no. 2016-2499-21; approval date: 24 October 2016).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The survey data are owned by Inuit and can be accessed through a request made to Qanuilirpitaa? 2017 DMC (nunavikhealthsurvey@ssss.gouv.qc.ca).
Acknowledgments
We would like to thank all Nunavimmiut participants who took part in the survey, as well as Veronique Boiteau who assisted with the analysis of the data and Marie-Josée Gauthier who helped our team with the results’ dissemination within Nunavik communities.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Batal, M.; Decelles, S. A Scoping Review of Obesity among Indigenous Peoples in Canada. J. Obes. 2019, 2019, 9741090. [Google Scholar] [CrossRef]
- Kellett, S.; Poirier, P.; Dewailly, E.; Sampasa, H.; Chateau-Degat, M.L. Is severe obesity a cardiovascular health concern in the Inuit population? Am. J. Hum. Biol. 2012, 24, 441–445. [Google Scholar] [CrossRef]
- Garnier, R.; Carrière, G.; Sanmartin, C. The Health of First Nations Living Off-Reserve, Inuit, and Métis Adults in Canada: The Impact of Socio-Economic Status on Inequalities in Health; Health Research Working Paper Series; Statistics Canada: Ottawa, ON, Canada, 2010. [Google Scholar]
- Allaire, J.; Levesque, B.; Poirier, P.; Gagnon, C.; Auclair, G.; Lemire, M.; Ayotte, P. Prevalence and determinants of hypertension in the adult Inuit population of Nunavik (northern Quebec, Canada). Can. J. Public Health 2023, 115, 168–179. [Google Scholar] [CrossRef]
- Chateau-Degat, M.L.; Dewailly, E.; Louchini, R.; Counil, E.; Noel, M.; Ferland, A.; Lucas, M.; Valera, B.; Ekoé, J.M.; Ladouceur, R.; et al. Cardiovascular burden and related risk factors among Nunavik (Quebec) Inuit: Insights from baseline findings in the circumpolar Inuit Health in Transition cohort study. Can. J. Cardiol. 2010, 26, 190–196. [Google Scholar] [CrossRef]
- Chateau-Degat, M.L.; Dannenbaum, D.A.; Egeland, G.M.; Nieboer, E.; Laouan Sidi, E.A.; Abdous, B.; Dewailly, E. A comparison of the metabolic response to abdominal obesity in two Canadian Inuit and First Nations population. Obesity 2011, 19, 2254–2260. [Google Scholar] [CrossRef]
- Young, T.K. Obesity, central fat patterning, and their metabolic correlates among the inuit of the central Canadian Arctic. Hum. Biol. 1996, 68, 245–263. [Google Scholar]
- Piche, M.E.; Tchernof, A.; Despres, J.P. Obesity Phenotypes, Diabetes, and Cardiovascular Diseases. Circ. Res. 2020, 126, 1477–1500. [Google Scholar] [CrossRef]
- Tchernof, A.; Despres, J.P. Pathophysiology of human visceral obesity: An update. Physiol. Rev. 2013, 93, 359–404. [Google Scholar] [CrossRef] [PubMed]
- Prince, S.A.; McDonnell, L.A.; Turek, M.A.; Visintini, S.; Nahwegahbow, A.; Kandasamy, S.; Sun, L.Y.; Coutinho, T. The State of Affairs for Cardiovascular Health Research in Indigenous Women in Canada: A Scoping Review. Can. J. Cardiol. 2018, 34, 437–449. [Google Scholar] [CrossRef] [PubMed]
- Hedayat, L.M.A.; Murchison, C.C.; Foulds, H.J.A. A systematic review and meta-analysis of cardiorespiratory fitness among Indigenous populations in North America and circumpolar Inuit populations. Prev. Med. 2018, 109, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Wharton, S.; Lau, D.C.W.; Vallis, M.; Sharma, A.M.; Biertho, L.; Campbell-Scherer, D.; Adamo, K.; Alberga, A.; Bell, R.; Boule, N.; et al. Obesity in adults: A clinical practice guideline. CMAJ 2020, 192, E875–E891. [Google Scholar] [CrossRef] [PubMed]
- Wharton, S.; Pedersen, S.D.; Lau, D.C.; Sharma, A.M.; Diabetes Canada Clinical Practice Guidelines Expert Committee. Weight Management in Diabetes. Can. J. Diabetes 2018, 42, S124–S129. [Google Scholar] [CrossRef] [PubMed]
- Després, J.P.; Carpentier, A.C.; Tchernof, A.; Neeland, I.J.; Poirier, P. Management of Obesity in Cardiovascular Practice: JACC Focus Seminar. J. Am. Coll. Cardiol. 2021, 78, 513–531. [Google Scholar] [CrossRef] [PubMed]
- Aziz, H.; Marchand, M.; Pop, C.; King, A.; Anand, S.S.; Arbour, L.; Atzema, C.; Spaziano, M.; Merveille, N.; Filimon, S.; et al. A Call to Action: Optimizing Indigenous Cardiovascular Health in Canada. Can. J. Cardiol. 2022, 38, 1584–1587. [Google Scholar] [CrossRef] [PubMed]
- Hamel, D.; Hamel, G.; Gagnon, S. Qanuilirpitaa? 2017 Nunavik Inuit Health Survey: Methodological Report. Nunavik Regional Board of Health and Social Services & Institut National de Santé Publique du Québec (INSPQ). Available online: http://nrbhss.ca/en/health-surveys (accessed on 4 January 2024).
- Faria, S.L.; Faria Op Fau-Cardeal, M.D.A.; Cardeal Md Fau-Ito, M.K.; Ito, M.K. Validation study of multi-frequency bioelectrical impedance with dual-energy X-ray absorptiometry among obese patients. Obes. Surg. 2014, 24, 1476–1480. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung and Blood Institute. Managing Overweight and Obesity in Adults: Systematic Evidence Review from the Obesity Expert Panel, 2013. US Department of Health and Human Services: National Institutes of Health. 2013. Available online: https://www.nhlbi.nih.gov/health-topics/managing-overweight-obesity-in-adults (accessed on 4 January 2024).
- Utter, A.C.; Nieman, D.C.; Ward, A.N.; Butterworth, D.E. Use of the leg-to-leg bioelectrical impedance method in assessing body-composition change in obese women. Am. J. Clin. Nutr. 1999, 69, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Liu, Y.A.-O.; Yan, C.; Yang, R.; Xu, L.; Guo, Z.; Yu, A.; Cheng, X.A.-O.; Ma, L.; Hu, C.; et al. Measurement of visceral fat and abdominal obesity by single-frequency bioelectrical impedance and CT: A cross-sectional study. BJM Open 2021, 11, e048221. [Google Scholar] [CrossRef]
- Schorr, M.; Dichtel, L.E.; Gerweck, A.V.; Valera, R.D.; Torriani, M.; Miller, K.K.; Bredella, M.A. Sex differences in body composition and association with cardiometabolic risk. Biol. Sex. Differ 2018, 9, 28. [Google Scholar] [CrossRef]
- Lear, S.A.; James, P.T.; Ko, G.T.; Kumanyika, S. Appropriateness of waist circumference and waist-to-hip ratio cutoffs for different ethnic groups. Eur. J. Clin. Nutr. 2010, 64, 42–61. [Google Scholar] [CrossRef]
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar] [PubMed]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Manjoo, P.; Dannenbaum, D.; Joseph, L.; Torrie, J.; Dasgupta, K. Utility of current obesity thresholds in signaling diabetes risk in the James Bay Cree of Eeyou Istchee. BMJ Open Diabetes Res. Care 2015, 3, e000114. [Google Scholar] [CrossRef] [PubMed]
- Punthakee, Z.; Goldenberg, R.; Katz, P.; Diabetes Canada Clinical Practice Guidelines Expert Committee. Definition, Classification and Diagnosis of Diabetes, Prediabetes and Metabolic Syndrome. Can. J. Diabetes 2018, 42, S10–S15. [Google Scholar] [CrossRef] [PubMed]
- Pearson, G.J.; Thanassoulis, G.; Anderson, T.J.; Barry, A.R.; Couture, P.; Dayan, N.; Francis, G.A.; Genest, J.; Grégoire, J.; Grover, S.A.; et al. 2021 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in Adults. Can. J. Cardiol. 2021, 37, 1129–1150. [Google Scholar] [CrossRef] [PubMed]
- Stevens, P.E.; Levin, A.; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The Fatty Liver Index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006, 6, 33. [Google Scholar] [CrossRef]
- Sterling, R.K.; Lissen, E.; Clumeck, N.; Sola, R.; Correa, M.C.; Montaner, J.; Sulkowski, M.S.; Torriani, F.J.; Dieterich, D.T.; Thomas, D.L.; et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006, 43, 1317–1325. [Google Scholar] [CrossRef]
- Shah, A.G.; Lydecker, A.; Murray, K.; Tetri, B.N.; Contos, M.J.; Sanyal, A.J.; Nash Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 2009, 7, 1104–1112. [Google Scholar] [CrossRef]
- Muhammad, A.G.; Hansen, F.O.; Gantzel, R.H.; Rex, K.F.; Villadsen, G.E.; Gronbaek, H.; Pedersen, M.L. Non-alcoholic fatty liver disease in patients with type 2 diabetes in Greenland: A register-based cross-sectional study. Int. J. Circumpolar Health 2022, 81, 2065755. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Hughes, G. Youden’s index and the weight of evidence. Methods Inf. Med. 2015, 54, 198–199. [Google Scholar] [CrossRef]
- Riediger, N.; Ian, C. Prevalence of metabolic syndrome in the Canadian adult population. CMAJ 2011, 183, E1127–E1133. [Google Scholar] [CrossRef]
- Erem, C.; Hacıhasanoglu, A.; Deger, O.; Topbaş, M.; Hosver, I.; Ersoz, H.O.; Can, G. Prevalence of metabolic syndrome and associated risk factors among Turkish adults: Trabzon MetS study. Endocrine 2008, 33, 9–20. [Google Scholar] [CrossRef]
- Esteghamati, A.; Meysamie, A.; Khalilzadeh, O.; Rashidi, A.; Haghazali, M.; Asgari, F.; Kamgar, M.; Gouya, M.M.; Abbasi, M. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007) in Iran: Methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health 2009, 9, 167. [Google Scholar] [CrossRef]
- Rowe, A.; Hernandez, P.; Kuhle, S.; Kirkland, S. The association between anthropometric measures and lung function in a population-based study of Canadian adults. Respir. Med. 2017, 131, 199–204. [Google Scholar] [CrossRef]
- Statistics Canada. Overweight and Obese Adults, 2018. Health Fact Sheet 2019, 82, 65. [Google Scholar]
- Ronn, P.F.; Andersen, G.S.; Lauritzen, T.; Christensen, D.L.; Aadahl, M.; Carstensen, B.; Grarup, N.; Jorgensen, M.E. Abdominal visceral and subcutaneous adipose tissue and associations with cardiometabolic risk in Inuit, Africans and Europeans: A cross-sectional study. BMJ Open 2020, 10, e038071. [Google Scholar] [CrossRef]
- Ronn, P.F.; Andersen, G.S.; Lauritzen, T.; Christensen, D.L.; Aadahl, M.; Carstensen, B.; Jorgensen, M.E. Ethnic differences in anthropometric measures and abdominal fat distribution: A cross-sectional pooled study in Inuit, Africans and Europeans. J. Epidemiol. Community Health 2017, 71, 536–543. [Google Scholar] [CrossRef]
- Lajeunesse-Trempe, F.; Dufour, R.; du Souich, P.; Paquette, M.; Kaduka, L.U.; Christensen, D.L. Anthropometric measures and their association with risk factors for cardio-metabolic diseases in Kenyan adults. Ann. Hum. Biol. 2018, 45, 486–495. [Google Scholar] [CrossRef]
- Statistics Canada. Niveaux de cholesterol chez les adultes 2012 à 2013, 2018. Health Fact Sheet 2014, 82, 65. [Google Scholar]
- Statistics Canada. Diabetes in Canada: Facts and Figures from a Public Health Perspective. Available online: https://www.canada.ca/en/public-health/services/chronic-diseases/reports-publications/diabetes/diabetes-canada-facts-figures-a-public-health-perspective.html (accessed on 7 January 2024).
- Government of Canada. Heart Disease in Canada: Highlights from the Canadian Chronic Disease Surveillance System. Available online: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/heart-disease-canada-fact-sheet.html (accessed on 6 January 2024).
- Swain, M.G.; Ramji, A.; Patel, K.; Sebastiani, G.; Shaheen, A.A.; Tam, E.; Marotta, P.; Elkhashab, M.; Bajaj, H.S.; Estes, C.; et al. Burden of nonalcoholic fatty liver disease in Canada, 2019–2030: A modelling study. CMAJ Open 2020, 8, E429–E436. [Google Scholar] [CrossRef]
- Nazare, J.A.; Smith, J.D.; Borel, A.L.; Haffner, S.M.; Balkau, B.; Ross, R.; Massien, C.; Almeras, N.; Despres, J.P. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: The International Study of Prediction of Intra-Abdominal Adiposity and Its Relationship With Cardiometabolic Risk/Intra-Abdominal Adiposity. Am. J. Clin. Nutr. 2012, 96, 714–726. [Google Scholar] [CrossRef]
- Guerrero, R.; Vega, G.L.; Grundy, S.M.; Browning, J.D. Ethnic differences in hepatic steatosis: An insulin resistance paradox? Hepatology 2009, 49, 791–801. [Google Scholar] [CrossRef]
- Labonté, M.È.; Dewailly, É.; Lucas, M.; Chateau-Degat, M.L.; Couture, P.; Lamarche, B. Traditional dietary pattern is associated with elevated cholesterol among the Inuit of Nunavik. J. Acad. Nutr. Diet. 2014, 114, 1208–1215.e3. [Google Scholar] [CrossRef]
- Lewis, J.A.-O.X.; Lind, M.V.; Møller, G.; Hansen, T.; Pedersen, H.; Christensen, M.M.B.; Laursen, J.C.; Nielsen, S.; Ottendahl, C.B.; Larsen, C.V.L.; et al. The effect of traditional diet on glucose homoeostasis in carriers and non-carriers of a common TBC1D4 variant in Greenlandic Inuit: A randomised crossover study. Br. J. Nutr. 2023, 130, 1871–1884. [Google Scholar] [CrossRef]
- Marushka, L.; Batal, M.; David, W.; Schwartz, H.; Ing, A.; Fediuk, K.; Sharp, D.; Black, A.; Tikhonov, C.; Chan, H.M. Association between fish consumption, dietary omega-3 fatty acids and persistent organic pollutants intake, and type 2 diabetes in 18 First Nations in Ontario, Canada. Environ. Res. 2017, 156, 725–737. [Google Scholar] [CrossRef]
- Girard, C.A.-O.; Tromas, N.; Amyot, M.; Shapiro, B.A.-O. Gut Microbiome of the Canadian Arctic Inuit. Microorganisms 2023, 11, 625. [Google Scholar] [CrossRef]
- Singh, K.; Chan, H.M. Persistent organic pollutants and diabetes among Inuit in the Canadian Arctic. Environ. Int. 2017, 101, 183–189. [Google Scholar] [CrossRef]
- Manousaki, D.; Kent, J.W., Jr.; Haack, K.; Zhou, S.; Xie, P.; Greenwood, C.M.; Brassard, P.; Newman, D.E.; Cole, S.; Umans, J.G.; et al. Toward Precision Medicine: TBC1D4 Disruption Is Common Among the Inuit and Leads to Underdiagnosis of Type 2 Diabetes. Diabetes Care 2016, 39, 1889–1895. [Google Scholar] [CrossRef]
- Galloway, T.; Chateau-Degat, M.L.; Egeland, G.M.; Young, T.K. Does sitting height ratio affect estimates of obesity prevalence among Canadian Inuit? Results from the 2007–2008 Inuit Health Survey. Am. J. Hum. Biol. 2011, 23, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Charbonneau-Roberts, G.; Saudny-Unterberger, H.; Kuhnlein, H.V.; Egeland, G.M. Body mass index may overestimate the prevalence of overweight and obesity among the Inuit. Int. J. Circumpolar Health 2005, 64, 163–169. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).