Association between Child Nutritional Anthropometric Indices and Iron Deficiencies among Children Aged 6–59 Months in Nepal
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Participants
2.3. Data Collection
2.4. Anthropometric Measurements
2.5. Biological Indicators
2.6. Specimen Collection and Processing
2.7. Study Outcomes
3. Exposure Variables
3.1. Stunting (Height-for-Age)
3.2. Wasting (Weight-for-Height)
3.3. Underweight (Weight-for-Age)
3.4. Potential Confounding Variables
3.5. Statistical Analysis
4. Results
4.1. Characteristics of the Sample
4.2. Prevalence of Anaemia and Iron Deficiency by Nutritional Anthropometric Index
4.2.1. Anaemia
4.2.2. Iron Deficiency (Ferritin Biomarker)
4.2.3. Iron Deficiency (sTfR Biomarker)
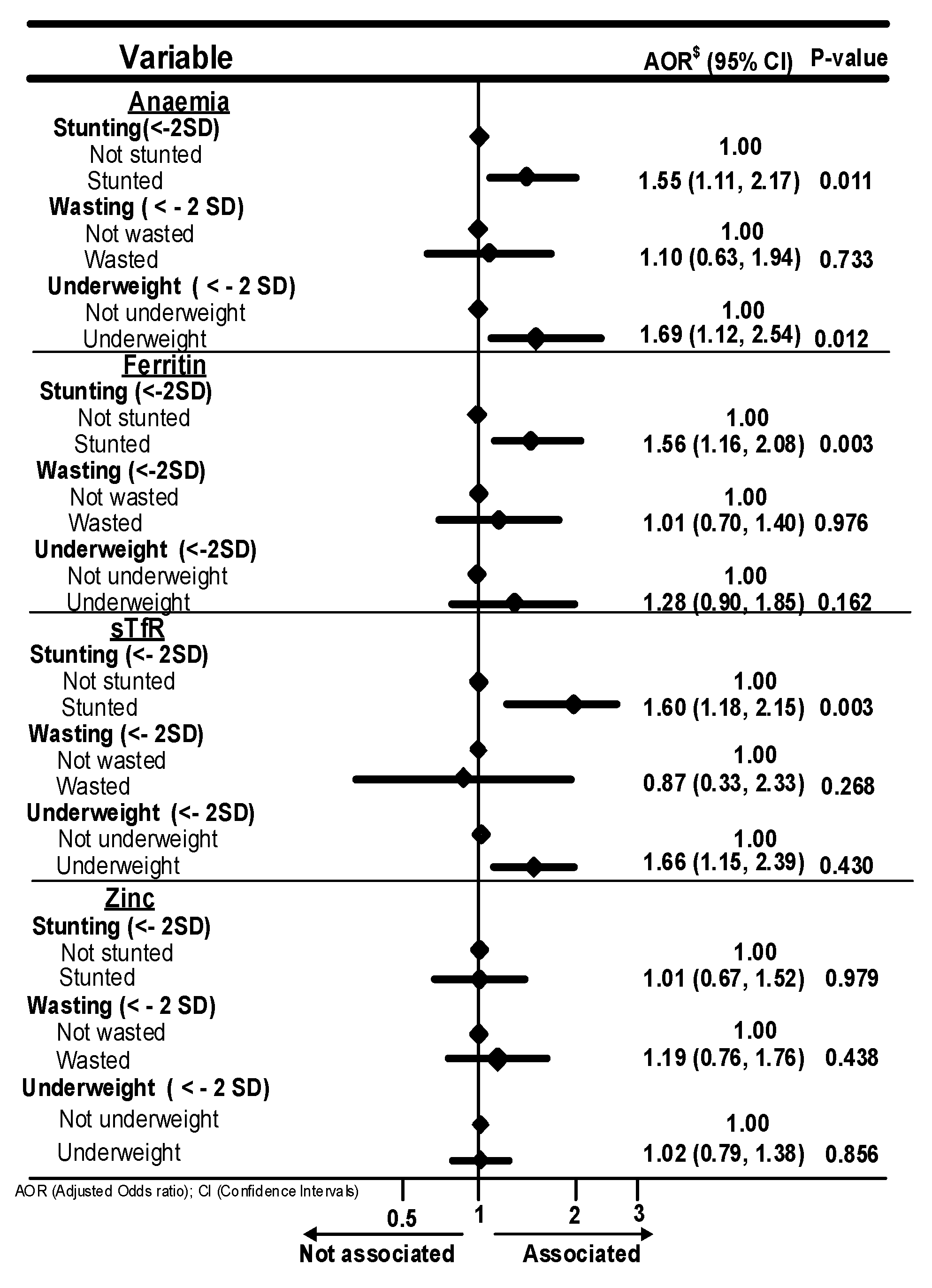
4.2.4. Association of Nutritional Anthropometric Indices with Anaemia and Iron Deficiencies
5. Discussion
6. Recommendations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kalaivani, K. Prevalence & consequences of anaemia in pregnancy. Indian J. Med. Res. 2009, 130, 627–633. [Google Scholar] [PubMed]
- Crawley, J. Reducing the burden of anemia in infants and young children in malaria-endemic countries of Africa: From evidence to action. Am. J. Trop. Med. Hyg. 2004, 71 (Suppl. 2), 25–34. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Iron Deficiency Anaemia: Assessment, Prevention, and Control. 2001. Available online: http://apps.who.int/iris/bitstream/10665/66914/1/WHO_NHD_01.3.pdf?ua=1 (accessed on 9 September 2018).
- Anaemias, W.N. Tools for Effective Prevention and Control; World Health Organization: Geneva, Switzerland, 2017; pp. 1–83. [Google Scholar]
- Engle-Stone, R.; Aaron, G.J.; Huang, J.; Wirth, J.P.; Namaste, S.M.; Williams, A.M.; Peerson, J.M.; Rohner, F.; Varadhan, R.; Addo, O.Y.; et al. Predictors of anemia in preschool children: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am. J. Clin. Nutr. 2017, 106 (Suppl. 1), 402S–415S. [Google Scholar] [CrossRef] [PubMed]
- Green, R.; Mitra, A.D. Megaloblastic anemias: Nutritional and other causes. Med. Clin. 2017, 101, 297–317. [Google Scholar]
- Global Health Metrics. Anaemia–Level 1 Impairment. Lancet 2019, 393. Available online: https://www.healthdata.org/research-analysis/diseases-injuries/factsheets/anemia-level-1-impairment (accessed on 27 December 2023).
- WHO. UNICEF Focusing on Anaemia: Towards an Integrated Approach for Effective Anaemia Control. 2004. Available online: https://www.who.int/publications/m/item/focusing-on-anaemia-towards-an-integrated-approach-for-effective-anaemia-control (accessed on 9 September 2018).
- Stevens, G.A.; Finucane, M.M.; De-Regil, L.M.; Paciorek, C.J.; Flaxman, S.R.; Branca, F.; Peña-Rosas, J.P.; Bhutta, Z.A.; Ezzati, M. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: A systematic analysis of population-representative data. Lancet Glob. Health 2013, 1, e16–e25. [Google Scholar] [CrossRef]
- Sustainable Development Goals. Available online: https://sustainabledevelopment.un.org/ (accessed on 9 September 2018).
- UNICEF The State of the World’s Children. 2015. Available online: https://data.unicef.org/resources/state-worlds-children-2015/ (accessed on 9 September 2018).
- World Food Programme. A Manual: Measuring and Interpreting Malnutrition and Mortality; Nutrition Service WFP: Rome, Italy, 2005; pp. 1–222. [Google Scholar]
- Stevens, G.A.; Finucane, M.M.; De-Regil, L.M.; Paciorek, C.J.; Flaxman, S.R.; Branca, F. Assessing the iron status of populations. Report of a Joint World Health Organization/Centers. Trends Cell Biol. 2020, 201424, 30312. [Google Scholar]
- Yip, R. Iron deficiency: Contemporary scientific issues and international programmatic approaches. J. Nutr. 1994, 124, S1479–S1490. [Google Scholar] [CrossRef]
- Suteerojntrakool, O.; Khongcharoensombat, T.; Chomtho, S.; Bongsebandhu-Phubhakdi, C.; Tempark, T.; Fewtrell, M. Anthropometric Markers and Iron Status of 6–12-Year-Old Thai Children: Associations and Predictors. J. Nutr. Metab. 2021, 2021, 9629718. [Google Scholar] [CrossRef]
- Ministry of Health Nepal; New ERA; UNICEF; EU; USAID; CDC. Nepal National Micronutrient Status Survey–2016; Minisry of Health, Nepal: Kathmandu, Nepal, 2017. [Google Scholar]
- World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Balcı, Y.I.; Karabulut, A.; Gürses, D.; Çövüt, I.E. Prevalence and risk factors of anemia among adolescents in Denizli, Turkey. Iran. J. Pediatr. 2012, 22, 77. [Google Scholar]
- Alzaheb, R.A.; Al-Amer, O. The Prevalence of Iron Deficiency Anemia and its Associated Risk Factors among a Sample of Female University Students in Tabuk, Saudi Arabia. Clin. Med. Insights: Women’s Health 2017, 10, 1179562X17745088. [Google Scholar] [CrossRef]
- Alaofè, H.; Burney, J.; Naylor, R.; Taren, D. Prevalence of anaemia, deficiencies of iron and vitamin A and their determinants in rural women and young children: A cross-sectional study in Kalalé district of northern Benin. Public Health Nutr. 2017, 20, 1203–1213. [Google Scholar] [CrossRef]
- Harding, K.L.; Aguayo, V.M.; Namirembe, G.; Webb, P. Determinants of anemia among women and children in Nepal and Pakistan: An analysis of recent national survey data. Matern. Child Nutr. 2018, 14, e12478. [Google Scholar] [CrossRef] [PubMed]
- Filmer, D.; Pritchett, L.H. Estimating Wealth Effects without Expenditure Data—Or Tears: An Application to Educational Enrollments in States of India. Demography 2001, 38, 115–132. [Google Scholar]
- Verhoef, H.; West, C.E.; Veenemans, J.; Beguin, Y.; Kok, F.J. Stunting may determine the severity of malaria-associated anemia in African children. Pediatrics 2002, 110, e48. [Google Scholar] [CrossRef]
- Mupfasoni, D.; Karibushi, B.; Koukounari, A.; Ruberanziza, E.; Kaberuka, T.; Kramer, M.H.; Mukabayire, O.; Kabera, M.; Nizeyimana, V.; Deville, M.-A. Polyparasite helminth infections and their association to anaemia and undernutrition in Northern Rwanda. PLoS Neglected Trop. Dis. 2009, 3, e517. [Google Scholar] [CrossRef]
- Bhandari, N.; Bahl, R.; Taneja, S. Effect of micronutrient supplementation on linear growth of children. Br. J. Nutr. 2001, 85, S131–S137. [Google Scholar] [CrossRef] [PubMed]
- Pandey, J.P.; Dhakal, M.R.; Sujan Karki, S.K.; Pradeep Poudel, P.P.; Pradhan, M.S. Maternal and Child Health in Nepal: The Effects of Caste, Ethnicity, and Regional Identity: Further Analysis of the 2011 Nepal Demographic and Health Survey. Available online: https://dhsprogram.com/publications/publication-fa73-further-analysis.cfm (accessed on 25 February 2024).
- Uyoga, M.A.; Karanja, S.; Paganini, D.; Cercamondi, C.I.; Zimmermann, S.A.; Ngugi, B.; Holding, P.; Moretti, D.; Zimmermann, M.B. Duration of exclusive breastfeeding is a positive predictor of iron status in 6-to 10-month-old infants in rural Kenya. Matern. Child Nutr. 2017, 13, e12386. [Google Scholar] [CrossRef]
- Tatala, S.; Kihamia, C.; Kyungu, L.; Svanbergrhaaa, U. Risk factors for anaemia in schoolchildren in Tanga Region, Tanzania. Tanzan. J. Health Res. 2008, 10, 4. [Google Scholar] [CrossRef]
- Ngesa, O.; Mwambi, H. Prevalence and risk factors of anaemia among children aged between 6 months and 14 years in Kenya. PLoS ONE 2014, 9, e113756. [Google Scholar] [CrossRef] [PubMed]
- Magalhaes, R.J.S.; Clements, A.C. Mapping the risk of anaemia in preschool-age children: The contribution of malnutrition, malaria, and helminth infections in West Africa. PLoS Med. 2011, 8, e1000438. [Google Scholar]
- Desalegn, A.; Mossie, A.; Gedefaw, L. Nutritional iron deficiency anemia: Magnitude and its predictors among school age children, southwest ethiopia: A community based cross-sectional study. PLoS ONE 2014, 9, e114059. [Google Scholar] [CrossRef]
- Herrador, Z.; Sordo, L.; Gadisa, E.; Buño, A.; Gómez-Rioja, R.; Iturzaeta, J.M.; de Armas, L.F.; Benito, A.; Aseffa, A.; Moreno, J. Micronutrient deficiencies and related factors in school-aged children in Ethiopia: A cross-sectional study in Libo Kemkem and Fogera districts, Amhara Regional State. PLoS ONE 2014, 9, e112858. [Google Scholar] [CrossRef]
- International Zinc Nutrition Consultative Group (IZiNCG). Determining the Risk of Zinc Deficiency: Assessment of Dietary Zinc Intake. 2007. Available online: https://static1.squarespace.com/static/56424f6ce4b0552eb7fdc4e8/t/5c7d940dc830258ac74be573/1551733775429/IZiNCG_Technical+Brief+%233_2nd+Ed_04Mar2019_final.pdf (accessed on 30 April 2018).
- Preziosi, P.; Prual, A.; Galan, P.; Daouda, H.; Boureima, H.; Hercberg, S. Effect of iron supplementation on the iron status of pregnant women: Consequences for newborns. Am. J. Clin. Nutr. 1997, 66, 1178–1182. [Google Scholar] [CrossRef] [PubMed]
- Kuziga, F.; Adoke, Y.; Wanyenze, R.K. Prevalence and factors associated with anaemia among children aged 6 to 59 months in Namutumba district, Uganda: A cross-sectional study. BMC Pediatr. 2017, 17, 25. [Google Scholar] [CrossRef] [PubMed]
- Chitekwe, S.; Parajuli, K.R.; Paudyal, N.; Haag, K.C.; Renzaho, A.; Issaka, A.; Agho, K. Individual, household and national factors associated with iron, vitamin A and zinc deficiencies among children aged 6–59 months in Nepal. Matern. Child Nutr. 2022, 18, e13305. [Google Scholar] [CrossRef] [PubMed]
- Belay, A.; Gashu, D.; Joy, E.J.; Lark, R.M.; Chagumaira, C.; Likoswe, B.H.; Zerfu, D.; Ander, E.L.; Young, S.D.; Bailey, E.H.; et al. Zinc deficiency is highly prevalent and spatially dependent over short distances in Ethiopia. Sci. Rep. 2021, 11, 6510. [Google Scholar] [CrossRef]
- Galetti, V.; Mitchikpè, C.E.; Kujinga, P.; Tossou, F.; Hounhouigan, D.J.; Zimmermann, M.B.; Moretti, D. Rural Beninese children are at risk of zinc deficiency according to stunting prevalence and plasma zinc concentration but not dietary zinc intakes. J. Nutr. 2016, 146, 114–123. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kavosi, E.; Rostami, Z.H.; Kavosi, Z.; Nasihatkon, A.; Moghadami, M.; Heidari, M. Prevalence and determinants of under-nutrition among children under six: A cross-sectional survey in Fars province, Iran. Int. J. Health Policy Manag. 2014, 3, 71. [Google Scholar] [CrossRef] [PubMed]
- Masibo, P.K.; Makoka, D. Trends and determinants of undernutrition among young Kenyan children: Kenya Demographic and Health Survey; 1993, 1998, 2003 and 2008–2009. Public Health Nutr. 2012, 15, 1715–1727. [Google Scholar] [CrossRef]
- Agho, K.E.; Inder, K.J.; Bowe, S.J.; Jacobs, J.; Dibley, M.J. Prevalence and risk factors for stunting and severe stunting among under-fives in North Maluku province of Indonesia. BMC Pediatr. 2009, 9, 64. [Google Scholar]
- Darteh, E.K.M.; Acquah, E.; Kumi-Kyereme, A. Correlates of stunting among children in Ghana. BMC Public Health 2014, 14, 504. [Google Scholar] [CrossRef]
- Akombi, B.J.; Agho, K.E.; Hall, J.J.; Merom, D.; Astell-Burt, T.; Renzaho, A.M. Stunting and severe stunting among children under-5 years in Nigeria: A multilevel analysis. BMC Pediatr. 2017, 17, 15. [Google Scholar] [CrossRef]
- Masiye, F.; Chama, C.; Chitah, B.; Jonsson, D. Determinants of child nutritional status in Zambia: An analysis of a national survey. Zamb. Soc. Sci. J. 2010, 1, 4. [Google Scholar]
- Tiwari, R.; Ausman, L.M.; Agho, K.E. Determinants of stunting and severe stunting among under-fives: Evidence from the 2011 Nepal Demographic and Health Survey. BMC Pediatr. 2014, 14, 239. [Google Scholar] [CrossRef] [PubMed]
- Biswas, S.; Bose, K. Association between place of delivery and undernutrition. Nutr Segm. 2011, 1, 154. [Google Scholar]
- Rahman, A.; Chowdhury, S. Determinants of chronic malnutrition among preschool children in Bangladesh. J. Biosoc. Sci. 2007, 39, 161–173. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | N (%) |
|---|---|
| Individual level factors | |
| Child’s age (months) | |
| 6–23 | 520 (30.6) |
| 24–59 | 1180 (69.4) |
| Child’s gender | |
| Male | 909 (53.5) |
| Female | 791 (46.5) |
| Relation to child | |
| Biological parents | 1643 (96.7) |
| Others | 57 (3.3) |
| Health status | |
| Child had fever | |
| Yes | 619 (36.4) |
| No | 1080 (61.6) |
| Child had cough | |
| Yes | 649 (38.2) |
| No | 1051 (61.8) |
| Child had diarrhoea | |
| Yes | 334 (19.6) |
| No | 1366 (80.4) |
| Anthropometry and nutrition | |
| Current Breastfeeding | |
| No | 1229 (71.9) |
| Yes | 481 (28.1) |
| Child Stunted (<−2 SD) | |
| No | 1095 (64.4) |
| Yes | 605 (35.6) |
| Child wasted (<−2 SD) | |
| No | 1495 (88.3) |
| Yes | 199 (11.7) |
| Child underweight (<−2 SD) | |
| No | 1206 (71.0) |
| Yes | 494 (29.0) |
| Household level factors | |
| Household Wealth Index | |
| Poor | 698 (41.1) |
| Middle | 676 (39.8) |
| Rich | 325 (19.1) |
| Ethnicity (Caste) | |
| Brahmin/Chettri | 518 (30.5) |
| Dalit | 313 (18.4) |
| Janajati | 496 (29.2) |
| Others | 371 (21.9) |
| Community level factors | |
| Residence | |
| Urban | 220 (13.0) |
| Rural | 1480 (87.0) |
| Geographical region | |
| Eastern | 369 (21.6) |
| Central | 620 (36.5) |
| Western | 297 (17.5) |
| Mid-western | 242 (14.3) |
| Far-western | 171 (10.1) |
| Ecological zone | |
| Mountain | 130 (7.6) |
| Hill | 709 (41.7) |
| Terai | 861 (50.7) |
| Dietary Diversity | |
| <4 foods | 1304 (76.7) |
| 4 or more foods Household food security | 395 (23.3) |
| Food security | 909 (53.5) |
| Mild food security | 183 (10.8) |
| Moderate food security | 464 (27.3) |
| Severe food insecurity | 143 (8.4) |
| Water and Sanitation | |
| Source of drinking water | |
| Improved | 1564 (92.0) |
| Unimproved | 136 (8.0) |
| Type of toilet facility | |
| Flush or Pour flush toilet | 1210 (71.2) |
| Pit Latrine | 490 (28.8) |
| Water treatment habit | |
| Yes | 282 (16.6) |
| No | 1417 (83.4) |
| Variable | Prevalence (95%CI) | OR (95% CI) | p-Value |
|---|---|---|---|
| Anaemia (Haemoglobin < 11.0 g/dL) | |||
| Stunting (<−2 SD) | |||
| Not stunted | 17.1 (13.9, 20.7) | 1.00 | |
| Stunted | 22.8 (18.3, 28.2) | 1.44 (1.04, 1.98) | 0.027 |
| Wasting (<−2 SD) | |||
| Not wasted | 16.9 (13.9, 20.6) | 1.00 | |
| Wasted | 24.4 (19.2, 30.5) | 1.58 (1.11, 2.26) | 0.012 |
| Underweight (<−2 SD) | |||
| Not underweight | 18.6 (15.4, 22.2) | 1.00 | |
| Underweight | 23.1 (15.6, 32.9) | 1.32 (0.78, 2.21) | 0.294 |
| BRINDA adjusted Ferritin (<15 μg/L) | |||
| Stunting (<−2 SD) | |||
| Not stunted | 33.1 (29.7, 36.7) | 1.00 | |
| Stunted | 40.1 (33.2, 47.5) | 1.35 (1.04, 1.77) | 0.026 |
| Wasting (<−2 SD) | |||
| Not wasted | 34.7 (30.8, 38.8) | 1.00 | |
| Wasted | 37.7 (31.0, 44.9) | 1.14 (0.87, 1.49) | 0.328 |
| Underweight (<−2 SD) | |||
| Not underweight | 35.2 (31.2, 39.3) | 1.00 | |
| Underweight | 39.2 (29.4, 49.8) | 1.19 (0.80, 1.77) | 0.397 |
| BRINDA adjusted sTfR (>8.3 mg/L) | |||
| Stunting (<−2 SD) | |||
| Not stunted | 34.8 (30.5, 39.4) | 1.00 | |
| Stunted | 40.3 (33.0, 48.0) | 1.26 (0.96, 1.66) | 0.089 |
| Wasting (<−2 SD) | |||
| Not wasted | 34.9 (30.2, 39.9) | 1.00 | |
| Wasted | 41.3 (34.3, 48.7) | 1.31 (0.99, 1.73) | 0.054 |
| Underweight (<−2 SD) | |||
| Not underweight | 36.8 (31.8, 42.0) | 1.00 | |
| Underweight | 37.3 (29.1, 46.3) | 1.02 (0.70, 1.49) | 0.906 |
| Zinc deficiency (adjusted serum zinc < 65.0 μg/dL) | |||
| Stunting (<−2 SD) | |||
| Not stunted | 20.3 (16.5, 24.7) | 1.00 | |
| Stunted | 20.8 (15.9, 26.8) | 1.03 (0.70, 1.51) | 0.874 |
| Wasting (<−2 SD) | |||
| Not wasted | 20.0 (16.9, 23.6) | 1.00 | |
| Wasted | 24.2 (16.3, 34.2) | 1.27 (0.81, 1.99) | 0.293 |
| Underweight (<−2 SD) | |||
| Not underweight | 20.1 (16.6, 24.1) | 1.00 | |
| Underweight | 21.3 (17.0, 26.3) | 1.08 (0.83, 1.40) | 0.579 |
| Characteristics | Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value |
|---|---|---|---|---|---|---|---|---|
| Anaemia | Ferritin | sTfR | Zinc | |||||
| Ecological zone | ||||||||
| Mountain | 1.00 | |||||||
| Hill | 1.39 (0.86, 2.25) | 0.170 | ||||||
| Terai | 3.80 (2.20, 6.59) | <0.001 | ||||||
| Place of residence | ||||||||
| Urban | 1.00 | |||||||
| Rural | 3.03 (1.56, 5.92) | 0.001 | ||||||
| Ethnicity (Caste) | ||||||||
| Brahmin/chettri | 1.00 | 1.00 | ||||||
| Dalit | 1.13 (0.70, 1.86) | 0.595 | 0.96 (0.61, 1.52) | 0.859 | ||||
| Janajati | 1.20 (0.76, 1.88) | 0.425 | 0.50 (0.32, 0.77) | 0.002 | ||||
| Others | 2.60 (1.65, 4.10) | <0.001 | 1.51 (1.08, 2.13) | 0.019 | ||||
| Child Age | ||||||||
| 24–59 months | 1.00 | 1.00 | 1.00 | |||||
| 6–23 months | 3.26 (2.43, 4.38) | <0.001 | 4.18 (3.00, 5.83) | <0.001 | 4.39 (3.39, 5.95) | <0.001 | ||
| Child had diarrhoea | ||||||||
| Yes | 1.00 | 1.00 | ||||||
| No | 0.61 (0.38, 0.97) | 0.036 | 0.63 (0.46, 0.86) | 0.004 | ||||
| Child’s household treated water | ||||||||
| No | 1.00 | |||||||
| Yes | 0.53 (0.34, 0.83) | 0.007 | ||||||
| Child had fever | ||||||||
| No | 1.00 | |||||||
| Yes | 1.83 (1.30, 0.57) | 0.001 | ||||||
| Household wealth index | ||||||||
| Food secure | 1.00 | |||||||
| Mild food security | 0.88 (0.53, 1.39) | 0.540 | ||||||
| Moderate food security | 1.24 (0.86, 1.80) | 0.244 | ||||||
| Severe food insecurity | 1.41 (1.00, 1.99) | 0.048 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agho, K.E.; Chitekwe, S.; Rijal, S.; Paudyal, N.; Sahani, S.K.; Akombi-Inyang, B.J. Association between Child Nutritional Anthropometric Indices and Iron Deficiencies among Children Aged 6–59 Months in Nepal. Nutrients 2024, 16, 698. https://doi.org/10.3390/nu16050698
Agho KE, Chitekwe S, Rijal S, Paudyal N, Sahani SK, Akombi-Inyang BJ. Association between Child Nutritional Anthropometric Indices and Iron Deficiencies among Children Aged 6–59 Months in Nepal. Nutrients. 2024; 16(5):698. https://doi.org/10.3390/nu16050698
Chicago/Turabian StyleAgho, Kingsley Emwinyore, Stanley Chitekwe, Sanjay Rijal, Naveen Paudyal, Sanjeev Kumar Sahani, and Blessing Jaka Akombi-Inyang. 2024. "Association between Child Nutritional Anthropometric Indices and Iron Deficiencies among Children Aged 6–59 Months in Nepal" Nutrients 16, no. 5: 698. https://doi.org/10.3390/nu16050698
APA StyleAgho, K. E., Chitekwe, S., Rijal, S., Paudyal, N., Sahani, S. K., & Akombi-Inyang, B. J. (2024). Association between Child Nutritional Anthropometric Indices and Iron Deficiencies among Children Aged 6–59 Months in Nepal. Nutrients, 16(5), 698. https://doi.org/10.3390/nu16050698







