Cost and Affordability of Habitual and Recommended Diets in Welfare-Dependent Households in Australia
Abstract
1. Introduction
2. Materials and Methods
2.1. Household Composition
2.2. Randomisation of Locations and Stores
2.3. Calculation of Household Income
2.4. Assessment of Diet Cost and Affordability
2.4.1. Diet Pricing Tools
2.4.2. Collection of Food and Drink Prices
2.5. Data Entry, Analysis and Reporting
3. Results
3.1. Cost of Habitual and Recommended Diets
3.1.1. Diet Cost in Median Households
3.1.2. Diet Cost in Welfare-Dependent Households Using Popular Brands
Comparison of Diet Cost in Median and Welfare-Dependent Households
3.1.3. Diet Cost in Welfare-Dependent Households Using Cheapest Available Products
Comparison of Diet Cost Using Popular Brands and Cheapest Available Products
3.1.4. Proportion of Habitual Diet Cost Spent on Discretionary Foods and Drinks
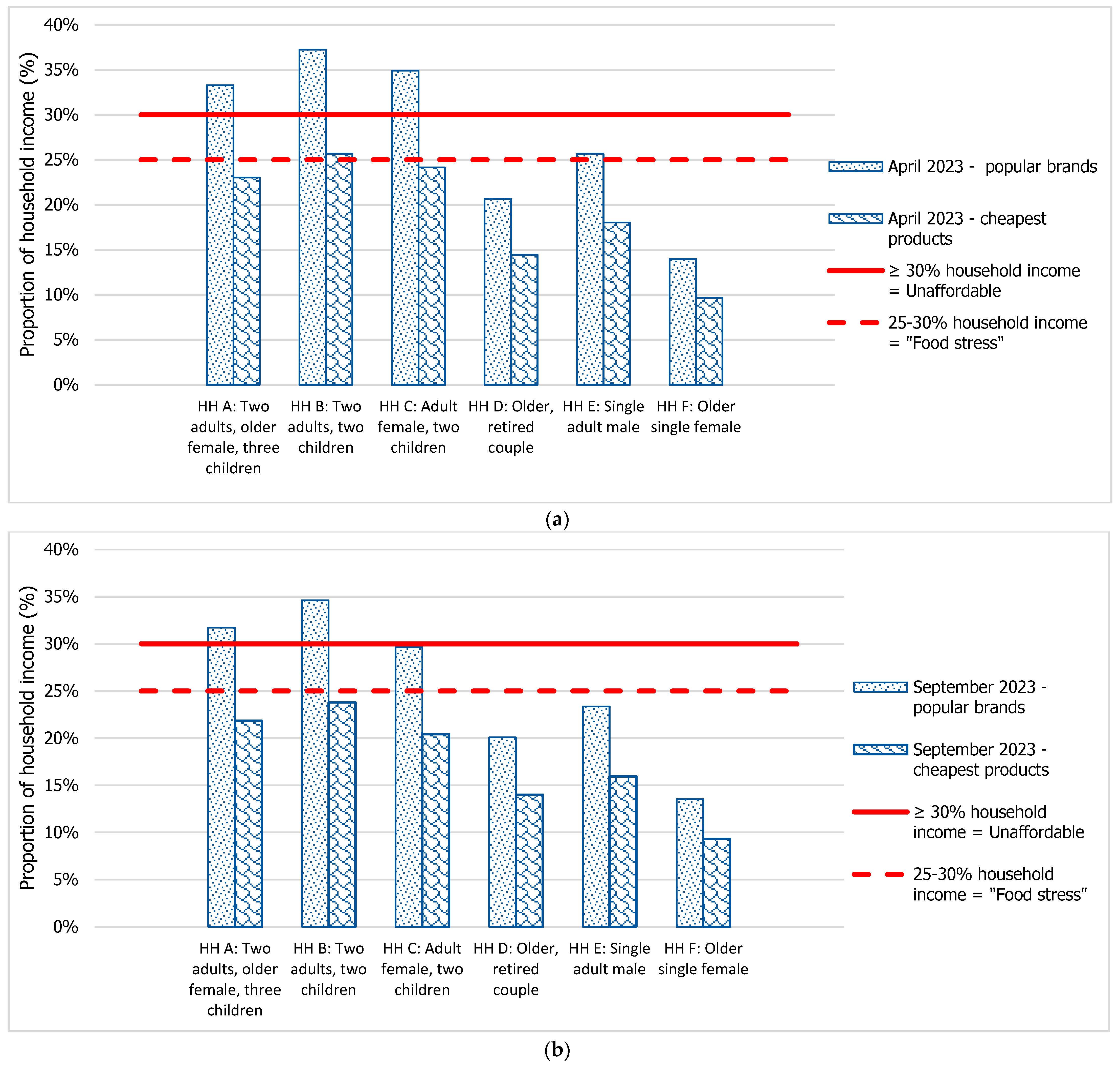
3.2. Diet Affordability in Welfare-Dependent Households
3.2.1. Household Income
3.2.2. Affordability of the Recommended Diet in Welfare-Dependent Households
4. Discussion
4.1. Cost of Habitual and Recommended Diets
4.2. Effect of Purchasing the Cheapest Available Option
4.3. Diet Affordability before and after Changes in Welfare
4.4. Differences in Diet Cost and Affordability in Households of Different Compositions
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Australian Institute of Health and Welfare. Australian Burden of Disease Study: Impact and Causes of Illness and Death in Australia 2018; AIHW: Canberra, Australia, 2021. [Google Scholar]
- GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Australian Dietary Guidelines—Providing the Scientific Evidence for Healthier Australian Diets; National Health and Medical Research Council: Canberra, Australia, 2013. [Google Scholar]
- National Health and Medical Research Council. Australian Guide to Healthy Eating; National Health and Medical Research Council: Canberra, Australia, 2013. [Google Scholar]
- Australian Bureau of Statistics. 4364.0.55.007—Australian Health Survey: Nutrition First Results—Foods and Nutrients, 2011–2012; Australian Bureau of Statistics: Canberra, Australia, 2014. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0072011-12?OpenDocument (accessed on 12 November 2017).
- Stringhini, S.; Carmeli, C.; Jokela, M.; Avendaño, M.; Muennig, P.; Guida, F.; Ricceri, F.; d’Errico, A.; Barros, H.; Bochud, M.; et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: A multicohort study and meta-analysis of 1.7 million men and women. Lancet 2017, 389, 1229–1237. [Google Scholar] [CrossRef] [PubMed]
- Harris, B.; Fetherston, H.; Calder, R. Australia’s Health Tracker by Socio-Economic Status 2017; Australian Health Policy Collaboration Victoria University: Melbourne, Australia, 2017. [Google Scholar]
- Australian Institute of Health and Welfare. Australia’s Health 2020—Health of Population Groups: Health across Socioeconomic Groups. Available online: https://www.aihw.gov.au/reports/australias-health/health-across-socioeconomic-groups (accessed on 27 January 2022).
- Livingstone, K.M.; Olstad, D.L.; Leech, R.M.; Ball, K.; Meertens, B.; Potter, J.; Cleanthous, X.; Reynolds, R.; McNaughton, S.A. Socioeconomic inequities in diet quality and nutrient intakes among Australian adults: Findings from a nationally representative cross-sectional study. Nutrients 2017, 9, 1092. [Google Scholar] [CrossRef] [PubMed]
- Lewis, M.; McNaughton, S.A.; Rychetnik, L.; Chatfield, M.D.; Lee, A.J. Dietary Intake, Cost, and Affordability by Socioeconomic Group in Australia. Int. J. Environ. Res. Public Health 2021, 18, 13315. [Google Scholar] [CrossRef] [PubMed]
- Friel, S.; Pescud, M.; Malbon, E.; Lee, A.; Carter, R.; Greenfield, J.; Cobcroft, M.; Potter, J.; Rychetnik, L.; Meertens, B. Using systems science to understand the determinants of inequities in healthy eating. PLoS ONE 2017, 12, e0188872. [Google Scholar] [CrossRef] [PubMed]
- Backholer, K.; Spencer, E.; Gearon, E.; Magliano, D.J.; McNaughton, S.A.; Shaw, J.E.; Peeters, A. The association between socio-economic position and diet quality in Australian adults. Public Health Nutr. 2016, 19, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Zorbas, C.; Palermo, C.; Chung, A.; Iguacel, I.; Peeters, A.; Bennett, R.; Backholer, K. Factors perceived to influence healthy eating: A systematic review and meta-ethnographic synthesis of the literature. Nutr. Rev. 2018, 76, 861–874. [Google Scholar] [CrossRef] [PubMed]
- INFORMAS about Us International Network for Food and Obesity/Non-Communicable Diseases Research Monitoring and Action Support; The University of Auckland: Auckland, New Zealand, 2013; Available online: https://www.informas.org/about-informas/ (accessed on 14 October 2021).
- Lee, A.J.; Kane, S.; Lewis, M.; Good, E.; Pollard, C.M.; Landrigan, T.J.; Dick, M. Healthy diets ASAP—Australian Standardised Affordability and Pricing methods protocol. Nutr. J. 2018, 17, 88. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Patay, D.; Herron, L.M.; Parnell Harrison, E.; Lewis, M. Affordability of current, and healthy, more equitable, sustainable diets by area of socioeconomic disadvantage and remoteness in Queensland: Insights into food choice. Int. J. Equity Health 2021, 20, 153. [Google Scholar] [CrossRef]
- Lee, A.J.; Patay, D.; Herron, L.M.; Tan, R.C.; Nicoll, E.; Fredericks, B.; Lewis, M. Affordability of Heathy, Equitable and More Sustainable Diets in Low-Income Households in Brisbane before and during the COVID-19 Pandemic. Nutrients 2021, 13, 4386. [Google Scholar] [CrossRef]
- Batis, C.; Marrón-Ponce, J.A.; Stern, D.; Vandevijvere, S.; Barquera, S.; Rivera, J.A. Adoption of healthy and sustainable diets in Mexico does not imply higher expenditure on food. Nat. Food 2021, 2, 792–801. [Google Scholar] [CrossRef]
- Vandevijvere, S.; Young, N.; Mackay, S.; Swinburn, B.; Gahegan, M. Modelling the cost differential between healthy and current diets: The New Zealand case study. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 16. [Google Scholar] [CrossRef] [PubMed]
- Youl, T. Supermarkets and Grocery Stores in Australia. AU Industry (ANZSIC) Report G4111. Available online: https://my.ibisworld.com/download/au/en/industry/1834/1/0/pdf (accessed on 10 September 2020).
- Chapman, K.; Innes-Hughes, C.; Goldsbury, D.; Kelly, B.; Bauman, A.; Allman-Farinelli, M. A comparison of the cost of generic and branded food products in Australian supermarkets. Public Health Nutr. 2013, 16, 894–900. [Google Scholar] [CrossRef] [PubMed]
- Zorbas, C.; Lee, A.; Peeters, A.; Lewis, M.; Landrigan, T.; Backholer, K. Streamlined data-gathering techniques to estimate the price and affordability of healthy and unhealthy diets under different pricing scenarios. Public Health Nutr. 2021, 24, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lewis, M.; McNaughton, S.A.; Rychetnik, L.; Lee, A.J. Cost and Affordability of Healthy, Equitable and Sustainable Diets in Low Socioeconomic Groups in Australia. Nutrients 2021, 13, 2900. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, J. You Don’t Have to Be an Economist to Know Australia is in a Cost-of-Living Crisis. What Are the Signs and What Needs to Change? The Conversation Media Group Ltd.: Canberra, Australia, 2023; Available online: https://theconversation.com/you-dont-have-to-be-an-economist-to-know-australia-is-in-a-cost-of-living-crisis-what-are-the-signs-and-what-needs-to-change-210373 (accessed on 15 December 2023).
- Office of the Prime Minister of Australia. Appointment of Dr Craig Emerson as Independent Reviewer of the Food and Grocery Code of Conduct; Office of the Prime Minister of Australia: Canberra, Australia, 2024. Available online: https://www.pm.gov.au/media/appointment-dr-craig-emerson-independent-reviewer-food-and-grocery-code-conduct (accessed on 24 January 2024).
- Eaton, M.; Jones, C. Supermarkets to Face Queensland Parliamentary Inquiry into High Cost of Groceries and Low Farmgate Prices. ABC News, 19 January 2024. [Google Scholar]
- Australian Bureau of Statistics. 6523.0—Household Income and Wealth, Australia, 2017–2018. Available online: https://www.abs.gov.au/statistics/economy/finance/household-income-and-wealth-australia/latest-release (accessed on 12 November 2019).
- Bradbury, A.; Whiteford, P. JobSeeker: How do Australia’s Unemployment Benefits Rank in the OECD? BusinessThink University of New South Wales Business School: Sydney, Australia, 2021; Available online: https://www.businessthink.unsw.edu.au/articles/jobseeker-australia-unemployment-benefits-oecd (accessed on 16 July 2023).
- Australian Council of Social Service. Poverty in Australia. Available online: https://povertyandinequality.acoss.org.au/poverty/ (accessed on 7 February 2022).
- Phillips, B.; Gray, M.; Joesph, C.; Webster, R. Newstart and Other Government Allowances: Incomes, Financial Stress and Poverty; Australian National University: Canberra, Australia, 2019. [Google Scholar]
- Saunders, P. Using a budget standards approach to assess the adequacy of newstart allowance. Aust. J. Soc. Issues 2018, 53, 4–17. [Google Scholar] [CrossRef]
- The Commonwealth of Australia. Budget Measures—Budget Paper No.2; The Treasury of the Australian Government, Ed.; The Commonwealth of Australia: Canberra, Australia, 2023. [Google Scholar]
- Australian Council of Social Service. Survey of 955 People Receiving the New Rate of Jobseeker and Other Allowances; Australian Council of Social Service: Canberra, Australia, 2020. Available online: https://www.acoss.org.au/wp-content/uploads/2020/06/200624-I-Can-Finally-Eat-Fresh-Fruit-And-Vegetables-Results-Of-The-Coronaviru.._.pdf (accessed on 29 July 2020).
- Payment and Service Finder Services Australia. 2023. Available online: https://www.servicesaustralia.gov.au/ (accessed on 20 September 2023).
- Australian Bureau of Statistics. 4324.0.55.002 Microdata: Australian Health Survey: Nutrition and Physical Activity, 2011–2012. 2013. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/PrimaryMainFeatures/4324.0.55.002?OpenDocument (accessed on 12 November 2017).
- Lee, A.J.; Lewis, M.; Goodwin, S. Healthy Diets ASAP Portal. Available online: https://healthydiets.azurewebsites.net/ (accessed on 10 August 2020).
- Australian Bureau of Statistics. 6401.0—Consumer Price Index, Australia, June 2023. Available online: https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/latest-release (accessed on 18 September 2023).
- Burns, C.; Friel, S. It’s time to determine the cost of a healthy diet in Australia. Aust. N. Zeal. J. Public Health 2007, 31, 363–365. [Google Scholar] [CrossRef] [PubMed]
- Landrigan, T.J.; Kerr, D.A.; Dhaliwal, S.S.; Pollard, C.M. Protocol for the Development of a Food Stress Index to Identify Households Most at Risk of Food Insecurity in Western Australia. Int. J. Environ. Res. Public Health 2018, 16, 79. [Google Scholar] [CrossRef] [PubMed]
- Hendrie, G.A.; Ridoutt, B.G.; Wiedmann, T.O.; Noakes, M. Greenhouse gas emissions and the Australian diet--comparing dietary recommendations with average intakes. Nutrients 2014, 6, 289–303. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Household Expenditure Survey, Australia: Summary of Results, 2015–2016. Available online: https://www.abs.gov.au/statistics/economy/finance/household-expenditure-survey-australia-summary-results/2015-16#data-downloads (accessed on 16 February 2024).
- Burns, C.; Cook, K.; Mavoa, H. Role of expendable income and price in food choice by low income families. Appetite 2013, 71, 209–217. [Google Scholar] [CrossRef]
- Queensland Council of Social Services. Living Affordability in Queensland; QCOSS: Brisbane, Australia, 2022. [Google Scholar]
- Rachwani, M. Australia’s Rental Affordability Drops to Worst Levels in Nearly a Decade. The Guardian, 29 May 2023. [Google Scholar]
- Kettings, C.; Sinclair, A.J.; Voevodin, M. A healthy diet consistent with Australian health recommendations is too expensive for welfare-dependent families. Aust. N. Z. J. Public Health 2009, 33, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Klapdor, M.; Thomas, M. Social Security Cost-of-Living Measures; Parliament of Australia: Canberra, Australia, 2023. [Google Scholar]
- Brownie, S.; Coutts, R. Older Australians’ perceptions and practices in relation to a healthy diet for old age: A qualitative study. J. Nutr. Health Aging 2013, 17, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Standing Committee on Indigenous Affairs. Report on Food Pricing and Food Security in Remote Indigenous Communities; Commonwealth of Australia, Ed.; The Parliament of the Commonwealth of Australia: Canberra, Australia, 2020. [Google Scholar]
- Australian Government. National Preventative Health Strategy 2021–2030; Department of Health, Ed.; Australian Government: Canberra, Australia, 2021. [Google Scholar]

| Household Structure | Two Adults, Older Female, Three Children (Household A) | Adult Male and Female, Two Children (Household B) | Adult Female, Two Children (Household C) | Older, Retired Couple (Household D) | Single Adult Male (Household E) | Older Single Female (Household F) |
|---|---|---|---|---|---|---|
| Median households | Female (31–50 y) Male (31–50 y) Older female (70+ y) Boy (14 y) Girl (8 y) Boy (4 y) | Female (31–50 y) Male (31–50 y) Boy (14 y) Girl (8 y) | Female (31–50 y) Boy (14 y) Girl (8 y) | Older female (70+ y) Older male (70+ y) | Male (31–50 y) | Older female, (70+ y) |
| Welfare-dependent households | Female (31–50 y) Male (31–50 y) Older female (70+ y) Boy (14–18 y *) Child (4–8 y *) Child (4–8 y *) | Female (31–50 y) Male (31–50 y) Boy (14–18 y *) Child (4–8 y *) | Female (31–50 y) Boy (14–18 y *) Child (4–8 y *) | Older female (70+ y) Older male (70+ y) | Male (31–50 y) | Older female, (70+ y) |
| Assumptions used to calculate welfare-dependent income | • Adult male is unemployed and looking for work • Adult female is a stay-at-home parent • Older female receives full age pension (maximum rate) • The children attend school/kindy • None of the family are disabled • No savings or investments • The family is living in public housing | • Both adults are unemployed and looking for work • Both children attend school • None of the family are disabled • No savings or investments • Private rent at AUD 379/week | • Adult female is unemployed and looking for work • No child support received • Both children attend school • None of the family are disabled • No savings or investments • Private rent at AUD 379/week | • Neither are in paid employment • Both receive the full age pension (maximum rate) • Neither are disabled or frail-aged • The couple has no dependent children • Private rent at AUD 379/week | • Is unemployed and looking for work • Is not disabled • No dependent children • No savings or investments • Is renting a room in 3-bedroom house at AUD 125/week (AUD 376/3) | • Not in paid employment • Receives full age pension (maximum rate) • Not disabled or frail-aged • Has no dependent children • Private rent at AUD 379/week |
| Habitual (Unhealthy) Diet | Recommended (Healthy) Diet |
|---|---|
| Healthy foods and drinks as per the seven food groups in the “Recommended diet” column; in reduced amounts reflecting reported intake. Artificially sweetened beverages. Discretionary (unhealthy) foods and drinks: Drinks: sugar sweetened beverages. Cereals, snacks, and desserts: muffin, sweet biscuits, savoury crackers, confectionery, chocolate, potato crisps, muesli bar, mixed nuts (salted), ice cream, fruit salad (canned in juice). Processed meats: beef sausages, ham. Spreads, sauces, condiments, and ingredients: butter, tomato sauce, salad dressing, white sugar. Convenience meals: frozen lasagne, chicken soup (canned), frozen fish fillet (crumbed), instant noodles, meat and vegetable stew (canned). Fast food: pizza, meat pie, hamburger, potato chips/fries. Alcohol: beer (full strength), white wine (sparkling), red wine, whisky. | Water (bottled). Fruit: apples, bananas, oranges. Vegetables: potatoes, broccoli, white cabbage, iceberg lettuce, onion, carrot, pumpkin, tomatoes, sweetcorn (canned), four bean mix (canned), diced tomatoes (canned), baked beans (canned), frozen mixed vegetables, frozen peas, salad vegetables in sandwiches. Grain (cereals): wholegrain cereal biscuits (Weet-bix™), rolled oats, cornflakes, wholemeal bread, white bread, white rice, white pasta, dry water crackers, bread in sandwiches. Lean meats and alternatives: beef mince and steak, lamb chops, cooked chicken, tuna (canned), eggs, peanuts (unsalted), meat in sandwiches. Milk, yoghurt, and cheese: cheddar cheese (full fat, reduced fat), milk (full fat, reduced fat), yoghurt (full fat plain, reduced fat flavoured). Unsaturated oils and spreads: olive oil, sunflower oil, canola (margarine). |
| Household | A: Two Adults, Older Female, Three Children | B: Two Adults, Two Children | C: Adult Female, Two Children | D: Older, Retired Couple | E: Single Adult Male | F: Older Single Female |
|---|---|---|---|---|---|---|
| Fortnightly income—April 2023 | AUD3192 | AUD 2033 | AUD 1591 | AUD 1752 | AUD 786 | AUD 1221 |
| Fortnightly income—September 2023 | AUD 3400 | AUD 2218 | AUD 1901 | AUD 1827 | AUD 875 | AUD 1282 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewis, M.; Nash, S.; Lee, A.J. Cost and Affordability of Habitual and Recommended Diets in Welfare-Dependent Households in Australia. Nutrients 2024, 16, 659. https://doi.org/10.3390/nu16050659
Lewis M, Nash S, Lee AJ. Cost and Affordability of Habitual and Recommended Diets in Welfare-Dependent Households in Australia. Nutrients. 2024; 16(5):659. https://doi.org/10.3390/nu16050659
Chicago/Turabian StyleLewis, Meron, Stephen Nash, and Amanda J. Lee. 2024. "Cost and Affordability of Habitual and Recommended Diets in Welfare-Dependent Households in Australia" Nutrients 16, no. 5: 659. https://doi.org/10.3390/nu16050659
APA StyleLewis, M., Nash, S., & Lee, A. J. (2024). Cost and Affordability of Habitual and Recommended Diets in Welfare-Dependent Households in Australia. Nutrients, 16(5), 659. https://doi.org/10.3390/nu16050659




