Plant-Based Diet and Glycemic Control in Type 2 Diabetes: Evidence from a Thai Health-Promoting Hospital
Abstract
1. Introduction
2. Materials and Methods
2.1. Participant Recruitment
2.2. Dietary Assessment
2.3. Calculation of the Plant Food Score (PFS)
2.4. Plasma Glucose Determination
2.5. Anthropometric Measurement
2.6. Statistical Analysis
3. Results
3.1. Characteristics of Controls and Diabetics
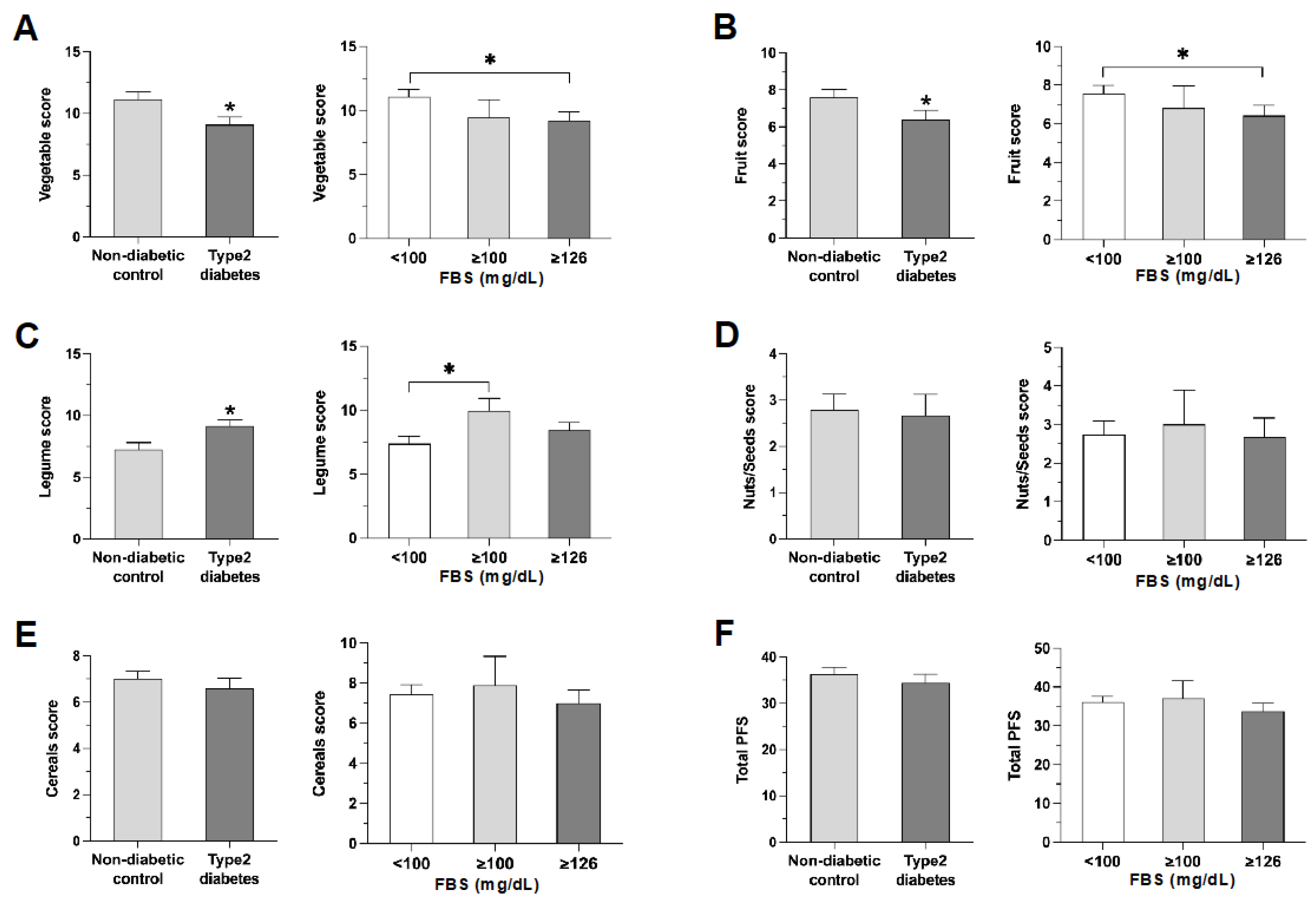
3.2. Comparing PFS in Diabetics and Controls
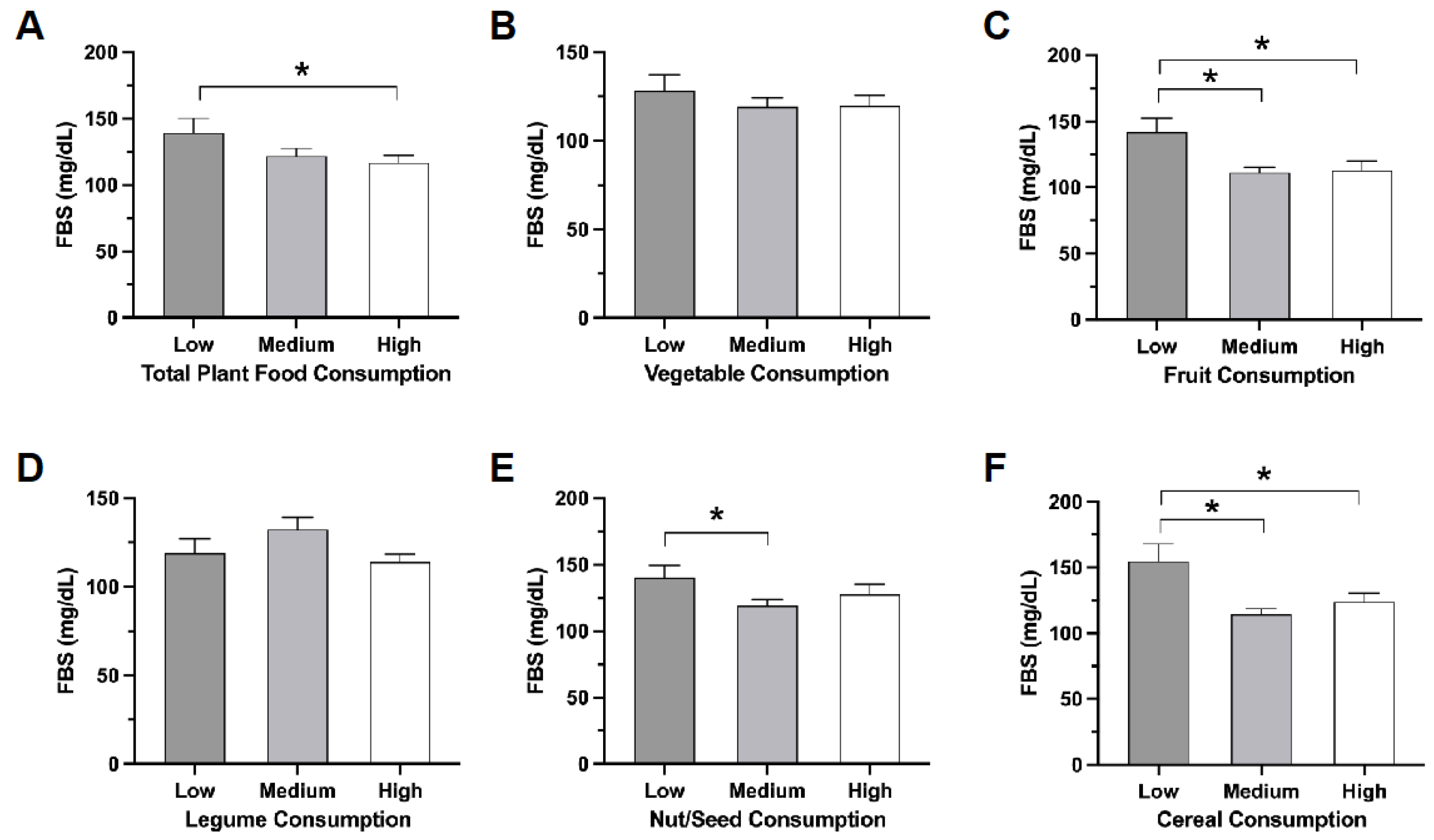
3.3. Effects of Specific Plant Food Groups on FBS Levels
3.4. Associations of High FSB and T2DM Diagnosis with Plant Foods
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Kaka, A.S.; Landsteiner, A.; Ensrud, K.E.; Logan, B.; Sowerby, C.; Ullman, K.; Yoon, P.; Wilt, T.J.; Sultan, S. Risk prediction models for diabetic foot ulcer development or amputation: A review of reviews. J. Foot Ankle Res. 2023, 16, 13. [Google Scholar] [CrossRef] [PubMed]
- Aekplakorn, W.; Chariyalertsak, S.; Kessomboon, P.; Assanangkornchai, S.; Taneepanichskul, S.; Putwatana, P. Prevalence of Diabetes and Relationship with Socioeconomic Status in the Thai Population: National Health Examination Survey, 2004–2014. J. Diabetes Res. 2018, 2018, 1654530. [Google Scholar] [CrossRef] [PubMed]
- Russo, S.; Kwiatkowski, M.; Govorukhina, N.; Bischoff, R.; Melgert, B.N. Meta-Inflammation and Metabolic Reprogramming of Macrophages in Diabetes and Obesity: The Importance of Metabolites. Front. Immunol. 2021, 12, 746151. [Google Scholar] [CrossRef] [PubMed]
- Toi, P.L.; Anothaisintawee, T.; Chaikledkaew, U.; Briones, J.R.; Reutrakul, S.; Thakkinstian, A. Preventive Role of Diet Interventions and Dietary Factors in Type 2 Diabetes Mellitus: An Umbrella Review. Nutrients 2020, 12, 2722. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Xu, J.; Chen, G.; Liu, H.; Liu, J.; Wang, J.; Zhang, X.; Hao, Y.; Wu, Q.; Jiao, M. Self-management behavior and fasting plasma glucose control in patients with type 2 diabetes mellitus over 60 years old: Multiple effects of social support on quality of life. Health Qual. Life Outcomes 2021, 19, 254. [Google Scholar] [CrossRef] [PubMed]
- Magkos, F.; Tetens, I.; Bügel, S.G.; Felby, C.; Schacht, S.R.; Hill, J.O.; Ravussin, E.; Astrup, A. A Perspective on the Transition to Plant-Based Diets: A Diet Change May Attenuate Climate Change, but Can It Also Attenuate Obesity and Chronic Disease Risk? Adv. Nutr. 2020, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, A.H.; Appel, L.J.; Vadiveloo, M.; Hu, F.B.; Kris-Etherton, P.M.; Rebholz, C.M.; Sacks, F.M.; Thorndike, A.N.; Van Horn, L.; Wylie-Rosett, J. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement from the American Heart Association. Circulation 2021, 144, e472–e487. [Google Scholar] [CrossRef] [PubMed]
- Storz, M.A. What makes a plant-based diet? A review of current concepts and proposal for a standardized plant-based dietary intervention checklist. Eur. J. Clin. Nutr. 2022, 76, 789–800. [Google Scholar] [CrossRef]
- Aschemann-Witzel, J.; Gantriis, R.F.; Fraga, P.; Perez-Cueto, F.J.A. Plant-based food and protein trend from a business perspective: Markets, consumers, and the challenges and opportunities in the future. Crit. Rev. Food Sci. Nutr. 2021, 61, 3119–3128. [Google Scholar] [CrossRef]
- Pointke, M.; Pawelzik, E. Plant-Based Alternative Products: Are They Healthy Alternatives? Micro- and Macronutrients and Nutritional Scoring. Nutrients 2022, 14, 601. [Google Scholar] [CrossRef] [PubMed]
- Yimthiang, S.; Pouyfung, P.; Khamphaya, T.; Kuraeiad, S.; Wongrith, P.; Vesey, D.A.; Gobe, G.C.; Satarug, S. Effects of Environmental Exposure to Cadmium and Lead on the Risks of Diabetes and Kidney Dysfunction. Int. J. Environ. Res. Public Health 2022, 19, 2259. [Google Scholar] [CrossRef]
- Kittisakmontri, K.; Lanigan, J.; Sangcakul, A.; Tim-Aroon, T.; Meemaew, P.; Wangaueattachon, K.; Fewtrell, M. Comparison of 24-Hour Recall and 3-Day Food Records during the Complementary Feeding Period in Thai Infants and Evaluation of Plasma Amino Acids as Markers of Protein Intake. Nutrients 2021, 13, 653. [Google Scholar] [CrossRef] [PubMed]
- Dennis, K.K.; Judd, S.E.; Alvarez, J.A.; Kahe, K.; Jones, D.P.; Hartman, T.J. Plant food intake is associated with lower cadmium body burden in middle-aged adults. Eur. J. Nutr. 2021, 60, 3365–3374. [Google Scholar] [CrossRef]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Xu, R.; Tan, X.; Li, T.; Liu, S.; Li, Y.; Li, H. Norepinephrine-induced AuPd aerogels with peroxidase- and glucose oxidase-like activity for colorimetric determination of glucose. Mikrochim. Acta 2021, 188, 362. [Google Scholar] [CrossRef]
- Satija, A.; Bhupathiraju, S.N.; Rimm, E.B.; Spiegelman, D.; Chiuve, S.E.; Borgi, L.; Willett, W.C.; Manson, J.E.; Sun, Q.; Hu, F.B. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. PLoS Med. 2016, 13, e1002039. [Google Scholar] [CrossRef] [PubMed]
- Glenn, A.J.; Li, J.; Lo, K.; Jenkins, D.J.A.; Boucher, B.A.; Hanley, A.J.; Kendall, C.W.C.; Shadyab, A.H.; Tinker, L.F.; Chessler, S.D.; et al. The Portfolio Diet and Incident Type 2 Diabetes: Findings from the Women’s Health Initiative Prospective Cohort Study. Diabetes Care 2023, 46, 28–37. [Google Scholar] [CrossRef]
- Chen, G.C.; Koh, W.P.; Neelakantan, N.; Yuan, J.M.; Qin, L.Q.; van Dam, R.M. Diet Quality Indices and Risk of Type 2 Diabetes Mellitus: The Singapore Chinese Health Study. Am. J. Epidemiol. 2018, 187, 2651–2661. [Google Scholar] [CrossRef]
- Kim, J.; Giovannucci, E. Healthful Plant-Based Diet and Incidence of Type 2 Diabetes in Asian Population. Nutrients 2022, 14, 3078. [Google Scholar] [CrossRef]
- Adebayo, F.A.; Itkonen, S.T.; Koponen, P.; Prättälä, R.; Härkänen, T.; Lamberg-Allardt, C.; Erkkola, M. Consumption of healthy foods and associated socio-demographic factors among Russian, Somali and Kurdish immigrants in Finland. Scand. J. Public Health 2017, 45, 277–287. [Google Scholar] [CrossRef]
- Nie, Q.; Chen, H.; Hu, J.; Fan, S.; Nie, S. Dietary compounds and traditional Chinese medicine ameliorate type 2 diabetes by modulating gut microbiota. Crit. Rev. Food Sci. Nutr. 2019, 59, 848–863. [Google Scholar] [CrossRef]
- Sun, C.; Zhao, C.; Guven, E.C.; Paoli, P.; Simal-Gandara, J.; Ramkumar, K.M.; Wang, S.; Buleu, F.; Pah, A.; Turi, V. Dietary polyphenols as antidiabetic agents: Advances and opportunities. Food Front. 2020, 1, 18–44. [Google Scholar] [CrossRef]
- Wang, Y.; Alkhalidy, H.; Liu, D. The Emerging Role of Polyphenols in the Management of Type 2 Diabetes. Molecules 2021, 26, 703. [Google Scholar] [CrossRef] [PubMed]
- Al-Jaidi, B.A.; Odetallah, H.a.M.; Chandrasekaran, B.; Amro, R. Herbal Medications for the Management of Diabetes Mellitus: A Review. Curr. Tradit. Med. 2020, 6, 332–350. [Google Scholar] [CrossRef]
- Chen, H.; Li, N. An Overview of Hypoglycemic Traditional Drugs. In Structure and Health Effects of Natural Products on Diabetes Mellitus; Springer: Berlin/Heidelberg, Germany, 2021; pp. 57–80. [Google Scholar]
- Santos-Sánchez, N.F.; Salas-Coronado, R.; Hernández-Carlos, B.; Villanueva-Cañongo, C. Shikimic acid pathway in biosynthesis of phenolic compounds. In Plant Physiological Aspects of Phenolic Compounds; Springer: Berlin/Heidelberg, Germany, 2019; Volume 1, pp. 1–15. [Google Scholar]
- Xu, L.; Zang, E.; Sun, S.; Li, M. Main flavor compounds and molecular regulation mechanisms in fruits and vegetables. Crit. Rev. Food Sci. Nutr. 2023, 63, 11859–11879. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xiong, B.; Zhu, M.; Ren, Y.; Lan, Y.; Hu, T.; Wang, Y.; Yang, H.; Liao, Z.; Xiao, K.; et al. Associations of starchy and non-starchy vegetables with risk of metabolic syndrome: Evidence from the NHANES 1999–2018. Nutr. Metab. 2023, 20, 36. [Google Scholar] [CrossRef] [PubMed]
- Becerra-Tomás, N.; Díaz-López, A.; Rosique-Esteban, N.; Ros, E.; Buil-Cosiales, P.; Corella, D.; Estruch, R.; Fitó, M.; Serra-Majem, L.; Arós, F.; et al. Legume consumption is inversely associated with type 2 diabetes incidence in adults: A prospective assessment from the PREDIMED study. Clin. Nutr. 2018, 37, 906–913. [Google Scholar] [CrossRef] [PubMed]
- Yu, G.; Fu, H.; Huang, W.; Zhang, N.; Deng, D.; Li, G.; Lei, H. A Dietary Pattern of Higher Fish, Egg, Milk, Nut, Vegetable and Fruit, and Lower Salt Intake Correlates with the Prevalence and Control of Hypertension. Am. J. Hypertens. 2018, 31, 679–686. [Google Scholar] [CrossRef]
- Murai, U.; Yamagishi, K.; Sata, M.; Kokubo, Y.; Saito, I.; Yatsuya, H.; Ishihara, J.; Inoue, M.; Sawada, N.; Iso, H.; et al. Seaweed intake and risk of cardiovascular disease: The Japan Public Health Center-based Prospective (JPHC) Study. Am. J. Clin. Nutr. 2019, 110, 1449–1455. [Google Scholar] [CrossRef]
- Han, K.C.; Wong, W.C.; Benzie, I.F. Genoprotective effects of green tea (Camellia sinensis) in human subjects: Results of a controlled supplementation trial. Br. J. Nutr. 2011, 105, 171–179. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ho, C.K.; Choi, S.W.; Siu, P.M.; Benzie, I.F. Effects of single dose and regular intake of green tea (Camellia sinensis) on DNA damage, DNA repair, and heme oxygenase-1 expression in a randomized controlled human supplementation study. Mol. Nutr. Food Res. 2014, 58, 1379–1383. [Google Scholar] [CrossRef]
- Choi, S.W.; Yeung, V.T.; Collins, A.R.; Benzie, I.F. Redox-linked effects of green tea on DNA damage and repair, and influence of microsatellite polymorphism in HMOX-1: Results of a human intervention trial. Mutagenesis 2015, 30, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Hahn, D.; Shin, S.H.; Bae, J.S. Natural Antioxidant and Anti-Inflammatory Compounds in Foodstuff or Medicinal Herbs Inducing Heme Oxygenase-1 Expression. Antioxidants 2020, 9, 1191. [Google Scholar] [CrossRef] [PubMed]

| Parameters | Non-Diabetic Control, n = 74 | Participants with Type 2 Diabetes, n = 61 | p-Value |
|---|---|---|---|
| Age, years | 60.10 ± 1.081 | 59.90 ± 1.320 | 0.089 |
| (Min, Max) | (41, 80) | (41, 81) | |
| FBS, mg/dL | 93.66 ± 1.243 | 177 ± 9.354 | 0.001 |
| (Min, Max) | (74, 143) | (110, 509) | |
| Female, n (%) | 60 (81.10) | 48 (78.7) | 0.729 |
| BMI, kg/m2 | 24.75 ± 0.545 | 25.88 ± 0.646 | 0.087 |
| (Min, Max) | (14.69, 36.04) | (15.09, 48.13) | |
| Underweight (<18.5) | 3 (4.05) | 6 (9.84) | |
| Normal weight (18.5–22.9) | 24 (32.43) | 12 (16.67) | |
| Overweight (23.0–24.9) | 12 (16.22) | 8 (13.11) | |
| Obese (25.0–29.9) | 30 (40.54) | 25 (40.98) | |
| Extremely obese (>30) | 5 (6.76) | 10 (16.39) | |
| Waist circumference, (cm) | 88.28 ± 1.267 | 93.60 ± 1.468 | 0.003 |
| (Min, Max) | (145, 174) | (65, 176) | |
| Smoker, n (%) | 9 (12.2) | 7 (11.5) | 0.902 |
| Alcoholic n (%) | 1 (1.40) | 5 (8.20) | 0.055 |
| Medicine n (%) | 6 (8.11) | 48 (78.69) | 0.000 |
| Dietary supplements n (%) | 3 (4.05) | 7 (11.48) | 0.101 |
| Hypertension, n (%) | 31(41.9) | 37 (60.7) | 0.030 |
| SBP, mmHg ≥ 140 | 134.30 ± 1.851 | 142.10 ± 2.182 | 0.004 |
| (Min. Max) | (141, 173) | (158, 183) | |
| DBP, mmHg ≥ 90 | 83.23 ± 1.084 | 84.42 ± 1.265 | 0.234 |
| (Min, Max) | (91, 103) | (91, 107) | |
| Body composition, body fat, n (%) | |||
| Low | 33 (44.6) | 27 (44.3) | 0.016 |
| Normal | 24 (32.4) | 9 (14.8) | |
| High | 13 (17.6) | 13 (21.3) | |
| Very high | 4 (5.40) | 12 (19.7) |
| Parameters | FBS (<100 mg/dL) n = 55 (%) | FBS (≥100 mg/dL) n = 80 (%) | Adjusted OR b | 95%CI | p-Value |
|---|---|---|---|---|---|
| Total PFS | |||||
| Low | 11 (20.00) | 22 (27.50) | Ref | ||
| Medium | 27 (49.09) | 34 (42.50) | 0.984 | 0.322–3.013 | 0.978 |
| High | 17 (30.91) | 24 (30.00) | 0.992 | 0.296–3.324 | 0.990 |
| Vegetables | |||||
| Low | 14 (25.45) | 21 (26.25) | Ref | ||
| Medium | 29 (52.73) | 39 (48.75) | 1.192 | 0.391–3.631 | 0.758 |
| High | 12 (21.82) | 20 (25.00) | 1.898 | 0.520–6.926 | 0.332 |
| Fruits | |||||
| Low | 14 (25.45) | 20 (25.00) | Ref | ||
| Medium | 27 (40.09) | 41 (51.25) | 1.733 | 0.566–5.308 | 0.336 |
| High | 14 (25.45) | 19 (23.75) | 3.121 | 0.834–11.678 | 0.091 |
| Legumes | |||||
| Low | 21 (38.18) | 15 (18.75) | Ref | ||
| Medium | 22 (40.00) | 47 (58.75) | 3.723 | 1.255–11.045 | 0.018 * |
| High | 12 (21.82) | 18 (22.50) | 0.822 | 0.198–3.408 | 0.787 |
| Nuts/seeds | |||||
| Low | 20 (36.36) | 32 (40.00) | Ref | ||
| Medium | 24 (43.64) | 25 (31.25) | 1.056 | 0.385–2.894 | 0.916 |
| High | 11 (20.00) | 23 (28.75) | 1.215 | 0.359–4.109 | 0.754 |
| Cereals | |||||
| Low | 12 (21.82) | 26 (32.50) | Ref | ||
| Medium | 32 (58.18) | 29 (36.25) | 0.751 | 0.251–2.249 | 0.609 |
| High | 11 (20.00) | 25 (31.25) | 1.183 | 0.352–3.977 | 0.786 |
| Parameters | Controls n = 74 (%) | T2DM Cases, n = 61 | Adjusted OR a | 95%CI | p-Value |
|---|---|---|---|---|---|
| Total PFS | |||||
| Low | 13 (17.57) | 20 (32.79) | Ref | ||
| Medium | 36 (48.65) | 25 (40.98) | 0.499 | 0.141–1.768 | 0.281 |
| High | 25 (33.78) | 16 (26.23) | 0.267 | 0.062–1.162 | 0.078 |
| Vegetable | |||||
| Low | 15 (20.27) | 20 (32.79) | Ref | ||
| Medium | 40 (54.05) | 28 (45.90) | 0.420 | 0.116–1.521 | 0.186 |
| High | 19 (25.68) | 13 (21.31) | 0.236 | 0.093–1.794 | 0.236 |
| Fruit | |||||
| Low | 16 (21.62) | 18 (29.51) | Ref | ||
| Medium | 35 (47.30) | 33 (54.10) | 1.137 | 0.332–3.891 | 0.838 |
| High | 23 (31.08) | 10 (16.39) | 0.768 | 0.166–3.553 | 0.736 |
| Legume | |||||
| Low | 26 (35.14) | 10 (16.39) | Ref | ||
| Medium | 34 (45.95) | 35 (57.38) | 3.551 | 0.887–14.220 | 0.073 |
| High | 14 (18.92) | 16 (26.23) | 1.002 | 0.199–5.048 | 0.998 |
| Nuts/seeds | |||||
| Low | 23 (31.08) | 29 (47.54) | Ref | ||
| Medium | 35 (47.30) | 14 (22.95) | 0.237 | 0.064–0.872 | 0.030 * |
| High | 16 (21.62) | 18 (29.51) | 0.343 | 0.079–1.500 | 0.155 |
| Cereals | |||||
| Low | 15 (20.27) | 23 (37.70) | Ref | ||
| Medium | 43 (58.11) | 18 (29.51) | 0.353 | 0.099–1.254 | 0.107 |
| High | 16 (21.62) | 20 (32.79) | 0.789 | 0.205–3.041 | 0.731 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adokwe, J.B.; Waeyeng, D.; Suwan, K.; Camsanit, K.; Kaiduong, C.; Nuanrat, P.; Pouyfung, P.; Yimthiang, S.; Petchoo, J.; Satarug, S.; et al. Plant-Based Diet and Glycemic Control in Type 2 Diabetes: Evidence from a Thai Health-Promoting Hospital. Nutrients 2024, 16, 619. https://doi.org/10.3390/nu16050619
Adokwe JB, Waeyeng D, Suwan K, Camsanit K, Kaiduong C, Nuanrat P, Pouyfung P, Yimthiang S, Petchoo J, Satarug S, et al. Plant-Based Diet and Glycemic Control in Type 2 Diabetes: Evidence from a Thai Health-Promoting Hospital. Nutrients. 2024; 16(5):619. https://doi.org/10.3390/nu16050619
Chicago/Turabian StyleAdokwe, Jonah Bawa, Donrawee Waeyeng, Kanyamon Suwan, Kanchana Camsanit, Chanakan Kaiduong, Pawida Nuanrat, Phisit Pouyfung, Supabhorn Yimthiang, Jaruneth Petchoo, Soisungwan Satarug, and et al. 2024. "Plant-Based Diet and Glycemic Control in Type 2 Diabetes: Evidence from a Thai Health-Promoting Hospital" Nutrients 16, no. 5: 619. https://doi.org/10.3390/nu16050619
APA StyleAdokwe, J. B., Waeyeng, D., Suwan, K., Camsanit, K., Kaiduong, C., Nuanrat, P., Pouyfung, P., Yimthiang, S., Petchoo, J., Satarug, S., & Khamphaya, T. (2024). Plant-Based Diet and Glycemic Control in Type 2 Diabetes: Evidence from a Thai Health-Promoting Hospital. Nutrients, 16(5), 619. https://doi.org/10.3390/nu16050619