Effect of Creatine Supplementation on Body Composition and Malnutrition-Inflammation Score in Hemodialysis Patients: An Exploratory 1-Year, Balanced, Double-Blind Design
Abstract
1. Introduction
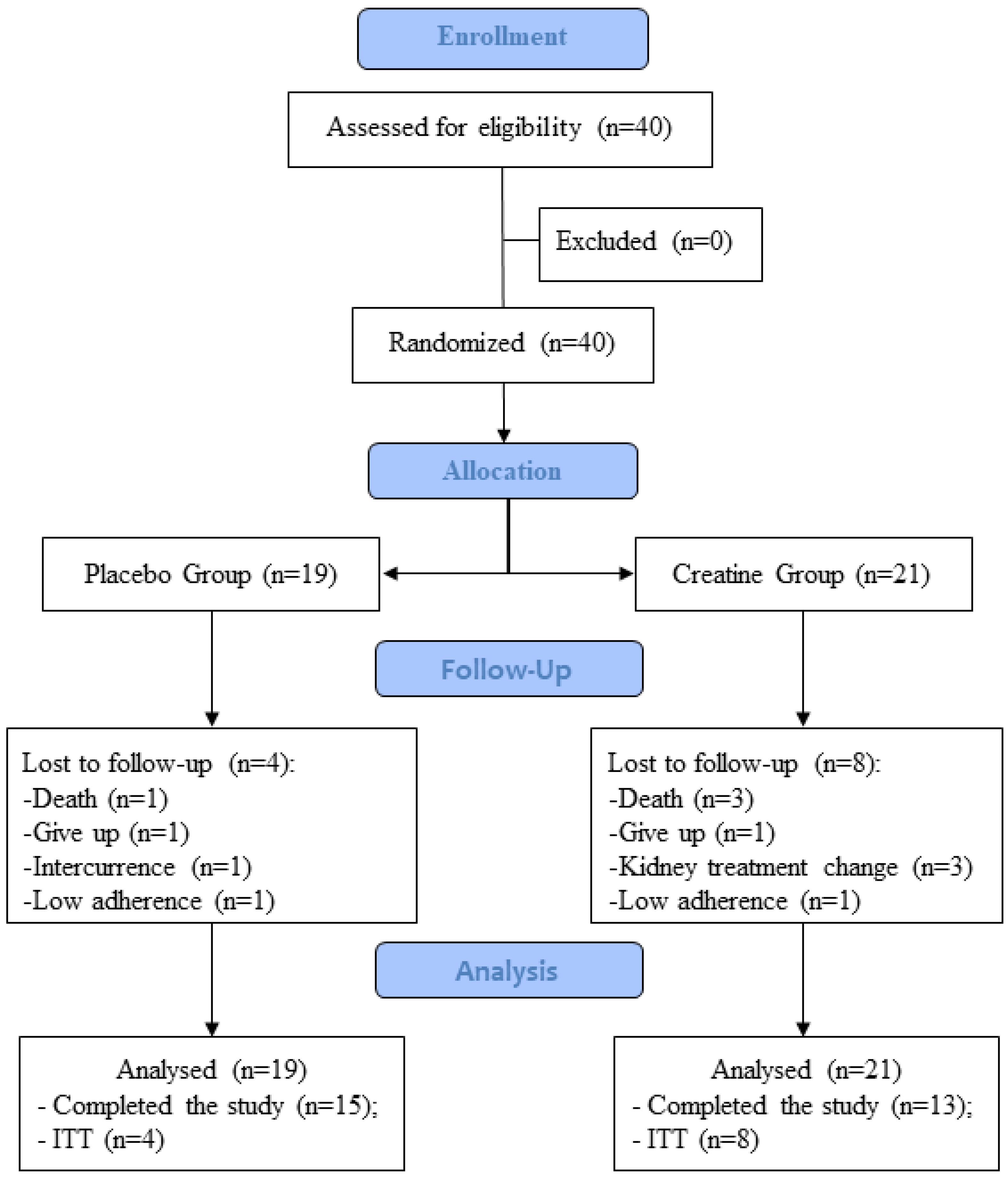
2. Materials and Methods
2.1. Design of Study
2.2. Recruitment and Sample Selection
2.3. Experimental Groups
2.4. Protocol Supplementation
2.5. Malnutrition-Inflammation Score (MIS)
2.6. Anthropometric and Body Composition Assessment
2.7. Biochemical Analysis
2.8. Statistical Analyses
3. Results
3.1. Baseline Characteristics and Food Intake
3.2. Malnutrition-Inflammation Score (MIS)
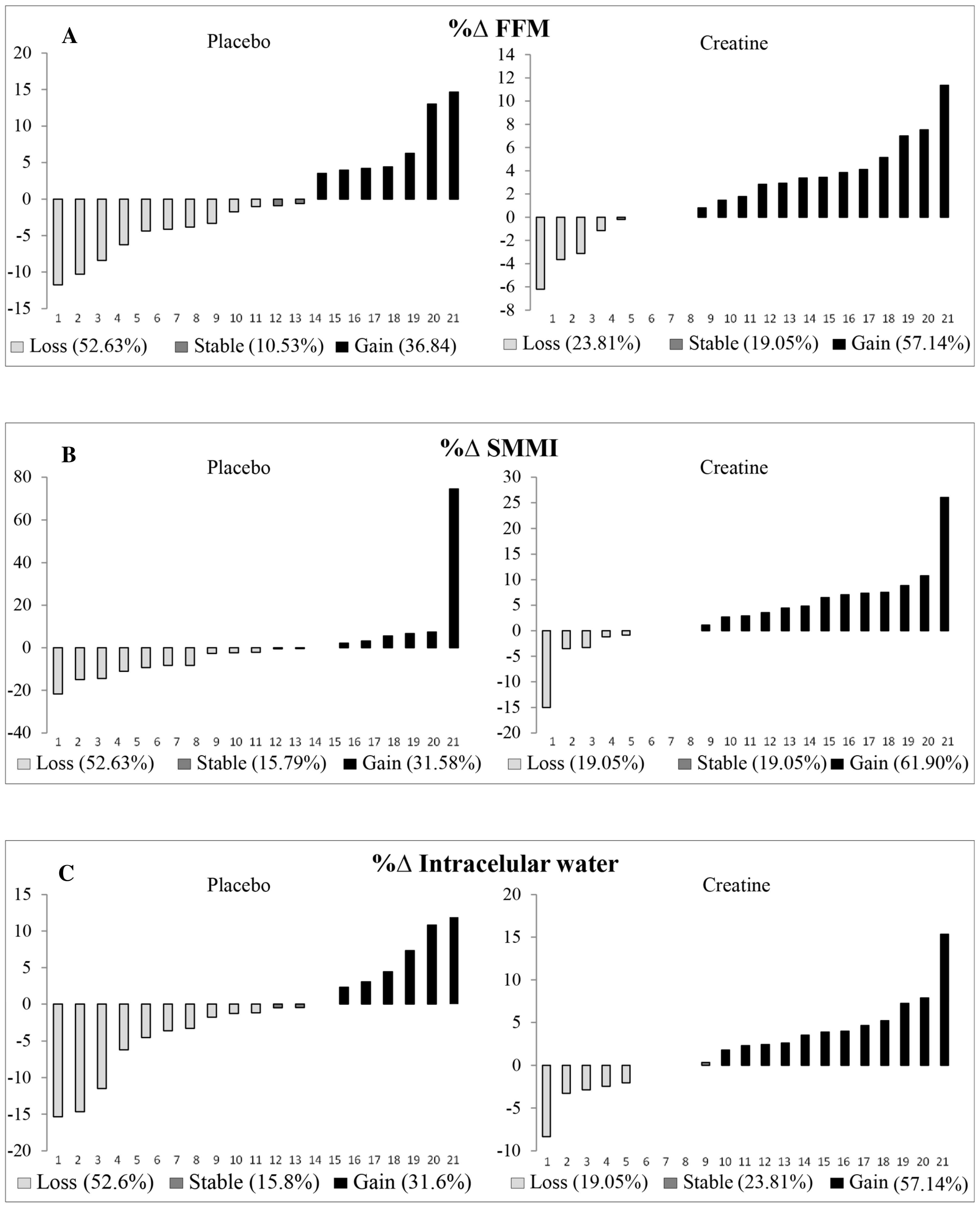
3.3. Intention to Treat
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- KDIGO. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3. [Google Scholar]
- Webster, A.C.; Nagler, E.V.; Morton, R.L.; Masson, P. Chronic Kidney Disease. Lancet 2016, 6736, 1238–1252. [Google Scholar] [CrossRef]
- Blumberg Benyamini, S.; Katzir, Z.; Biro, A.; Cernes, R.; Shalev, B.; Chaimy, T.; Barnea, Z. Nutrition assessment and risk prediction in dialysis patients-a new integrative score. J. Ren. Nutr. 2014, 24, 401–410. [Google Scholar] [CrossRef]
- Zhang, H.; Tao, X.; Shi, L.; Jiang, N.; Yang, Y. Evaluation of body composition monitoring for assessment of nutritional status in hemodialysis patients. Ren. Fail. 2019, 41, 377–383. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Kopple, J.D.; Block, G.; Humphreys, M.H. A malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am. J. Kidney Dis. 2001, 38, 1251–1263. [Google Scholar] [CrossRef] [PubMed]
- Marini, A.C.B.; Pimentel, G.D. Is body weight or muscle strength correlated with the Malnutrition Inflammation Score (MIS)? A cross-sectional study in hemodialysis patients. Clin. Nutr. ESPEN 2019, 33, 276–278. [Google Scholar] [CrossRef] [PubMed]
- Pasiakos, S.M.; Vislocky, L.M.; Carbone, J.W.; Altieri, N.; Konopelski, K.; Freake, H.C.; Anderson, J.M.; Ferrando, A.A.; Wolfe, R.R.; Rodriguez, N.R. Acute energy deprivation affects skeletal muscle protein synthesis and associated intracellular signaling proteins in physically active adults. J. Nutr. 2010, 140, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, F.K.; Smeets, J.S.J.; Broers, N.J.H.; van Kranenburg, J.M.X.; van der Sande, F.M.; Kooman, J.P.; Van Loon, L.J.C. End-stage renal disease patients lose a substantial amount of amino acids during hemodialysis. J. Nutr. 2020, 150, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, F.K.; Smeets, J.S.J.; Van Kranenburg, J.M.X.; Broers, N.J.H.; Van Der Sande, F.M.; Verdijk, L.B.; Kooman, J.P.; Van Loon, L.J.C. Amino acid removal during hemodialysis can be compensated for by protein ingestion and is not compromised by intradialytic exercise: A randomized controlled crossover trial. Am. J. Clin. Nutr. 2021, 114, 2074–2083. [Google Scholar] [CrossRef]
- Hendriks, F.K.; Kooman, J.P.; van Loon, L.J.C. Dietary protein interventions to improve nutritional status in end-stage renal disease patients undergoing hemodialysis. Curr. Opin. Clin. Nutr. Metab. Care 2021, 24, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Post, A.; Schutten, J.C.; Kremer, D.; van der Veen, Y.; Groothof, D.; Sotomayor, C.G.; Koops, C.A.; de Blaauw, P.; Kema, I.P.; Westerhuis, R.; et al. Creatine homeostasis and protein energy wasting in hemodialysis patients. J. Transl. Med. 2021, 19, 115. [Google Scholar] [CrossRef] [PubMed]
- Araujo, E.R.; dos Santos Ribeiro, P.; Carvalho, S.F.D. Creatina: Metabolismo e efeitos de sua suplementação sobre o treinamento de força e composição corporal. Rev. Bras. Nutr. Esportiva 2009, 3, 63–69. [Google Scholar]
- Post, A.; Tsikas, D.; Bakker, S.J.L. Creatine is a conditionally essential nutrient in chronic kidney disease: A hypothesis and narrative literature review. Nutrients 2019, 11, 1044. [Google Scholar] [CrossRef] [PubMed]
- Van Loon, L.J.C.; Murphy, R.; Oosterlaar, A.M.; Cameron-Smith, D.; Hargreaves, M.; Wagenmakers, A.J.M.; Snow, R. Creatine supplementation increases glycogen storage but not GLUT-4 expression in human skeletal muscle. Clin. Sci. 2004, 106, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Marini, A.C.B.; Motobu, R.D.; Freitas, A.T.V.; Mota, J.F.; Wall, B.T.; Pichard, C.; Laviano, A.; Pimentel, G.D. Short-Term Creatine Supplementation May Alleviate the Malnutrition-Inflammation Score and Lean Body Mass Loss in Hemodialysis Patients: A Pilot Randomized Placebo-Controlled Trial. J. Parenter. Enter. Nutr. 2020, 44, 815–822. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Enia, G.; Sicuso, C.; Alati, G.; Zoccali, C.; Pustorino, D.; Biondo, A. Subjective global assessment of nutrition in dialysis patients. Nephrol. Dial. Transplant. 1993, 8, 1094–1098. [Google Scholar]
- Steiber, A.L.; Kalantar-Zadeh, K.; Secker, D.; McCarthy, M.; Sehgal, A.; McCann, L. Subjective Global Assessment in chronic kidney disease: A review. J. Ren. Nutr. 2004, 14, 191–200. [Google Scholar] [CrossRef]
- Gibson, R.S. Principles of nutritional assessment. In Principles of Nutritional Assessment; Oxford University Press: Oxford, UK, 2005; p. 908. [Google Scholar]
- WHO. Physical Status: The Use and Interpretation of Anthropometry; WHO: Geneva, Switzerland, 1995. [Google Scholar]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.-C.; Pirlich, M.; et al. Bioelectrical impedance analysis—Part I: Review of principles and methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef]
- KDOQI. Clinical Practice Guidelines For Chronic Kidney Disease: Evaluation, Classification and Stratification; KDOQI: New York, NY, USA, 2002. [Google Scholar]
- Marini, A.C.B.; Pimentel, G.D. Creatine supplementation plus neuromuscular electrical stimulation improves lower-limb muscle strength and quality of life in hemodialysis men. Einstein 2020, 18, eCE5623. [Google Scholar] [CrossRef] [PubMed]
- Van der Veen, Y.; Post, A.; Kremer, D.; Koops, C.A.; Marsman, E.; Appeldoorn, T.Y.J.; Touw, D.J.; Westerhuis, R.; Heiner-Fokkema, M.R.; Franssen, C.F.M.; et al. Chronic dialysis patients are depleted of creatine: Review and rationale for intradialytic creatine supplementation. Nutrients 2021, 13, 2709. [Google Scholar] [CrossRef] [PubMed]
- Barril, G.; Nogueira, A.; Cigarrán, S.; La Torre, J.; Sanchez, R.; Santos, A.; Hadad, F.; Amair, R.R.; Truissar, I. Differences in Malnutrition-Inflammation Score of hemodialysis patients associated with hemodialysis factors. A Spanish multicenter epidemiologic study. J. Ren. Nutr. 2022, 33, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Beaudart, C.; Dawson, A.; Shaw, S.C.; Harvey, N.C.; Kanis, J.A.; Binkley, N.; Reginster, J.Y.; Chapurlat, R.; Chan, D.C.; Bruyère, O.; et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: Systematic review. Osteoporos. Int. 2017, 28, 1817–1833. [Google Scholar] [CrossRef] [PubMed]
- Antonio, J.; Candow, D.G.; Forbes, S.C.; Gualano, B.; Jagim, A.R.; Kreider, R.B.; Rawson, E.S.; Smith-Ryan, A.E.; VanDusseldorp, T.A.; Willoughby, D.S.; et al. Common questions and misconceptions about creatine supplementation: What does the scientific evidence really show? J. Int. Soc. Sports Nutr. 2021, 18, 13. [Google Scholar] [CrossRef] [PubMed]
- Dolan, E.; Artioli, G.G.; Pereira, R.M.R.; Gualano, B. Muscular atrophy and sarcopenia in the elderly: Is there a role for creatine supplementation? Biomolecules 2019, 9, 642. [Google Scholar] [CrossRef] [PubMed]
- Gualano, B.; Macedo, A.R.; Alves, C.R.R.; Roschel, H.; Benatti, F.B.; Takayama, L.; de Sá Pinto, A.L.; Lima, F.R.; Pereira, R.M.R. Creatine supplementation and resistance training in vulnerable older women: A randomized double-blind placebo-controlled clinical trial. Exp. Gerontol. 2014, 53, 7–15. [Google Scholar] [CrossRef]
- Wyss, M.; Kaddurah-Daouk, R. Creatine and creatinine metabolism. Physiol. Rev. 2000, 80, 1107–1213. [Google Scholar] [CrossRef]
- Powers, M.E.; Arnold, B.L.; Weltman, A.L.; Perrin, D.H.; Mistry, D.; Kahler, D.M.; Kraemer, W.; Volek, J. Creatine supplementation increases total body water without altering fluid distribution. J. Athl. Train. 2003, 38, 44–50. [Google Scholar]



| Variables | Placebo (n = 19) Mean ± SD | Creatine (n = 21) Mean ± SD | p |
|---|---|---|---|
| Sex (n) a | |||
| Female | 7 | 8 | 1.000 |
| Male | 12 | 13 | |
| Age (years) b | 52.8 ± 17.2 | 52.9 ± 15.6 | 0.998 |
| Body mass index (kg/m²) b | 25.0 ± 2.8 | 25.5 ± 4.3 | 0.661 |
| Hemodialysis time (months) b | 54.0 ± 37.4 | 37.0 ±24.6 | 0.096 |
| Kt/v b | 1.6 ± 0.3 | 1.6 ± 0.3 | 0.694 |
| Creatinine (mg/dL) | 11.1 ± 4.3 | 9.4 ± 2.9 | 0.140 |
| Urea pre (mg/dL) | 116.3 ± 31.3 | 113.2 ± 30.4 | 0.759 |
| Urea post (mg/dL) | 31.0 ± 11.7 | 29.9 ± 15.0 | 0.790 |
| Phosphorus (mg/dL) | 5.2 ± 1.7 | 5.2 ± 1.6 | 0.934 |
| PNA (g/kg) | 1.0 ± 0.2 | 1.0 ± 0.2 | 0.547 |
| Physical activity a | |||
| Active | 6 | 9 | 0.527 |
| Inactive | 13 | 12 | |
| Smoking c | |||
| Smoker | 2 | 2 | 0.894 |
| Non-smoking | 10 | 13 | |
| Ex-smoker | 7 | 6 | |
| Alcohol intake c | |||
| Yes | 5 | 4 | 0.712 |
| No | 14 | 17 |
| Variables | Placebo (n = 19) | Creatine (n = 21) | 1 Pre p | 1 Inter p | 1 Post p | 2 PG p | 2 CG p | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Intermediate | Post | Pre | Intermediate | Post | ||||||
| MIS | 4.7 ± 2.4 | 3.8 ± 2.4 | 4.5 ± 2.4 | 4.4 ± 3.4 | 3.9 ± 2.4 | 4.4 ± 2.4 | 0.434 | 0.901 | 0.061 | 0.362 | 0.545 |
| Body composition | |||||||||||
| Body weight (kg) | 67.5 ± 13.6 | 67.8 ± 13.0 | 67.4 ± 12.7 | 71.4 ± 15.4 | 72.4 ± 15.7 | 72.2 ± 16.1 | 0.629 | 0.597 | 0.588 | 0.167 | 0.018 *a |
| Handgrip strength (kg) | 29.58 ± 7.72 | 29.59 ± 7.32 | 31.13 ± 7.64 | 28.91 ± 9.65 | 30.91 ± 11.62 | 30.43 ± 11.29 | 0.745 | 0.839 | 0.655 | 0.223 | 0.291 |
| Gait speed (m/s) | 1.02 ± 0.95 | 0.90 ± 0.27 | 0.82 ± 0.24 | 1.00 ± 0.22 | 0.94 ± 0.16 | 0.90 ± 0.17 | 0.087 | 0.859 | 0.390 | 0.338 | 0.150 |
| Fat free mass (kg) | 47.83 ± 9.28 | 47.98 ± 11.57 | 48.45 ± 11.50 | 47.97 ± 10.02 | 48.95 ± 10.61 | 49.50 ± 10.52 | 0.989 | 0.871 | 0.695 | 0.399 | 0.010 *ab |
| SMMI (kg) | 21.54 ± 5.36 | 21.42 ± 5.71 | 21.88 ± 5.58 | 21.70 ± 6.01 | 22.55 ± 6.77 | 22.85 ± 6.42 | 0.924 | 0.755 | 0.695 | 0.389 | 0.022 *ab |
| TBW (L) | 35.17 ± 6.80 | 35.39 ± 8.54 | 35.70 ± 8.50 | 35.45 ± 7.31 | 36.12 ± 7.64 | 36.51 ± 7.62 | 0.935 | 0.715 | 0.645 | 0.453 | 0.008 *ab |
| TBW (%) | 52.83 ± 7.18 | 52.00 ± 8.09 | 52.82 ± 7.57 | 50.23 ± 7.48 | 50.22 ± 7.67 | 51.00 ± 8.41 | 0.303 | 0.569 | 0.473 | 0.882 | 0.750 |
| ECW (L) | 14.81 ± 3.18 | 15.19 ± 4.14 | 15.28 ± 4.15 | 15.21 ± 3.00 | 15.38 ± 2.78 | 15.51 ± 2.93 | 0.635 | 0.569 | 0.616 | 0.945 | 0.066 |
| ECW (%) | 22.16 ± 2.96 | 22.30 ± 4.03 | 22.53 ± 3.67 | 21.60 ± 3.31 | 21.50 ± 3.33 | 21.76 ± 3.74 | 0.448 | 0.850 | 0.542 | 0.986 | 0.901 |
| ECW/TBW (%) | 42.06 ± 3.03 | 42.85 ± 3.19 | 42.67 ± 3.48 | 43.12 ± 3.36 | 42.97 ± 4.19 | 42.76 ± 3.41 | 0.329 | 0.725 | 0.924 | 0.691 | 0.481 |
| ICW (L) | 20.36 ± 3.93 | 20.20 ± 4.66 | 20.42 ± 4.66 | 20.24 ± 4.60 | 20.75 ± 5.23 | 21.00 ± 5.00 | 0.675 | 0.924 | 0.860 | 0.476 | 0.016 *ab |
| ICW (%) | 30.67 ± 4.84 | 29.70 ± 4.68 | 30.28 ± 4.74 | 28.63 ± 4.93 | 28.71 ± 5.37 | 29.24 ± 5.44 | 0.223 | 0.579 | 0.379 | 0.128 | 0.427 |
| Biochemical parameters | |||||||||||
| Creatinine (mg/dL) | 11.15 ± 4.36 | 11.42 ± 3.47 | 10.94 ± 2.60 | 9.40 ± 2.92 | 11.50 ± 3.69 | 11.40 ± 3.39 | 0.203 | 0.914 | 0.776 | 0.135 | 0.001 *ab |
| Urea pre (mg/dL) | 116.3± 31.3 | 102.6 ± 23.3 | 118.8 ± 37.2 | 113.2 ± 30.4 | 121.1 ± 34.5 | 124.6 ± 31.5 | 0.957 | 0.040 * | 0.432 | 0.082 | 0.220 |
| Urea post (mg/dL) | 31.0 ± 11.7 | 26.6 ± 7.4 | 31.2 ± 9.3 | 29.9 ± 15.0 | 32.3 ± 14.0 | 34.7 ± 12.7 | 0.569 | 0.212 | 0.481 | 0.135 | 0.003 *b |
| Phosphorus (mg/dL) | 5.3 ±1.8 | 4.8 ± 1.4 | 5.2 ± 1.6 | 5.2 ± 1.6 | 5.1 ± 1.4 | 5.6 ± 1.6 | 0.935 | 0.626 | 0.597 | 0.037 * | 0.257 |
| PNA (g/kg) | 1.05 ± 0.27 | 0.95 ± 0.21 | 1.07 ± 0.33 | 1.00 ± 0.20 | 1.09 ± 0.29 | 1.06 ± 0.27 | 0.935 | 0.067 | 0.850 | 0.014 *ac | 0.137 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marini, A.C.B.; Schincaglia, R.M.; Candow, D.G.; Pimentel, G.D. Effect of Creatine Supplementation on Body Composition and Malnutrition-Inflammation Score in Hemodialysis Patients: An Exploratory 1-Year, Balanced, Double-Blind Design. Nutrients 2024, 16, 615. https://doi.org/10.3390/nu16050615
Marini ACB, Schincaglia RM, Candow DG, Pimentel GD. Effect of Creatine Supplementation on Body Composition and Malnutrition-Inflammation Score in Hemodialysis Patients: An Exploratory 1-Year, Balanced, Double-Blind Design. Nutrients. 2024; 16(5):615. https://doi.org/10.3390/nu16050615
Chicago/Turabian StyleMarini, Ana Clara B., Raquel M. Schincaglia, Darren G. Candow, and Gustavo D. Pimentel. 2024. "Effect of Creatine Supplementation on Body Composition and Malnutrition-Inflammation Score in Hemodialysis Patients: An Exploratory 1-Year, Balanced, Double-Blind Design" Nutrients 16, no. 5: 615. https://doi.org/10.3390/nu16050615
APA StyleMarini, A. C. B., Schincaglia, R. M., Candow, D. G., & Pimentel, G. D. (2024). Effect of Creatine Supplementation on Body Composition and Malnutrition-Inflammation Score in Hemodialysis Patients: An Exploratory 1-Year, Balanced, Double-Blind Design. Nutrients, 16(5), 615. https://doi.org/10.3390/nu16050615







