Impact of Dietary Nutrients on the Prevalence of Dry Eye Syndrome among Korean Women Aged 40 and above: Evidence from the Korea National Health and Nutrition Examination Survey
Abstract
1. Introduction
2. Materials and Methods
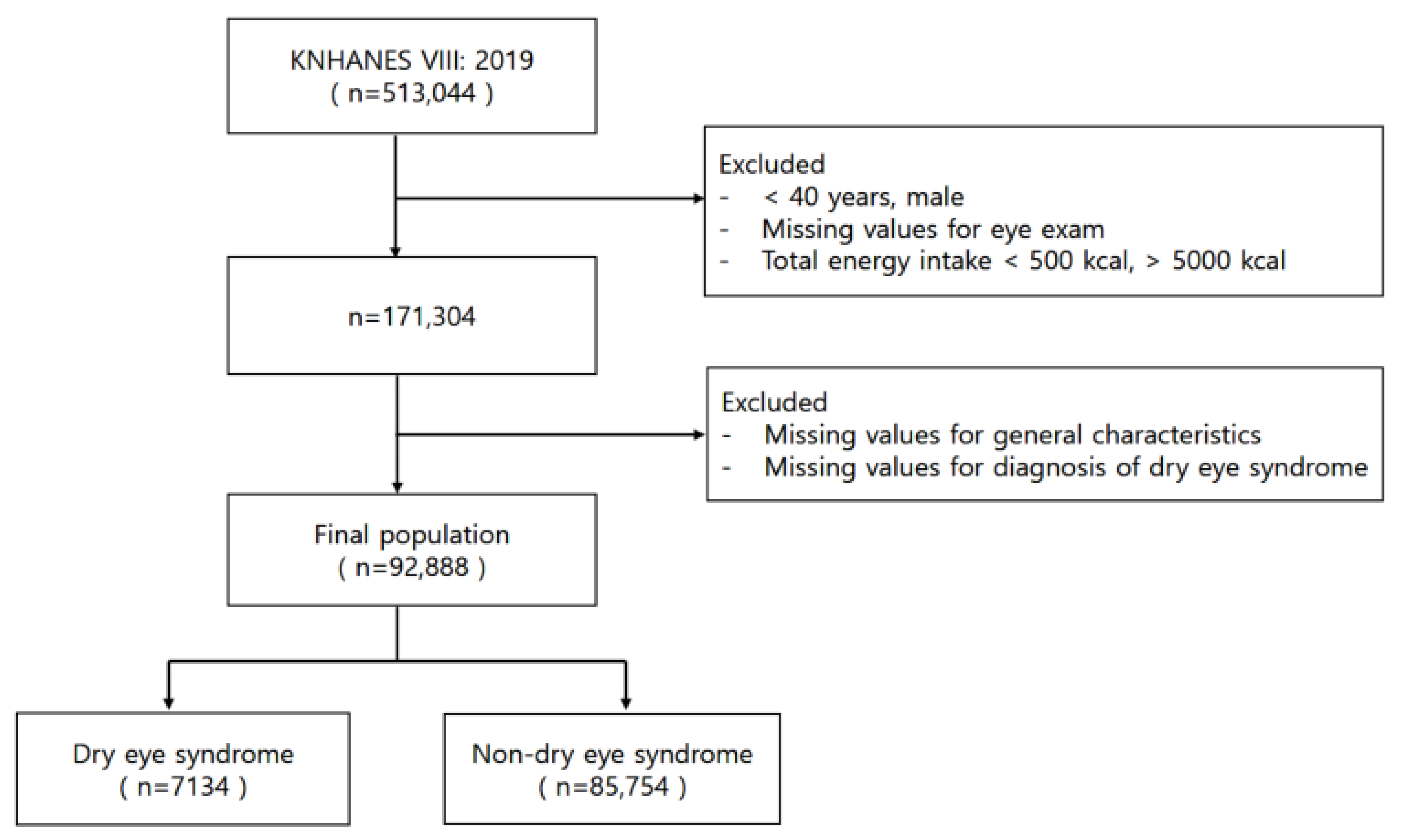
2.1. Data Resource and Study Population
2.2. Socio-Demographic and Health Variables
2.3. Diagnosis of Dry Eye Syndrome and Dietary Nutrient Intake Assessment
2.4. Statistical Analysis
3. Results
3.1. Study Population and Characteristics
3.2. Risk Factors for Dry Eye Syndrome
3.3. Association between Daily Intake of Dietary Nutrients and Dry Eye Syndrome
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Craig, J.P.; Nichols, K.K.; Akpek, E.K.; Caffery, B.; Dua, H.S.; Joo, C.K.; Liu, Z.; Nelson, J.D.; Nichols, J.J.; Tsubota, K.; et al. TFOS DEWS II definition and classification report. Ocul. Surf. 2017, 15, 276–283. [Google Scholar] [CrossRef] [PubMed]
- International Dry Eye WorkShop. The definition and classification of dry eye disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop. Ocul. Surf. 2007, 5, 75–92. [Google Scholar] [CrossRef]
- Lemp, M.A. Epidemiology and classification of dry eye. Adv. Exp. Med. Biol. 1998, 438, 791–803. [Google Scholar] [PubMed]
- Sullivan, D.A.; Rocha, E.M.; Aragona, P.; Clayton, J.A.; Ding, J.; Golebiowski, B.; Hampel, U.; McDermott, A.M.; Schaumberg, D.A.; Srinivasan, S.; et al. TFOS DEWS II sex, gender, and hormones report. Ocul. Surf. 2017, 15, 284–333. [Google Scholar] [CrossRef] [PubMed]
- Miljanović, B.; Dana, R.; Sullivan, D.A.; Schaumberg, D.A. Impact of dry eye syndrome on vision-related quality of life. Am. J. Ophthalmol. 2007, 143, 409–415. [Google Scholar] [CrossRef]
- HIRA Bigdata Open Portal: Health Insurance Review & Assessment Service. Available online: http://opendata.hira.or.kr/op/opc/olapMfrnIntrsIlnsInfo.do (accessed on 27 August 2023).
- Matossian, C.; McDonald, M.; Donaldson, K.E.; Nichols, K.K.; MacIver, S.; Gupta, P.K. Dry eye disease: Consideration for women’s health. J. Womens Health 2019, 28, 502–514. [Google Scholar] [CrossRef]
- Schaumberg, D.A.; Uchino, M.; Christen, W.G.; Semba, R.D.; Buring, J.E.; Li, J.Z. Patient-reported differences in dry eye disease between men and women: Impact, management, and patient satisfaction. PLoS ONE 2013, 8, e76121. [Google Scholar] [CrossRef]
- Paulsen, A.J.; Cruickshanks, K.J.; Fischer, M.E.; Huang, G.H.; Klein, B.E.; Klein, R.; Dalton, D.S. Dry eye in the Beaver Dam Offspring Study: Prevalence, risk factors, and health-related quality of life. Am. J. Ophthalmol. 2014, 157, 799–806. [Google Scholar] [CrossRef]
- Baudouin, C. A new approach for better comprehension of diseases of the ocular surface. J. Fr. Ophtalmol. 2007, 30, 239–246. [Google Scholar] [CrossRef]
- Uchino, M.; Schaumberg, D.A. Dry eye disease: Impact on quality of life and vision. Curr. Ophthalmol. Rep. 2013, 1, 51–57. [Google Scholar] [CrossRef]
- Bhargava, R.; Kumar, P.; Phogat, H.; Kaur, A.; Kumar, M. Oral omega-3 fatty acids treatment in computer vision syndrome related dry eye. Cont. Lens Anterior Eye 2015, 38, 206–210. [Google Scholar] [CrossRef]
- Miljanović, B.; Trivedi, K.A.; Dana, M.R.; Gilbard, J.P.; Buring, J.E.; Schaumberg, D.A. Relation between dietary n−3 and n−6 fatty acids and clinically diagnosed dry eye syndrome in women. Am. J. Clin. Nutr. 2005, 82, 887–893. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.H.; Albietz, J.; Harkin, D.G.; Kimlin, M.G.; Schmid, K.L. Impact of oral vitamin D supplementation on the ocular surface in people with dry eye and/or low serum vitamin D. Cont. Lens Anterior Eye 2018, 41, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, S.A.; El-Hiti, G.A.; Al-Baloud, A.A.; Alfarhan, M.I.; Al-Shahrani, A.; Albakri, A.A.; Alqahtani, S.; Masmali, A.M. Effects of short-term oral vitamin A supplementation on the ocular tear film in patients with dry eye. Clin. Ophthalmol. 2019, 13, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Drouault-Holowacz, S.; Bieuvelet, S.; Burckel, A.; Rigal, D.; Dubray, C.; Lichon, J.L.; Bringer, P.; Pilon, F.; Chiambaretta, F.R. Antioxidants intake and dry eye syndrome: A crossover, placebo-controlled, randomized trial. Eur. J. Ophthalmol. 2009, 19, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.; Sullivan, D.A. Aging and dry eye disease. Exp. Gerontol. 2012, 47, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Schaumberg, D.A.; Buring, J.E.; Sullivan, D.A.; Dana, M.R. Hormone replacement therapy and dry eye syndrome. JAMA 2001, 286, 2114–2119. [Google Scholar] [CrossRef] [PubMed]
- Sriprasert, I.; Warren, D.W.; Mircheff, A.K.; Stanczyk, F.Z. Dry eye in postmenopausal women: A hormonal disorder. Menopause 2016, 23, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Askeroglu, U.; Alleyne, B.; Guyuron, B. Pharmaceutical and herbal products that may contribute to dry eyes. Plast. Reconstr. Surg. 2013, 131, 159–167. [Google Scholar] [CrossRef]
- Lemp, M.A. Dry eye (keratoconjunctivitis sicca), rheumatoid arthritis, and Sjögren’s syndrome. Am. J. Ophthalmol. 2005, 140, 898–899. [Google Scholar] [CrossRef]
- Fujita, M.; Igarashi, T.; Kurai, T.; Sakane, M.; Yoshino, S.; Takahashi, H. Correlation between dry eye and rheumatoid arthritis activity. Am. J. Ophthalmol. 2005, 140, 808–813. [Google Scholar] [CrossRef]
- Nichols, J.J.; Sinnott, L.T. Tear film, contact lens, and patient-related factors associated with contact lens–related dry eye. Investig. Ophthalmol. Vis. Sci. 2006, 47, 1319–1328. [Google Scholar] [CrossRef]
- Yu, E.Y.; Leung, A.; Rao, S.; Lam, D.S. Effect of laser in situ keratomileusis on tear stability. Ophthalmology 2000, 107, 2131–2135. [Google Scholar] [CrossRef]
- Wolkoff, P.; Nojgaard, J.K.; Franck, C.; Skov, P. The modern office environment desiccates the eye? Indoor Air 2006, 16, 258–265. [Google Scholar] [CrossRef]
- Courtin, R.; Pereira, B.; Naughton, G.; Chamoux, A.; Chiambaretta, F.; Lanhers, C.; Dutheil, F. Prevalence of dry eye disease in visual display terminal workers: A systematic review and meta-analysis. BMJ Open 2016, 6, e009675. [Google Scholar] [CrossRef]
- Liu, J.; Rehm, C.D.; Onopa, J.; Mozaffarian, D. Trends in diet quality among youth in the United States, 1999–2016. JAMA 2020, 323, 1161–1174. [Google Scholar] [CrossRef]
- Calder, P.C. N-3 polyunsaturated fatty acids and inflammation: From molecular biology to the clinic. Lipids 2003, 38, 343–352. [Google Scholar] [CrossRef]
- Erdinest, N.; Shmueli, O.; Grossman, Y.; Ovadia, H.; Solomon, A. Anti-inflammatory effects of alpha linolenic Acid on human corneal epithelial cells. Investig. Ophthalmol. Vis. Sci. 2012, 53, 4396–4406. [Google Scholar] [CrossRef]
- Giannaccare, G.; Pellegrini, M.; Sebastiani, S.; Bernabei, F.; Roda, M.; Taroni, L.; Versura, P.; Campos, E.C. Efficacy of omega-3 fatty acid supplementation for treatment of dry eye disease: A meta-analysis of randomized clinical trials. Cornea 2019, 38, 565–573. [Google Scholar] [CrossRef]
- Rosenberg, E.S.; Asbell, P.A. Essential fatty acids in the treatment of dry eye. Ocul. Surf. 2010, 8, 18–28. [Google Scholar] [CrossRef]
- Molina-Leyva, I.; Molina-Leyva, A.; Bueno-Cavanillas, A. Efficacy of nutritional supplementation with omega-3 and omega-6 fatty acids in dry eye syndrome: A systematic review of randomized clinical trials. Acta Ophthalmol. 2017, 95, e677–e685. [Google Scholar] [CrossRef]
- Bhargava, R.; Kumar, P.; Kumar, M.; Mehra, N.; Mishra, A. A randomized controlled trial of omega-3 fatty acids in dry eye syndrome. Int. J. Ophthalmol. 2013, 6, 811. [Google Scholar]
- Donthineni, P.R.; Das, A.V.; Basu, S. Dry eye disease in children and adolescents in India. Ocul. Surf. 2020, 18, 777–782. [Google Scholar] [CrossRef]
- Khandait, D.W.; Vasudeo, N.D.; Zodpey, S.P.; Ambadekar, N.N.; Koram, M.R. Vitamin A intake and xerophthalmia among Indian children. Public Health 1999, 113, 69–72. [Google Scholar] [CrossRef]
- McCusker, M.M.; Durrani, K.; Payette, M.J.; Suchecki, J. An eye on nutrition: The role of vitamins, essential fatty acids, and antioxidants in age-related macular degeneration, dry eye syndrome, and cataract. Clin. Dermatol. 2016, 34, 276–285. [Google Scholar] [CrossRef]
- Feng, Z.; Liu, Z.; Li, X.; Jia, H.; Sun, L.; Tian, C.; Jia, L.; Liu, J. α-Tocopherol is an effective Phase II enzyme inducer: Protective effects on acrolein-induced oxidative stress and mitochondrial dysfunction in human retinal pigment epithelial cells. J. Nutr. Biochem. 2010, 21, 1222–1231. [Google Scholar] [CrossRef]
- Davidson, H.J.; Kuonen, V.J. The tear film and ocular mucins. Vet. Ophthalmol. 2004, 7, 71–77. [Google Scholar] [CrossRef]
- Olenik, A.; Jimenez-Alfaro, I.; Alejandre-Alba, N.; Mahillo-Fernandez, I. A randomized, double-masked study to evaluate the effect of omega-3 fatty acids supplementation in meibomian gland dysfunction. Clin. Interv. Aging 2013, 8, 1133–1138. [Google Scholar] [CrossRef]
- Caffery, B.E. Influence of diet on tear function. Optom. Vis. Sci. 1991, 68, 58–72. [Google Scholar] [CrossRef]
- Dao, A.H.; Spindle, J.D.; Harp, B.A.; Jacob, A.; Chuang, A.Z.; Yee, R.W. Association of dyslipidemia in moderate to severe meibomian gland dysfunction. Am. J. Ophthalmol. 2010, 150, 371–375.e1. [Google Scholar] [CrossRef]
- Zou, S.; Jiao, X.; Liu, J.; Qi, D.; Pei, X.; Lu, D. High-fat nutritional challenge reshapes circadian signatures in murine extraorbital lacrimal glands. Investig. Ophthalmol. Vis. Sci. 2022, 63, 23. [Google Scholar] [CrossRef]
- Calder, P.C. Polyunsaturated fatty acids, inflammation, and immunity. Lipids 2001, 36, 1007–1024. [Google Scholar] [CrossRef]
- Brignole-Baudouin, F.; Baudouin, C.; Aragona, P.; Rolando, M.; Labetoulle, M.; Pisella, P.J. A multicentre, double-masked, randomized, controlled trial assessing the effect of oral supplementation of omega-3 and omega-6 fatty acids on a conjunctival inflammatory marker in dry eye patients. Acta Ophthalmol. 2011, 89, e591–e597. [Google Scholar] [CrossRef]
- Zhu, W.; Wu, Y.; Li, G.; Wang, J.; Li, X. Efficacy of polyunsaturated fatty acids for dry eye syndrome: A meta-analysis of randomized controlled trials. Nutr. Rev. 2014, 72, 662–671. [Google Scholar] [CrossRef]
- Gorimanipalli, B.; Shetty, R.; Sethu, S.; Khamar, P. Vitamin D and eye: Current evidence and practice guidelines. Indian J. Ophthalmol. 2023, 71, 112–1134. [Google Scholar] [CrossRef]
- Rolando, M.; Barabino, S. Dry Eye Disease: What Is the Role of Vitamin D? Int. J. Mol. Sci. 2023, 24, 1458. [Google Scholar] [CrossRef]
- Liu, J.; Dong, Y.; Wang, Y. Vitamin D deficiency is associated with dry eye syndrome: A systematic review and meta-analysis. Acta Ophthalmol. 2020, 98, 749–754. [Google Scholar] [CrossRef]
- Askari, G.; Rafie, N.; Miraghajani, M.; Heidari, Z.; Arab, A. Association between vitamin D and dry eye disease: A systematic review and meta-analysis of observational studies. Cont. Lens Anterior Eye 2020, 43, 418–425. [Google Scholar] [CrossRef]
- Hwang, J.S.; Lee, Y.P.; Shin, Y.J. Vitamin D enhances the efficacy of topical artificial tears in patients with dry eye disease. Cornea 2019, 38, 304–310. [Google Scholar] [CrossRef]
| Total | DES * | Non-DES | |
|---|---|---|---|
| Number | 92,888 | 7134 (7.7%) | 85,754 (92.3%) |
| Age (years) | 63.35 ± 8.86 ** | 58.52 ± 7.26 | 63.76 ± 8.87 |
| Age (years) | |||
| 40–49 | 3608 (3.9%) | 356 (5.0%) | 3252 (3.8%) |
| 50–59 | 31,674 (34.1%) | 4499 (63.1%) | 27,175 (31.7%) |
| 60–69 | 33,254 (35.8%) | 1580 (22.2%) | 31,674 (36.9%) |
| 70+ | 24,352 (26.2%) | 699 (9.8%) | 23,653 (27.6%) |
| BMI *** (kg/m2) | |||
| Underweight | 2297 (2.5%) | 210 (2.9%) | 2087 (2.4%) |
| Normal | 59,535 (64.1%) | 4866 (68.2%) | 54,669 (63.8%) |
| Overweight | 27,219 (29.3%) | 1941 (27.2%) | 25,278 (29.5%) |
| Obese | 3837 (4.1%) | 117 (1.7%) | 3720 (4.3%) |
| Educational level | |||
| Less than high school | 47,068 (50.7%) | 2167 (30.4%) | 44,901 (52.4%) |
| More than high school | 45,820 (49.3%) | 4967 (69.6%) | 40,853 (47.6%) |
| Household income | |||
| Lower | 39,633 (42.7%) | 2569 (36.0%) | 37,064 (43.2%) |
| Middle | 17,798 (19.1%) | 1313 (18.4%) | 16,485 (19.2%) |
| Higher | 35,457 (38.2%) | 3252 (45.6%) | 32,205 (37.6%) |
| Occupational category | |||
| White-collar worker | 9204 (9.9%) | 1458 (20.5%) | 7746 (9.0%) |
| Indoor worker | 18,661 (20.1%) | 1728 (24.2%) | 16,933 (19.8%) |
| Outdoor worker | 65,023 (70.0%) | 3948 (55.3%) | 61,075 (71.2%) |
| Near work | |||
| ≤1 h/D | 52,957 (57.0%) | 2760 (38.7%) | 50,197 (58.5%) |
| 1–3 h/D | 27,862 (30.0%) | 3120 (43.7%) | 24,742 (28.9%) |
| ≥4 h/D | 12,069 (13.0%) | 1254 (17.6%) | 10,815 (12.6%) |
| Menopause | |||
| Yes | 84,965 (91.5%) | 6485 (90.9%) | 78,480 (91.5%) |
| No | 7923 (8.5%) | 649 (9.1%) | 7274 (8.5%) |
| Rheumatoid arthritis | |||
| Yes | 3557 (3.8%) | 378 (5.3%) | 3179 (3.7%) |
| No | 89,331 (96.2%) | 6756 (94.7%) | 82,575 (96.3%) |
| Osteoporosis | |||
| Yes | 20,546 (22.1%) | 1382 (19.4%) | 19,164 (22.4%) |
| No | 72,342 (77.9%) | 5752 (80.6%) | 66,590 (77.6%) |
| Thyroid disease | |||
| Yes | 7937 (8.5%) | 900 (12.6%) | 7037 (8.2%) |
| No | 84,951 (91.5%) | 6234 (87.4%) | 78,717 (91.8%) |
| Diabetes | |||
| Yes | 12,311 (13.3%) | 947 (13.3%) | 11,364 (13.3%) |
| No | 80,577 (86.7%) | 6187 (86.7%) | 74,390 (86.7%) |
| Model 1 (1) | Model 2 (2) | |||
|---|---|---|---|---|
| OR [95% CI] | p-Value | OR [95% CI] | p-Value | |
| Age (years) | ||||
| 40–49 | 1 | 1 | ||
| 50–59 | 1.51 [1.35–1.70] | <0.0001 | 1.81 [1.58–2.07] | <0.0001 |
| 60–69 | 0.46 [0.40–0.51] | <0.0001 | 0.77 [0.64–0.94] | <0.0001 |
| 70+ | 0.27 [0.24–0.31] | <0.0001 | 0.60 [0.45–0.80] | <0.0001 |
| BMI (kg/m2) | ||||
| Underweight | 1.13 [0.98–1.31] | <0.0001 | 1.74 [1.47–2.05] | <0.0001 |
| Normal | 1 | 1 | ||
| Overweight | 0.86 [0.82–0.91] | 0.0006 | 0.74 [0.68–0.81] | 0.9664 |
| Obese | 0.35 [0.29–0.43] | <0.0001 | 0.23 [0.18–0.30] | <0.0001 |
| Educational level | ||||
| Less than high school | 1 | 1 | ||
| Beyond high school | 2.52 [2.39–2.65] | <0.0001 | 1.52 [1.42–1.62] | <0.0001 |
| Household income | ||||
| Lower | 1 | 1 | ||
| Middle | 1.15 [1.07–1.23] | 0.1215 | 0.74 [0.69–0.80] | 0.0025 |
| Higher | 1.46 [1.38–1.54] | <0.0001 | 0.67 [0.62–0.71] | <0.0001 |
| Occupational category | ||||
| White-collar worker | 1 | 1 | ||
| Indoor worker | 0.54 [0.50–0.58] | 0.0097 | 0.66 [0.61–0.72] | <0.0001 |
| Outdoor worker | 0.34 [0.32–0.37] | <0.0001 | 0.61 [0.57–0.66] | <0.0001 |
| Near work | ||||
| ≤1 h/D | 1 | 1 | ||
| 1–3 h/D | 2.29 [2.17–2.42] | <0.0001 | 1.46 [1.37–1.55] | <0.0001 |
| ≥4 h/D | 2.11 [1.97–2.26] | <0.0001 | 1.00 [0.92–1.08] | <0.0001 |
| Model 1 (1) | Model 2 (2) | |||
|---|---|---|---|---|
| OR [95% CI] | p-Value | OR [95% CI] | p-Value | |
| Menopause | ||||
| Yes | 0.93 [0.85–1.01] | 0.0741 | 1.31 [1.20–1.43] | <0.0001 |
| No | 1 | 1 | ||
| Rheumatoid arthritis | ||||
| Yes | 1.45 [1.30–1.62] | <0.0001 | 1.54 [1.37–1.72] | <0.0001 |
| No | 1 | 1 | ||
| Osteoporosis | ||||
| Yes | 0.84 [0.79–0.89] | <0.0001 | 1.47 [1.37–1.57] | <0.0001 |
| No | 1 | 1 | ||
| Diabetes | ||||
| Yes | 1.00 [0.93–1.08] | 0.9568 | 1.41 [1.29–1.53] | <0.0001 |
| No | 1 | 1 | ||
| Thyroid disease | ||||
| Yes | 1.62 [1.50–1.74] | <0.0001 | 1.41 [1.31–1.53] | <0.0001 |
| No | 1 | 1 | ||
| Nutrients | Model 1 (1) | Model 2 (2) | ||
|---|---|---|---|---|
| OR [95% CI] | p-Value | OR [95% CI] | p-Value | |
| Carbohydrate (g) | 1.31 [1.25–1.38] | <0.0001 | 1.23 [1.17–1.29] | <0.0001 |
| Sugar (g) | 1.59 [1.51–1.67] | <0.0001 | 1.30 [1.24–1.37] | <0.0001 |
| Fiber (g) | 0.88 [0.84–0.92] | <0.0001 | 0.72 [0.69–0.76] | <0.0001 |
| Protein (g) | 1.10 [1.05–1.16] | 0.0001 | 0.84 [0.80–0.88] | <0.0001 |
| Fat (g) | 1.63 [1.55–1.71] | <0.0001 | 1.25 [1.18–1.32] | <0.0001 |
| ω-3 fatty acid (g) | 1.09 [1.04–1.14] | 0.0006 | 0.90 [0.86–0.95] | <0.0001 |
| ω-6 fatty acid (g) | 1.23 [1.17–1.29] | <0.0001 | 0.98 [0.93–1.03] | 0.3798 |
| Cholesterol (mg) | 1.57 [1.49–1.65] | <0.0001 | 1.32 [1.25–1.39] | <0.0001 |
| Water (mL) | 1.03 [0.99–1.09] | 0.1784 | 0.76 [0.72–0.80] | <0.0001 |
| Calcium (mg) | 0.98 [0.93–1.03] | 0.3384 | 0.82 [0.78–0.87] | <0.0001 |
| Phosphate (mg) | 1.08 [1.03–1.13] | 0.0017 | 0.87 [0.82–0.91] | <0.0001 |
| Sodium (mg) | 1.41 [1.34–1.48] | <0.0001 | 1.18 [1.12–1.24] | <0.0001 |
| Potassium (mg) | 1.09 [1.04–1.14] | 0.0005 | 0.88 [0.83–0.92] | <0.0001 |
| Magnesium (mg) | 1.05 [1.00–1.11] | 0.0374 | 0.87 [0.82–0.91] | <0.0001 |
| Iron (mg) | 1.46 [1.39–1.53] | <0.0001 | 1.28 [1.22–1.35] | <0.0001 |
| Zinc (mg) | 1.50 [1.43–1.58] | <0.0001 | 1.26 [1.19–1.32] | <0.0001 |
| Vitamin A (μg RAE) | 1.05 [1.00–1.10] | 0.0383 | 0.78 [0.74–0.82] | <0.0001 |
| Carotene (μg) | 1.03 [0.98–1.08] | 0.2437 | 0.82 [0.78–0.86] | <0.0001 |
| Vitamin C (mg) | 0.90 [0.85–0.94] | <0.0001 | 0.73 [0.70–0.77] | <0.0001 |
| Vitamin D (μg) | 1.10 [1.05–1.15] | 0.0001 | 1.01 [0.96–1.06] | 0.7034 |
| Vitamin E (mg α-TE) | 1.14 [1.08–1.19] | <0.0001 | 0.86 [0.82–0.90] | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-M.; Choi, Y.-J. Impact of Dietary Nutrients on the Prevalence of Dry Eye Syndrome among Korean Women Aged 40 and above: Evidence from the Korea National Health and Nutrition Examination Survey. Nutrients 2024, 16, 372. https://doi.org/10.3390/nu16030372
Kim J-M, Choi Y-J. Impact of Dietary Nutrients on the Prevalence of Dry Eye Syndrome among Korean Women Aged 40 and above: Evidence from the Korea National Health and Nutrition Examination Survey. Nutrients. 2024; 16(3):372. https://doi.org/10.3390/nu16030372
Chicago/Turabian StyleKim, Jeong-Mee, and Yean-Jung Choi. 2024. "Impact of Dietary Nutrients on the Prevalence of Dry Eye Syndrome among Korean Women Aged 40 and above: Evidence from the Korea National Health and Nutrition Examination Survey" Nutrients 16, no. 3: 372. https://doi.org/10.3390/nu16030372
APA StyleKim, J.-M., & Choi, Y.-J. (2024). Impact of Dietary Nutrients on the Prevalence of Dry Eye Syndrome among Korean Women Aged 40 and above: Evidence from the Korea National Health and Nutrition Examination Survey. Nutrients, 16(3), 372. https://doi.org/10.3390/nu16030372






