Examining Associations Between Fasting Behavior, Orthorexia Nervosa, and Eating Disorders
Abstract
1. Introduction
1.1. Fasting Behavior
1.2. Fasting and Eating Disorders
1.3. The Current Study
- Fasting people score higher compared with non-fasting individuals in terms of symptoms of orthorexia and eating disorders.
- There is a positive association between fasting, dieting, overweight, orthorexia, and eating disorders symptoms.
- Fasting contributes to eating disorder symptoms directly (path c) and indirectly via orthorexia (paths a and b) (Figure 1).
2. Materials and Methods
2.1. Study Design and Procedure
2.2. Measures
2.2.1. Eating Patterns Related to Fasting and Dieting
2.2.2. Eating Disorders
2.2.3. Orthorexia Nervosa
2.2.4. Demographics
2.3. Participant Demographic Characteristics
2.4. Statistical Analyses
3. Results
3.1. Eating Behaviors in Participants
3.2. Intergroup Differences in Orthorexia and Eating Disorder Symptoms
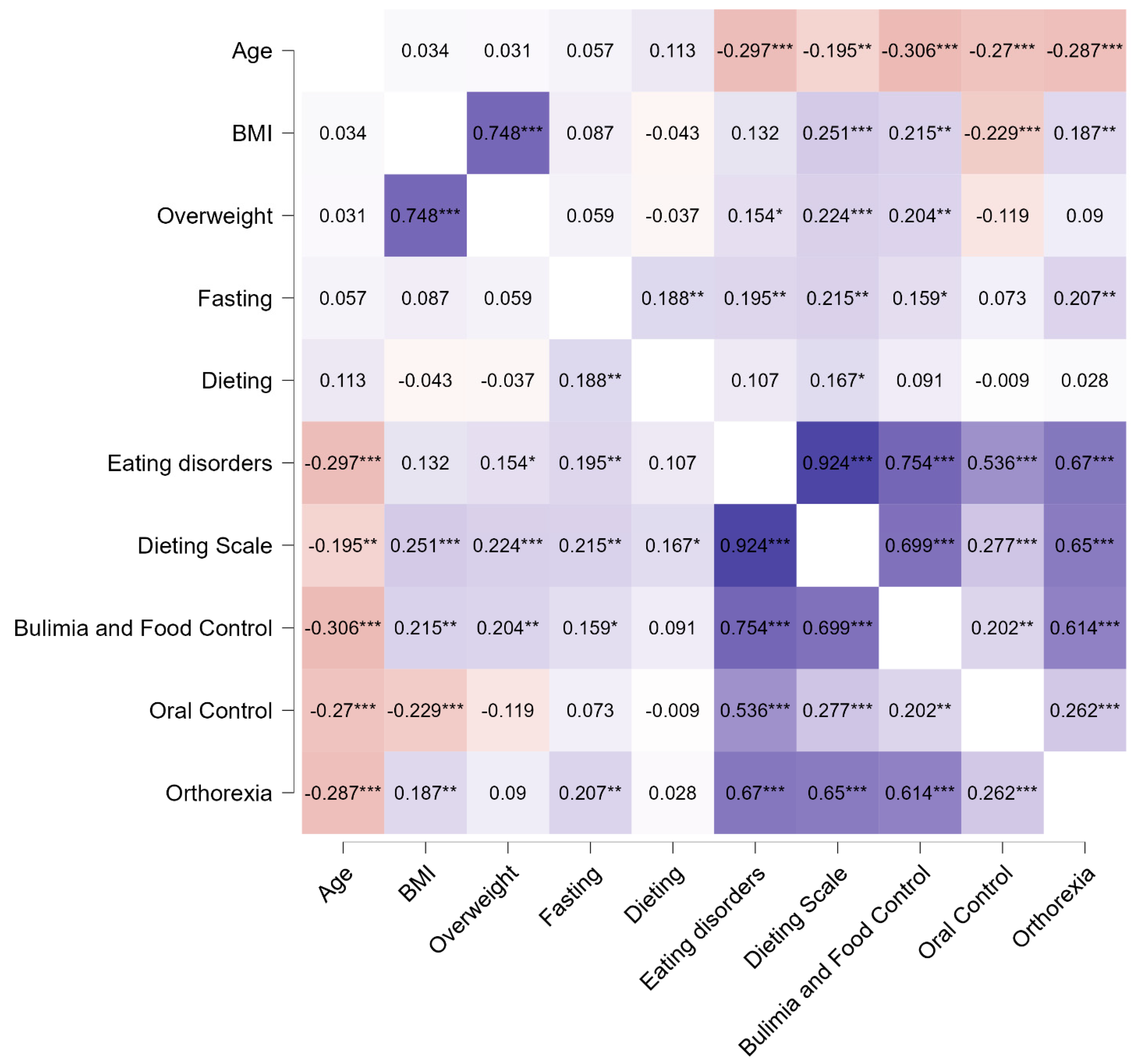
3.3. Associations Between Fasting, Dieting, Overweight, and Symptoms of Orthorexia and Eating Disorder
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mackieh, R.; Al-Bakkar, N.; Kfoury, M.; Okdeh, N.; Pietra, H.; Roufayel, R.; Legros, C.; Fajloun, Z.; Sabatier, J.-M. Unlocking the Benefits of Fasting: A Review of Its Impact on Various Biological Systems and Human Health. Curr. Med. Chem. 2024, 31, 1781–1803. [Google Scholar] [CrossRef] [PubMed]
- Sarro, A.A.; Payedimarri, A.B.; Concina, D.D.; Farsoni, M.F.; Piu, N.N.; Rinaldi, C.; Panella, M.P. The Efficacy of Fasting Regimens on Health Outcomes: A Systematic Overview. Minerva Gastroenterol. 2021, 67, 289–298. [Google Scholar] [CrossRef]
- Shazman, S. A Machine Learning Approach to Select the Type of Intermittent Fasting in Order to Improve Health by Effects on Type 2 Diabetes. In Proceedings of the BIOINFORMATICS 2020-11th International Conference on Bioinformatics Models, Methods and Algorithms, Proceedings. Part of 13th International Joint Conference on Biomedical Engineering Systems and Technologies, BIOSTEC 2020, Valletta, Malta, 24–26 February 2020; pp. 131–137. [Google Scholar] [CrossRef]
- Vasim, I.; Majeed, C.N.; DeBoer, M.D. Intermittent Fasting and Metabolic Health. Nutrients 2022, 14, 631. [Google Scholar] [CrossRef]
- Aragon, A.A.; Schoenfeld, B.J. Does Timing Matter? A Narrative Review of Intermittent Fasting Variants and Their Effects on Bodyweight and Body Composition. Nutrients 2022, 14, 5022. [Google Scholar] [CrossRef] [PubMed]
- Lecerf, J.-M. Update on Intermittent Diets | Le Point Sur Les Régimes Intermittents. Prat. Nutr. 2022, 18, 30–34. [Google Scholar] [CrossRef]
- Cienfuegos, S.; Corapi, S.; Gabel, K.; Ezpeleta, M.; Kalam, F.; Lin, S.; Pavlou, V.; Varady, K.A. Effect of Intermittent Fasting on Reproductive Hormone Levels in Females and Males: A Review of Human Trials. Nutrients 2022, 14, 2343. [Google Scholar] [CrossRef] [PubMed]
- Domaszewski, P.; Konieczny, M.; Pakosz, P.; Baczkowicz, D.; Sadowska-Krępa, E. Effect of a Six-Week Intermittent Fasting Intervention Program on the Composition of the Human Body in Women over 60 Years of Age. Int. J. Environ. Res. Public Health 2020, 17, 4138. [Google Scholar] [CrossRef]
- Domaszewski, P.; Konieczny, M.; Pakosz, P.; Łukaniszyn-Domaszewska, K.; Mikuláková, W.; Sadowska-Krępa, E.; Anton, S. Effect of a Six-Week Times Restricted Eating Intervention on the Body Composition in Early Elderly Men with Overweight. Sci. Rep. 2022, 12, 1–6. [Google Scholar] [CrossRef]
- Domaszewski, P.; Konieczny, M.; Dybek, T.; Łukaniszyn-Domaszewska, K.; Anton, S.; Sadowska-Krępa, E.; Skorupska, E. Comparison of the Effects of Six-Week Time-Restricted Eating on Weight Loss, Body Composition, and Visceral Fat in Overweight Older Men and Women. Exp. Gerontol. 2023, 174, 112116. [Google Scholar] [CrossRef]
- Noon, M.J.; Khawaja, H.A.; Ishtiaq, O.; Khawaja, Q.; Minhas, S.; Niazi, A.K.; Minhas, A.M.K.; Malhi, U.R. Fasting with Diabetes: A Prospective Observational Study. BMJ Glob. Health 2016, 1, e000009. [Google Scholar] [CrossRef]
- Malinowski, B.; Zalewska, K.; Węsierska, A.; Sokołowska, M.M.; Socha, M.; Liczner, G.; Pawlak-Osińska, K.; Wiciński, M. Intermittent Fasting in Cardiovascular Disorders—An Overview. Nutrients 2019, 11, 673. [Google Scholar] [CrossRef]
- Schoonakker, M.P.; van den Burg, E.L.; van Peet, P.G.; Lamb, H.J.; Numans, M.E.; Pijl, H. Intermittent Fasting. In Visceral and Ectopic Fat. Risk Factors for Type 2 Diabetes, Atherosclerosis, and Cardiovascular Disease; Lamb, H.J., Ed.; Elsevier Inc.: New York, NY, USA, 2023; pp. 307–319. [Google Scholar] [CrossRef]
- Varady, K.A.; Cienfuegos, S.; Ezpeleta, M.; Gabel, K. Cardiometabolic Benefits of Intermittent Fasting. Annu. Rev. Nutr. 2021, 41, 333–361. [Google Scholar] [CrossRef] [PubMed]
- Dong, T.A.; Sandesara, P.B.; Dhindsa, D.S.; Mehta, A.; Arneson, L.C.; Dollar, A.L.; Taub, P.R.; Sperling, L.S. Intermittent Fasting: A Heart Healthy Dietary Pattern? Am. J. Med. 2020, 133, 901–907. [Google Scholar] [CrossRef]
- Aparicio, A.; Lorenzo-Mora, A.M.; Trabado-Fernández, A.; Loria-Kohen, V.; López-Sobaler, A.M. Cardiometabolic Effects of Intermittent Fasting in Women|Efectos Cardiometabólicos Del Ayuno Intermitente En La Mujer. Nutr. Hosp. 2023, 40, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Zeng, M.; Wan, W.; Huang, M.; Li, X.; Xie, Z.; Wang, S.; Cai, Y. The Health-Promoting Effects and the Mechanism of Intermittent Fasting. J. Diabetes Res. 2023, 2023, 4038546. [Google Scholar] [CrossRef]
- Song, D.-K.; Kim, Y.-W. Beneficial Effects of Intermittent Fasting: A Narrative Review. J. Yeungnam Med. Sci. 2023, 40, 4–11. [Google Scholar] [CrossRef]
- Lushchak, O.; Strilbyska, O.; Piskovatska, V.; Koliada, A.; Storey, K.B. Intermittent Fasting. In Encyclopedia of Biomedical Gerontology; Rattan, S.I.S., Ed.; Elsevier Inc.: New York, NY, USA, 2019; pp. 279–290. [Google Scholar] [CrossRef]
- Lange, M.G.; Coffey, A.A.; Coleman, P.C.; Barber, T.M.; Van Rens, T.; Oyebode, O.; Abbott, S.; Hanson, P. Metabolic Changes with Intermittent Fasting. J. Hum. Nutr. Diet. 2024, 37, 256–269. [Google Scholar] [CrossRef] [PubMed]
- Hoddy, K.K.; Marlatt, K.L.; Çetinkaya, H.; Ravussin, E. Intermittent Fasting and Metabolic Health: From Religious Fast to Time-Restricted Feeding. Obesity 2020, 28, S29–S37. [Google Scholar] [CrossRef]
- Molina-Jiménez, A.; López-Oliva, S.; Garicano-Vilar, E.; Morais-Moreno, M.D.C.; De Cuevillas, B.; De Prado, J.G.; Ávila-Díaz, E.; Mauro-Martín, I.S. Biochemistry and Endocrine Changes after a 6-Week Mediterranean Diet Intervention with Fasting for Weight Loss. EuroMediterranean Biomed. J. 2019, 14, 90–95. [Google Scholar] [CrossRef]
- Sofi, F. FASTING-MIMICKING DIET a Clarion Call for Human Nutrition Research or an Additional Swan Song for a Commercial Diet? Int. J. Food Sci. Nutr. 2020, 71, 921–928. [Google Scholar] [CrossRef]
- Ghaderi, A. Eating Disorders. Eating disorders. In Functional Analysis in Clinical Treatment, 2nd ed.; Sturmey, P., Ed.; Elsevier Inc.: New York, NY, USA, 2020; pp. 421–449. [Google Scholar] [CrossRef]
- Galmiche, M.; Déchelotte, P.; Lambert, G.; Tavolacci, M.P. Prevalence of Eating Disorders over the 2000–2018 Period: A Systematic Literature Review. Am. J. Clin. Nutr. 2019, 109, 1402–1413. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.A.; Ortiz, A.M.L.; Smith, G.T. The Occurrence and Covariation of Binge Eating and Compensatory Behaviors Across Early to Mid-Adolescence. J. Pediatr. Psychol. 2018, 43, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Schaumberg, K.; Anderson, D.A.; Reilly, E.E.; Anderson, L.M. Does Short-Term Fasting Promote Pathological Eating Patterns? Eat. Behav. 2015, 19, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.H.; Joo, Y.; Kim, M.-S.; Choe, H.K.; Tong, Q.; Kwon, O. Effects of Intermittent Fasting on the Circulating Levels and Circadian Rhythms of Hormones. Endocrinol. Metab. 2021, 36, 745–756. [Google Scholar] [CrossRef]
- Akgül, S.; Derman, O.; Kanbur, O.N. Fasting during Ramadan: A Religious Factor as a Possible Trigger or Exacerbator for Eating Disorders in Adolescents. Int. J. Eat. Disord. 2014, 47, 905–910. [Google Scholar] [CrossRef]
- Ganson, K.T.; Cuccolo, K.; Hallward, L.; Nagata, J.M. Intermittent Fasting: Describing Engagement and Associations with Eating Disorder Behaviors and Psychopathology among Canadian Adolescents and Young Adults. Eat. Behav. 2022, 47, 101681. [Google Scholar] [CrossRef]
- Longobardi, C.; Badenes-Ribera, L.; Fabris, M.A. Adverse Childhood Experiences and Body Dysmorphic Symptoms: A Meta-Analysis. Body Image 2022, 40, 267–284. [Google Scholar] [CrossRef]
- Badenes-Ribera, L.; Longobardi, C.; Gastaldi, F.G.M.; Fabris, M.A. The Roles of Attachment to Parents and Gender in the Relationship between Parental Criticism and Muscle Dysmorphia Symptomatology in Adolescence. Int. J. Adolesc. Youth 2021, 26, 513–528. [Google Scholar] [CrossRef]
- Chia, J.L.P.; Fuller-Tyszkiewicz, M.; Buck, K.; Chamari, K.; Richardson, B.; Krug, I. An Ecological Momentary Assessment of the Effect of Fasting during Ramadan on Disordered Eating Behaviors. Appetite 2018, 127, 44–51. [Google Scholar] [CrossRef]
- Cserép, M.; Szumska, I. Disordered Eating among Adolescents with Chronic Illnesses | Evészavartünetek, Problematikus Evési Magatartás Egyes Kamaszkori Krónikus Betegségekben. Orvosi Hetil. 2020, 161, 1872–1876. [Google Scholar] [CrossRef]
- Cuccolo, K.; Kramer, R.; Petros, T.; Thoennes, M. Intermittent Fasting Implementation and Association with Eating Disorder Symptomatology. Eat. Disord. 2022, 30, 471–491. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, W.R.; Neves, A.N.; Donofre, G.S.; Bratman, S.; Teixeira, P.C.; Campos, J.A.D.B. Conceptualizing and Evaluating the Healthy Orthorexia Dimension. In Eating Disorders; Patel, V.B., Preedy, V.R., Eds.; Springer: Cham, Switzerland, 2023; Volume 2, pp. 1479–1502. [Google Scholar] [CrossRef]
- Goutaudier, N.; Rousseau, A. Orthorexia, a Pathological Obsession|L’orthorexie, Une Obsession Pathologique. Prat. Nutr. 2021, 17, 28–30. [Google Scholar] [CrossRef]
- Olejniczak, D.; Bugajec, D.; Panczyk, M.; Brytek-Matera, A.; Religioni, U.; Czerw, A.; Grąbczewska, A.; Juszczyk, G.; Jabłkowska-Górecka, K.; Staniszewska, A. Analysis Concerning Nutritional Behaviors in the Context of the Risk of Orthorexia. Neuropsychiatr. Dis. Treat. 2017, 13, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Luck-Sikorski, C.; Jung, F.; Schlosser, K.; Riedel-Heller, S.G. Is Orthorexic Behavior Common in the General Public? A Large Representative Study in Germany. Eat. Weight Disord. 2019, 24, 267–273. [Google Scholar] [CrossRef]
- Foyster, M.; Sultan, N.; Tonkovic, M.; Govus, A.; Burton-Murray, H.; Tuck, C.J.; Biesiekierski, J.R. Assessing the Presence and Motivations of Orthorexia Nervosa among Athletes and Adults with Eating Disorders: A Cross-Sectional Study. Eat. Weight Disord. 2023, 28, 101. [Google Scholar] [CrossRef]
- Romano, K.A.; Heron, K.E.; Amerson, R.; Howard, L.M.; MacIntyre, R.I.; Mason, T.B. Changes in Disordered Eating Behaviors over 10 or More Years: A Meta-Analysis. Int. J. Eat. Disord. 2020, 53, 1034–1055. [Google Scholar] [CrossRef]
- Rodgers, R.F.; White, M.; Berry, R. Orthorexia Nervosa, Intuitive Eating, and Eating Competence in Female and Male College Students. Eat. Weight Disord. 2021, 26, 2625–2632. [Google Scholar] [CrossRef]
- Barthels, F.; Meyer, F.; Huber, T.; Pietrowsky, R. Analysis of Orthorexic Eating Behavior in Patients with Eating Disorder and Obsessive-Compulsive Disorder | Analyse Des Orthorektischen Ernährungsverhaltens von Patienten Mit Essstörungen Und Mit Zwangsstörungen. Z. Klin. Psychol. Psychother. 2017, 46, 32–41. [Google Scholar] [CrossRef]
- Cosh, S.M.; Olson, J.; Tully, P.J. Exploration of Orthorexia Nervosa and Diagnostic Overlap with Eating Disorders, Anorexia Nervosa and Obsessive-Compulsive Disorder. Int. J. Eat. Disord. 2023, 56, 2155–2161. [Google Scholar] [CrossRef]
- Novara, C.; Pardini, S.; Visioli, F.; Meda, N. Orthorexia Nervosa and Dieting in a Non-Clinical Sample: A Prospective Study. Eat. Weight Disord. 2022, 27, 2081–2093. [Google Scholar] [CrossRef]
- Rogowska, A.M.; Kwaśnicka, A.; Ochnik, D. Validation and Polish Adaptation of the Authorized Bratman Orthorexia Self-Test (Abost): Comparison of Dichotomous and Continuous Likert-Type Response Scales. Psychol. Res. Behav. Manag. 2021, 14, 921–931. [Google Scholar] [CrossRef] [PubMed]
- Skella, P.; Chelmi, M.E.; Panagouli, E.; Garoufi, A.; Psaltopoulou, T.; Mastorakos, G.; Sergentanis, T.N.; Tsitsika, A. Orthorexia and Eating Disorders in Adolescents and Young Adults: A Systematic Review. Children 2022, 9, 514. [Google Scholar] [CrossRef] [PubMed]
- Messer, M.; Liu, C.; Linardon, J. Orthorexia Nervosa Symptoms Prospectively Predict Symptoms of Eating Disorders and Depression. Eat. Behav. 2023, 49, 101734. [Google Scholar] [CrossRef] [PubMed]
- Mintz, L.B.; O’Halloran, M.S. The Eating Attitudes Test: Validation With DSM-IV Eating Disorder Criteria. J. Personal. Assess. 2000, 74, 489–503. [Google Scholar] [CrossRef]
- Rogoza, R.; Brytek-Matera, A.; Garner, D.M. Analysis of the EAT-26 in a Non-Clinical Sample. Arch. Psychiatry Psychother. 2016, 18, 54–58. [Google Scholar] [CrossRef]
- Desai, M.N.; Miller, W.C.; Staples, B.; Bravender, T. Risk Factors Associated With Overweight and Obesity in College Students. J. Am. Coll. Health 2008, 57, 109–114. [Google Scholar] [CrossRef]
- Efron, B.; Tibshirani, R.J. Chapter 17: Cross-Validation. In An Introduction to Bootstrap; Chapman and Hall: New York, NY, USA, 1993; p. 436. [Google Scholar]
- Kline, R.B. Response to Leslie Hayduk’s Review of Principles and Practice of Structural Equation Modeling,1 4th Edition. Can. Stud. Popul. 2018, 45, 188–195. [Google Scholar] [CrossRef]
- Kim, J.Y. Optimal Diet Strategies for Weight Loss and Weight Loss Maintenance. J. Obes. Metab. Syndr. 2021, 30, 20–31. [Google Scholar] [CrossRef]
- Savas, E.; Öztürk, Z.A.; Tanrıverdi, D.; Kepekçi, Y. Do Ramadan Fasting Restrictions Alter Eating Behaviours in Obese Women? J. Relig. Health 2014, 53, 135–140. [Google Scholar] [CrossRef]
- Cena, H.; Barthels, F.; Cuzzolaro, M.; Bratman, S.; Brytek-Matera, A.; Dunn, T.; Varga, M.; Missbach, B.; Donini, L.M. Definition and Diagnostic Criteria for Orthorexia Nervosa: A Narrative Review of the Literature. Eat. Weight Disord. 2019, 24, 209–246. [Google Scholar] [CrossRef]
- Tamam, L.; Yılmaz, H. Linking Orthorexia and Obsessive-Compulsive Symptoms. In Eating Disorders; Patel, V.B., Preedy, V.R., Eds.; Springer: Cham, Switzerland, 2023; Volume 2, pp. 1353–1380. [Google Scholar] [CrossRef]
- Messer, M.; Liu, C.; McClure, Z.; Mond, J.; Tiffin, C.; Linardon, J. Negative Body Image Components as Risk Factors for Orthorexia Nervosa: Prospective Findings. Appetite 2022, 178, 106280. [Google Scholar] [CrossRef]
- Sultan, N.; Foyster, M.; Tonkovic, M.; Noon, D.; Burton-Murray, H.; Biesiekierski, J.R.; Tuck, C.J. Presence and Characteristics of Disordered Eating and Orthorexia in Irritable Bowel Syndrome. Neurogastroenterol. Motil. 2024, 36, e14797. [Google Scholar] [CrossRef] [PubMed]
- Tuck, C.J.; Sultan, N.; Tonkovic, M.; Biesiekierski, J.R. Orthorexia Nervosa Is a Concern in Gastroenterology: A Scoping Review. Neurogastroenterol. Motil. 2022, 34, e14427. [Google Scholar] [CrossRef] [PubMed]
- Stutts, L.A. It’s Complicated: The Relationship between Orthorexia and Weight/Shape Concerns, Eating Behaviors, and Mood. Eat. Behav. 2020, 39, 101444. [Google Scholar] [CrossRef]
- Barthels, F. New Developments in Orthorexia Research: Use of Social Media, Healthy Orthorexia and Testimonials from Affected Individuals. Ernahr. Umsch. 2023, 70, 36–40. [Google Scholar] [CrossRef]
- Walker-Swanton, F.E.; Hay, P.; Conti, J.E. Perceived Need for Treatment Associated with Orthorexia Nervosa Symptoms. Eat. Behav. 2020, 38, 101415. [Google Scholar] [CrossRef]
- Barthels, F.; Meyer, F.; Pietrowsky, R. Orthorexic Eating Behavior. Ernahr. Umsch. 2015, 62, M568–M573. [Google Scholar]


| Variable | Categories | n/M | %/SD |
|---|---|---|---|
| Age | Years old | 27.95 | 9.44 |
| Gender | Women | 185 | 86.45 |
| Men | 26 | 12.15 | |
| Nonbinary person | 3 | 1.4 | |
| Biometric data | Height | 168.82 | 7.86 |
| Weight | 66.02 | 13.94 | |
| Body mass index | 23.06 | 3.97 | |
| Underweight | 18 | 8.41 | |
| Average weight | 143 | 66.82 | |
| Overweight | 42 | 19.63 | |
| Obese | 11 | 5.14 | |
| Education | Primary | 4 | 1.87 |
| Professional | 3 | 1.4 | |
| Secondary | 65 | 30.37 | |
| Bachelor’s degree | 73 | 34.11 | |
| Master’s degree or higher | 68 | 31.78 | |
| Place of residence | Village | 65 | 30.37 |
| City with up to 20,000 inhabitants | 34 | 15.89 | |
| City with 20,000–100,000 inhabitants | 29 | 13.55 | |
| City with 100,000 to 500,000 inhabitants | 66 | 30.84 | |
| City with more than 500,000 inhabitants | 20 | 9.35 | |
| Economic status | Poor (not enough to meet basic needs) | 4 | 1.87 |
| Sufficient (enough to meet basic needs) | 48 | 22.43 | |
| Good (slightly more than to meet basic needs) | 109 | 50.94 | |
| Very good (enough to meet all needs) | 53 | 24.77 |
| Variable | Categories | n | % |
|---|---|---|---|
| Fasting | No | 116 | 54.21 |
| Yes | 98 | 45.79 | |
| Duration of fasting | I don’t use any fasts | 117 | 54.67 |
| From a week to two months | 21 | 9.81 | |
| From 2 to 6 months | 10 | 4.67 | |
| From 6 to 12 months | 22 | 10.28 | |
| From 1 to 5 years | 28 | 13.08 | |
| Over 5 years old | 16 | 7.48 | |
| Fasting pattern | I don’t use any fasts | 117 | 54.67 |
| Every day 12/12 h | 12 | 5.61 | |
| Every day 14/10 h | 10 | 4.67 | |
| 16/8 h every day | 36 | 16.82 | |
| 18/6 h every day | 7 | 3.27 | |
| Every other day | 4 | 1.87 | |
| Once a week | 10 | 4.67 | |
| Twice weekly | 5 | 2.34 | |
| Other pattern | 13 | 6.07 | |
| Dieting | No | 147 | 68.69 |
| Yes | 67 | 31.31 | |
| Type of diet | I don’t follow any special diet, but I try to eat healthily | 117 | 54.67 |
| I don’t follow any special diet, I eat whatever I want | 30 | 14.02 | |
| Meatless diet (vegetarian, vegetarian, vegan, fruitarian, etc.) | 22 | 10.28 | |
| Clean eating diet (no artificial additives, preservatives, sugar, etc.) | 15 | 7.01 | |
| Slimming diet | 10 | 4.67 | |
| Paleo diet (based on meat and animal fats) | 3 | 1.40 | |
| Colorful diet (based on colorful fruits and vegetables) | 3 | 1.40 | |
| Other diets | 14 | 6.54 | |
| Motives of dieting | For my health | 103 | 48.13 |
| I don’t follow any special diet | 84 | 39.25 | |
| Because the doctor recommended it to me | 5 | 2.34 | |
| To avoid unpleasant ailments (e.g., heartburn, stomach pain, headaches) | 22 | 10.28 | |
| Health problems | I do not have allergies or other chronic diseases | 144 | 67.29 |
| Allergy | 46 | 21.50 | |
| Diabetes, insulin resistance | 5 | 2.34 | |
| Reflux, stomach or duodenal ulcers, irritable bowel syndrome, liver disease | 12 | 5.61 | |
| Other reasons (i.e., Hashimoto’s disease, hypothyroidism, high cholesterol, hypertension, low iron, or obesity) | 7 | 3.27 |
| Variable | Categories | n/M | %/SD |
|---|---|---|---|
| Orthorexia test | ABOST total score (M, SD) | 12.08 | 5.55 |
| Orthorexia symptoms | No (ABOST < 19) | 187 | 87.38 |
| Yes (ABOST > 18) | 27 | 12.62 | |
| Eating disorder test | EAT-26 total score (M, SD) | 15.96 | 12.69 |
| Dieting subscale (M, SD) | 10.17 | 8.11 | |
| Bulimia and food preoccupation subscale (M, SD) | 2.37 | 3.50 | |
| Oral control subscale (M, SD) | 3.42 | 3.39 | |
| Eating disorders symptoms | No (EAT-26 < 20) | 187 | 87.38 |
| Yes (EAT-26 > 19) | 27 | 12.62 | |
| Binge eating | No (EAT_A = 0) | 157 | 73.36 |
| Yes (EAT_A = 1) | 57 | 26.64 | |
| Shape control | No (EAT_B = 0) | 175 | 81.78 |
| Yes (EAT_B = 1) | 39 | 18.22 | |
| Purging | No (EAT_C = 0) | 168 | 78.51 |
| Yes (EAT_C = 1) | 46 | 21.50 | |
| Excessive exercise | No (EAT_D = 0) | 197 | 92.06 |
| Yes (EAT_D = 1) | 17 | 7.94 | |
| Weight loss | No (EAT_E = 0) | 188 | 87.85 |
| Yes (EAT_E = 1) | 26 | 12.15 |
| Variable | Not Fasting (n = 98) | Fasting (n = 116) | U-Test | p | RBC | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Orthorexia symptoms | 10.99 | 4.86 | 13.37 | 6.05 | 4323.50 | 0.002 | –0.24 |
| Eating disorder symptoms | 13.60 | 10.99 | 18.77 | 14.00 | 4404.00 | 0.005 | –0.23 |
| Dieting | 8.41 | 6.74 | 12.27 | 9.07 | 4271.50 | 0.002 | –0.25 |
| Bulimia and food preoccupation | 1.95 | 3.28 | 2.88 | 3.70 | 4688.00 | 0.021 | –0.18 |
| Oral control | 3.24 | 3.39 | 3.62 | 3.38 | 5205.00 | 0.285 | –0.08 |
| Model | Variable | b | SE b | β | t | R | R2 | F | df |
|---|---|---|---|---|---|---|---|---|---|
| H0 | Intercept | 23.03 | 2.56 | 8.99 *** | 0.44 | 0.19 | 12.36 *** | 4.209 | |
| Age | –0.44 | 0.09 | –0.32 | –5.12 *** | |||||
| Fasting | 4.22 | 1.61 | 2.62 ** | ||||||
| Dieting | 5.73 | 1.75 | 3.27 ** | ||||||
| Overweight | 5.50 | 1.83 | 3.00 ** | ||||||
| H1 | Intercept | –0.82 | 2.30 | –0.36 | 0.79 | 0.63 | 71.03 *** | 5.208 | |
| Age | –0.19 | 0.06 | –0.14 | –3.13 ** | |||||
| Fasting | 0.54 | 1.12 | 0.49 | ||||||
| Dieting | 4.25 | 1.19 | 3.56 *** | ||||||
| Overweight | 3.87 | 1.25 | 3.10 ** | ||||||
| Orthorexia | 1.61 | 0.10 | 0.71 | 15.73 *** |
| BCa 95% CI | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Effect | Predictor | Mediator | Outcome | b | SE b | z | p | LL | UL |
| Total | Fasting | => | Eating disorders | 5.17 | 1.70 | 3.04 | 0.002 | 2.01 | 8.64 |
| Path | Fasting | => | Orthorexia | 2.38 | 0.74 | 3.20 | 0.001 | 0.76 | 3.84 |
| Path | Orthorexia | => | Eating disorders | 1.72 | 0.10 | 16.70 | <0.001 | 1.48 | 1.96 |
| Indirect | Fasting | Orthorexia | Eating disorders | 4.10 | 1.30 | 3.14 | 0.002 | 1.33 | 6.78 |
| Direct | Fasting | Orthorexia | Eating disorders | 1.08 | 1.15 | 0.94 | 0.349 | –1.18 | 3.27 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domaszewski, P.; Rogowska, A.M.; Żylak, K. Examining Associations Between Fasting Behavior, Orthorexia Nervosa, and Eating Disorders. Nutrients 2024, 16, 4275. https://doi.org/10.3390/nu16244275
Domaszewski P, Rogowska AM, Żylak K. Examining Associations Between Fasting Behavior, Orthorexia Nervosa, and Eating Disorders. Nutrients. 2024; 16(24):4275. https://doi.org/10.3390/nu16244275
Chicago/Turabian StyleDomaszewski, Przemysław, Aleksandra M. Rogowska, and Kaja Żylak. 2024. "Examining Associations Between Fasting Behavior, Orthorexia Nervosa, and Eating Disorders" Nutrients 16, no. 24: 4275. https://doi.org/10.3390/nu16244275
APA StyleDomaszewski, P., Rogowska, A. M., & Żylak, K. (2024). Examining Associations Between Fasting Behavior, Orthorexia Nervosa, and Eating Disorders. Nutrients, 16(24), 4275. https://doi.org/10.3390/nu16244275







