Adherence to the Cancer Prevention Recommendations from World Cancer Research Fund/American Institute for Cancer Research After Cancer Diagnosis on Mortality in South Korea
Abstract
1. Introduction
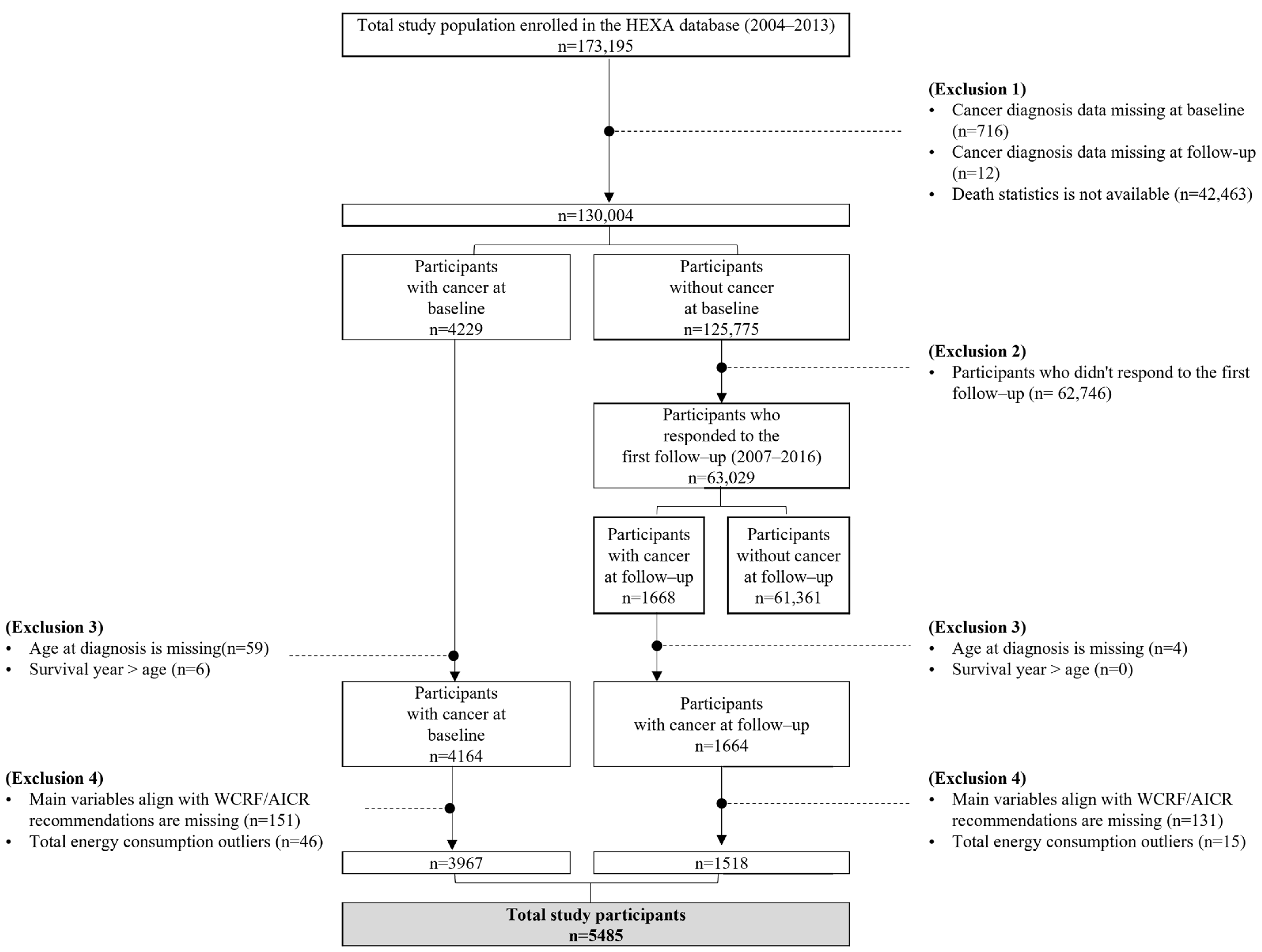
2. Materials and Methods
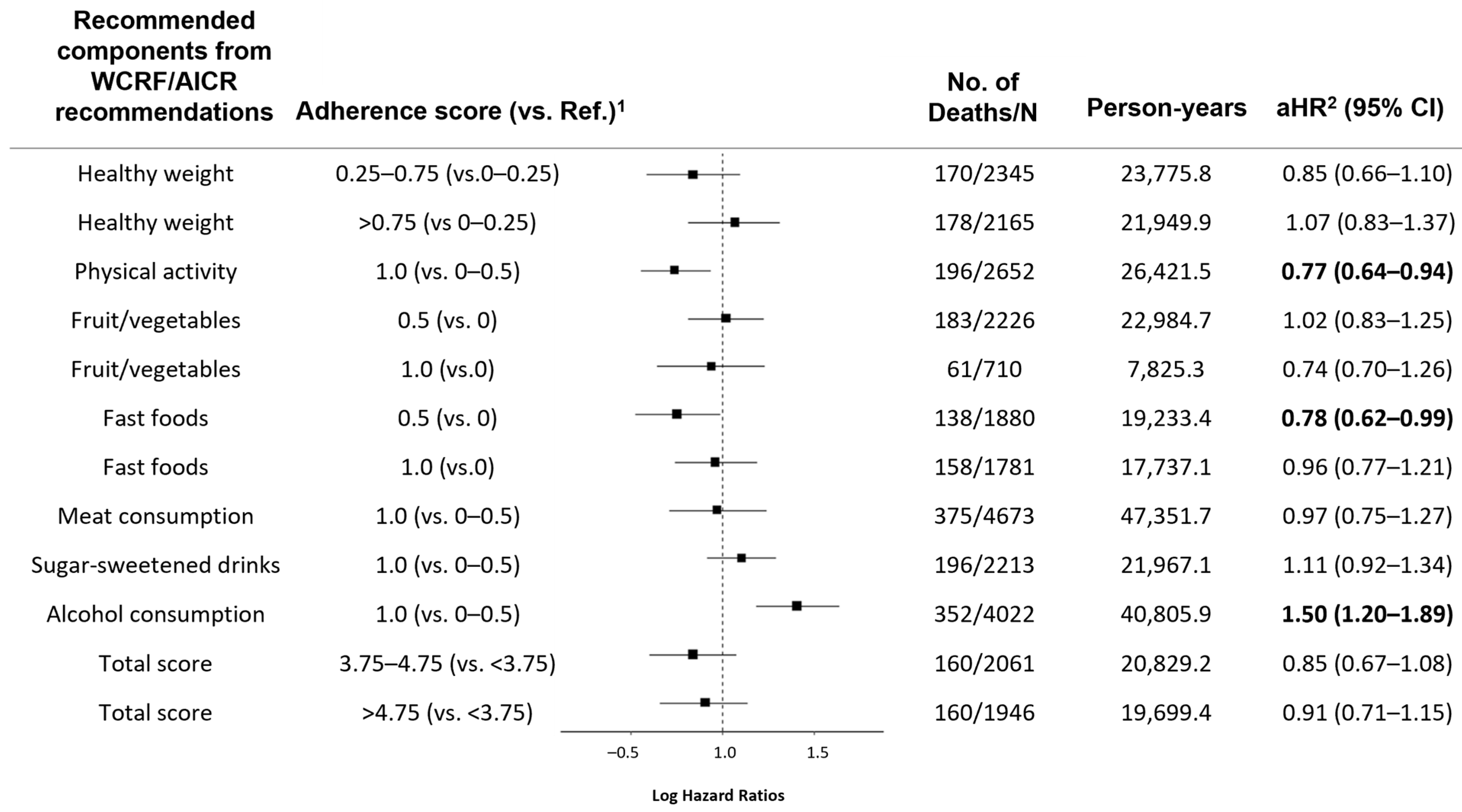
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Denlinger, C.S.; Carlson, R.W.; Are, M.; Baker, K.S.; Davis, E.; Edge, S.B.; Friedman, D.L.; Goldman, M.; Jones, L.; King, A. Survivorship: Introduction and definition. J. Natl. Compr. Cancer Netw. 2014, 12, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Gallicchio, L.; Tonorezos, E.; de Moor, J.S.; Elena, J.; Farrell, M.; Green, P.; Mitchell, S.A.; Mollica, M.A.; Perna, F.; Saiontz, N.G. Evidence gaps in cancer survivorship care: A report from the 2019 National Cancer Institute Cancer Survivorship Workshop. JNCI J. Natl. Cancer Inst. 2021, 113, 1136–1142. [Google Scholar] [CrossRef] [PubMed]
- Park, E.H.; Jung, K.-W.; Park, N.J.; Kang, M.J.; Yun, E.H.; Kim, H.-J.; Kim, J.-E.; Kong, H.-J.; Im, J.-S.; Seo, H.G. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2021. Cancer Res. Treat. 2024, 56, 357–371. [Google Scholar] [CrossRef]
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hütterer, E.; Isenring, E.; Kaasa, S. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017, 36, 11–48. [Google Scholar] [CrossRef]
- Rock, C.L.; Thomson, C.A.; Sullivan, K.R.; Howe, C.L.; Kushi, L.H.; Caan, B.J.; Neuhouser, M.L.; Bandera, E.V.; Wang, Y.; Robien, K. American Cancer Society nutrition and physical activity guideline for cancer survivors. CA A Cancer J. Clin. 2022, 72, 230–262. [Google Scholar] [CrossRef]
- Clinton, S.K.; Giovannucci, E.L.; Hursting, S.D. The world cancer research fund/American institute for cancer research third expert report on diet, nutrition, physical activity, and cancer: Impact and future directions. J. Nutr. 2020, 150, 663–671. [Google Scholar] [CrossRef]
- Shams-White, M.M.; Brockton, N.T.; Mitrou, P.; Romaguera, D.; Brown, S.; Bender, A.; Kahle, L.L.; Reedy, J. Operationalizing the 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) cancer prevention recommendations: A standardized scoring system. Nutrients 2019, 11, 1572. [Google Scholar] [CrossRef]
- Shams-White, M.M.; Romaguera, D.; Mitrou, P.; Reedy, J.; Bender, A.; Brockton, N.T. Further guidance in implementing the standardized 2018 world cancer research fund/american institute for cancer research (WCRF/AICR) score. Cancer Epidemiol. Biomark. Prev. 2020, 29, 889–894. [Google Scholar] [CrossRef]
- Greenlee, H.; Unger, J.M.; LeBlanc, M.; Ramsey, S.; Hershman, D.L. Association between body mass index and cancer survival in a pooled analysis of 22 clinical trials. Cancer Epidemiol. Biomark. Prev. 2017, 26, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Takemura, N.; Chan, S.L.; Smith, R.; Cheung, D.S.T.; Lin, C.-C. The effects of physical activity on overall survival among advanced cancer patients: A systematic review and meta-analysis. BMC Cancer 2021, 21, 242. [Google Scholar] [CrossRef] [PubMed]
- Rinninella, E.; Mele, M.C.; Cintoni, M.; Raoul, P.; Ianiro, G.; Salerno, L.; Pozzo, C.; Bria, E.; Muscaritoli, M.; Molfino, A. The facts about food after cancer diagnosis: A systematic review of prospective cohort studies. Nutrients 2020, 12, 2345. [Google Scholar] [CrossRef] [PubMed]
- Molina-Montes, E.; Salamanca-Fernández, E.; Garcia-Villanova, B.; Sánchez, M.J. The impact of plant-based dietary patterns on cancer-related outcomes: A rapid review and meta-analysis. Nutrients 2020, 12, 2010. [Google Scholar] [CrossRef]
- Spring, B.; Moller, A.C.; Coons, M.J. Multiple health behaviours: Overview and implications. J. Public Health 2012, 34 (Suppl. S1), i3–i10. [Google Scholar] [CrossRef]
- Tollosa, D.N.; Tavener, M.; Hure, A.; James, E.L. Adherence to multiple health behaviours in cancer survivors: A systematic review and meta-analysis. J. Cancer Surviv. 2019, 13, 327–343. [Google Scholar] [CrossRef]
- Song, R.; Petimar, J.; Wang, M.; Tabung, F.K.; Song, M.; Liu, L.; Lee, D.H.; Giovannucci, E.L.; Zhang, X.; Smith-Warner, S.A. Adherence to the world cancer research fund/American institute for cancer research cancer prevention recommendations and colorectal cancer survival. Cancer Epidemiol. Biomark. Prev. 2021, 30, 1816–1825. [Google Scholar] [CrossRef]
- Van Zutphen, M.; Boshuizen, H.C.; Kenkhuis, M.-F.; Wesselink, E.; Geijsen, A.J.; De Wilt, J.H.; Van Halteren, H.K.; Bilgen, E.J.S.; Keulen, E.T.; Janssen-Heijnen, M.L. Lifestyle after colorectal cancer diagnosis in relation to recurrence and all-cause mortality. Am. J. Clin. Nutr. 2021, 113, 1447–1457. [Google Scholar] [CrossRef]
- Langlais, C.S.; Graff, R.E.; Van Blarigan, E.L.; Neuhaus, J.M.; Cowan, J.E.; Broering, J.M.; Carroll, P.; Kenfield, S.A.; Chan, J.M. Post-diagnostic health behaviour scores and risk of prostate cancer progression and mortality. Br. J. Cancer 2023, 129, 346–355. [Google Scholar] [CrossRef]
- Gali, K.; Orban, E.; Ozga, A.K.; Möhl, A.; Behrens, S.; Holleczek, B.; Becher, H.; Obi, N.; Chang-Claude, J. Does breast cancer modify the long-term relationship between lifestyle behaviors and mortality? A prospective analysis of breast cancer survivors and population-based controls. Cancer 2024, 130, 781–791. [Google Scholar] [CrossRef]
- Kim, Y.; Han, B.-G.; Group, K. Cohort profile: The Korean genome and epidemiology study (KoGES) consortium. Int. J. Epidemiol. 2017, 46, e20. [Google Scholar] [CrossRef] [PubMed]
- Willett, W. Nutritional Epidemiology; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Ahn, Y.; Kwon, E.; Shim, J.; Park, M.; Joo, Y.; Kimm, K.; Park, C.; Kim, D. Validation and reproducibility of food frequency questionnaire for Korean genome epidemiologic study. Eur. J. Clin. Nutr. 2007, 61, 1435–1441. [Google Scholar] [CrossRef] [PubMed]
- Tollosa, D.N.; Tavener, M.; Hure, A.; James, E.L. Compliance with multiple health behaviour recommendations: A cross-sectional comparison between female cancer survivors and those with no cancer history. Int. J. Environ. Res. Public Health 2019, 16, 1345. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.H.; Lee, W.-Y.; Kim, S.S.; Kang, J.-H.; Kang, J.-H.; Kim, K.K.; Kim, B.-Y.; Kim, Y.-H.; Kim, W.-J.; Kim, E.M. 2018 Korean society for the study of obesity guideline for the management of obesity in Korea. J. Obes. Metab. Syndr. 2019, 28, 40. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Park, H.S.; Kim, D.J.; Han, J.H.; Kim, S.M.; Cho, G.J.; Kim, D.Y.; Kwon, H.S.; Kim, S.R.; Lee, C.B. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res. Clin. Pract. 2007, 75, 72–80. [Google Scholar] [CrossRef]
- Lee, J.; Shin, A.; Shin, W.-K.; Choi, J.-Y.; Kang, D.; Lee, J.-K. Adherence to the World Cancer Research Fund/American Institute for Cancer Research and Korean Cancer Prevention Guidelines and cancer risk: A prospective cohort study from the Health Examinees-Gem study. Epidemiol. Health 2023, 45, e2023070. [Google Scholar] [CrossRef]
- Kaluza, J.; Harris, H.R.; Håkansson, N.; Wolk, A. Adherence to the WCRF/AICR 2018 recommendations for cancer prevention and risk of cancer: Prospective cohort studies of men and women. Br. J. Cancer 2020, 122, 1562–1570. [Google Scholar] [CrossRef]
- Canchola, A.J.; Stewart, S.L.; Bernstein, L.; West, D.W.; Ross, R.K.; Deapen, D.; Pinder, R.; Reynolds, P.; Wright, W.; Anton-Culver, H. Cox Regression Using Different Time-Scales; Western Users of SAS Software: San Francisco, CA, USA, 2003. [Google Scholar]
- Martinez, C.F.; Di Castelnuovo, A.; Costanzo, S.; Ruggiero, E.; de Gaetano, G.; Iacoviello, L.; Bonaccio, M. Adherence to the WCRF/AICR Cancer Prevention Recommendations and All-Cause Mortality among Cancer Survivors from the Moli-sani Study Cohort. In Proceedings; MDPI: Basel, Switzerland, 2024; Volume 91, p. 156. [Google Scholar]
- Karavasiloglou, N.; Pestoni, G.; Wanner, M.; Faeh, D.; Rohrmann, S. Healthy lifestyle is inversely associated with mortality in cancer survivors: Results from the Third National Health and Nutrition Examination Survey (NHANES III). PLoS ONE 2019, 14, e0218048. [Google Scholar] [CrossRef]
- Schroeder, J.; Reitz, L.K.; Vieira, F.G.K.; da Silva, E.L.; Di Pietro, P.F. Low to moderate adherence to 2018 diet and physical exercise recommendations of the World Cancer Research Fund/American Institute for Cancer Research is associated with prooxidant biochemical profile in women undergoing adjuvant breast cancer treatment. Nutr. Res. 2023, 109, 1–11. [Google Scholar] [CrossRef]
- Penfold, C.M.; Thomas, S.J.; Waylen, A.; Ness, A.R. Change in alcohol and tobacco consumption after a diagnosis of head and neck cancer: Findings from head and neck 5000. Head Neck 2018, 40, 1389–1399. [Google Scholar] [CrossRef]
- Wu, W.; Guo, F.; Ye, J.; Li, Y.; Shi, D.; Fang, D.; Guo, J.; Li, L. Pre-and post-diagnosis physical activity is associated with survival benefits of colorectal cancer patients: A systematic review and meta-analysis. Oncotarget 2016, 7, 52095. [Google Scholar] [CrossRef] [PubMed]
- Salam, A.; Woodman, A.; Chu, A.; Al-Jamea, L.H.; Islam, M.; Sagher, M.; Sager, M.; Akhtar, M. Effect of post-diagnosis exercise on depression symptoms, physical functioning and mortality in breast cancer survivors: A systematic review and meta-analysis of randomized control trials. Cancer Epidemiol. 2022, 77, 102111. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Morielli, A.R.; Heer, E.; Kirkham, A.A.; Cheung, W.Y.; Usmani, N.; Friedenreich, C.M.; Courneya, K.S. Effects of exercise on cancer treatment efficacy: A systematic review of preclinical and clinical studies. Cancer Res. 2021, 81, 4889–4895. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.L.; Winters-Stone, K.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.; Matthews, C.; Ligibel, J.; Gerber, L. Exercise guidelines for cancer survivors: Consensus statement from international multidisciplinary roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375. [Google Scholar] [CrossRef]
- Hang, D.; Du, M.; Wang, L.; Wang, K.; Fang, Z.; Khandpur, N.; Rossato, S.L.; Steele, E.M.; Chan, A.T.; Hu, F.B. Ultra-processed food consumption and mortality among patients with stages I–III colorectal cancer: A prospective cohort study. EClinicalMedicine 2024, 71, 102572. [Google Scholar] [CrossRef]
- Schmidt, D.R.; Patel, R.; Kirsch, D.G.; Lewis, C.A.; Vander Heiden, M.G.; Locasale, J.W. Metabolomics in cancer research and emerging applications in clinical oncology. CA A Cancer J. Clin. 2021, 71, 333–358. [Google Scholar] [CrossRef]
- Kim, Y.; Je, Y.; Giovannucci, E.L. Association between alcohol consumption and survival in colorectal cancer: A meta-analysis. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1891–1901. [Google Scholar] [CrossRef]
- Minami, Y.; Kanemura, S.; Oikawa, T.; Suzuki, S.; Hasegawa, Y.; Miura, K.; Nishino, Y.; Kakugawa, Y.; Fujiya, T. Associations of cigarette smoking and alcohol drinking with stomach cancer survival: A prospective patient cohort study in Japan. Int. J. Cancer 2018, 143, 1072–1085. [Google Scholar] [CrossRef]
- Kwan, M.L.; Valice, E.; Ergas, I.J.; Roh, J.M.; Caan, B.J.; Cespedes Feliciano, E.M.; Kolevska, T.; Hartman, T.J.; Quesenberry, C.P., Jr.; Ambrosone, C.B. Alcohol consumption and prognosis and survival in breast cancer survivors: The Pathways Study. Cancer 2023, 129, 3938–3951. [Google Scholar] [CrossRef]
- Farris, M.S.; Courneya, K.S.; Kopciuk, K.A.; McGregor, S.E.; Friedenreich, C.M. Post-diagnosis alcohol intake and prostate cancer survival: A population-based cohort study. Int. J. Cancer 2018, 143, 253–262. [Google Scholar] [CrossRef]
- Kline, R.M.; Arora, N.K.; Bradley, C.J.; Brauer, E.R.; Graves, D.L.; Lunsford, N.B.; McCabe, M.S.; Nasso, S.F.; Nekhlyudov, L.; Rowland, J.H. Long-term survivorship care after cancer treatment-summary of a 2017 National Cancer Policy Forum Workshop. JNCI J. Natl. Cancer Inst. 2018, 110, 1300–1310. [Google Scholar] [CrossRef] [PubMed]
- Firkins, J.; Hansen, L.; Driessnack, M.; Dieckmann, N. Quality of life in “chronic” cancer survivors: A meta-analysis. J. Cancer Surviv. 2020, 14, 504–517. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Shin, A.; Song, D.; Park, J.K.; Kim, Y.; Choi, J.-Y.; Kang, D.; Lee, J.-K. Validity of self-reported cancer history in the health examinees (HEXA) study: A comparison of self-report and cancer registry records. Cancer Epidemiol. 2017, 50, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Panagiota Mitrou, K.O.-T.; Wiseman, M. Cancer Prevention Recommendations. Available online: https://www.wcrf.org/diet-activity-and-cancer/cancer-prevention-recommendations/ (accessed on 8 April 2024).
| WCRF/AICR Adherence (Score, n) | ||||
|---|---|---|---|---|
| Lowest Adherence (≤3.75, n = 1478) | Middle Adherence (3.75–≤4.75, n = 2061) | Highest Adherence (>4.75, n = 1946) | p Value 1 | |
| N (%) | N (%) | N (%) | ||
| Sex | ||||
| Men | 453 (30.6) | 552 (26.8) | 474 (24.4) | <0.001 |
| Women | 1025 (69.4) | 1509 (73.2) | 1472 (75.6) | |
| Age | ||||
| <50 | 375 (25.4) | 407 (19.7) | 305 (15.7) | <0.001 |
| 50–59 | 582 (39.4) | 794 (38.5) | 854 (43.9) | |
| 60–69 | 443 (30.0) | 740 (35.9) | 668 (34.3) | |
| ≥70 | 78 (5.3) | 120 (5.8) | 119 (6.1) | |
| Education level 2 | ||||
| ≤Elementary school | 232 (15.7) | 352 (17.1) | 319 (16.4) | 0.01 |
| Middle school | 219 (14.8) | 370 (18.0) | 375 (19.3) | |
| ≥High school | 1012 (68.5) | 1326 (64.3) | 1239 (63.7) | |
| Missing | 15 (1.0) | 13 (0.6) | 13 (0.7) | |
| Income level (104 Korean won) | ||||
| Low (<150) | 286 (19.4) | 452 (21.9) | 433 (22.3) | 0.05 |
| Lower-middle (150–<300) | 485 (32.8) | 667 (32.4) | 576 (29.6) | |
| Upper-middle (300–<400) | 253 (17.1) | 323 (15.7) | 339 (17.4) | |
| High (≥400) | 322 (21.8) | 438 (21.3) | 387 (19.9) | |
| Not measured | 20 (1.4) | 40 (1.9) | 40 (2.1) | |
| Missing | 112 (7.6) | 141 (6.8) | 171 (8.8) | |
| Smoking status | ||||
| Non-smokers | 1077 (72.9) | 1589 (77.1) | 1582 (81.3) | <0.001 |
| Former smokers | 266 (18.0) | 376 (18.2) | 311 (16.0) | |
| Current smokers | 132 (8.9) | 93 (4.5) | 49 (2.5) | |
| Missing | 3 (0.2) | 3 (0.1) | 4 (0.2) | |
| Years post diagnosis 3 | ||||
| <5 | 878 (59.4) | 1213 (58.9) | 1189 (61.1) | 0.33 |
| ≥5 | 600 (40.6) | 848 (41.1) | 757 (38.9) | |
| Cancer type | ||||
| Stomach | 193 (13.1) | 300 (14.6) | 298 (15.3) | <0.001 |
| Liver | 24 (1.6) | 51 (2.5) | 38 (2.0) | |
| Colorectum | 112 (7.6) | 141 (6.8) | 159 (8.2) | |
| Breast | 172 (11.6) | 316 (15.3) | 411 (21.1) | |
| Cervix | 167 (11.3) | 190 (9.2) | 146 (7.5) | |
| Lung | 28 (1.9) | 49 (2.4) | 62 (3.2) | |
| Thyroid | 376 (25.4) | 477 (23.1) | 394 (20.2) | |
| Prostate | 43 (2.9) | 62 (3.0) | 39 (2.0) | |
| Bladder | 23 (1.6) | 28 (1.4) | 26 (1.3) | |
| Others | 309 (20.9) | 416 (20.2) | 347 (17.8) | |
| Missing | 31 (2.1) | 31 (1.5) | 26 (1.3) | |
| Disease history of diabetes | ||||
| Yes | 106 (7.2) | 141 (6.8) | 162 (8.3) | 0.13 |
| No | 1372 (92.8) | 1920 (93.2) | 1782 (91.6) | |
| Missing | 0 (0.0) | 0 (0.0) | 2 (0.1) | |
| Total energy intake 4 | ||||
| Lowest intake (tertile 1) | 373 (25.2) | 752 (36.5) | 701 (36.0) | <0.001 |
| Middle intake (tertile 2) | 474 (32.1) | 675 (32.8) | 685 (35.2) | |
| Highest intake (tertile 3) | 631 (42.7) | 634 (30.8) | 560 (28.8) | |
| Men (n = 1479) | Women (n = 4006) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| WCRF/AICR Adherence (Score) | N/No. Deaths | Person-Years | HR (95% CI) | aHR 1 (95% CI) | p Trend | N/No. Deaths | Person-Years | HR 1 (95% CI) | aHR 2 (95% CI) | p Trend |
| Lowest adherent (≤3.75) | 453/77 | 4302.5 | Ref. | Ref. | 0.68 | 1025/46 | 10,701.6 | Ref. | Ref. | 0.29 |
| Middle adherent (3.75–≤4.75) | 552/87 | 5202.0 | 0.86 (0.63–1.17) | 0.88 (0.65–1.21) | 1509/73 | 15,627.1 | 1.00 (0.69–1.44) | 1.01 (0.70–1.47) | ||
| Highest adherent (>4.75) | 474/78 | 4526.0 | 0.85 (0.62–1.17) | 0.93 (0.68–1.29) | 1472/82 | 15,173.4 | 1.17 (0.81–1.68) | 1.20 (0.83–1.73) | ||
| Years Post Diagnosis < 5 (n = 3280) | Years Post Diagnosis ≥ 5 (n = 2205) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| WCRF/AICR Adherence (Score) | N/No. Deaths | Person-Years | HR 1 (95% CI) | aHR 2 (95% CI) | p Trend | N/No. Deaths | Person-Years | HR 1 (95% CI) | aHR 2 (95% CI) | p Trend |
| Lowest adherent (≤3.75) | 878/73 | 8566.3 | Ref. | Ref. | 0.08 | 600/50 | 6437.9 | Ref. | Ref. | 0.05 |
| Middle adherent (3.75–≤4.75) | 1213/98 | 11,544.2 | 0.96 (0.71–1.30) | 1.06 (0.78–1.43) | 848/62 | 9285.0 | 0.69 (0.48–1.01) | 0.74 (0.51–1.08) | ||
| Highest adherent (>4.75) | 1189/116 | 11,474.6 | 1.13 (0.84–1.52) | 1.29 (0.96–1.74) | 757/44 | 8224.8 | 0.58 (0.38–0.86) | 0.66 (0.43–0.99) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Won, D.; Lee, J.; Cho, S.; Baek, J.Y.; Kang, D.; Shin, A. Adherence to the Cancer Prevention Recommendations from World Cancer Research Fund/American Institute for Cancer Research After Cancer Diagnosis on Mortality in South Korea. Nutrients 2024, 16, 4049. https://doi.org/10.3390/nu16234049
Won D, Lee J, Cho S, Baek JY, Kang D, Shin A. Adherence to the Cancer Prevention Recommendations from World Cancer Research Fund/American Institute for Cancer Research After Cancer Diagnosis on Mortality in South Korea. Nutrients. 2024; 16(23):4049. https://doi.org/10.3390/nu16234049
Chicago/Turabian StyleWon, Donghyun, Jeeyoo Lee, Sooyoung Cho, Ji Yoon Baek, Daehee Kang, and Aesun Shin. 2024. "Adherence to the Cancer Prevention Recommendations from World Cancer Research Fund/American Institute for Cancer Research After Cancer Diagnosis on Mortality in South Korea" Nutrients 16, no. 23: 4049. https://doi.org/10.3390/nu16234049
APA StyleWon, D., Lee, J., Cho, S., Baek, J. Y., Kang, D., & Shin, A. (2024). Adherence to the Cancer Prevention Recommendations from World Cancer Research Fund/American Institute for Cancer Research After Cancer Diagnosis on Mortality in South Korea. Nutrients, 16(23), 4049. https://doi.org/10.3390/nu16234049







