Changes in Food Waste among a Sample of U.S. Consumers after Beginning Anti-Obesity Medication
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Sample Characteristics
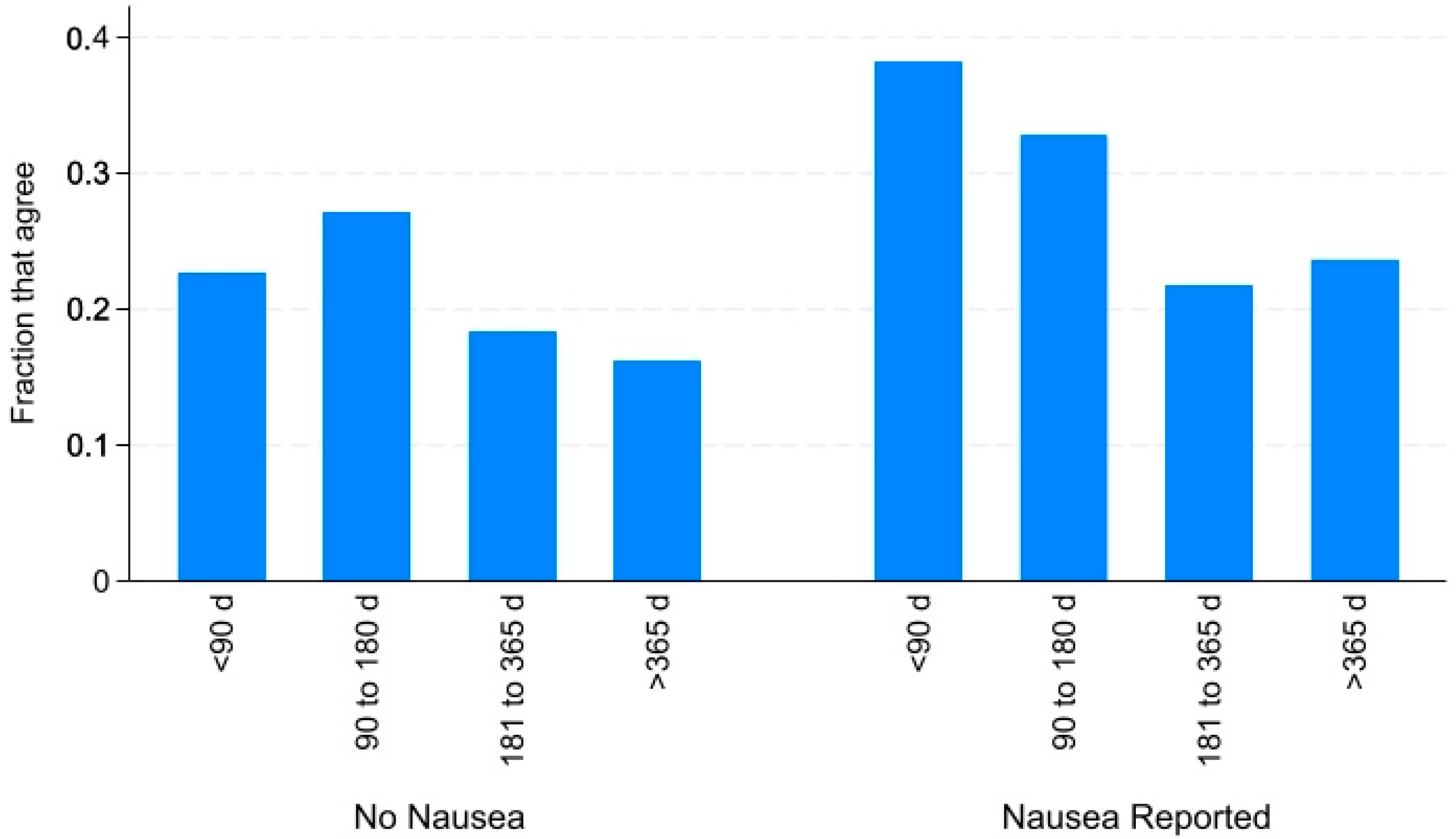
3.2. Changes in Food Waste after GLP1A Uptake
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aldawsari, M.; Almadani, F.A.; Almuhammadi, N.; Algabsani, S.; Alamro, Y.; Aldhwayan, M. The efficacy of GLP-1 analogues on appetite parameters, gastric emptying, food preference and taste among adults with obesity: Systematic review of randomized controlled trials. Diabetes Metab. Syndr. Obes. 2023, 16, 575–595. [Google Scholar] [CrossRef] [PubMed]
- Eren-Yazicioglu, C.Y.; Yigit, A.; Dogruoz, R.E.; Yapici-Eser, H. Can GLP-1 be a target for reward system related disorders? A qualitative synthesis and systematic review analysis of studies on palatable food, drugs of abuse, and alcohol. Front. Behav. Neurosci. 2021, 14, 614884. [Google Scholar] [CrossRef] [PubMed]
- Couzin-Frankel, J. Obesity meets its match. Science 2023, 382, 1226–1227. [Google Scholar] [CrossRef] [PubMed]
- Lafferty, R.A.; Flatt, P.R.; Irwin, N. GLP-1/GIP analogs: Potential impact in the landscape of obesity pharmacotherapy. Expert Opin. Pharmacother. 2023, 24, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Montero, A.; Sparks, G.; Presiado, M.; Hamel, L. KFF Health Tracking Poll May 2024: The Public’s Use and Views of GLP-1 Drugs. 10 May 2024. Available online: https://www.kff.org/health-costs/poll-finding/kff-health-tracking-poll-may-2024-the-publics-use-and-views-of-glp-1-drugs/ (accessed on 25 August 2024).
- National Academies of Sciences, Engineering, and Medicine. A National Strategy to Reduce Wasted Food at the Consumer Level; The National Academies Press: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Babbitt, C.W.; Neff, R.A.; Roe, B.E.; Siddiqui, S.; Chavis, C.; Trabold, T.A. Transforming wasted food will require systemic and sustainable infrastructure innovations. Curr. Opin. Environ. Sustain. 2022, 54, 101151. [Google Scholar] [CrossRef]
- Yu, Y.; Jaenicke, E.C. Estimating food waste as household production inefficiency. Am. J. Agric. Econ. 2020, 102, 525–547. [Google Scholar] [CrossRef]
- Schanes, K.; Dobernig, K.; Gözet, B. Food waste matters—A systematic review of household food waste practices and their policy implications. J. Clean. Prod. 2018, 182, 978–991. [Google Scholar] [CrossRef]
- Hebrok, M.; Boks, C. Household food waste: Drivers and potential intervention points for design—An extensive review. J. Clean. Prod. 2017, 151, 380–392. [Google Scholar] [CrossRef]
- Friedrichsen, M.; Breitschaft, A.; Tadayon, S.; Wizert, A.; Skovgaard, D. The effect of semaglutide 2.4 mg once weekly on energy intake, appetite, control of eating, and gastric emptying in adults with obesity. Diabetes Obes. Metab. 2021, 23, 754–762. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Shu, Y.; Bender, K.E.; Roe, B.E. Household food waste trending upwards in the United States: Insights from a National Tracking Survey. J. Agric. Appl. Econ. Assoc. 2023, 2, 306–317. [Google Scholar] [CrossRef]
- Savelli, E.; Francioni, B.; Curina, I. Healthy lifestyle and food waste behavior. J. Consum. Mark. 2020, 37, 148–159. [Google Scholar] [CrossRef]
- Conrad, Z.; Niles, M.T.; Neher, D.A.; Roy, E.D.; Tichenor, N.E.; Jahns, L. Relationship between food waste, diet quality, and environmental sustainability. PLoS ONE 2018, 13, e0195405. [Google Scholar] [CrossRef]
- Scharadin, B.; Yu, Y.; Jaenicke, E.C. Household time activities, food waste, and diet quality: The impact of non-marginal changes due to COVID-19. Rev. Econ. Househ. 2021, 19, 399–428. [Google Scholar] [CrossRef] [PubMed]
- Vittuari, M.; Herrero, L.G.; Masotti, M.; Iori, E.; Caldeira, C.; Qian, Z.; Bruns, H.; van Herpen, E.; Obersteiner, G.; Kaptan, G.; et al. How to reduce consumer food waste at household level: A literature review on drivers and levers for behavioural change. Sustain. Prod. Consum. 2023, 38, 104–114. [Google Scholar] [CrossRef]
- Van der Werf, P.; Seabrook, J.A.; Gilliland, J.A. The quantity of food waste in the garbage stream of southern Ontario, Canada households. PLoS ONE 2018, 13, e0198470. [Google Scholar] [CrossRef] [PubMed]
- Aitken, J.; Alaybek, B.; Hartman, H.; Leets, L.; Mika, G.; Rao, D.; Sprenger, A.; Viani, D.; Archer, K.; Davoodi, T.; et al. The State of Food Waste in America. 2023. Available online: https://sites.mitre.org/household-food-waste/ (accessed on 19 September 2024).
- Adelodun, B.; Kim, S.H.; Choi, K.S. Assessment of food waste generation and composition among Korean households using novel sampling and statistical approaches. Waste Manag. 2021, 122, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Hallström, E.; Gee, Q.; Scarborough, P.; Cleveland, D.A. A healthier US diet could reduce greenhouse gas emissions from both the food and health care systems. Clim. Chang. 2017, 142, 199–212. [Google Scholar] [CrossRef]
- Talay, L.; Vickers, M. Patient adherence to a real-world digital, asynchronous weight loss program in Australia that combines behavioural and GLP-1 RA therapy: A mixed methods study. Behav. Sci. 2024, 14, 480. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean or % |
|---|---|
| More waste since beginning medication | |
| Strongly disagree | 26.7 |
| Somewhat disagree | 34.1 |
| Neither agree nor disagree | 13.9 |
| Somewhat agree | 18.6 |
| Strongly agree | 6.7 |
| Side effects | |
| Abdominal pain | 28.7 |
| Constipation | 32.3 |
| Low blood sugar | 10.5 |
| Nausea | 49.3 |
| Diarrhea | 25.1 |
| Injection site redness | 15.0 |
| Vomiting | 16.0 |
| Other | 11.7 |
| Change in consumption since beginning AOM * | |
| Carbohydrates | −0.49 |
| Protein | 0.49 |
| Alcohol | −0.63 |
| Healthy fats | 0.25 |
| Fried foods | −0.64 |
| Savory foods | −0.17 |
| Sweets | −0.49 |
| Fruit | 0.43 |
| Vegetables | 0.55 |
| Dairy | −0.22 |
| Fish | 0.17 |
| Meat | 0.00 |
| Pasta and rice | −0.41 |
| Started diet since beginning medication | |
| Paleo | 0.10 |
| Atkins | 0.11 |
| Dukan | 0.07 |
| Intermittent fasting | 0.25 |
| Vegetarian | 0.12 |
| Vegan | 0.11 |
| Pescatarian | 0.11 |
| Mediterranean | 0.12 |
| Kosher | 0.08 |
| Halal | 0.07 |
| Low fat | 0.26 |
| Other | 0.07 |
| Type of medication | |
| Liraglutide | 4.1 |
| Semaglutide | 68.5 |
| Tirzepatide | 22.4 |
| Other/not sure | 5.0 |
| Out of pocket medication cost ($/month) | 175.40 |
| Days since beginning medication | |
| <90 | 29.9 |
| 90–180 | 22.6 |
| 181–365 | 21.0 |
| 365+ | 26.5 |
| Age | |
| 18–24 | 5.8 |
| 25–34 | 25.6 |
| 35–44 | 26.8 |
| 45–54 | 28.8 |
| 55–64 | 9.2 |
| 65+ | 3.8 |
| Household income (annual) | |
| <$50,000 | 20.4 |
| $50,000–$99,999 | 35.4 |
| $100,000+ | 44.2 |
| Education | |
| Less than bachelor’s degree | 26.5 |
| Bachelor’s degree | 45.5 |
| Beyond bachelor’s degree | 27.9 |
| Racial self-identification | |
| White/Caucasian | 63.8 |
| Black/African American | 25.3 |
| All other identifications | 10.9 |
| Employed full time | 76.8 |
| Has medical insurance | 89.1 |
| Identify as male | 43.4 |
| Identify as Hispanic or Latina/o | 9.3 |
| Variable | Coefficient | Robust Standard Error | p-Value |
|---|---|---|---|
| Side effects | |||
| Abdominal pain | 0.20 | 0.14 | 0.15 |
| Constipation | −0.05 | 0.12 | 0.68 |
| Low blood sugar | 0.24 | 0.19 | 0.21 |
| Nausea | 0.26 | 0.12 | 0.02 * |
| Diarrhea | 0.04 | 0.14 | 0.78 |
| Injection site redness | −0.05 | 0.15 | 0.76 |
| Vomiting | 0.19 | 0.18 | 0.30 |
| Other | 0.15 | 0.19 | 0.43 |
| Food consumption since beginning AOM | |||
| Carbohydrates | 0.06 | 0.11 | 0.62 |
| Protein | 0.06 | 0.11 | 0.60 |
| Alcohol | 0.18 | 0.12 | 0.12 |
| Healthy fats | −0.12 | 0.11 | 0.26 |
| Fried foods | 0.16 | 0.13 | 0.22 |
| Savory foods | −0.10 | 0.10 | 0.32 |
| Sweets | 0.14 | 0.12 | 0.25 |
| Fruit | −0.05 | 0.11 | 0.63 |
| Vegetables | −0.27 | 0.13 | 0.04 * |
| Dairy | 0.03 | 0.10 | 0.73 |
| Fish | −0.05 | 0.11 | 0.63 |
| Meat | 0.07 | 0.10 | 0.49 |
| Pasta | −0.14 | 0.11 | 0.23 |
| Started diet since beginning medication | |||
| Paleo | 0.04 | 0.37 | 0.91 |
| Atkins | 0.12 | 0.22 | 0.59 |
| Dukan | 0.42 | 0.28 | 0.14 |
| Intermittent fasting | −0.13 | 0.15 | 0.40 |
| Vegetarian | 0.22 | 0.23 | 0.34 |
| Vegan | −0.46 | 0.24 | 0.06 |
| Pescatarian | −0.20 | 0.23 | 0.37 |
| Mediterranean | 0.07 | 0.18 | 0.69 |
| Kosher | 0.01 | 0.26 | 0.98 |
| Halal | −0.00 | 0.32 | 0.99 |
| Low fat | 0.10 | 0.15 | 0.49 |
| Other | −0.02 | 0.26 | 0.95 |
| Type of medication | |||
| Liraglutide (omitted category) | - | - | - |
| Semaglutide | 0.10 | 0.31 | 0.74 |
| Tirzepatide | 0.21 | 0.33 | 0.52 |
| Other/not sure | 0.24 | 0.38 | 0.54 |
| Days since beginning medication | |||
| <90 (omitted category) | - | - | - |
| 90–180 | −0.13 | 0.16 | 0.41 |
| 181–365 | −0.22 | 0.16 | 0.16 |
| 365+ | −0.35 | 0.15 | 0.03 * |
| Age | |||
| 18–24 (omitted category) | - | - | - |
| 25–34 | 0.19 | 0.28 | 0.49 |
| 35–44 | −0.00 | 0.29 | 0.99 |
| 45–54 | 0.15 | 0.29 | 0.62 |
| 55–64 | −0.17 | 0.33 | 0.61 |
| 65+ | 0.06 | 0.39 | 0.89 |
| Household income (annual) | |||
| <$50,000 (omitted category) | - | - | - |
| $50,000–$99,999 | 0.15 | 0.16 | 0.35 |
| $100,000+ | 0.07 | 0.16 | 0.64 |
| Education | |||
| Less than bachelor’s degree (omitted) | - | - | - |
| Bachelor’s degree | −0.38 | 0.15 | 0.02 * |
| Beyond bachelor’s degree | 0.20 | 0.18 | 0.26 |
| Racial self-identification | |||
| White/Caucasian | 0.08 | 0.19 | 0.66 |
| Black/African American | 0.30 | 0.23 | 0.19 |
| All other identifications (omitted) | - | - | - |
| Employed full time | −0.00 | 0.15 | 0.98 |
| Has medical insurance | −0.05 | 0.18 | 0.79 |
| Identify as male | 0.07 | 0.13 | 0.59 |
| Identify as Hispanic or Latina/o | −0.24 | 0.18 | 0.19 |
| R2 | 0.15 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mansouri, J.; Roe, B.E. Changes in Food Waste among a Sample of U.S. Consumers after Beginning Anti-Obesity Medication. Nutrients 2024, 16, 3274. https://doi.org/10.3390/nu16193274
Mansouri J, Roe BE. Changes in Food Waste among a Sample of U.S. Consumers after Beginning Anti-Obesity Medication. Nutrients. 2024; 16(19):3274. https://doi.org/10.3390/nu16193274
Chicago/Turabian StyleMansouri, Jamil, and Brian E. Roe. 2024. "Changes in Food Waste among a Sample of U.S. Consumers after Beginning Anti-Obesity Medication" Nutrients 16, no. 19: 3274. https://doi.org/10.3390/nu16193274
APA StyleMansouri, J., & Roe, B. E. (2024). Changes in Food Waste among a Sample of U.S. Consumers after Beginning Anti-Obesity Medication. Nutrients, 16(19), 3274. https://doi.org/10.3390/nu16193274






