Characterizing and Predicting Outcomes in Critically Ill Patients Receiving Low or High Protein Doses with Moderate Energy Support: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
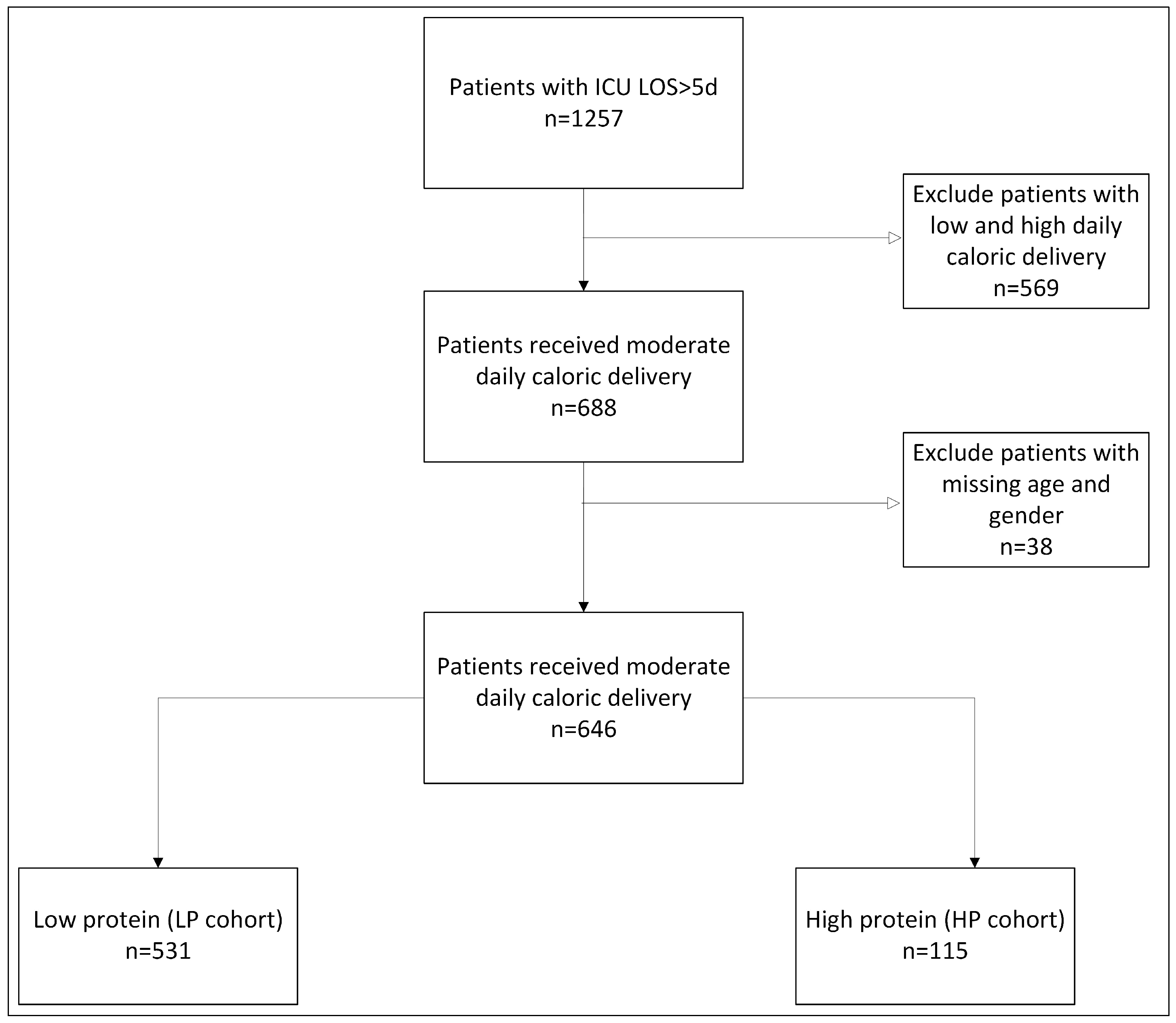
2.2. Study Design and Participants
2.3. Patient Demographic and Clinical Characteristics
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics of LP and HP Cohorts
3.2. Comparing Survivors and Non-Survivors in LP and HP Cohorts
3.3. Sensitivity Analysis
3.3.1. Renal Patients
3.3.2. Elderly Patients in the HP Cohort
4. Discussion
Limitations and Advantages
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bels, J.L.M.; Abdelhamid, A.Y.; van de Poll, M.C.G. Protein supplementation in critical illness: Why, when and how? Curr. Opin. Clin. Nutr. Metab. Care 2023, 26, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Wischmeyer, P.E. Tailoring nutrition therapy to illness and recovery. Crit. Care 2017, 21, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Weijs, P.J.; Stapel, S.N.; de Groot, S.D.; Driessen, R.H.; de Jong, E.; Girbes, A.R.; Strack van Schijndel, R.J.; Beishuizen, A. Optimal protein and energy nutrition decrease mortality in mechanically ventilated, critically ill patients: A prospective observational cohort study. JPEN J. Parenter. Enter. Nutr. 2012, 36, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Allingstrup, M.J.; Esmailzadeh, N.; Wilkens Knudsen, A.; Espersen, K.; Hartvig Jensen, T.; Wiis, J.; Perner, A.; Kondrup, J. Provision of protein and energy in relation to measured requirements in intensive care patients. Clin. Nutr. 2012, 31, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Zusman, O.; Theilla, M.; Cohen, J.; Kagan, I.; Bendavid, I.; Singer, P. Resting energy expenditure, calorie and protein consumption in critically ill patients: A retrospective cohort study. Crit. Care 2016, 20, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Compher, C.; Chittams, J.; Sammarco, T.; Nicolo, M.; Heyland, D.K. Greater protein and energy intake may be associated with improved mortality in higher risk critically ill patients: A patient multicenter, multinational observational study. Crit. Care Med. 2017, 45, 156–163. [Google Scholar] [CrossRef]
- Looijaard, W.G.; Dekker, I.M.; Stapel, S.N.; Girbes, A.R.; Twisk, J.W.; Oudemans-van Straaten, H.M.; Weijs, P.J. muscle quality, as assessed by CT-derived muscle density, is associated with a 6-month mortality in mechanically ventilated patients. Crit. Care 2016, 20, 386–394. [Google Scholar] [CrossRef]
- Umbrello, M.; Sterchele, E.D.; Cioata, A.C.; Mistraletti, G.; Formenti, P. The effect of protein administration during critical illness depends on body composition: A secondary analysis of a prospective, observational study. Clin. Nutr. 2024, 43, 1993–1996. [Google Scholar] [CrossRef]
- Fusco, A.; Galluccio, C.; Castelli, L.; Pazzaglia, C.; Pastorino, R.; Pires Marafon, D.; Bernabei, R.; Giovannini, S.; Padua, L. Severe Acquired Brain Injury: Prognostic Factors of Discharge Outcome in Older Adults. Brain Sci. 2022, 12, 1232. [Google Scholar] [CrossRef]
- Giovannini, S.; Iacovelli, C.; Loreti, C.; Lama, E.; Morciano, N.; Frisullo, G.; Biscotti, L.; Padua, L.; Castelli, L. The role of nutritional supplement on post-stroke fatigue: A pilot randomized controlled trial. J. Nutr. Health Aging 2024, 28, 100256. [Google Scholar] [CrossRef]
- Allingstrup, M.J.; Kondrup, J.; Wiis, J.; Claudius, C.; Pedersen, U.G.; Hein-Rasmussen, R.; Bjerregaard, M.R.; Steensen, M.; Jensen, T.H.; Lange, T.; et al. Early goal-directed nutrition versus standard of care in adult intensive care patients: The single-center, randomized, outcome assessor-blinded EAT-ICU trial. Intensive Care Med. 2017, 43, 1637–1647. [Google Scholar] [CrossRef] [PubMed]
- Heyland, D.K.; Patel, J.; Compher, C.; Rice, T.W.; Bear, D.E.; Lee, Z.Y.; González, V.C.; O’Reilly, K.; Regala, R.; Wedemire, C.; et al. The effect of higher protein dosing in critically ill patients with high nutritional risk (EFFORT Protein): An international, multicentre, pragmatic, registry-based randomized trial. Lancet 2023, 401, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Huang, J.; Ping, X.; Zheng, H.; Zhang, K.; Xu, X.; Yu, J. No benefit of higher protein dosing in critically ill patients: A systematic review and meta-analysis of randomized controlled trials. PeerJ 2024, 12, e17433. [Google Scholar] [CrossRef] [PubMed]
- Lee, Z.Y.; Yap, C.S.L.; Hasan, M.S.; Engkasan, J.P.; Barakatun-Nisak, M.Y.; Day, A.G.; Patel, J.J.; Heyland, D.K. The effect of higher versus lower protein delivery in critically ill patients: A systematic review and meta-analysis of randomized controlled trials. Crit. Care 2021, 25, 260–269. [Google Scholar] [CrossRef]
- Hartl, W.H.; Kopper, P.; Bender, A.; Scheipl, F.; Day, A.G.; Elke, G.; Küchenhoff, H. Protein intake and outcome of critically ill patients: Analysis of a large international database using piece-wise exponential additive mixed models. Crit. Care 2022, 26, 7. [Google Scholar] [CrossRef]
- Pardo, E.; Lescot, T.; Preiser, J.C.; Massanet, P.; Pons, A.; Jaber, S.; Fraipont, V.; Levesque, E.; Ichai, C.; Petit, L.; et al. Association between early nutrition support and 28-day mortality in critically ill patients: The FRANS prospective nutrition cohort study. Crit. Care 2023, 27, 7. [Google Scholar] [CrossRef]
- Lin, J.; Chen, W.; Ye, X.; Lv, C.; Liu, Y.; Jiang, X.; Tong, Z.; Liu, Y.; Ke, L.; Li, W. Trajectories of protein intake and 28-day mortality in critically ill patients: A secondary analysis of a cluster-randomized controlled trial. Clin. Nutr. 2022, 41, 1644–1650. [Google Scholar] [CrossRef]
- Matejovic, M.; Huet, O.; Dams, K.; Elke, G.; Vaquerizo Alonso, C.; Csomos, A.; Krzych, Ł.J.; Tetamo, R.; Puthucheary, Z.; Rooyackers, O.; et al. Medical nutrition therapy and clinical outcomes in critically ill adults: A European multinational, prospective observational cohort study (EuroPN). Crit. Care 2022, 26, 143. [Google Scholar] [CrossRef]
- Weijs, P.J.; Looijaard, W.G.; Beishuizen, A.; Girbes, A.R.; Oudemans-van Straaten, H.M. Early high protein ntake is associated with low mortality and energy overfeeding with high mortality in non-septic mechanically ventilated critically ill patients. Crit. Care 2014, 18, 701. [Google Scholar] [CrossRef]
- Singer, P. Protein metabolism and requirements in the ICU. Clin. Nutr. ESPEN 2020, 38, 3–8. [Google Scholar] [CrossRef]
- Rahman, A.; Hasan, R.M.; Agarwala, R.; Martin, C.; Day, A.G.; Heyland, D.K. Identifying critically ill patients who will benefit most from nutritional therapy: Further validation of the “modified NUTRIC” nutritional risk assessment tool. Clin. Nutr. 2016, 35, 158–162. [Google Scholar] [CrossRef] [PubMed]
- APACHE II Score. Available online: https://www.mdcalc.com/calc/1868/apache-ii-score (accessed on 16 July 2024).
- Lee, Z.Y.; Loh, C.T.I.; Lew, C.C.H.; Ke, L.; Heyland, D.K.; Hasan, M.S. Nutrition therapy in the older critically ill patients: A scoping review. Ann. Acad. Med. Singap. 2022, 51, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Peng, M.; Ye, Z.; Ai, Y.; Liu, Z. The mode and timing of administrating nutritional treatment of critically ill elderly patients in intensive care units: A multicenter prospective study. Front. Med. 2024, 11, 1321599. [Google Scholar] [CrossRef]
- Hsu, P.H.; Lee, C.H.; Kuo, L.K.; Kung, Y.C.; Chen, W.G.; Tzeng, M.S. Higher Energy and Protein Intake from Enteral Nutrition May Reduce Hospital Mortality in Mechanically Ventilated Critically Ill Elderly Patients. Int. J. Gerontol. 2018, 12, 285–289. [Google Scholar] [CrossRef]
- Compher, C.; Chittams, J.; Sammarco, T.; Higashibeppu, N.; Higashiguchi, T.; Heyland, D.K. Greater Nutrient Intake Is Associated with Lower Mortality in Western and Eastern Critically Ill Patients With Low BMI: A Multicenter, Multinational Observational Study. J. Parenter. Enter. Nutr. 2019, 43, 63–69. [Google Scholar] [CrossRef]
- Pepper, D.J.; Sun, J.; Welsh, J.; Cui, X.; Suffredini, A.F.; Eichacker, P.Q. Increased body mass index and adjusted mortality in ICU patients with sepsis or septic shock: A systematic review and meta-analysis. Crit. Care 2016, 20, 181–189. [Google Scholar] [CrossRef]
- Tweel, L.E.; Compher, C.; Bear, D.E.; Gutierrez-Castrellon, P.; Leaver, S.K.; MacEachern, K.; Ortiz-Reyes, L.; Pooja, L.; León, A.; Wedemire, C.; et al. Comparison of High and Usual Protein Dosing in Critically Ill Patients With Obesity: A Post Hoc Analysis of an International, Pragmatic, Single-Blinded, Randomized, Clinical Trial. Crit. Care Med. 2023, 52, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Bendavid, I.; Singer, P.; Theilla, M.; Themessl-Huber, M.; Sulz, I.; Mouhieddine, M.; Schuh, C.; Mora, B.; Hiesmayr, M. NutritionDay ICU: A 7-year worldwide prevalence study of nutrition practice in intensive care. Clin. Nutr. 2017, 36, 1122–1129. [Google Scholar] [CrossRef]
- Vankrunkelsven, W.; Derde, S.; Gunst, J.; Vander Perre, S.; Declerck, E.; Pauwels, L.; Derese, I.; Van den Berghe, G.; Langouche, L. Obesity attenuates inflammation, protein catabolism, dyslipidaemia, and muscle weakness during sepsis, independent of leptin. J. Cachexia Sarcopenia Muscle 2022, 13, 418–433. [Google Scholar] [CrossRef]
- Deutz, N.E.; Ziegler, T.R.; Matheson, E.M.; Matarese, L.E.; Tappenden, K.A.; Baggs, G.E.; Nelson, J.L.; Luo, M.; Hegazi, R.; Jonnalagadda, S.S.; et al. Reduced mortality risk in malnourished hospitalized older adult patients with COPD treated with a specialized oral nutritional supplement: Sub-group analysis of the NOURISH study. Clin. Nutr. 2021, 40, 1388–1395. [Google Scholar] [CrossRef] [PubMed]
- Stoppe, C.; Patel, J.J.; Zarbock, A.; Lee, Z.Y.; Rice, T.W.; Mafrici, B.; Wehner, R.; Chan, M.H.M.; Lai, P.C.K.; MacEachern, K.; et al. The impact of higher protein dosing on outcomes in critically ill patients with acute kidney injury: A post hoc analysis of the EFFORT protein trial. Crit. Care 2023, 27, 399. [Google Scholar] [CrossRef]
- Dickerson, R.N.; Pitts, S.L.; Maish, G.O.; Schroeppel, T.J.; Magnotti, L.J.; Croce, M.A.; Minard, G.; Brown, R.O. A reappraisal of nitrogen requirements for patients with critical illness and trauma. J. Trauma Acute Care Surg. 2012, 73, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Li, P.F.; Wang, Y.L.; Fang, Y.L.; Nan, L.; Zhou, J.; Zhang, D. Effect of early enteral nutrition on outcomes of trauma patients requiring intensive care. Chin. J. Traumatol. 2020, 23, 163–167. [Google Scholar] [CrossRef]
- Hartwell, J.L.; Cotton, A.; Wenos, C.D.; Timsina, L.; Zarzaur, B.L.; Rozycki, G. Early Achievement of Enteral Nutrition Protein Goals by Intensive Care Unit Day 4 is Associated With Fewer Complications in Critically Injured Adults. Ann. Surg. 2021, 274, e988–e994. [Google Scholar] [CrossRef]
- de Koning, M.L.Y.; Koekkoek, W.A.C.K.; Kars, J.C.N.H.; van Zanten, A.R.H. Association of PROtein and CAloric Intake and Clinical Outcomes in Adult SEPTic and Non-Septic ICU Patients on Prolonged Mechanical Ventilation: The PROCASEPT Retrospective Study. J. Parenter. Enter. Nutr. 2020, 44, 434–443. [Google Scholar] [CrossRef]
- Elke, G.; Wang, M.; Weiler, N.; Day, A.G.; Heyland, D.K. Close to recommended caloric and protein intake by enteral nutrition is associated with better clinical outcomes of critically ill septic patients: Secondary analysis of a large international nutrition database. Crit. Care 2014, 18, R29. [Google Scholar] [CrossRef] [PubMed]
- Arunachala Murthy, T.; Chapple, L.S.; Lange, K.; Marathe, C.S.; Horowitz, M.; Peake, S.L.; Chapman, M.J. Gastrointestinal dysfunction during enteral nutrition delivery in intensive care unit (ICU) patients: Risk factors, natural history, and clinical implications. A post-hoc analysis of The Augmented versus Routine approach to Giving Energy Trial (TARGET). Am. J. Clin. Nutr. 2022, 116, 589–598. [Google Scholar] [CrossRef]
- Heyland, D.K.; Ortiz, A.; Stoppe, C.; Patel, J.J.; Yeh, D.D.; Dukes, G.; Chen, Y.J.; Almansa, C.; Day, A.G. Incidence, Risk Factors, and Clinical Consequence of Enteral Feeding Intolerance in the Mechanically Ventilated Critically Ill: An Analysis of a Multicenter, Multiyear Database. Crit. Care Med. 2021, 49, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Bels, J.L.M.; Thiessen, S.; van Gassel, R.J.J.; Beishuizen, A.; De Bie Dekker, A.; Fraipont, V.; Lamote, S.; Ledoux, D.; Scheeren, C.; De Waele, E.; et al. PRECISe study team. Effect of high versus standard protein provision on functional recovery in people with critical illness (PRECISe): An investigator-initiated, double-blinded, multicentre, parallel-group, randomised controlled trial in Belgium and the Netherlands. Lancet 2024, 17, 659–669. [Google Scholar]
- Bear, D.E.; Summers, M.J.; Chapple, L.S. Dietary protein in the ICU in relation to health outcomes. Curr. Opin. Clin. Nutr. Metab. Care, 2024; ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Reignier, J.; Plantefeve, G.; Mira, J.P.; Argaud, L.; Asfar, P.; Aissaoui, N.; Badie, J.; Botoc, N.V.; Brisard, L.; Bui, H.N.; et al. NUTRIREA-3 Trial Investigators; Clinical Research in Intensive Care; Sepsis (CRICS-TRIGGERSEP) Group. Low versus standard calorie and protein feeding in ventilated adults with shock: A randomised, controlled, multicentre, open-label, parallel-group trial (NUTRIREA-3). Lancet Respir. Med. 2023, 11, 602–612. [Google Scholar]
- Raphaeli, O.; Statlender, L.; Kagan, I.; Hellerman-Itshaki, M.; Robinson, E.; Singer, P. Characterizing phenotypes of protein administration strategies among critically ill patients receiving moderate energy intake: A retrospective observational study. Clin. Nutr. ESPEN 2024, 63, 1037–1038. [Google Scholar] [CrossRef]
| Variable 1 | Overall Cohort (n = 646) | LP Cohort (n = 531) | HP Cohort (n = 115) |
|---|---|---|---|
| Age | 60.2 (±17.2) | 60.1(±17.3) | 60.6 (±16.9) |
| Gender Male | 453 (79.1%) | 374 (70.4%) | 79 (68.7%) |
| BMI (kg/m2) | 28.6 (±6.6) | 29.1 (±6.6) | 26.2 (±5.8) |
| Admission Type | |||
| Medical | 96 (14.9%) | 81 (15.3%) | 15 (13%) |
| Surgical | 289 (44.7%) | 246 (46.3%) | 43 (37.4%) |
| Transplantation | 36 (5.6%) | 29 (5.5%) | 7 (6.1%) |
| Trauma | 225 (34.8%) | 175 (33%) | 50 (43.5%) |
| APACHE II | 23.1 (±6.6) | 23.4 (±6.7) | 21.8 (±5.9) |
| Nutrition therapy | |||
| EN | 487 (75.4%) | 404 (76.1%) | 83 (72.2%) |
| EN and SPN | 148 (22.9%) | 116 (21.8%) | 32 (27.8%) |
| PN | 11 (1.7%) | 11 (2.1%) | - |
| Average protein (kg/d) | 0.78 (±0.39) | 0.68 (±0.15) | 1.3 (±0.67) |
| Cardiac | 345 (53.4%) | 283 (53.3%) | 62 (53.9%) |
| Metabolic | 335 (51.9%) | 276 (52.0%) | 59 (51.3%) |
| Neurologic | 180 (27.9%) | 144 (27.1%) | 36 (31.3%) |
| Oncology | 141 (21.8%) | 116 (21.8%) | 25 (21.7%) |
| Pulmonary | 232 (35.9%) | 179 (33.7%) | 53 (46.1%) * |
| Renal | 258 (39.9%) | 213 (40.1%) | 45 (39.1%) |
| Sepsis | 45 (7%) | 37 (7%) | 8 (7%) |
| 90-day survival | 375 (58%) | 307 (57.8%) | 68 (59.1%) |
| Variable 1 | LP Cohort (n = 531) | HP Cohort (n = 115) | ||
|---|---|---|---|---|
| 90-Day Survivors (n = 307) | Non- Survivors (n = 224) | 90-Day Survivors (n = 68) | Non- Survivors (n = 47) | |
| Age | 57.0 (±18.6) * | 64.3 (±14.3) | 56.6 (±18.2) * | 66.5 (±12.8) |
| Gender Male | 214 (69.7%) | 160 (71.4%) | 46 (67.6%) | 33 (70.2%) |
| BMI (kg/m2) | 28.9 (±6.1) | 29.5 (±7.3) | 27.2 (±6.2) * | 24.7 (±4.9) |
| Admission type | ||||
| Medical | 40 (13%) | 41 (18.3%) | 8 (11.8%) | 7 (14.9%) |
| Surgical | 137 (44.6%) | 109 (48.7%) | 23 (33.8%) | 20 (42.6%) |
| Transplantation | 12 (3.9%) | 17 (7.6%) | 2 (2.9%) | 5 (10.6%) |
| Trauma | 118 (38.4%) * | 57 (25.4%) | 35 (51.5%) * | 15 (31.9%) |
| APACHE II | 21.55 (±6.3) * | 25.9 (±6.5) | 21.1 (±6.0) | 23.0 (±5.6) |
| Nutrition therapy | ||||
| EN | 243 (79.2%) | 161 (71.9%) | 49 (72.1%) | 34 (72.3%) |
| EN+SPN | 57 (18.6%) | 59 (26.3%) | 19 (27.9%) | 13 (27.7%) |
| PN | 7 (2.3%) | 4 (1.8%) | - | - |
| Average protein (kg/d) | 0.68 (±0.2) | 0.67 (±0.2) | 1.2 (±0.3) | 1.4 (±0.9) |
| Cardiac | 139 (45.3%) * | 146 (64.3%) | 34 (50%) | 28 (59.6%) |
| Metabolic | 150 (48.9%) | 126 (56.3%) | 32 (47.1%) | 27 (57.4%) |
| Neurologic | 92 (30%) | 52 (23.2%) | 26 (38.2%) * | 10 (21.3%) |
| Oncology | 66 (21.5%) | 50 (23.2%) | 11 (16.2%) | 14 (29.8%) |
| Pulmonary | 97 (31.6%) | 82 (36.6%) | 30 (44.1%) | 23 (48.9%) |
| Renal | 103 (33.6%) * | 110 (49.1%) | 23 (33.8%) | 22 (46.8%) |
| Sepsis | 17 (5.5%) | 20 (8.9%) | 2 (2.9%) * | 6 (12.8%) |
| Cohort | Variable | Odds Ratio | 95% CI | p-Value |
|---|---|---|---|---|
| LP | age | 0.986 | [0.973, 0.999] | 0.04 |
| APACHE II score | 0.915 | [0.886, 0.944] | 0.001 | |
| EN + SPN route (reference category is EN) | 0.579 | [0.366, 0.917] | 0.02 | |
| Trauma admission type (reference category is medical) | 1.826 | [1.001, 3.329] | 0.05 | |
| HP | age | 0.956 | [0.924, 0.998] | 0.008 |
| BMI | 1.137 | [1.028, 1.258] | 0.013 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raphaeli, O.; Singer, P.; Robinson, E.; Statlender, L.; Kagan, I. Characterizing and Predicting Outcomes in Critically Ill Patients Receiving Low or High Protein Doses with Moderate Energy Support: A Retrospective Study. Nutrients 2024, 16, 3258. https://doi.org/10.3390/nu16193258
Raphaeli O, Singer P, Robinson E, Statlender L, Kagan I. Characterizing and Predicting Outcomes in Critically Ill Patients Receiving Low or High Protein Doses with Moderate Energy Support: A Retrospective Study. Nutrients. 2024; 16(19):3258. https://doi.org/10.3390/nu16193258
Chicago/Turabian StyleRaphaeli, Orit, Pierre Singer, Eyal Robinson, Liran Statlender, and Ilya Kagan. 2024. "Characterizing and Predicting Outcomes in Critically Ill Patients Receiving Low or High Protein Doses with Moderate Energy Support: A Retrospective Study" Nutrients 16, no. 19: 3258. https://doi.org/10.3390/nu16193258
APA StyleRaphaeli, O., Singer, P., Robinson, E., Statlender, L., & Kagan, I. (2024). Characterizing and Predicting Outcomes in Critically Ill Patients Receiving Low or High Protein Doses with Moderate Energy Support: A Retrospective Study. Nutrients, 16(19), 3258. https://doi.org/10.3390/nu16193258





