The Combination Effect of the Red Blood Cell Distribution Width and Prognostic Nutrition Index on the Prognosis in Patients Undergoing PCI
Abstract
1. Introduction
2. Materials and Methods
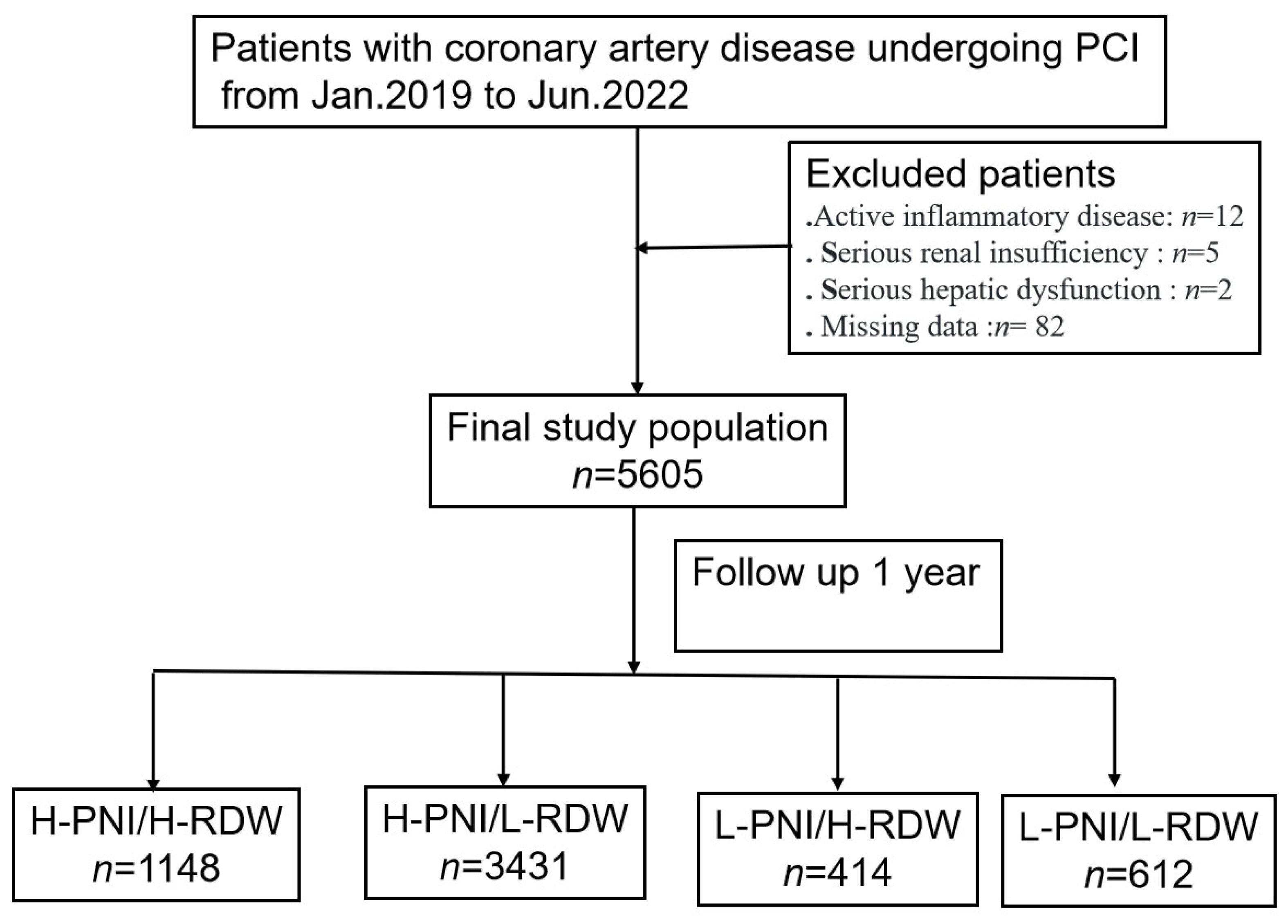
2.1. Study Patients and Design
2.2. Demographic and Clinical Data Collection
2.3. Endpoints and Follow-Up
3. Statistical Analysis
4. Results
4.1. Baseline Characteristics
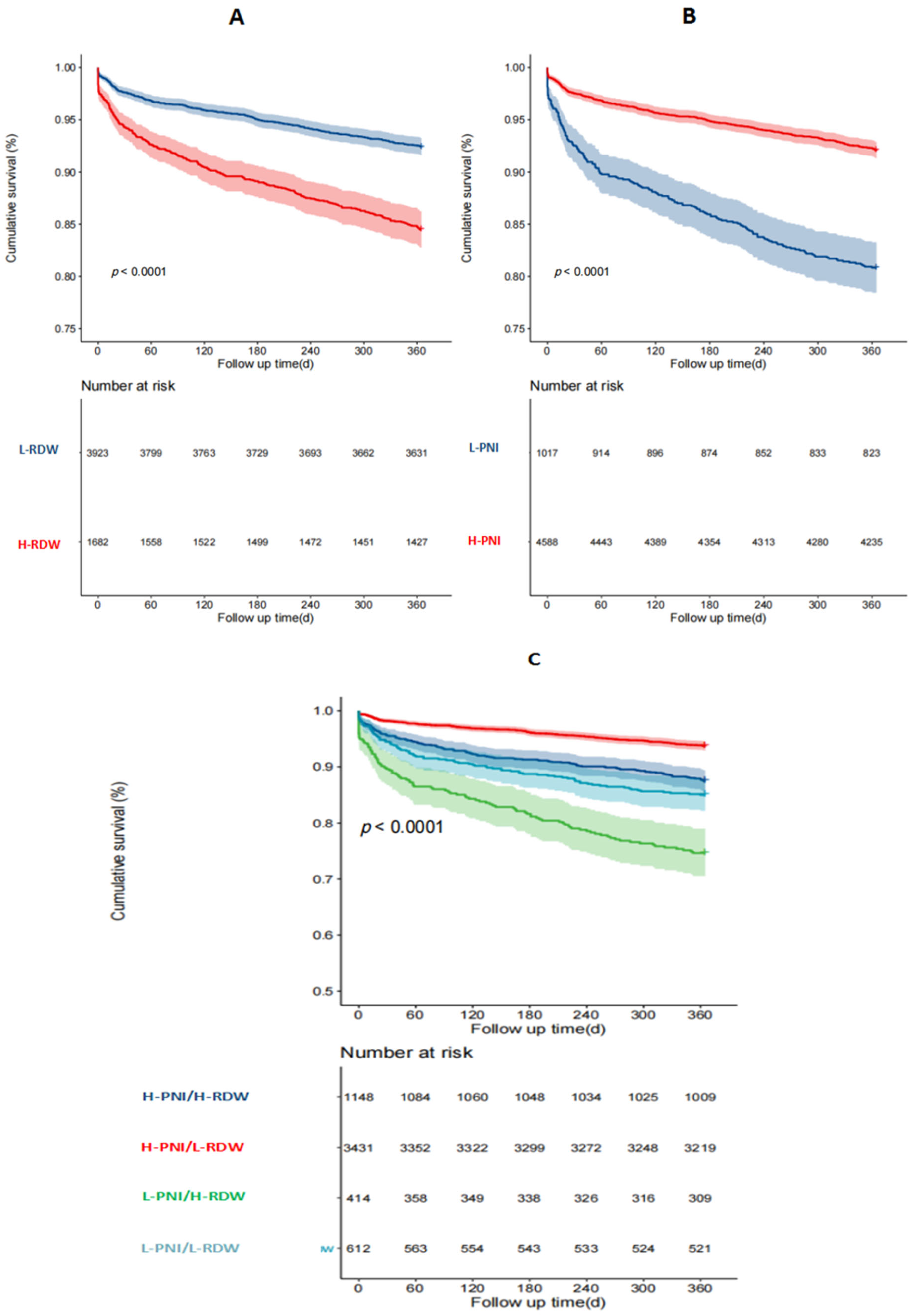
4.2. Relationship between PNI Combined with RDW and Clinical Outcomes
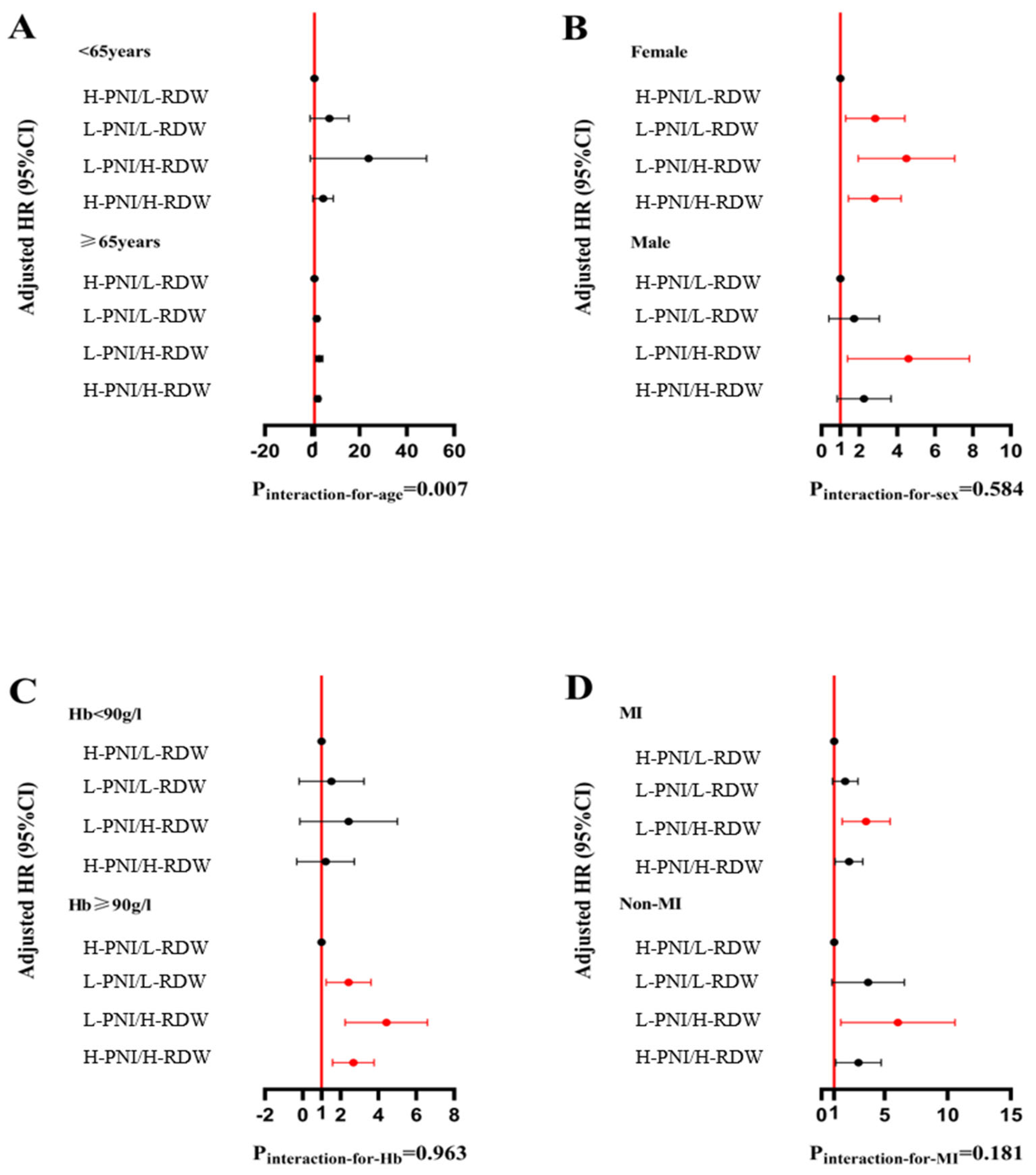
4.3. Subgroup Analysis
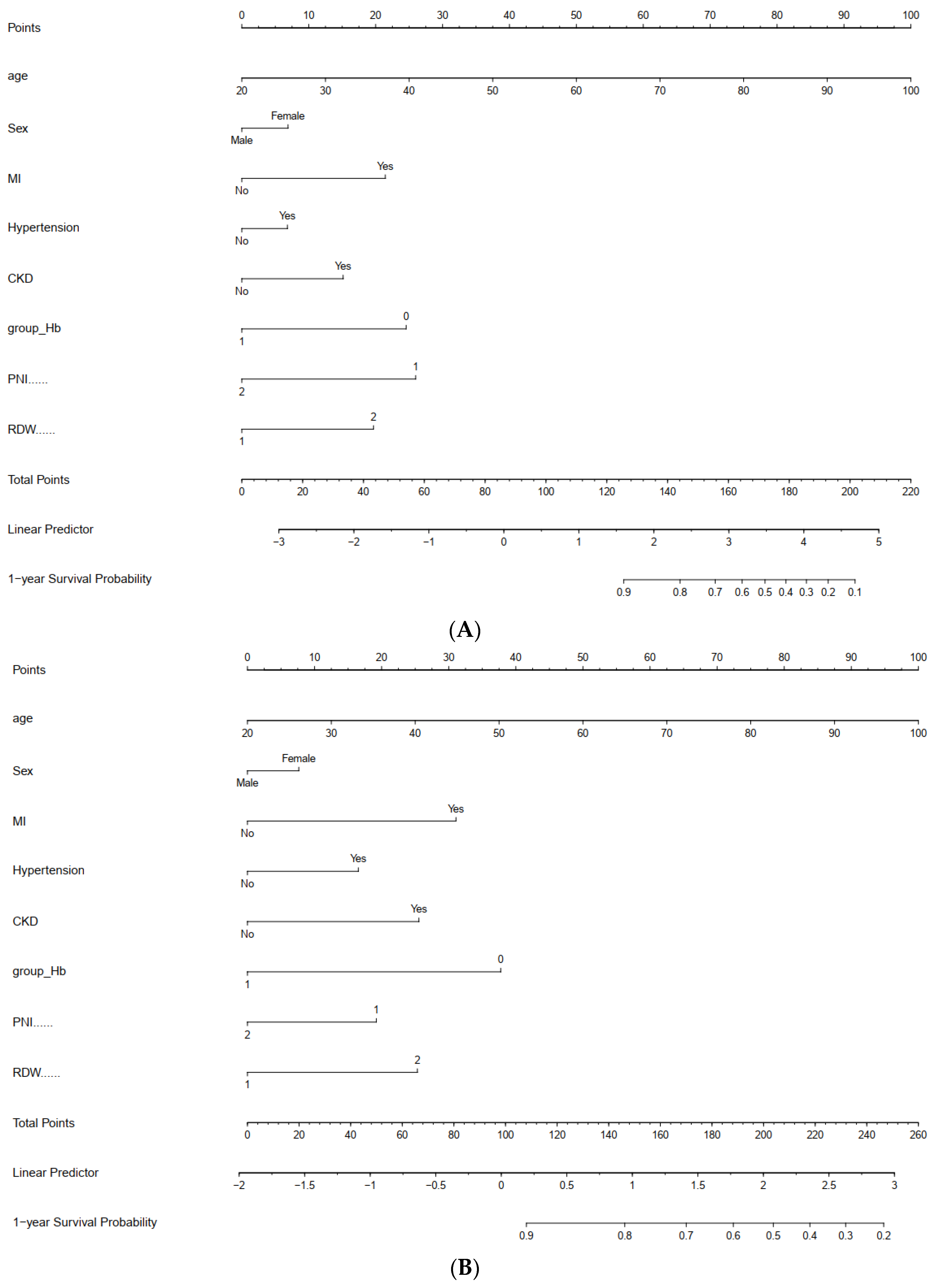
4.4. A Novel Nomogram for 1-Year Adverse Prognosis via PCI
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, H.; Liu, F.; Ma, H.; Yin, H.; Wang, P.; Bai, B.; Guo, L.; Geng, Q. Associations between depression, nutrition, and outcomes among individuals with coronary artery disease. Nutrition 2021, 86, 111157. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Song, H.N.; Moon, J.Y.; Kim, S.-H.; Sung, J.-H.; Kim, I.J.; Lim, S.-W.; Cha, D.-H.; Kim, W.-J. Prevalence and prognostic significance of malnutrition in patients with acute coronary syndrome treated with percutaneous coronary intervention. Medicine 2022, 101, e30100. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Wang, H.; Chen, S.; Cai, S.; Zhou, S.; Wang, C.; Ni, X. Prognostic nutritional index and prognosis of patients with coronary artery disease: A systematic review and meta-analysis. Front. Nutr. 2023, 10, 1114053. [Google Scholar] [CrossRef]
- Yıldırım, A.; Kucukosmanoglu, M.; Koyunsever, N.Y.; Cekici, Y.; Belibagli, M.C.; Kılıc, S. Combined effects of nutritional status on long-term mortality in patients with non-st segment elevation myocardial infarction undergoing percutaneous coronary intervention. Rev. Assoc. Med. Bras. 2021, 67, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Sueta, D.; Hokimoto, S.; Sakamoto, K.; Naruse, M.; Ogawa, H. Validation of the high mortality rate of Malnutrition-Inflammation-Atherosclerosis syndrome: Community-based observational study. Int. J. Cardiol. 2017, 230, 97–102. [Google Scholar] [CrossRef]
- Bao, D.; Luo, G.; Kan, F.; Wang, X.; Luo, J.; Jiang, C. Prognostic value of red cell distribution width in patients undergoing percutaneous coronary intervention: A meta-analysis. BMJ Open 2020, 10, e033378. [Google Scholar] [CrossRef]
- He, F.; Huang, H.; Xu, W.; Cui, K.; Ruan, Y.; Guo, Y.; Wang, J.; Bin, J.; Wang, Y.; Chen, Y. Prognostic impact of malnutrition in patients with coronary artery disease: A systematic review and meta-analysis. Nutr. Rev. 2023, 82, 1013–1027. [Google Scholar] [CrossRef]
- Arero, G.; Arero, A.G.; Mohammed, S.H.; Vasheghani-Farahani, A. Prognostic Potential of the Controlling Nutritional Status (CONUT) Score in Predicting All-Cause Mortality and Major Adverse Cardiovascular Events in Patients With Coronary Artery Disease: A Meta-Analysis. Front. Nutr. 2022, 9, 850641. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; He, L.; Zhou, Y.; Man, C. Predictive Value of Geriatric Nutritional Risk Index in Patients With Coronary Artery Disease: A Meta-Analysis. Front. Nutr. 2021, 8, 736884. [Google Scholar] [CrossRef]
- Mullen, J.L.; Buzby, G.P.; Matthews, D.C.; Smale, B.F.; Rosato, E.F. Reduction of operative morbidity and mortality by combined preoperative and postoperative nutritional support. Ann. Surg. 1980, 192, 604–613. [Google Scholar] [CrossRef]
- Ma, S.; Zhang, B.; Lu, T.; Li, D.; Li, T.; Shen, Z.; He, C.; Wang, Y.; Li, B.; Zhang, H. Value of the prognostic nutritional index (PNI) in patients with newly diagnosed, CD5-positive diffuse large B-cell lymphoma: A multicenter retrospective study of the Huaihai Lymphoma Working Group. Cancer 2022, 128, 3487–3494. [Google Scholar] [CrossRef] [PubMed]
- Gremese, E.; Bruno, D.; Varriano, V.; Perniola, S.; Petricca, L.; Ferraccioli, G. Serum Albumin Levels: A Biomarker to Be Repurposed in Different Disease Settings in Clinical Practice. J. Clin. Med. 2023, 12, 6017. [Google Scholar] [CrossRef] [PubMed]
- Manolis, A.A.; Manolis, T.A.; Melita, H.; Mikhailidisd, D.P.; Manolis, A.S. Low serum albumin: A neglected predictor in patients with cardiovascular disease. Eur. J. Intern. Med. 2022, 102, 24–39. [Google Scholar] [CrossRef]
- Libby, P. Inflammation in Atherosclerosis-No Longer a Theory. Clin. Chem. 2021, 67, 131–142. [Google Scholar] [CrossRef]
- Zhu, L.; Chen, M.; Lin, X. Serum albumin level for prediction of all-cause mortality in acute coronary syndrome patients: A meta-analysis. Biosci. Rep. 2020, 40, BSR20190881. [Google Scholar] [CrossRef]
- Oduncu, V.; Erkol, A.; Karabay, C.Y.; Kurt, M.; Akgün, T.; Bulut, M.; Pala, S.; Kirma, C. The prognostic value of serum albumin levels on admission in patients with acute ST-segment elevation myocardial infarction undergoing a primary percutaneous coronary intervention. Coron. Artery Dis. 2013, 24, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, U.; Frantz, S. Role of lymphocytes in myocardial injury, healing, and remodeling after myocardial infarction. Circ. Res. 2015, 116, 354–367. [Google Scholar] [CrossRef] [PubMed]
- Demirtas, I.S.; Sunman, H.; Ibis, A.N.O.; Erzurum, M.; Özbeyaz, N.B.; Algül, E.; Gündüz, Y.; Pamukcu, H.E.; Gayretli, K.; Sahan, H.F. The role of prognostic nutritional index in patients with non-ST segment elevation acute coronary syndrome. Kardiologiia 2021, 61, 59–65. [Google Scholar] [CrossRef]
- Huang, Y.; Zhang, Q.; Li, P.; Chen, M.; Wang, R.; Hu, J.; Chi, J.; Cai, H.; Wu, N.; Xu, L. The prognostic nutritional index predicts all-cause mortality in critically ill patients with acute myocardial infarction. BMC Cardiovasc. Disord. 2023, 23, 339. [Google Scholar] [CrossRef]
- Chen, Q.J.; Qu, H.J.; Li, D.Z.; Li, X.-M.; Zhu, J.-J.; Xiang, Y.; Li, L.; Ma, Y.-T.; Yang, Y.-N. Prognostic nutritional index predicts clinical outcome in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Sci. Rep. 2017, 7, 3285. [Google Scholar] [CrossRef]
- Wada, H.; Dohi, T.; Miyauchi, K.; Jun, S.; Endo, H.; Doi, S.; Konishi, H.; Naito, R.; Tsuboi, S.; Ogita, M. Relationship between the prognostic nutritional index and long-term clinical outcomes in patients with stable coronary artery disease. J. Cardiol. 2018, 72, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.D.; Zheng, Y.Y.; Tang, J.N.; Wang, W.; Dai, X.-Y.; Zhang, J.-C.; Guo, Q.-Q.; Cheng, M.-D.; Song, F.-H.; Fan, L. Prognostic Nutritional Index as a Novel Predictor of Long-Term Prognosis in Patients with Coronary Artery Disease After Percutaneous Coronary Intervention. Clin. Appl. Thromb. Hemost. 2022, 28, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Talarico, M.; Manicardi, M.; Vitolo, M.; Malavasi, V.L.; Valenti, A.C.; Sgreccia, D.; Rossi, R.; Boriani, G. Red Cell Distribution Width and Patient Outcome in Cardiovascular Disease: A “Real-World” Analysis. J. Cardiovasc. Dev. Dis. 2021, 8, 120. [Google Scholar] [CrossRef] [PubMed]
- Liao, M.T.; Lai, C.L.; Wang, T.C.; Lin, J.-W.; Ho, Y.-L.; Chan, K.A. Red Cell Distribution Width and Mortality in Patients Undergoing Percutaneous Coronary Intervention. Biomedicines 2021, 10, 45. [Google Scholar] [CrossRef]


| Variable | All Participants (n = 5905) | Survival (n = 5370) | Non-Survival (n = 235) | p |
|---|---|---|---|---|
| Age, years | 66.0 [60.0, 73.0] | 66.0 [60.0, 72.0] | 73.0 [66.0, 80.0] | <0.001 |
| Male, n (%) | 3554 (63.4%) | 3397 (63.3%) | 157 (66.8%) | 0.300 |
| MI, n (%) | 1933 (34.5%) | 1780 (33.1%) | 153 (65.1%) | <0.001 |
| STEMI, n (%) | 1049 (18.7%) | 971 (18.1%) | 78 (33.2%) | <0.001 |
| Non-STEMI, n (%) | 884 (15.8%) | 809 (15.1%) | 75 (31.9%) | <0.001 |
| Pre-PCI, n (%) | 1254 (22.4%) | 1210 (22.5%) | 44 (18.7%) | 0.197 |
| Pre-MI, n (%) | 750 (13.4%) | 708 (13.2%) | 42 (17.9%) | 0.049 |
| Pre-AF, n (%) | 221 (3.94%) | 202 (3.76%) | 19 (8.09%) | 0.002 |
| Hypertension, n (%) | 4089 (73.0%) | 3897 (72.6%) | 192 (81.7%) | 0.003 |
| DM, n (%) | 2029 (36.2%) | 1930 (35.9%) | 99 (42.1%) | 0.063 |
| Dyslipidemia, n (%) | 654 (11.7%) | 630 (11.7%) | 24 (10.2%) | 0.544 |
| Pre-IS, n (%) | 829 (14.8%) | 768 (14.3%) | 61 (26.0%) | <0.001 |
| PAD, n (%) | 87 (1.55%) | 81 (1.51%) | 6 (2.55%) | 0.180 |
| CKD, n (%) | 247 (4.41%) | 201 (3.74%) | 46 (19.6%) | <0.001 |
| Current smoker, n (%) | 1499 (26.7%) | 1435 (26.7%) | 64 (27.2%) | 0.922 |
| Hb, g/L | 136 [124, 148] | 137 [125, 149] | 119 [97.0, 135] | <0.001 |
| Lmy, 109/L | 1.64 [1.23, 2.10] | 1.65 [1.25, 2.11] | 1.25 [0.88, 1.77] | <0.001 |
| RDW, % | 13.0 [12.6, 13.8] | 13.0 [12.6, 13.7] | 14.0 [13.1, 16.3] | <0.001 |
| UA, μmol/L | 344 [283, 410] | 343 [283, 408] | 373 [300, 486] | <0.001 |
| Cr, μmol/L | 74.7 [61.9, 93.9] | 74.1 [61.6, 91.9] | 105 [71.0, 215] | <0.001 |
| WBC, 109/L | 7.25 [5.96, 8.96] | 7.22 [5.95, 8.92] | 8.07 [6.11, 10.6] | <0.001 |
| TC, mmol/L | 4.55 [3.79, 5.26] | 4.56 [3.80, 5.28] | 4.32 [3.48, 4.98] | <0.001 |
| TG, mmol/L | 1.46 [1.05, 1.97] | 1.46 [1.06, 1.98] | 1.30 [0.93, 1.71] | <0.001 |
| LDL, mmol/L | 2.89 [2.26, 3.46] | 2.90 [2.26, 3.47] | 2.77 [2.10, 3.20] | 0.014 |
| Alb, g/L | 40.6 [38.0, 43.3] | 40.6 [38.3, 43.4] | 36.2 [33.2, 39.6] | <0.001 |
| PNI | 49.4 [45.8, 53.0] | 49.4 [46.0, 53.2] | 42.6 [38.7, 48.1] | <0.001 |
| Variable | All n = 5605 | H-PNI/H-RDW n = 1148 | H-PNI/L-RDW n = 3431 | L-PNI/L-RDW n = 612 | L-PNI/H-RDW n = 414 | p |
|---|---|---|---|---|---|---|
| Age, years | 66.0 [60.0, 73.0] | 65.0 [58.0, 71.0] | 66.0 [60.0; 72.0] | 70.0 [64.0, 78.0] | 66.0 [65.0, 78.0] | <0.001 |
| Male, n (%) | 3554 (63.4%) | 730 (63.6) | 2070 (62.0%) | 424 (69.3) | 269 (65.0) | 0.012 |
| MI, n (%) | 1933 (34.5%) | 446 (38.9%) | 873 (26.1%) | 332 (57.3%) | 239 (58.2%) | <0.001 |
| STEMI, n (%) | 1049 (18.7%) | 255 (22.2%) | 488 (14.6%) | 168 (29.0%) | 114 (27.7%) | <0.001 |
| Non-STEMI, n (%) | 884 (15.8%) | 191 (16.6%) | 385 (11.5%) | 164 (28.3%) | 125 (30.4%) | <0.001 |
| Pre-PCI, n (%) | 1254 (22.4%) | 234 (20.4%) | 758 (22.7%) | 128 (22.1%) | 86 (20.9%) | <0.001 |
| Pre-MI, n (%) | 750 (13.4%) | 149 (13.0%) | 414 (12.4%) | 81 (14.0%) | 82 (20.0%) | <0.001 |
| Pre-AF, n (%) | 221 (3.94%) | 56 (4.88%) | 90 (2.70%) | 35 (6.04%) | 34 (8.27%) | <0.001 |
| Hypertension, n (%) | 4089 (73.0%) | 827 (72.0%) | 2408 (72.1%) | 421 (72.7%) | 328 (79.8%) | 0.002 |
| DM, n (%) | 2029 (36.2%) | 407 (35.5%) | 1177 (35.3%) | 224 (38.7%) | 179 (43.6%) | 0.010 |
| Dyslipidemia, n (%) | 654 (11.7%) | 131 (11.4%) | 390 (11.7%) | 72 (12.4%) | 49 (11.9%) | 0.897 |
| Pre-IS, n (%) | 829 (14.8%) | 176 (15.3%) | 442 (13.2%) | 101 (17.4%) | 91 (22.1%) | <0.001 |
| PAD, n (%) | 87 (1.55%) | 29 (2.53%) | 38 (1.14%) | 9 (1.55%) | 11 (2.68%) | 0.003 |
| CKD, n (%) | 247 (4.41%) | 51 (4.44%) | 47 (1.41%) | 54 (9.33%) | 90 (21.9%) | <0.001 |
| Current smoker, n (%) | 1499 (26.7%) | 343 (29.9%) | 854 (25.6%) | 148 (25.6%) | 116 (28.2%) | 0.049 |
| Hb, g/L | 136 [124, 148] | 135 [121, 147] | 140 [130, 151] | 127 [112, 140] | 114 [95.0, 130] | <0.001 |
| Lym, 109/L | 1.64 [1.23, 2.10] | 1.77 [1.44, 2.30] | 1.76 [1.39, 2.19] | 1.05 [0.79, 1.31] | 1.04 [0.78, 1.35] | <0.001 |
| RDW, % | 13.0 [12.6, 13.8] | 16.4 [14.1, 41.1 | 12.8 [12.5, 13.1] | 12.8 [12.5, 13.1] | 15.2 [14.2, 41.7] | <0.001 |
| UA, μmol/L | 344 [283, 410] | 354 [288, 417] | 337 [281, 399] | 351 [283, 427] | 372 [299, 458] | <0.001 |
| Cr, μmol/L | 74.7 [61.9, 93.9] | 76.0 [62.2, 97.8] | 71.3 [60.7, 85.2] | 85.5 [66.2, 128] | 107 [74.3, 230] | <0.001 |
| WBC, 109/L | 7.25 [5.96, 8.96] | 7.76 [6.42, 9.43] | 7.05 [5.88, 8.63] | 7.12 [5.78, 9.54] | 7.40 [5.74, 9.36] | <0.001 |
| TC, mmol/L | 4.55 [3.79, 5.26] | 4.58 [3.88, 5.27] | 4.58 [3.84, 5.34] | 4.20 [3.56, 4.89] | 4.24 [3.58, 4.90] | <0.001 |
| TG, mmol/L | 1.46 [1.05, 1.97] | 1.54 [1.11, 2.01] | 1.50 [1.10, 2.06] | 1.20 [0.88, 1.67] | 1.23 [0.91, 1.71] | <0.001 |
| LDL, mmol/L | 2.89 [2.26, 3.46] | 2.91 [2.31, 3.49] | 2.91 [2.29, 3.52] | 2.64 [2.08, 3.26] | 2.67 [2.08, 3.13] | <0.001 |
| Alb, g/L | 40.6 [38.0, 43.3] | 40.6 [39.0, 42.8] | 41.8 [39.7, 44.4] | 35.8 [33.9, 37.7] | 34.9 [32.7, 37.0] | <0.001 |
| PNI | 49.4 [45.8, 53.0] | 49.4 [47.5, 53.1] | 50.8 [48.1, 54.2] | 41.7 [39.5, 43.0] | 40.9 [38.0, 42.6] | <0.001 |
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Age, per 1 year | 1.07 | 1.06, 1.09 | <0.001 | 1.05 | 1.03, 1.06 | <0.001 |
| Age ≥ 65 | 2.86 | 2.11, 3.85 | <0.001 | 2.13 | 1.76, 3.06 | <0.001 |
| Sex, male as reference | 0.86 | 0.66, 1.13 | 0.300 | |||
| MI | 3.68 | 2.82, 4.82 | <0.001 | 2.20 | 1.66, 2.91 | <0.001 |
| Pre-MI | 1.42 | 1.02, 1.99 | 0.039 | |||
| Pre-AF | 2.20 | 1.37, 3.51 | 0.001 | |||
| Hypertension | 1.67 | 1.20, 2.33 | 0.002 | |||
| DM | 1.29 | 1.00, 1.68 | 0.052 | |||
| Dyslipidemia | 0.86 | 0.56, 1.30 | 0.500 | |||
| Pre-IS | 2.06 | 1.54, 2.76 | <0.001 | 1.52 | 1.13, 2.04 | 0.005 |
| PAD | 1.69 | 0.75, 3.79 | 0.200 | |||
| CKD | 5.75 | 4.17, 7.94 | <0.001 | 1.83 | 1.28, 2.62 | <0.001 |
| Current smoker | 1.03 | 0.77, 1.37 | 0.800 | |||
| RDW, RDW ≤ 13.6 as reference | 3.49 | 2.69, 4.53 | <0.001 | |||
| PNI, PNI > 44.2 as reference | 6.92 | 5.34, 8.98 | <0.001 | |||
| Hb, Hb ≤ 90 g/L as reference | 0.11 | 0.08, 016 | <0.001 | 0.42 | 0.28, 0.59 | <0.001 |
| Hb | 0.96 | 0.96, 0.97 | <0.001 | |||
| Alb | 0.82 | 0.81, 0.84 | <0.001 | 0.94 | 0.91, 0.97 | <0.001 |
| H-PNI/L-RDW | - | |||||
| L-PNI/L-RDW | 7.73 | 4.88, 10.86 | <0.001 | 3.96 | 2.60, 6.00 | <0.001 |
| H-PNI/H-RDW | 3.68 | 2.45, 5.50 | <0.001 | 3.00 | 1.99, 4.50 | <0.001 |
| L-PNI/H-RDW | 18.50 | 12.83, 26.68 | <0.001 | 8.85 | 5.96, 13.15 | 0.020 |
| Outcome | Events/Total | Crude HR (95% CI) | p | Adjusted HR (95% CI) | p |
|---|---|---|---|---|---|
| 1-year ACM | 235/5605 | ||||
| H-PNI/L-RDW | 43/3431 | reference | reference | ||
| H-PNI/H-RDW | 52/1148 | 3.68 (2.45, 5.50) | <0.001 | 3.00 (1.99, 4.50) | <0.001 |
| L-PNI/L-RDW | 54/612 | 7.73 (4.88, 10.86) | <0.001 | 3.96 (2.60, 6.00) | <0.00 |
| L-PNI/R-RDW | 86/414 | 18.5 (12.83, 26.68) | <0.001 | 8.85 (5.96, 13.15) | 0.02 |
| MACCEs | 560/5605 | ||||
| H-PNI/L-RDW | 219/3431 | reference | reference | ||
| H-PNI/H-RDW | 144/1148 | 2.04 (1.65, 2.52) | <0.001 | 1.81 (1.46, 2.24) | <0.001 |
| L-PNI/L-RDW | 92/612 | 2.49 (1.96, 3.18) | <0.001 | 1.74 (1.35, 2.25) | <0.001 |
| L-PNI/R-RDW | 105/414 | 4.49 (3.56, 5.68) | <0.001 | 2.74 (2.12, 3.54) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huo, L.; Zhao, W.; Ji, X.; Chen, K.; Liu, T. The Combination Effect of the Red Blood Cell Distribution Width and Prognostic Nutrition Index on the Prognosis in Patients Undergoing PCI. Nutrients 2024, 16, 3176. https://doi.org/10.3390/nu16183176
Huo L, Zhao W, Ji X, Chen K, Liu T. The Combination Effect of the Red Blood Cell Distribution Width and Prognostic Nutrition Index on the Prognosis in Patients Undergoing PCI. Nutrients. 2024; 16(18):3176. https://doi.org/10.3390/nu16183176
Chicago/Turabian StyleHuo, Likun, Wenjuan Zhao, Xiang Ji, Kangyin Chen, and Tong Liu. 2024. "The Combination Effect of the Red Blood Cell Distribution Width and Prognostic Nutrition Index on the Prognosis in Patients Undergoing PCI" Nutrients 16, no. 18: 3176. https://doi.org/10.3390/nu16183176
APA StyleHuo, L., Zhao, W., Ji, X., Chen, K., & Liu, T. (2024). The Combination Effect of the Red Blood Cell Distribution Width and Prognostic Nutrition Index on the Prognosis in Patients Undergoing PCI. Nutrients, 16(18), 3176. https://doi.org/10.3390/nu16183176






