Joint Trajectories of Lifestyle Indicators and Their Associations with Blood Pressure among Chinese Middle School Students
Abstract
1. Introduction
2. Materials and Methods
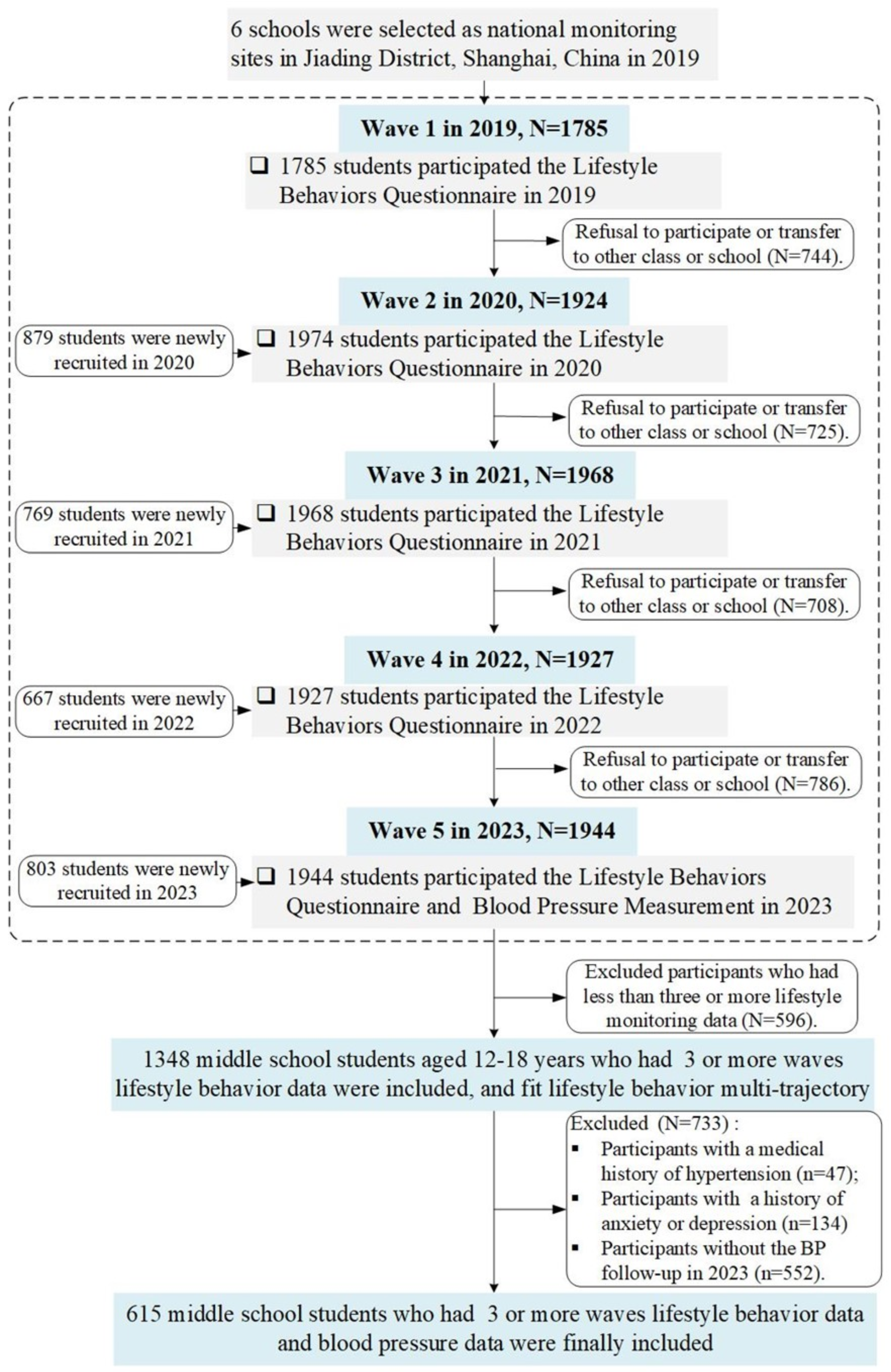
2.1. Study Design and Participants
2.2. Lifestyle Behavior Measurement
2.2.1. Dietary Behavior Score
2.2.2. PA
2.2.3. ST
2.2.4. Sleep Duration
2.3. Identifing Joint Trajectories of Lifestyle Behaviors
2.4. Students’ BP
2.5. Covariates
2.6. Statistical Analysis
2.6.1. Sociodemographic Characteristics across Trajectory Groups
2.6.2. Associations between Students’ Lifestyle Trajectories and Later BP
3. Results
3.1. Characteristics of Lifestyle Trajectories
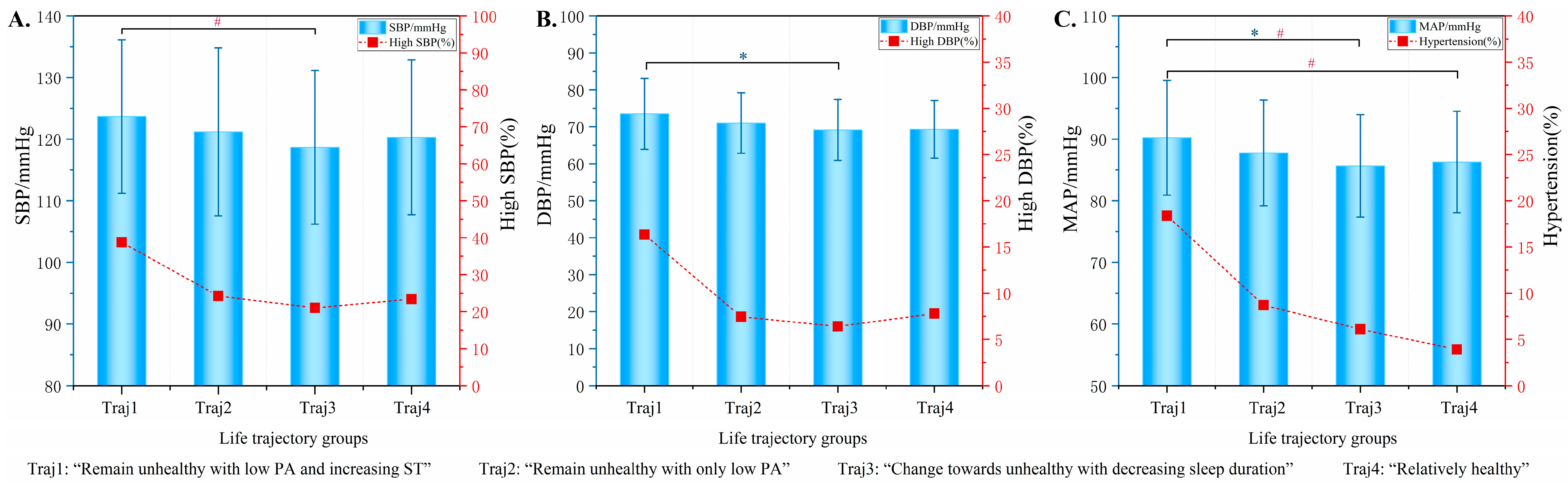
3.2. Associations between Students’ Lifestyle Trajectories and Later BP
3.3. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [CrossRef]
- Zhou, B.; Perel, P.; Mensah, G.A.; Ezzati, M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat. Rev. Cardiol. 2021, 18, 785–802. [Google Scholar] [CrossRef]
- Noubiap, J.J.; Essouma, M.; Bigna, J.J.; Jingi, A.M.; Aminde, L.N.; Nansseu, J.R. Prevalence of elevated blood pressure in children and adolescents in Africa: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e375–e386. [Google Scholar] [CrossRef]
- Song, P.; Zhang, Y.; Yu, J.; Zha, M.; Zhu, Y.; Rahimi, K.; Rudan, I. Global Prevalence of Hypertension in Children: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019, 173, 1154–1163. [Google Scholar] [CrossRef]
- Hardy, S.T.; Urbina, E.M. Blood Pressure in Childhood and Adolescence. Am. J. Hypertens. 2021, 34, 242–249. [Google Scholar] [CrossRef]
- Liu, K.; Li, C.; Gong, H.; Guo, Y.; Hou, B.; Chen, L.; Liu, F.; Liu, Y.; Wang, J.; Hou, Q.; et al. Prevalence and Risk Factors for Hypertension in Adolescents Aged 12 to 17 Years: A School-Based Study in China. Hypertension 2021, 78, 1577–1585. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wang, Y. Tracking of blood pressure from childhood to adulthood: A systematic review and meta-regression analysis. Circulation 2008, 117, 3171–3180. [Google Scholar] [CrossRef] [PubMed]
- Königstein, K.; Büschges, J.C.; Schmidt-Trucksäss, A.; Neuhauser, H. Cardiovascular Risk in Childhood is Associated With Carotid Intima-Media Thickness and Stiffness in Adolescents and Young Adults: The KiGGS Cohort. J. Adolesc. Health 2024, 74, 123–129. [Google Scholar] [CrossRef]
- Högström, G.; Nordström, A.; Eriksson, M.; Nordström, P. Risk factors assessed in adolescence and the later risk of stroke in men: A 33-year follow-up study. Cerebrovasc. Dis. 2015, 39, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Lili, Y.; Chuanwei, M.; Yajun, L.; Bo, X. Effect of sugar-sweetened beverage consumption on blood pressure among Chinese children and adolescents. Chin. J. Sch. Health 2016, 37, 1456–1459. [Google Scholar] [CrossRef]
- Chen, J.; Wang, Y.; Li, W.; Zhang, Y.; Cao, R.; Peng, X.; Zhang, J.; Liu, K.; Han, M.; Fu, L. Physical activity and eating behaviors patterns associated with high blood pressure among Chinese children and adolescents. BMC Public Health 2023, 23, 1516. [Google Scholar] [CrossRef] [PubMed]
- Krupp, D.; Shi, L.; Egert, S.; Wudy, S.A.; Remer, T. Prospective relevance of fruit and vegetable consumption and salt intake during adolescence for blood pressure in young adulthood. Eur. J. Nutr. 2015, 54, 1269–1279. [Google Scholar] [CrossRef]
- Gopinath, B.; Hardy, L.L.; Teber, E.; Mitchell, P. Association between physical activity and blood pressure in prepubertal children. Hypertens. Res. 2011, 34, 851–855. [Google Scholar] [CrossRef]
- Morgan, T.; Basalely, A.; Singer, P.; Castellanos, L.; Sethna, C.B. The association between sleep duration and cardiometabolic risk among children and adolescents in the United States (US): A NHANES study. Child Care Health Dev. 2024, 50, e13273. [Google Scholar] [CrossRef] [PubMed]
- Farhangi, M.A.; Fathi Azar, E.; Manzouri, A.; Rashnoo, F.; Shakarami, A. Prolonged screen watching behavior is associated with high blood pressure among children and adolescents: A systematic review and dose–response meta-analysis. J. Health Popul. Nutr. 2023, 42, 89. [Google Scholar] [CrossRef] [PubMed]
- Chia, A.; Toh, J.Y.; Natarajan, P.; Cai, S.; Ong, Y.Y.; Descarpentrie, A.; Lioret, S.; Bernard, J.Y.; Müller-Riemenschneider, F.; Godfrey, K.M.; et al. Trajectories of lifestyle patterns from 2 to 8 years of age and cardiometabolic risk in children: The GUSTO study. Int. J. Behav. Nutr. Phys. Act. 2024, 21, 9. [Google Scholar] [CrossRef]
- Zhang, A.; Fang, J.; Wan, Y.; Su, P.; Tao, F.; Sun, Y. Joint trajectories of life style indicators and their links to psychopathological outcomes in the adolescence. BMC Psychiatry 2021, 21, 407. [Google Scholar] [CrossRef]
- Doggui, R.; Ward, S.; Johnson, C.; Belanger, M. Trajectories of Eating Behaviour Changes during Adolescence. Nutrients 2021, 13, 1313. [Google Scholar] [CrossRef]
- Cosier, D.; Charlton, K.; Schoenaker, D.A.J.M. The association between dietary trajectories across childhood and blood pressure in early adolescence: The Longitudinal Study of Australian Children. Eur. J. Clin. Nutr. 2023, 77, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Gallant, F.; Sylvestre, M.P.; O’Loughlin, J.; Bélanger, M. Teenage Sport Trajectory Is Associated With Physical Activity, but Not Body Composition or Blood Pressure in Early Adulthood. J. Adolesc. Health 2022, 71, 119–126. [Google Scholar] [CrossRef]
- Trude, A.C.B.; Armstrong, B.; Kramer Fiala Machado, A.; Wickwire, E.M.; Covington, L.B.; Wang, Y.; Hager, E.; Black, M.M. Waking up to sleep’s role in obesity and blood pressure among Black adolescent girls in low-income, US urban communities: A longitudinal analysis. Sleep Health 2022, 8, 200–207. [Google Scholar] [CrossRef]
- Garcidueñas-Fimbres, T.E.; Gómez-Martínez, C.; Pascual-Compte, M.; Jurado-Castro, J.M.; Leis, R.; Moreno, L.A.; Navas-Carretero, S.; Codoñer-Franch, P.; Echeverria, A.M.; Pastor-Villaescusa, B.; et al. Adherence to a healthy lifestyle behavior composite score and cardiometabolic risk factors in Spanish children from the CORALS cohort. Eur. J. Pediatr. 2024, 183, 1819–1830. [Google Scholar] [CrossRef]
- Mao, B.; Yang, Y.; Fan, Z.; Li, Y.; Xiang, W.; Dong, B.; Hu, J. Association of a healthy lifestyle with ambulatory 24-hour blood pressure among Chinese youths: A cross-sectional study. Am. J. Hypertens. 2024, 37, 674–681. [Google Scholar] [CrossRef] [PubMed]
- Falkner, B.; Lurbe, E. Primordial Prevention of High Blood Pressure in Childhood: An Opportunity Not to be Missed. Hypertension 2020, 75, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Circular of the General Office of the National Health Commission ofthe PRC on Issuing the 2019 National Monitoring and Intervention of Common Diseases and Health Influencing Factors among Students [EB/OL]. 26 March 2019. Available online: http://www.nhc.gov.cnjkj/s5898bm/201903/1bcbac21e1864377ad24984fac01c7d.shtml (accessed on 5 July 2024).
- Zhang, N.; Zhu, W.; Zhang, M.; Ma, G. Interpretation on Dietary Guidelines for Chinese School-aged Children in 2022. Chin. J. Sch. Health 2022, 43, 805–808. [Google Scholar] [CrossRef]
- Nagin, D.S.; Jones, B.L.; Passos, V.L.; Tremblay, R.E. Group-based multi-trajectory modeling. Stat. Methods Med. Res. 2018, 27, 2015–2023. [Google Scholar] [CrossRef]
- Joint Committee for Guideline, R. 2018 Chinese Guidelines for Prevention and Treatment of Hypertension-A report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J. Geriatr. Cardiol. 2019, 16, 182–241. [Google Scholar] [CrossRef]
- Du, B.; Wang, H.; Wu, Y.; Li, Z.; Niu, Y.; Wang, Q.; Zhang, L.; Chen, S.; Wu, Y.; Huang, J.; et al. The association of gestational age and birthweight with blood pressure, cardiac structure, and function in 4 years old: A prospective birth cohort study. BMC Med. 2023, 21, 103. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Ma, J.; Song, Y.; Dong, B.; Wang, Z.; Yang, Z.; Wang, X.; Prochaska, J.J. National Blood Pressure Reference for Chinese Han Children and Adolescents Aged 7 to 17 Years. Hypertension 2017, 70, 897–906. [Google Scholar] [CrossRef]
- Cui, L.; Li, J.; Lou, X.; Yang, L.; Chen, T.; Guo, Y.; Zhou, H.; Yang, X.; Li, Z.; Wang, X. Associations between sleep characteristics and risk for high blood pressure among students aged 9-18: A cross-sectional study in China. Sleep Med. 2023, 107, 72–80. [Google Scholar] [CrossRef]
- Blodgett, J.M.; Ahmadi, M.N.; Atkin, A.J.; Chastin, S.; Chan, H.-W.; Suorsa, K.; Bakker, E.A.; Hettiarcachchi, P.; Johansson, P.J.; Sherar, L.B.; et al. Device-measured physical activity and cardiometabolic health: The Prospective Physical Activity, Sitting, and Sleep (ProPASS) consortium. Eur. Heart J. 2024, 45, 458–471. [Google Scholar] [CrossRef]
- Buckland, G.; Northstone, K.; Emmett, P.M.; Taylor, C.M. The inflammatory potential of the diet in childhood is associated with cardiometabolic risk in adolescence/young adulthood in the ALSPAC birth cohort. Eur. J. Nutr. 2022, 61, 3471–3486. [Google Scholar] [CrossRef]
- Zhao, W.; Su, D.; Mo, L.; Chen, C.; Ye, B.; Qin, S.; Liu, J.; Pang, Y. Lifestyle Clusters and Cardiometabolic Risks in Adolescents: A Chinese School-Based Study Using a Latent Class Analysis Approach. Front. Pediatr. 2021, 9, 728841. [Google Scholar] [CrossRef] [PubMed]
- Cortes, C.; Brandão, J.M.; Cunha, D.B.; Paravidino, V.B.; Sichieri, R. Blood pressure variation and ultra-processed food consumption in children with obesity. Eur. J. Pediatr. 2023, 182, 4077–4085. [Google Scholar] [CrossRef]
- Oliveira, T.; Ribeiro, I.; Jurema-Santos, G.; Nobre, I.; Santos, R.; Rodrigues, C.; Oliveira, K.; Henrique, R.; Ferreira-E-Silva, W.; Araújo, A. Can the Consumption of Ultra-Processed Food Be Associated with Anthropometric Indicators of Obesity and Blood Pressure in Children 7 to 10 Years Old? Foods 2020, 9, 1567. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Wong, F.K.Y. The Association Between Time Spent in Sedentary Behaviors and Blood Pressure: A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 867–880. [Google Scholar] [CrossRef]
- Nagata, J.M.; Weinstein, S.; Alsamman, S.; Lee, C.M.; Dooley, E.E.; Ganson, K.T.; Testa, A.; Gooding, H.C.; Kiss, O.; Baker, F.C.; et al. Association of physical activity and screen time with cardiovascular disease risk in the Adolescent Brain Cognitive Development Study. BMC Public Health 2024, 24, 1346. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; He, M.; Zhang, M.; Chu, Y.; Ban, B. Non-linear relationship between sleep duration and blood pressure in children with short stature. Front. Pediatr. 2023, 11, 1302750. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Lioret, S.; Hesketh, K.D.; Spence, A.; Taylor, R.; Campbell, K.J. Association Between Longitudinal Trajectories of Lifestyle Pattern and BMI in Early Childhood. Obesity 2021, 29, 879–887. [Google Scholar] [CrossRef]
- Hanson, S.K.; Munthali, R.J.; Micklesfield, L.K.; Lobelo, F.; Cunningham, S.A.; Hartman, T.J.; Norris, S.A.; Stein, A.D. Longitudinal patterns of physical activity, sedentary behavior and sleep in urban South African adolescents, Birth-To-Twenty Plus cohort. BMC Pediatr. 2019, 19, 241. [Google Scholar] [CrossRef]
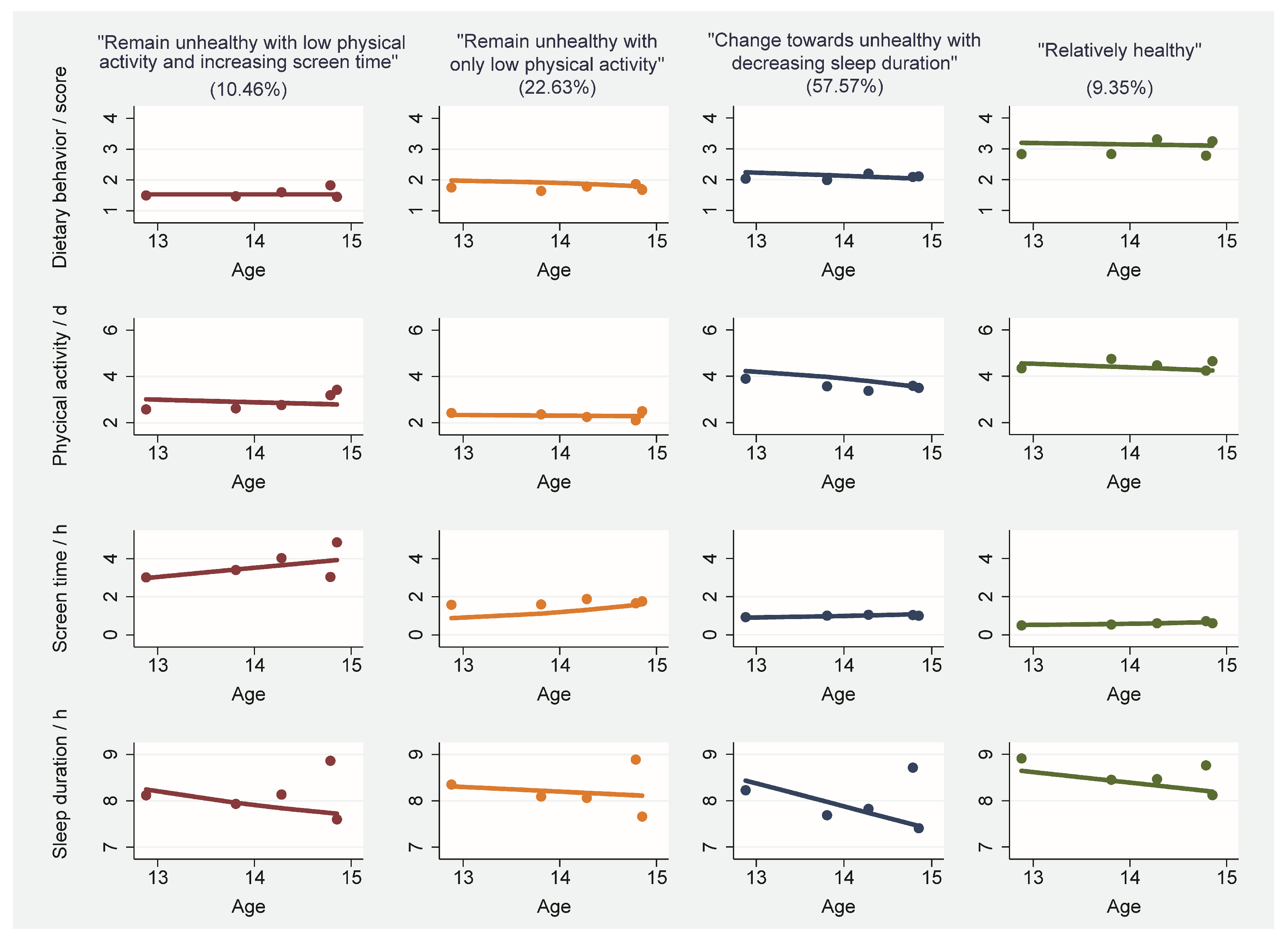

| Characteristic | Overall | “Remain Unhealthy with Low PA and Increasing ST” | “Remain Unhealthy with Only Low PA” | “Change towards Unhealthy with Decreasing Sleep Duration” | “Relatively Healthy” | p |
|---|---|---|---|---|---|---|
| N | 1348 | 141 (10.46) | 305 (22.63) | 776 (57.57) | 126 (9.35) | |
| Sex (%) | ||||||
| Boys | 795 (58.98) | 103 (73.05) | 202 (66.23) | 417 (53.74) | 73 (57.94) | <0.001 |
| Girls | 553 (41.02) | 38 (26.95) | 103 (33.77) | 359 (46.26) | 53 (42.06) | |
| Age (median [IQR]) | 14.36 [13.30, 17.28] | 13.69 [12.69, 17.20] | 17.07 [14.14, 17.58] | 13.96 [12.88, 14.99] | 14.48 [13.48, 17.09] | <0.001 |
| Self-perceived family income (%) | ||||||
| Fine | 506 (37.54) | 27 (19.15) | 114 (37.38) | 308 (39.69) | 57 (45.24) | <0.001 |
| Poor | 842 (62.46) | 114 (80.85) | 191 (62.62) | 468 (60.31) | 69 (54.76) | |
| Maternal education (%) | ||||||
| Junior high school or below | 323 (23.96) | 74 (52.48) | 85 (27.87) | 143 (18.43) | 21 (16.67) | <0.001 |
| High school | 251 (18.62) | 23 (16.31) | 53 (17.38) | 155 (19.97) | 20 (15.87) | |
| College degree or above | 774 (57.42) | 44 (31.21) | 167 (54.75) | 478 (61.60) | 85 (67.46) | |
| n | 615 | 49 (8.01) | 161 (26.31) | 328 (53.59) | 77 (12.68) | |
| BMI (median [IQR]) | 20.36 [17.88, 24.07] | 19.70 [17.40, 23.85] | 20.86 [18.36, 24.24] | 20.07 [17.70, 23.89] | 20.99 [18.44, 23.74] | 0.172 |
| SBP (mean [SD]) | 119.93 (12.86) | 123.67 (12.46) | 121.18 (13.63) | 118.67 (12.47) | 120.29 (12.58) | 0.031 |
| DBP (mean [SD]) | 70.01 (8.36) | 73.51 (9.59) | 71.04 (8.17) | 69.15 (8.23) | 69.30 (7.80) | 0.002 |
| MAP (mean [SD]) | 86.65 (8.55) | 90.23 (9.32) | 87.76 (8.58) | 85.66 (8.31) | 86.29 (8.25) | 0.001 |
| High SBP (%) | ||||||
| Normal | 470 (76.42) | 30 (61.22) | 122 (75.78) | 259 (78.96) | 59 (76.62) | 0.060 |
| High SBP | 145 (23.58) | 19 (38.78) | 39 (24.22) | 69 (21.04) | 18 (23.38) | |
| High DBP (%) | ||||||
| Normal | 568 (92.36) | 41 (83.67) | 149 (92.55) | 307 (93.60) | 71 (92.21) | 0.110 |
| High DBP | 47 (7.64) | 8 (16.33) | 12 (7.45) | 21 (6.40) | 6 (7.79) | |
| Hypertension (%) | ||||||
| Normal | 569 (92.52) | 40 (81.63) | 147 (91.30) | 308 (93.90) | 74 (96.10) | 0.010 |
| Hypertension | 46 (7.48) | 9 (18.37) | 14 (8.70) | 20 (6.10) | 3 (3.90) | |
| Lifestyle Trajectory Groups | SBP | DBP | MAP | |||
|---|---|---|---|---|---|---|
| β (95% CI) | p | β (95% CI) | p | β (95% CI) | p | |
| “Relatively healthy” | Reference | Reference | Reference | |||
| “Change towards unhealthy with decreasing sleep duration” | −0.68 (−3.41, 2.06) | 0.628 | −0.05 (−2.07, 1.97) | 0.964 | −0.26 (−2.19, 1.68) | 0.795 |
| “Remain unhealthy with only low PA” | 0.02 (−2.98, 3.03) | 0.987 | 1.32 (−0.90, 3.54) | 0.243 | 0.89 (−1.24, 3.01) | 0.412 |
| “Remain unhealthy with low PA and increasing ST” | 2.58 (−1.41, 6.57) | 0.205 | 3.49 (0.55, 6.44) | 0.020 | 3.19 (0.37, 6.01) | 0.027 |
| p for trend | 0.200 | 0.006 | 0.012 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jing, G.; Liu, X.; Shi, J.; Xue, J.; Peng, H.; Shi, H. Joint Trajectories of Lifestyle Indicators and Their Associations with Blood Pressure among Chinese Middle School Students. Nutrients 2024, 16, 2994. https://doi.org/10.3390/nu16172994
Jing G, Liu X, Shi J, Xue J, Peng H, Shi H. Joint Trajectories of Lifestyle Indicators and Their Associations with Blood Pressure among Chinese Middle School Students. Nutrients. 2024; 16(17):2994. https://doi.org/10.3390/nu16172994
Chicago/Turabian StyleJing, Guangzhuang, Xinxin Liu, Jiaojiao Shi, Junlei Xue, Hui Peng, and Huijing Shi. 2024. "Joint Trajectories of Lifestyle Indicators and Their Associations with Blood Pressure among Chinese Middle School Students" Nutrients 16, no. 17: 2994. https://doi.org/10.3390/nu16172994
APA StyleJing, G., Liu, X., Shi, J., Xue, J., Peng, H., & Shi, H. (2024). Joint Trajectories of Lifestyle Indicators and Their Associations with Blood Pressure among Chinese Middle School Students. Nutrients, 16(17), 2994. https://doi.org/10.3390/nu16172994








